Introduction
Nearly 10.0 per cent of patients undergoing cholecystectomy for lithiasis have one or more stones in the common bile duct (CBD)1,2. In patients with asymptomatic CBD stones with a non-dilated CBD, the main options are either early endoscopic sphincterotomy (ES) or long-term expectant management3–10. Expectant management is based on the principle of spontaneous duodenal passage of stones, with transcystic drain (TCD) placement during cholecystectomy and postoperative cholangiography to check the CBD. ES is then only indicated for patients with stones still present at the 6-week cholangiography9,10.
The aim of this study was to assess the efficacy of long-term expectant management and to identify factors associated with failure of this strategy.
Methods
This is a retrospective single-centre cohort study in a teaching hospital. According to the General Data Protection Regulation, this study was registered in the register of retrospective studies of our centre (register number: RnIPH 2021-53) and cover by the MR-004 (CNIL number: 2206723 v 0).
Setting and participants
All consecutive patients admitted for laparoscopic cholecystectomy with CBD stones in non-dilated CBD discovered during intraoperative cholangiography from 1 January 2010 to 31 December 2020 at our centre were included.
Eligibility criteria
The inclusion criteria were an intraoperative cholangiography carried out, at least one CBD stone, laparoscopic approach, non-dilated CBD (<8 mm) and TCD placement. The exclusion criteria were severe cholangitis, ES before surgical treatment, immediate laparotomy and transcystic stone extraction.
Outcomes
The success of expectant management was defined by CBD clearance at 6 weeks. The failure of the strategy was defined by the need for a postoperative ES. All patients were followed up until complete CBD clearance.
Study variables and measurements
Data were collected retrospectively and came from electronic patient records.
Cholecystectomy procedure
Cholecystectomy was carried out laparoscopically using a standardized technique11,12. An intraoperative cholangiogram was done systematically. In patients with CBD stones, a TCD (PVC ESCAT, Coloplast) was placed during cholecystectomy, fixed to the cystic duct with an absorbable wire single stitch, with a diameter adapted to the cystic duct diameter.
Postoperative management
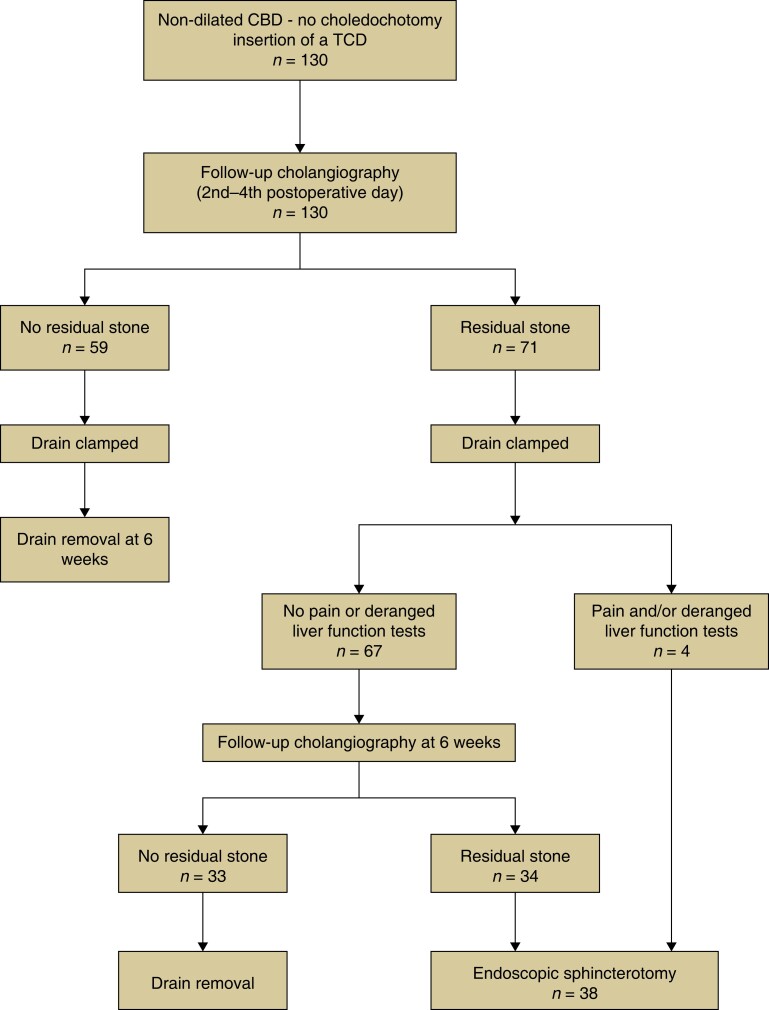
The expectant management was standardized and is reported in Fig. 1.
