Abstract
Background
There is evidence that community-based palliative care programmes can improve patient outcomes and caregiver experiences cost-effectively. However, little is known about which specific components within these programmes contribute to improving the outcomes.
Aim
To systematically review research that evaluates the effectiveness of community-based palliative care components.
Design
A systematic mixed studies review synthesising quantitative, qualitative and mixed-methods study findings using Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. PROSPERO: ID # CRD42022302305.
Data sources
Four databases were searched in August 2021 (CINAHL, Web of Science, ProQuest Federated and PubMed including MEDLINE) and a close review of included article references. Inclusion criteria required articles to evaluate a single, specific component of a community-based palliative care programme either within an individual programme or across several programmes.
Results
Overall, a total of 1,674 articles were identified, with 57 meeting the inclusion criteria. Of the included studies, 21 were qualitative, 25 were quantitative and 11 had mixed methods. Outcome measures consistently examined included patient/caregiver satisfaction, hospital utilisation and home deaths. The components of standardised sessions (interdisciplinary meetings about patients), volunteer engagement and early intervention contributed to the success of community-based palliative care programmes.
Conclusions
Certain components of community-based palliative care programmes are effective. Such components should be implemented and tested more in low- and middle-income countries and key and vulnerable populations such as lower-income and marginalised racial or ethnic groups. In addition, more research is needed on the cost-effectiveness of individual programme components.
Keywords: palliative care, systematic review, telehealth, education, volunteers, older people
Key Points
Standardised sessions, volunteer involvement and early intervention are beneficial aspects of community-based palliative care.
There is a paucity of research on individual community-based palliative care components in low- and middle-income countries.
Future community-based palliative care programmes would benefit from standardised sessions to provide consistent training.
Volunteers can be an effective addition to the community-based palliative care team when properly trained and supported.
Future research on community-based palliative care components should strive to incorporate cost-effectiveness as an outcome.
Introduction
With a rising prevalence of chronic disease extending illness periods for populations worldwide, the need for palliative care is growing [1]. Research projects that the need for palliative care globally will almost double by 2060 due to the increase in health-related suffering, with the largest rise in such suffering occurring in low-income countries [2]. With half of the world lacking access to essential health services, many of which can be costly [3], providing palliative care in the community or at home is essential. This is especially true for low- and middle-income countries where access to pain medications is lower than for high-income countries and the socio-cultural belief system may not regard palliative care [4].
Palliative care often includes considering social services needs beyond that of traditional clinic-based services. At its centre, palliative care prevents and relieves suffering for individuals with advanced chronic illness or life-limiting conditions and focuses on the physical, psychosocial or spiritual aspects of care [1]. ‘Community-based palliative care’ is a delivery model that integrates such care across inpatient and outpatient care settings. Specifically, community-based palliative care ‘seeks to integrate palliative and serious illness care with local health care systems’ [5]. The World Health Organization has emphasised the importance of integrating palliative care into primary care and community and home-based care to make such care accessible and sustainable [1].
Interventions providing palliative care have been shown to improve both quality and cost outcomes [6]. A global systematic review of holistic community-based palliative care programmes found they increased the likelihood of dying at home and reduced costs [7]. That studies in that review examined place of death is not surprising because research shows most individuals would prefer to die at home, and place of death is a common way to measure quality in end-of-life care [8, 9]. Relatedly, avoiding hospitalisations has also been viewed as higher quality in end-of-life care since symptoms that cause such admissions can often be relieved at home [10, 11]. While existing research highlights the general overall value of comprehensive community-based palliative care programmes, there is a lack of studies examining the effectiveness of specific components found within community-based palliative care offerings. More clarity about particular components could help providers better determine which facets of community-based palliative care to implement. In addition, more information about how the community-based palliative care components work for certain groups (e.g. key and vulnerable populations, specific countries) will inform policymakers making funding allocation decisions regarding resources for seriously ill people. Key and vulnerable populations are groups at higher risk for poor health care outcomes or that lack access to health services due to biological, behavioural, social or structural factors. Increasing the knowledge about such groups related to community-based palliative care may help reduce existing inequalities in health care access and quality.
Aims
A previous systematic review examined the overall effectiveness of community-based palliative care programmes [7]. The review highlighted the need for a deeper understanding of the specific components within programmes that could contribute to overall effectiveness. This systematic review is a complementary follow-up with the novel objective of thoroughly synthesising quantitative and qualitative research examining specific component effectiveness within community-based palliative care programmes. We aimed to determine what components of community-based palliative care have been examined in peer-reviewed literature for effectiveness. We also aimed to ascertain what specific outcome measures were examined, the reported results, and whether costs or key and vulnerable population outcomes were included in the analysis.
Search strategy and selection criteria
Review questions
Our systematic review design followed the recommendations from the Cochrane Handbook for Systematic Reviews of Interventions [12]. We first developed our questions, including a rationale. In developing our research questions, we applied the FINER criteria, ensuring our questions were Feasible, Interesting, Novel, Ethical and Relevant [13]. Conversations with stakeholders and the existing literature helped inform our research questions. Specifically, conversations with hospice policy leaders highlighted the need for a more evidence-based understanding of which components within community-based palliative care programmes are most effective. A review of the literature confirmed this gap exists within academic research.
Search strategy
The systematic review study protocol is registered at PROSPERO (CRD42022302305). Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14], we conducted database searches for full-length articles published through August 2021. We searched the four databases of CINAHL, Web of Science, ProQuest Federated and PubMed including MEDLINE. The search string is presented in Appendix 1.
Inclusion/exclusion criteria
The articles had to evaluate a single, specific component of a community-based palliative care programme (e.g. music programme and telehealth service). An article was excluded if it examined a comprehensive community-based palliative care programme with multiple components holistically. Such programmes were examined in a separate review [7]. Both qualitative and quantitative analysis articles were included. Articles could examine the single component within an individual community-based palliative care programme or across several programmes. Articles that described components without any form of evaluation were not included. Review articles were also excluded.
Extraction process
At least two researchers independently examined the titles and abstracts of all articles for possible inclusion. Any disagreements defaulted to accessing full-text articles. At least two researchers independently read through the full-text articles to determine study inclusion. We solved disagreements at this level with discussions involving all researchers.
