Abstract
Unusual presentations and uncommon clinical manifestations of Monkeypox (Mpox) in the current outbreak highlight the need to focus on cardiac symptoms of the virus. Owing to limited discussion regarding cardiac involvement in recent cases of Mpox, we conducted a scoping review to determine the range of existing research and provide a descriptive overview of the current literature on these manifestations. This review was conducted using a previously developed six-stage methodological approach and keeping in view the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews (PRISMA-ScR). Records retrieved from PubMed, ScienceDirect and Google Scholar, using a two-step search strategy, were subjected to title and abstract screening, followed by full text screening of remaining articles against specified eligibility criteria. Relevant information was extracted and summarized. Our search yielded 707 records. Following title and abstract screening, 23 articles were retrieved for full text screening. Finally, a total of nine articles were included in this review (three case series and six case reports discussing a total of 13 patients). Myocarditis was identified as the most frequently reported cardiac manifestation of Mpox. Novel clinical presentations included pharyngitis, sore throat, proctalgia, and perianal irritation. Most patients reported chest pain as the primary symptom of cardiac system involvement. Elevated troponin was the most commonly reported investigation finding followed by an elevated C- Reactive Protein. There exists a lack of high-quality studies investigating cardiac system involvement in the current outbreak of Mpox. More information is needed regarding risk factors for cardiac complications, disease progression, and cardio tropism and immunological response to improve preventive/therapeutic strategies. We highlight the paucity of relevant data and call for further discussion to improve the understanding of cardiac manifestations of Mpox. This scoping review sheds light on the underexplored cardiac manifestations of Mpox and highlights the need for heightened awareness of cardiac symptoms in the current outbreak.
Keywords: Monkeypox, Myocarditis, Pericarditis, Heart, Smallpox.
SUMMARY
1. Introduction
2. Identifying Relevant Studies
3. Study Selection Process
4. Data Charting
5. Collating, Summarizing, and Reporting the Results
6. Search Results and Characteristics of Included Studies
7. Patient Characteristics
8. History of Sexual Contact
9. Clinical Presentation
10. Cardiac Manifestations
11. Investigation Findings
12. Diagnosis
13. Management
14. Discussion
14.1 Cardiovascular events following vaccination
-
14.2 Cardiac Manifestations of Mpox
14.2.1 Pathogenesis of Mpox-induced Myocarditis
14.2.2 Pathogenesis of Mpox-induced Pericarditis
14.3 Investigations and Management
14.4 Limitations
14.5 Future Recommendations
15. Conclusion
1. Introduction
As the world had begun to recover from the damage coronavirus disease 2019 (COVID-19) had caused, health systems around the globe were faced with another emerging infection the cases of which, although date back to the 1950s, became a public health emergency of global concern only recently. As of January 31, 2023, over eighty-five thousand people in 110 countries have been reported to be infected with Monkeypox (Mpox)1. Only seven of these countries, in the region of Central and West Africa, have had reports of Mpox in the past2. Over the past couple of months, as the spread of the disease intensified and became more widespread, more than ten thousand new cases have been documented and four new geographical locations have been impacted2. With the emergence of cases in non-endemic regions, the World Health Organization (WHO) declared it a global health emergency in July 2022, having issued an alert two months earlier in May2. Since then, reports of cases in new locations have uncovered clusters of novel clinical manifestations that provide important insight into the clinicopathological differences of the current cases from the previous ones.
Patients with Mpox infection typically report nonspecific prodromal symptoms such as fever, fatigue, malaise, and headache, however, in the current outbreak, presentation with classic lesions without a prodromal phase is not uncommon2. The cutaneous lesion classically presents as singular vesicles or a cluster of painful umblicated papules having centrifugal pattern of distribution with local lymphadenopathy and a myriad of systemic symptoms2. However, skin lesions with unusual distribution and characteristics have been documented over the genitalia, anus, and perianal area. Additionally, anorectal manifestations such as proctitis, tenesmus, diarrhea, and proctalgia have also been reported2. Similarly, pharyngitis, tonsillar lesions, and epiglottitis are some of the oropharyngeal presentations of the novel Mpox outbreak2. Other uncommon presentations include ocular lesions such as conjunctivitis3, as well as certain cardiovascular manifestations. As cardiac symptoms of Mpox remain underdiscussed, we performed a scoping review to assess the extent, range, and nature of available research and to provide a descriptive summary of the existing literature on these manifestations using a systematic approach.
This review was undertaken using the six-stage methodological approach developed by Arksey and O’Malley4, presented in their 2005 guidelines titled ‘Scoping studies: Towards a methodological framework’, which is also in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews (PRISMA-ScR). With reports of unusual presentations and uncommon clinical manifestations of Mpox, a broad review question, in line with the recommendations for scoping reviews, was developed to guide the course of this review: What are the manifestations of cardiac involvement in patients diagnosed with Mpox in the current outbreak? This scoping review only included previously published scientific literature, without direct involvement of any patient population, therefore, ethical committee approval was not required.
2. Identifying Relevant Studies
In order to identify articles reporting cardiac manifestations in Mpox patients, a thorough literature search was performed on the following databases: PubMed, ScienceDirect, and Google Scholar using a two-step search strategy. First, an initial search of the information sources listed above was undertaken using key terms, modified accordingly for each database, separately and in combination. The search string employed to retrieve relevant data on PubMed is provided in Table 1.
Table 1. Search string for retrieving relevant records on PubMed.
| Concepts | Search String |
|---|---|
| Cardiac manifestations | (heart) OR (cardiac) OR (st segment) OR (heart failure) OR (cardiogenic shock) OR (myocarditis) OR (pericarditis) OR (acute coronary syndrome) |
| Monkeypox virus | (monkeypox) OR (monkeypox virus) OR (monkey pox) OR (mpox) OR (mpxv) |
In the next step, citation lists of relevant studies were manually screened to develop a comprehensive list of literature eligible to proceed to the screening process.
