Abstract
Background
Negative pressure wound therapy (NPWT) is commonly used in wound management of both acute and chronic wounds. As wound care has advanced, traditional NPWT has evolved to include instillation and dwell time (NPWTi-d). To better understand the potential clinical benefits of NPWTi-d, an assessment of the available literature focusing on NPWTi-d mechanisms of action in wound management was conducted. Methods. A literature search was performed for abstracts and articles published between 2010 and 2023. Published studies in English that discussed NPWTi-d mechanisms of action and included a study population larger than 10 patients were examined.
Results
A total of 1878 articles were identified through the literature search. After removal of duplicates and article reviews, 29 studies discussing the mechanisms of action for NPWTi-d were found. Study types included case series (n = 20), comparative study (n = 6), randomized controlled trial (n = 2), and retrospective study (n = 1). These studies included approximately 1108 patients who received NPWTi-d as part of a wound care treatment plan. NPWTi-d use was associated with improved wound and clinical outcomes through wound cleansing, removal of exudate and infectious materials, and promotion of granulation tissue development.
Conclusions
The mechanisms of action for NPWTi-d helps provide wound management through wound cleansing, removal of exudate and infectious materials, and promoting the development of granulation tissue. Additional studies are warranted to fully assess the potential clinical and health economic benefits of NPWTi-d use.
Keywords: Literature Review, Negative Pressure Wound Therapy, Wound Cleansing, Wound Healing
Introduction
Negative pressure wound therapy (NPWT) is commonly used in wound management of both acute and chronic wounds. This therapy utilizes negative pressure to draw wound edges together, remove exudate and infectious materials, and promote the development of granulation tissue.1 Published literature has associated the use of NPWT with reduction in the following outcomes: time to wound healing, time to granulation tissue development, length of hospital stay (LOS), wound size, and time to wound closure.2,7 Additionally, published studies have associated use of NPWT with improved graft take.8 As wound care has advanced, traditional NPWT has evolved to include a therapy phase encompassing instillation and dwell time (NPWTi- d). This evolution allows NPWTi-d to provide wound cleansing capabilities along with traditional NPWT benefits (Figure 1).1
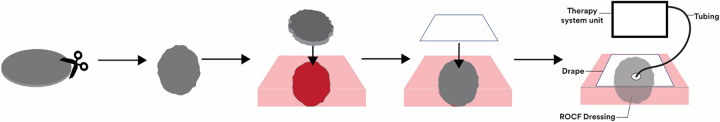
Figure 1.
NPWTi-d mechanisms of action. Blue circles represent mechanisms of action for the instillation cycle; gray circles represent mechanisms of action for the negative pressure cycle. NPWTi, negative pressure wound therapy with instillation.
NPWTi-d utilizes reticulated open-cell foam (ROCF) dressings that can be cut to fit the wound bed and a drape that is placed over the ROCF dressings and the periwound skin to provide a negative pressure and instillation solution seal (Figure 2). Once NPWTi-d therapy has been initiated, negative pressure and instillation of topical wound solution is provided in cyclical phases (Figure 3).9 During the negative pressure phase, both the dressing and wound bed are under negative pressure. The ROCF dressing collapses onto the wound bed and draws the wound edges together and removes infectious materials and exudate. Upon the removal of negative pressure, the ROCF dressing decompresses, and a user-selected volume of topical wound solution is instilled into the wound bed.9 After the topical wound solution has been allowed to soak the wound bed for a defined time limit, negative pressure is initiated, and the instillation solution is removed along with solubilized slough and debris, infectious materials, and exudate.9
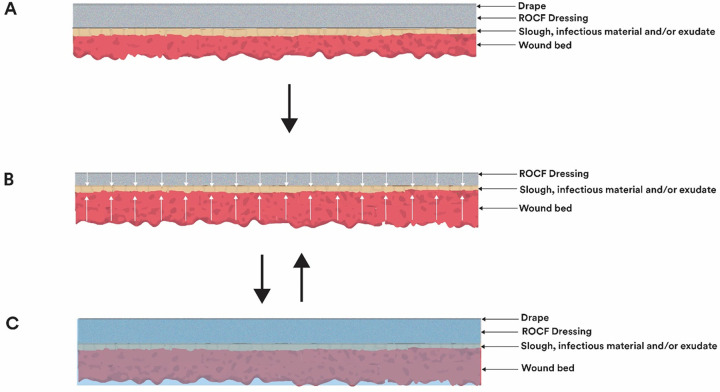
Figure 2.
Application of NPWTi-d. The ROCF dressing is cut to fit the wound bed. The ROCF dressing is then placed in the wound bed, followed by application of the drape over the foam dressing and periwound skin. The NPWTi-d tubing is then positioned over the drape and ROCF dressing, then connected to the therapy unit. NPWTi, negative pressure wound therapy with instillation; ROCF, reticulated open cell foam.
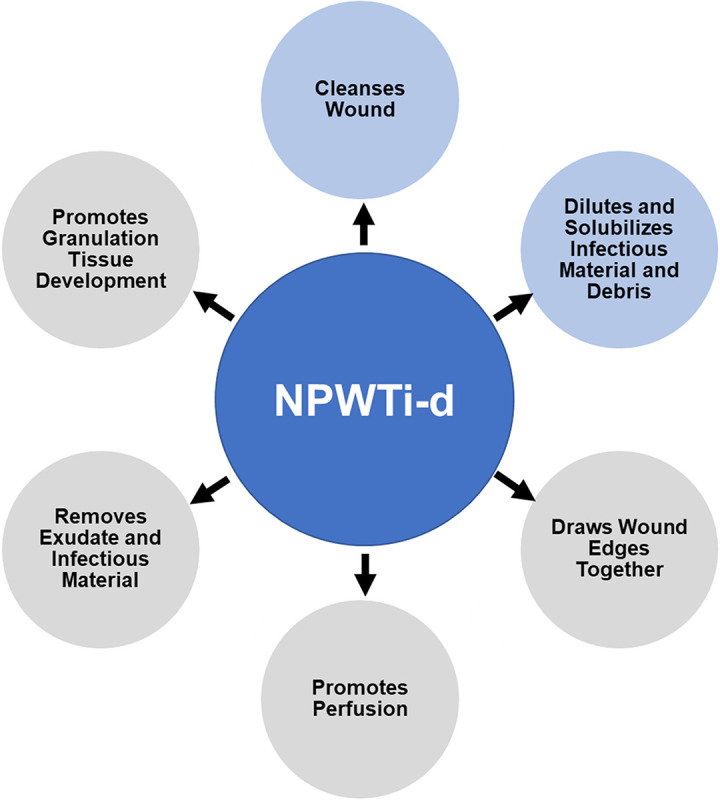
Figure 3.
