Abstract
Background
Acute Achilles tendon rupture is a common injury and when missed leads to the development of a chronic Achilles tendon rupture. Studies suggest surgical treatment (either repair or reconstruction) for most patients with a chronic Achilles rupture due to the functional deficit caused by the lack of an intact Achilles tendon. Numerous autograft options such as the flexor hallucis longus, hamstrings, peroneal and quadriceps tendon have been used to reconstruct the Achilles tendon, either as a tendon transfer or as an interposition graft. The choice of autograft used usually depends on the size of the defect left after debridement of the Achilles tendon edges, but is often dictated by surgeon preference and tissue availability. Currently, there is no consensus as to the best autograft option.
Aims and methodology
The aim of this study was to evaluate the various autograft options used to reconstruct the Achilles tendon, and the advantages and disadvantages of using each tendon, focussing specifically on the harvesting technique, anatomical and biomechanical properties. This was done by reviewing the current published literature, supplemented by carrying out anatomical dissection in the cadaveric lab.
Results
The flexor hallucis longus is synergistically related to the Achilles tendon and biomechanically strong, however harvesting can result in weakness in big toe flexion. The peroneus brevis whilst being biomechanically strong is a much shorter tendon compared to the other autograft options. Similarly, the quadriceps tendon is also a strong tendon option, but may not be appropriate for larger chronic Achilles tendon rupture gaps. The semitendinosus tendon can be tripled/quadrupled to resemble the Achilles tendon, but is associated with higher risks of patient morbidity when harvesting the tendon.
Conclusion
Treatment of chronic Achilles tendon ruptures remains a challenge. Each autograft option has its own unique advantages and disadvantages which should be considered on a case-specific basis. Further work is required to analyse the biomechanical properties of the autograft options to determine if one option is superior.
Keywords: Orthopaedics, Tendoachilles, Achilles rupture, Autograft, Tendon transfer, Interposition graft, Flexor hallucis longus, Hamstrings, Quadriceps, Peroneus brevis
1. Introduction
The annual incidence of acute Achilles tendon rupture (ATR) is approximately 4500 cases in the United Kingdom.1,2 Patients with ATRs are classically men in their late 30s, however there has been an increasing incidence in older patients, likely due to a more active lifestyle in this demographic.3 The vast majority of ruptures occur during sporting activities (football, squash, basketball) which involve forceful plantar flexion of the foot. Patients typically tend to be intermittently active (termed as “weekend warriors”) and therefore do not condition their muscles prior to participating in sports, thus increasing their risk of sustaining an ATR. Interestingly, up to 25% of ruptures occur in sedentary patients and this is often linked to underlying systemic diseases such as diabetes, inflammatory arthropathies, and/or prolonged use of medications (corticosteroids, quinolone antibiotics).4,5
Despite being a fairly common injury, which can be easily diagnosed clinically or via imaging modalities such as an ultrasound or magnetic resonance imaging (MRI), more than 1 in 5 cases are misdiagnosed, leading to the development of a chronic ATR.6 Whilst there are several definitions in the literature of a chronic ATR, a systematic review by Flint et al.7 suggested that any ATR diagnosed 4 weeks or more after the initial injury should be classed as being chronic.
Chronic ATRs often result in gait abnormalities due to the loss of push-off strength, which can negatively impact patients’ quality of life. Surgery forms the mainstay of treatment for the majority of patients due to unfavourable outcomes following non-operative management.8 Surgery involves debriding the scar tissue that forms a bridge between the 2 tendon edges, and reconstructing the Achilles tendon either through a primary repair, V–Y plasty, tendon transfer, interposition graft or using a combination of techniques. The surgical treatment choice is dictated by patient factors (graft availability, condition of the skin, medical co-morbidities), size of the residual gap following debridement of the fibrous scar tissue and surgeon preference.9, 10, 11 There are numerous studies in the literature that describe good outcomes following reconstruction of the Achilles tendon using various autografts either as tendon transfers or as interposition grafts. Unfortunately, most of these studies are case series with small sample sizes that often employ non-validated, subjective measures to assess patient outcomes post-operatively, making it difficult to truly assess the effectiveness of the surgical treatment described and apply the results of the general population.
The aim of this article was therefore to review the available literature for the four most commonly used autografts (either as tendon transfers or interposition grafts) in the surgical management of chronic ATRs. Particular emphasis was placed on the relevant clinical anatomy, techniques for safe harvesting and the advantages and disadvantages of each autograft option.
