Abstract
Objective
Curriculum development and reviews are of paramount importance for academic programs curriculum management. Medical curricula need proper construction and frequent updates to suits learning outcomes considering their integrative nature and rapid scientific advancement. Curriculum alignment and mapping are fundamental for proper integration and planning of medical curriculum. This process is beneficial in detecting gaps and redundancies, and ensuring proper instruction, integration, and transparency. However, there is a paucity in the literature of a practical guidance to such process. Hence, this manuscript provides a practical guidance that was adopted in our institutes.
Methods
A detailed description of twelve step-by-step guidance to curriculum alignment and mapping was provided. The process needed for each step and the flow chart of work was detailed.
Results
This guide was developed and implemented successfully. Among many benefits encountered, many gaps in the contents, learning outcomes and assessment methods were detected and rectified. Additionally, better curriculum integration has been achieved. The current mapping will make any future curriculum reviews easier.
Conclusion
This guide could be utilized by newly developed and existing programs for curriculum alignment and mapping. It fills a gap in academic literature through stepwise workflow which has been tested and implemented.
Keywords: curriculum, mapping, learning outcomes
Introduction
A curriculum defines the intended knowledge skills and learning outcomes expected by students.1 A curriculum is designed based on learning and instruction principles and requires a composite of different educational strategies, course content, learning outcomes, educational experiences, assessment, and a suitable educational environment considering individual students’ learning styles and programs of work.1,2 To have a constructive curriculum, harmonization is a mainstay between declared or planned curriculum, operational curriculum (taught or learned), and experienced curriculum.1,3 This requires proper alignment between the intended learning outcomes (curricular intent) expected in the declared curriculum and other instructional components, namely teaching methods, within-class teaching activities, and assessment, to ensure coherency.4 Communicability, transparency, and versatility are crucial pillars in the design and execution of curriculum, as they allow for continuous revision, evaluation, and modification without difficulty.5,6 These attributes are frequently neglected in favor of more prominent curricular components, including content, pedagogy of participation, and assessment.7
Curriculum mapping is an essential active process that allows holistic spatial visualization of the various parts of the curriculum’s interrelationships and connections.1 The advantages of mapping are multifaceted, as it allows assessing the degree of attainability of learning outcomes, detecting redundancies and gaps, weaknesses and strengths, and rectifying them.1,8 Also, it aids in constructing proper assessment plans for the whole curriculum and ensures proper coordination across curriculum contents.9,10 Mapping enhances student achievement and faculty involvement.11 As more medical schools increasingly shift to integrated curricula replacing traditional curricula, mapping can ensure balanced horizontal, longitudinal, and spiral integration and blending of the curricular content through all phases.
On the other hand, curriculum mapping in medical programs has multiple challenges. The alignment of discipline-specific intended learning outcomes with one another and the achievement of numerous inter-discipline learning outcomes that are essential for fostering students’ transition to their chosen specialty are just two of the many challenges faced by curriculum mapping in medical programs. Additionally, because medical curricula are dynamic, they must be reviewed and updated on a regular basis to reflect quick scientific progress, ongoing community demands, advancements in technology and their applications, and modifications to the policies put out by healthcare authorities. This was compounded by the increasing diversity of instructional methods and advancements in the field of medical education.12–14
Curriculum mapping, including constructive alignment, requires involvement from leaders, multidisciplinary content experts, curriculum developers, medical educators, instructors, and students.12,15 Curriculum management, which includes alignment, mapping, and monitoring, is becoming more and more crucial in education. For the goal of curriculum mapping, computerized tools are frequently employed to guarantee ongoing accessibility of the curricular pillars, evaluate efficacy, and facilitate the integration of modifications.16
In higher education, curriculum mapping becomes pivotal at the institutional and program levels. Various international bodies supported their medical schools’ use of electronic curriculum mapping systems such as Curriculum Management and Information Tool (CurrMIT), which was recommended by the Association of American Medical Colleges (AAMC) in the United States.17 National accreditation has become obligatory in many countries worldwide including Saudi Arabia as the result of recent and rapid expansion in the number of medical education institutions. Program accreditation relies heavily on accumulating evidence from curricular congruence and mapping. A well-documented curriculum, including its alignment and mapping of programs and courses, is a hallmark of good practice and a guarantee of efficient management.18,19 In the last three decades, one of the most significant changes has been the rise of outcome-based education.