Cyclic instillation of topical wound solutions. (A) The ROCF dressing is placed in the wound bed. (B) Under negative pressure, the ROCF dressing collapses onto the wound bed, wound edges are drawn together, and infectious material and exudate are removed. (C) Negative pressure is removed, the ROCF dressing decompresses, and a user-selected amount of topical wound solution is instilled into the wound bed. After the topical wound solution has been allowed to soak the wound bed for a defined time limit, negative pressure is initiated, and the instillation solution is removed along with slough, solubilized debris, infectious materials, and exudate. Adapted from Kim PJ, Applewhite A, Dardano AN, et al. Use of a novel foam dressing with negative pressure wound therapy and instillation: Recommendations and clinical experience. Wounds. 2018;30(Suppl 3):S1-S17. NPWTi, negative pressure wound therapy with instillation; ROCF, reticulated open cell foam.
NPWTi-d (3M Veraflo Therapy; 3M Company, St. Paul, MN) utilizes several different dressings to tailor the therapy to the wound and patient. ROCF dressings for NPWTi-d have higher tensile strength and are less hydrophobic than dressings used in traditional NPWT.10 The higher tensile strength helps ensure the foam dressings are completely removed from the wound bed during dressing changes while the less hydrophobic properties allow for even distribution of topical wound solutions across the wound bed.10 NPWTi-d dressings (ROCF-VF, 3M Veraflo Dressing, 3M Company) are used for open wounds, including those with shallow undermining or tunnel areas. NPWTi-d cleansing dressings (ROCF-C, 3M Veraflo Cleanse Dressings, 3M Company) are used for wounds with complex geometries, including explored tunnels or undermining. NPWTi-d dressings with through-holes (ROCF-CC, 3M Veraflo Cleanse Choice Dressing, 3M Company) are used for wounds with thick wound exudate (such as fibrin, slough, and infectious materials) and are provided as a 3-piece dressing kit.11 One-piece NPWTi-d dressings with through holes (ROCF-CCC, 3M Veraflo Cleanse Choice Complete Dressing, 3M Company) are also used for wounds with thick wound exudate. The one-piece dressing design of ROCF-CCC allows for quick application during dressing changes.
The topical wound solutions instilled into the wound bed may also be tailored to the patient's needs. Examples of solutions compatible for use with NPWTi-d include hypochlorite-based solutions, silver nitrate (0.5%), sulfur-based solutions, biguanides (polyhexanide), isotonic solutions, and topical lidocaine.12 Care should be taken not to use instillation solutions with hydrogen peroxide or solutions that are alcohol-based or contain alcohol as this can damage the ROCF dressings. While no single instillation solution has been found to be superior to another, a 2020 consensus publication of 13 clinicians recommended the use of saline for the majority of wounds. Panel members also recommended topical antiseptic solutions (such as hypochlorous acid solutions or sodium hypochlorite solutions) as a first choice for wounds with acute infection or high levels of bacteria colonization along with appropriate institutional infection management protocols.12 However, panel members noted that antiseptic solutions should be used for the first 24 to 48 hours then switched to saline to mitigate any potential cytotoxic effects of long-term use of antiseptic solutions.12 Additionally, several panel members also recommended the use of antiseptic solutions for wounds with orthopedic fixation hardware.12
The amount of instillation solution necessary for NPWTi-d use varies based on wound characteristics.13 Larger and deeper wounds require a larger volume of instillation solution than smaller and shallower wounds. Use of too much instillation solution can lead to fluid leaks or maceration, while too little instillation solution can lead to incomplete wound cleansing. The NPWTi-d device allows the clinician to set the instillation solution volume by initiating a fluid fill check.13 Here, the clinician monitors dressing and wound saturation to determine the optimal amount instillation solution and selects the instillation volume that fully saturates the dressing and covers the wound without fluid pooling.
NPWTi-d is indicated for use in patients who would benefit from vacuum-assisted drainage and the controlled delivery of topical wound solutions over the wound bed. NPWTi-d can be used in patients with chronic, acute, traumatic, sub-acute, and dehisced wounds; partial-thickness burns; diabetic, pressure, and venous leg ulcers (VLUs); and grafts.12 However, NPWTi-d is not intended for home use. Care should also be taken when applying the NPWTi-d dressings as they should not be placed directly in contact with exposed blood vessels, anastomotic sites, organs, or nerves.12 NPWTi-d is contraindicated for patients with malignancy in the wound, untreated osteomyelitis, nonenteric and unexplored fistulas, necrotic tissue with eschar, or sensitivity to silver.12 This strategy is also contraindicated for delivering fluids to the thoracic or abdominal cavity as there is a potential risk for core body temperature alteration and fluid retention within the cavity. NPWTi-d should not be used to treat biofilm or infection; however, it can be used for management of infected wounds as adjunctive therapy to the use of good clinical practice such as debridement and use of antibiotics. Additionally, neither systemic antibiotics nor topical drugs should be instilled into the wound bed via NPWTi-d.12 To better understand the potential clinical benefits of NPWTi-d, an assessment of the available literature focusing on NPWTi-d mechanisms of action in wound management was conducted. A brief summary was provided for comparative studies and randomized controlled trials (RCTs) for each mechanism of action section.
Methods
A literature search was conducted for abstracts and articles published from 2010 to 2023. Search terms included “Negative Pressure Wound Therapy” OR “Vacuum Assisted Closure” OR “Vacuum Sealing” OR “topical negative pressure” OR “negative pressure therapy” OR “subatmospheric pressure” OR “sub-atmospheric pressure” OR “NPWT” OR “NPWTi” OR “NPWTi-d” or “NPWTid” OR “NPWT-i” OR “NPWT-id” OR “Ulta” OR “VERAFLO” OR “VERAFLOW”) AND (“Lavage” OR “Instill” OR “Instillation” OR “Irrigate” OR “Irrigation” OR “Topical Solution” OR “Topic Solution” OR “Topical wound solution” OR “VERAFLO” OR “VERAFLOW”. The following inclusion criteria were used: mechanism of action, cleanse wound bed, wound coverage with topical solution during dwell time, solubilizes infectious material and wound debris, draws wound edges together, removes exudate and infectious material, promotes perfusion, promotes granulation tissue development, and NPWTi-d. Reviews and preclinical studies were excluded, as were articles published in languages other than English and those evaluating a non-NPWTi-d device, pediatric populations, sample sizes <10, and off-label use of NPWTi-d. Descriptive statistics were employed to quantitate the amount of published literature supporting NPWTi-d mechanisms of action.
