Abstract
Background:
Axillary breast tissue includes any combination of fat, nipple, areolae, and glandular tissue alongside breasts and affects 2%–6% of women and 1%–3% of men. Patients may experience functional and/or cosmetic concerns due to axillary breast tissue. There are nonsurgical options for its removal, such as CoolSculpting and Kybella, and surgical options such as liposuction, BodyTite liposuction, and excision. Determining which technique to use in each case is critical in achieving an excellent outcome. Currently, there are no established treatment algorithms for the removal of axillary breast tissue.
Methods:
A retrospective review between January 1, 2013, and June 20, 2022, was performed. Data that were extracted included age, BMI, date of procedure, procedure, fat suctioned, tissue excised, and follow-up period. The authors analyzed outcomes and formulated a treatment algorithm based on tissue type (fat versus glandular), amount of tissue excess, skin laxity, and accessory nipple presence.
Results:
A total of 43 patients (83 axillae) met our inclusion criteria and were included in our analysis. All patients were female with a mean age of 35.5 ± 10.9 years, a mean BMI of 23.0 ± 3.1, and a mean follow-up period of 8.8 ± 11.1 months. For inclusion, patients had to have undergone CoolSculpting, liposuction, BodyTite liposuction, liposuction with excision, or excision alone. All patients tolerated the procedures well and reported no serious complications.
Conclusions:
Nonsurgical and surgical removal of axillary breast tissue is safe and effective. The algorithm presented can be utilized by plastic and reconstructive surgeons to ensure optimal results for axillary breast tissue removal.
Takeaways
Question: What is the best way to manage axillary breast tissue based on skin laxity, tissue type, and the presence of accessory nipples?
Findings: Axillary breast tissue removal serves as a powerful adjunct to breast procedures. The treatment algorithm presented can be used by plastic and reconstructive surgeons to ensure optimal results. In our study, we report high patient satisfaction and no significant complications. Based on our results and current literature, nonsurgical and surgical removal of axillary breast tissue are safe and effective.
Meaning: We present an algorithm for axillary breast tissue management based on results from our retrospective study and the senior author’s clinical experience.
INTRODUCTION
Axillary breast tissue includes any combination of fat, nipple, areolae, and glandular breast tissue alongside developed breasts on the chest. This tissue is most often identified within the embryonic milk line in the embryonic mammary ridge.1 Accessory axillary breast tissue affects approximately 2%–6% of women and 1%–3% of men.2 It can be asymptomatic; however, patients may experience tenderness, swelling, limited shoulder range of motion, and irritation, which may worsen during puberty, menstruation, and/or pregnancy.3 Additionally, patients may have cosmetic concerns regarding axillary breast tissue. Unwanted axillary breast tissue can be addressed nonsurgically with CoolSculpting or Kybella (deoxycholic acid; Allergan Aesthetics, AbbVie Inc., North Chicago, Ill.) or surgically with liposuction and/or excision of the tissue. Minimally invasive energy-based technology such as the bipolar radiofrequency device, BodyTite (InMode Aesthetic Solutions), can be used simultaneously with liposuction to tighten skin and remodel adipose tissue.4
Axillary breast tissue conditions exhibit wide variability in presentation, and there is currently no established classification system to guide its management.3,5 The aim of this retrospective study was to examine the outcomes of 43 patients (83 axillae) who underwent axillary breast tissue removal using CoolSculpting (CoolMini handpiece, Allergan via Zeltiq Asthetics, Pleaston, Calif.), liposuction only, BodyTite liposuction (FaceTite handpiece, InMode Corp., Toronto, Ontario, Canada), liposuction with excision or excision alone and present an algorithm for axillary breast tissue management based on our results and the senior author’s clinical experience.