As in other parts of the world, health professional bodies and the leaders of medical programs in Saudi Arabia have developed a competency-based national medical education framework to standardize the essential combined requirements of knowledge, skill, and behavior needed to become a medical doctor.20 The National Center for Academic and Evaluation (NCAAA) recognized the Saudi Medical Education Directives Framework (SaudiMED) as meeting the NCAAA’s baseline standards for accrediting medical education programs.21 As a method of quality assurance, accreditation of medical programs is rapidly gaining acceptance as a requirement in many parts of the world. To a similar extent, all medical programs in Saudi Arabia and the Middle East must be accredited by a national or international certifying authority. The International Federation for Medical Education (WFME) has recognized the National Accrediting Agency for Academic Institutions in Saudi Arabia (NCAAA) as an accrediting organization for medical programs in Saudi Arabia and the region.22 Additionally, the Educational Commission for Foreign Medical graduates (ECFMG) in the United States has stated that as of 2024, only graduates from accredited medical schools/programs will be allowed to apply for postgraduate training in the United States.23
Studies showed that different models of curriculum mapping, ie centralized and/or decentralized, are useful in developing the mapping.7,24 These studies provide structured guidance for implementing constructive curriculum alignment and mapping in medical programs. However, published guidelines for competency-based curriculum mapping in medical education are limited.25 To the best of our knowledge there is only one publication on medical curriculum alignment and mapping in the Middle East.26 Frequently, medical schools acquire their own curriculum mapping process to meet their needs.26 Similarly, medical programs in the region will need a specialized curriculum alignment and mapping procedure to meet their needs. Therefore, this manuscript aims to disseminate information and provide other medical educators with our stepwise guidelines for curriculum alignment and mapping that carefully blend contents, detect gaps and redundancies, and ensure horizontal, longitudinal, and spiral integration and linking in a competency-based curriculum. Medical programs in the region and around the world can use these guidelines to enhance their competency-based curricula and provide evidence for curriculum improvement and accreditation.
Methods: (Curriculum Alignment and Mapping Steps)
The steps below were followed to constructively align and map the medical curriculum of King Saud bin Abdulaziz University for Health Sciences, Saudi Arabia, and are currently being followed by the United Arab Emirates University, UAE. These steps were developed and executed by the authors based on available literature, focused group discussions, Delphi method and experience. Institutional approval of the study was waived as the study is on curriculum and does not involve humans.
Step 1: Leadership Commitment and Support
This is a very important first step as mapping and constructive alignment is complex and resource intense. Leadership support is crucial to empower the working group, provide access to all course material, and ensure involvement of all stakeholders in the process.
Step 2: Build the Team and Agree on the Process of Work
As this is a multidisciplinary process, the team needed for curriculum alignment and mapping must include experts in medical education and content matter as well as the program leaders. Building the team and engaging them in the process is of paramount importance. A small, centralized team may work better than a large one as too many members could lead to fragmentation, inconsistency, and lack of ownership of the work. A small group of medical education experts who know the curriculum content and have been involved in its conduction for some time is ideal. This team can lead the process and liaise with other stakeholders such as course content experts, course coordinators/directors, students, and program leaders.
Step 3: Selection of a Model for Constructive Alignment of Mapping
The model we have adopted is based on a conceptual framework for the curriculum mapping (Figure 1). This model is utilizing the planned curriculum as a starting point which is guided by program learning outcomes and graduation requirements. The second level is the delivered or communicated curriculum as represented by detailed content scheduling, instruction methods, etc. The third level involves the confirmation that the delivered curriculum is well implemented with high quality. The last level is the assessed or the learned curriculum, since assessment drives learning, this necessitates that assessment should be used strategically to enhance students learning.27,28 All these levels are guided by accreditation requirements and local environment and contextual factors.
Figure 1.
Conceptual Framework for Curriculum Mapping.