For the included articles, at least two researchers independently extracted key information, including the type of study, the component examined, country, disease focus (if applicable), age of patients (if applicable), programme(s) studied, outcomes measured and reported outcome success. We also noted whether costs were examined and if key and vulnerable populations’ outcomes were analysed.
To provide the reader with a critical appraisal of the included studies, we noted study quality as high, medium or low based on criteria outlined in the Mixed Methods Appraisal Tool version 2018. This tool appraises the quality of the methods used for qualitative, quantitative and mixed-methods studies [15]. The quality assignment depended on the percentage of methodology criteria met, with low-quality studies meeting under 75%, medium-quality studies meeting between 76 and 86%, and high-quality meeting 87% and above [16]. The researchers resolved any extraction result differences through discussion.
Results
Search results
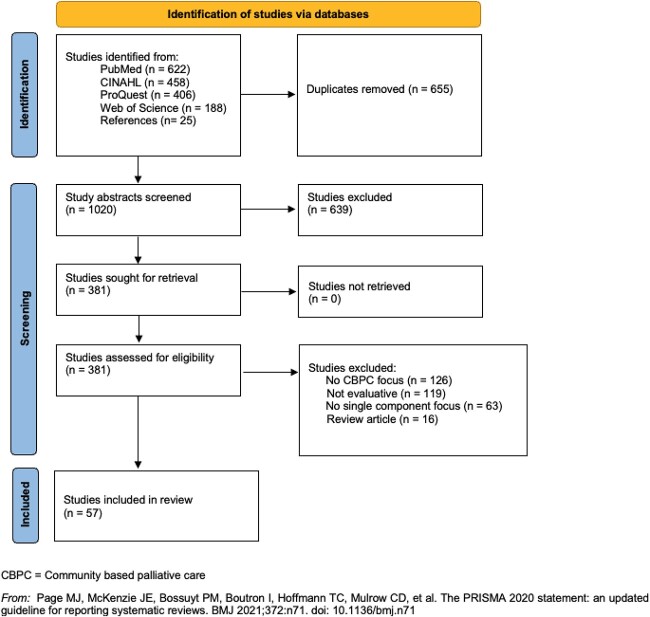
A total of 1,674 articles were initially retrieved from PubMed, CINAHL, ProQuest Federated and Web of Science. Following PRISMA guidelines [14], the researchers reviewed the references of the retrieved articles, resulting in an additional 25 articles for screening. Figure 1 highlights the selection process as suggested by PRISMA guidelines [14]. Table 1 presents the study characteristics. In addition, Tables 2 and 3 summarise the included 25 quantitative and 21 qualitative research articles, respectively, sorted by the main component examined. The 11 mixed-methods articles appear in both tables. The supplementary file includes more detailed information about all the articles. We present the following results by the types of community-based palliative care components examined and indicate the direction of effect for the quantitative studies. Note that three articles are dated 2022 because they were published in journal issues after being published online first by August 2021.
Figure 1.
PRISMA flow diagram.
Table 1.
Characteristics of the studies
| All studies | Number of studies (n = 57) |
| Country economies | |
| Low-income and lower-middle-income | 1 (1.8%) |
| Upper-middle-income | 1 (1.8%) |
| High-income | 55 (96.4%) |
| Study quality | |
| Low | 8 (14.0%) |
| Medium | 19 (33.3%) |
| High | 30 (52.6%) |
| Key and vulnerable populations controlled for or studied * | |
| Rural | 15 (26.3%) |
| Lower-income | 9 (15.8%) |
| Marginalised racial or ethnic groups | 9 (15.8%) |
| Component examined * | |
| Early intervention | 6 (10.5%) |
| Education | 11 (19.3%) |
| Innovative approaches (roles) | 12 (21.1%) |
| Innovative approaches (services) | 9 (15.8%) |
| Standardised sessions | 6 (10.5%) |
| Telehealth | 7 (12.3%) |
| Volunteers | 9 (15.8%) |
| Quantitative studies | Number of studies (n = 36) |
| Outcome measures * | |
| Advance care planning | 3 (8.3%) |
| Costs | 3 (8.3%) |
| Death location | 7 (19.4%) |
| Hospice utilisation | 5 (13.9%) |
| Hospital utilisation | 12 (33.3%) |
| Knowledge | 14 (39.0%) |
| Quality of life | 6 (16.7%) |
| Symptoms | 8 (22.2%) |
| Qualitative studies | Number of studies (n = 32) |
| Participants * | |
| Caregivers and family members | 13 (40.6%) |
| Healthcare providers | 21 (66.0%) |
| Patients | 9 (28.1%) |
| Volunteers | 5 (15.6%) |
Note: Percentages might not add to 100% due to rounding; mixed-methods studies included in both qualitative and quantitative categories.
aSome studies include multiple categories, resulting in percentages not adding to 100%.
Table 2.