METHODS
A retrospective chart review of patients who underwent CoolSculpting, liposuction only, BodyTite liposuction, liposuction with excision, or excision alone of axillary breast tissue from January 1, 2013, to June 20, 2022, was performed. For Coolsculpting treatment, the CoolMini hand piece was applied to each axilla at −11°C. When BodyTite was used, the FaceTite hand piece was utilized. The surgical log of Dr. B. Aviva Preminger’s practice, Preminger Plastic Surgery, was reviewed. Data from patient charts that were extracted included age at the time of surgery, BMI, date of the procedure, procedure title, total fat suctioned, total tissue excised, follow-up period, and follow-up notes. The authors analyzed treatment outcomes and formulated a treatment algorithm based upon tissue type (fat, glandular tissue), skin laxity, and accessory nipple presence.
TECHNIQUES
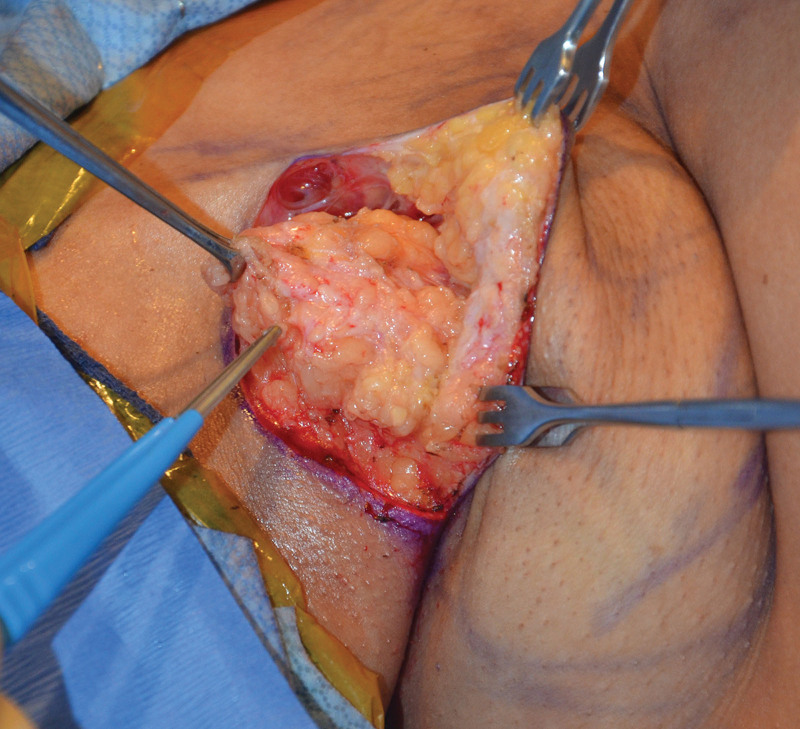
The technique used for liposuction and excision of axillary breast tissue is as follows: a #15 blade is used to make an incision in each axilla for insertion of the liposuction cannulas. The planned axillary incisions are always marked within the axillary crease, and the length of this incision depends on the amount of excess tissue present. The patient’s axillae and axilla/chest wall junction are then infiltrated with tumescent solution. (See Video 1 [online], which displays the infiltration and liposuction technique. For the infiltration, the patient's axillae and axilla/chest wall junction are infiltrated with tumescent solution. For the liposuction technique, the patient's anterior chest and chest/axilla junction are suctioned using 3–4 mm liposuction cannulas in a fanning pattern towards the tail of the breast so as to feather the junction between the anterior chest and the axillary region.) After allowing adequate time for the tumescent solution to take effect, the patient’s anterior chest and chest/axilla junction are suctioned using 3–4 mm liposuction cannulas in a fanning pattern toward the tail of the breast so as to feather the junction between the anterior chest and the axillary region (see Video 1 [online]). The skin is then redraped, and redundancy is removed in a stepwise fashion using a Gorney scissor. When BodyTite is used, the FaceTite hand piece is applied with the settings at 65°C internal and 38°C external. Average energy delivery is 2–3 kJ. A 7- to 10-cm incision is placed high within the axillary crease. A small ellipse of skin is then removed from each side along with excess axillary tissue (Figs. 1 and 2), which is removed using a combination of curved Mayo scissors to carefully elevate the skin flaps and Bovie cautery for hemostasis. (See Video 2 [online], which displays axillary tissue removal. Part 1.) (See Video 3 [online], which displays axillary tissue removal. Part 2.) Care is taken to avoid the axillary structures and lymphatics. The remaining excess skin is then removed from each axilla. (See Video 4 [online], which displays the skin removal technique and drain placement. For the skin removal, the skin is re-draped, and redundancy is removed in a stepwise fashion using a Gorney scissor. For the drain placement, a #7 flat JP drain is inserted in each axilla, brought out through the posterior aspect of the incisions, and secured in place with a 2-0 silk suture.) A #7 flat JP drain is then inserted in each axilla, brought out through the posterior aspect of the incisions, and secured in place with a 2-0 silk suture (see Video 4 [online]). The wound is closed with 3-0 Monocryl deep dermal and a running 4-0 Monocryl subcuticular suture.