*In our case, the environment, context, and accreditation requirements set by the SaudiMED and NCAAA
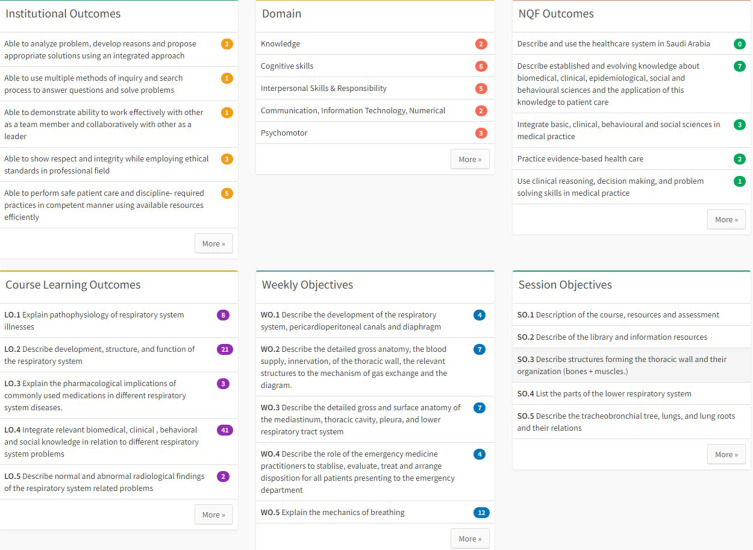
Step 4: Selection of Variables
Using the Delphi method,29 medical educators and teaching faculty can identify the variables needed for each phase of the conceptual framework. The following is an example of identified variables required for each session in the curriculum:
Planned/Intended Curriculum variables: Institutional Learning Outcomes (ILOs)
Program Learning Outcomes (PLOs)
Course Learning Outcomes (CLOs)
Weekly Learning Objectives (WLOs) with Weekly Theme and Weekly Problem
Course Learning Topics (Topics)
Topic/Session Objectives
Entrustable Professional Activities (EPAs)
Core Clinical Problems (CCPs)
Clinical Presentations (Presentations)
- 1. Delivered/Communicated Curriculum variables
- Session Title
- Venue, date, duration
- Teaching Method
- Instructor(s)
- Discipline
- Assessment methods
- 2. Quality-Assurance variables/Key Performance Indicators (KPIs)
- 1. Session completed according to timetable and in correct sequence
- 2. Session objectives covered/not covered
- 3. Session rapid survey evaluation by students
- 4. Percentage of students attending each session
- 5. Qualification of session’s presenters
-
3. Assessed Curriculum variables:
Assessment Type (MCQ, Short Answer, Essay, OSCE, Clinical Exam, etc.)
- For MCQ type:
- 1. Item Discipline
- 2. Item Process (Diagnosis, Management, Procedures, Physical Exam, Professional, etc.)
- 3. Item link to Session
- 4. Item link to CLO
- 5. Item Cognitive Level
- 6. Item Difficulty Index
- 7. Item Quality Index
- 8. Item Status (New or Used)
- For Non-MCQ types:
- 1. Rubric with items to be assessed
- 2. Each item in the Rubric must have a mark and links to Discipline, Session and CLO.
The leadership team and the faculty members have access to the mapping variables. Moreover, the students also have access to most of the variables except the assessment items.
Step 5: Purchasing or Building an Alignment and Mapping Platform
Existing digital platforms in the market may be sufficient for some programs, however, building an in-house digital platform has the advantage of customization to specific need of the curriculum. We chose to develop an in-house system based on the planned process as the existing platforms in the market were found to be insufficient to accommodate all our identified variables and feature requirements. The team worked with a programmer step by step to reach a full fledge system that fully satisfies all the requirements. At the beginning, the data collection step was completed using spreadsheets for initial record keeping and as a backup then later incorporated into the digital system as the final curriculum alignment and mapping record. In both purchase and build scenarios, data entry into the system is a crucial step to successful implementation.
Step 6: Determine and Review the Program Learning Outcomes (PLOs)
PLOs are the essence of any curriculum, and they should always come first to be developed or reviewed. For medical curricula, PLOs are commonly derived and aligned with a list of competencies the student must achieve upon graduation. In our context, the PLOs for medical programs are guided by the SaudiMED framework and competencies. The SaudiMED competencies were developed through a rigorous process involving multiple workshops by experts in the field. SaudiMED competencies are further aligned with a list of 17 PLOs that are adopted as the national PLOs for all medical programs in Saudi Arabia as endorsed by the National Center for Academic Accreditation and Assessment (NCAAA).21 The PLOs cover different domains relevant to medical curricula and future medical practice (Table 1 SaudiMED). The use of a national competencies framework to guide medical curricula development are similarly practiced in other regions around the world such as in Canada (Can MEDs).30 Adoption of national level PLOs ensures to some extent equally competent graduates to start postgraduate residency training.
Table 1.