2. Methodology
Whilst not a systematic review, a thorough literature search was carried out of PubMed, Medline and Embase databases for papers written in English, on the surgical management of chronic Achilles tendon ruptures using autografts. Additionally, the authors also carried out cadaveric dissections of each of the 4 autograft options at the Keele Anatomy and Surgical Training Centre, Keele University. One matched pair of specimens (mid – thigh to foot) was used to perform the approaches necessary to harvest the tendons. Photographs taken at the time of dissection have been included in this review [Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5]. The cadaveric dissection was performed in line with the Human Tissue Act (2004) and the necessary ethics approval was sought through Keele University.
Fig. 1.
Dissected section of the Achilles tendon at its narrowest measuring 1.6 cm in width. The Achilles tendon is wider at its origin, and narrows distally, with the narrowest part of the tendon being approximately 80% down its length. The tendon widens again at its insertion. Majority of ATRs tend to occur at the narrowest portion of the tendon.
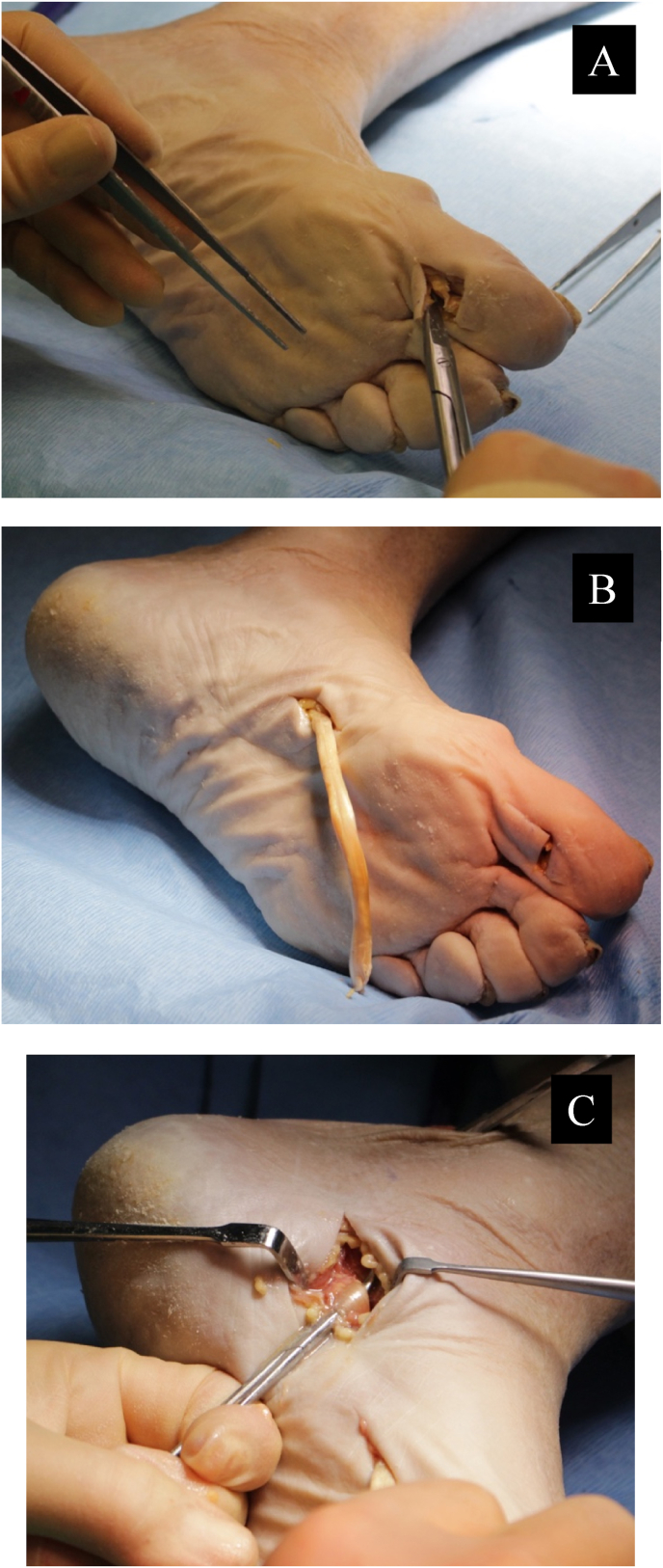
Fig. 2.
Harvesting options for flexor hallucis longus (FHL) in the same cadaver. A – FHL being harvested at the level of the interphalangeal joint of the hallux B – FHL at the level of the master knot of Henry. C – FHL harvested proximal to the master knot of Henry, at the level of the ankle joint.
