Abstract
Background
Globally, the prevalence of childhood obesity has increased considerably, including in Indonesia. Obesity results from multifactorial interactions at the personal, familial, and environmental levels. However, little is known about the factors associated with overweight/obesity among children in Indonesia. This study is intended to identify personal, familial, and environmental factors associated with overweight/obesity in children aged 6–12 years in Indonesia.
Methods
Study design was a secondary data analysis using the Indonesia Family Life Survey in 2014/2015, focusing on 6,090 children aged 6–12 years. The questions covered the child’s body mass index and potential personal, familial, and environmental factors. Logistic regression analysis was performed to identify the personal, familial, and environmental factors.
Results
The mean age of participants was 8.9 years (SD = 2.0); 51.0% were boys; 9.4% were overweight; and 8.1% were obese. Overweight and obesity were associated with age [AOR 1.09 (95% CI 1.04–1.14)], having an overweight [AOR 1.93 (95% CI 1.58–2.36)] or obese [AOR 3.36 (95% CI 2.43–4.61)] father compared with a normal father, being of Chinese [AOR 9.51 (95% CI 1.43–79.43)] or Javanese [AOR 1.60 (95% CI 1.16–2.24)] ethnicity compared with Sundanese ethnicity, and residing in an urban area [AOR 1.36 (95% CI 1.10–1.70)]. A lower risk of child overweight/obesity was associated with the father’s perception [AOR 0.56 (95% CI 0.38–0.80)] and mother’s perception [AOR 0.66 (95% CI 0.43–0.98)] of the child’s food consumption as being less than adequate compared with adequate.
Conclusions
Risk factors in children for overweight/obesity were older age, having an overweight/obese father, membership of certain ethnic groups, and urban residence. The main protective factor was parents’ perception that a child’s food consumption was less than adequate. Health promotion programs focused on these factors could help control or prevent childhood obesity in Indonesia.
Keywords: Child, Indonesia, Obesity, Overweight, Pediatric obesity
Background
Overweight and obesity among children are becoming a crucial public health issues in lower-middle-income countries (LMICs) such as Indonesia, which have lagged high-income countries (HICs) where overweight and obesity began to increase significantly from as early as the mid-1980s [1, 2]. Globally, the prevalence of overweight and obesity among children and adolescents aged 5–19 years has approximately doubled between 1996 and 2016, from 8.9 to 18.4%, respectively, and it has tripled in LMICs, from 3.8 to 11.2%. In Indonesia, the prevalence of overweight and obesity among children and adolescents aged 5–19 years increased fourfold, from 3.9 to 15.4%, between 1996 and 2016, respectively [3]. Meanwhile, in 2018, 10.8% and 9.2% of children aged 5 − 12 years were overweight and obese, respectively [4].
Overweight and obesity during childhood and adolescence can result in short-term adverse consequences including high-blood pressure, [5–8] obstructive sleep apnea, [9] and severe COVID-19, [10–12] as well as long-term consequences, including adult obesity [13] and higher mortality risk: children with obesity were at three times greater risk of premature death than normal children [14]. Overweight and obesity are not only caused by personal characteristics but they also reflect multifactorial interactions of personal, familial, environmental, and cultural factors [15].
Among personal factors, overweight and obesity has been associated with high consumption of obesogenic food, for instance, fast food, snacks, ultra-processed food, and sweet beverages; [16, 17] sedentary behavior; [18] and sleep time [19]. Family-level factors include education, [20, 21] parents’ nutritional status, [17, 19, 22] and parents’ food consumption [23]. A systematic review and meta-analysis found residence in rural or urban areas to be an environmental-level factor contributing to children being overweight and obese, [24, 25] and a 2018 qualitative study identified the diverse ways in which culture influences food preferences that potentially contribute to overweight and obesity [26].
