Abstract
Sexual violence can have an overwhelming impact on the victim’s physical and mental health; the consequences include unintended pregnancy and sexually transmitted infections (STIs). Therefore, the examiners must assess victims for possible pregnancy and sexually transmitted infections as a part of the sexual assault examination. This article aims to orient the medico-legal examiners towards their role in preventing unintended pregnancy and sexually transmitted infections among victims of sexual assault. Prompt detection of pregnancy or STIs is critical, as any delay would adversely affect the successful administration of emergency contraception and post-exposure prophylaxis (PEP) against human immunodeficiency virus (HIV) and other sexually transmitted infections.
Keywords: Contraception, Crime victims, Forensic nursing, Forensic sciences, Post-exposure prophylaxis, Pregnancy, Preventive health service, Sex offences, Sexually transmitted diseases
Background
The overwhelming effect of sexual assaults (SA) is short, but the long-term physical and psychological consequences can be more deleterious. These consequences include pregnancy, sexually transmitted infections (STIs), and reproductive tract infections [1, 2]. Therefore, the medico-legal professionals attending to female sexual assault victims (SAVs) must assess for the possibility of pregnancy and STIs as a part of the sexual assault examination [3]. The examination and subsequent medical support should include assessing the victim for pregnancy and STIs, care for victims, informed consent for treatment, emergency contraception, follow-up care, etc. [4–6]. It is also mandatory that an experienced clinician conducts the examinations of survivors of sexual assault in a way that minimises further trauma.
Unintended pregnancy as a consequence of sexual assault has dire impacts on the health and socioeconomic well-being of the victims and their loved ones. Although the risk of conception after an unprotected sexual encounter (UPSE) may be low and is based on several factors [7], the socioeconomic impact of rape-related pregnancy (RRP) could be devastating. Therefore, RRP is considered a public health concern that adds to the adverse outcomes of sexual assaults [8] and, therefore, needs to be assessed at the earliest with appropriate measures taken for prevention. Furthermore, unintended pregnancy is the main reason for abortions [9], which may again add to the adverse outcomes of RRP. STIs are another significant consequence of sexual assault [10, 11]. Therefore, SAVs need multidisciplinary care, which include assessing and managing STIs [12, 13]. Even the presence of STIs and the isolation of the causative organisms are strong indicators of child sexual abuse [14]. STIs are generally caused by bacteria, viruses, protozoa, and fungi and can be transmitted through body fluids or by direct contact with the skin.
Assessing for pregnancy and STIs is very critical as any delay in the diagnosis would affect the successful administration of emergency contraceptives (EC) and post-exposure prophylaxis (PEP) against HIV and other STIs [15]. Therefore, this paper aims to orient medico-legal professionals about their role in preventing and managing pregnancy and STIs among the SAVs.
Main text
I. Prophylaxis against pregnancy
Probability of pregnancy: considerations
The probability of getting pregnant after sexual assault is dependent upon various factors, some of which are discussed below.
The type of sexual assault
Contact of seminal fluid with the vagina of the victim poses a high risk of pregnancy. The unprotected vaginal penetration by the penis is always on top of the list. Sodomy will also become a risk if the seminal fluid flows from the anus to the vagina. An additional case that needs to be considered is the perpetrator ejaculating near the vagina.
The victim’s menstrual cycle and the life span of the ovum and sperm
The exact duration of the menstrual cycle varies for each woman. The average menstrual cycle is considered to be 28 days. In some cases, menstrual cycles can be shorter than 21 days or longer than 41 days, during which the period can be regular and normal. Ovulation occurs approximately on the 14th day of the menstrual cycle. The life span of an ovum is about 24–48 h, whereas the life span of sperm is about 4–5 days. These gamete characteristics mean that the highest risk of conception following a single UPSE is from days 9–16 of the menstrual cycle (4.9 to 9.7%) [16]. Li, Wilcox, and Dunson (2015) also estimate that the risk of pregnancy after a single UPSE, irrespective of the day of the menstrual cycle, is about 9.7%. They further observed that the highest probability of pregnancy was on the 13th day of the menstrual cycle. The probability of becoming pregnant is nearly zero (0.001–0.002) in the initial 3 days of the menstrual cycle. Women with irregular menstruation have a higher probability of getting pregnant in the latter part of the cycle.
Use of condoms by the perpetrator
A study conducted by O'Neal et al. found that only 11.7 to 15.6% of perpetrators use condoms [17]. Not using a condom, any damage to the condom, or the condom slipping off during the assault increases the risk of pregnancy.
Use of contraceptive methods by the victim/perpetrator
-
Sterilisation and long-acting reversible contraception (LARC)
LARC methods provide birth control measures for both the perpetrator and the victim. This includes vasectomy for the perpetrator and a variety of methods such as tubectomy, hysterectomy, Nexplanon, progesterone-based intrauterine devices (IUDs), copper IUDs, and non-hormonal IUDs for the victim. The rate of pregnancies after using LARC is lower when compared with oral contraceptives. However, tubal ligation had demonstrated a failure rate of 2.6 per 100 women [18].
-
Combined oral contraceptive pills, progesterone pills, and depot preparations (shots)
Oral contraceptive pills contain either progestin or a combination of oestrogen and progestin. The combination of oestrogen and progestin inhibits the release of luteinising hormones and follicle-stimulating hormones from the pituitary gland. Progestin inhibits ovulation and changes the mucus surrounding the ovum, making it difficult for sperm to penetrate. The circulating serum levels of exogenous oestrogen or progesterone that interfere with their action at a cellular level determine the efficacy of oral contraceptives. Inadvertent pregnancies (6–9%) are not uncommon in combined pill users and are usually due to poor compliance [19, 20].
-
Condom for men and women
The pregnancy rate among men or women who used condoms is 13–21% [21].