Summary of quantitative article outcomes
| Advance care planning | Costs | Death location | Hospice use | Hospital use | Knowledge | Quality of life | Symptoms | |
|---|---|---|---|---|---|---|---|---|
| Early intervention | ||||||||
| McNamara (2013) [18] | Y | |||||||
| Webel (2018) [20] | N | M | N | M | ||||
| Wright (2018) [17] | Y | M | ||||||
| Qureshi (2019) [19] | Y | |||||||
| Mittmann (2020) [82] | Y | Y | ||||||
| Education | ||||||||
| Connolly (2018) [22] | Y | |||||||
| Gardner* (2022) [30] | M | |||||||
| Harrison* (2016) [27] | Y | |||||||
| Kelley (2004) [24] | Y | |||||||
| Pesut* (2015) [26] | Y | |||||||
| Claxton-Oldfield (2022) [33] | Y | |||||||
| Innovative approaches (service) | ||||||||
| Carey (2017) [54] [respite service] | Y | M | ||||||
| Ghesquiere (2018) [60] [ageing services palliative care screening tool] | Y | |||||||
| Itoh (2021) [63] [financial incentives for advanced care management] | N | |||||||
| Landers (2014) [62] [portable ultrasonography] | Y | |||||||
| Wowchuk (2009) [61] [palliative medication kit] | Y | |||||||
| Murakami (2018) [25] [community outreach, information sharing and education programme] | Y | |||||||
| Innovative approaches (personnel role) | ||||||||
| Daley* (2006) [66] [heart failure nurse-led collaboration] | N | |||||||
| Fedel* (2021) [67] [nurse specialist collaboration role with palliative care] | N | |||||||
| Fischer (2018) [70] [culturally tailored patient navigator] | Y | N | N | N | N | |||
| Moreton (2020) [64] [nurse-led specialist community palliative care model] | Y | Y | M | N | ||||
| van de Mortel (2017) [68] [general practitioner communication palliative care team facilitator] | Y | Y | ||||||
| Sussman (2011) [65] [oncology nurse-led coordinator] | Y | |||||||
| Standardised sessions | ||||||||
| Burnod (2012) [40] | Y | |||||||
| Di Pollina (2017) [41] | Y | Y | N | |||||
| Abernethy (2013) [28] | Y | Y | N | |||||
| Fletcher* (2008) [83] | Y | |||||||
| Spettell (2009) [42] | Y | Y | ||||||
| Telehealth | ||||||||
| Jiang* (2020) [36] | Y | M | ||||||
| Nguyen (2020) [39] | Y | N | N | |||||
| Riggs (2017) [38] | Y | |||||||
| Saysell* (2003) [37] | N | |||||||
| Tieman (2016) [34] | Y | |||||||
| Volunteers | ||||||||
| Lee* (2020) [45] | Y | |||||||
| Luijkx* (2009) [46] | Y | |||||||
| Pesut* (2018) [47] | Y |
Y = approach significantly improved outcome, N = approach did not significantly improve outcome, M = approach had mixed results on outcome. The studies are listed under their main component of focus; therefore, the total study counts may not exactly match those of the ‘Component examined’ section of Table 1.
aStudies are both quantitative and qualitative.
Table 3.
Qualitative study result summary
| Caregivers and family members | Healthcare providers | Patients | Volunteers | |
|---|---|---|---|---|
| Early intervention | ||||
| Akyar (2019) [21] | Y | Y | ||
| Education | ||||
| Gardner* (2022) [30] | M | |||
| Hall (1998) [29] | M | |||
| Harrison* (2016) [27] | Y | |||
| Ingleton (2011) [32] | Y | Y | ||
| Naicker (2016) [31] | Y | |||
| Pesut* (2015) [26] | M | M | M | |
| Innovative approaches (service) | ||||
| Bracken (2011) [58] [palliative care needs assessment tool] | N | |||
| Carey (2016) [53] [respite service] | M | M | M | |
| Cortis (2017) [57] [medication management service] | Y | |||
| Horseman (2019) [59] [caregiver needs assessment tool] | M | |||
| Lindenfelser (2008) [55] [paediatric music therapy] | Y | |||
| Spelten (2019) [56] [after-hours nurse service] | Y | M | ||
| Innovative approaches (personnel role) | ||||
| Daley* (2006) [66] [heart failure nurse-led collaboration] | Y | |||
| Fedel* (2021) [67] [nurse specialist collaboration role with palliative care] | Y | |||
| O’Connor (2011) [69] [pharmacists’ role in community-based palliative care] | M | |||
| Percival (2014) [71] [domiciliary care workers’ role in palliative care team] | Y | Y | Y | |
| Standardised sessions | ||||
| Fletcher* (2008) [83] | Y | |||
| Kramer (2014) [43] | M | |||
| Telehealth | ||||
| Collier (2016) [84] | Y | |||
| Hughes (2011) [35] | M | |||
| Jiang* (2020) [36] | Y | Y | ||
| Saysell* (2003) [37] | M | |||
| Volunteers | ||||
| Allen (2016) [44] | M | |||
| Claxton-Oldfield (2010) [50] | Y | |||
| Lee* (2020) [45] | Y | |||
| Luijkx* (2009) [46] | Y | |||
| Pesut* (2018) [47] | Y | Y | Y | |
| Pesut (2020) [51] | Y | M | Y | Y |
| Subramanian (2022) [48] | M | M | ||
| Warner (2021) [52] | M | |||
| Weeks (2008) [49] | Y |
Y = overall positive feedback, M = mixed positive and negative feedback, N = overall negative feedback.
aStudies are both quantitative and qualitative.
Early community-based palliative care intervention
Five studies examined early community-based palliative care interventions, all from high-income countries. For all these studies, ‘early’ was in advance of a patient needing to make final decisions regarding palliative care. Three of the studies framed early in terms of time before death (2 or 3 months, depending on the study) [17–19]. The other two studies stated that early intervention happened before the individual’s disease continued to progress [20, 21]. All five studies showed that intervening early with palliative care is generally positive for patients. For groups with early community-based palliative care intervention, emergency department use was lower [17, 18], acute care stays in the last 2 weeks of death was lower [19] and symptom distress/HIV self-management understanding 9 months into the programme improved compared to the beginning of the programme [20].
Education
Eleven studies examined educational interventions. Seven different types of learners were the recipients of education in the studies. The learners were community nurses [22], volunteers [23], a variety of types of direct care providers [24, 25], students in health-related fields [26, 27], community physicians [28, 29], geriatric case managers [30] and health care aids [31, 32]. Over half of the educational interventions trained non-palliative care-focused health care providers about palliative care [24, 25, 29–32], while two trained students (nursing students [26] and medical residents [27]) about palliative care. Another intervention focused on teaching community nurses knowledge and skills to help individuals die with dignity in Ireland [22]. Finally, an intervention in Canada taught community-based palliative care programme volunteers about end-of-life phenomena [33]. All six studies that quantitatively examined education approaches found that knowledge increased for the learners [22, 24, 26, 27, 30, 33]. Two of these studies also found that the interventions increased competence or skill [22, 24].
Telehealth
Seven studies examined telehealth programmes, all from high-income countries. Three of four Australian studies were acceptability or feasibility studies. These acceptability and feasibility findings were positive [34–36], suggesting that future telehealth efficacy studies should be conducted. One older, low-quality study from the United Kingdom used mixed methods to examine telehealth to facilitate communication between nurses and palliative medicine specialists [37]. Another examined telephonic outreach by a nurse after an individual had been referred to a community-based palliative care programme finding that over half of the patients who enrolled in palliative care did so after telephonic outreach without an in-person visit [38]. Another study examined a programme that used patient/physician video consultation while a nurse was in the patient’s home but ended early, partly due to low video visit uptake [39].