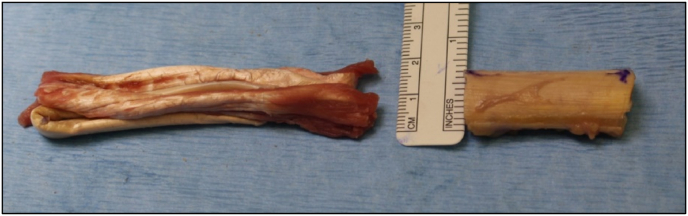
Fig. 3.
Triple folded peroneus brevis (PB) specimen [left] alongside a cut segment of the Achilles tendon [right] from the same cadaver, highlighting the anatomical differences between the 2 tendons.
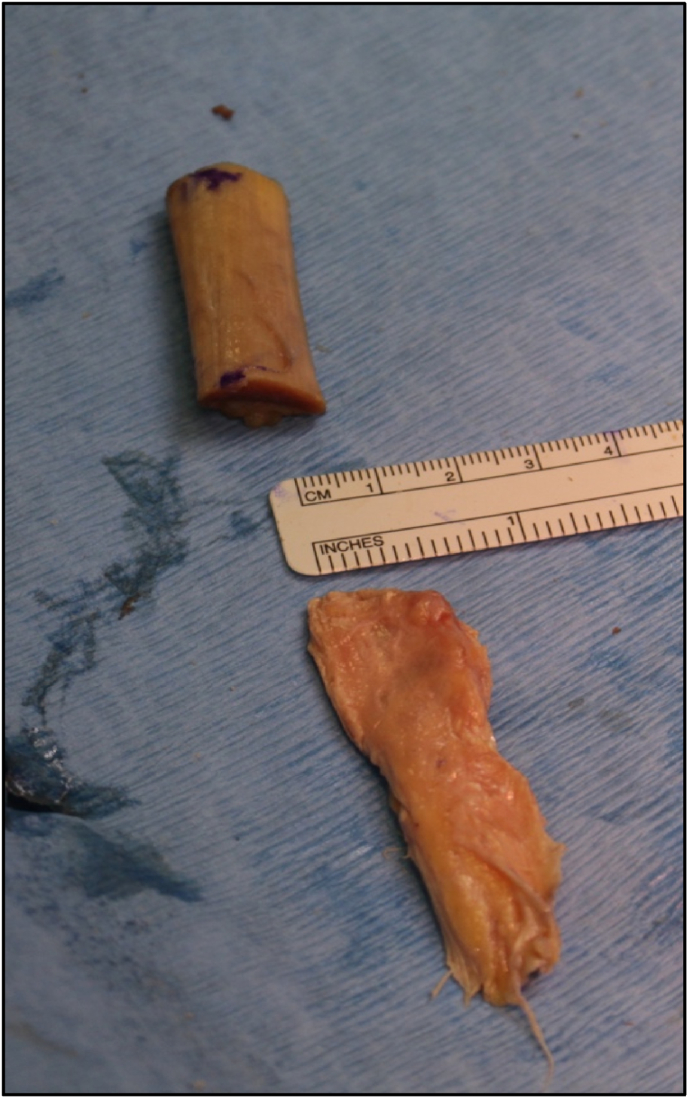
Fig. 4.
A transected segment of the Achilles tendon [left] with a quadrupled semitendinosus tendon (ST) on the right, from the same cadaver. Once the ST is quadrupled, its size and shape resemble that of the Achilles tendon, hence its popularity when it comes to choosing an autograft for reconstruction in chronic ATRs.
Fig. 5.
A transected segment of the Achilles tendon [top] with a harvested quadriceps tendon (QT) without the bone plug [bottom], from the same cadaver. Whilst the length and width of the QT is fairly similar to that of the cut Achilles tendon, the QT is a much thinner tendon compared to the Achilles. This difference in morphology may be one of the reasons why the QT is a less popular choice for surgical reconstruction of chronic ATRs.
3. Discussion
3.1. Achilles tendon anatomy
The Achilles tendon is formed by the confluence of the gastrocnemius and soleus muscles.12 There is significant variation in the anatomy of the Achilles tendon in adults, with the length, width and thickness dependent on patient characteristics such as height, sex and activity levels.13 However, on average, the Achilles tendon measures approximately 15 cm (range 11–26 cm) and is wider at its origin and insertion [Table 1].14 In our cadaver study, the narrowest portion of the Achilles tendon measured 1.6 cm [Fig. 1].
Table 1.