Fig. 1.
Glandular breast tissue in the axillary region. This tissue is removed using a combination of curved Mayo scissors to elevate the skin flaps and Bovie cautery for hemostasis.
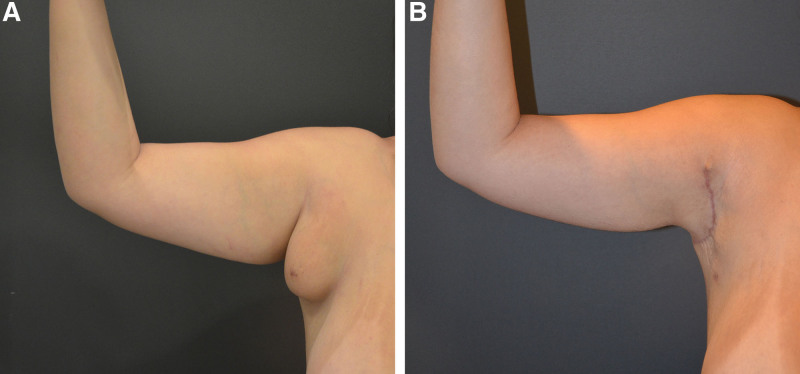
Fig. 2.
A patient with severe skin laxity, fat, and glandular tissue underwent bilateral liposuction with excision of the excess axillary breast tissue (A). The postoperative image (B) demonstrates the hidden scar placed high in the axillary crease.
Video 1. displays the infiltration and liposuction technique.
Video 2. displays axillary tissue removal. Part 1.
Video 3. displays axillary tissue removal. Part 2.
Video 4. displays the skin removal technique and drain placement.
RESULTS
A total of 43 patients (83 axillae) met our inclusion criteria and were included in our analysis. All patients were female with a mean age of 35.5 ± 10.9 years, a mean BMI of 23.0 ± 3.1, and a mean follow-up period of 8.8 ± 11.1 months. Twenty patients (58.1%) were White, 14 patients (32.6%) were Asian, and four patients (9.3%) were Hispanic. For inclusion in our study, patients had to have undergone CoolSculpting, liposuction, BodyTite liposuction, liposuction with excision, or excision alone.
Four patients (eight axillae) (mean age: 30.5 ± 3.3 years) with a mean BMI of 21.9 ± 2.4 and mean follow-up period of 14.8 ± 24.3 months underwent bilateral CoolSculpting of the axilla (Table 1). Of note, one patient who underwent one cycle of CoolSculpting to each axilla wanted a more substantial result, so she underwent tissue excision 4 years later. One patient did not see significant results, and two patients were pleased with their results after one cycle of CoolSculpting to each axilla (Table 1). Nine patients (18 axillae) (mean age: 41.2 ± 13.2 years) with a mean BMI of 22.3 ± 3.2 and mean follow-up period of 10.2 ± 15.1 months underwent bilateral liposuction only (mean fat suctioned per axilla: 131.3 ± 108.5 mL) (Table 2). Three patients (six axillae) (mean age: 42.7 ± 12.6 years) with a mean BMI of 23.0 ± 0.6 and mean follow-up period of 1.5 ± 0.7 months underwent bilateral BodyTite liposuction treatment (mean fat suctioned per axilla: 166.7 ± 143.8 mL; mean energy applied per axilla: 2.9 ± 2.3kJ (Table 3). Twenty patients (48 axillae) (mean age: 34.5 ± 9.3 years) with a mean BMI of 23.6 ± 3.2 and mean follow-up period of 4.9 ± 5.2 months underwent liposuction (mean fat suctioned per axilla: 208.2 ± 147.6 mL) and excision (mean tissue excised per axilla: 40.4 ± 36.5 g) of axillary breast tissue (Table 4). In this group, 24 patients underwent bilateral removal of axillary breast tissue, and two patients underwent unilateral procedures. One patient in this group underwent unilateral excision of the left accessory nipple and one patient underwent bilateral excision of accessory nipples. Additionally, one patient (two axillae) underwent bilateral excision of excess axillary breast tissue, and one patient (one axilla) underwent unilateral excision of excess axillary breast tissue (Table 5).