Standardised sessions
Six studies from high-income countries examined the incorporation of standardised communication sessions among community-based palliative care team participants. Standardised sessions broadly included any consistently scheduled interdisciplinary team meetings discussing patients. These sessions varied in design specifics but usually started with an initial session during the introduction of a patient into the programme and then consistent, planned meeting times for community-based palliative care staff to come together and discuss patient-related concerns. While the initial meetings at times included patients, the following sessions typically involved physicians, nurses, social workers and other programme providers discussing the patient. This categorisation summarised specific organisations’ attempts to have health care providers work across silos within palliative care.
The quantitative research examined standardised sessions between community-based palliative care programmes and prehospital emergency services personnel [40], a geriatric unit home evaluation and follow-ups [41], doctors, patients and/or caregivers, and palliative care nurses [28], and case managers establishing an initial outreach call and planned follow-ups [42]. Most reported positive results, including an increase in respecting a patient’s life will [40], home deaths [41] and hospital utilisation rates [28, 41, 42]. A randomised controlled trial study that tested adding a single interdisciplinary case conference after referral to palliative care was the only quantitative standardised sessions study to examine quality of life, for which it reported no positive impact [28]. The one qualitative study on this topic reported that interdisciplinary teams primarily benefited from consultation sessions with social workers and hospice registered nurses but noted communication challenges regarding best practises [43].
Volunteers
Nine studies examined aspects of volunteerism within community-based palliative care programmes. Almost all reported overall positive experiences of volunteer involvement within programmes from the perspective of the volunteers [44–48], the patient/caregivers [45–50] and involved medical professionals [51, 52]. One study from India highlighted mixed results of volunteer interactions from the patient’s perspective noting that patient dissatisfaction might result from other barriers preventing volunteer success [48].
Innovative approaches: service provision
Twelve studies across seven high-income countries examined innovative service provision approaches within community-based palliative care programmes. This category included studies examining types of services described as either unique or not always occurring within community-based palliative care programmes. Of the studies reporting positive results, two stated positive outcomes related to cost-effectiveness, patient/caregiver satisfaction and hospitalisation rates resulting from a rural Australian respite service within a programme serving a rural, vulnerable patient population [53, 54]. Three other Australian qualitative studies reported positive outcomes related to various forms of service provision. First, an interview-based study of music therapy within a paediatric community-based palliative care programme reported a high level of satisfaction from bereaved mothers [55]. Another study found positive family caregiver experiences with a 24/7 nursing care component of a rural programme [56]. Last, a study reported the potential to improve swallowing and digestion issues as well as reduced falls by including a medication management system within a programme [57].
Other innovative service approaches reported mixed results. Two qualitative studies reported nurses’ mixed perspectives related to using a needs assessment tool within programmes in Ireland [58] and Scotland [59]. In addition, a small US pilot study did find a palliative care screening tool to be acceptable and feasible within programmes but noted room for improvements with respect to provider training and consistency of use [60]. A Canadian study examining the provision of palliative medicine kits noted an increase in home deaths but noted the need for cost-effectiveness research [61]. The use of portable ultrasonography for cancer patients in need within a New Zealand community-based palliative care improved symptoms including level of pain and shortness of breath for several patients in the study and was suggested to provide cost savings although no cost details were shared [62]. One Japanese study noted that financial incentives for advanced care management did not improve the progression of care-need levels [63]. Another Japanese article highlighted the success of a comprehensive community-based palliative care awareness-enhancing programme on the number of home deaths but did not examine the cost-effectiveness [25].
Innovative approaches: personnel roles
Eight studies from high-income countries examined specific personnel roles and their impact on community-based palliative care outcomes. This category included studies of different types of roles that were described as unique or not always occurring within community-based palliative care programmes. Four studies specifically looked at various nurse-led programme roles. Of these, the studies examining quality of life reported no improvements from such programmes [64, 65]. One study noted improvements in home deaths [64], while another reported no change in this outcome [66]. Similarly, hospital utilisation rates did not improve for two of the nurse-led programmes studied [64, 67] but did in another study [65]. Qualitative research showed that both patients and staff were highly satisfied with these programmes [66, 67].
Four studies examined outcomes related to various other roles within a community-based palliative care programme, including having a practitioner-leader [68], a pharmacist [69], a culturally competent patient navigator [70] and domiciliary workers [71].
Discussion
Main findings
This systematic review reveals that certain components—standardised sessions, volunteer involvement and early intervention—of community-based palliative care programmes improve health outcomes such as home deaths, hospitalisations and patient/caregiver satisfaction. We found that quality of life-related outcomes proved more difficult to improve with community-based palliative care components. This finding differed from previous research examining comprehensive community-based palliative care programmes holistically, which found that such comprehensive programmes can improve quality of life [7]. The few studies in the review herein examining the cost-effectiveness of community-based palliative care programme components were promising; however, more research is needed on programme components’ cost-effectiveness to better guide resource allocation to certain interventions (see Table 4).
Table 4.
Results and relevance to practise
| Programme component | Results | Relevance to practise |
|---|---|---|
| Early intervention | —Lower emergency department use —Fewer acute care stays —Symptom distress/disease understanding improved |
Start palliative care as soon as it is apparent the patient needs such services |
| Education | —Increased learner knowledge —Increased learner competence or skill |
Train palliative care team members, volunteers and students in palliative care topics; it may improve their knowledge, confidence and skills |
| Telehealth | —Using telehealth is feasible and acceptable —Increased patient access to services —Improved patient satisfaction |
Use telehealth to potentially augment palliative care services, being mindful of facilitating access to such services by making technology training and electronic devices available |
| Standardised sessions | —Increased respecting patient’s life will —Increased home deaths —Lower hospital utilisation rates |
Conduct interdisciplinary team meetings that are planned in advance and focus on patient-related concerns |
| Volunteers | —Positive experiences reported by volunteers, patient/caregivers and medical professionals | Engage and train volunteers to assist with palliative care to increase and enhance the provision of services |
| Innovative approaches (service provision) | —Overall, positive experiences were reported by patients/caregivers | Testing innovative approaches (e.g. music therapy) in community-based palliative care may lead to improvements in outcomes and patient and caregiver experiences |
| Innovative approaches (personnel roles) | —Overall, a lack of improvements | Establishing new types of personnel roles within community-based palliative care may not be the best use of resources until further research can determine the value of specific roles |
Standardised sessions stood out among the categories of programme component types. Overall, quantitative outcome measures, including home deaths, hospitalisations and performance of activities of daily living scores improved when community-based palliative care programmes had established standardised sessions across disciplines. In addition, the qualitative findings suggest that those working within the community-based palliative care programmes appreciated the support and knowledge transfer these sessions provided. The research also suggests that these sessions are relatively cost-effective. The one outcome improvement exception from standardised sessions was patient quality of life, which was not statistically different across multiple studies.
