Abstract
A combination of forces have markedly increased challenges to research-active faculty achieving sustained success. This article describes how one department at the University of Cincinnati College of Medicine (UCCOM) implemented a strategic plan, the Research Initiative Supporting Excellence at the University of Cincinnati (RISE-UC), to promote the research activity of its research-active faculty, fiscal year (FY) 2011–FY 2021. RISE-UC was implemented and regularly updated to address evolving needs. RISE-UC supported faculty members pursuing research via fiscal and administrative services to grow a critical mass of investigators; establish a shared governance model; create pathways for developing physician–scientists; develop discrete and targeted internal research funding; establish an Academic Research Service (ARS) unit (as infrastructure to support research); enhance faculty member mentorship; and recognize, celebrate, and reward research success. RISE-UC was informed by shared governance and resulted in substantial increases in total size of the faculty and external funding. More than 50% of Physician-Scientist Training Program graduates are active researchers at UCCOM. The internal awards program realized a return on investment of ~16.4-fold, and total external direct cost research funds increased from ~$55,400,000 (FY 2015) to ~$114,500,000 (FY 2021). The ARS assisted in the submission of 57 grant proposals and provided services faculty members generally found very helpful or helpful. The peer-mentoring group for early-career faculty members resulted in 12 of 23 participants receiving major grant funding (≥ $100,000; spring 2017–spring 2021) from sources including National Institutes of Health awards, Department of Defense funding, Veterans Affairs funding, and foundation awards. Research recognition included ~$77,000/year in incentive payments to faculty members for grant submissions and grants awarded. RISE-UC is an example of a comprehensive approach to promote research faculty member success and may serve as a model for other institutions with similar aspirations.
Traditionally, research in academic medical centers has been pursued by individual investigators working on mostly independent projects confined to their basic, translational, clinical, health care outcomes, or educational laboratories.1 Although such work required investment from the institution, sustaining a successful research career meant primarily being supported by external funding,2 and robust tenure systems rewarded success and provided employment stability.3 However, a combination of forces have markedly increased the prerequisites for research-active faculty members to sustain success.4,5
These challenges include a longer duration of sophisticated training to become competitive for external funding,6 increase in debt burdens,7 increasingly uncertain research funding,8,9 higher demands of board certification,10 increased regulatory burden,11–13 insufficient mentoring plans,14 work–life imbalance,15 and health care system economics that favor higher patient care volumes at the expense of protected research time.16 Moreover, unexpected developments, such as the COVID-19 pandemic, provide further challenges to a successful research career.17 As a stark manifestation of these trends, the average age at the time of receiving a first National Institutes of Health (NIH) R01 award for a principal investigator with an MD degree increased from less than 38 years old in 1980 to more than 45 years old in 2013.6 Correspondingly, the percent of R01 principal investigators who were 36 years old or younger decreased to 3% of all R01 principal investigators in 2010 from 18% in 1983.6 Qualitatively similar trends are observed for principal investigators with PhD degrees.6 The consequences of these challenges are not only a weakening of the ability of academic departments to sustain a thriving research mission but also more generally a threat to the viability of the nation’s research competitiveness.18
This article describes how a specific Department of Internal Medicine (DOIM) implemented a strategic plan engaging all faculty members and addressing the tripartite mission of patient care, education, and research to promote, in particular, a thriving research environment despite many challenges. Specifically, we describe the efforts of the DOIM at the University of Cincinnati College of Medicine (UCCOM; ranked 43rd research medical school in the 2021 U.S. News & World Report) to sustain and grow the research activity of its faculty during fiscal year (FY) 2011 to FY 2021. The efforts were guided by a core set of objectives (see below), but the process was intentionally iterative to enable programs to be created and modified, consistent with models of change, such as the Institute for Healthcare Improvement’s Breakthrough Series approach.19
Strategic Plan, Structure, and Objectives
Needs assessment and departmental research objectives
Before 2011, the DOIM had significant strengths. These included the nationally recognized prowess of its graduate medical education programs. However, the number of PhDs and clinical scientists, in addition to support infrastructure for research activities, had waned over the previous decade, as both the UCCOM and university had transitioned through several leadership changes. Despite a departmental loan repayment program, start-up packages for new faculty members, a departmental bridge funding program, a training program for physician–scientists, and college- and university-level support programs, research-active faculty members reported feeling undervalued and unsupported. Additionally, there was a perception that research was not a departmental priority due to unaddressed challenges, such as inadequate protected time and excessive administrative burdens.
We developed a strategic plan (see below) with set objectives that took into account the strengths and weaknesses of the DOIM and also flattened the hierarchy of the administrative leadership of the department. In 2011, the incoming department chair, who had been a faculty member in the department for many decades and was well aware of its history and mission, led a disciplined and deliberate strengths, weaknesses, opportunities, and threats analysis. This analysis was performed in conjunction with a new senior executive non-MD leader. Consultations were held with the associate chairs and division directors to develop a strategic plan based on the tripartite mission and outcomes of the analysis. The mission-based strategic plan needed to not only provide tangible financial resources to promising investigators but also aid our current and future faculty members to thrive in all aspects of their careers. Although the primary focus of the strategic plan was research support, the interrelated nature of a tripartite mission led to the identification of the following objectives:
Grow the critical mass of investigators through strategic recruitment and increasing faculty member engagement and support.
Establish a shared governance model using governance committees for each component of the tripartite mission (e.g., the Research Governance Committee [RGC]; see below) and a fourth finance executive committee.
Devise a strategy to develop and train physician–scientists within our medical student, residency, and fellowship programs to create pathways for future faculty member recruitment.
Develop discrete and targeted mechanisms to dispense internal funding through pilot awards to support faculty members and trainees in purposeful ways, promote collaboration between divisions and departments, and cultivate innovative ideas that lead to external funding.
Establish an Academic Research Services (ARS) unit to serve as infrastructure to support research through regulatory services, laboratory services, financial services, and grantsmanship training.
Enhance faculty member mentorship at all levels using individual development plans (IDPs) and multiple mentoring approaches.
Recognize, celebrate, and reward research success across the department for the faculty, staff, and trainees.
These objectives were coalesced into a single strategic plan called the Research Initiative Supporting Excellence at the University of Cincinnati (RISE-UC), which was iteratively revised and implemented over several years to address evolving needs (Figure 1).
Figure 1.