3. Study Selection Process
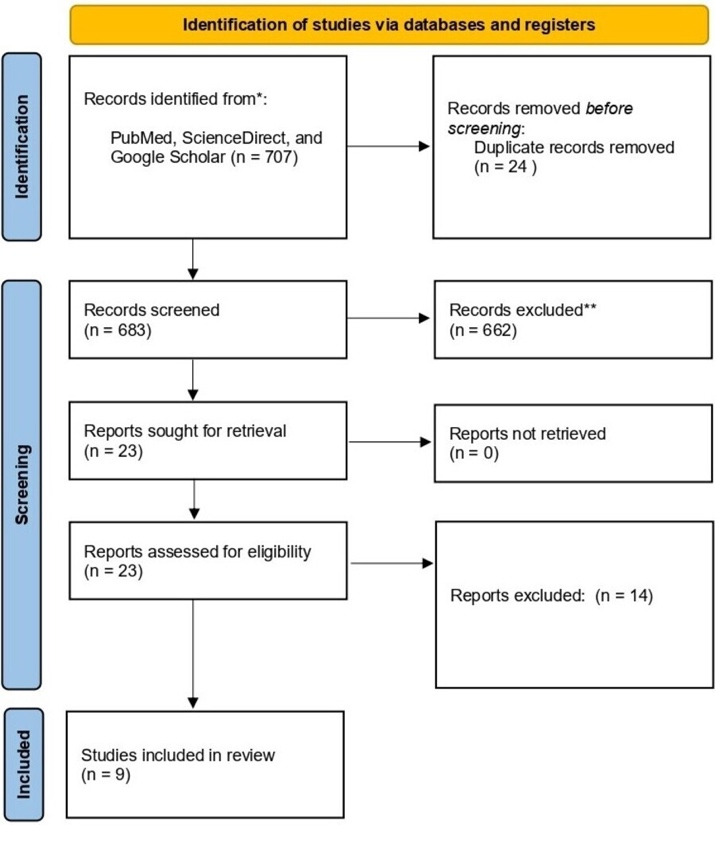
Eligibility criteria: Primary literature, published in the English language from January 2022 to January 2023, that reported cardiac manifestations in patients of Mpox, was considered eligible for inclusion without any restrictions regarding race, geographical location, gender, or setting. Letters, correspondence, opinions, perspectives, and book chapters were excluded. Studies evaluating cardiac complications of monkeypox vaccines were also not included. Before each phase, a pilot stage was conducted to ensure understanding of eligibility criteria between reviewers and the level of agreement was measured using the Cohen’s Kappa with a value of >0.8 required to initiate the complete screening process. Study screening process: Following the removal of duplicates, screening of extracted articles was carried out using a two-step process. During the first phase of screening, title/abstract of extracted studies were screened independently and in duplicate by two authors using Rayyan. In case of any disagreement during title/abstract screening, the article was included. Title/abstract screening was followed by full-text screening of the remaining articles. Any disagreement during the second phase of screening was resolved through mutual discussion and consensus. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flowchart developed to systematically present the article screening process has been shown in Figure 1.
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta- analyses (PRISMA) flowchart showing the article screening process.
4. Data Charting
A structured data extraction form was developed on Microsoft Excel and checked independently by two reviewers for clarity and relevance. Key data points from each article were extracted which included the Author name, article type, and country of affiliation of corresponding author. Data pertaining to the objectives of this scoping review included; age of the patient, sex of the patient, presenting complaint, characteristics of cutaneous lesions, sexual history, comorbidities, previous and concurrent sexually transmitted diseases (STDs), investigation findings, diagnosis, management, duration of hospital stay, and patient outcome.
5. Collating, Summarizing, and Reporting the results
The final version of the summary of findings extracted was revised to include feedback from all co-authors and results obtained are discussed in detail under the relevant heading.
6. Search Results and Characteristics of Included studies
Using the two-step search strategy, our search yielded a total of 707 records from the three databases. Following the removal of duplicates, a total of 683 articles were considered eligible for screening. Of these, 662 articles failing to meet the eligibility criteria were excluded, and 23 articles were retrieved for full-text screening. Finally, a total of nine articles were included in this review, which included three case series5-7, and six case reports8-13, discussing a total of 13 patients. Out of these articles, two each were published from Canada and the United States of America, while one article each was published from institutions based in France, Portugal, Italy, Spain, and Pakistan. Summary of all 13 cases has been presented in Table 2 and Table 3.
Table 2. Summary of demographic characteristics, presentation, and medical history of 13 patients discussed in our review.