Average dimensions of the Achilles tendon and autograft options that are used either as tendon transfers or interposition grafts for reconstruction of chronic ATRs.
| Length | Width | |
|---|---|---|
| Achilles | 15 cm | 6.8 mm |
| Flexor hallucis longus | 10–12 cm | 5.1 mm |
| Peroneus brevis | 8 cm | 4.4 mm |
| Semitendinosus | 28 cm | 6 mm |
| Quadriceps | 8 cm | 2.7 cm |
As it inserts onto the calcaneal tuberosity, it forms a 90° spiral twist and has a periosteal extension into the plantar fascia.15 Microscopically, it is formed by fascicles containing fibrils which are covered in an endotenon, with an epitenon enveloping the entire tendon.16 Type 1 collagen fibres make up the majority of the tendon, and are arranged in a parallel fashion, with strong covalent bonds between them.17,18 This is probably why the Achilles tendon is considered to be one of the strongest tendons in the human body, being able to withstand large loads.19 The unique spiral twist and extension into the plantar fascia further help with dissipation of forces during the gait cycle.20
The tibial nerve supplies motor fibres to the gastrocnemius and soleus, giving off the sural nerve, which runs from the medial to the lateral side of the Achilles tendon, approximately 9–11 cm from the calcaneal tuberosity.16,21 The posterior tibial and peroneal arteries contribute to the anastomotic branches providing blood supply to the tendon.
3.2. Flexor hallucis longus (FHL) tendon transfer
The FHL tendon is the most commonly used autograft for the treatment of chronic ATRs.22 The muscle lies in the deep posterior compartment of the lower leg, and primarily causes flexion of the hallux. However, it also acts as a weak ankle plantarflexor. It originates from the posterior surface of the fibula and inserts onto the base of the distal phalanx of the big toe. As it courses distally, the FHL tendon crosses the flexor digitorum longus (FDL) tendon at the master knot of Henry.23 On average, the FHL tendon is approximately 10–12 cm long and 5.1 mm wide.24,25
Multiple techniques to harvest the FHL tendon are described in the literature, with the FHL tendon being harvested at the level of its insertion, at the master knot of Henry or proximal to the knot of Henry at the level of the ankle [Fig. 2]. All techniques require the patient to be in a prone or ‘floppy lateral’ position, which is ideal when it comes to accessing the Achilles tendon for the reconstruction in addition to autograft harvesting. A two – incision technique is most commonly used and is the authors preferred method of harvesting FHL, wherein a medial plantar incision is made to expose the long flexors at the master knot of Henry (harvesting at the IPJ is possible, but not common practice). The FHL is then detached as distally as possible, and brought through a proximal posteromedial incision, after which it is typically secured to the calcaneum with interference screws.26 In a single incision technique, the FHL is harvested through the same posteromedial incision through with the Achilles tendon edges are debrided. The drawback of this technique however, is that the harvested FHL is significantly shorter as compared to the two – incision technique due to the tendon being incised more proximally.27
The advantages of using FHL include its long tendon length (10–12 cm on average), anatomic proximity to the Achilles and ease of harvest, as well as the tendon being synergistically closely related to the Achilles tendon. Moreover, it is twice as powerful as the FDL and approximately 30% stronger than the peroneus brevis.25,28,29 A potential drawback of utilising the FHL though is the potential weakness of big toe flexion, which may have an impact during the push – off phase of the gait cycle.23 However, studies have shown that hallux flexion is maintained, especially if the FHL is harvested proximal to the master knot of Henry due to the forces being transferred from the FDL.30 Other potential complications include injury to the sural and medial plantar nerves during the FHL harvest [Table 2].28,29
Table 2.
The advantages and disadvantages of different autograft options for surgical treatment of chronic ATRs.