Results
Literature Search Results
A total of 1878 articles were identified through the literature search (Table 1). After removal of duplicates and review articles, 29 studies discussing the mechanisms of action for NPWTi-d were found. Study types included case series (n = 20), comparative study (n = 6), RCT (n = 2), and retrospective study (n = 1). These studies represented approximately 1108 patients who received NPWTi-d as part of a wound care treatment plan.
TABLE 1.
LITERATURE SEARCH RESULTS
| Type of study | Number of studies | Number of patients |
|---|---|---|
| Case series | 20 | 718 |
| Comparative study | 6 | 186 |
| Randomized controlled trial | 2 | 104 |
| Retrospective study | 1 | 100 |
| Total | 29 | 1108 |
Patient wound types included traumatic injuries, diabetic foot ulcers, VLUs, pressure injuries, surgical wounds, dehiscence, necrotizing fasciitis, and burns. Patient comorbidities included tobacco use, obesity, diabetes, hypertension, cerebrovascular accident, heart failure, and chronic kidney disease. The patient populations identified in the literature search point to use of NPWTi-d in complex patients with potential barriers to healing.
Instillation Cycle Mechanisms of Action
Cleanses wound bed. Nine published articles (6 case series, 2 comparative studies, and 1 retrospective study) reported wound cleansing with NPWTi-d (Table 2).14,22 Two comparative studies reported wound cleansing with NPWTi-d in 85 patients compared with 71 patients receiving either standard NPWT or primary closure.21,22 Gabriel et al examined the clinical outcomes following use of NPWTi-d in patients with extremity and trunk wounds.21 A historical cohort of 34 patients managed with traditional NPWT was compared with 48 NPWTi-d patients. NPWTi-d parameters included instillation of saline or a polyhexanide solution with a 1- to 60- second dwell time, followed by 1 to 2 hours of negative pressure at −125 mm Hg. Patients in the NPWTi-d group required fewer surgical debridements (2.0 vs 4.4), experienced reduced LOS (8.1 vs 27.4 days), and reduced time to wound closure (4.1 vs 20.9 days) than patients within the NPWT group (P < .0001). Additionally, patients in the NPWTi-d group reported less painful dressing changes than those in the NPWT group. The authors stated that the improved clinical outcomes in the NPWTi-d group were due to wound cleansing and exudate removal.
TABLE 2.
ARTICLES REPORTING WOUND BED CLEANSING WITH NPWTi-d USE
| Article | Study type | Study population | Outcomes |
|---|---|---|---|
| Blome-Eberwein et al, 201814 | Case series | 21 patients
|
|
| Delapena et al, 202015 | Case series | 10 patients
|
|
| Latouche et al, 202016 | Case series | 15 patients
|
|
| Porfidia et al, 202017 | Case series | 13 patients
|
|
| Yang et al, 201518 | Case series | 10 patients
|
|
| Zhang et al, 202119 | Case series | 32 patients
|
|
| Bassetto et al, 202120 | Retrospective | 100 patients
|
|
| Gabriel et al, 201421 | Comparative study | 34 historical controls, 48 NPWTi-d patients
|
|
| Yane et al, 202222 | Comparative study | 37 historical controls, 37 NPWTi-d patients
|
|
DFU, diabetic foot ulcer; LOS, length of hospital stay; NPWTi-d, negative pressure wound therapy with instillation and dwell time; PI, pressure injury; SSI, surgical site infection; VLU, venous leg ulcer.
Yane et al assessed the use the NPWTi-d in patients undergoing stoma closure.22 Patients underwent either primary closure (n = 37) or fascial closure followed by NPWTi-d (n = 37).22 Propensity score matching was utilized to reduce selection bias. NPWTi-d parameters included a 2-minute dwell time followed by 2 hours of negative pressure at −75 mm Hg. Granulation tissue development in the NPWTi-d group was confirmed by visual assessment. As the control group underwent immediate primary closure, assessment of granulation tissue development was not performed in this group. Results indicated similar LOS between the 2 groups (9 vs 10 days) and reduced rates of surgical site infection (SSI) in the NPWTi-d group (0 vs 6 patients). The authors surmised that NPWTi-d contributed to reduced SSI rates due to wound bed cleansing along with removal of solubilized devitalized tissue and exudate and the promotion of granulation tissue, which helped to reduce dead space.
Dilutes and solubilizes infectious material and wound debris. Ten articles (9 case series, 1 comparative study) reported the dilution and solubilization of infectious material and wound debris (Table 3).11,14,15,17,23,28 Chowdhry and colleagues compared outcomes in 30 patients (15 NPWTi-d and 15 wet-to-dry dressings) with sternal wounds.28 NPWTi-d parameters included use of the ROCF-CC dressing and instillation of 0.0625% sodium hypochlorite solution with a 20- minute dwell time followed by 2 hours of negative pressure at −125 mm Hg. ROCF-CC dressings were changed every 2 to 3 days. The control group received wet-to-dry dressing soaked in 0.0625% sodium hypochlorite solution and changed every 6 hours. The NPWTi-d group demonstrated a shorter time to closure (7.9 ± 2.3 vs 13.9 ± 3.2 days), fewer surgical debridements (1.8 ± 0.7 vs 3.1 ± 1.0), and a shorter duration for drain use (15.0 ± 2.0 vs 21.7 ± 3.9 days) than the control group. This was attributed to the ability of NPWTi-d to solubilize and remove slough, thick exudate, and debris from the wound bed.
TABLE 3.