Perimenopausal women
Perimenopause is the time around menopause, starting a few years before menopause and ending 12 months after the last menses. As a result, the pregnancy rate is considerably low, although perimenopausal women can also become pregnant [22, 23].
Special population (transgender men)
Transgender men (female to male) also risk pregnancy with unprotected sexual intercourse if they do have not had a sterilisation procedure or achieved menopause [24].
The use of emergency contraception
Pregnancy associated with sexual assault can be prevented using emergency contraception (EC). It can prevent over 95% when taken within 5 days after the unprotected sexual encounter. However, emergency contraceptives should be taken only in cases of emergency and not as an alternative to regular contraception. The most effective method is a copper intrauterine device (Cu-IUD), which can be left in place as ongoing contraception afterwards. Selective progesterone receptor modulators such as ulipristal acetate are among the most effective emergency contraceptive pills (ECPs) available [25]. ECPs containing levonorgestrel are another method of EC. The details of the ECs are mentioned in Table 1.
Table 1.
Emergency contraceptive methods and their action, failure rate, the window of efficacy, and advantages
| Emergency contraceptive method and dose | Mechanism of action | Failure rate (occurrence of pregnancy after the use of EC) | The window of efficacy after an unprotected sexual encounter (UPSE) | Advantages over other ECs |
|---|---|---|---|---|
| Copper IUD |
• The toxic effect on sperm and ova • Harmfully affect motility and viability of sperm • Adversely affect viability and transportation of ova • It prevents implementation by a local endometrial inflammatory reaction |
< 1% | It can be inserted within 5 days after the UPSE in a cycle or within 5 days of the earliest estimated date of ovulation, whichever is later |
• Copper IUD is the only method that is effective after the starting of ovulation • Copper IUD is not affected by BMI of the individual or action of any drugs |
| ECPs containing ulipristal acetate (30 mg single oral dose) | • Delays ovulation for at least 5 days until sperm from the UPSE is no longer viable (It delays ovulation even after the start of the luteinising hormone (LH) surge) |
1.3–2.1% Fine et al. [52] |
Within 3–5 days after UPSE Glasier et al. [53] |
• UPA–ECP is the only oral EC that is expected to be effective if UPSE took place 96–120 h ago (LNG-ECP is ineffective if taken more than 96 h after UPSE) |
|
ECPs containing Levonorgestrel (LNG) (1.5 mg single oral dose or 3 mg when the woman is taking the enzyme-inducing drug or has a BMI of more than 26 kg/m2) |
• If taken before the start of the LH surge, it delays or prevents follicular rupture and causes luteal dysfunction • Delays ovulation for at least 5 days until sperm from the UPSE is no longer viable |
0.6–2.6% | Within 72 h after UPSE | • LNG-ECP is effective even if a woman has recently taken progestogen (The effectiveness of UPA-EC could theoretically be reduced in this case) |
Follow-up care and diagnosis of pregnancy
In cases of sexual assault, a follow-up visit to a healthcare facility is essential. A visit within 2 to 4 weeks after the initial examination can help the victim be tested for possible pregnancy and get early termination of the pregnancy if needed. A blood and/or urine sample analysis is required for pregnancy testing. A pregnancy test within 5 days after sexual assault may show positive but does not necessarily indicate that the victim became pregnant because of assault.
The accuracy of different pregnancy tests varies depending on the assay method, the specimen, and the date of specimen collection. The freely available urine beta-hCG strip method is a point of care testing (POCT) device based on lateral-flow immunochromatography. It qualitatively detects the presence of beta-hCG in urine specimens at 20 mIU/mL sensitivity in most cases [26]. It should be noted that false-negative pregnancy results may occur in very high urine beta-hCG concentration due to the ‘high-dose hook effect’ with the assay method, which can be overcome by testing diluted urine [27]. The serum beta-hCG analysis is a quantitative immunoassay method with 97% and 100% specificity [28].
Medical termination of pregnancy (MTP)
SAVs with unwanted pregnancies may choose to have induced abortions. The principal determinants of the safety of induced abortions are the gestational age at abortion and the method used. The earlier the MTP is performed, the safer the procedure is. The lowest risk is when the procedure is performed 7–10 weeks after the last menstrual period. Induced abortions are restricted by law in a few regions of the world, while safe abortion techniques are legalised and practised in most countries [29]. The legalisation of abortions reduces the chances of illegal and unsafe practices. For example, the Government of India amended the Medical Termination of Pregnancy Act, 1971 [30] and established rules giving power to the medical board to allow or deny termination of pregnancy beyond 24 weeks of the gestation period. Medical termination of pregnancy can be attained by administering mifepristone combined with a suitable prostaglandin, such as misoprostol or a prostaglandin analogue [31]. If the products of conception remain within the uterus, a manual vacuum aspiration can be conducted under local anaesthesia on the cervix head. Intrauterine injection of hypertonic solutions, such as saline or urea, augmented by oxytocin, prostaglandin, laminaria, or some combination of these can also be used for MTP. The other methods of MTPs are extra-amniotic injections of ethacridine lactate and surgical procedures such as dilatation and evacuation (D&E).
Pre- and post-procedure counselling in cases of MTPs
Counselling is a continuous, structured, and systematic interaction in which an individual voluntarily receives emotional support and guidance from a competent person in an environment that is helpful for to open sharing of thoughts that influences health and well-being [32]. The main focus of counselling before and after a medical termination of pregnancy is to reduce the stigma around the issue by normalising it. An adolescent who has an unwanted pregnancy or an STI may feel embarrassed or ashamed. Therefore, it is essential that counsellors actively minimise the stigma associated with the issue by stating to the victim, ‘I have treated several people with the same problem you have’ [31, 33].
Medico-legal aspects of MTPs
Globally, the legality of abortion can be grouped into five categories.
All types of abortions are prohibited or illegal.
Unlawful abortions are prohibited and penalised, but no additional information on lawful abortions.
Allows or permits abortion only on one or more legal grounds.