SaudiMED Framework and PLOs (Education and Training Evaluation Commission Saudi Arabia 2021; Zaini et al 2011)
| Theme I: Scientific Approach to Practice |
| The integration and application of basic, clinical, behavioral and social science in clinical practice |
| PLO1. Integrate basic, clinical, behavioral and social sciences in medical practice |
| PLO2. Practice evidence-based health care |
| Theme II: Patient care |
| The establishment and maintenance of essential clinical and interpersonal skills to demonstrate proficient assessment and delivery of patient-centered management. |
| PLO3. Demonstrate the essential clinical skills |
| PLO4. Use clinical reasoning, decision making, and problem solving skills in medical practice |
| PLO5. Manage patients with life-threatening medical conditions |
| PLO6. Formulate and implement appropriate management plans for patients with common medical problems |
| PLO7. Place patients’ needs and safety at the center of the care process |
| Theme III: Community oriented practice |
| The health care practicing is based on an understanding of the Saudi health care system and the application of health promotion and advocacy roles for the benefit and wellbeing of individual patients, communities, and populations. |
| PLO8. Adhere to the regulations of Saudi healthcare system in the Kingdom |
| PLO9. Advocate health promotion and disease prevention |
| Theme IV: Communication and Collaboration |
| The effective communication with patients and their families and the practicing of collaborative care by working in partnership within a multi-professional team |
| PLO10. Effectively communicate verbally and in writing with patients, their families, colleagues, and other health professionals |
| PLO11. Practice teamwork and inter-professional collaboration |
| PLO12. Apply medical informatics in healthcare system effectively |
| Theme V: Professionalism |
| The commitment to deliver the highest standards of ethical and professional behavior in all aspects of health practice, and take a responsibility for own personal and professional development. |
| PLO13. Demonstrate professional attitudes and ethical behaviors of physicians |
| PLO14. Apply Islamic, legal and ethical principles in professional practice |
| PLO15. Demonstrate the capacity for self-reflection and professional development |
| Theme VI: Research and scholarship |
| The contribution to the advancement of medical practice with the rigors of scientific research. |
| PLO16. Demonstrate basic research skills |
| PLO17. Critically appraise and demonstrate scholarly activities related to health sciences research |
Step 7: Constructive Alignment and Mapping of Courses Learning Outcomes (CLOs) and Weekly Learning Objectives (WLOs) with the PLOs
To achieve the PLOs of a program, courses and course learning outcomes are developed or reviewed to collectively achieve all the PLOs. In our context, all the course CLOs were reviewed and aligned with the PLOs in term of its relevance and appropriateness. Content experts were invited by the leading team and collectively reviewed each course learning outcome in view of the PLOs. This involved experts from various fields of study as the courses are integrated with basic and clinical sciences, the experts of each discipline had an input toward the course learning outcomes and content with emphasis on the course coordinator role.
This step can be helpful in revising and updating the CLOs and allows for inclusion of any missing CLOs deemed necessary to be added by the content experts. Therefore, the CLOs were reviewed to ensure that they are deemed comprehensive to guide the course content. Afterwards the CLOs were categorized according to the PLOs domains, ie knowledge, skills and attributes. This step again was done for each course in consultation with the content experts to ensure that the CLOs are appropriately aligned and categorized according to the domains of learning. Moreover, in this step it was possible to identify any redundancy in term of CLOs between courses and the depth of overage of each CLO in different courses.
In a problem-based curriculum where there is a weekly problem as the center of the week learning activities, and to facilitate each week alignment and mapping, it is also important to develop Weekly Learning Objectives (WLOs) based on the week’s theme. The WLOs can subsequently be aligned to the CLOs and the PLOs.
Of importance in this step is that the CLOs must be reasonable in term of number and depth for the particular course duration and level. In general, for the Saudi example, courses were maintained around 18–22 CLOs per course. However, each CLO branched to more defined WLOs.
Step 8: Constructive Alignment and Mapping of Sessions and Session Objectives with CLOs and WLOs
This step is looking at the session level and aligning either the session with the appropriate CLOs and WLOs or aligning each session objective with the appropriate CLOs and WLOs. This is done in consultation with content experts. We aligned and mapped all course learning activities including each session objective to the WLOs which ultimately aligned and mapped the learning activities to the CLOs paying attention to the domain of each CLO. For example, lectures are aligned and mapped to CLOs under knowledge domain while practical and clinical skills sessions are aligned to CLOs under skills domain. In addition, sessions focusing on professional attributes of the future physician were aligned with CLOs under attributes/values domain.