Timeline of Research Initiative Supporting Excellence at the University of Cincinnati (RISE-UC) activities summarizing many of the significant programmatic additions from 2011 through 2021, University of Cincinnati College of Medicine (UCCOM) Department of Internal Medicine (DOIM). Abbreviations: NIH, National Institutes of Health; ARS, Academic Research Services; IMSTAR, Internal Medicine Scholarly Training for Academic Research; UC A&F, University of Cincinnati Accounting & Finance.
Recognizing that these objectives would require direct or indirect financial support, we scrutinized the use of endowments, indirect revenues from grants, general funds, and other philanthropic sources and funds. On average, indirect support to the DOIM was ~20% of the total indirect support awarded to the university from extramural grants that had DOIM principal investigators (e.g., in FY 2021, the department received 21.6% of indirect support awarded to the university). In addition, unobligated departmental funds from the department’s overall budget were earmarked to support research. In 2011, a financial review process was implemented annually to identify existing and new funding sources. By diversifying funding sources in this manner, we were able to acquire a stable set of funds to sustain investment in research.
RISE-UC was also structured to align with UCCOM’s overall goals and the strengths of its existing and emerging programs. We were particularly careful to support a broad array of emerging researchers in basic, translational, clinical, health care outcomes, and educational research areas. The DOIM leadership, division directors, and the RGC identified broad and specific programmatic areas in which to recruit new faculty members and support the research mission; this process was also iterative.
Growing a critical mass of investigators
Our assessment of highly productive research activity within other DOIMs suggested a total faculty size of ~350–400 would be needed (clinicians, researchers, and clinician–educators) to sustain a robust research mission. This would enable balancing of clinical responsibilities among clinicians, clinician–educators, and clinician–scientists, allowing research-oriented faculty members to have protected time for research. In addition, increasing the generation of clinical revenues would allow some funds to be earmarked for investment in research. Each division director was asked to hire academic clinicians, while identifying specific research needs that could be addressed through targeted recruitment for tenure research tracks, nontenure research tracks, and nontenure clinician–scholar tracks over the duration of RISE-UC.
Establishing a shared governance model
To sustain a dynamic and responsive strategic plan,20 the RGC was implemented, which included 2–3 researchers (MDs and PhDs) from each of the 9 divisions and administrative staff. Diverse demographic representation was sought; membership was 39% female, 2% Black, 2% Hispanic/Latino, and 21% Asian/South Asian. The mandate of the RGC, under the direction of the associate chairs for research, was to advise the departmental leadership on research priorities and to monitor and evaluate progress. The focus of the RGC was on strengthening basic, translational, clinical, and health care outcomes research infrastructure; developing mechanisms to encourage and strengthen collaborative interdisciplinary research; and engaging government, industry, and community support of research. The underlying organizational principles of the RGC were based, in part, on well-established concepts of shared governance.21–24
Creating pathways for developing physician–scientists
Developing pathways for new researchers is critical to sustaining research in most departments. Several mechanisms were initiated before RISE-UC and strengthened during its implementation. There were 3 main mechanisms used to identify promising candidates for an academic career and foster their career development. The first mechanism (initiated in 2005, before RISE-UC) was an optional “long block” that was available to all residents from early in the second year through early in the third year of residency.25 This block consisted of 12 months of consecutive non-service-related rotations that included an optional mentored research experience. This experience included up to 3 months of research concentrated during the long block as part of the 4 total months of research allowed by the Accreditation Council for Graduate Medical Education (ACGME) requirements. Although the definition of scholarly activity as defined by ACGME is broad, the scholarly activity that was required of the residents was redefined in the department to include only research and quality improvement projects. A second, more intensive, mechanism (established in 2006, again before RISE-UC) called the Physician-Scientist Training Program (PSTP) was available for all residents to apply to and was based on the American Board of Internal Medicine Research Pathway guidelines,20 which had been demonstrated to effectively meet the goal of training biomedical scientists.26 The PSTP included an abbreviated internal medicine residency followed by integrated fellowship and research training. Participants typically spent 2 years in internal medicine residency training (with up to 2 months of elective rotation time replaceable with research time), 2–3 years in fellowship training (guaranteed admission upon successful completion of residency), and 3 years conducting laboratory or clinical subspecialty research with 80% protected time for research. The third mechanism was the Internal Medicine Scholarly Training for Academic Research (IMSTAR) fellowship program initiated in FY 2015 as a component of RISE-UC. Resident physicians applied to IMSTAR as part of the fellowship application process. The program was also open to PhDs intending to incorporate clinical research into their career. The IMSTAR fellowships were 1–2 years in duration and provided up to 80% protected time for scholarly training in research. The program culminated in an appointment to the faculty at the instructor or assistant professor level. In addition to these established programs, an NIH R38 (Stimulating Access to Research in Residency) grant application was awarded to the DOIM in FY 2021.
Developing discrete and targeted internal research funding
The department organized an internal program to fund research focusing on projects that would lead to external funding. The program consisted of annual competitive internal requests for applications starting in 2013, including early-career faculty pilot awards for assistant professors ($30,000/award); an endowed cardiovascular-focused award for early-career faculty ($16,000/award); senior faculty pilot awards for associate and full professors ($30,000/award); distinguished research achievement awards for highly productive senior investigators developing new areas of research27 ($50,000/award); and collaborative pilot awards focused on interdisciplinary research ($30,000/award). In 2019, a set of twice-yearly trainee-focused awards were initiated; these included postdoc travel awards ($2,000/award), safety and quality in health care outcomes research awards ($5,000/award), and trainee research awards (i.e., pilot funding for preliminary data for extramural research grant applications; $3,000/award). All the proposals underwent reviews by an NIH-style study section under the direction of the associate chairs for research to determine funding. The study sections also provided applicants with independent critiques of their studies and opportunities for early-career faculty members to serve as reviewers. Bridge funding requests were also accepted from faculty members and reviewed administratively by the departmental leadership. In FY 2017, bridge funding was centralized in the UCCOM dean’s office. Total annual investment for these programs (excluding bridge funding) averaged ~$230,000.