| Pros | Cons | |
|---|---|---|
| Flexor hallucis longus |
|
|
| Peroneus brevis |
|
|
| Semitendinosus |
|
|
| Quadriceps |
|
|
A systematic review of 8 studies which used FHL autografts for chronic ATRs showed that patient reported outcome measures (PROMs) improved significantly following surgery.22 Unfortunately, the studies failed to mention any effects on big toe function post-operatively. Overall, the FHL was felt to be a viable autograft option for surgical treatment of chronic ATRs with minimal donor site morbidity in comparison to other autografts.25
3.3. Peroneus brevis (PB) tendon transfer
The PB originates from the lateral fibular surface, runs in the lateral compartment of the lower leg anterior to the peroneus longus, and inserts onto the 5th metatarsal. It helps in eversion of the foot, providing medial-lateral stability and preventing uncontrolled ankle inversion.17,31 On average, the PB tendon was found to be 80 mm long and 4 mm wide [Fig. 3].32
The PB can be harvested from its insertion site with the patient either supine or prone. It is then passed proximally through an incision over the Achilles tendon and sutured to the 2 free Achilles tendon edges, forming a loop.33
Advantages of using PB include having a strong repair under physiological tension which helps maintain muscle power, thus promoting quicker recovery. It provides immobilisation in a plantigrade position, which minimises stiffness in a non-functional position, and permits early weight bearing, thus facilitating healing and minimising disuse atrophy or osteoporosis. Lastly, it avoids the potential risk of big toe flexion weakness which can occur with an FHL tendon transfer.34 Disadvantages of using the PB however are its smaller tendon length in comparison with the FHL and resultant weakness of foot eversion. Although biomechanically, the PB has a higher failure load than the FHL, this difference is not thought to be clinically relevant.35
Long term follow-up of patients who underwent PB tendon transfers for chronic ATRs demonstrated good functional outcomes.36 Studies have shown that patients undergoing this procedure have mild objective eversion weakness, however patients compensate well for this with no functional deficit found on subjective evaluation.33,34
3.4. Semitendinosis tendon (ST) interposition graft
Although commonly used for anterior cruciate ligament reconstruction, the ST can be used to reconstruct large ATR defects.37,38 It originates from the ischial tuberosity, inserts onto the pes anserine, with the tendon being approximately 28 cm long and 6 mm wide [Fig. 4].39
Patients need to be supine when harvesting the ipsilateral ST, as it can be quite challenging to harvest the tendon with the patient prone. An incision is made over the pes anserinus, and the ST cleared of any fascial attachments, following which a tendon stripper is utilised to release the ST from its proximal attachment. The patient then needs to be put in a prone position, and 2 incisions made – the first over the proximal Achilles tendon remnant to which the ST is sutured, and the second distally in order to suture the harvested tendon to the distal Achilles tendon remnant and secure it to the calcaneum, usually with an interference screw. Alternatively, the ST can be harvested through a small incision over the popliteal fossa, with the patient prone, although this technique is less commonly used.37
The main advantage of using the ST is its long length, which means it can be used to reconstruct very large Achilles tendon defects, whilst at the same time not compromising overall knee function. The disadvantages are mainly related to complications that can occur during tendon harvesting such as injuries to the underlying superficial medial collateral ligament, saphenous nerve, or premature graft amputation due to accessory insertions and fascial bands around the tendon.37
Good results have been reported in long term follow up studies of patients who have undergone chronic ATR reconstruction using the ST as an interposition graft, with the majority returning to their pre-injury activity levels, and only a few patients reporting temporary hamstring weakness or post-operative donor site pain.40 Conversely, Stenroos AJ et al.41 reported a high rate of complications such as infections in their patient cohort following ST autograft use for treatment of Achilles tendon ruptures, and therefore advised against its use. Interestingly however, the ST was used to augment acute primary repairs of the Achilles in the study rather than being used as an interposition graft for chronic ATRs, and therefore the results may not be applicable to patients with chronic ATRs.
3.5. Quadriceps tendon (QT) interposition graft
The QT is formed by the union of the rectus femoris, vastus intermedius, vastus medialis and vastus lateralis. It tends to be approximately 27 mm wide, and 8 mm thick, with the length varying between 74 and 81 mm, depending on the gender and height of the patient [Fig. 5].42
It can be harvested with the patient either supine or in a lateral position. An incision is made just medial to the superior pole of the patella, extending proximally for about 5 cm. Typically a 1 cm wide and 8 cm long strip of central tendon is obtained along with a 10–12 mm long bone plug. The thickest part of the QT is the medial aspect of the tendon, and the graft harvest should therefore deviate towards the medial half of the tendon. Following debridement of the bridging scar tissue and delineating the gap in the Achilles tendon, the QT is sutured to both ends of the remnant Achilles in a side-to-side fashion, and further secured by fitting the bone plug into a trough created in the calcaneum.43,44
The benefits of using the QT as an interposition graft is that the tendon itself is very strong, and the use of a bone plug has a higher reliability in terms of healing than using the tendon alone. Additionally, harvesting the QT results in minimal donor-site morbidity post-operatively.43 The downside is the potential risk of synovial fluid leakage if the suprapatellar pouch is violated during the tendon harvest which can result in scarring, thereby restricting knee movement. A meticulous, water-tight closure and early aggressive post-operative knee exercises can help to pre-empt this complication, whilst at the same time aiding in the return of quadriceps muscle strength. Unfortunately, the biggest drawback of the QT is the dependence on the distance of the Achilles tendon gap from the calcaneum. If it is more than 5–6 cm proximal from the calcaneum, the QT graft may be too short to bridge the gap, necessitating the use of a different graft.