| Cases | Age (years) | Sex | History of COVID-19 | Presentation | Fever | Myalgia | Malaise | Head-ache | Lymph-adenopathy | History of recent sexual contact | PrEP Use | Co-morbidities | Previous STDs | Concurrent STDs |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 18 | 34 | M | Negative | Fever, chills, and chest pain | Yes | Yes | NR | NR | B/L tender Inguinal | Heterosexual Also history of contact with potentially contaminated fomites | None | None | None | Chlamydia |
| Case 29 | 31 | M | Positive | Malaise, myalgias, and fever followed by eruption of multiple cutaneous lesions. | Yes | Yes | Yes | NR | Lt. inguinal | NR | Yes | None | None | None |
| Case 312 | 51 | M | NR | Chest Pain | Yes | - | Yes | NR | None | NR | None | None | None | None |
| Case 413 | >40 | M | NR | Skin lesions, constitutional symptoms | Yes | Yes | NR | Yes | Rt. tender Sub-mandibular | MSM, engaged in oral sex, rimming, and condomless, insertive anal sex | None | None | None | Stable HIV |
| Case 56 | 32 | M | Negative | Chest pain and dyspnoea | NR | NR | Yes | Yes | Cervical Left inguinal | MSM | None | None | Syphilis (Treated) | None |
| Case 66 | 37 | M | Negative | Rash, fever, dyspnoea, and decreased exercise tolerance 13 days after a sexual encounter | Yes | NR | Yes | NR | B/L inguinal | Unclear but with multiple Partners | Yes | None | Syphilis (Treated) | None |
| Case 75 | 21 | M | Negative | Fever with anal pain four days after unprotected homosexual intercourse | Yes | NR | NR | NR | None | MSM, Several sexual intercourses with at risk partners during the previous month | None | None | None | None |
| Case 85 | 25 | M | NR | Pustules on face and penis a few days after unprotected sexual intercourse | NR | NR | NR | NR | None | Unclear | None | None | None | None |
| Case 95 | 32 | M | NR | Erosive cutaneous lesions on the penis one week after unprotected sexual intercourse | Yes | NR | NR | NR | None | Heterosexual | None | None | None | None |
| Case 1011 | 40 | M | NR | Odynophagia, a swollen right submandibular lymph node, cervical pain, and a fever of up to 38◦C. | Yes | NR | NR | NR | Rt. Sub-mandibular | MSM, mainly oral. Partner diagnosed with genital Mpox | None | None | HPV Condyloma | None |
| Case 1110 | 45 | M | Negative | Recent onset of pustular lesions | NR | Yes | Yes | NR | Painful U/L inguinal | MSM | No, but history of ARVT use | None | None | HIV |
| Case 127 | Middle aged | M | NR | Sore throat, fever, myalgias, headache, chest pain. | Yes | Yes | NR | Yes | B/L Painful inguinal | MSM | No, but history of ARVT use | Asthma, OSA | None | HSV-2 |
| Case 137 | Young adult | M | NR | Flu-like symptoms, constant, non-radiating, dull, left-sided groin pain and rectal pain | Yes | Yes | NR | Yes | Rt. tender inguinal | MSM | None | OSA, external hemorrhoids, Obesity | Syphilis | HSV-2 |
Table 3. Summary of cardiac manifestations and relevant investigations carried out in 13 patients discussed in our review.
| Cases | Nature of Chest Pain | ECG Findings | TTE | VEF | Echo Findings | CMR Findings | Blood tests | Chest X Ray | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|
| Case 18 | Constant, sharp, nonradiating, pleuritic chest pain, relieved when sitting upright and worse when lying down | Concave ST-elevations | NR | 44% | ↓LV EF | Myocardial edema | ↑TLC, ↑Neutrophils ↑Monocytes ↑CRP ↑Troponin | Non-specific retro-cardiac opacities. | Acute myocarditis |
| Case 29 | Chest tightness radiating to the left upper extremity | Repolarization abnormalities | Preserved biventricular systolic function and no pericardial effusion | 56% | U/R | Myocardial edema and enhancements likely due to necrosis | ↑CRP ↑CPK ↑Troponin ↑BNP | Normal cardiothoracic index, and no interstitial infiltrates, pleural effusion, or masses | Acute myocarditis |
| Case 312 | Retrosternal chest pain radiating to the left arm. Chest tightness after the commencement of the pain | Widespread ST-elevations | Good bi-ventricular function with preserved systolic ejection fraction over 55%, hyperdynamic systolic function | NR | Mild pericardial effusion | NR | ↑CRP ↑ESR ↑TLC | No acute pathology | Pericarditis |
| Case 413 | Central, nonradiating, pressure-like chest pain | ST changes consistent with myopericarditis | NR | 61% | LV dysfunction | Mild pericardial effusion Focal edema | ↑Troponin ↑CPK | NR | Myopericarditis |
| Case 56 | Chest pain and dyspnoea | Normal | NR | 69% | U/R | NR | ↑Troponin ↑ Pro-NT-BNP | U/R | Acute myocarditis |
| Case 66 | Dyspnoea and decreased exercise tolerance without chest pain | T wave inversions in the inferior and anterolateral leads | NR | NR | U/R | NR | ↑Troponin Normal BNP | NR | Acute myocarditis |
| Case 75 | Acute chest pain radiating to the arms and jaw | ST elevation in inferior leads | Nondilated, nonhypertrophied left ventricle with segmental hypokinesis of inferior and inferolateral walls | 56% | Segmental hypokinesis | No cardiac inflammation at four weeks | ↑Troponin ↑CPK ↑CRP | NR | Acute myocarditis |
| Case 85 | Constant chest pain and palpitations | ST elevation in the inferior and anterior territories | inferolateral akinesia | 45% | ↓LVEF | NR | ↑Troponin ↑CRP | NR | Acute myocarditis |
| Case 95 | Retrosternal chest pain and fever | Normal | Normal | NR | Normal | Segmental myocarditis on 11th day | ↑Troponin ↑CPK ↑CRP | NR | Acute segmental myocarditis |
| Case 1011 | Oppressive epigastric pain extending to the chest | Concave ST-elevations, negative T wave, and depressed PR segment | Normal | Normal | NR | Myocardial edema Subepicardial and mesocardial enhancements and mild signs of pericarditis | ↑CRP ↑Troponin | No significant findings | Acute myopericarditis |
| Case 1110 | NR | NR | NR | NR | NR | NR | ↑CPK ↑Lymphocytes ↑AST ↑Lactate dehydrogenase | NR | Uncertain |
| Case 127 | Intermittent pleuritic chest pain | Normal | NR | NR | NR | NR | ↑Troponin | NR | Demand ischemia |
| Case 137 | Sharp chest pain that resolved spontaneously | Normal | NR | NR | NR | Normal | ↑Troponin | NR | Demand ischemia |
7. Patient Characteristics
Age of the patient was reported in 10/13 cases with a median age of 33 years ranging from 21 to 51 years. All of the patients included in this review were men. Out of the 13 patients, three were reported to be positive for the Human Immunodeficiency Virus (HIV)7,10,13, while three had been previously treated for Syphilis6,7, and one had previous history of Human Papillomavirus Condyloma11. Pre-exposure prophylaxis for HIV was reported in two patients6,9. Moreover, asthma and obstructive sleep apnea (OSA) were reported comorbidities in one patient7, and one case had been previously treated for OSA, external hemorrhoids, and obesity7.