ARTICLES REPORTING DILUTION AND SOLUBILIZATION OF INFECTIOUS MATERIAL AND WOUND DEBRIS WITH NPWTi-d USE
| Article | Study type | Study population | Outcomes |
|---|---|---|---|
| Blalock, 201923 | Case series | 19 patients
|
|
| Blome-Eberwein et al, 201814 | Case series | 21 patients
|
|
| Delapena et al, 202015 | Case series | 10 patients
|
|
| Elhessy et al, 202124 | Case series | 20 patients
|
|
| Fernández et al, 202025 | Case series | 19 patients
|
|
| McElroy, 201926 | Case series | 14 patients
|
|
| Porfidia et al, 202017 | Case series | 13 patients
|
|
| Téot et al, 201711 | Case series | 21 patients
|
|
| Willmore et al, 202127 | Case series | 15 patients
|
|
| Chowdhry et al, 201928 | Comparative study | 15 NPWTi-d patients, 15 wet-to-dry dressing patients
|
|
DFU, diabetic foot ulcer; LOS, length of hospital stay; NPWTi-d, negative pressure wound therapy with instillation and dwell time; PI, pressure injury; SSI, surgical site infection; VLU, venous leg ulcer.
Negative Pressure Cycle Mechanisms of Action
Draws wound edges together. While no published studies were found to have assessed the ability of NPWTi-d to draw the wound edges together, it is expected that NPWTi-d performs this action during the negative pressure cycle as drawing the wound edges together has been linked with the use of NPWT.29,31
Removes exudate and infectious material. Fourteen studies (8 case series, 3 comparative, 1 retrospective, 2 RCT) reported on the removal of exudate and infectious material (Table 4).11,20,21,23,32,41 Four comparative studies involving a total of 138 patients reported removal of exudate and infectious materials with the use of NPWTi-d compared with traditional dressings or NPWT.21,37,39 A 2014 article from Gabriel et al examined clinical outcomes of NPWTi-d use in patients with extremity and trunk wounds and has already been described in a previous section.21 In a 2008 article, Gabriel and colleagues assessed the use of NPWTi-d in the management of patients with infected wounds.37 Outcomes in a group of 15 patients receiving instillation NPWT (NPWTi) were compared with those of a historic cohort of 15 patients who received traditional dressings. All patients received antibiotic therapy. Wound types assessed included necrotizing fasciitis, pressure injury, traumatic wounds, and wound dehiscence. NPWTi therapy parameters included instillation of silver nitrate (0.5%) with a 1-second dwell time followed by continuous negative pressure at −125 mm Hg for 2 hours.37 Patients in the NPWTi group displayed a shorter length of therapy (9.9 ± 4.3 vs 36.5 ± 13.1 days) and LOS (14.7 ± 9.2 vs 39.2 ± 12.1 days), earlier clearance of wound infection (6.0 ± 1.5 vs 25.9 ± 6.6 days), and shorter time to wound closure (13.2 ± 6.8 vs 29.6 ± 6.5 days) attributed to the removal of infectious materials.37
TABLE 4.
ARTICLES REPORTING THE REMOVAL OF EXUDATE AND INFECTIOUS MATERIAL WITH NPWTi-d USE
| Article | Study type | Study population | Outcomes |
|---|---|---|---|
| Blalock, 201923 | Case series | 19 patients
|
|
| Diehm et al, 202032 | Case series | 30 patients
|
|
| Eckstein et al, 201933 | Case series | 15 patients
|
|
| Felte et al, 201634 | Case series | 11 patients
|
|
| Ludolph et al, 201935 | Case series | 267 patients
|
|
| Sir et al, 201936 | Case series | 10 patients
|
|
| Téot et al, 201711 | Case series | 21 patients
|
|
| Bassetto et al, 202120 | Retrospective | 100 patients
|
|
| Gabriel et al, 201421 | Comparative study | 48 NPWTi-d patients, 34 historical controls
|
|
| Gabriel et al, 200837 | Comparative study | 15 NPWTi patients, 15 historic controls
|
|
| Goss et al, 201438 | Comparative study | 7 NPWTi patients, 7 traditional NPWT patients
|
|
| Kim et al, 201439 | Comparative study | 34 NPWTi-d (6-minute dwell) patients, 34 NPWTi-d (20-minute dwell) patients, 74 traditional NPWT patients
|
|
| Kim et al, 202040 | RCT | 93 NPWTi-d patients, 88 traditional NPWT patients
|
|
| Yang et al, 201741 | RCT | 11 NPWTi-d patients, 9 traditional NPWT patients
|
|
CFU, colony-forming unit; DFU, diabetic foot ulcer; LOS, length of hospital stay; NPWT, negative pressure wound therapy; NPWTi, negative pressure wound therapy with instillation; NPWTi-d, negative pressure wound therapy with instillation and dwell time; PI, pressure injury; RCT, randomized controlled trial; SSI, surgical site infection; VLU, venous leg ulcer.
Goss et al compared wound bioburden in patients with chronically infected wounds (ie, VLU, diabetic foot ulcer, necrotizing fasciitis, and trauma) receiving 1 week of NPWTi-d (n = 7) or traditional NPWT (n = 7).38 The NPWTi-d group received instillation of 0.5% Dakin's solution into the wound bed followed by a 10-minute dwell time and 1 hour of continuous negative pressure at −125 mm Hg. The authors reported a mean absolute reduction in wound bioburden of 10.6 × 106 bacteria per gram of tissue in the NPWTi-d group due to wound cleansing and the removal by NPWTi-d of infectious materials.38
Kim et al compared clinical outcomes following the use of traditional NPWT (n = 74) or NPWTi-d with either a 6-minute dwell time (n = 34) or 20-minute dwell time (n = 34).39 Patient wound types included traumatic, ischemic wounds, neuropathic wounds, and ulcers. The NPWTi-d groups received a polyhexanide instillation solution that was allowed to dwell in the wound bed for either 6 or 20 minutes followed by 2 to 3.5 hours of continuous negative pressure at −125 mm Hg. The number of operating room visits were significantly fewer with 6-minute NPWTi-d (2.4 ± 0.9) and 20-minute NPWTi-d (2.6 ± 0.9) compared with traditional NPWT (3.0 ± 0.9, P < .05). Similarly, both 6- and 20-minute NPWTi-d groups experienced a shorter time to wound closure (7.8 ± 5.2 days and 7.5 ± 3.1 days, respectively) than the NPWT group (9.23 ± 5.2 days, P < .05). A shorter LOS was observed in the 20-minute dwell NPWTi-d group (11.4 ± 5.1) compared to the NPWT group (14.92 ± 9.2 days; P < .05).39 Additionally, a higher percentage of wounds closed (94% vs 62%) and gram-positive wound culture improvement (90% vs 63%) was observed in the 6-minute dwell NPWTi-d group.39 These results point to the removal of infectious materials with NPWTi-d use.