There are only a few studies which have looked at using the QT as an interposition graft for chronic ATRs, and these have reported good morphological and functional outcomes in the short term.45,46 The lack of use of the QT is likely due to surgeon unfamiliarity with the QT harvesting technique, trying to avoid changing the position of the patient from a lateral/supine position to prone mid-way through surgery and the risk of the QT being of insufficient length.
4. Conclusion
Chronic ATRs can be quite challenging to treat. Multiple autograft options are available for surgical reconstruction of the Achilles tendon, each with their unique advantages and disadvantages. Majority of the studies looking at each autograft option have reported good post-operative outcomes and the superiority of one autograft tendon has not been proven over the others. Further work is needed to analyse the biomechanical properties of all autograft options compared to the Achilles tendon, as well as high quality cohort studies to determine if the use of one autograft option should be better than the rest.
Ethics
The cadaveric dissection was performed in line with the Human Tissue Act (2004) and necessary board approval was sought through Keele University.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or non-profit sectors.
Declaration of competing interest
None.
Acknowledgements
The authors would like to thank the staff at Keele anatomy and surgical training centre, Keele University, UK for their help with the cadaveric dissection. The authors would also like to thank Pip Divall for her help with the literature search.
References
- 1.Maffulli N., Waterston S.W., Squair J., Reaper J., Douglas A.S. Changing incidence of Achilles tendon rupture in Scotland: a 15 – year study. Clin J Sport Med. 1999;9(3):157–160. doi: 10.1097/00042752-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Leppilahti J., Puranen J., Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67(3):277–279. doi: 10.3109/17453679608994688. [DOI] [PubMed] [Google Scholar]
- 3.Ganestam A., Kallemose T., Troelsen A., Barfod K.W. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3730–3737. doi: 10.1007/s00167-015-3544-5. [DOI] [PubMed] [Google Scholar]
- 4.Maffulli N., Via A.G., Oliva F. Chronic Achilles tendon disorders: tendinopathy and chronic rupture. Clin Sports Med. 2015;34(4):607–624. doi: 10.1016/j.csm.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Shamrock A.G., Varacallo M. StatPearls publishing; 2022. Achilles Tendon Rupture. Treasure Island (Florida) [PubMed] [Google Scholar]
- 6.Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81(7):1019–1036. doi: 10.2106/00004623-199907000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Flint J.H., Wade A.M., Giuliani J., Rue J.-P. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42(1):235–241. doi: 10.1177/0363546513490656. [DOI] [PubMed] [Google Scholar]
- 8.Steginsky B.D., Van Dyke B., Berlet G.C. The missed Achilles tear: now what? Foot Ankle Clin. 2017 Dec;22(4):715–734. doi: 10.1016/j.fcl.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Myerson M.S., McGarvey W. Disorders of the Achilles tendon insertion and Achilles tendinitis. Instr Course Lect. 1999;48:211–218. [PubMed] [Google Scholar]
- 10.Maffulli N, Aicale R, Tarantino D. Autograft reconstruction for chronic Achilles tendon disorders. Tech Foot Ankle Surg. 16 (3): 117–123.