However, the above-referenced literature has few gaps that need to be clarified in future studies. For instance, while some studies have focused entirely on how mothers influence children’s nutritional status [17], little attention has been paid to how fathers influence children’s nutritional status. Moreover, weight and height data from Indonesian studies are based on self-reporting from parents, and these data might differ from direct measurement results [19]. Moreover, inconsistencies in research findings related to the relative impacts of rural and urban residence on overweight and obesity in HICs and LMICs [24, 25] need to be resolved. Lastly, although previous researchers have investigated environment-level impacts of culture on food preferences, [26] few have identified associations between cultural factors and children’s nutritional status. Due to the high level of cultural diversity in Indonesia, future studies should aim to clarify the relationship between cultural diversity and children’s nutritional status in the country.
This study focused on children aged 6–12 years. An ecological study among 34 provinces in Indonesia found that children aged 5–12 years had a higher prevalence of overweight/obesity than adolescents (aged 13–15 and 16–18 years) [27]. In addition, body mass index (BMI) changes during childhood, and children’s BMI begins to increase after six years [28, 29]. The present study was intended to fill these research gaps by identifying personal, familial, and environmental factors associated with overweight and obesity among children aged 6–12 years in Indonesia, an LMIC.
Methods
Survey design and study population
Study design was a secondary data analysis using data from the fifth wave of the Indonesia Family Life Survey (IFLS-5), an extension to 2014/2015 of an ongoing longitudinal survey that was conducted jointly by the RAND Corporation in the United States and University Gadjah Mada in Indonesia. IFLS-5 based on a sample of household represented approximately 83% of the Indonesian population living in 13 of the country’s 27 provinces in 1993. Provinces were selected to represent Indonesia’s population and to capture its cultural diversity. From each province, 321 enumeration areas were randomly chosen from the nationally representative sample frame used in the 1993 National Socioeconomic Survey. Twenty households were randomly selected from each urban enumeration area, and 30 were randomly selected from each rural enumeration area. In the subsequent survey waves, the original household and split-off household were recontacted. IFLS-5 included 16,931 households, a 28.2% overlap with the total of 60,000 households that participated in the 1993 National Socioeconomic Survey [30].
To be included in the data analysis for this study, participants had to be children aged 6–12 years old and their parents, for whom data on weight and height were available to calculate BMI. To focus on either children of normal weight or overweight children, as our primary exclusion criterion, we excluded thin or underweight children (BMI-for-age z-score (BAZ) < − 2SD); we also excluded children who did not live with their parents. The total number of children aged 6 − 12 years, as detected in IFLS-5, was 8780. After we filtered out all duplicated data (n = 455), missing data on the child’s weight and height (n = 1135), children classified as thin or underweight (n = 632), and children who did not live with their parents (n = 468), we had data available for analysis from 6,090 children.
Survey questions
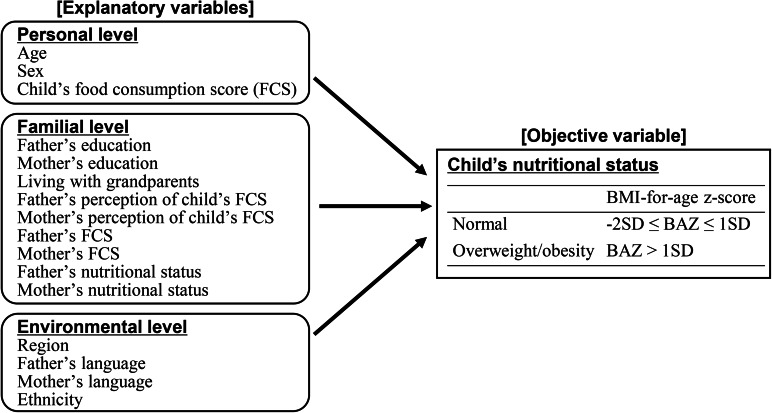
This study used a framework for understanding obesity in children and youth, [31] which explains that changes in individual characteristics are a result of multifactorial interactions, including personal factors (e.g., age, gender, and genetic profile), behavioral settings (e.g., home and school), and the environmental contexts in which people live. We focus on some variables from this framework that are available in a questionnaire from IFLS-5. We used survey questions to capture potential personal, familial, and environmental factors that could contribute to overweight and obesity in children. Figure 1 shows the conceptual framework of this study.