Two RCTs reporting the removal of exudate and infectious material were identified in the literature search.40,41 In 2020, Kim et al assessed the impact of NPWTi-d use in patients requiring surgical debridement.40 The NPWTi-d group (n = 93) received instillation of a polyhexanide solution with a 20-minute dwell time, followed by 2 hours of negative pressure at −125 mm Hg. The control group (n = 88) received traditional NPWT. The patient population had arterial ulcers, burn wounds, diabetic foot ulcers, necrotizing fasciitis, pressure injuries, surgical wounds, traumatic wounds, or VLUs.40 No differences were found between the NPWTi-d or control groups in the number of surgical debridements, time to wound closure, percentage of wounds closed or complications. However, the NPWTi-d group did show a decrease in total bacterial counts (0.18 ± 2.15 log colony-forming units/g reduction), indicating the removal of infectious materials with NPWTi-d use.40 Yang and colleagues examined the effect of NPWTi-d use on bioburden in infected wounds (ie, VLU, diabetic foot ulcers, and mixed etiology ulcers).41 The NPWTi-d group (n = 11) received 0.125% sodium hypochlorite solution instilled into the wound bed with a 10-minute dwell time followed by 1 hour of negative pressure at −125 mm Hg. The control group (n = 9) received traditional NPWT. In both groups, surgical debridement was performed before therapy initiation, and therapy was continued for 1 week. The authors reported a 43% reduction in biofilm-protected bacteria in the NPWTI-d group. The authors believe that the fluid irrigation of the wound bed and subsequent removal of the irrigant may disrupt wound biofilm.41
Promotes perfusion. The promotion of perfusion has been associated with NPWT use.42,44 Therefore, this mechanism of action is expected to occur during the negative pressure cycle within the user-selected therapy parameters.
Promotes granulation tissue development. Thirteen studies (12 case series, 1 comparative) reported the promotion of granulation tissue development (Table 5)16,18,19,22,23,25,26,33,34,36,45,47 One comparative study reporting observation of granulation tissue development after NPWTi-d use in 37 patients undergoing stoma closure with and without use of NPWTi-d before closure was identified in the literature search.22 Yane et al assessed the use of NPWTi-d in 37 patients undergoing stoma closure and had been previously discussed in the wound bed cleansing section.22 Briefly, visual inspection of the wound noted that granulation tissue development was observed in the NPWTi-d group, which the authors attributed to use of NPWTi-d.
TABLE 5.
ARTICLES REPORTING GRANULATION TISSUE DEVELOPMENT WITH NPWTi-d USE
| Article | Study type | Study population | Outcomes |
|---|---|---|---|
| Blalock, 201923 | Case series | 19 patients
|
|
| Brinkert et al, 201345 | Case series | 131 patients
|
|
| Eckstein et al, 201933 | Case series | 15 patients
|
|
| Felte et al, 201634 | Case series | 11 patients
|
|
| Fernández et al, 202025 | Case series | 19 patients
|
|
| Fluieraru et al, 201346 | Case series | 24 patients
|
|
| Latouche et al, 202016 | Case series | 15 patients
|
|
| McElroy, 201926 | Case series | 14 patients
|
|
| Sir et al, 201936 | Case series | 10 patients
|
|
| Uncu et al, 201747 | Case series | 15 patients
|
|
| Yang et al, 201518 | Case series | 10 patients
|
|
| Zhang et al, 202119 | Case series | 32 patients
|
|
| Yane et al, 202222 | Comparative study | 37 historical controls, 37 NPWTi-d patients
|
|
DFU, diabetic foot ulcer; LOS, length of hospital stay; NPWTi, negative pressure wound therapy with instillation; NPWTi-d, negative pressure wound therapy with instillation and dwell time; PI, pressure injury; SSI, surgical site infection; VLU, venous leg ulcer.
Discussion
A total of 29 articles discussing the mechanisms of action for NPWTi-d use were identified. These articles encompassed a wide range of acute and chronic wound types in 1108 patients. Based on our literature search, the use of NPWTi-d has been associated with wound cleansing; the removal of slough, solubilized debris, exudate, and infectious materials; and promoting granulation tissue development.
The wound healing associated with NPWTi-d use can also impact other clinical outcomes, such as length of therapy, time to wound closure, and LOS. A 2021 article from Gabriel et al reported significantly shorter length of NPWTi-d therapy compared with that of the control group (standardized means across studies of 1.52 vs 3.49 days) in a meta-analysis of 13 comparative studies.48 Similarly, Garcia-Ruano et al reported a shorter total time of treatment in the NPWTi-d group (2.4 ± 1.6 months) compared with patients receiving conventional dressings (31.3 ± 37.2 months) in abdominal wounds with mesh exposure.49 A 2008 article by Gabriel and colleagues that examined the use of NPWTi-d in infected wounds also reported reduced treatment time in the NPWTi-d group compared with a historical control managed with traditional wound dressings (9.9 ± 4.3 days vs 36.5 ± 1.5 days, respectively).37
Use of NPWTi-d has also been associated with reduced time to wound closure. A 2021 13-study meta-analysis by Gabriel et al reported reduced time to wound closure in patients that received NPWTi-d compared with that seen in patients whose wounds were managed with standard dressings (standardized means across studies 3.02 vs 4.16 days).48 This is similar to the findings reported in 2008 and 2014 publications from Gabriel and colleagues that assessed the use of NPWTi-d in patients with infected wounds, dehiscence, pressure injuries, or traumatic wounds.21,37 In these 2 earlier articles, reduced time to closure was approximately 16 days shorter in the NPWTi-d groups. Other studies have shown similar results; Chowdhry et al reported a 1.75-fold shorter time needed for closure, while Kim et al (2014) and Garcia-Ruano reported decreases ranging from 1.5 days to 28 months in patients receiving NPWTi-d versus those who received traditional dressings or traditional NPWT.28,39,49 The wide differences in reporting were due to how time to closure was assessed, the patient population, and wound types assessed.28,39,49 However, an RCT by Kim et al reported similar time to wound closure in NPWTi-d patients compared with that seen with traditional NPWT.40 Of note, while time to wound closure was found to be similar between the NPWTi-d and control groups, the control group was found to have a risk of re-hospitalization that was 3.1 times higher than that of the NPWTi-d group.40 This would putatively indicate that, while time to wound closure was not affected in this population, NPWTi-d use did provide a clinical benefit to the patients.