Establishing an ARS unit
To provide infrastructure support, an ARS unit, which consisted of a senior business administrator, research manager, administrative assistant, grant writer/educator, grant matcher/web designer, and 25% full-time equivalent biostatistician was created in FY 2016. Initially, the research manager met with all division directors to identify key priorities for improving research. The implementation of programs to address these priorities were pursued using theory of change and systems theory.28–32 Support services were provided to faculty members, staff, and trainees alike. Furthermore, they were provided for basic, translational, clinical, health care outcomes, and educational research, with some research publications involving a mix of individuals from different areas of research.33 Services were widely advertised to investigators through emails, departmental meetings, and divisional meetings. A monthly curriculum of grantsmanship training was developed that complemented existing educational infrastructure. All faculty members were eligible to receive grant and manuscript writing assistance. To emphasize team science and collaborations, researchers from graduate students and residents to senior faculty members and staff were encouraged to attend a monthly research seminar series, which included networking time. Beginning in FY 2015, laboratory processing services were offered for all clinical researchers in the DOIM. These centralized processing services were meant to offload work historically done by clinical coordinators in each program, enabling them to focus more on the accrual and implementation of clinical research projects. In 2019, a research regulatory services component was formed to provide support services to clinical researchers in the areas of regulatory training, monitoring visits and audits, institutional review board submissions, and maintenance of required regulatory documentation. A research financial services component of ARS was initiated a year later and was charged with assisting in the financial management of clinical trials, including budgeting projections, set up of trial accounts, invoicing of sponsors, effort allocations, and contracting with sponsors. These 3 services were all provided to faculty for a fee or supported by the annual departmental budget. ARS focused its support of the pre-award process on providing consultations, working largely on science and regulatory needs. The UCCOM’s Office of Operations and Administration provided staff to help faculty members with administrative tasks associated with grant submissions, and the Office of Sponsored Research Services overseen by the university’s Vice President for Research had ultimate oversight of grant submission, contract negotiation, and post-award grants management.
Enhancing faculty member mentorship
We addressed mentorship through IDPs, traditional (senior to early-career) mentoring, and peer (early-career to early-career) mentoring. In 2015, the department chair convened a faculty development cabinet to create a departmental IDP template for research-active faculty members and outline the expectations of mentoring for early-career faculty members. All early-career faculty members were expected, with the assistance of their division director and the associate chairs for research, clinical affairs, and education, to identify a mentoring committee composed of 2–3 senior faculty members. The ideal composition would include 2 mentors from within the department and 1 mentor external to the department. Early-career faculty members were to meet at least semiannually with the mentorship committee and to complete the IDP template within their first year. The IDP template had early-career faculty members identify their long-term career goals, followed by short- and medium-term goals (extending out ~36 months). The goals were modeled off of SMART (specific, measurable, achievable, relevant, and time-bound) criteria.23,34 In addition to listing each goal, the IDP template also required that learning objectives and activities, resources and support needed, and checkpoints and end dates be listed for each goal. Goals were to be provided for career development, clinical, education, and research activities as appropriate for each faculty member’s individual effort allocation.
To further support mentoring, in the spring of 2017, a peer mentoring group for early-career faculty members, called the J-club, was established, modeled on the peer mentoring approaches of the successful KL2 program.35 The associate chair of translational research and an early-career faculty member with peer-to-peer mentoring experience who was nearing promotion to associate professorship codirected the J-club. This codirectorship was intentional such that both experienced leadership and near-peer leadership benefits could be realized. Additionally, the departmental ARS grant writer also regularly participated, both as a means to provide feedback and facilitate offline assistance through the ARS. Early-career faculty members were initially invited to the J-club based on the recommendation of division directors within the department. Subsequently, new early-career faculty members with protected research time were identified through the ARS and the hiring and onboarding processes and invited to join. To facilitate their inclusion into the departmental and university research environment, new members completed an IDP that was reviewed by the codirectors. The group met twice monthly with one early-career faculty member presenting information for which they wished to receive feedback or periodically a didactic session or panel discussion organized by the codirectors.
Recognizing, celebrating, and rewarding research success
Recognizing, celebrating, and rewarding research success was considered critical to demonstrating the departmental prioritization of research. Monthly departmental meetings attended by the faculty and staff included slides highlighting receipt of new awards, publications in high-impact journals, and links to news stories covering departmental research activities. Additionally, these meetings included a report from a division director, which included an overview of divisional research interests and successes. These achievements were also highlighted in the monthly departmental e-newsletter and on physical display boards purchased for each division. Recognizing the significant effort required to successfully submit an extramural grant on time, faculty members received an award of $500, $750, or $1,000 reflected in their salary for each extramural grant application with total direct costs of at least $100,000, $200,000, or $500,000, respectively. To recognize faculty members who received extramural funding, research awards of $1,000, $2,500, or $5,000 were issued to faculty members for total direct cost awards of at least $100,000, $200,000, and $500,000, respectively. Finally, departmental leadership nominated faculty members who had demonstrated exemplary research activities for various internal and external awards.
Results of Implementing RISE-UC
Each of the 7 objectives were achieved through a variety of specific activities, which were initiated at different times. These activities required an initial investment of ~$50,000–$70,000/year over the first 2 years. That increased to $600,000–$1,600,000/year with the primary cost drivers being competitive internal awards, the IMSTAR program (which includes protected time costs for participants), the ARS unit, and establishing departmental regulatory services infrastructure. Figure 2 demonstrates that the RISE-UC investments increased both the external grant success rate and the total external direct cost research funds of the department. The external grant submission success rate increased from less than 20% to over 40%, while maintaining approximately the same number of applications per year. This resulted in the new external direct cost awards rising from $17,000,000 in FY 2016 to $26,500,000 in FY 2021 and total external direct cost research funds increasing from ~$55,400,000 in FY 2015 to ~$114,500,000 in FY 2021.
Figure 2.
Departmental total external direct cost research funds and external grant success rate from fiscal year (FY) 2015 to FY 2021, Research Initiative Supporting Excellence at the University of Cincinnati, University of Cincinnati College of Medicine Department of Internal Medicine. Over this 6-year period, total funds increased over 2-fold from ~$55,400,000 to ~$114,500,000. Success rates also increased over the same period. The number of active externally funded principal investigators for each FY, given as numbers at the bottom of the graph, remained relatively constant over this period.
Growing a critical mass of investigators
The total size of the DOIM faculty increased from 195 individuals in FY 2011 to 325 individuals in FY 2021 (Figure 3). There was a trend toward a greater number of new recruits per year, with an average number of new recuirts per year of ~30. This sustained ability to recruit coupled with a decrease in the attrition rate contributed to the overall increase in the departmental faculty. The number of active extramurally funded principal investigators was approximately constant (49–61; see Figure 2). Coupled with the increased extramural finding (see Figure 2), the average funding amount per investigator increased over time.
Figure 3.