Fig. 1.
Conceptual framework for nutritional status and potential influencing factors among Indonesian children aged 6–12
The personal-level potential factors were the children’s age, sex, and food consumption score (FCS). The World Food Programme defines the FCS as “a score calculated using the frequency of consumption of different food groups consumed by a household during the 7 days before the survey,” noting “there are standard weights for each of the food groups that comprise the FCS” [32]. IFLS-5 documented consumption of 11 food items (leafy green vegetables, carrots, bananas, papayas, mangos, sweet potatoes, rice, meat, fish, eggs, and dairy) categorized into five groups: vegetables (green leafy vegetables and carrots), fruit (bananas, papayas, and mangos), staples (sweet potatoes and rice), protein (meat, fish, and eggs), and dairy. We categorized food consumption based on the FCS as poor (< 21), borderline (21–35), or acceptable (> 35) [33].
The family-level potential factors were the parents’ education, whether children lived with or without their grandparents, parents’ perceptions of their children’s food consumption as well as the parents’ FCS, and parents’ nutritional status. For education level, the questionnaire included a question on the highest level of education attained by the parents, and we grouped their responses into one of five categories: no school, primary school, middle school, high school, or higher education. There were four options in the question for parent’s perceptions of their children’s food consumption: “it is less than adequate for their needs,” “it is just adequate for their needs,” “it is more than adequate for their needs,” and “do not know.” We categorized parents’ FCS according to the World Food Programme scoring, and we classified parents’ BMI (body weight in kilograms divided by the square of body height in meters) as underweight (BMI < 18.5), normal (18.5 ≤ BMI < 25), overweight (25 ≤ BMI < 30), or obese (BMI ≥ 30) following the guidelines of the World Health Organization (WHO) [34].
For the potential environmental factors, we looked at the region and cultural diversity factors such as ethnicity and language. For region, we used the IFLS-5 question that asks whether respondents live in an urban or a rural area. Indonesia has approximately 1,300 ethnicities, [35] and IFLS-5 included a multiple-choice list for parents to choose from; for this study, we focused on the following 26 ethnicities: Sundanese, Acehnese, Ambon, Bali, Banjar, Banten, Batak, Betawi, Bima-Dompu, Bugis, Cirebon, Chinese, Dayak, Javanese, Komering, Maduranese, Makasar, Manado, Melayu, Minang, Nias, Palembang, Sasak, Sumbawa, Other Southern Sumatrans, and Toraja. We classified parents’ languages as Indonesian, other than Indonesian, or Indonesian and other languages. The category “other than Indonesian” includes local languages that participants used.
Weight and height were measured by the trained interviewers of IFLS-5. Interviewers learned how to take physical health measurements during training. Heights were measured using a Seca plastic height board, model 213, which measured children’s height to the nearest millimeter. Weights were measured using a Camry model EB1003 scale, which measured children’s weight to the nearest tenth of a kilogram [30]. We calculated the child’s BAZ using a method approved by the WHO and classified it as normal (− 2SD ≤ BAZ ≤ 1SD) or overweight/obese (BAZ > 1SD) [36]. In this study, we used the WHO 2007 R macro package to calculate children’s BAZ [37].
Statistical analysis
We conducted data analysis using the following steps. First, we calculated descriptive statistics for all variables. Then, we conducted bivariate analysis using t test and Fisher’s exact test to identify relationships between objective and explanatory variables, excluding variables with perfect separation (i.e., outcome variable separates a predictor variable completely) from the multivariate analyses. We deleted missing values listwise. Univariate and multivariate analysis was conducted by specifying logistic regression models. Crude and adjusted odds ratios (ORs and AORs) were calculated for each variable. We also computed adjusted generalized variance inflation factors (GVIFs) to detect potential multicollinearity in the models [38]. We set significance at p < 0.05 for the t test and Fisher’s exact test, and for the logistic regression models, we set significance at a 95% confidence interval (CI). We analyzed the data using R version 4.0.5 [39].