Entitles a woman for abortion on request with no requirement for justification.
Abortion is regulated only as a health intervention in the health system [29].
Abortion laws and policies vary across countries and regional jurisdictions. On a global scale, the World Health Organization has laid out specific standard for abortions [29, 32, 33]. These guidelines recommend that MTP be performed by a specialised doctor with postgraduate clinical training and a specialisation in obstetrics and gynaecology and reiterate the need to obtain consent from the individual undergoing MTP. Additionally, it is a best practice to ensure the presence of a female health care professional during the examination and the MTP procedure.
Aborted foetal material (abortus evidence)
Abortus will be assessed to identify the biological parents using deoxyribonucleic acid (DNA) typing after the voluntary interruption of pregnancy [34–36]. The aborted material consists of the placenta, which contains maternal and foetal sections. The foetal DNA will be isolated from the aborted material and a foetal profile will be obtained through repeated sampling. Chorionic villi samples usually give a ‘clean’ or ‘nearly clean’ foetal DNA profile without maternal DNA contamination. However, excess maternal DNA can hinder the detection of foetal genotypes [36
II. Prophylaxis against sexually transmitted infections
Factors affecting STI risk
The actual risk of contracting STIs depend on many factors like the prevalence of STIs in the population, the type of sexual activity performed, the use of condoms, the level of immunity, and the rate of serial monogamy in society. STIs are common in young individuals due to the presence of columnar epithelium on the ectocervix (cervical ectropion) [37]. Condoms may help in preventing STIs which are transmitted through seminal or vaginal fluids (chlamydia and gonorrhoea), but are less effective in preventing STIs that are transmitted through sores or cuts on the skin (genital herpes, syphilis, and human papillomavirus).
Barriers to assessing STI risk
Individuals may be afraid to be tested for STIs to avoid revealing pre-existing infection and previous sexual activities. The prior use of antibiotics (prescribed either for any other condition or over-the-counter medication) can also mask any STIs that may be present otherwise. Underestimating the risk of STIs is also another barrier effectively assessing STI risk [38].
Types of STIs
More than 30 different infectious agents are known to cause STIs. Out of these, eight pathogens cause major STIs. These include curable infections such as syphilis, gonorrhoea, chlamydia, and trichomoniasis, as well as incurable infections such as hepatitis B, herpes simplex virus (HSV), human immunodeficiency virus (HIV), and human papilloma virus (HPV). Globally, more than a million cases of STIs are reported daily. In 2020 alone, the WHO estimated 374 million new cases of curable STI around the globe, with chlamydia being the highest, amounting to 129 million cases, followed by gonorrhoea (82 million), syphilis (7.1 million), and trichomoniasis (156 million) [39–41]. The details of curable STIs are mentioned in Table 2.
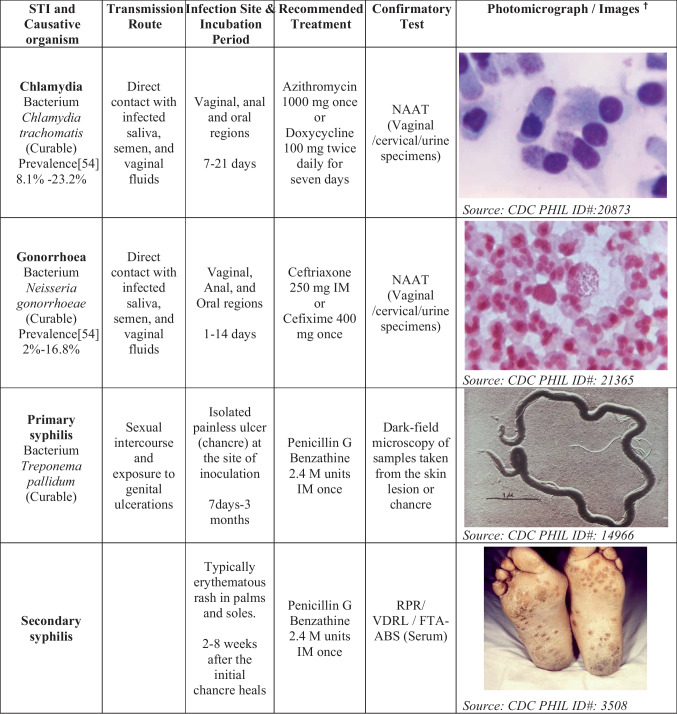
Chlamydia
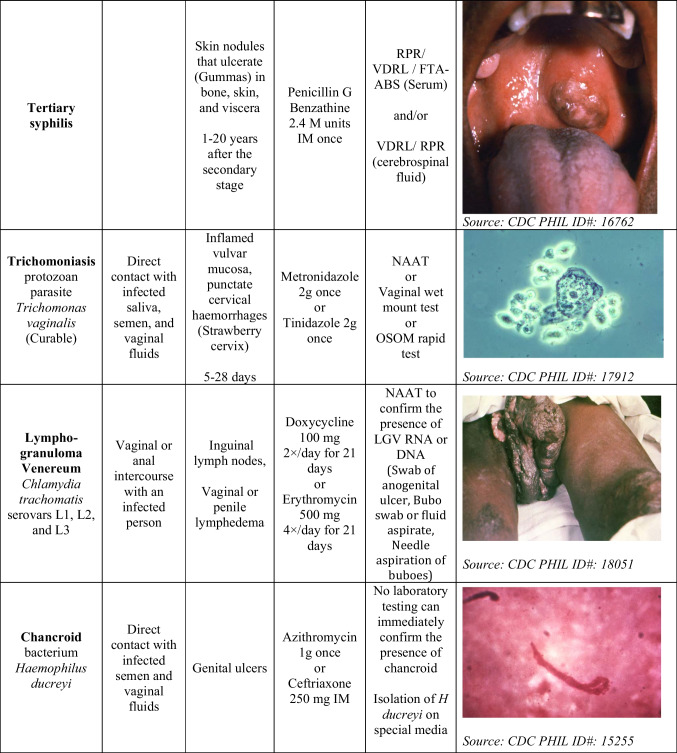
Table 2.