Summary of the changes in the size of the faculty from fiscal year (FY) 2011 to FY 2021, Research Initiative Supporting Excellence at the University of Cincinnati (RISE-UC), University of Cincinnati College of Medicine Department of Internal Medicine. A major objective of RISE-UC was to grow a critical mass of investigators, which was achieved as the total size of the faculty increased by 67% (from 195 to 325 individuals) from FY 2011 to FY 2021. The number of new faculty member hires and attrition rates, expressed as a percentage of the total size of the faculty, are also shown. The overall increase in the total size of the faculty was achieved by consistent hiring of new faculty members at rates greater than the attrition rate and reducing the attrition rate over time.
Establishing a shared governance model
The RGC met monthly and provided reports to DOIM staff and leadership, prompting many of the ideas and innovations implemented by RISE-UC over time. To build research infrastructure, the committee members approved the purchase of laboratory equipment and funding for laboratory infrastructure updates. The committee also made recommendations regarding the types and amounts of funding that constituted the targeted internal research funding mechanisms. Subcommittee meetings occurred on the topics of policy, educational programming, and encouraging participation of division staff, faculty members, and trainees in the opportunities available to them. In FY 2020, in alignment with quality improvement36 and change theory models,28,37 the RGC created new subcommittees on mentoring, impact, strategic planning and recognition, and equity.
Creating pathways for developing physician–scientists
Five cohorts have completed the IMSTAR program. Each cohort averaged 3 ± 1.7 individuals. A total of 10 IMSTAR participants have pursued a research track. Two were in private practice, 2 were at academic hospitals, and 6 were assistant professors at the University of Cincinnati. Four of the 6 were members of the department’s J-club, 1 individual transitioned out of research, and 1 participated in an alternate peer mentoring group through the Center for Clinical and Translational Science and Training. The participants were 40% female, 70% Asian, and 30% White. Between FY 2012 and FY 2021, the PSTP program had 13 participants, 6 of whom are still active in the program. The participants were 36% female, 9% Hispanic/Latino, 18% Asian/South Asian, and 73% White. Three of the 7 graduates were in fellowship programs. Of the 4 who completed training, 1 was a faculty member at the University of Cincinnati, 1 was in private practice, 1 was at the NIH, and 1 was a faculty member at another university. More than 50% of the program’s graduates are active researchers at UCCOM. Seventy-five percent of PSTP participants published at least one original research article.
Developing discrete and targeted internal research funding
The total DOIM investment in bridge funding (FY 2013–FY 2016) was $1,800,000 (all bridge funding was distributed through UCCOM from FY 2017 onward). From FY 2013 to FY 2021, pilot internal awards totaled $1,870,000 ($233,000/year on average; Figure 4). The total awards were divided into 19 awards for early-career faculty members ($570,000), 9 endowed cardiovascular-focused awards for early-career faculty members ($117,000), 14 awards for senior faculty members ($420,000), 5 collaborative awards for faculty members of any rank ($150,000), 6 distinguished research awards for senior faculty members ($300,000), 2 associate chairs awards for faculty members of any rank ($80,000), 14 trainee awards ($28,000), and 8 bridge awards for faculty members of any rank ($913,000). Including bridge funding, awardee demographics were as follows: 68% male, 32% female, 68% White, 3% Black, 23% Asian/South Asian, 3% Hispanic/Latino, and 4% other race/ethnicity. Approximately 70% of bridge and pilot awardees ultimately obtained external funding within 3 years of internal funding. For FY 2014–FY 2021, extramural direct funding for faculty members who received bridge or pilot funding was $61,600,000 (an ROI of ~16.4; equation applied: [(total external funds) − (total internal funds)]/total internal funds). The number of peer-reviewed publications per awardee for the 4 years before an internal award relative to the 4 years after increased from 4.1 to 4.7.
Figure 4.
Investment and return on investment (ROI) from fiscal year (FY) 2013 to FY 2021, Research Initiative Supporting Excellence at the University of Cincinnati (RISE-UC), University of Cincinnati College of Medicine Department of Internal Medicine. The major cost drivers of RISE-UC included the physician–scientist pathways (Internal Medicine Scholarly Training for Academic Research [IMSTAR] and Physician-Scientist Training Program [PSTP] programs), administrative units (Academic Research Services [ARS] and non-ARS components), and internal awards (competitive awards [in gray] and bridge funding [in white]). The external funds received by faculty members who received internal competitive or bridge funding awards is shown, with the ROI being ~16.4-fold (equation applied: [(total external awards) − (total internal awards)]/total internal awards). Abbreviation: Admin, administration.
Establishing an ARS unit
To provide a representative assessment of the workload, in FY 2019, the ARS grant writer worked on ~14 grants or manuscripts each month, with 9 manuscripts published in FY 2019. Of the 57 grant proposals ultimately submitted with ARS support, 26% were funded. The number of submissions per month or quarter demonstrated a significant variance, influenced by submission deadlines. The ARS also provided approximately one educational session per month. The total DOIM investment to support ARS personnel and expenses (FY 2016–FY 2021) was $1,670,000.
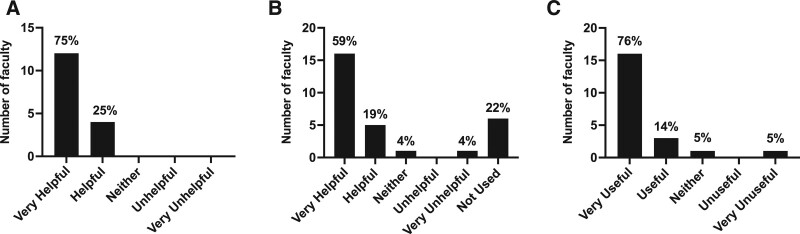
In 2021, an institutional review board-approved deidentified satisfaction survey was conducted to assess faculty member’s perception of the impact of ARS. All 126 research-active faculty members (of the 326 total faculty members) were solicited anonymously, with a 36% response rate (n = 45). The overall satisfaction with ARS was 82/100. Statistical services (Figure 5A) and grant proposal assistance (Figure 5B) were generally noted to be either very helpful or helpful. Supplemental Digital Appendix 1 (at http://links.lww.com/ACADMED/B422) depicts the number of statistical service consultations/year from FY 2018 through FY 2021; the number of consultations provides a quantitative measure of the demand for statistical support and the survey indicates considerable satisfaction. Importantly, Figure 5C shows that investigators who received internal funding perceived this funding to be helpful in ultimately obtaining external funding.
Figure 5.