- 11.Kuwada G.T. Classification of tendo Achilles rupture with consideration of surgical repair techniques. J Foot Surg. 1990;29(4):361–365. [PubMed] [Google Scholar]
- 12.Apaydin N., Bozkurt M., Loukas M., Vefali H., Tubbs R.S., Esmer A.F. Relationships of the sural nerve with the calcaneal tendon: an anatomical study with surgical and clinical implications. Surg Radiol Anat. 2009;31(10):775–780. doi: 10.1007/s00276-009-0520-0. [DOI] [PubMed] [Google Scholar]
- 13.Patel N.N., Labib S.A. The Achilles tendon in healthy subjects: an anthropometric and ultrasound mapping study. J Foot Ankle Surg. 2018;57(2):285–288. doi: 10.1053/j.jfas.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Buono A.D., Chan O., Maffulli N. Achilles tendon: functional anatomy and novel emerging models of imaging classification. Int Orthop. 2013;37(4):715–721. doi: 10.1007/s00264-012-1743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snow S.W., Bohne W.H., DiCarlo E., Chang V.K. Anatomy of the Achilles tendon and plantar fascia in relation to the calcaneus in various age groups. Foot Ankle Int. 1995;16(7):418–421. doi: 10.1177/107110079501600707. [DOI] [PubMed] [Google Scholar]
- 16.Doral M.N., Alam M., Bozkurt M., et al. Functional anatomy of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2010;18(5):638–643. doi: 10.1007/s00167-010-1083-7. [DOI] [PubMed] [Google Scholar]
- 17.O'Brien M. Functional anatomy and physiology of tendons. Clin Sports Med. 1992;11(3):505–520. [PubMed] [Google Scholar]
- 18.Bailey A.J., Lapiere C.M. Effect of an additional peptide extension of the N-terminus of collagen from dermatosparactic calves on the cross – linking of the collagen fibres. Eur J Biochem. 1973;34(1):91–96. doi: 10.1111/j.1432-1033.1973.tb02732.x. [DOI] [PubMed] [Google Scholar]
- 19.Smart G.W., Taunton J.E., Clement D.B. Achilles tendon disorders in runners – a review. Med Sci Sports Exerc. 1980;12(4):231–243. [PubMed] [Google Scholar]
- 20.Alexander R.M., Bennet-Clark H.C. Storage of elastic strain energy in muscle and other tissues. Nature. 1977;265(5590):114–117. doi: 10.1038/265114a0. [DOI] [PubMed] [Google Scholar]
- 21.Webb J., Moorjani N., Radford M. Anatomy of the sural nerve and its relation to the Achilles tendon. Foot Ankle Int. 2000;21(6):475–477. doi: 10.1177/107110070002100604. [DOI] [PubMed] [Google Scholar]
- 22.Arshad Z., Lau E.J.S., Leow S.H., Bhatia M. Management of chronic Achilles ruptures: a scoping review. Int Orthop. 2021;45(10):2543–2559. doi: 10.1007/s00264-021-05102-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas D., Thordarson D., Nelson T.J., Charlton T.P., Eberlein S., Metzger M.F. Knot of Henry variation and the effect on plantar flexion strength. Foot Ankle Int. 2020;41(1):94–100. doi: 10.1177/1071100719875229. [DOI] [PubMed] [Google Scholar]
- 24.Seybold J.D., Campbell J.T., Jeng C.L., Myerson M.S. Anatomic comparison of lateral transfer of the long flexors for concomitant peroneal tears. Foot Ankle Int. 2013;34(12):1718–1723. doi: 10.1177/1071100713503817. [DOI] [PubMed] [Google Scholar]
- 25.Ozer H., Ergisi Y., Harput G., Senol M.S., Baltaci G. Short-term results of flexor hallucis longus transfer in delayed and neglected Achilles tendon repair. J Foot Ankle Surg. 2018;57(5):1042–1047. doi: 10.1053/j.jfas.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Abubeih H., Khaled M., Saleh W.R., Said G.Z. Flexor hallucis longus transfer clinical outcome through a single incision for chronic Achilles tendon rupture. Int Orthop. 2018;42(11):2699–2704. doi: 10.1007/s00264-018-3976-x. [DOI] [PubMed] [Google Scholar]
- 27.Mao H., Shi Z., Wapner K.L., Dong W., Yin W., Xu D. Anatomical study for flexor hallucis longus tendon transfer in treatment of Achilles tendinopathy. Surg Radiol Anat. 2015;37(6):639–647. doi: 10.1007/s00276-014-1399-y. [DOI] [PubMed] [Google Scholar]
- 28.Lehnert B., Nyska M., Ip W., Huynh E., Palmanovich E. Flexor digitorum longus (FDL) or flexor hallucis longus (FHL) harvesting: technical tip and case studies. Foot Ankle Int. 2017;38(11):1267–1270. doi: 10.1177/1071100717722365. [DOI] [PubMed] [Google Scholar]
- 29.Mahajan R.H., Dalal R.B. Flexor hallucis longus tendon transfer for reconstruction of chronically ruptures Achilles tendons. J Orthop Surg. 2009;17(2):194–198. doi: 10.1177/230949900901700215. [DOI] [PubMed] [Google Scholar]