STIs and their transmission route, infections site, incubation period, recommended treatment, confirmatory test, and images
M units—million units, IM- intramuscularly
† Photos adopted from Public Health Image Library (PHIL) maintained by CDC
Globally, chlamydia is the most prevalent bacterial STI [41]. The infection can be asymptomatic or show various symptoms, such as pelvic pain, rectal pain, dysuria, vaginal discharge, and a sore throat [39]. The severity of the symptoms is usually subjective to the level of infection and the route of exposure. These asymptomatic infections can be spread inadvertently by the infected person to others [13].
-
(b)
Gonorrhoea
Gonorrhoea also remains a major global public health concern. Patients with gonorrhoea can be asymptomatic or present with localised infection, showing symptoms such as pelvic pain or rectal pain, joint pain, penile or vaginal discharge, or sore throat [39].
-
(iii)
Syphilis
Treponema pallidum is a spirochete responsible for syphilis, which spreads from individual to individual by direct contact with genital ulcerations or through sore (chancre). These sores can occur in, on, or around the vagina, penis, rectum, anus, and mouth or lips. Syphilis can spread during oral, anal, or vaginal intercourse with an infected person.
-
(iv)
Trichomonas
Trichomonas is the most widespread protozoan STI caused by trichomonas vaginalis. The initial symptoms start within 3–28 days. For a few women, the infection may be asymptomatic. Epididymitis urethritis and prostatitis are the common symptoms present in men, whereas women may show vaginal discharge, dysuria, or vulval irritation. Women may also have vulvar erythema and punctate cervical haemorrhages, described as a ‘strawberry cervix’.
-
(e)
Human immunodeficiency virus (HIV)
HIV is a viral infection caused by an enveloped ribonucleic acid (RNA) virus that may be passed through sexual contact and sharing syringes and/or sharing needles with an infected person. Various factors increase the risk of transmitting HIV including bite injuries caused by the offenders, multiple offenders, anal and vaginal penetration, occurrence of genital trauma, anal or vaginal tear, the presence of sperm or semen in/around the genital area, and the offender(s) being injection drug user(s).
-
(f)
Hepatitis B virus (HBV)
HBV is a hepatotropic virus transmitted through the serum, semen, and vaginal fluids [42]. HBV is 50 to 100 times more virulent than HIV and can cause severe liver diseases, including acute and chronic hepatitis, cirrhosis, and hepatocellular carcinoma [43].
Prevention counselling
Counselling related to STIs, especially symptoms, treatment options, and care after discharge from the hospital, is essential. The risk associated with STI exposure and the potential risk of transferring to future or current consensual partners also needs to be discussed with the SAVs. High psychological distress can be alleviated by giving proper information about the follow-up assessment and care [44].
Screening for STI
STI screening is advised between 3 and 7 days and 2 weeks after the assault (as dictated by incubation periods of Neisseria gonorrhoeae and Chlamydia trachomatis) or later if prophylactic antibiotics have been taken.
Protocol for testing
Nucleic acid amplification test (NAAT)
Neisseria gonorrhoeae and Chlamydia trachomatis can cause asymptomatic infections and the diagnosis based on the symptoms alone is not an effective approach to treatment. In contrast, NAAT can be adopted for a more accurate diagnosis. The sample can be collected from urine in both sexes or by swabbing the vagina or cervix in women. Pharyngeal or rectal swabs can also be considered depending on the case [45]. NAAT is extremely sensitive and specific for diagnosing the existence of Chlamydia trachomatis (sensitivity: 97.5–98.5 and specificity: 98.4–99.4) and Neisseria gonorrhoeae (sensitivity: 98.0–98.5 and specificity: 99.6–99.8) [46].
-
(b)
Cervical cytology
In a conventional cervical cytological test, the sample is spread on a thin film over a small area onto a dry slide and examined under the microscope. This test is typically conducted 10–20 days after the last menstrual periods, whereas a liquid-based cytology can be executed at any time during the menstrual cycle. Some women may present a mucopurulent discharge and the test can be done after clearing the discharge with a cotton swab soaked with saline. Using a cytobrush to sample the cervical transformation zone improves the accuracy of the cytological test [40].
-
(iii)
Dark-field microscopy
Dark-field microscopy is a sensitive and specific imaging technique for demonstrating T. pallidum by creating a contrast between the object and the adjacent field so that the background is dark and the object is bright. It is the most specific and sensitive technique to diagnose syphilis when an active chancre or condyloma lata is present, as it allows for a presumptive diagnosis of syphilis even before the development of antibodies. Thus, a dark-field microscopy has the advantage of detecting infection early and on-site, which helps in early identification and treatment, which indirectly helps in containing the spread of infection [47, 48].
-
(iv)
Serological testing
HIV, HBV, and syphilis infections can be detected using serological testing by analysing the presence of antibodies (Ab) or antigens (Ag). An antigen or antibody test can usually detect HIV infection between 18 and 45 days after exposure, whereas a NAAT can usually detect an HIV infection between 10 and 33 days after exposure. The hepatitis B surface antigen (HBsAg) is the first serologic marker appearing in the serum between 6 and 16 weeks following exposure to the HBV, which can be used for the diagnosis of HBV infection. If HBsAg and anti-HBc (hepatitis B core Ab) are present in the absence of IgM anti-HBc, this can be used to diagnose a chronic HBV infection. Screening for syphilis can be done by detecting Abs against T. pallidum using the venereal disease research laboratory (VDRL) test and can be confirmed by Treponema pallidum particle agglutination assay (TP-PA).