Satisfaction survey results from 2021, Research Initiative Supporting Excellence at the University of Cincinnati, University of Cincinnati College of Medicine Department of Internal Medicine. The satisfaction survey was conducted to assess the impact of the Academic Research Services unit. Results are shown for the perceived usefulness of (Panel A) statistical services, (Panel B) grant proposal assistance, and (Panel C) internal funding for ultimately obtaining external funding. The percentage of respondents (out of a total of 45) in each category is displayed above the corresponding bar.
Enhancing faculty member mentorship
An initial cohort of 10 research-oriented early-career faculty members at the assistant professor level were invited to join and all matriculated into the J-club. The group included basic, translational, and clinical scientists from 7 of the 9 divisions within the department. Participation was targeted at faculty members who had not yet received R01-equivalent funding (though early-career faculty members with R01-equivalent funding were allowed to join). Between fall 2017 and spring 2021, an additional 13 faculty members matriculated into the program on a rolling basis. The average number of participants at any time was 9 (excluding program leaders). The 23 members were 17% female, 13% Black, 13% Hispanic/Latino, 17% White, and 57% Asian/South Asian.
For the time span of spring 2017 to spring 2021, 12 of the 23 J-club participants received major grant funding (≥ $100,000), 8 withdrew without receiving grant funding (2 left due to insufficient protected research time and/or support, 3 transitioned out of research, 1 transitioned to industry, and 2 moved to other academic institutions), and 3 were still actively participating and seeking their first major grant. Excluding those who withdrew in less than 12 months (n = 4), the average time spent in the program was 30 ± 15 months (with some of these participants active past FY 2021). For those participants who have received major grant funding, the average time between matriculation and receiving a notice of award was 17 months. Funding mechanisms include NIH R01 and equivalent awards, NIH K-awards, NIH KL2 awards, Department of Defense funding, Veterans Affairs funding, and foundation awards.
Recognizing, celebrating, and rewarding research success
For the data available (FY 2013–FY 2016), an average incentive total of $40,000/year was paid out to faculty members for grant submissions and $37,000/year was paid out to faculty members for grants awarded. From FY 2017 to FY 2020, $40,000/year and $22,500/year were budgeted for grant submission and research award incentives, respectively (actual expenditures are unavailable due to centralization of the business function). The grant submission and award incentive program was suspended after FY 2020 due to financial constraints associated with the COVID-19 pandemic. There was no significant change in the number of grants submitted over the duration of RISE-UC, though the total funding amount requested and received increased. Ten faculty members won various awards from the UCCOM, including early-career research recognition awards and faculty mentorship awards. Another 6 faculty members won university-wide awards for distinguished research service.
Discussion
Our results suggest that even in these times of increased challenges, it is possible to implement a strategic plan that can increase external funding and nurture the academic careers of research-active faculty members. The essential underpinnings of RISE-UC were to clearly define objectives, identify funding that could be made available to support the department’s research mission, and then to use an evolving multipronged approach to invest these funds to promote a positive research culture. Although most of the individual components of RISE-UC are similar to other programs that have been reported elsewhere,38–40 a distinctive feature of RISE-UC is the coordinated aggregation of the individual components aligned with a proactive strategic plan.
Identifying internal resources was a prerequisite, and our approach relied on a funds flow41 model. Funding sources included clinical margins ([total clinical revenue − total clinical expenses]/total clinical revenue) from increased total clinical faculty size and revenue, philanthropic sources,42 external grant indirect funds, endowments, and general funds. Although different institutions may vary significantly in where funds are found43,44 and how clinical revenues are distributed,45 a critical feature for supporting a strategic plan is to have mission alignment among the important sources of funding, including the department, medical school, university, and health care system. In our system and probably others, sustaining continuous funding was also important because even with increased extramural funding and associated indirect costs, the complete cost of the research enterprise was not self-sustaining. The ongoing perceived success in achieving the RISE-UC objectives prompted the addition of more programs (Figure 1); this was accompanied by increasing costs averaging $170,000/year in FY 2011–FY 2013 to $1,200,000/year in FY 2017–FY 2022. With continued flat funding levels for the NIH since FY 2003, the need to secure other funding sources has become greater for all research-active departments.9
We view the targeted internal funding initiative to be a core strength of RISE-UC. Key attributes of our targeted internal funding initiative include the scale of the investment ($233,000/year on average) compared with other institutions of similar ranking,46 the frequency (biannually), the variety of specific requests for applications (e.g., early-career, senior, collaborative, trainee), and in-depth NIH-style reviews that provided meaningful feedback regardless of the ultimate awarding. We performed a detailed review of the websites of DOIMs ranked from 31 to 75 based on the 2021 Blue Ridge Institute for Medical Research analysis of total NIH funding awarded47 and determined 39 (87%) of 45 had a specific research-focused area on their website, that only 10 (22%) websites highlighted DOIM-specific internal awards, and none (0%) were of the same scope (see Supplemental Digital Appendix 2 at http://links.lww.com/ACADMED/B422).