Palliative care is intended to improve the quality of life for seriously ill patients and their families [1]. However, several studies in this review did not show significant improvements in quality of life yet indicated improvements in other outcomes such as hospitalisations or home deaths. One reason for this result may be that quality of life is challenging to measure and can encompass various aspects depending on the individual conditions of a patient (e.g. disease and values) [72]. In addition, the lack of improvements, coupled with our previous finding that holistic community-based palliative care programmes improved quality of life [7], suggests that components alone do not move the needle on quality of life. Rather, combining interventions to meet the multiple needs of palliative care patients and their families may be a necessary strategy to meet the goal of improving lives through community-based palliative care.
Our review highlights the dearth of studies examining the effectiveness of programme components in lower-income countries. Of the 57 studies reviewed, 55 were from high-income countries, one from an upper-middle-income country (South Africa) [31] and one from a lower-middle-income country (India) [48]. The two studies that were not from high-income countries were qualitative. That no quantitative studies examine the effectiveness of community-based palliative care components in countries other than high-income countries is problematic because the effectiveness of community-based palliative care programme components may be different when tested in resource-constrained environments. With fewer health care resources, lower- and middle-income countries especially stand to benefit from innovative community-based palliative care programmes that use lower-cost components such as volunteers or training family caregivers. Future research should focus on implementing and examining community-based palliative care components in low-income and lower-middle-income countries.
Our review also revealed a gap in research that considers key and vulnerable populations. For example, only about 5% of the studies included race/ethnicity in their analyses and just 12% controlled for participant income levels. The absence of research focused on these groups is not surprising, given that key and vulnerable populations are often understudied and under-consulted in research [73]. There is, however, more representation in community-based palliative care component effectiveness studies of rural populations. About one quarter of the reviewed articles focused on or considered rural populations. This attention to rural areas may be driven by the necessity to provide palliative care services in locations where the distance to facilities may be more significant and the availability of health care providers scarcer [74].
Several of the components reviewed may help address the scarcity of health care providers. For example, volunteers helping to support palliative care patients and their families can perform certain helpful tasks that would typically fall to the nurses or social workers. Similarly, educating members across the community-based palliative care team and providing standardised sessions that allow for better communication about patients help professionals beyond physicians and nurses take on new tasks. Telehealth, where providers deliver comfort care remotely [75], can also help alleviate this issue.
While there has been increasing reliance on telehealth for health care services during the COVID-19 pandemic [76] and greater acceptance of technology among older adults [77], few studies on telehealth are included here. This is not surprising, given that hospice and palliative care had slow telehealth adoption before COVID-19 [78]. Previous research with caregivers of individuals with serious illnesses in the United States showed that having a good internet connection, having access to video and the patient being younger than 65 years old were associated with greater telehealth satisfaction [75]. Designers of community-based palliative care telehealth intervention components should keep these characteristics in mind to create telehealth-enabled solutions that can improve access and quality for all seriously ill individuals and their families.
Limitations
This study is limited in scope to peer-reviewed academic literature and, as such, could be missing out on case reports or other pilot programme findings. In addition, due to the heterogeneity of the research methods across similar components, we did not perform a meta-analysis to quantitatively examine the community-based palliative care programme component impact. Another limitation is that our study assumed home death and fewer hospitalisations were positive outcomes. While this is common in the literature examining quality of end-of-life care [8–11], this does not consider that some individuals may prefer the hospital over their home and that a patient’s surroundings may be less about geography and more about the social space (e.g. individuals with whom they interact) [79]. Last, including only evaluative studies eliminated potentially innovative approaches within community-based palliative care. For example, descriptive research on the benefits of including end-of-life doula care [80] and clergy [81] on the community-based palliative care team appear promising. Yet, to our knowledge, no evaluative research has examined these roles at the time of this study.
Conclusions and future directions
This review found that certain components of community-based palliative care programmes are effective, particularly from a hospital utilisation, home death and patient/caregiver satisfaction perspective. Such components may be cost-effective, but more research is needed to draw firm conclusions on their economic outcomes for specific payers (e.g. patients, families, private and public insurers). There is a significant gap in researching community-based palliative care programme component effectiveness in low- and middle-income countries. Furthermore, focusing interventions on and examining outcomes for key and vulnerable populations worldwide is a necessary research next step. We recommend collaboration between researchers, health professionals and policymakers to design, implement and test community-based palliative care interventions to improve the evidence base and, ultimately, quality outcomes for all seriously ill and their families.
Supplementary Material
Acknowledgements
We would like to acknowledge Monica Kowalczyk for assisting with the article retrieval process and table construction and Sadia Afrin for assisting with organisational management of the articles.
Contributor Information
M Courtney Hughes, Department of Public Health, Northern Illinois University, DeKalb, IL 60115, USA.
Erin Vernon, Department of Economics, Seattle University, Seattle, WA 98122, USA.
Allison Hainstock, Department of Economics, Seattle University, Seattle, WA 98122, USA.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
None.
References
- 1. World Health Organization . Palliative Care. https://www.who.int/news-room/fact-sheets/detail/palliative-care. Published 4 February. 2020.
- 2. Sleeman KE, de Brito M, Etkind S et al. The escalating global burden of serious health-related suffering: projections to 2060 by world regions, age groups, and health conditions. Lancet Glob Health 2019; 7: e883–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Bank and WHO . Half the World Lacks Access to Essential Health Services, 100 Million Still Pushed into Extreme Poverty because of Health Expenses. World Health Organization, Published 13 December, 2017. https://www.who.int/news/item/13-12-2017-world-bank-and-who-half-the-world-lacks-access-to-essential-health-services-100-million-still-pushed-into-extreme-poverty-because-of-health-expenses. [Google Scholar]
- 4. Poudel A, Bhuvan K, Shrestha S et al. Access to palliative care: discrepancy among low-income and high-income countries. J Glob Health 2019; 9: 1–5. 10.7189/jogh.09.020309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. California Health Care Foundation . Community-based palliative care. https://www.chcf.org/resource/community-based-palliative-care/ (1 September 2023, date last accessed).