Table 1.
Excess Axillary Breast Tissue Treatment with CoolSculpting
| Patient | Age | BMI | No. Treatments |
|---|---|---|---|
| 1 | 28 | 20.3 | 1 |
| 2 | 28 | 21.9 | 1 |
| 3 | 35 | 25.2 | 1 |
| 4 | 31 | 20.1 | 1 |
Table 2.
Excess Axillary Breast Tissue Removal with Liposuction Only
| Patient | Age | BMi | Fat Suctioned R (mL) | Fat Suctioned L (mL) | Total Fat Suctioned (mL) |
|---|---|---|---|---|---|
| 5 | 60 | 24.6 | 100 | 100 | 200 |
| 6 | 44 | 22.7 | 400 | 400 | 800 |
| 7 | 38 | 17.1 | 55 | 55 | 110 |
| 8 | 42 | 23.2 | 50 | 50 | 100 |
| 9 | 62 | 20.4 | 100 | 100 | 200 |
| 10 | 37 | 19.1 | 100 | 100 | 200 |
| 11 | 39 | 25.2 | 150 | 100 | 250 |
| 12 | 25 | 21.2 | 120 | 120 | 240 |
| 13 | 24 | 27.5 | 150 | 150 | 300 |
Table 3.
Excess Axillary Breast Tissue Removal with BodyTite Liposuction
| Patient | Age | BMI | Fat Suctioned R (mL) | Fat Suctioned L (mL) | Total Fat Suctioned (mL) | Energy R (kJ) | Energy L (kJ) | Total Energy (kJ) |
|---|---|---|---|---|---|---|---|---|
| 14 | 56 | 22.9 | 350 | 350 | 700 | 1.2 | 1.2 | 2.4 |
| 15 | 31 | 22.4 | 50 | 50 | 100 | N/A | N/A | N/A |
| 16 | 41 | 23.6 | 100 | 100 | 200 | 6 | 3 | 9 |
N/A, value not recorded.
Table 4.
Excess Axillary Breast Tissue Removal with Liposuction and Excision
| Patient | Age | BMI | Fat Suctioned R (mL) | Fat Suctioned L (mL) | Total Fat Suctioned (mL) | Tissue Excised R (g) | Tissue Excised L (g) | Total Tissue Excised (g) |
|---|---|---|---|---|---|---|---|---|
| 1 | 32 | 20.3 | 100 | 200 | 300 | 38 | 17 | 55 |
| 17 | 41 | 23.6 | 100 | 100 | 200 | 26 | 0 | 26 |
| 18 | 41 | 26.3 | 175 | 175 | 350 | 89 | 90 | 179 |
| 19 | 28 | 21.6 | 150 | 150 | 300 | 38 | 16 | 54 |
| 20 | 31 | 21.7 | 175 | 200 | 375 | 21 | 8 | 29 |
| 21 | 23 | 24.1 | 150 | 150 | 300 | 16 | 9 | 25 |
| 22 | 29 | 21 | 200 | 200 | 400 | 17 | 22 | 39 |
| 23 | 30 | 20 | 200 | 200 | 400 | 22 | 12 | 34 |
| 24 | 47 | 24.3 | 0 | 300 | 300 | N/A | N/A | N/A |
| 25 | 23 | 23.4 | N/A | N/A | 950 | 47 | 39 | 86 |
| 26 | 57 | 25.5 | N/A | N/A | 350 | N/A | N/A | N/A |
| 27 | 16 | 19.1 | N/A | N/A | 100 | N/A | N/A | N/A |