The J-club aspect of RISE-UC shares some elements with the Clinical and Translational Scholars (CATS) “matrix mentoring model” at the University of Utah,38 which involved a mix of self, senior, peer, scientific, and staff mentorship. Approximately 92% of CATS participants achieved the objective of becoming principal investigators (being awarded a grant of $25,000 or more). The CATS mentoring program reported an ROI of 19, similar in magnitude to our own internal awards initiative ROI and other reports in the literature.46,48,49 These ROIs suggest that even modest internal support can result in substantial external awards, in addition to earlier promotion and retention50 and enhanced career development.51 These returns are significantly higher than ROIs typical found in business where a gross margin of 7%–10% is considered healthy and a recent analysis of the gross margins of 26 large companies on the Dow Jones Industrial Average report an average gross margin of 46.5%, which is equivalent to an ROI of 0.869.52
The ability to implement a strategic plan like RISE-UC requires not only the identification of substantial funding but also dedicated faculty and staff members. The 2 associate chairs for research dedicated ~20% full-time equivalent effort to their leadership roles in the DOIM, including implementing RISE-UC. In addition to these individuals and ARS staff, concerted faculty effort was needed to lead the IMSTAR, PSTP, and J-club programs. A general culture shift also needed to be implemented so that individual research-active faculty members would participate in the various opportunities. The use of shared governance may have facilitated a feeling of ownership and culture change. Furthermore, effective shared governance was facilitated by leadership ensuring that a member of the RGC (i.e., the ARS research manager) had expertise in theory of change and was sufficiently empowered so that policy ideas could be effectively implemented. Additionally, the almost continuous rollout of programs (see Figure 1) further facilitated a culture change where research activities were valued and faculty members were encouraged to pursue research-related career development. The culture was further shifted by the persistent effort of ARS staff in ways that are not necessarily countable (e.g., grant or manuscript submissions). For example, the ARS grant writer assisted non-native English-speaking principal investigators with grammatical issues for grants and manuscripts and offloaded some of the mundane activities of grant writing from the principal investigators of larger grants (e.g., T32 tables). Our review of the websites of DOIMs ranked from 31 to 75 based on the 2021 Blue Ridge Institute for Medical Research analysis of total NIH funding awarded47 indicated that 13 (29%) of 45 had an organizational structure that was similar to the ARS and only 5 (11%) had an individual identified as a grant writer (see Supplemental Digital Appendix 2 at http://links.lww.com/ACADMED/B422). Publicly available data indicate that many institutions do not have the staffing to help effectuate positive research culture changes. A key component of culture change is also removing structural barriers faced by underrepresented groups. The RISE-UC strategic plan aligned with university-wide equity and inclusion initiatives, in addition to making separate efforts, such as representation within various initiatives (see above) and establishing an equity RGC subcommittee. Future efforts could include techniques to advance the full and equitable participation of all faculty members through structures and education that impacts faculty member discretion and workloads.53,54
The combined success of our initiatives has also yielded other fruits. The department’s clinical enterprise grew so significantly that many new clinicians quickly became saturated with ambulatory and in-patient responsibilities. Although this limited the time freed up for clinician–scientists to pursue research, it did increase the department’s clinical revenues, which were partially used to support research. These funds played an important role in increasing the average extramural research funds per principal investigator. Another benefit was that RISE-UC outcomes facilitated the department receiving an NIH-sponsored R38 grant in FY 2021. We have built the program resulting from this grant around the key component of a personalized curriculum based on the residents’ different prior research experiences.
There are a number of limitations with respect to the interpretation of RISE-UC and its potential applicability to other institutions. First, the research success of the departmental faculty cannot solely be associated with RISE-UC as the UCCOM and university both support other research programs, such as the NIH Clinical and Translation Science Award-supported Center for Clinical and Translational Science and Training,55 the Faculty Enrichment Center, and faculty development seminar series from both the UCCOM and Office of the Vice President for Research. All faculty members within the department were invited to participate in offerings from all of these programs. Second, a limitation of the results presented is that the services were offered to the entire faculty and thus a control arm for comparison is not available to determine whether the same outcomes might have been achieved without RISE-UC. Third, the simultaneous implementation of initiatives with different applicability to faculty members at various career stages and with different research interests makes it challenging to determine the value of each individual initiative. For example, the ROI does not take into account investments in faculty members’ research programs beyond the internal awards initiative. However, the exact value of the ROI is not as important as the fact that the intramural awards ROI was robust and aligned with other programs.46,48,49 Fourth, the lack of assessment of the effectiveness of RISE-UC or any of its individual components by means of comparison with other institutions’ departments is another limitation. This type of assessment was not attempted herein due to the numerous confounding factors and, in the case of the review of websites, the inherent incompleteness of data. Finally, another factor that may limit the generalizability of the results is the unique environment and culture of the UCCOM DOIM.
Despite these limitations, we believe that the process of creating the RISE-UC strategic plan and its individual components are of potential value to other institutions. RISE-UC was implemented over time, following components of theory of change and improvement theory, including identifying specific and measurable aims; measuring improvement over time; and incorporating cycles that allow small changes to be made,28,37,56 implemented, studied, and revised as a path to larger sustainable changes.19,57,58 Using this or similar theories and models for change and implementation, other departments, regardless of their size, can select those components of RISE-UC that are most aligned with their institutional needs and the constraints of their local environment. By implementing an iterative process, it is possible for departments to build their research program over time, as was accomplished with RISE-UC.
Our description of RISE-UC may be particularly informative to those who are taking on departmental leadership roles, particularly as they consider theories of change, including the Model for Improvement.19 It is also important to note that while this article focuses on support for research activities, other activities were pursued to support faculty members with efforts that were more deeply associated with patient care or clinical education. The UCCOM DOIM made a point to demonstrate its interest in and that it valued the patient care and education missions. For example, shared governance committees, similar to the RGC, were established in these areas. Additionally, as clinical revenues increased over time, a new physician compensation plan was implemented to increase health care professionals’ salaries based on a work-relative value unit productivity model.
Conclusions
The RISE-UC strategic plan was a part of a broader strategic plan initiated in 2011 with the explicit goals of expanding faculty numbers, supporting their growth and development, and prioritizing the research mission in the DOIM. A funds flow model using a diverse number of sources enabled sustained, substantial funding for carrying out the RISE-UC strategic plan. Critical aspects of this model included a shared governance model; development and training of physician–scientists; using internal funding to support faculty member and trainee research projects; establishing infrastructure to support research; enhancing faculty member mentorship; and recognizing, celebrating, and rewarding research success across the department. Combined, these strategic activities contributed to a doubling of both external funding and external grant success rates, with a 16.4-fold ROI. The implications of this approach were that other institutions may benefit from implementing, in full or part, many of the initiatives that led to our success. Using constructs from theories of change and implementation, engaging the faculty, and providing an overall strategic vision within an iterative process of implementation is likely applicable to many academic departments.
Acknowledgments:
The authors thank the staff of the Academic Research Services for their contribution to the Research Initiative Supporting Excellence at the University of Cincinnati. The authors also thank Max Weed for assisting in collating the number of publications. Finally, the authors thank the faculty and staff of the Department of Internal Medicine for their efforts to improve the research culture and excel in their efforts to create new knowledge and strengthen the departmental community.
Supplementary Material
Footnotes
Supplemental digital content for this article is available at http://links.lww.com/ACADMED/B422.
Funding/Support: This work was funded by the Department of Internal Medicine at the University of Cincinnati.
Other disclosures: M.S. was affiliated with the University of Cincinnati during the implementation of RISE-UC but is now a faculty member of the Department of Medicine, University of New Mexico School of Medicine, and a senior clinician–scientist investigator with the Department of Veterans Affairs. K.J.H. provides consulting for Boston Scientific, Inc. S.S. provides consulting and collaborative research studies to the Foundation Leducq (CURE PLaN), Red Saree, Inc., Greater Cincinnati Tamil Sangam, Novo Nordisk, Pfizer, AavantiBio, Inc., AstraZeneca, MyoKardia, Inc., Merck, and Amgen, but this work is unrelated to the content of this article. C.J.F. serves as an advisor for ViiV Healthcare and Theratechnologies, Inc. He also receives research grants to the institution from Gilead Sciences, Inc., ViiV Healthcare, Merck, Moderna, and CytoDyn, all outside of the content of this article.