- 30.Richardson D.R., Willers J., Cohen B.E., Davis W.H., Jones C.P., Anderson R.B. Evaluation of the hallux morbidity of single incision flexor hallucis longus tendon transfer. Foot Ankle Int. 2009;30(7):627–630. doi: 10.3113/FAI.2009.0627. [DOI] [PubMed] [Google Scholar]
- 31.Willegger M., Benca E., Hirtler L., et al. Peroneus brevis as source of instability in Jones fracture fixation. Int Orthop. 2020;44(7):1409–1416. doi: 10.1007/s00264-020-04581-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Imre N., Kocabiyik N., Sanal H.T., Uysal M., Ozan H., Yazar F. The peroneus brevis tendon at its insertion site on fifth metatarsal bone. Foot Ankle Surg. 2016;22(1):41–45. doi: 10.1016/j.fas.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 33.Maffulli N., Via A.G., Oliva F. Chronic Achilles tendon rupture. Open Orthop J. 2017;11:660–669. doi: 10.2174/1874325001711010660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gallant G.G., Massie C., Turco V.J. Assessment of eversion and plantar flexion strength after repair of Achilles tendon rupture using peroneus brevis tendon transfer. Am J Orthoped. 1995;24(3):257–261. [PubMed] [Google Scholar]
- 35.Sebastian H., Datta B., Maffulli N., Neil M., Walsh R. Mechanical properties of reconstructed Achilles tendon with transfer of peroneus brevis or flexor hallucis longus tendon. J Foot Ankle Surg. 2007;46(6):424–428. doi: 10.1053/j.jfas.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 36.Maffulli N., Spiezia F., Pintore E., et al. Peroneus brevis tendon transfer for reconstruction of chronic tears of the Achilles tendon: a long-term follow-up study. J Bone Joint Surg Am. 2012;94(10):901–905. doi: 10.2106/JBJS.K.00200. [DOI] [PubMed] [Google Scholar]
- 37.Maffulli N., Longo U.G., Spiezia F., Denaro V. Free hamstrings tendon transfer and interference screw fixation for less invasive reconstruction of chronic avulsions of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):269–273. doi: 10.1007/s00167-009-0968-9. [DOI] [PubMed] [Google Scholar]
- 38.Patil S.S.D., Patil V.S.D., Basa V.R., Dombale A.B. Semitendinosis tendon autograft for reconstruction of large defects in chronic Achilles tendon ruptures. Foot Ankle Int. 2014;35(7):699–705. doi: 10.1177/1071100714531228. [DOI] [PubMed] [Google Scholar]
- 39.Mishra P., Ajay, Goyal A., Mehta N., Lal H., Kumar S. Comparison of semitendinosus tendon length and diameter in sports and non-sports group for ACL reconstruction. J Clin Orthop Trauma. 2020;11(Suppl 5):S795–S798. doi: 10.1016/j.jcot.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maffulli N., Buono A.D., Spiezia F., Maffulli G.D., Longo U.G., Denaro V. Less – invasive semitendinosus tendon graft augmentation for the reconstruction of chronic tears of the Achille tendon. Am J Sports Med. 2013;41(4):865–871. doi: 10.1177/0363546512473819. [DOI] [PubMed] [Google Scholar]
- 41.Stenroos A.J., Brinck T. Achilles tendon reconstruction with semitendinous tendon grafts is associated with a high complication rate. J Am Podiatr Med Assoc. 2020;110(2) doi: 10.7547/18-014. doi: 10.7547/18-014. [DOI] [PubMed] [Google Scholar]
- 42.Shelton W. 2. Elsevier; 2018. The Case for Quadriceps Autograft : The Anterior Cruciate Ligament Reconstruction and Basic Science. [Google Scholar]
- 43.Arriaza R., Gayoso R., Lopez-Vidriero E., Aizpurua J., Agrasar C. Quadriceps autograft to treat Achilles chronic tears: a simple surgical technique. BMC Muscoskel Disord. 2016;17:116. doi: 10.1186/s12891-016-0967-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Noyes F.R., Barber-Westin S.D. Posterior cruciate ligament injuries : noyes' knee disorders – surgery, rehabilitation, clinical outcomes. Elsevier. 2017 [Google Scholar]
- 45.Besse J.L., Lerat J.L., Moyen B., Vincent P., Brunet-Guedj E. Distal reconstruction of the Achilles tendon with a bone-tendon graft from extensor system of the knee. Rev Chir Orthop Reparatric Appar Mot. 1995;81(5):453–457. [PubMed] [Google Scholar]
- 46.Mudgal C.S., Martin T.L., Wilson M.G. Reconstruction of Achilles tendon defect with a free quadriceps bone – tendon graft without anastomosis. Foot Ankle Int. 2000;21(1):10–13. doi: 10.1177/107110070002100102. [DOI] [PubMed] [Google Scholar]