8. History of Sexual Contact
A total of 53.84% (7/13) patients had a history of sexual contact with a same sex partner5-7,10,11,13. Two patients reported a history of sexual contact with a partner of opposite sex5,8. One patient reported having sexual contact with multiple partners6. Sexual history in the remaining patients was unclear.
9. Clinical Presentation
Patients most commonly presented with fever5-9,11-13, myalgia7-10,13, malaise6,9,10,12, and headache6,7,13. Classical cutaneous lesions which were umblicated6-8,11,13, erythematous7, pustular5,6,9, vesiculo-pustular6,12,13, vesicular6,10, papular13, and erosive5, in nature were reported in almost all cases with wide ranging distribution patterns as shown in Table 4. Lymphadenopathy was reported in 69.23% (9/13) of the cases with inguinal being the most common site6-10. Submandibular11,13, and cervical lymphadeno-pathy6, was also reported. Out of these nine patients with lymphadenopathy, 55.55% (5/9) were reported as having painful or tender lymph node enlargement7,8,10,13.
Table 4. Summary of novel presentations and cutaneous lesions described in 13 patients included in our review.
| Cases | Novel Presentations | Cutaneous Lesions | Characteristics of cutaneous lesions | Distribution |
|---|---|---|---|---|
| Case 18 | None | Yes | Umblicated and ulcerated | Genital |
| Case 29 | None | Yes | Pustular and ulcerated | Face, limbs, and genitals |
| Case 312 | None | Yes | Vesiculopustular | Face and limbs |
| Case 413 | None | Yes | Umblicated, Papules, and vesiculopustular | Genital, trunk, and upper lip |
| Case 56 | None | Yes | Vesiculopapular, pustular, and ulcerated with erythematous borders | Disseminated and genital |
| Case 66 | None | Yes | Umblicated and vesicular | Upper limb and pubis |
| Case 75 | Anal pain | NR | NR | NR |
| Case 85 | None | Yes | Pustules | Face and genitals |
| Case 95 | None | Yes | Erosive | Genitals |
| Case 1011 | Pharyngitis | Yes | Umbilicated | Trunk and proximal limbs |
| Case 1110 | Sore throat | Yes | Vesicular and ulcerated | Genital and diffuse |
| Case 127 | Oropharyngeal | Yes | Erythematous rash and some umblicated | Chest, back, extremities, and genitals |
| Case 137 | Proctalgia, perianal irritation | Yes | Erythematous | NR |
A total of four patients reported novel clinical presentations documented in the current Mpox outbreak. These included pharyngitis11, sore throat7, proctalgia5,7, and perianal irritation7. Some patients were also concurrently diagnosed with STDs along with Mpox, which included chlamydia and Herpes simplex virus-2 (HSV-2)7.
10. Cardiac Manifestations
Most of the patients reported chest pain as the primary manifestation of cardiac system involvement5-8,12,13. Other presentations included chest tightness9, dyspnoea6, palpitations5, and epigastric pain radiating to chest11. The characteristics of chest pain have been documented in Table 3 and percentage of occurrence of each symptom involving the cardiac system is given in Table 5.
Table 5. Percentage of occurrence of cardiac symptoms in 13 patients discussed in our review.
| Cardiac Manifestation | Percentage occurring |
|---|---|
| Dyspnea | 15.38% (2/13) |
| Acute chest pain | 69.2% (9/13) |
| Chest tightness | 15.38% (2/13) |
| Palpitations | 7.69% (1/13) |
| Decreased exercise tolerance without chest pain | 7.69% (1/13) |
11. Investigation Findings
Elevated troponin was the most commonly reported investigation finding, which was observed in 84.6% (11/13) of the patients5-9,11,13, followed by an elevated C-Reactive protein (CRP) which was reported in 53.84% (7/13) of the patients5,8,9,11,12. Some of the other reported investigation findings were elevated creatine phosphokinase (CPK)5,9,10,13, Pro-N type brain natriuretic peptide6, brain natriuretic peptide9, total leukocyte count8,10,12, Erythrocyte sedimentation rate12, aspartate transaminase10, and lactate dehydrogenase10. A total of six patients had ST-elevations on electrocardiogram (ECG)5,8,11-13, while T-wave inversion6,11, was observed on two ECGs, PR-segment depression on one11, repolarization abnormalities on one9, and no changes on ECG were noted for four patients5-7. Echocardiography was performed for almost all patients and was unremarkable for 7/12 patients5-7,9,11, while three patients had left ventricular dysfunction5,8,13. Segmental hypokinesia5, and mild pericardial effusion12, were also noted on echocardiography. Out of 13, six cases report findings of cardiac magnetic resonance imaging (MRI) suggesting myocardial edema8,9,11,13, pericardial effusion13, and subepicardial and mesocardial enhancements11.
12. Diagnosis
A definitive diagnosis was provided for 10 of the 13 patients, with Mpox-associated acute myocarditis being the most common cardiac manifestation which was observed in 70% of these patients5,6,8,9. Other diagnosis included pericarditis12, and acute myopericarditis11,13. Two patients were labelled having ‘demand ischemia’7, and another patient was only noted to have an increased CPK10- no definitive diagnosis was reached for these three patients.
13. Management
Most of the patients received supportive care for acute myocarditis6,9,13as summarized in Table 6. One patient diagnosed with Mpox associated pericarditis received therapy with 1gm Aspirin 8-hourly for 14 days12. Tecovirimat was the most commonly employed antiviral medication used in this patient population5,6,8,11. Certain other medications used were ceftriaxone for chlamydia8, doxycycline for syphilis of unknown latency6, valaciclovir for HSV-27, dexketoprofen11, colchicine11, bisoprolol5, and ramipril/angiotensin converting enzyme-inhibitors5,8. Almost all of the patients recovered without complication.