This step can serve as a major part of quality assurance in the curriculum. For example, in this step each session objective was reviewed and potentially revised in term of its relevance, phrasing and for any redundancies. Session titles were also reviewed to ensure correct reflection of the covered objectives. Moreover, each session duration was confirmed to be appropriate to cover the content to be delivered and to maintain the contact and credit hours of the course. Quality assurance variables such as maintenance of the session sequence within the course without rescheduling and proper instructor selection in term of qualification are embedded in the scheduling process of each session for future use to improve and or maintain good quality delivery of these sessions.
Step 9: Review of Session Conduction Method
After fully aligning and mapping each course in term of session objectives, WLOs, CLOs and PLOs, it’s now important to ensured that appropriate instructional methods were used for each session. For example, practical activities were the instructional method used for sessions focused on psychomotor skills while small group activities were the instructional method of choice for communication skills and so on.
Step 10: Constructive Alignment of CLOs with the Assessment Methods
Assessment alignment starts in this step where CLOs are aligned with the proper assessment method based on the domain the CLO belongs to. This automatically results in each session and session objective being aligned with how it will be assessed. For example, pure knowledge CLOs which are usually taught via lectures are assessed using written exams (mainly MCQs). On the other hand, practical sessions taught in laboratories are assessed by objective structured practical exam (OSPE) and clinical skills were assessed by objective structured clinical exam (OSCE). Moreover, pre- and post-exam analysis of the items can be performed to ensure appropriateness with CLOs alignment, as well as confirming depth and breadth of coverage is achieved.
Step 11: Development of Curriculum Assessment Rubric and Blueprints
After finalizing the documents pertinent to alignment and mapping, the assessment blueprints including multiple parameters are to be developed for each assessment to ensure appropriate and comprehensive assessment of the course’s CLOs which leads to comprehensive assessment of PLOs. The assessment blueprints are crucial to ensure that all CLOs and other intended learning outcomes are covered by valid assessment.
Step 12: Alignment of Assessment Items with CLOs and Sessions
At the exam papers level, each assessment item should be mapped to the appropriate CLO and appropriate session (if possible). This ensures the ability to generate the CLO-Assessment grades sheet to produce the CLO-Assessment report which tells us student performance per CLO. This will also in turn produce the PLO-Assessment report. If assessment item mapping to session is also complete then this will provide item-level mapping to all variables mapped to sessions such as learning topics, discipline, EPAs, core clinical problems and clinical presentations. This will make it possible to provide students with multiple feedback that goes beyond a simple final course grade.
Results
The resulting benefits of the curriculum alignment and mapping are many which are summarized here.
The PLOs Align with the National Qualification Framework (NQF) and Become Homogenous Between All National Medical Colleges
As a result of the curriculum constructive alignment and mapping, the program PLOs were adopted to be in alignment with the national competencies of medical school (SaudiMED). These common PLOs ensure homogenous education of medical students across the nation as they all are educated toward achieving the same PLOs and competencies. This makes it possible to compare medical schools’ performance (benchmarking) in terms of program learning outcomes.
Revision and Amendment of Multiple CLOs
The curriculum constructive alignment and mapping process identified redundancies and deficiencies in terms of CLOs to be covered. Moreover, as medical practice is always evolving, this process was a chance to update the outdated CLOs. Redundancy in the curriculum was obvious at multiple levels and we were able to minimize this via the reported dashboard, by using sessions delivered in each parameter, and in consultation with the content experts of each course. Moreover, multiple deficiencies in the curriculum were identified and rectified. New CLOs were developed in consultation with content experts and many existing CLOs were updated.
Development of Competency View Reports
Competency view reports can show details and number of delivered sessions for each competency (Figure 2).
Figure 2.
A screen shot of the competency view of a week of a block showing details of the week learning activities.
Abbreviation: NQF, National Qualification Framework.
Development of Weekly Learning Objectives (WLOs) for All Courses
WLOs are recognized to be an important step in curriculum mapping. In PBL based curricula or in curricula where there is a weekly theme, WLOs are of great benefit to connect CLOs with the specific sessions’ objectives.
Revision of Course Content in View of CLOs
Since multiple CLOs were updated or newly developed, this resulted in the creation of new course content in terms of sessions and session objectives in order to achieve these CLOs. The content varied from knowledge-based content to skills and professionalism learning activities.
Adjustment of Teaching Methods as Necessary
The mapping and alignment process enabled us to revise the curriculum delivery plan to ensure proper CLOs and session teaching method. Throughout the process, the focus was on adjusting teaching methods to be appropriately aligned with the CLO and session topic. The selection of the appropriate instructional method was based on having more active learning and student centered as much as possible and where appropriate.