Fig. 1.
Long-term expectant management of common bile duct stones in non-dilated common bile duct
This figure summarizes the postoperative management of patients undergoing long-term expectant management. Endoscopic sphincterotomy is only for patients with residual stones at 6 weeks, or in case of pain and/or abnormal liver test after drain clamping.
Statistical analysis
To seek predictive factors for the success or failure of expectant management, univariate analyses were carried out with a Pearson chi-squared test or a Fisher’s exact test for qualitative variables, and by a Mann–Whitney–Wilcoxon test for quantitative variables, using the ES variable as the variable to be explained. Statistical analyses were performed using STATA software. All statistical tests were bilateral with a significance threshold of 5 per cent.
Results
Between January 2010 and December 2020, 3762 cholecystectomies were carried out at our centre. Four hundred and ninety patients (13.0 per cent) had one or more CBD stones. Following selection criteria, 130 patients having received expectant management were included.
Preoperative and intraoperative characteristics (Table 1)
Table 1.
Preoperative and postoperative characteristics between success and failure of long-term expectant management—univariable analysis
| Total (n = 130) | Successful expectant management (n = 92) | Failed expectant management (n = 28) | P | |
|---|---|---|---|---|
| Sex (n, %) | ||||
| Female | 54 (41.5) | 40 (43.5) | 14 (36.8) | 0.480 |
| Male | 76 (58.5) | 52 (56.5) | 24 (63.2) | |
| Age (years, mean(s.d.)) | 55.5 (11.3) | 54.3 (16.7) | 58.4 (20.0) | 0.160 |
| BMI (mean(s.d.)) | 27.5 (5) | 27.9 (5.18) | 26.7 (5.07) | 0.120 |
| ASA score (n, %) | ||||
| 1 | 53 (40.8) | 39 (42.4) | 14 (36.8) | 0.520 |
| 2 | 53 (40.8) | 37 (40.2) | 16 (42.1) | |
| 3 | 24 (18.4) | 16 (17.4) | 8 (21.1) | |
| Charlson score (mean(s.d.)) | 2.3 (2.36) | 2.1 (2.27) | 2.84 (2.53) | 0.097 |
| Previous abdominal surgery (n, %) | ||||
| No | 97 (74.6) | 74 (80.4) | 23 (60.5) | 0.018 |
| Yes | 33 (25.4) | 18 (19.6) | 15 (39.5) | |
| Emergency presentation (n, %) | ||||
| No | 74 (56.9) | 53 (57.6) | 21 (55.3) | 0.810 |
| Yes | 56 (43.1) | 39 (42.4) | 17 (44.7) | |
| Clavien–Dindo score at initial admission (n, %) | ||||
| No complication | 107 (82.3) | 81 (88.0) | 26 (68.4) | <0.010 |
| I | 12 (9.2) | 8 (8.7) | 4 (10.5) | |
| II | 5 (3.8) | 1 (1.1) | 4 (10.5) | |
| IIIb | 4 (3.1) | 1 (1.1) | 3 (7.9) | |
| IVa | 1 (0.8) | 0 (0.0) | 1 (2.7) | |
| V | 1 (0.8) | 1 (1.1) | 0 (0.0) | |
| Clamped drain at the end of initial admission (n, %) | ||||
| No | 8 (6.3) | 4 (4.4) | 4 (10.8) | 0.230 |
| Yes | 120 (93.7) | 87 (95.6) | 33 (89.2) | |
| Missing | 1 | 0 | 1 | |
| Complication at drain clamping (n, %) | ||||
| No | 120 (96.8) | 87 (97.8) | 33 (94.3) | 0.320 |
| Yes | 4 (3.2) | 2 (2.2) | 2 (5.7) | |
| Missing | 5 | 2 | 3 | |
| Initial length of stay (days, mean(s.d.)) | 7.5 (4.52) | 7.1 (4.74) | 8.2 (3.87) | 0.032 |
| Readmission (n, %) | ||||
| No | 115 (89.1) | 87 (95.6) | 28 (73.7) | <0.001 |
| Yes | 14 (10.9) | 4 (4.4) | 10 (26.3) | |
| Time between drain insertion and removal (days, mean(s.d.)) | 51.1 (19.3) | 45.6 (14.1) | 64.6 (23.4) | <0.001 |
| Complication at drain removal (n, %) | ||||