Results
Data gathered from 6,090 children aged 6–12 years that met inclusion criteria were analyzed. Table 1 shows the results of the descriptive and bivariate analysis of the children’s nutritional status and potential factors. The mean age was 8.9 years (SD = 2.0) (not presented in the table), and the sex ratio was 104. More than half of the participants lived in urban areas (59.5%). One-fifth of fathers (21.9%) and mothers (21.5%) spoke both Indonesian and other languages. The ethnic group with the highest proportion was Javanese (39.9%), followed by Sundanese (12.2%), Minang (6.1%), and Batak (6.0%). The percentages of overweight and obese children were 9.4% and 8.1%, respectively. Half of the mothers were overweight/obese (50.1%), while one-third of the fathers were overweight/obese (30.8%). In two-thirds of cases, the child’s FCS was acceptable (68.5%), but fewer fathers (61.6%) and mothers (54.8%) perceived that their child’s food consumption was just adequate for their needs.
Table 1.
Participants’ characteristics and bivariate analysis of child’s nutritional status and potential factors
| Child’s nutritional status | P-value | ||||||
|---|---|---|---|---|---|---|---|
| Total (n = 6090) |
Normal (n = 5022) |
Overweight/ obesity (n = 1068) |
|||||
| n | % | n | % | n | % | ||
| Personal level | |||||||
| Age (n = 6090) | |||||||
| 6 years old | 921 | 15.1 | 773 | 83.9 | 148 | 16.1 | 0.134 |
| 7 years old | 869 | 14.3 | 734 | 84.5 | 135 | 15.5 | |
| 8 years old | 918 | 15.1 | 768 | 83.7 | 150 | 16.3 | |
| 9 years old | 900 | 14.8 | 732 | 81.3 | 168 | 18.7 | |
| 10 years old | 858 | 14.1 | 698 | 81.4 | 160 | 18.6 | |
| 11 years old | 891 | 14.6 | 732 | 82.2 | 159 | 17.8 | |
| 12 years old | 733 | 12.0 | 585 | 79.8 | 148 | 20.2 | |
| Sex (n = 6090) | |||||||
| Boys | 3105 | 51.0 | 2535 | 81.6 | 570 | 18.4 | 0.890 |
| Girls | 2985 | 49.0 | 2487 | 83.3 | 498 | 16.7 | |
| Child’s FCS (n = 6079) | |||||||
| Acceptable (> 35) | 4166 | 68.5 | 3405 | 81.7 | 761 | 18.3 | 0.022 |
| Borderline (21–35) | 1720 | 28.3 | 1439 | 83.7 | 281 | 16.3 | |
| Poor (< 21) | 193 | 3.2 | 170 | 88.1 | 23 | 11.9 | |
| Familial level | |||||||
| Father’s education (n = 5452) | |||||||
| No school | 107 | 2.0 | 101 | 94.4 | 6 | 5.6 | < 0.001 |
| Primary school | 1703 | 31.2 | 1507 | 88.5 | 196 | 11.5 | |
| Middle school | 1056 | 19.3 | 900 | 85.2 | 156 | 14.8 | |
| High school | 1896 | 34.8 | 1513 | 79.8 | 383 | 20.2 | |
| Higher education | 690 | 12.7 | 492 | 71.3 | 198 | 28.7 | |
| Mother’s education (n = 5831) | |||||||