Ethical approval: The satisfaction survey of the research-active faculty was completed with the approval of the University of Cincinnati Institutional Review Board (approval number 2021-0623, August 23, 2021).
Contributor Information
Kelly C. Niederhausen, Email: niederkc@ucmail.uc.edu.
Eric P. Smith, Email: smithep@ucmail.uc.edu.
Sakthivel Sadayappan, Email: sadayasl@ucmail.uc.edu.
Yolanda Wess, Email: wessyy@ucmail.uc.edu.
Jack Rubinstein, Email: rubinsjk@ucmail.uc.edu.
Daniel P. Schauer, Email: schauedp@ucmail.uc.edu.
Manoocher Soleimani, Email: MSoleimani@salud.unm.edu.
Gregory W. Rouan, Email: rouangw@ucmail.uc.edu.
Carl J. Fichtenbaum, Email: FICHTECJ@UCMAIL.UC.EDU.
References
- 1.Mallon WT. The financial management of research centers and institutes at U.S. medical schools: Findings from six institutions. Acad Med. 2006;81:513–519. [DOI] [PubMed] [Google Scholar]
- 2.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: Continuing challenges in the 21st century. FASEB J. 2014;28:1049–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bunton SA, Mallon WT. The continued evolution of faculty appointment and tenure policies at U.S. medical schools. Acad Med. 2007;82:281–289. [DOI] [PubMed] [Google Scholar]
- 4.National Institutes of Health. Physician-Scientist Workforce Working Group Report. https://acd.od.nih.gov/documents/reports/PSW_Report_ACD_06042014.pdf. Published 2014. Accessed April 19, 2023. [DOI] [PMC free article] [PubMed]
- 5.King L, Mallon WT, Kosik RO, et al. Physician scientist training in the United States: A survey of the current literature. Trends Biochem Sci. 2016;38:373–375. [Google Scholar]
- 6.Daniels RJ. A generation at risk: Young investigators and the future of the biomedical workforce. Proc Natl Acad Sci U S A. 2015;112:313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adashi EY, Gruppuso PA. Commentary: The unsustainable cost of undergraduate medical education: An overlooked element of U.S. health care reform. Acad Med. 2010;85:763–765. [DOI] [PubMed] [Google Scholar]
- 8.Johnson JA. NIH Funding: FY1994-FY2016. https://www.everycrsreport.com/files/20150306_R43341_c4a3e25094fc2f547dcaec1dfaf1fc100725a5c4.pdf. Published March 6, 2015. Accessed April 30, 2023.
- 9.Congressional Research Service. National Institutes of Health (NIH) Funding: FY1996-FY2023. https://fas.org/sgp/crs/misc/R43341.pdf. Updated March 8, 2023. Accessed April 19, 2023.
- 10.Sandhu AT, Dudley RA, Kazi DS. A cost analysis of the American Board of Internal Medicine’s maintenance-of-certification program. Ann Intern Med. 2015;163:401–408. [DOI] [PubMed] [Google Scholar]
- 11.Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians. Acad Med. 2017;92:237–243. [DOI] [PubMed] [Google Scholar]
- 12.Meador KJ. Decline of clinical research in academic medical centers. Neurology. 2015;85:1171–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKinney RE. The daunting career of the physician-investigator. Acad Med. 2017;92:1368–1370. [DOI] [PubMed] [Google Scholar]
- 14.Chen MM, Sandborg CI, Hudgins L, Sanford R, Bachrach LK. A multi-faceted mentoring program for junior faculty in academic pediatrics. Teach Lean Med. 2016;28:320–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strong EA, De Castro R, Sambuco D, et al. Work–life balance in academic medicine: Narratives of physician-researchers and their mentors. J Gen Intern Med. 2013;28:1596–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mazur S, Bazemore A, Merenstein D. Characteristics of early recipients of patient-centered outcomes research institute funding. Acad Med. 2016;91:491–496. [DOI] [PubMed] [Google Scholar]
- 17.Levine RL, Rathmell WK. COVID-19 impact on early career investigators: A call for action. Nat Rev Cancer. 2020;20:357–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moses H, III, Matheson DHM, Cairns-Smith S, George BP, Palisch C, Dorsey ER. The anatomy of medical research. JAMA. 2015;313:174–189. [DOI] [PubMed] [Google Scholar]
- 19.Institute for Healthcare Improvement. The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. Diabetes Spectr. 2004;17:97–101. [Google Scholar]
- 20.American Board of Internal Medicine. Research Pathway Policies and Requirements. https://www.abim.org/certification/policies/research-pathway. Accessed April 19, 2023.