| 28 | 32 | 21.8 | 175 | 175 | 350 | 46 | 40 | 86 |
| 29 | 37 | 25.5 | 125 | 125 | 250 | 23 | 28 | 51 |
| 30 | 29 | 24.3 | 160 | 200 | 360 | 27 | 26 | 53 |
| 31 | 28 | 20.1 | 125 | 100 | 225 | 15 | 14.8 | 29.8 |
| 32 | 45 | 20.2 | 200 | 200 | 400 | 7.8 | 6.1 | 13.9 |
| 33 | 31 | 23.6 | 175 | 175 | 350 | 10 | 15 | 25 |
| 34 | 44 | 24.9 | 700 | 850 | 1500 *includes bra roll and axilla* | N/A | N/A | N/A |
| 35 | 33 | 19.36 | 200 | 100 | 300 | N/A | N/A | N/A |
| 36 | 38 | 26.2 | 350 | 250 | 600 | 140 | 130 | 270 |
| 37 | 49 | 31.1 | 380 | 320 | 700 *includes bra roll and axilla* | 109 | 90 | 199 |
| 38 | 29 | 27.8 | 350 | 0 | 350 | 88 | 0 | 88 |
| 39 | 40 | 30 | 200 | 200 | 400 | 64 | 95 | 158 |
| 40 | 30 | 23.1 | 200 | 200 | 400 | 63 | 50 | 113 |
N/A, value not recorded.
Table 5.
Excess Axillary Breast Tissue Removal with Excision Only
| Patient | Age | BMI | Tissue Excised R (g) | Tissue Excised L (g) | Total Tissue Excised (g) |
|---|---|---|---|---|---|
| 41 | 20 | 21.6 | 0 | 13 | 13 |
| 42 | 18 | 16.8 | 155 | 130 | 285 |
All patients tolerated the procedures well and reported no serious complications. In the liposuction with excision group, four patients presented with hypertrophy and hyperpigmentation of scars. Scars were injected with Kenalog to improve their appearance. Four patients presented with seromas of the axilla at 2 weeks postoperative, which all resolved after aspiration. Additionally, two patients experienced stiffness in both arms after surgery which resolved with routine exercises.
DISCUSSION
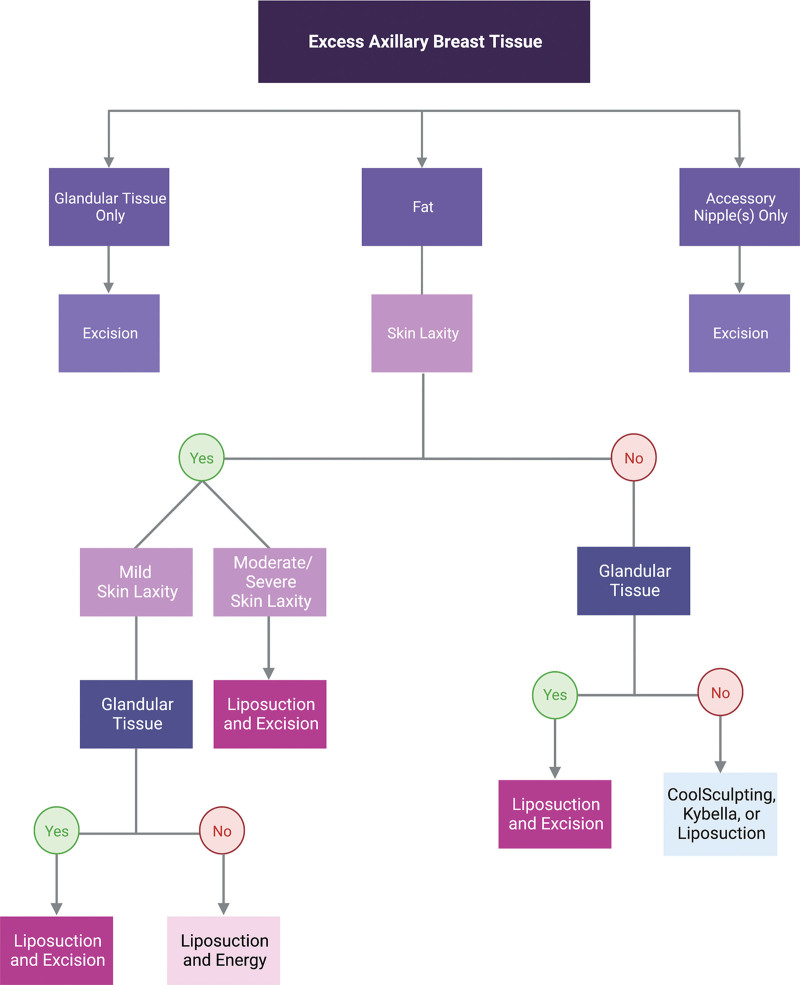
Given the cosmetic and functional concerns associated with unwanted axillary breast tissue, it can and should be addressed by plastic and reconstructive surgeons. Current literature supports that accessory axillary breast tissue is found in approximately 2%–6% of women and 1%–3% of men.2 The significant prevalence of axillary breast tissue warrants attention and treatment, as it may be functionally bothersome and cosmetically unappealing. Currently, there are no established guidelines for