| No school | 120 | 2.0 | 109 | 90.8 | 11 | 9.2 | < 0.001 |
| Primary school | 1814 | 31.1 | 1585 | 87.4 | 229 | 12.6 | |
| Middle school | 1322 | 22.7 | 1141 | 86.3 | 181 | 13.7 | |
| High school | 1835 | 31.5 | 1439 | 78.4 | 396 | 21.6 | |
| Higher education | 740 | 12.7 | 532 | 71.9 | 208 | 28.1 | |
| Living with grandparents (n = 6081) | |||||||
| Yes | 1375 | 22.6 | 1121 | 81.5 | 254 | 18.5 | 0.294 |
| No | 4706 | 77.4 | 3895 | 82.8 | 811 | 17.2 | |
| Father’s perception of child’s food consumption (n = 4593) | |||||||
| Less than adequate | 679 | 14.8 | 635 | 93.5 | 44 | 6.5 | < 0.001 |
| Just adequate | 2831 | 61.6 | 2356 | 83.2 | 475 | 16.8 | |
| More than adequate | 1083 | 23.6 | 848 | 78.3 | 235 | 21.7 | |
| Mother’s perception of child’s food consumption (n = 5554) | |||||||
| Less than adequate | 648 | 11.7 | 587 | 90.6 | 61 | 9.4 | < 0.001 |
| Just adequate | 3046 | 54.8 | 2563 | 84.1 | 483 | 15.9 | |
| More than adequate | 1860 | 33.5 | 1456 | 78.3 | 404 | 21.7 | |
| Father’s FCS (n = 4639) | |||||||
| Acceptable (> 35) | 2884 | 62.2 | 2388 | 82.8 | 496 | 17.2 | 0.112 |
| Borderline (21–35) | 1586 | 34.2 | 1338 | 84.4 | 248 | 15.6 | |
| Poor (< 21) | 169 | 3.6 | 149 | 88.2 | 20 | 11.8 | |
| Mother’s FCS (n = 5589) | |||||||
| Acceptable (> 35) | 3354 | 60.0 | 2765 | 82.4 | 589 | 17.6 | 0.121 |
| Borderline (21–35) | 2037 | 36.5 | 1693 | 83.1 | 344 | 16.9 | |
| Poor (< 21) | 198 | 3.5 | 174 | 87.9 | 24 | 12.1 | |
| Father’s nutritional status (n = 4758) | |||||||
| Underweight | 344 | 7.2 | 322 | 93.6 | 22 | 6.4 | < 0.001 |
| Normal | 2949 | 62.0 | 2577 | 87.4 | 372 | 12.6 | |
| Overweight | 1202 | 25.3 | 909 | 75.6 | 293 | 24.4 | |
| Obesity | 263 | 5.5 | 167 | 63.5 | 96 | 36.5 | |
| Mother’s nutritional status (n = 5657) | |||||||
| Underweight | 207 | 3.7 | 167 | 80.7 | 40 | 19.3 | 0.011 |
| Normal | 2621 | 46.3 | 2209 | 84.3 | 412 | 15.7 | |
| Overweight | 1932 | 34.2 | 1582 | 81.9 | 350 | 18.1 | |
| Obesity | 897 | 15.9 | 716 | 79.8 | 181 | 20.2 | |
| Environmental level | |||||||
| Region (n = 6090) | |||||||
| Rural | 2467 | 40.5 | 2170 | 88.0 | 297 | 12.0 | < 0.001 |
| Urban | 3623 | 59.5 | 2852 | 78.7 | 771 | 21.3 | |
| Father’s language (n = 5051) | |||||||
| Indonesia | 733 | 14.5 | 558 | 76.1 | 175 | 23.9 | < 0.001 |
| Other | 3211 | 63.6 | 2765 | 86.1 | 446 | 13.9 | |
| Indonesia and other | 1107 | 21.9 | 881 | 79.6 | 226 | 20.4 | |
| Mother’s language (n = 5711) | |||||||
| Indonesia | 888 | 15.5 | 666 | 75.0 | 222 | 25.0 | < 0.001 |
| Other | 3600 | 63.0 | 3060 | 85.0 | 540 | 15.0 | |