Empiric antimicrobial regimen for bacterial STIs
The Center for Disease Control and Prevention (CDC) recommends a single dose of Ceftriaxone 500 mg/IM (if weight weighing ≥ 150 kg, 1 g of Ceftriaxone) with doxycycline 100 mg two times a day orally and metronidazole 500 mg two times a day orally for 7 days as empiric antibiotics for sexually transmitted bacterial infections [40]. However, the efficacy of these regimens in preventing infections after a sexual assault has not been evaluated. Therefore, if the victim requires specific treatment, the organism needs to be identified.
Non-occupational post-exposure prophylaxis (PEP) against HIV
Prevention of HIV infection after a possible exposure can be achieved by administering antiretroviral therapy (ART) within 72 h (3 days). PEP should be used only in emergencies and not meant for regular use [49]. The PEP should be given to SAVs who are HIV negative or do not know their status. The effectiveness of the regimen is higher when administered early after the potential exposure. A rapid fourth-generation HIV testing preferably needs to be done before the initiation of PEP and a negative result requires immediate starting of PEP. If such fourth-generation tests are not available, then PEP can be started and the samples can be sent to labs for confirmation. Upon a positive result, the PEP regimen is stopped, starting of therapeutic regimen [49–51], The PEP regimen and alternative treatment regimen recommended by CDC are given in Table 3.
Table 3.
PEP regimen and alternative treatment regimen recommended by CDC
| Population | PEP regimen(preferred) | Alternative regimen |
|---|---|---|
| Adults and adolescents (≥ 13 years) with normal renal function (Cr CL ≥ 60 mL/min) |
Tenofovir disoproxil fumarate 300 mg once daily or emtricitabine 200 mg once daily + Dolutegravir 50 mg once daily or Raltegravir 400 mg twice daily |
Tenofovir disoproxil fumarate 300 mg once daily or emtricitabine 200 mg once daily + Darunavir 800 mg (as two, 400-mg tablets) once daily and ritonavirb 100 mg once daily |
| Adults and adolescents (≥ 13 years) with renal dysfunction (Cr CL ≤ 59 mL/min) |
Zidovudine and Lamivudine, with both doses adjusted to degree of renal function + Raltegravir 400 mg twice daily + Dolutegravir 50 mg once daily or Raltegravir 400 mg twice daily |
Zidovudine and Lamivudine, with both doses adjusted to degree of renal function + Darunavir 800 mg (as two 400-mg tablets) once daily + Ritonavirb 100 mg once daily |
| Children aged 2–12 years | Tenofovir DF, emtricitabine, and Raltegravir, with each drug dosed to age and weight |
Zidovudine and Lamivudine + Raltegravir or lopinavir/ritonavir + Raltegravir (lopinavir/ritonavir dosed to age and weight) |
Cr CL, creatinine clearance
Risk assessment for PEP
There is substantial risk for HIV acquisition when SAVs had exposure to semen, rectal secretions, vaginal secretions, breast milk, blood, or any body fluids that are visibly contaminated with blood on the non-intact skin, mouth, eye, vagina, penis, rectum, or another mucous membrane, or percutaneous contact from a known source of HIV.
There is negligible risk for HIV acquisition when SAVs had exposure to urine, nasal secretions, saliva, sweat, tears without any visible blood on the non-intact skin, mouth, eye, vagina, penis, rectum, or another mucous membrane, or percutaneous contact from a from a known or suspected source of HIV.
A PEP regimen needs to be started if there are signs of substantial risk, provided such exposures occur within 72 h [49, 50].
PEP regimen (CDC)
A 28-day course of PEP is recommended for HIV-uninfected persons who have a substantial risk for HIV acquisition within 72 h [50].
Prophylaxis against hepatitis B
SAVs who are not previously vaccinated or partially vaccinated need to administer a single dose of the hepatitis B vaccine. If the perpetrator is available for examination and found to be HBsAg positive, then the SAV who was not vaccinated prior should receive the hepatitis B vaccine and hepatitis B immunoglobulin during the initial medico-legal assessment. Follow-up vaccines should be administered during 1–2 months and 4–6 months after the initial dose. If the SAV has been vaccinated before, then a single booster dose of the hepatitis B vaccine needs to be administered [40, 50].
Prophylaxis against human papilloma virus
The HPV vaccine can be administered to SAVs (9–21 years for males and 9–26 years for females) at the time of the initial medico-legal examination and two follow-up doses need to be administered 1–2 months and 6 months after the first dose [40].
Counselling for individuals taking PEP
The counselling sessions should primarily focus on coping strategies for the victimised individual. Motivational interviewing and training of adaptive coping skills can be considered part of the counselling sessions. PEP can reduce the risk of infection, but it is not always effective. Counselling also needs to focus on the protective behaviour of the individuals with their sex partners. Adherence counselling can also separately be provided to the individuals [49, 50].
Conclusion
SAVs have a higher risk of becoming pregnant and acquiring STIs, which can cause a severe impact on their physiological, psychological, and social functioning. Consequently, it also affects their sense of self, health, and well-being. Thus, the early detection of STIs and pregnancy is very critical, and any delay would adversely affect the successful administration of EC and PEP against HIV and other STIs.
Key points
The overwhelming effect of sexual assault is short, but the long-term physical and psychological consequences can be more harmful.
Unintended pregnancy as a consequence of sexual assault has dire impacts on the health and socio-economic well-being of the victims and their loved ones.
Promptness in the diagnosis of pregnancy and sexually transmitted infections is very critical as any delay would affect the successful administration of emergency contraceptives and post-exposure prophylaxis against HIV and other STIs.
Pregnancy-associated with sexual assault can be prevented using emergency contraception (over 95%) when taken within five days after the unprotected sexual encounter.