Table 6. Summary of management of 13 cases included in our review.
| Cases | Other causes ruled out | Monkeypox Diagnosed | Management | Resolution of lesions/symptoms | Hospital Stay | Final Outcome |
|---|---|---|---|---|---|---|
| Case 18 | Yes | Yes | Tecovirimat Ceftriaxone and Azithromycin ACE inhibitor | Skin lesions and lymphadenopathy resolved in nine days | 10 days (LAMA) | Uncertain |
| Case 29 | Yes | Yes | Supportive care | Complete | Seven days | Discharged upon resolution |
| Case 312 | Yes | Yes | Supportive care + 1gm Aspirin/8 hourly for 14 days | On seventh day | Seven days | Discharged with high dose aspirin prescription |
| Case 413 | Yes, except EBV, CMV, Parvovirus B19, Chagas | Yes | Supportive care | LV function restored on fifth day Full recovery on 25th day | NR | Full recovery |
| Case 56 | Yes | Yes | Tecovirimat Doxycycline for syphilis of unknown latency No specific treatment for myocarditis | Chest pain resolved at day two, Skin lesions resolved at day 10 | 10 days | Discharged with isolation precautions |
| Case 66 | Yes | Yes | Supportive care | Dyspnea resolved on fourth day | Four days | Discharged after isolation precautions |
| Case 75 | Yes | Yes | Bisoprolol and Ramipril | No recurrence of pain | NR | NR |
| Case 85 | Yes | Yes | Bisoprolol and Ramipril | Rapid and favourable | NR | NR |
| Case 95 | Yes | Yes | Bisoprolol Tecovirimat | Chest pain resolved on day two | NR | NR |
| Case 1011 | Yes | Yes | Dexketoprofen Colchicine Tecovirimat | Skin lesions and lymphadenopathy resolved in nine days | NR | Discharged with instructions to follow with a CMR on 20th March, 2023 |
| Case 1110 | Yes | Yes | NR | NR | NR | NR |
| Case 127 | NR | Yes | Unclear Valacyclovir for HSV2 | NR | NR | Discharged with instructions to quarantine |
| Case 137 | NR | Yes | Unclear Valacyclovir for HSV2 | NR | NR | Discharged with instructions to quarantine |
14. Discussion
Given the atypical clinical manifestations, diverse modes of transmission and rapid spread from endemic to non-endemic areas, Mpox is emerging as a significant global health concern14. Thus, it is important not to undervalue the onset of chest pain in an infected patient, which should trigger immediate cardiac investigations.
14.1. Cardiovascular events following vaccination
There appears to be a considerable overlap in the antigenic properties of various Orthopoxviruses such as variola virus, cowpox virus, and the Mpox. Several reports have documented that patients with hemorrhagic smallpox can develop acute onset late-stage myocarditis15. These findings have also been replicated in Crab-Eating Macaque model using the cowpox virus which mimics hemorrhagic smallpox in humans15. Furthermore, smallpox vaccine is strongly linked to post-vaccination myocarditis, with a reported incidence of 12 per 100,000 vaccinations16. The incidence of myocarditis following administration of ACAM2000 is 3.6 times greater among the vaccinated USA military personnel17,18. Within this group, definite vaccinia myocarditis was reported in 1 out of every 10,000 vaccinated individuals, typically manifesting 8 to 14 days after receiving the smallpox vaccine. In addition to these, less frequently reported adverse events involving the cardiac system include dilated cardiomyopathy and cardiac ischemia17,18. The vaccine against smallpox called the ‘JYNNEOS’ is prepared using the Vaccinia virus as the inoculating agent and has a reported efficacy of 85% against Mpox8. As a result of these viruses’ similar antigenic or immunogenic properties, it can be extrapolated that Mpox may also cause myopericarditis via direct cardiac tropism or by an immune-mediated response.
14.2. Cardiac Manifestations of Mpox
As indicated by the results of our scoping review, myocarditis was the most prevalent cardiac lesion among the 13 patients included in our review with acute chest pain as the most frequently reported symptom of cardiac system involvement. In addition to myocarditis and pericarditis, recently published literature reports congestive heart failure17, arrythmias19, and vascular complications20 following Mpox infection.
14.2.1. Pathogenesis of Mpox-induce Myocarditis
The mechanism by which Mpox may cause inflammation of the myocardium remains largely unclear given the limited data available regarding Mpox associated myocarditis. The primary pathogenic process of viral myocarditis involves lymphocytic infiltration coupled with myonecrosis, which usually becomes evident at around 10 to 14 days following infection21. Previously published literature reports direct damage caused by viral antigens as one of the possible mechanisms of myocardial injury. The virus may directly invade the myocardium and undergo replication within the cardiac myocytes, resulting in inflammatory disease22,23. However, an absence of evidence of direct viral infection of myocardial cells observed on histopathological investigation suggests that the mechanism of myocarditis in Mpox and other orthopoxvirus infections may be immune-mediated6,24. Furthermore, the most frequently reported histologic finding associated with viral myocarditis is infiltration of the myocardium with lymphocytes. Additionally, edema of myocardial interstitium has also been reported. This is further suggestive of the immune-mediated pathophysiology of Mpox induced myocarditis23. An inflammatory response, characterized by the infiltration of immune cells, release of proinflammatory cytokines, and activation of cytotoxic T cells, results from the binding of viral genome to the immune cells that triggers the immune system22. This complex interplay between direct damage induced by the virus and the immune response is likely to contribute to the development of myocardial inflammation and subsequent impairment of cardiac function25. This inflammation of the myocardium may be self-limiting or progress to severe fulminant myocarditis26. Further research is warranted to achieve a thorough understanding of the pathological mechanisms underlying myocarditis development in individuals with Mpox.
14.2.2. Pathogenesis of Mpox-induced Pericarditis
Pericarditis refers to the inflammation of the pericardium surrounding the heart. As indicated by our findings, as well as previously published literature, Mpox can cause pericarditis through direct invasion and immune mediated mechanisms22. The pericardium may be directly invaded by the virus or an immune response following viral invasion may be observed27.