| Indonesia and other | 1223 | 21.5 | 1002 | 81.9 | 221 | 18.1 | |
| Ethnicity (n = 6056) | |||||||
| Sundanese | 740 | 12.2 | 617 | 83.4 | 123 | 16.6 | < 0.001 |
| Acehnese | 11 | 0.2 | 5 | 45.5 | 6 | 54.5 | |
| Ambon | 2 | 0.0 | 2 | 100.0 | 0 | 0.0 | |
| Bali | 286 | 4.7 | 236 | 82.5 | 50 | 17.5 | |
| Banjar | 203 | 3.4 | 165 | 81.3 | 38 | 18.7 | |
| Banten | 24 | 0.4 | 24 | 100.0 | 0 | 0.0 | |
| Batak | 362 | 6.0 | 315 | 87.0 | 47 | 13.0 | |
| Betawi | 283 | 4.7 | 214 | 75.6 | 69 | 24.4 | |
| Bima-Dompu | 118 | 1.9 | 109 | 92.4 | 9 | 7.6 | |
| Bugis | 259 | 4.3 | 221 | 85.3 | 38 | 14.7 | |
| Cirebon | 2 | 0.0 | 0 | 0.0 | 2 | 100.0 | |
| Chinese | 14 | 0.2 | 8 | 57.1 | 6 | 42.9 | |
| Dayak | 3 | 0.0 | 2 | 66.7 | 1 | 33.3 | |
| Javanese | 2415 | 39.9 | 1919 | 79.5 | 496 | 20.5 | |
| Komering | 19 | 0.3 | 17 | 89.5 | 2 | 10.5 | |
| Maduranese | 135 | 2.2 | 117 | 86.7 | 18 | 13.3 | |
| Makasar | 123 | 2.0 | 109 | 88.6 | 14 | 11.4 | |
| Manado | 2 | 0.0 | 1 | 50.0 | 1 | 50.0 | |
| Melayu | 39 | 0.6 | 28 | 71.8 | 11 | 28.2 | |
| Minang | 368 | 6.1 | 305 | 82.9 | 63 | 17.1 | |
| Nias | 40 | 0.7 | 39 | 97.5 | 1 | 2.5 | |
| Palembang | 60 | 1.0 | 47 | 78.3 | 13 | 21.7 | |
| Sasak | 253 | 4.2 | 234 | 92.5 | 19 | 7.5 | |
| Sumbawa | 25 | 0.4 | 23 | 92.0 | 2 | 8.0 | |
| Other Southern Sumatrans | 234 | 3.9 | 203 | 86.8 | 31 | 13.2 | |
| Toraja | 36 | 0.6 | 33 | 91.7 | 3 | 8.3 | |
Fisher’s exact test. FCS: food consumption score
From the results of the bivariate analysis using t test (mean age) and Fisher’s exact test, 12 of 16 potential factors were related to the child’s nutritional status. The mean age of overweight/obese children was significantly higher than that of children of normal weight (9.1 vs. 8.9, p < 0.001) (not presented in the table). More overweight/obese children lived in urban areas than in rural areas (21.3% vs. 12.0%, p < 0.001). A higher prevalence of childhood overweight/obesity was associated with a higher educational level of the father (28.7%, p < 0.001) and mother (28.1%, p < 0.001). The prevalence was higher if the father (21.7%, p < 0.001) and mother (21.7%, p < 0.001) perceived their child as consuming more than an adequate amount of food. The higher prevalence was associated with an overweight (24.4%) and obese father (36.5%, p < 0.001), but it was also seen in underweight mothers (19.3%, p = 0.011). The prevalence was higher if language of the father (23.9%, p < 0.001) and mother (25.0%, p < 0.001) was the Indonesian language. Some ethnicities were prone to higher prevalence such as Acehnese with 54.5% (p < 0.001).