Assessment Blueprints
The curriculum map exposed assessment gaps. CLO-based blueprints were developed for the courses. Moreover, the type of assessment and its appropriateness to the CLO and the domain of learning was ensured.
PLO Assessment
Using the CLO-PLO mapping it is possible to have the PLO assessment rubric developed through aligning each CLO assessment to its appropriate PLO. This gave us the ability to have a clear and solid PLO assessment plan for the program.
Curriculum Repository
Throughout the curriculum mapping process, it’s important to document the curriculum data initially on tools such as spreadsheets but later on more sophisticated tools such as databases which can be utilized as the data source for the curriculum management system. This is of paramount importance to store, document and maintain the curriculum so that it may be used for future curriculum reviews.
Discussion
Medical Curricula are complex and require continuous revisions and update to ensure that they remain current, relevant and outcome based. Learning outcomes at different levels (program then course) are crucial to guide medical curricula design and reviews and this requires a holistic approach in viewing the medical curriculum.7
Medical curricula are in particularly complex as many competencies/PLOs are required to be achieved by graduates. These competencies range from in depth knowledge of basic sciences to advanced psychomotor and cognitive skills while maintaining high standards of professional and ethical practice. To ensure the achievement of all these competencies, proper curriculum constructive alignment and mapping is crucial. This is particularly important when each course usually requires many teaching faculty members and it’s not uncommon that gaps will develop in term of coherence and alignment of these courses. Overall, medical curricula can easily get de-aligned and fragmented unless frequent reviews of the curriculum map is practiced.
Moreover, undergraduate medical curricula aim to prepare graduates to continue their learning in postgraduate programs. A smooth transition of the learners from the undergraduate to the postgraduate phase could be achieved with proper undergraduate curriculum planning and mapping. Moreover, regular curriculum reviews and mapping give the chance to utilize the new advancements in the medical education field, such as Entrustable Professional Activities (EPAs), simulation, and E-learning. During the COVID-19 pandemic, like undergraduate education, many postgraduate programs got affected in terms of training, which highlighted the need for regular alignment of the undergraduate medical curricula with the postgraduate competencies in different environments.31,32
Curriculum alignment/mapping could be looked at as a process to review or refine an existing curriculum in addition to its utility at the curriculum design level. Overall, many benefits could be achieved from curriculum alignment and mapping, this includes the ability to clarify and review the learning outcomes at different levels, ensure and improve program coherence, eliminate redundancies while rectifying gaps, as well as align instructional and assessment methods properly to learning outcomes. This will eventually result in designing a full roadmap for the student’s journey through the curriculum. Moreover, the faculty members involved in the program will be on the same page toward achieving the PLOs of the program through each of the courses in which they teach.1,33
Curriculum constructive alignment and mapping is a tedious process with multiple challenges. A clear challenge is the lack of guidance in the literature on how it could be done. In this article we summarized the essential steps needed to develop/review a curriculum alignment mapping. In order to successfully align and map a curriculum, it is of paramount importance to have a motivated team as well as stakeholders who see and believe in the value of doing such a task. Ownership of the process must be clearly identified, moreover ownership of the courses and the role of each stakeholder needs to be clear. Agreement on how to address conflicts and vague learning outcomes is necessary.13,34
The end result of curriculum mapping should aim for clear learning outcomes at all levels. Participants should look at this task as a chance to update and improve the curriculum. By creating a curriculum map, the course outcomes must be clearly articulated, aligned with the course scope, updated based on content and latest knowledge, and reasonable to the course duration and level. Moreover, the instructional methods must be appropriate for each CLO and need to be up to date with new developments in the field, both in terms of being stimulating to students and more student-centered. Similarly, it is important to utilize the curriculum mapping process to ensure comprehensive and appropriate assessment methods for all CLOs. With comprehensive curriculum mapping, it will be possible to sequence the courses properly so that building student competencies through proper reinforcement of CLOs throughout the curriculum is achieved.8,18,35
Going through the process of curriculum alignment and mapping was a necessary exercise for our medical schools. Multiple benefits were gained including, identifying, and rectifying deficiencies and redundancies in term of content, improving CLOs to be more comprehensive and clearer, and alignment of the assessment methods properly with the course content.
Curriculum alignment and mapping is a pillar of quality assurance practice in curriculum management and it is necessary to be planned frequently enough to cope with any expected development in the fields of medicine and medical education.