- 6. Luta X, Ottino B, Hall P et al. Evidence on the economic value of end-of-life and palliative care interventions: a narrative review of reviews. BMC Palliat Care 2021; 20: 89. 10.1186/s12904-021-00782-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vernon E, Hughes MC, Kowalczyk M. Measuring effectiveness in community-based palliative care programs: a systematic review. Soc Sci Med 2022; 296: 114731. 10.1016/j.socscimed.2022.114731. [DOI] [PubMed] [Google Scholar]
- 8. Ali M, Capel M, Jones G, Gazi T. The importance of identifying preferred place of death. BMJ Support Palliat Care 2019; 9: 84–91. [DOI] [PubMed] [Google Scholar]
- 9. Gomes B, Calanzani N, Curiale V et al. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev 2013; 2022: CD007760. 10.1002/14651858.CD007760.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De Korte-Verhoef MC, Pasman HRW, Schweitzer BP et al. General practitioners’ perspectives on the avoidability of hospitalizations at the end of life: a mixed-method study. Palliat Med 2014; 28: 949–58. [DOI] [PubMed] [Google Scholar]
- 11. Gott M, Gardiner C, Ingleton C et al. What is the extent of potentially avoidable admissions amongst hospital inpatients with palliative care needs? BMC Palliat Care 2013; 12: 9. 10.1186/1472-684X-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Higgins JP, Thomas J, Chandler J et al. Cochrane Handbook for Systematic Reviews of Interventions. Hoboken, New Jersey: Wiley-Blackwell, 2019. [Google Scholar]
- 13. Cummings SR, Browner WS, Hulley SB. Conceiving the research question and developing the study plan. Des Clin Res 2013; 4: 14–22. [Google Scholar]
- 14. Page MJ, McKenzie JE, Bossuyt PM et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hong Q, Pluye P, Fàbregues S. et al. Mixed methods appraisal tool (MMAT) Version 2018: User Guide. McGill University, 2018. http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf.
- 16. Pace R, Pluye P, Bartlett G et al. Testing the reliability and efficiency of the pilot mixed methods appraisal tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012; 49: 47–53. 10.1016/j.ijnurstu.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 17. Wright CM, Youens D, Moorin RE. Earlier initiation of community-based palliative care is associated with fewer unplanned hospitalizations and emergency department presentations in the final months of life: a population-based study among cancer decedents. J Pain Symptom Manage 2018; 55: 745–754.e8. [DOI] [PubMed] [Google Scholar]
- 18. McNamara BA, Rosenwax LK, Murray K, Currow DC. Early admission to community-based palliative care reduces use of emergency departments in the ninety days before death. J Palliat Med 2013; 16: 774–9. [DOI] [PubMed] [Google Scholar]
- 19. Qureshi D, Tanuseputro P, Perez R, Pond GR, Seow HY. Early initiation of palliative care is associated with reduced late-life acute-hospital use: a population-based retrospective cohort study. Palliat Med 2019; 33: 150–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Webel A, Prince-Paul M, Ganocy S et al. Randomized clinical trial of a community navigation intervention to improve well-being in persons living with HIV and other co-morbidities. AIDS Care 2019; 31: 529–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Akyar I, Dionne-Odom JN, Bakitas MA. Using patients and their caregivers feedback to develop ENABLE CHF-PC: an early palliative care intervention for advanced heart failure. J Palliat Care 2019; 34: 103–10. [DOI] [PubMed] [Google Scholar]
- 22. Connolly M, Charnley K, Collins R et al. Evaluating an educational programme for dignity care intervention with community nurses in Ireland. Int J Palliat Nurs 2018; 24: 474–81. [DOI] [PubMed] [Google Scholar]
- 23. Claxton-Oldfield S. Got volunteers? The selection, training, roles, and impact of hospice palliative care volunteers in Canada’s community-based volunteer programs. Home Health Care Manag Pract 2015; 27: 36–40. [Google Scholar]
- 24. Kelley ML, Habjan S, Aegard J. Building capacity to provide palliative care in rural and remote communities: does education make a difference? J Palliat Care 2004; 20: 308–15. [PubMed] [Google Scholar]
- 25. Murakami N, Tanabe K, Morita T et al. Impact of a six-year project to enhance the awareness of community-based palliative care on the place of death. J Palliat Med 2018; 21: 1494–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pesut B, McLean T, Reimer-Kirkham S, Hartrick-Doane G, Hutchings D, Russell LB. Educating registered nursing and healthcare assistant students in community-based supportive care of older adults: a mixed methods study. Nurse Educ Today 2015; 35: e90–6. [DOI] [PubMed] [Google Scholar]
- 27. Harrison KL, Boyden JY, Kalish VB, Muir JC, Richardson S, Connor SR. A hospice rotation for military medical residents: a mixed methods. Palliat Med 2016; 19: 542–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Abernethy AP, Currow DC, Shelby-James T et al. Delivery strategies to optimize resource utilization and performance status for patients with advanced life-limiting illness: results from the “palliative care trial” [ISRCTN 81117481]. J Pain Symptom Manage 2013; 45: 488–505. [DOI] [PubMed] [Google Scholar]
- 29. Hall P, Hupé D, Scott J. Palliative care education for community-based family physicians: the development of a program, the evaluation, and its consequences. J Palliat Care 1998; 14: 69–74. [PubMed] [Google Scholar]
- 30. Gardner DS, Doherty M, Ghesquiere A et al. Palliative care for case managers: building capacity to extend community-based palliative care to underserved older adults. Gerontol Geriatr Educ 2022; 43: 269–84. [DOI] [PubMed] [Google Scholar]
- 31. Naicker SN, Richter L, Stein A, Campbell L, Marston J. Development and pilot evaluation of a home-based palliative care training and support package for young children in southern Africa. BMC Palliat Care 2016; 15: 41. 10.1186/s12904-016-0114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ingleton C, Chatwin J, Seymour J, Payne S. The role of health care assistants in supporting district nurses and family carers to deliver palliative care at home: findings from an evaluation project. J Clin Nurs 2011; 20: 2043–52. [DOI] [PubMed] [Google Scholar]