Abbreviations
- EC
Emergency contraception
- ECP
Emergency contraceptive pill
- HBV
Hepatitis B virus
- HPV
Human papilloma virus
- IUD
Intrauterine devices
- LARC
Long-acting reversible contraception
- MTP
Medical Termination of Pregnancy
- NAAT
Nucleic acid amplification test
- PEP
Post exposure prophylaxis
- RRP
Rape-related pregnancy
- SA
Sexual assault
- SAV
Sexual assault victim
- STI
Sexually transmitted infection
- UPSE
Unprotected sexual encounter
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal.
Declarations
Ethics approval and consent to participate
This manuscript is a part of the study approved by the Kasturba Medical College and Kasturba Hospital Institutional Ethics Committee through vide reference no 653/2018. This manuscript does not report on or involve the use of any animal or human data or tissue.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Renjulal Yesodharan, Email: renjulal.y@manipal.edu.
Pratibha Kamath, Email: pratibha.prakash@manipal.edu.
Vishnu Renjith, Email: vishnurenjith@yahoo.co.in, Email: vishnurenjith@rcsi.com.
Nirmal M. Krishnan, Email: nirmal.krishnan@manipal.edu
Udara Dilrukshi Senarathne, Email: udara.senarathne@sjp.ac.lk.
Suja Kumari Sasidharan, Email: sujaks@nursing.aims.amrita.edu.
Tessy Treesa Jose, Email: tessy.j@manipal.edu.
Vinod C. Nayak, Email: vinod.nayak@manipal.edu
References
- 1.de Souza Costa YR, Lavorato SN, de Campos JJ. Violence against women and drug-facilitated sexual assault (DFSA): a review of the main drugs. J Forensic Leg Med [Internet]. 2020;74:102020. Available from: https://www.sciencedirect.com/science/article/pii/S1752928X2030127X. [DOI] [PubMed]
- 2.Castagna P, Ricciardelli R, Piazza F, Mattutino G, Pattarino B, Canavese A, et al. Violence against African migrant women living in Turin: clinical and forensic evaluation. Int J Legal Med [Internet]. 2018;132:1197–204. Available from: 10.1007/s00414-017-1769-1. [DOI] [PubMed]
- 3.Topçu ET, Kazan EE. The opinions of senior nursing students about forensic nursing. Egypt J Forensic Sci [Internet]. 2018;8:16. Available from: 10.1186/s41935-018-0045-y.
- 4.Yesodharan R, Jose TT, Nirmal Krishnan M, Anitha S, Nayak VC. Looking through the lens of a sexual assault examiner: novel trends and approaches in forensic photography. Egypt J Forensic Sci [Internet]. 2021 [cited 2021 Sep 28];11:27. Available from: https://ejfs.springeropen.com/articles/10.1186/s41935-021-00241-7.
- 5.Yesodharan R, Renjith V, Kumar A, Nayak VC. Forensic clinical photography: a game changer in medicolegal investigation and forensic science. Indian J Forensic Med Toxicol. 2018;12:262–266. doi: 10.5958/0973-9130.2018.00113.5. [DOI] [Google Scholar]
- 6.Ludes B, Geraut A, Väli M, Cusack D, Ferrara D, Keller E, et al. Guidelines examination of victims of sexual assault harmonization of forensic and medico-legal examination of persons. Int J Legal Med [Internet]. 2018;132:1671–4. Available from: 10.1007/s00414-018-1791-y. [DOI] [PubMed]
- 7.Kaur S, Kaur S, Rawat B. Medico-legal evidence collection in child sexual assault cases: a forensic significance. Egypt J Forensic Sci [Internet]. 2021;11:41. Available from: 10.1186/s41935-021-00258-y.
- 8.Zerbo S, Milone L, Scalici E, Procaccianti S, Nardello R, Ventura Spagnolo E, et al. Medico legal procedures related to sexual assault: a 10-year retrospective experience of a Daphne protocol application. Egypt J Forensic Sci [Internet]. 2018;8:4. Available from: 10.1186/s41935-018-0039-9.
- 9.Taft AJ, Shankar M, Black KI, Mazza D, Hussainy S, Lucke JC. Unintended and unwanted pregnancy in Australia: a cross-sectional, national random telephone survey of prevalence and outcomes. Med J Aust. 2018;209(9):407–408. 10.5694/mja17.01094. Epub 2018 Oct 8. PMID: 30282564. [DOI] [PubMed]
- 10.Sommers MS, Brown KM, Buschur C, Everett JS, Fargo JD, Fisher BS, et al. Injuries from intimate partner and sexual violence: significance and classification systems. J Forensic Leg Med [Internet]. 2012;19:250–63. Available from: https://www.sciencedirect.com/science/article/pii/S1752928X1200039X. [DOI] [PMC free article] [PubMed]
- 11.Rowse J, Bolt C, Gaya S. Swipe right: the emergence of dating-app facilitated sexual assault. A descriptive retrospective audit of forensic examination caseload in an Australian metropolitan service. Forensic Sci Med Pathol [Internet]. 2020;16:71–7. Available from: 10.1007/s12024-019-00201-7. [DOI] [PubMed]
- 12.Park JH, Kim N, Shin S, Roh EY, Yoon JH, Park H. Prevalence and correlated factors of sexually transmitted infections among women attending a Korean sexual assault center. J Forensic Leg Med [Internet]. 2020;71:101935. Available from: https://www.sciencedirect.com/science/article/pii/S1752928X2030041X. [DOI] [PubMed]
- 13.Barbeyrac B de, Benali L, Clerc M, Garapon S, Bébéar C, Gromb S. Chlamydia trachomatis infection in children: Do not forget perinatal acquisition: a case report of a 7-year old girl, C. trachomatis infected, presumed sexually assaulted. J Forensic Leg Med [Internet]. 2010;17:96–8. Available from: https://www.sciencedirect.com/science/article/pii/S1752928X09001267. [DOI] [PubMed]
- 14.Sathirareuangchai S, Phuangphung P, Leelaporn A, Boon-yasidhi V. The usefulness of Neisseria gonorrhoeae strain typing by Pulse-Field Gel Electrophoresis (PFGE) and DNA detection as the forensic evidence in child sexual abuse cases: a case series. Int J Legal Med [Internet]. 2015;129:153–7. Available from: 10.1007/s00414-014-1007-z. [DOI] [PubMed]
- 15.Makasa I, Heathfield LJ. A retrospective study of sexual offences in Zambia. J Forensic Leg Med [Internet]. 2018;54:23–33. Available from: https://www.sciencedirect.com/science/article/pii/S1752928X17302019. [DOI] [PubMed]
- 16.Li D, Wilcox AJ, Dunson DB. Benchmark pregnancy rates and the assessment of post-coital contraceptives: an update. Contraception [Internet]. 2015/01/12. 2015;91:344–9. Available from: https://pubmed.ncbi.nlm.nih.gov/25592079. [DOI] [PMC free article] [PubMed]
- 17.O’Neal EN, Decker SH, Spohn C, Tellis K. Condom use during sexual assault. J Forensic Leg Med [Internet]. 2013;20:605–9. Available from: https://www.sciencedirect.com/science/article/pii/S1752928X13000759. [DOI] [PubMed]
- 18.Schwarz EB, Lewis CA, Dove MS, Murphy E, Zuckerman D, Nunez-Eddy C, et al. Comparative effectiveness and safety of intrauterine contraception and tubal ligation. J Gen Intern Med. 2022;1–8. [DOI] [PMC free article] [PubMed]
- 19.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Secura GM, McNicholas C. Long-acting reversible contraceptive use among teens prevents unintended pregnancy: a look at the evidence. Expert Rev Obstet Gynecol [Internet]. Taylor & Francis. 2013;8:297–9. Available from: 10.1586/17474108.2013.811942.