- 21.Westrope RA, Vaughn L, Bott M, Taunton RL. Shared governance. From vision to reality. J Nurs Adm. 1995;25:45–54. [DOI] [PubMed] [Google Scholar]
- 22.Belfi LM, Weissman E, Haramati A. Grit, gratitude, grace, and guidance: Moving academic medicine from crisis to transformation. Acad Med. 2022;97:1438–1440. [DOI] [PubMed] [Google Scholar]
- 23.Yemm G. Essential Guide to Leading Your Team: How to Set Goals, Measure Performance and Reward Talent. London, UK: Financial Times; 2012. [Google Scholar]
- 24.Gavin M, Ash D, Wakefield S, Wroe C. Shared governance: Time to consider the cons as well as the pros. J Nurs Manag. 1999;7:193–200. [DOI] [PubMed] [Google Scholar]
- 25.Warm EJ, Schauer DP, Diers T, et al. The ambulatory long-block: An Accreditation Council for Graduate Medical Education (ACGME) educational innovations project (EIP). J Gen Intern Med. 2008;23:921–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Todd RF, III, Salata RA, Klotman ME, et al. Career outcomes of the graduates of the American Board of Internal Medicine Research Pathway, 1995–2007. Acad Med. 2013;88:1747–1753. [DOI] [PubMed] [Google Scholar]
- 27.Golper TA, Feldman HI. New challenges and paradigms for mid-career faculty in academic medical centers: Key strategies for success for mid-career medical school faculty. Clin J Am Soc Nephrol. 2008;3:1870–1874. [DOI] [PubMed] [Google Scholar]
- 28.Fullan M. Change theory as a force for school improvement. In: Burger JM, Webber CF, Klinck, eds. Intelligent Leadership: Constructs for Thinking Education Leaders. Dordrecht, The Netherlands: Springer; 2007:27–39. [Google Scholar]
- 29.Godfrey M, Foster VL, Nilsson M. IHI ID 22 Validation of the quality improvement assessment (QIA) tool. BMJ Open Qual. 2018;7(suppl 1):A30–A33. [Google Scholar]
- 30.Ellner AL, Stout S, Sullivan EE, Griffiths EP, Mountjoy A, Phillips RS. Health systems innovation at academic health centers. Acad Med. 2015;90:872–880. [DOI] [PubMed] [Google Scholar]
- 31.Greiner AC, Knebel E, eds. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003. https://www.ncbi.nlm.nih.gov/books/NBK221528. Accessed April 19, 2023. [PubMed] [Google Scholar]
- 32.Wolfe A. Institute of Medicine Report: Crossing the quality chasm: A new health care system for the 21st century. Policy Polit Nurs Pract. 2001;2:233–235. [Google Scholar]
- 33.Warm EJ, Mathis BR, Held JD, et al. Entrustment and mapping of observable practice activities for resident assessment. J Gen Intern Med. 2014;29:1177–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frey BS, Osterloh M, eds. Successful Management by Motivation: Balancing Intrinsic and Extrinsic Incentives. 2nd ed. Berlin, Germany: Springer; 2002. [Google Scholar]
- 35.Sorkness CA, Scholl L, Fair AM, Umans JG. KL2 mentored career development programs at clinical and translational science award hubs: Practices and outcomes. J Clin Transl Sci. 2019;4:43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schierhout G, Hains J, Si D, et al. Evaluating the effectiveness of a multifaceted, multilevel continuous quality improvement program in primary health care: Developing a realist theory of change. Implement Sci. 2013;8:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sopact. Theory of Change. https://www.sopact.com/theory-of-change. Accessed April 19, 2023.
- 38.Byington CL, Keenan H, Phillips JD, et al. A matrix mentoring model that effectively supports clinical and translational scientists and increases inclusion in biomedical research: Lessons from the University of Utah. Acad Med. 2016;91:497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fleming GM, Simmons JH, Xu M, et al. A facilitated peer mentoring program for junior faculty to promote professional development and peer networking. Acad Med. 2015;90:819–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Freel SA, Smith PC, Burns EN, Downer JB, Brown AJ, Dewhirst MW. Multidisciplinary mentoring programs to enhance junior faculty research grant success. Acad Med. 2017;92:1410–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lakshminrusimha S, Murin S, Kirk JD, et al. “Funds flow” implementation at academic health centers: Unique challenges to pediatric departments. J Pediatr. 2022;249:6–10. [DOI] [PubMed] [Google Scholar]
- 42.Collins ME, Rum S, Wheeler J, et al. ; Participants in the Summit on the Ethics of Grateful Patient Fundraising. Ethical issues and recommendations in grateful patient fundraising and philanthropy. Acad Med. 2018;93:1631–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bailey DN, Crawford JM, Jensen PE, Leonard DGB, McCarthy S, Sanfilippo F. Generating discretionary income in an academic department of pathology. Acad Pathol. 2021;8:23742895211044811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Itri JN, Mithqal A, Krishnaraj A. Funds flow in the era of value-based health care. J Am Coll Radiol. 2017;14:818–824. [DOI] [PubMed] [Google Scholar]
- 45.Ringel MD, Murphy EJ, Hammes SR. Compensation, productivity, and other demographics of academic divisions of endocrinology, diabetes, and metabolism. J Endocr Soc. 2019;3:1485–1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paller MS, Cerra FB. Investing in research: The impact of one academic health center’s research grant program. Acad Med. 2006;81:520–526. [DOI] [PubMed] [Google Scholar]
- 47.Roskoski R, Parslow TG. BRIMR Rankings of NIH Funding in 2021. https://brimr.org/brimr-rankings-of-nih-funding-in-2021. Published December 26, 2022. Accessed January 20, 2022. [DOI] [PMC free article] [PubMed]
- 48.Weber-Main AM, Thomas-Pollei KA, Grabowski J, Steer CJ, Thuras PD, Kushner MG. The proposal preparation program: A group mentoring, faculty development model to facilitate the submission and funding of NIH grant applications. Acad Med. 2022;97:53–61. [DOI] [PubMed] [Google Scholar]
- 49.Swaminathan A, David FS, Geary LN, Slavik JM. Results of a portfolio approach to intramural research funding at an academic medical center. PLoS One. 2020;15:e0241425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Connelly MT, Sullivan AM, Chinchilla M, et al. The impact of a junior faculty fellowship award on academic advancement and retention. Acad Med. 2017;92:1160–1167. [DOI] [PubMed] [Google Scholar]
- 51.Mughal A, Wahlberg KJ, Li Z, Flyer JN, Olson NC, Cushman M. Impact of an institutional grant award on early career investigator applicants and peer reviewers. Res Pract Thromb Haemost. 2021;5:e12555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Angilella S, Morelli D. Are the stock prices influenced by the publication of the annual financial statements? Evidence from the Dow Jones Industrial Average. Oper Res. 2021;21:1031–1040. [Google Scholar]
- 53.O’Meara K. Leveraging, checking, and structuring faculty discretion to advance full participation. Rev High Educ. 2021;44:555–585. [Google Scholar]
- 54.Griffin K, Gibbs KD, Jr, Bennett J, Staples C, Robinson T. “Respect me for my science”: A Bourdieuian analysis of women scientists’ interactions with faculty and socialization into science. J Women Minorities Sci Eng. 2015;21:159–179. [Google Scholar]
- 55.Center for Clinical & Translational Science & Training. Accelerating & Improving Clinical & Translational Research. http://cctst.uc.edu. Accessed April 19, 2023.
- 56.Douglass A, Halle T, Tout K. The Culture of Continuous Learning Project: A Breakthrough Series Collaborative for Improving Child Care and Head Start Quality: Theory of Change. https://www.acf.hhs.gov/sites/default/files/documents/opre/ccl_theory_of_change_brief.pdf. Published 2019. Accessed April 19, 2023.
- 57.Langley J, Nolan K, Nolan T, Norman C PL, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco, CA: Jossey-Bass; 1996. [Google Scholar]
- 58.Headrick LA, Knapp M, Neuhauser D, et al. Working from upstream to improve health care: The IHI Interdisciplinary Professional Education Collaborative. Jt Comm J Qual Improv. 1996;22:149–164. [DOI] [PubMed] [Google Scholar]