Table 2 shows the results of the logistic regression models. A univariate logistic regression revealed an association between the child’s nutritional status and 13 factors: age, child’s FCS, father’s and mother’s education, father’s and mother’s perception of the child’s food consumption, mother’s FCS, father’s and mother’s nutritional status, father’s and mother’s language, ethnicity, and region. A multivariate logistic regression revealed the association between the child’s nutritional status and six factors: age, father’s perception of the child’s food consumption, mother’s perception of the child’s food consumption, father’s nutritional status, ethnicity, and region. A higher risk of child overweight/obesity was associated with older age which increases age by each one year increased the odds being overweight or obese by 9% (AOR = 1.09, 95% CI: 1.04–1.14), an overweight father (AOR = 1.93, 95% CI: 1.58–2.36) or obese father (AOR = 3.36, 95% CI: 2.43–4.61), Chinese (AOR = 9.51, 95% CI: 1.43–79.43) or Javanese ethnicity (AOR = 1.60, 95% CI: 1.16–2.24), and residing in an urban area (AOR = 1.36, 95% CI: 1.10–1.70). In contrast, a lower risk of child overweight/obesity was associated with the father (AOR = 0.56, 95% CI: 0.38–0.80) and mother (AOR = 0.66, 95% CI: 0.43–0.98) perceiving their child’s food consumption as being less than adequate. The GVIF ranged from 1.01 to 1.23, indicating no multicollinearity between the explanatory variables.
Table 2.
Logistic regression model identifying factors associated with overweight/obesity among children
| Unadjusted | P-value | Adjusted | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||||||
| Personal level | |||||||||
| Agea | 1.06 | 1.01 | 1.10 | 0.014 | 1.09 | 1.04 | 1.14 | < 0.001 | |
| Sex | |||||||||
| Boys | 1.00 | (ref) | 1.00 | (ref) | |||||
| Girls | 0.89 | 0.75 | 1.06 | 0.191 | 0.94 | 0.79 | 1.13 | 0.537 | |
| Child’s FCS | |||||||||
| Acceptable | 1.00 | (ref) | 1.00 | (ref) | |||||
| Borderline | 0.82 | 0.67 | 0.99 | 0.042 | 0.97 | 0.78 | 1.22 | 0.813 | |
| Poor | 0.63 | 0.33 | 1.12 | 0.138 | 1.00 | 0.49 | 1.88 | 0.992 | |
| Familial level | |||||||||
| Father’s education | |||||||||
| No school | 1.00 | (ref) | 1.00 | (ref) | |||||
| Primary school | 2.83 | 1.03 | 11.66 | 0.081 | 2.41 | 0.82 | 10.33 | 0.159 | |
| Middle school | 3.16 | 1.14 | 13.10 | 0.055 | 2.23 | 0.74 | 9.69 | 0.205 | |
| High school | 5.84 | 2.15 | 24.00 | 0.003 | 3.06 | 1.03 | 13.26 | 0.076 | |
| Higher education | 8.43 | 3.07 | 34.85 | < 0.001 | 3.45 | 1.12 | 15.17 | 0.054 | |
| Mother’s education | |||||||||
| No school | 1.00 | (ref) | 1.00 | (ref) | |||||
| Primary school | 1.10 | 0.55 | 2.53 | 0.802 | 0.65 | 0.30 | 1.58 | 0.303 | |