the application of various methods for the removal of axillary breast tissue. A classification system for polymastia was published in 1915 by Kajava, however, concordant treatment options were not elucidated.2 Previous studies have described utilizing liposuction and/or excision for the removal of axillary breast tissue; however, this study offers guidance for how to best apply different treatment modalities for axillary breast tissue removal based on tissue type and skin laxity (Fig. 3).3,5,6
Fig. 3.
Algorithm for excess axillary breast tissue management.
There are multiple treatment options for axillary breast tissue removal, including noninvasive, nonsurgical techniques such as CoolSculpting and Kybella, and surgical options such as liposuction and excision. Of note, CoolSculpting and Kybella are not FDA approved for this indication; however, their application may be appropriate in certain patients depending on the patient’s presentation and expectations. Additionally, surgeons may choose to utilize energy-based devices such as BodyTite (InMode Aesthetic Solutions), a bipolar radiofrequency device for skin tightening.
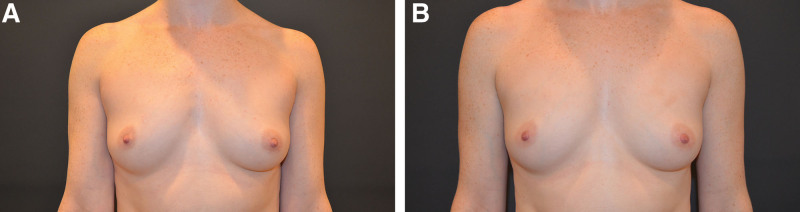
When determining the appropriate treatment for axillary breast tissue removal, surgeons must consider the amount and type of tissue, skin laxity, and patient expectations. If the axillary breast tissue is solely comprised of fat with no skin laxity, we consider this “grade 1” (Fig. 4), and suggest CoolSculpting, Kybella, or liposuction for treatment (Table 6). For noninvasive treatments such as CoolSculpting or Kybella, patients must be made aware that multiple treatments may be necessary to achieve their desired results. Interestingly, no patients chose to undergo Kybella, although it was offered in all instances after the product was approved by the FDA in 2015. It is important to note that in our study, one patient who underwent CoolSculpting wanted a more substantial result; therefore, she underwent tissue excision four years later.
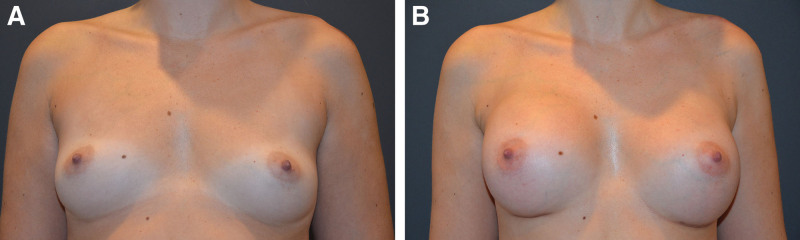
Fig. 4.