- 33. Claxton-Oldfield S, Hicks R, Claxton-Oldfield J. A pilot study evaluating the effectiveness of a training module designed to improve hospice palliative care volunteers’ ability to deal with unusual end-of-life phenomena. Omega 2022; 85: 75–87. [DOI] [PubMed] [Google Scholar]
- 34. Tieman JJ, Swetenham K, Morgan DD, To TH, Currow DC. Using telehealth to support end of life care in the community: a feasibility study. BMC Palliat Care 2016; 15: 94. 10.1186/s12904-016-0167-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hughes KL, Sargeant H, Hawkes AL. Acceptability of the distress thermometer and problem list to community-based telephone cancer helpline operators, and to cancer patients and carers. BMC Cancer 2011; 11: 46. 10.1186/1471-2407-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jiang B, Bills M, Poon P. Integrated telehealth-assisted home-based specialist palliative care in rural Australia: a feasibility study. J Telemed Telecare 2023; 29: 50–7. [DOI] [PubMed] [Google Scholar]
- 37. Saysell E, Routley C. Telemedicine in community-based palliative care: evaluation of a videolink teleconference project. Int J Palliat Nurs 2003; 9: 489–95. [DOI] [PubMed] [Google Scholar]
- 38. Riggs A, Breuer B, Dhingra L et al. Hospice enrollment after referral to community-based, specialist-level palliative care: incidence, timing, and predictors. J Pain Symptom Manage 2016; 52: 170–7. [DOI] [PubMed] [Google Scholar]
- 39. Nguyen HQ, McMullen C, Haupt EC et al. Findings and lessons learnt from early termination of a pragmatic comparative effectiveness trial of video consultations in home-based palliative care. BMJ Support Palliat Care 2022; 12: e432–40. [DOI] [PubMed] [Google Scholar]
- 40. Burnod A, Lenclud G, Ricard-Hibon A, Juvin P, Mantz J, Duchateau FX. Collaboration between prehospital emergency medical teams and palliative care networks allows a better respect of a patient’s will. Eur J Emerg Med 2012; 19: 46–7. [DOI] [PubMed] [Google Scholar]
- 41. Di Pollina L, Guessous I, Petoud V et al. Integrated care at home reduces unnecessary hospitalizations of community-dwelling frail older adults: a prospective controlled trial. BMC Geriatr 2017; 17: 53. 10.1186/s12877-017-0449-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Spettell CM, Rawlins WS, Krakauer R et al. A comprehensive case management program to improve palliative care. J Palliat Med 2009; 12: 827–32. [DOI] [PubMed] [Google Scholar]
- 43. Kramer BJ, Cleary JF, Mahoney JE. Enhancing palliative care for low-income elders with chronic disease: feasibility of a hospice consultation model. J Soc Work End--Life Palliat Care 2014; 10: 356–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Allen RS, Azuero CB, Csikai EL et al. “It was very rewarding for me …”: senior volunteers’ experiences with implementing a reminiscence and creative activity intervention. Gerontologist 2016; 56: 357–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lee J, Lee J-E. A palliative care program for volunteers in a community setting: a mixed-methods pilot study. Am J Hosp Palliat Care 2020; 37: 455–64. [DOI] [PubMed] [Google Scholar]
- 46. Luijkx KG, Schols JMGA. Volunteers in palliative care make a difference. J Palliat Care 2009; 25: 30–9. [PubMed] [Google Scholar]
- 47. Pesut B, Duggleby W, Warner G et al. Volunteer navigation partnerships: piloting a compassionate community approach to early palliative care. BMC Palliat Care 2018; 17: 2. 10.1186/s12904-017-0210-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Subramanian S, Sarkar S, Vijayageetha M, Adhinarayanan S. Experiences of volunteers and patient satisfaction in home based palliative care, Puducherry, South India-a descriptive qualitative study. J Palliat Care 2022; 37: 164–9. 10.1177/08258597211026400. [DOI] [PubMed] [Google Scholar]
- 49. Weeks LE, Macquarrie C, Bryanton O. Hospice palliative care volunteers: a unique care link. J Palliat Care 2008; 24: 85–93. [PubMed] [Google Scholar]
- 50. Claxton-Oldfield S, Gosselin N, Schmidt-Chamberlain K, Claxton-Oldfield J. A survey of family members’ satisfaction with the services provided by hospice palliative care volunteers. Am J Hosp Palliat Care 2010; 27: 191–6. [DOI] [PubMed] [Google Scholar]
- 51. Pesut B, Duggleby W, Warner G et al. Implementing volunteer-navigation for older persons with advanced chronic illness (Nav-CARE): a knowledge to action study. BMC Palliat Care 2020; 19: 72. 10.1186/s12904-020-00578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Warner G, Kervin E, Pesut B, Urquhart R, Duggleby W, Hill T. How do inner and outer settings affect implementation of a community-based innovation for older adults with a serious illness: a qualitative study. BMC Health Serv Res 2021; 21: 42. 10.1186/s12913-020-06031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Carey TA, Schouten K, Wakerman J et al. Improving the quality of life of palliative and chronic disease patients and carers in remote Australia with the establishment of a day respite facility. BMC Palliat Care 2016; 15: 62. 10.1186/s12904-016-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Carey TA, Arundell M, Schouten K et al. Reducing hospital admissions in remote Australia through the establishment of a palliative and chronic disease respite facility. BMC Palliat Care 2017; 16: 54. 10.1186/s12904-017-0247-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lindenfelser KJ, Grocke D, McFerran K. Bereaved parents’ experiences of music therapy with their terminally ill child. J Music Ther 2008; 45: 330–48. [DOI] [PubMed] [Google Scholar]
- 56. Spelten E, Timmis J, Heald S, Duijts SFA. Rural palliative care to support dying at home can be realised; experiences of family members and nurses with a new model of care. Aust J Rural Health 2019; 27: 336–43. [DOI] [PubMed] [Google Scholar]