The differential diagnoses of inflammatory cardiac complications in presence of mucocutaneous lesions and lymphadenopathy are vast, hence the diagnosis of these complications in Mpox cases becomes challenging. Thus, it is imperative to maintain a broad perspective when encountering such presentations. Considering the recent surge in cases and diagnostic uncertainty associated, a criterion is overdue to escalate the clinical suspicion of cardiac complications in patients with suspected or diagnosed Mpox.
14.3. Investigations and Management
The following clinical characteristics should prompt further investigations to identify Mpox as the underlying cause: 1) Diagnostic criteria satisfying clinically suspected myocarditis/pericarditis; 2) ECG showing ST changes, T-wave, or PR-segment abnormalities; 3) Temporally related to constitutional symptoms of a viral infection such as fever, myalgia, fatigue, headache, and/or other flu-like symptoms; 4) Painless or painful umblicated, vesiculopapular, and/or vesiculopustular lesions on skin with local lymphadenopathy; 5) Other novel manifestations of Mpox such as ocular, oropharyngeal, and/or anorectal; 6) History of sexual contact with a male or female partner within the last 3-17 days; 7) Common differentials ruled out via serology or Polymerase Chain Reaction (PCR). Investigations such as complete blood count, CRP, and cardiac troponins along with electrocardiogram and echocardiography play a crucial role in reaching the diagnosis of myopericarditis. Though Endomyocardial biopsy (EMB) is the gold standard for the diagnosis of myocarditis, it is not commonly performed given the invasive nature of the procedure9. Therefore, cardiac MRI remains the non-invasive gold standard for the prompt diagnosis of myocarditis9. Although the treatment strategy adopted will depend mainly on the severity of the presenting symptoms as well as the presence of any complications, the management of Mpox-induced cardiac lesions remains largely supportive28. For mild cases of viral myocarditis, supportive measures include taking rest, maintaining fluids and reducing inflammation6. In considerably severe cases, hospital admission with strict monitoring, and advanced interventions may become mandatory. Anti-inflammatory agents and immunosuppressive drugs may be employed29. For pericarditis, the use of NSAIDs, colchicine, corticosteroids in addition to supportive measures have been recommended30. Our results show that almost all patients made full recovery with no reported complications, but myopericarditis may have a significant impact on the prognosis as well as the quality of life of the patients, thus highlighting the need for accurate diagnosis31. Despite the positive outcome of myocarditis in some patients, caution is advised as the limited number of reported cases calls for further research. Thus, individuals with Mpox should promptly seek medical attention if they have chest pain. In countries with Mpox outbreaks, healthcare providers should consider Mpox as a potential cause if at-risk patients are diagnosed with myocarditis5.
14.4. Limitations
Although our review provides a broad overview, it does not present the depth of the existing literature and thus makes the conduct of a meta-analysis unlikely. However, in light of our objective this methodology seems appropriate. Currently, there is only limited literature available in the form of case reports and case series and given the continuously evolving nature of novel Mpox manifestations, it is unlikely that our results provide a comprehensive and generalizable picture of the cardiac manifestations of Mpox.
Additionally, quality assessment of the case reports meeting eligibility criteria was not performed since it falls beyond the scope of a scoping review. A descriptive summary of the results has been presented without any statistical aggregation of extracted data which is beyond the objectives of this scoping review. Overall, this scoping review provides a broad overview of the topic and calls attention towards the limitations of the existing literature.
14.5. Future Recommendations
Our scoping review has revealed a significant dearth of high-quality studies investigating the cardiac system involvement in the current outbreak of Mpox. The studies that were eligible for inclusion in our review were primarily limited to case reports and case series, highlighting the need for more rigorous research in this area. The current literature lacks information on potential risk factors that may predispose certain patient populations to cardiac complications associated with Mpox, as well as factors that may predict progression to severe disease. Additionally, there is a need to gain a deeper understanding of the underlying pathology of the cardio tropism of Mpox and the immunologic response generated by the virus in order to develop effective preventive and therapeutic strategies. The indications for antiviral therapy in patients with Mpox and cardiac involvement, as well as the choice of antiviral for these patients, remain unresolved questions.
15. Conclusion
Through this scoping review, we draw attention to the paucity of relevant data and advocate for increased research efforts to better understand the cardiac manifestations of Mpox. Larger, well-designed studies are necessary to establish a link between monkeypox and myocarditis and determine the course of disease and development of complications. It is worth noting that Mpox, like many viruses, exhibits a diverse range of manifestations, and prompt action is necessary to effectively manage and prevent inflammatory cardiac complications associated with Mpox.
KEY POINTS
◊ It is crucial to recognize novel cardiac manifestations in case of the current Monkeypox outbreak, to guide comprehensive surveillance, preparedness, and response efforts.
◊ This knowledge gap emphasizes the urgency for more comprehensive studies evaluating immune response, risk factors, and disease progression to guide better prevention and treatment strategies.
Acknowledgments
No acknowledgments to be mentioned. No funding sources to be disclosed.
Footnotes
Conflict of interests: The authors declare no conflicts of interest.
Abbreviations: Coronavirus disease 2019 (COVID-19); Male (M); Men who have sex with men (MSM); Antiretroviral Therapy (ARVT); Total leukocyte count (TLC); C Reactive Protein (CRP); Creatine phosphokinase (CPK); Aspartate transaminase (AST); Pro b-type natriuretic peptide (Pro-NT-BNP); Brain natriuretic peptide (BNP); Leave against medical advice (LAMA); Not reported (NR); Ebstein-barre virus (EBV); Cytomegalovirus (CMV); Herpes simplex virus 2 (HSV 2); Human immunodeficiency virus (HIV); Human papilloma virus (HPV); Angiotensin converting enzyme (ACE); Unremarkable (U/R); Transthoracic echocardiography (TTE); Cardiovascular magnetic resonance imaging (CMR); Right (Rt.); Bilateral (B/L); Unilateral (U/L); Left (Lt.); Obstructive sleep apnea (OSA); Sexually transmitted diseases (STDs); Electrocardiogram (ECG); Ejection fraction (EF); Left Ventricle (LV); Left ventricular ejection fraction (LVEF); Erythrocyte sedimentation rate (ESR); Monkeypox virus (Mpox).