Although NPWTi-d use can result in positive patient outcomes, its effect on patient LOS is unclear. Three studies reported similar LOS for patients who received NPWTi-d and those who received traditional treatment, while 3 studies reported reduced LOS with NPWTi-d use. The Gabriel et al meta-analysis reported similar LOS between NPWTi-d and control groups.48 The Garcia-Ruano et al and Yane et al articles also reported similar LOS between NPWTi-d and control groups in patients with abdominal wall wounds with mesh exposure or patients undergoing stoma closure.22,49 However, reports from 3 other comparative studies reported reduced LOS (ranging from 3.52 to 24.53 days shorter) in the group managed with NPWTi- d.21,37,39 These studies compared patients receiving NPWTi-d with those who received either traditional dressings or NPWT for surgical, trauma, ulcers, or infected wounds. As the patient populations and wound types assessed were similar across the 6 studies, it is unclear why some studies reported similar LOS while others reported reduced LOS between the groups. Larger- scale studies would be helpful to examine the effect of NPWTi-d use on patient LOS more fully. Clinical benefits have been associated with NPWTi-d use; however, only 3 articles have reported on the potential effect of NPWTi-d use on cost of care.18,21,50 The cost analysis by Yang and colleagues reported the estimated costs per wound for both NPWTi-d and compression therapy (including hospital stays, office visits, and additional wound care materials) resulted in a per patient cost savings of $1000 versus compression therapy alone.18 Gabriel et al utilized an economic model to assess potential cost-effectiveness of NPWTi-d in extremity and trunk wounds.21 Compared with traditional NPWT, the economic model suggested a potential reduction of operating room costs by $8143. Similarly, Kim et al observed potential per patient savings of $33,338, €8,467, or £5,626 in an economic model assessing the cost of care with NPWTi-d versus standard dressings in hospitalized patients in the US, Germany, and the United Kingdom, respectively.50 While these 3 articles report a potential cost savings with NPWTi-d use, caution should be used in associating a cost benefit with NPWTi-d use in all populations until this trend is confirmed with additional data from various specific populations.
Conclusions
NPWTi-d helps manage wounds by providing wound cleansing, removing exudate and infectious materials, and promoting development of granulation tissue. This literature search identified 29 articles that associated NPWTi-d use with wound bed cleansing; dilution; solubilization; removal of infectious materials, debris, and exudate; and promotion of granulation tissue development. Use of NPWTi-d was also reported to contribute to reduced length of therapy, reduced number of surgical debridements, and shortened time to wound closure when compared with standard of care dressings or traditional NPWT. However, additional studies are warranted to more fully assess the potential clinical and health economic benefits of NPWTi-d use.
Acknowledgments
The author thanks Ricardo Martinez (3M) and Julie M Robertson (3M) for assistance with manuscript preparation and editing. The author also thanks Christina Hernandez (3M) for assistance with figure development.
References
- 1.Normandin S, Safran T, Winocour S, et al. Negative pressure wound therapy: Mechanism of action and clinical applications. Semin Plast Surg. 2021;35(3):164–170. doi:10.1055/s-0041-1731792 10.1055/s-0041-1731792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen L, Zhang S, Da J, et al. A systematic review and meta-analysis of efficacy and safety of negative pressure wound therapy in the treatment of diabetic foot ulcer. Annals of palliative medicine. 2021;10(10):10830–10839. doi:10.21037/apm-21-2476 10.21037/apm-21-2476 [DOI] [PubMed] [Google Scholar]
- 3.Lin DZ, Kao YC, Chen C, Wang HJ, Chiu WK. Negative pressure wound therapy for burn patients: A meta-analysis and systematic review. Int Wound J. 2021;18(1):112–123. doi:10.1111/iwj.13500 10.1111/iwj.13500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maranna H, Lal P, Mishra A, et al. Negative pressure wound therapy in grade 1 and 2 diabetic foot ulcers: A randomized controlled study. Diabetes Metab Syndr. 2021;15(1):365–371. doi: 10.1016/j.dsx.2021.01.014 10.1016/j.dsx.2021.01.014 [DOI] [PubMed] [Google Scholar]
- 5.Sahin E, Rizalar S, Ozker E. Effectiveness of negative-pressure wound therapy compared to wet-dry dressing in pressure injuries. J Tissue Viability. 2022;31(1):164–172. doi:10.1016/j.jtv.2021.12.007 10.1016/j.jtv.2021.12.007 [DOI] [PubMed] [Google Scholar]
- 6.Seidel D, Diedrich S, Herrle F, et al. Negative pressure wound therapy vs conventional wound treatment in subcutaneous abdominal wound healing impairment: The SAWHI randomized clinical trial. JAMA Surg. 2020;155(6):469–478. doi:10.1001/jamasurg.2020.0414 10.1001/jamasurg.2020.0414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song YP, Wang L, Yuan BF, et al. Negative-pressure wound therapy for III/IV pressure injuries: A meta-analysis. Wound Repair Regen. 2021;29(1):20–33. doi: 10.1111/wrr.12863 10.1111/wrr.12863 [DOI] [PubMed] [Google Scholar]
- 8.Yin Y, Zhang R, Li S, Guo J, Hou Z, Zhang Y. Negative-pressure therapy versus conventional therapy on split-thickness skin graft: A systematic review and meta-analysis. Int J Surg. 2017;50:43–48. doi:10.1016/j.ijsu.2017.12.020 10.1016/j.ijsu.2017.12.020 [DOI] [PubMed] [Google Scholar]
- 9.Kim PJ, Applewhite A, Dardano AN, et al. Use of a novel foam dressing with negative pressure wound therapy and instillation: Recommendations and clinical experience. Wounds. 2018;30(Suppl 3:S1–S17. [PubMed] [Google Scholar]