This study highlighted the in-depth process of curriculum alignment and mapping; however, there are some limitations to the study. The limitations include being fully implemented on one program only and the lack of long-term follow-up of the curriculum mapping and alignment outcomes. Future longitudinal studies are needed to study the long-term effects of the adopted curriculum mapping.
Conclusions and Recommendations
Curriculum alignment and map have been adopted by our programs to reflect national strategic goals; revise learning outcomes, ensure quality, and involve various stakeholders in transparency. This article describes a stepwise approach to align and map curriculum at the undergraduate medical program level. We strongly believe that this work fills an important gap in literature in providing a usable practical guidance. Moreover, these steps will help other colleges to accomplish this task avoiding difficulties encountered in our sides. We highly recommend these steps to others.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for- profit sectors.
Ethics Approval
Not applicable as the research is curriculum related and no humans’ data included.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Harden RM. AMEE Guide No. 21: curriculum mapping: a tool for transparent and authentic teaching and learning. Med Teach. 2001;23(2):123–137. doi: 10.1080/01421590120036547 [DOI] [PubMed] [Google Scholar]
- 2.Bruinsma M, Jansen EP. Curriculum mapping: integrating multiple perspectives on the curriculum. Curric Teach. 2007;22(1):25–45. doi: 10.7459/ct/22.1.03 [DOI] [Google Scholar]
- 3.Lancaster JS. Rubric-based mapping for institutional curriculum development projects. Assess Update. 2015;27(1):8–12. doi: 10.1002/au.30011 [DOI] [Google Scholar]
- 4.UNESCO I. UNESCO international bureau of education glossary of curriculum terminology; 2013.
- 5.Prideaux D. Curriculum design. BMJ. 2003;326(7383):268–270. doi: 10.1136/bmj.326.7383.268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harden RM. AMEE Guide No. 14: outcome-based education: part 1-An introduction to outcome-based education. Med Teach. 1999;21(1):7–14. doi: 10.1080/01421599979969 [DOI] [PubMed] [Google Scholar]
- 7.Al-Eyd G, Achike F, Agarwal M, et al. Curriculum mapping as a tool to facilitate curriculum development: a new School of Medicine experience. BMC Med Educ. 2018;18(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balzer F, Hautz WE, Spies C, et al. Development and alignment of undergraduate medical curricula in a web-based, dynamic learning opportunities, objectives and outcome platform (LOOOP). Med Teach. 2016;38(4):369–377. doi: 10.3109/0142159X.2015.1035054 [DOI] [PubMed] [Google Scholar]
- 9.Kelley B, Hosp JL, Howell KW. Curriculum-based evaluation and math: an overview. Assess Eff Interv. 2008;33(4):250–256. doi: 10.1177/1534508407313490 [DOI] [Google Scholar]
- 10.Uchiyama KP, Radin JL. Curriculum mapping in higher education: a vehicle for collaboration. Innov High Educ. 2009;33(4):271–280. doi: 10.1007/s10755-008-9078-8 [DOI] [Google Scholar]
- 11.Squires D. Curriculum alignment research suggests that alignment can improve student achievement. Clear House. 2012;85(4):129–135. doi: 10.1080/00098655.2012.657723 [DOI] [Google Scholar]
- 12.Komenda M, Víta M, Vaitsis C, et al. Curriculum mapping with academic analytics in medical and healthcare education. PLoS One. 2015;10(12):e0143748. doi: 10.1371/journal.pone.0143748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arafeh S. Curriculum mapping in higher education: a case study and proposed content scope and sequence mapping tool. J Furth High Educ. 2016;40(5):585–611. doi: 10.1080/0309877X.2014.1000278 [DOI] [Google Scholar]
- 14.Bayer CR, Respress E, Willock RJ, Heiman HJ. Curriculum mapping and needs assessment to inform the training of health policy leaders. Ethn Dis. 2019;29(Suppl 2):413. doi: 10.18865/ed.29.S2.413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Changiz T, Yamani N, Tofighi S, Zoubin F, Eghbali B. Curriculum management/monitoring in undergraduate medical education: a systematized review. BMC Med Educ. 2019;19(1):1–9. doi: 10.1186/s12909-019-1495-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmed YA, Alneel S. Analyzing the curriculum of the faculty of medicine, University of Gezira using Harden’s 10 questions framework. J Adv Med Educ Prof. 2017;5(2):60. [PMC free article] [PubMed] [Google Scholar]