- 21.Centers for Disease Control and Prevention. Contraception [Internet]. CDC. 2022 [cited 2022 Nov 24]. Available from: https://www.cdc.gov/reproductivehealth/contraception/index.htm.
- 22.Shifren JL, Gass MLS. The North American Menopause Society recommendations for clinical care of midlife women. Menopause United States. 2014;21:1038–1062. doi: 10.1097/GME.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 23.Linton A, Golobof A, Shulman LP. Contraception for the perimenopausal woman. Climacteric England. 2016;19:526–534. doi: 10.1080/13697137.2016.1225033. [DOI] [PubMed] [Google Scholar]
- 24.Francis A, Jasani S, Bachmann G. Contraceptive challenges and the transgender individual. Women’s Midlife Heal [Internet]. 2018;4:12. Available from: 10.1186/s40695-018-0042-1. [DOI] [PMC free article] [PubMed]
- 25.Munuce MJ, Gómez-Elías MD, Caille AM, Bahamondes L, Cuasnicú PS, Cohen DJ. Mechanisms involved in the contraceptive effects of ulipristal acetate. Reproduction England. 2020;159:R139–R149. doi: 10.1530/REP-19-0355. [DOI] [PubMed] [Google Scholar]
- 26.Wilcox AJ, Baird DD, Dunson D, McChesney R, Weinberg CR. Natural limits of pregnancy testing in relation to the expected menstrual period. JAMA United States. 2001;286:1759–1761. doi: 10.1001/jama.286.14.1759. [DOI] [PubMed] [Google Scholar]
- 27.Yeung CW, Cheung ANY. Negative pregnancy test in patients with trophoblastic diseases. Curr Obstet Gynecol Rep. 2013;3:102–106. doi: 10.1007/s13669-013-0067-2. [DOI] [Google Scholar]
- 28.O’Connor RE, Bibro CM, Pegg PJ, Bouzoukis JK. The comparative sensitivity and specificity of serum and urine HCG determinations in the ED. Am J Emerg Med United States. 1993;434–6. [DOI] [PubMed]
- 29.Lavelanet AF, Schlitt S, Johnson BR, Ganatra B. Global Abortion Policies Database: a descriptive analysis of the legal categories of lawful abortion. BMC Int Health Hum Rights [Internet]. 2018;18:44. Available from: 10.1186/s12914-018-0183-1. [DOI] [PMC free article] [PubMed]
- 30.Ministry of Law and Justice. The Medical Termination of Pregnancy (Amendment) Act, 2021 [Internet]. 8 of 2021 India: The Gazatte of India. 2021. Available from: https://egazette.nic.in/WriteReadData/2021/226130.pdf.
- 31.World Health Organization (WHO). Medical management of abortion. Geneva. 2018. [PubMed]
- 32.World Health Organization. Health worker roles in providing safe abortion care and post-abortion contraception. 2015. [PubMed]
- 33.World Health Organization (WHO). Brief sexuality-related communication: recommendations for a public health approach. Geneva 27, Switzerland. 2015. [PubMed]
- 34.Mendoza O, Bonilla JC, Moreno L, Piedrahita C, Mosquera A, Parra-Medina R. Review of clinical non-medico-legal autopsy: a descriptive study in 747 patients. Egypt J Forensic Sci [Internet]. 2018;8:66. Available from: 10.1186/s41935-018-0093-3.
- 35.Rodriguez JJRB, Calacal GC, Laude RP, De Ungria MCA. Integrating presumptive and confirmatory semen tests into DNA profiling of sexual assault evidence: a Philippine example. Egypt J Forensic Sci [Internet]. 2019;9:45. Available from: 10.1186/s41935-019-0149-z.
- 36.Ullah S, Garg RK, Noor F. DNA perspectives of fixed and paraffin embedded human tissues as resource materials for the identification. Egypt J Forensic Sci [Internet]. 2017;7:23. Available from: 10.1186/s41935-017-0027-5.