| No | 114 (89.1) | 80 (87.9) | 34 (91.9) | 1 |
| Pain | 9 (7.0) | 7 (7.7) | 2 (5.4) | |
| Biliary peritonitis | 5 (3.9) | 4 (4.4) | 1 (2.7) | |
| Missing | 1 | 0 | 1 | |
| Clavien–Dindo score at readmission after drain removal (n, %) | ||||
| No complication | 1 (9.0) | 1 (12.5) | 0 (0.0) | 1 |
| I | 5 (45.5) | 3 (37.5) | 2 (66.7) | |
| IIIb | 5 (45.5) | 4 (50.0) | 1 (33.3) | |
| Total number of admissions (n, %) | ||||
| 1 | 88 (67.7) | 80 (87.0) | 8 (21.1) | <0.001 |
| 2 | 32 (24.6) | 12 (13.0) | 20 (52.6) | |
| 3 | 8 (6.2) | 0 (0.0) | 8 (21.1) | |
| 4 | 2 (1.5) | 0 (0.0) | 2 (5.2) | |
| Cumulative length of stay (days, mean(s.d.)) | 8.8 (5.45) | 7.7 (5.20) | 11.5 (5.16) | <0.001 |
| Number of procedures under GA (n, %) | ||||
| 1 | 87 (66.9) | 87 (94.6) | 0 (0.0) | <0.001 |
| 2 | 36 (27.7) | 5 (5.4) | 31 (81.6) | |
| Initial operation + reoperation | 5 | 5 | 0 | |
| Initial operation + ES | 31 | 0 | 31 | |
| ≥ 3 | 7 (5.4) | 0 (0.0) | 7 (18.4) | |
| Initial operation + reoperation + 1 ES | 4 | 0 | 4 | |
| Initial operation + 2 ES | 1 | 0 | 1 | |
| Initial operation + ES + stent removal | 2 | 0 | 2 | |
| Overall Clavien–Dindo score (n, %) | ||||
| No complications | 86 (66.2) | 71 (77.2) | 15 (39.5) | <0.001 |
| I | 20 (15.3) | 12 (13.0) | 8 (21.1) | |
| II | 10 (7.7) | 3 (3.3) | 7 (18.4) | |
| IIIa | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| IIIb | 12 (9.2) | 5 (5.4) | 7 (18.4) | |
| IVa | 1 (0.8) | 0 (0.0) | 1 (2.6) | |
| V | 1 (0.8) | 1 (1.1) | 0 (0.0) | |
| Comprehensive Complication Index (mean(s.d.)) | 7.4 (14.2) | 4.8 (13.2) | 13.6 (14.6) | <0.001 |
| Number of deaths after 6 weeks (n, %) | 1 (0.8) | 1 (1.1) | 0 (0.0) | 1 |
ES, endoscopic sphincterotomy; GA, general anaesthesia.
The mean age was 55 years, with 13.1 per cent of patients over 75 years. Patients were mostly ASA2 (59.2 per cent). Management was carried out as an emergency in 43.1 per cent of cases. Conversion to laparotomy was required in 11 patients (8.5 per cent).
Success of the procedure
Successful long-term expectant management was achieved in 92 patients (70.8 per cent).
Morbidity and mortality rates (Table 1)
The immediate postoperative morbidity rate was 17.7 per cent, with 13.1 per cent minor complications (Clavien–Dindo score ≤2; (n= 17)). Medical complications occurred in 10 patients (58.8 per cent) and complications associated with surgery in 7 patients (41.2 per cent). The rate of reoperation was 3.1 per cent (n = 4), all due to biliary peritonitis and all performed by laparoscopy.
Fourteen patients (10.8 per cent) needed to be readmitted to hospital in the period between surgery and drain removal, without revision surgery.
At TCD removal at 6 weeks, 10.8 per cent of patients (n = 14) presented had a complication, with biliary peritonitis requiring surgical revision for 5 patients (3.8 per cent), all performed by laparoscopy.
Overall morbidity rate at the end of treatment (6 weeks) was 33.8 per cent, with 23.1 per cent minor complications and 9.2 per cent reoperations (n = 12). The mean comprehensive complication index (CCI), reflecting the cumulative morbidity rate, was therefore 7.4.
Immediate and 6-week postoperative death occurred in 1 patient (0.8 per cent), who died following respiratory distress due to cancer recurrence.