- 10.Lessing C, Slack P, Hong KZ, Kilpadi D, McNulty A. Negative pressure wound therapy with controlled saline instillation (NPWTi): dressing properties and granulation response in vivo. Wounds. 2011;23(10:309–319. [PubMed] [Google Scholar]
- 11.Teot L, Boissiere F, Fluieraru S. Novel foam dressing using negative pressure wound therapy with instillation to remove thick exudate. Int Wound J. 2017;14(5):842–848. doi:10.1111/iwj.12719 10.1111/iwj.12719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim PJ, Attinger CE, Constantine T, et al. Negative pressure wound therapy with instillation: International consensus guidelines update. Int Wound J. 2020;17(1):174–186. doi: 10.1111/iwj.13254 10.1111/iwj.13254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Driver RK. Utilizing the VeraFlo instillation negative pressure wound therapy system with advanced care for a case study. Cureus. 2016;8(11):e903. doi: 10.7759/cureus.903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blome-Eberwein S, Lozano D, Amani H. Utility of negative pressure wound therapy with instillation in a burn center. Burns Open. 2018;2(4):208–212. doi: 10.1016/j.burnso.2018.05.004 10.1016/j.burnso.2018.05.004 [DOI] [Google Scholar]
- 15.Delapena S, Fernandez LG, Foster KN, Matthews MR. Negative pressure wound therapy with instillation and dwell time for the management of complex wounds: A case series. Wounds. 2020;32(12:E96–e100. [PubMed] [Google Scholar]
- 16.Latouche V, Devillers H. Benefits of negative pressure wound therapy with instillation in the treatment of hard-to-heal wounds: a case series. J Wound Care. 2020;29(4):248–253. doi: 10.12968/jowc.2020.29.4.248 10.12968/jowc.2020.29.4.248 [DOI] [PubMed] [Google Scholar]
- 17.Porfidia R, Grimaldi S, Ciolli MG, Romano A, Grimaldi S. Treatment of wound dehiscence utilizing negative pressure wound therapy with instillation and dwell time in emergency abdominal surgery: A step-by-step closure protocol. Wounds. 2020;32(12:E114–e119. [PubMed] [Google Scholar]
- 18.Yang CK, Alcantara S, Goss S, Lantis JC, II. Cost analysis of negative-pressure wound therapy with instillation for wound bed preparation preceding split-thickness skin grafts for massive (>100 cm(2)) chronic venous leg ulcers. J Vasc Surg. 2015;61(4):995–999. doi: 10.1016/j.jvs.2014.11.076 10.1016/j.jvs.2014.11.076 [DOI] [PubMed] [Google Scholar]
- 19.Zhang BR, Fan X, Zhao JC, Shi K, Yu JA. Negative pressure wound therapy with instillation and dwell time in the wound management of necrotizing fasciitis. J Tissue Viability. 2021;30(2):262–266. doi: 10.1016/j.jtv.2021.02.012 10.1016/j.jtv.2021.02.012 [DOI] [PubMed] [Google Scholar]
- 20.Bassetto F, de Antoni E, Rizzato S, Scarpa C. Management of acute and chronic wounds using negative pressure wound therapy with instillation and dwell time: A retrospective review of a 100-patient cohort in Padova, Italy. Wounds. 2021;doi:10.25270/wnds/081421.01 [DOI] [PubMed]
- 21.Gabriel A, Kahn K, Karmy-Jones R. Use of negative pressure wound therapy with automated, volumetric instillation for the treatment of extremity and trunk wounds: clinical outcomes and potential cost-effectiveness. Eplasty. 2014;14:e41. [PMC free article] [PubMed] [Google Scholar]
- 22.Yane Y, Hida JI, Chiba Y, et al. Effectiveness of negative pressure wound therapy with instillation and dwelling after stoma closure: a retrospective and propensity score matching analysis. Sci Rep. 2022;12(1):916. doi:10.1038/s41598-022-05016-1 10.1038/s41598-022-05016-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blalock L. Use of negative pressure wound therapy with instillation and a novel reticulated open-cell foam dressing with through holes at a level 2 trauma center. Wounds. 2019;31(2:55–58. [PubMed] [Google Scholar]
- 24.Elhessy AH, Chaudhry AR, Hammouda AI, Giacobbe SD, Gesheff MG, Conway JD. Experience with negative-pressure wound therapy with instillation in complex infected orthopaedic wounds. Int Wound J. 2021;doi:10.1111/iwj.13592 [DOI] [PMC free article] [PubMed]
- 25.Fernandez LG, Matthews MR, Ellman C, Jackson P, Villareal DH, Norwood S. Use of reticulated open cell foam dressings with through holes during negative pressure wound therapy with instillaton and dwell time: A large case study. Wounds. 2020;32(10:279–282. [PubMed] [Google Scholar]
- 26.McElroy EF. Use of negative pressure wound therapy with instillation and a reticulated open cell foam dressing with through holes in the acute care setting. Int Wound J. 2019;16(3):781–787. doi: 10.1111/iwj.13097 10.1111/iwj.13097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Willmore J, Wrotslavsky P Preoperative contaminated wound management using short-term negative pressure wound therapy with instillation. J Wound Care. 2021;30(12):994–1000. doi:10.12968/jowc.2021.30.12.994 10.12968/jowc.2021.30.12.994 [DOI] [PubMed] [Google Scholar]
- 28.Chowdhry SA, Wilhelmi BJ. Comparing negative pressure wound therapy with instillation and conventional dressings for sternal wound reconstructions. Plast Reconstr Surg Glob Open. 2019;7(1):e2087. doi:10.1097/GOX.0000000000002087 10.1097/GOX.0000000000002087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Putnis S, Khan WS, Wong JM. Negative pressure wound therapy - a review of its uses in orthopaedic trauma. Open Orthop J. 2014;8:142–147. doi:10.2174/1874325001408010142 10.2174/1874325001408010142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38(6:563–576. 10.1097/00000637-199706000-00002 [DOI] [PubMed] [Google Scholar]