DISCOVERIES is a peer-reviewed, open access, online, multidisciplinary and integrative journal, publishing high impact and innovative manuscripts from all areas related to MEDICINE, BIOLOGY and CHEMISTRY
References
- 1.2022 Mpox Outbreak Global Map. Centers for Disease Control and Prevention; Accessed: January 31, 2023. 2022. https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html
- 2.Monkeypox. Gessain Antoine, Nakoune Emmanuel, Yazdanpanah Yazdan. The New England journal of medicine. 2022;387(19):1783–1793. doi: 10.1056/NEJMra2208860. [DOI] [PubMed] [Google Scholar]
- 3.Ophthalmic manifestations of monkeypox virus. Abdelaal Abdelaziz, Serhan Hashem Abu, Mahmoud Mariam Abdelmageed, Rodriguez-Morales Alfonso J, Sah Ranjit. Eye (London, England) 2023;37(3):383–385. doi: 10.1038/s41433-022-02195-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scoping studies: towards a methodological framework. Arksey Hilary, O'Malley Lisa. International Journal of Social Research Methodology. 2005;8(1):19-32. [Google Scholar]
- 5.Myocarditis in monkeypox-infected patients: a case series. Dumont Maëlle, Guilhou Thomas, Gerin Magdalena, Frémont-Goudot Guillemette, Nivose Pierre-Louis, Koubbi Arnaud, Joly Véronique, Bouadma Lila, Yazdanpanah Yazdan, André Marie-Hélène, de La Porte des Vaux Clémentine. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2023;29(3):390.e5–390.e7. doi: 10.1016/j.cmi.2022.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myocarditis Attributable to Monkeypox Virus Infection in 2 Patients, United States, 2022. Rodriguez-Nava Guillermo, Kadlecik Peter, Filardo Thomas D, Ain David L, Cooper Joseph D, McCormick David W, Webber Bryant J, O'Laughlin Kevin, Petersen Brett W, Narasimhan Supriya, Sahni Harleen K. Emerging infectious diseases. 2022;28(12):2508–2512. doi: 10.3201/eid2812.221276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herpes and Chest Pain: Two Atypical Monkeypox Cases. Videlefsky Devin, Matos Noboa Constangela, Ramchandani Charu. Cureus. 2023;15(1):e33705. doi: 10.7759/cureus.33705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monkeypox associated myocarditis: A case report. Brouillard Philippe, Valin-Thorburn Anthony, Provost Yves, Chakravarti Arpita, Honos George, Tournoux François, Tremblay Cécile. IDCases. 2022;30:e01628. doi: 10.1016/j.idcr.2022.e01628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acute Myocarditis: A New Manifestation of Monkeypox Infection? Pinho Ana Isabel, Braga Marta, Vasconcelos Mariana, Oliveira Cátia, Santos Luís Daniel, Guimarães André Rodrigues, Martins António, Chen-Xu Juliana, Silva Sofia, Macedo Filipe. JACC. Case reports. 2022;4(21):1424–1428. doi: 10.1016/j.jaccas.2022.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monkeypox virus infection and creatine phosphokinase increase: A case from Italy. Pipitò Luca, Cascio Antonio. Travel medicine and infectious disease. 2022;50:102412. doi: 10.1016/j.tmaid.2022.102412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Case report: From monkeypox pharyngitis to myopericarditis and atypical skin lesions. Sanromán Guerrero María Ascensión, Sánchez Elena Hernández, Ruanes Belén de Nicolás, Fernández-González Pablo, Ugalde Sonia Antoñana, Leal Alejandra González, Fernández Marcelo Sanmartín, Rodríguez Jose Javier Alarcón, Martinez Garcia Laura, Escudero Rosa, Méndez Maria Ángeles Fernández, Zamorano Gómez Jose Luis, Llorente Beatriz Montero, Vivancos-Gallego Maria Jesús. Frontiers in cardiovascular medicine. 2022;9:1046498. doi: 10.3389/fcvm.2022.1046498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Monkeypox-Associated Pericarditis: A Maiden Case. Shaik Tanveer Ahamad, Voloshyna Diana, Nasr Tayseer H, Makki Ameer, Kosuru Suma Harsha, Khan Maryam H, Ghobriel Naglaa G, Sandhu Qudsia I, Saleem Farhan. Cureus. 2022;14(9):e29638. doi: 10.7759/cureus.29638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atypical Clinical Presentation of Monkeypox Complicated by Myopericarditis. Tan Darrell H S, Jaeranny Shelby, Li Maggie, Sukhdeo Sharon S, Monge Juan Carlos, Callejas Matias F, Hasso Maan, Fattouh Ramzi, Lalonde Spencer D, Lam Jeffrey, Mishra Sharmistha. Open forum infectious diseases. 2022;9(8):ofac394. doi: 10.1093/ofid/ofac394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Comparison of Biological, Pharmacological Characteristics, Indications, Contraindications and Adverse Effects of JYNNEOS and ACAM2000 Monkeypox Vaccines. Meo Sultan Ayoub, Al-Masri Abeer A, Klonoff David C, Alshahrani Abdullah Nasser, Al-Khlaiwi Thamir. Vaccines. 2022;10(11) doi: 10.3390/vaccines10111971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Acute Late-Stage Myocarditis in the Crab-Eating Macaque Model of Hemorrhagic Smallpox. Johnson Reed F, Keith Lauren A, Cooper Timothy K, Yellayi Srikanth, Josleyn Nicole M, Janosko Krisztina B, Pettitt James D, Thomasson David, Hagen Katie R, Gross Robin, Bernbaum John G, Douglas Debbie, Solomon Jeffrey, Martinez Mark, Cooper Kurt, St Claire Marisa, Ragland Danny R, Jahrling Peter B, Kuhn Jens H, Arai Andrew E. Viruses. 