Failure of the procedure and factors associated with failure
Long-term expectant management failed in 38 patients (29.2 per cent). All these patients underwent ES, resulting in a higher total number of hospital admissions: only 11 patients (28.9 per cent) were treated with ES during the same admission as cholangiography at 6 weeks. Consequently, the mean length of stay and the number of procedures under general anaesthesia (GA) were significantly higher in this subgroup (Table 1).
Factors associated with failure of the expectant management found to be significant in univariable analysis (Table 1) were the occurrence of a complication in the early postoperative period (31.6 per cent versus 12.0 per cent, P < 0.010) and the need for readmission in the period between surgery and removal of the drain (26.3 per cent versus 4.4 per cent, P < 0.001). Preoperative factors, such as biochemistry, were not predictive of failure in univariable analysis. The numbers were too small for predictive factors to proceed to a multivariable analysis.
Endoscopic management
ES following failure of long-term expectant management was carried out in 38 patients (29.2 per cent). ES did not find any residual stone in 23.7 per cent of cases (n = 9). Six patients (15.8 per cent) presented a complication post-ES: 2.6 per cent acute pancreatitis (n = 1); 5.3 per cent haemorrhage (n = 2); 7.9 per cent cholangitis (n = 3).
Discussion
The long-term expectant management allowed CBD clearance without any additional procedure in 70.8 per cent of cases.
One of the main problems is the placement of a TCD with its own specific morbidity rate. Indeed, revision surgery for biliary peritonitis was needed due to displacement of the TCD in 3.1 per cent of cases (4 patients) during the initial admission, or during removal of the TCD in 3.8 per cent of cases (5 patients).
In this study, only 29.2 per cent of patients underwent an ES to achieve CBD clearance (n = 38). This resulted in pancreatitis (2.6 per cent) and haemorrhage (5.3 per cent). In 23.7 per cent of patients (n = 9), no residual stone was found. These figures are similar to those found in the literature13–17. In 2.6 per cent of cases, it was necessary to perform more than one ES, which increases the risk of complications, the number of general anaesthetics, admission, and costs.
The use of systematic intraoperative cholangiogram during cholecystectomy at our centre precludes the need for expensive preoperative tests to detect CBD stones, such as magnetic resonance cholangiopancreatography (MRCP), which can be difficult to access in some institutions. Intraoperative cholangiography is relatively quick and easy and available to most gastrointestinal surgeons, unlike intraoperative ultrasound, for example. Long-term expectant management could avoid unnecessary endoscopic management, with its own associated morbidity rate. Postoperative assessment by cholangiography through TCD is quick, minimally invasive, and inexpensive.
This study complements the only two previous studies on the long-term expectant management in the literature9,10. The difference in morbidity rate could be explained by a higher, possibly more representative number of included patients, and by the preoperative characteristics of included patients (older and more co-morbid). These three series confirm that long-term expectant management is an option in patients with CBD stones in non-dilated CBD discovered incidentally at intraoperative cholangiogram and could avoid unnecessary endoscopic management. However, management could be optimized by doing ES before 6 weeks in patients with immediate complications or complications requiring readmission.
There are limitations inherent to a study that is single centre and retrospective. However, management was standardized within an expert team in biliary laparoscopic surgery1,18,19, limiting confounding factors and interpretive bias.
Contributor Information
Julien Pouplin, Department of Digestive Surgery and Transplantation, Toulouse University Hospital, Toulouse, France.
Charlotte Maulat, Department of Digestive Surgery and Transplantation, Toulouse University Hospital, Toulouse, France.
Gabriel Yubero, Department of Epidemiology, Toulouse University Hospital, Toulouse, France.
Jason Shourick, Department of Epidemiology, Toulouse University Hospital, Toulouse, France.
Emmanuel Cuellar, Department of Digestive Surgery and Transplantation, Toulouse University Hospital, Toulouse, France.
Adrian Culetto, Department of Gastroenterology, Toulouse University Hospital, Toulouse, France.
Fanny Castanet, Department of Digestive Surgery and Transplantation, Toulouse University Hospital, Toulouse, France.
Karl Barange, Department of Gastroenterology, Toulouse University Hospital, Toulouse, France.
Louis Buscail, Department of Gastroenterology, Toulouse University Hospital, Toulouse, France.
Nicolas Carrere, Department of Digestive Surgery and Transplantation, Toulouse University Hospital, Toulouse, France.
Jean-Marie Peron, Department of Gastroenterology, Toulouse University Hospital, Toulouse, France.
Bertrand Suc, Department of Digestive Surgery and Transplantation, Toulouse University Hospital, Toulouse, France.