- 17.Salas AA, Anderson MB, LaCourse L, et al. CurrMIT: a tool for managing medical school curricula. Acad Med. 2003;78(3):275–279. doi: 10.1097/00001888-200303000-00009 [DOI] [PubMed] [Google Scholar]
- 18.Shaheen AW, Fedoriw KB, Khachaturyan S, et al. Aligning medical student curriculum with practice quality goals: impacts on quality metrics and practice capacity for students. Am J Med. 2019;132(12):1478–1483. doi: 10.1016/j.amjmed.2019.08.011 [DOI] [PubMed] [Google Scholar]
- 19.Wijngaards-de Meij L, Merx S. Improving curriculum alignment and achieving learning goals by making the curriculum visible. Int J Acad Dev. 2018;23(3):219–231. doi: 10.1080/1360144X.2018.1462187 [DOI] [Google Scholar]
- 20.Zaini RG, Bin Abdulrahman KA, Al-Khotani AA, Al-Hayani AMA, Al-Alwan IA, Jastaniah SD. Saudi Meds: a competence specification for Saudi medical graduates. Med Teach. 2011;33(7):582–584. doi: 10.3109/0142159X.2011.578180 [DOI] [PubMed] [Google Scholar]
- 21.Education and Training Evaluation Commission Saudi Arabia. Education and training evaluation commission. 2021; Available from: https://etec.gov.sa/en/productsandservices/NCAAA/AccreditationProgrammatic/Pages/Medical-Colleges.aspx. Accessed September 19, 2023.
- 22.The World Federation for Medical Education. World federation for medical education-list of agencies with recognition status or applying (2023). Available from: https://wfme.org/download/list-agencies-recognition-status-applying. Accessed February 19, 2023.
- 23.ECFMG recognized accreditation policy. Available from: https://www.ecfmg.org/accreditation/?utm_source=blog&utm_medium=news&utm_campaign=recognized-accreditation-policy-annc. Accessed February 19, 2023.
- 24.Cottrell S, Hedrick JS, Lama A, et al. Curriculum mapping: a comparative analysis of two medical school models. Med Sci Educ. 2016;26:169–174. doi: 10.1007/s40670-016-0225-z [DOI] [Google Scholar]
- 25.Gulbis K, Krüger T, Dittmar M, Peters H. Approaches to mapping an undergraduate medical curriculum to a national competency-based catalogue of learning outcomes. Med Teach. 2021;43(4):439–447. doi: 10.1080/0142159X.2020.1854704 [DOI] [PubMed] [Google Scholar]
- 26.Watson EGS, Steketee C, Mansfield K, et al. Curriculum mapping for health professions education: a typology. Foc Health Prof Educ. 2020;21(1):91–113. doi: 10.11157/fohpe.v21i1.364 [DOI] [Google Scholar]
- 27.Blumberg P. Maximizing learning through course alignment and experience with different types of knowledge. Innov High Educ. 2009;34:93–103. doi: 10.1007/s10755-009-9095-2 [DOI] [Google Scholar]
- 28.Matveev AG, Veltri NF, Zapatero EG, Cuevas NM. Curriculum mapping: a conceptual framework and practical illustration; 2010.
- 29.Linstone HA, Turoff M. The Delphi Method. MA: Addison-Wesley Reading; 1975. [Google Scholar]
- 30.Frank JR, Snell L, Sherbino JC. Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015:1–30. [Google Scholar]
- 31.Jonker G, Hoff RG, Max S, Kalkman CJ, Ten Cate O. Connecting undergraduate and postgraduate medical education through an elective EPA-based transitional year in acute care: an early project report. GMS J Med Educ. 2017;34(5). doi: 10.3205/zma001141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moldovan F, Gligor A, Moldovan L, Bataga T. The impact of the COVID-19 pandemic on the orthopedic residents: a pan-Romanian survey. Int J Environ Res Public Health. 2022;19(15):9176. doi: 10.3390/ijerph19159176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kopera-Frye K, Mahaffy J, Svare GM. 2. The map to curriculum alignment and improvement. Coll Essay Learn Teach. 2008;1:8–14. doi: 10.22329/celt.v1i0.3171 [DOI] [Google Scholar]
- 34.Rawle F, Bowen T, Murck B, Hong R. Curriculum mapping across the disciplines: differences, approaches, and strategies. Coll Essay Learn Teach. 2017;10:75–88. doi: 10.22329/celt.v10i0.4765 [DOI] [Google Scholar]
- 35.Dyjur P, Kenny N. Analyzing curriculum mapping data: enhancing student learning through curriculum redesign; 2015.