- 31.Orgill DP, Manders EK, Sumpio BE, et al. The mechanisms of action of vacuum assisted closure: more to learn. Surgery. 2009;146(1):40–51. doi: 10.1016/j.surg.2009.02.002 10.1016/j.surg.2009.02.002 [DOI] [PubMed] [Google Scholar]
- 32.Diehm YF, Loew J, Will PA, et al. Negative pressure wound therapy with instillation and dwell time (NPWTi-d) with V.A.C. VeraFlo in traumatic, surgical, and chronic wounds-A helpful tool for decontamination and to prepare successful reconstruction. Int Wound J. 2020;17(6):1740–1749. doi:10.1111/iwj.13462 10.1111/iwj.13462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eckstein FM, Pinsel V, Wurm MC, et al. Antiseptic negative pressure instillation therapy for the treatment of septic wound healing deficits in oral and maxillofacial surgery. J Craniomaxillofac Surg. 2019;47(3):389–393. doi:10.1016/j.jcms.2018.12.006 10.1016/j.jcms.2018.12.006 [DOI] [PubMed] [Google Scholar]
- 34.Felte R, Gallagher KE, Tinkoff GH, Cipolle M. A case review series of Christiana Care Health System's experience with negative pressure wound therapy instillation. Cureus. 2016;8(11):e865. doi: 10.7759/cureus.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ludolph I, Fried FW, Kneppe K, Arkudas A, Schmitz M, Horch RE. Negative pressure wound treatment with computer-controlled irrigation/instillation decreases bacterial load in contaminated wounds and facilitates wound closure. Int Wound J. 2018;15(6):978–984. doi:10.1111/iwj.12958 10.1111/iwj.12958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sir E, Aksoy A, Ucar AD. The use of negative-pressure wound therapy with instillation before and after grafting in the surgical management of hidradenitis suppurativa. Turk J Colorectal Dis. 2019;29(4):177–182. doi: 10.4274/tjcd.galenos.2019.2019-6-1 10.4274/tjcd.galenos.2019.2019-6-1 [DOI] [Google Scholar]
- 37.Gabriel A, Shores J, Heinrich C, et al. Negative pressure wound therapy with instillation: a pilot study describing a new method for treating infected wounds. Int Wound J. 2008;5(3):399–413. doi: 10.1111/j.1742-481X.2007.00423.x 10.1111/j.1742-481X.2007.00423.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goss SG, Schwartz JA, Facchin F, Avdagic E, Gendics C, Lantis JC, II. Negative pressure wound therapy with instillation (NPWTi) better reduces postdebridement bioburden in chronically infected lower extremity wounds than NPWT alone. J Am Coll Clin Wound Spec. 2014;4(4):74–80. doi: 10.1016/j.jccw.2014.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim PJ, Attinger CE, Steinberg JS, et al. The impact of negative-pressure wound therapy with instillation compared with standard negative-pressure wound therapy: a retrospective, historical, cohort, controlled study. Plast Reconstr Surg. 2014;133(3):709–716. doi: 10.1097/01.prs.0000438060.46290.7a 10.1097/01.prs.0000438060.46290.7a [DOI] [PubMed] [Google Scholar]
- 40.Kim PJ, Lavery LA, Galiano RD, et al. The impact of negative-pressure wound therapy with instillation on wounds requiring operative debridement: Pilot randomised, controlled trial. Int Wound J. 2020;17(5):1194–1208. doi: 10.1111/iwj.13424 10.1111/iwj.13424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang C, Goss SG, Alcantara S, Schultz G, Lantis Ii JC. Effect of negative pressure wound therapy with instillation on bioburden in chronically infected wounds. Wounds. 2017;29(8:240–246. [PubMed] [Google Scholar]
- 42.Timmers MS, Le Cessie S, Banwell P, Jukema GN. The effects of varying degrees of pressure delivered by negative-pressure wound therapy on skin perfusion. Ann Plast Surg. 2005;55(6):665–671. doi: 10.1097/01.sap.0000187182.90907.3d 10.1097/01.sap.0000187182.90907.3d [DOI] [PubMed] [Google Scholar]
- 43.Schintler MV. Negative pressure therapy: theory and practice. Diabetes Metab Res Rev. 2012;28(Suppl 1):72–77. doi: 10.1002/dmrr.2243 10.1002/dmrr.2243 [DOI] [PubMed] [Google Scholar]
- 44.Muenchow S, Horch RE, Dragu A. Effects of topical negative pressure therapy on perfusion and microcirculation of human skin. Clin Hemorheol Microcirc. 2019;72(4):365–374. doi:10.3233/CH-180536 10.3233/CH-180536 [DOI] [PubMed] [Google Scholar]
- 45.Brinkert D, Ali M, Naud M, Maire N, Trial C, Teot L. Negative pressure wound therapy with saline instillation: 131 patient case series. Int Wound J. 2013;10(Suppl 1):56–60. doi:10.1111/iwj.12176 10.1111/iwj.12176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fluieraru S, Bekara F, Naud M, et al. Sterile-water negative pressure instillation therapy for complex wounds and NPWT failures. J Wound Care. 2013;22(6):293–299. doi: 10.12968/jowc.2013.22.6.293 10.12968/jowc.2013.22.6.293 [DOI] [PubMed] [Google Scholar]
- 47.Uncu H, Cetinkaya A. Negative pressure wound therapy with polyhexanide/betaine instillation. J Wound Care. 2017;26(SUPPL 6):196. doi:10.12968/jowc.2017.26.Sup6b.1 [Google Scholar]
- 48.Gabriel A, Camardo M, O'Rorke E, Gold R, Kim PJ. Effects of negative-pressure wound therapy with instillation versus standard of care in multiple wound types: Systematic literature review and meta-analysis. Plast Reconstr Surg. 2021;147(1S-1):68S–76S. doi:10.1097/PRS.0000000000007614 10.1097/PRS.0000000000007614 [DOI] [PubMed] [Google Scholar]
- 49.Garcia-Ruano A, Deleyto E, Garcia-Fernandez S. VAC-instillation therapy in abdominal mesh exposure: a novel indication. J Surg Res. 2016;206(2):292–297. doi:10.1016/j.jss.2016.08.030 10.1016/j.jss.2016.08.030 [DOI] [PubMed] [Google Scholar]
- 50.Kim PJ, Lookess S, Bongards C, Griffin LP, Gabriel A. Economic model to estimate cost of negative pressure wound therapy with instillation vs control therapies for hospitalised patients in the United States, Germany, and United Kingdom. Int Wound J. 2022;19(4):888–894. doi:10.1111/iwj.13689 10.1111/iwj.13689 [DOI] [PMC free article] [PubMed] [Google Scholar]