2021;13(8) doi: 10.3390/v13081571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Myocarditis secondary to smallpox vaccination. Keinath Kyle, Church Tyler, Kurth Benjamin, Hulten Edward. BMJ case reports. 2018;2018 doi: 10.1136/bcr-2017-223523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Precautions and recommendations towards possible cardiac manifestations of monkeypox vaccination. Dayyab Farouq Muhammad, Daiyab Haruna Muhammad, Farahat Ramadan Abdelmoez. International Journal of Surgery. 2022;105:106898. doi: 10.1016/j.ijsu.2022.106898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myopericarditis following smallpox vaccination among vaccinia-naive US military personnel. Halsell Jeffrey S, Riddle James R, Atwood J Edwin, Gardner Pierce, Shope Robert, Poland Gregory A, Gray Gregory C, Ostroff Stephen, Eckart Robert E, Hospenthal Duane R, Gibson Roger L, Grabenstein John D, Arness Mark K, Tornberg David N. JAMA. 2003;289(24):3283–9. doi: 10.1001/jama.289.24.3283. [DOI] [PubMed] [Google Scholar]
- 19.Cardiovascular manifestations of monkeypox virus outbreak: An overview of the reported cases. El-Qushayri Amr Ehab, Tawfik Abdelrahman G, Mahmoud-Elsayed Hani. Heart & lung : the journal of critical care. 2023;59:67–72. doi: 10.1016/j.hrtlng.2023.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Endothelial Cells in Emerging Viral Infections. Fosse Johanna Hol, Haraldsen Guttorm, Falk Knut, Edelmann Reidunn. Frontiers in cardiovascular medicine. 2021;8:619690. doi: 10.3389/fcvm.2021.619690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monkeypox virus infection and myocarditis: A review of current evidence and possible pathogenesis. Ahmed Sirwan K., Dabou Eman A., Abdelsamad Shaimaa, Mohamed Mona G., Chandran Deepak, Chakraborty Sandip, Emran Talha B., Dhama Kuldeep. Narra J. 2023;3(1):e104. doi: 10.52225/narra.v3i1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cardiovascular Manifestations of Human Monkeypox Virus: An Updated Review. Maqbool Khawaja Usama, Arsh Hina, Kumar Deepak, Veena Fnu, Punshi Ashish Kumar, Payal Fnu, Kumar Sameet, Kumar Saroop, Rani Deepa, Malik Jahanzeb. Current problems in cardiology. 2023;48(10):101869. doi: 10.1016/j.cpcardiol.2023.101869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Monkeypox-Induced Myocarditis: A Systematic Review. Jaiswal Vikash, Sultana Qamar, Lahori Simmy, Mukherjee Dattatreya, Agrawal Vibhor, Doshi Neel, Shrestha Abhigan Babu, Huang Helen, Nasir Yusra Minahil, Naz Sidra. Current problems in cardiology. 2023;48(5):101611. doi: 10.1016/j.cpcardiol.2023.101611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cardiac complications after smallpox vaccination. Mora Luis F, Khan Akbar H, Sperling Laurence S. Southern medical journal. 2009;102(6):615–9. doi: 10.1097/SMJ.0b013e31819fe55b. [DOI] [PubMed] [Google Scholar]
- 25.Role of cytokines and inflammation in heart function during health and disease. Bartekova Monika, Radosinska Jana, Jelemensky Marek, Dhalla Naranjan S. Heart failure reviews. 2018;23(5):733–758. doi: 10.1007/s10741-018-9716-x. [DOI] [PubMed] [Google Scholar]
- 26.An overview of the immune mechanisms of viral myocarditis. Lasrado Ninaad, Reddy Jay. Reviews in medical virology. 2020;30(6):1–14. doi: 10.1002/rmv.2131. [DOI] [PubMed] [Google Scholar]
- 27.Autoimmunity and autoinflammation as the yin and yang of idiopathic recurrent acute pericarditis. Cantarini Luca, Lopalco Giuseppe, Selmi Carlo, Napodano Salvatore, De Rosa Gabriella, Caso Francesco, Costa Luisa, Iannone Florenzo, Rigante Donato. Autoimmunity reviews. 2015;14(2):90–7. doi: 10.1016/j.autrev.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 28.Concerns over cardiovascular manifestations associated with monkeypox immunization: a literature review. Shrestha Abhigan Babu, Mehta Aashna, Zahid Muhammad Jawad, Candelario Katherine, Shrestha Sajina, Pokharel Pashupati. Annals of medicine and surgery (2012) 2023;85(6):2797–2801. doi: 10.1097/MS9.0000000000000861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Immunosuppressive therapy in myocarditis. Frustaci Andrea, Chimenti Cristina. Circulation journal : official journal of the Japanese Circulation Society. 2015;79(1):4–7. doi: 10.1253/circj.CJ-14-1192. [DOI] [PubMed] [Google Scholar]
- 30.A review of pericardial diseases: clinical, ECG and hemodynamic features and management. Aikat S, Ghaffari S. Cleveland Clinic journal of medicine. 2000;67(12):903–14. doi: 10.3949/ccjm.67.12.903. [DOI] [PubMed] [Google Scholar]
- 31.Outcomes, long-term quality of life, and psychologic assessment of fulminant myocarditis patients rescued by mechanical circulatory support. Mirabel Mariana, Luyt Charles-Edouard, Leprince Pascal, Trouillet Jean-Louis, Léger Philippe, Pavie Alain, Chastre Jean, Combes Alain. Critical care medicine. 2011;39(5):1029–35. doi: 10.1097/CCM.0b013e31820ead45. [DOI] [PubMed] [Google Scholar]