- 37.Kleppa E, Holmen SD, Lillebø K, Kjetland EF, Gundersen SG, Taylor M, et al. Cervical ectopy: associations with sexually transmitted infections and HIV. A cross-sectional study of high school students in rural South Africa. Sex Transm Infect [Internet]. 2014/10/03. BMJ Publishing Group. 2015;91:124–9. Available from: https://pubmed.ncbi.nlm.nih.gov/25281761. [DOI] [PMC free article] [PubMed]
- 38.Denison HJ, Bromhead C, Grainger R, Dennison EM, Jutel A. Barriers to sexually transmitted infection testing in New Zealand: a qualitative study. Aust N Z J Public Health [Internet]. 2017/06/29. 2017;41:432–7. Available from: https://pubmed.ncbi.nlm.nih.gov/28664644. [DOI] [PMC free article] [PubMed]
- 39.McCormack D, Koons K. Sexually transmitted infections. Emerg Med Clin North Am. United States. 2019;37:725–38. [DOI] [PubMed]
- 40.Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm reports Morb Mortal Wkly report Recomm reports [Internet]. Cent Dis Control Prevent. 2021;70:1–187. Available from: https://pubmed.ncbi.nlm.nih.gov/34292926. [DOI] [PMC free article] [PubMed]
- 41.World Health Organization (WHO). Global health sector strategy on sexually transmitted infections 2016–2021 Towards ending STIs. Geneva 27, Switzerland. 2016.
- 42.Chuang Y-C, Tsai K-N, Ou J-HJ. Pathogenicity and virulence of Hepatitis B virus. Virulence [Internet]. Taylor & Francis. 2022;13:258–96. Available from: 10.1080/21505594.2022.2028483. [DOI] [PMC free article] [PubMed]
- 43.World Health Organization. Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021: accountability for the global health sector strategies 2016–2021: actions for impact: web annex 2: data methods. World Health Organization. 2021.
- 44.Kalichman S, Banas E, Kalichman M, Dewing S, Jennings K, Daniels J, et al. Brief enhanced partner notification and risk reduction counseling to prevent sexually transmitted infections, Cape Town, South Africa. Sex Transm Dis [Internet]. Lippincott Williams & Wilkins. 2021;48:174–82. Available from: https://pubmed.ncbi.nlm.nih.gov/32976362. [DOI] [PMC free article] [PubMed]
- 45.Cosentino LA, Campbell T, Jett A, Macio I, Zamborsky T, Cranston RD, et al. Use of nucleic acid amplification testing for diagnosis of anorectal sexually transmitted infections. J Clin Microbiol [Internet]. 2012/04/04. Am Soc Microbiol. 2012;50:2005–8. Available from: https://pubmed.ncbi.nlm.nih.gov/22493338. [DOI] [PMC free article] [PubMed]
- 46.Tobin L, Guerra L, Ahouanvoeke L, Carpio JG, Irambona D, Nyarko EO, et al. Is it time to use nucleic acid amplification tests for identification of persons with sexually transmitted infections?: evidence from seroprevalence and behavioral epidemiology risk surveys in men with chlamydia and gonorrhea. Pan Afr Med J [Internet]. The African Field Epidemiology Network. 2020;36:299. Available from: https://pubmed.ncbi.nlm.nih.gov/33117493. [DOI] [PMC free article] [PubMed]
- 47.Wheeler HL, Agarwal S, Goh BT. Dark ground microscopy and treponemal serological tests in the diagnosis of early syphilis. Sex Transm Infect. 2004;80:411–414. doi: 10.1136/sti.2003.008821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramoni S, Genovese G, Pastena A, Casazza G, Lunghi G, Marzano AV, et al. Clinical and laboratory features of 244 men with primary syphilis: a 5-year single-centre retrospective study. Sex Transm Infect [Internet]. 2021;97:479 LP – 484. Available from: http://sti.bmj.com/content/97/7/479.abstract. [DOI] [PubMed]
- 49.Centers for Disease Control and Prevention. US Public Health Service: Pre-exposure prophylaxis for the prevention of HIV infection in the United States - 2021 Update: a clinical practice guideline [Internet]. Centers Dis. Control Prev. 2021. Available from: https://stacks.cdc.gov/view/cdc/53509.
- 50.Dominguez KL, Smith DK, Vasavi Thomas, Crepaz N, Lang K, Heneine W, et al. Updated guidelines for antiretroviral postexposure prophylaxis after sexual, injection drug use, or other nonoccupational exposure to HIV—United States, 2016 [Internet]. Atlanta, GA. 2016. Available from: https://stacks.cdc.gov/view/cdc/38856.
- 51.Ebert J, Sperhake JP, Degen O, Schröder AS. The use of HIV post-exposure prophylaxis in forensic medicine following incidents of sexual violence in Hamburg, Germany: a retrospective study. Forensic Sci Med Pathol [Internet]. 2018;14:332–41. Available from: 10.1007/s12024-018-9985-7. [DOI] [PubMed]
- 52.Fine P, Mathé H, Ginde S, Cullins V, Morfesis J, Gainer E. Ulipristal acetate taken 48-120 hours after intercourse for emergency contraception. Obstetrics and gynecology. United States; 2010;115:257–63. [DOI] [PubMed]
- 53.Glasier AF, Cameron ST, Fine PM, Logan SJS, Casale W, van Horn J, et al. Ulipristal acetate versus levonorgestrel for emergency contraception: a randomised non-inferiority trial and meta-analysis. The Lancet [Internet]. 2010;375:555–62. Available from: https://www.sciencedirect.com/science/article/pii/S0140673610601018. [DOI] [PubMed]
- 54.Rönn MM, Mc Grath-Lone L, Davies B, Wilson JD, Ward H. Evaluation of the performance of nucleic acid amplification tests (NAATs) in detection of chlamydia and gonorrhoea infection in vaginal specimens relative to patient infection status: a systematic review. BMJ Open [Internet]. 2019;9:e022510. Available from: http://bmjopen.bmj.com/content/9/1/e022510.abstract. [DOI] [PMC free article] [PubMed]