Grade 1 axillary breast tissue. Grade 1 before (A) and after (B) treatment. Patient with no skin laxity and minimal fat underwent bilateral CoolSculpting for removal of excess axillary breast tissue.
Table 6.
Classification of Axillary Breast Tissue and Management Algorithm
| Skin Laxity | Fat | Glandular Tissue/Accessory Nipple | Intervention | |
|---|---|---|---|---|
| Grade 1 | + | Coolsculpting, Kybella, Liposuction | ||
| Grade 2 | + | + | Liposuction and energy (BodyTite liposuction) | |
| Grade 3 | ++ | + | Liposuction and excision | |
| Grade 4 | +++ | ++ | + | Excision ± liposuction |
+ = mild.
++ = moderate.
+++ = severe.
For patients with axillary breast tissue comprised of fat with mild skin laxity, we consider this “grade 2” (Fig. 5) and recommend energy-based technology application such as BodyTite liposuction (InMode Aesthetic Solutions) (Table 6). This bipolar radiofrequency device delivers a controlled amount of energy to the treatment area, resulting in fat liquefaction, improved hemostasis, and skin tightening.7 Because skin laxity cannot be effectively addressed with liposuction alone, it is helpful when energy-based treatment is simultaneously applied for improved results.
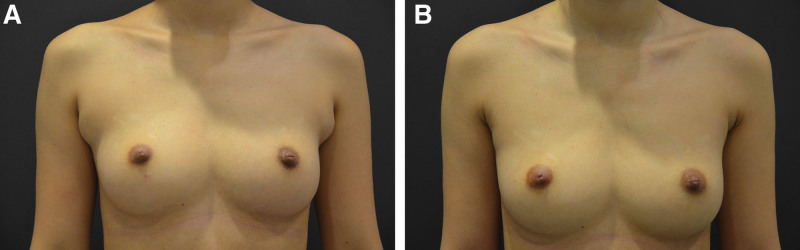
Fig. 5.
Grade 2 axillary breast tissue. Grade 2 before (A) and after (B) treatment. Patient with mild skin laxity and fat underwent bilateral BodyTite liposuction for removal of excess axillary breast tissue. The patient also underwent bilateral breast augmentation at the same time as the removal of axillary breast tissue.
If there is moderate skin laxity and fat in the axilla, we consider this “grade 3” (Fig. 6) and suggest liposuction with excision (Table 6). For patients with considerable skin laxity, liposuction with excision is the gold standard surgical option.6 For patients with severe skin laxity, fat, and glandular tissue in the axilla, we consider this “grade 4” (Fig. 7), and suggest liposuction with excision. Glandular tissue is generally not amenable to liposuction alone; therefore, concurrent excision is necessary to remove unwanted tissue.8 If there is only glandular tissue and/or accessory nipples, surgical excision is recommended (Fig. 8).
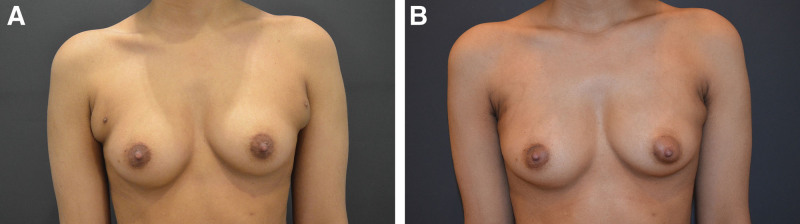
Fig. 6.
Grade 3 axillary breast tissue. Grade 3 before (A) and after (B) treatment. Patient with moderate skin laxity and fat underwent bilateral liposuction with excision of excess axillary breast tissue.