Barbara Bournet, Department of Gastroenterology, Toulouse University Hospital, Toulouse, France.
Fabrice Muscari, Department of Digestive Surgery and Transplantation, Toulouse University Hospital, Toulouse, France.
Author contributions
Julien Pouplin (Study design, Data collection, Data analysis, Writing, Review and editing), Charlotte Maulat (Conceptualization, Methodology, Supervision), Gabriel Yubero (Methodology, Conceptualization, Data analysis), Jason Shourick (Methodology, Conceptualization, Data analysis), Emmanuel Cuellar (Study design, Review and editing), Adrian Culetto (Review and editing), Fanny Castanet (Review and editing), Karl Barange (Review and editing), Louis Buscail (Study design, Review and editing), Nicolas Carrere (Review and editing), Jean-Marie Peron (Review and editing), Bertrand Suc (Study design, Writing, Supervision, Review and editing), Barbara Bournet (Review and editing) and Fabrice Muscari (Study design, Writing, Supervision, Review and editing).
Funding
None.
Conflict of interest
The authors declare no conflict of interest.
Data availability
The data sets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
- 1. Payen JL, Muscari F, Vibert É, Ernst O, Pelletier G. Lithiase biliaire. Presse Méd 2011;40:567–580 [DOI] [PubMed] [Google Scholar]
- 2. Tazuma S. Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol 2006;20:1075–1083 [DOI] [PubMed] [Google Scholar]
- 3. Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M. Guidelines on the management of common bile duct stones (CBDS). Gut 2008;57:1004–1021 [DOI] [PubMed] [Google Scholar]
- 4. Scientific Committee of the European Association for Endoscopic Surgery (E.A.E.S.) . Diagnosis and treatment of common bile duct stones (CBDS). Results of a consensus development conference. Surg Endosc 1998;12:856–864 [PubMed] [Google Scholar]
- 5. EASL . EASL Clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 2016;65:146–181 [DOI] [PubMed] [Google Scholar]
- 6. Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster Get al. Updated guideline on the management of common bile duct stones (CBDS). Gut 2017;66:765–782 [DOI] [PubMed] [Google Scholar]
- 7. Phillips EH, Toouli J, Pitt HA, Soper NJ. Treatment of common bile duct stones discovered during cholecystectomy. J Gastrointest Surg 2008;12:624–628 [DOI] [PubMed] [Google Scholar]
- 8. Rosseland AR, Glomsaker TB. Asymptomatic common bile duct stones. Eur J Gastroenterol Hepatol 2000;12:1171–1173 [DOI] [PubMed] [Google Scholar]
- 9. Balandraud P, Biance N, Peycru T, Tardat E, Bonnet PM, Cazeres Cet al. Fortuitous discovery of common bile duct stones: results of a conservative strategy. Gastroentérologie Clin Biol 2008;32:408–412 [DOI] [PubMed] [Google Scholar]
- 10. Collins C, Maguire D, Ireland A, Fitzgerald E, O’Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg 2004;239:28–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 2010;211:132–138 [DOI] [PubMed] [Google Scholar]
- 12. Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJet al. Tokyo guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepato-Biliary-Pancreat Sci 2018;25:73–86 [DOI] [PubMed] [Google Scholar]
- 13. El Nakeeb A, Geidie A E, Hanafy E E, Atef E, Askar W, Sultan AMet al. Management and outcome of borderline common bile duct with stones: a prospective randomized study. J Laparoendosc Adv Surg Tech 2016;26:161–167 [DOI] [PubMed] [Google Scholar]
- 14. Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RCG, Meyers WCet al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991;37:383–393 [DOI] [PubMed] [Google Scholar]
- 15. Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis Fet al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 1998;48:1–10 [DOI] [PubMed] [Google Scholar]
- 16. Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli Met al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol 2001;96:417–423 [DOI] [PubMed] [Google Scholar]
- 17. Tranter SE, Thompson MH. Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg 2002;89:1495–1504 [DOI] [PubMed] [Google Scholar]
- 18. Suc B. Surgery vs endoscopy as primary treatment in symptomatic patients with suspected common bile duct stones: a multicenter randomized trial. Arch Surg 1998;133:702. [DOI] [PubMed] [Google Scholar]
- 19. Muscari F, Delebecq T, Foppa B, Suc B. Prise en charge de la lithiase de la voie biliaire principale. J Chir (Paris) 2006;143:148–154 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated and/or analysed during the current study are available from the corresponding author on reasonable request.