- 57. Cortis LJ. A qualitative study to describe patient-specific factors that relate to clinical need for and potential to benefit from a medication management service in palliative care. J Pharm Pract Res 2017; 47: 34–40. [Google Scholar]
- 58. Bracken M, McLoughlin K, McGilloway S, McMahon E. Use of dependency and prioritization tools by clinical nurse specialists in palliative care: an exploratory study. Int J Palliat Nurs 2011; 17: 599–606. [DOI] [PubMed] [Google Scholar]
- 59. Horseman Z, Milton L, Finucane A. Barriers and facilitators to implementing the carer support needs assessment tool in a community palliative care setting. Br J Community Nurs 2019; 24: 284–90. [DOI] [PubMed] [Google Scholar]
- 60. Ghesquiere A, Gardner DS, McAfee C et al. Development of a community-based palliative care screening tool for underserved older adults with chronic illnesses. Am J Hosp Palliat Med 2018; 35: 929–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wowchuk SM, Wilson EA, Embleton L, Garcia M, Harlos M, Chochinov HM. The palliative medication kit: an effective way of extending care in the home for patients nearing death. J Palliat Med 2009; 12: 797–803. [DOI] [PubMed] [Google Scholar]
- 62. Landers A, Ryan B. The use of bedside ultrasound and community-based paracentesis in a palliative care service. J Prim Health Care 2014; 6: 148–51. [PubMed] [Google Scholar]
- 63. Itoh S, Mori T, Jeon B et al. Comparison of progression of care-need levels among long-term care recipients with and without advanced care management in a rural municipality of Japan: a population-based observational study. Int J Nurs Stud 2021; 113: 103804. 10.1016/j.ijnurstu.2020.103804. [DOI] [PubMed] [Google Scholar]
- 64. Moreton SG, Saurman E, Salkeld G et al. Economic and clinical outcomes of the nurse practitioner-led Sydney Adventist hospital community palliative care service. Aust Health Rev 2020; 44: 791. 10.1071/AH19247. [DOI] [PubMed] [Google Scholar]
- 65. Sussman J, Howell D, Bainbridge D et al. The impact of specialized oncology nursing on patient supportive care outcomes. J Psychosoc Oncol 2011; 29: 286–307. [DOI] [PubMed] [Google Scholar]
- 66. Daley A, Matthews C, Williams A. Heart failure and palliative care services working in partnership: report of a new model of care. Palliat Med 2006; 20: 593–601. [DOI] [PubMed] [Google Scholar]
- 67. Fedel PR, Pennington G. Clinical nurse specialist collaboration with a community-based palliative care program: an evidence-based practice project. Clin Nurse Spec 2021; 35: 88–95. [DOI] [PubMed] [Google Scholar]
- 68. van de Mortel TF, Marr K, Burmeister E et al. Reducing avoidable admissions in rural community palliative care: a pilot study of care coordination by general practice registrars. Aust J Rural Health 2017; 25: 141–7. [DOI] [PubMed] [Google Scholar]
- 69. O’Connor M, Fisher C, French L, Halkett G, Jiwa M, Hughes J. Exploring the community pharmacist’s role in palliative care: focusing on the person not just the prescription. Patient Educ Couns 2011; 83: 458–64. [DOI] [PubMed] [Google Scholar]
- 70. Fisher A, Craigie AM, Macleod M, Steele RJC, Anderson AS. The impact of social deprivation on the response to a randomised controlled trial of a weight management intervention (BeWEL) for people at increased risk of colorectal cancer. J Hum Nutr Diet 2018; 31: 306–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Percival J, Lasseter G, Purdy S, Wye L. “Earthly angels”? A qualitative study of the domiciliary care worker role in meeting the needs of families caring for those dying at home. Palliat Support Care 2014; 12: 445–53. [DOI] [PubMed] [Google Scholar]
- 72. McCaffrey N, Bradley S, Ratcliffe J, Currow DC. What aspects of quality of life are important from palliative care patients’ perspectives? A systematic review of qualitative research. J Pain Symptom Manage 2016; 52: 318–328.e5. [DOI] [PubMed] [Google Scholar]
- 73. Editors RE. Striving for diversity in research studies. N Engl J Med 2021; 385: 1429–30. [DOI] [PubMed] [Google Scholar]
- 74. Bringing HC. Palliative care to underserved rural communities. Health Aff Proj Hope 2019; 38: 1971–5. [DOI] [PubMed] [Google Scholar]
- 75. Hughes MC, Vernon E, Kowalczyk M, Zhou H. Experiences of caregivers and hospice leaders with telehealth for palliative care: a mixed methods study. Ann Palliat Med 2022; 11: 2302–13. [DOI] [PubMed] [Google Scholar]
- 76. Omboni S, Padwal RS, Alessa T et al. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Health 2022; 1: 7–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Sixsmith A, Horst BR, Simeonov D, Mihailidis A. Older people’s use of digital technology during the COVID-19 pandemic. Bull Sci Technol Soc 2022; 42: 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Whitten P, Holtz B, Meyer E, Nazione S. Telehospice: reasons for slow adoption in home hospice care. J Telemed Telecare 2009; 15: 187–90. [DOI] [PubMed] [Google Scholar]
- 79. Driessen A, Borgstrom E, Cohn S. Placing death and dying: making place at the end of life. Soc Sci Med 2021; 291: 113974. 10.1016/j.socscimed.2021.113974. [DOI] [PubMed] [Google Scholar]
- 80. Krawczyk M, Rush M. Describing the end-of-life doula role and practices of care: perspectives from four countries. Palliat Care Soc Pract 2020; 14: 263235242097322. 10.1177/2632352420973226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Koss SE, Weissman R, Chow V et al. Training community clergy in serious illness: balancing faith and medicine. J Relig Health 2018; 57: 1413–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Mittmann N, Liu N, MacKinnon M et al. Does early palliative identification improve the use of palliative care services? PloS One 2020; 15: e0226597. 10.1371/journal.pone.0226597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Fletcher S. Supervision needs of nurses working in the community. Int J Palliat Nurs 2008; 14: 196–200. [DOI] [PubMed] [Google Scholar]
- 84. Collier A, Morgan DD, Swetenham K, To THM, Currow DC, Tieman JJ. Implementation of a pilot telehealth programme in community palliative care: a qualitative study of clinicians’ perspectives. Palliat Med 2016; 30: 409–17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.