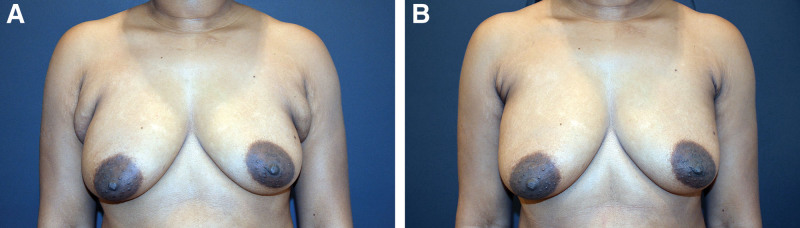
Fig. 7.
Grade 4 axillary breast tissue. Grade 4 before (A) and after (B) treatment. Patient with severe skin laxity, fat, and glandular tissue underwent bilateral liposuction with excision of the excess axillary breast tissue.
Fig. 8.
Axillary breast tissue with bilateral accessory nipples. Before (A) and after (B) treatment. Patient with bilateral accessory nipples underwent bilateral excision of axillary nipples and excess axillary breast tissue.
In addition to applying this algorithm, as always, plastic surgeons must consider patient goals and expectations. The patient’s tolerance for a scar must be balanced against the desire for complete removal. However, as evidenced by the disproportionate number of patients who chose to proceed with excision in our study, it seems that most patients seeking this treatment are willing to accept scars in exchange for a more substantial result.
LIMITATIONS
This study was conducted as a single center retrospective study, limited to a single surgeon’s experience. Follow-up times were variable between patients. Additionally, there was no objective measurement of patient satisfaction. Patient satisfaction described in this article is subjective. Future studies should elucidate patient satisfaction in an objective manner.
CONCLUSIONS
Axillary breast tissue removal has become popular in the senior author’s practice, and it is commonly performed alone or at the same time as other breast procedures such as breast augmentation, mastopexy, and breast reduction. Axillary breast tissue removal serves as a powerful adjunct to breast procedures. In our study, we report no significant complications, and a high level of patient satisfaction. Based on our results, as well as current literature, nonsurgical and surgical removal of axillary breast tissue is safe and effective. The treatment algorithm presented in this article can be utilized by plastic and reconstructive surgeons to ensure optimal results.
DISCLOSURES
Dr. Aviva Preminger is a consultant for InMode. The other authors have no financial interest to declare.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Loukas M, Clarke P, Tubbs RS. Accessory breasts: a historical and current perspective. Am Surg. 2007;73:525–528. [PubMed] [Google Scholar]
- 2.Patel PP, Ibrahim AM, Zhang J, et al. Accessory breast tissue. Eplasty. 2012;12:ic5. [PMC free article] [PubMed] [Google Scholar]
- 3.Lesavoy MA, Gomez-Garcia A, Nejdl R, et al. Axillary breast tissue: clinical presentation and surgical treatment. Ann Plast Surg. 1995;35:356–360. [PubMed] [Google Scholar]
- 4.Dayan E, Chia C, Burns AJ, et al. Adjustable depth fractional radiofrequency combined with bipolar radiofrequency: a minimally invasive combination treatment for skin laxity. Aesthetic Surg J. 2019;39:S112–S119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartsich SA, Ofodile FA. Accessory breast tissue in the axilla: classification and treatment. Plast Reconstr Surg. 2011;128:35e–36e. [DOI] [PubMed] [Google Scholar]
- 6.Hwang SB, Choi BS, Byun GY, et al. Accessory axillary breast excision with liposuction using minimal incision: a preliminary report. Aesthetic Plast Surg. 2017;41:10–18. [DOI] [PubMed] [Google Scholar]
- 7.Theodorou SJ, Paresi RJ, Chia CT. Radiofrequency-assisted liposuction device for body contouring: 97 patients under local anesthesia. Aesthetic Plast Surg. 2012;36:767–779. [DOI] [PubMed] [Google Scholar]
- 8.Fagerlund A, Lewin R, Rufolo G, et al. Gynecomastia: a systematic review. J Plast Surg Hand Surg. 2015;49:311–318. [DOI] [PubMed] [Google Scholar]