| Middle school | 1.26 | 0.62 | 2.90 | 0.553 | 0.61 | 0.28 | 1.51 | 0.254 | |
| High school | 2.22 | 1.12 | 5.07 | 0.035 | 0.81 | 0.36 | 2.02 | 0.634 | |
| Higher education | 2.85 | 1.41 | 6.58 | 0.007 | 0.76 | 0.33 | 1.94 | 0.534 | |
| Living with grandparents | |||||||||
| No | 1.00 | (ref) | 1.00 | (ref) | |||||
| Yes | 1.16 | 0.93 | 1.43 | 0.177 | 1.10 | 0.87 | 1.38 | 0.438 | |
| Father’s perception of child’s food consumption | |||||||||
| Less than adequate | 0.36 | 0.25 | 0.50 | < 0.001 | 0.56 | 0.38 | 0.80 | 0.002 | |
| Just adequate | 1.00 | (ref) | 1.00 | (ref) | |||||
| More than adequate | 1.38 | 1.14 | 1.67 | < 0.001 | 1.00 | 0.81 | 1.24 | 0.976 | |
| Mother’s perception of child’s food consumption | |||||||||
| Less than adequate | 0.40 | 0.27 | 0.58 | < 0.001 | 0.66 | 0.43 | 0.98 | 0.043 | |
| Just adequate | 1.00 | (ref) | 1.00 | (ref) | |||||
| More than adequate | 1.56 | 1.30 | 1.86 | < 0.001 | 1.17 | 0.96 | 1.43 | 0.128 | |
| Father’s FCS | |||||||||
| Acceptable | 1.00 | (ref) | 1.00 | (ref) | |||||
| Borderline | 0.88 | 0.73 | 1.06 | 0.184 | 0.99 | 0.81 | 1.22 | 0.938 | |
| Poor | 0.64 | 0.36 | 1.06 | 0.099 | 1.04 | 0.57 | 1.80 | 0.890 | |
| Mother’s FCS | |||||||||
| Acceptable | 1.00 | (ref) | 1.00 | (ref) | |||||
| Borderline | 0.93 | 0.77 | 1.11 | 0.398 | 1.01 | 0.82 | 1.25 | 0.892 | |
| Poor | 0.48 | 0.24 | 0.85 | 0.020 | 0.80 | 0.38 | 1.50 | 0.506 | |
| Father’s nutritional status | |||||||||
| Underweight | 0.36 | 0.20 | 0.62 | < 0.001 | 0.41 | 0.22 | 0.70 | 0.002 | |
| Normal | 1.00 | (ref) | 1.00 | (ref) | |||||
| Overweight | 2.38 | 1.97 | 2.87 | < 0.001 | 1.93 | 1.58 | 2.36 | < 0.001 | |
| Obesity | 4.09 | 3.01 | 5.53 | < 0.001 | 3.36 | 2.43 | 4.61 | < 0.001 | |
| Mother’s nutritional status | |||||||||
| Underweight | 1.39 | 0.88 | 2.12 | 0.142 | 1.31 | 0.81 | 2.07 | 0.257 | |
| Normal | 1.00 | (ref) | 1.00 | (ref) | |||||
| Overweight | 1.24 | 1.02 | 1.50 | 0.032 | 1.15 | 0.94 | 1.41 | 0.180 | |
| Obesity | 1.37 | 1.07 | 1.74 | 0.012 | 1.21 | 0.93 | 1.57 | 0.149 | |
| Environmental level | |||||||||
| Region | |||||||||
| Rural | 1.00 | (ref) | 1.00 | (ref) | |||||
| Urban | 2.17 | 1.80 | 2.62 | < 0.001 | 1.36 | 1.10 | 1.70 | 0.005 | |
| Father’s language | |||||||||
| Indonesia | 1.00 | (ref) | 1.00 | (ref) | |||||
| Other | 0.54 | 0.43 | 0.69 | < 0.001 | 0.84 | 0.60 | 1.18 | 0.317 | |
| Indonesia and other | 0.83 | 0.64 | 1.09 | 0.176 | 0.99 | 0.72 | 1.35 | 0.941 | |
| Mother’s language | |||||||||
| Indonesia | 1.00 | (ref) | 1.00 | (ref) | |||||
| Other | 0.53 | 0.42 | 0.66 | < 0.001 | 0.83 | 0.60 | 1.16 | 0.280 | |
| Indonesia and other | 0.64 | 0.49 | 0.83 | <0.001 | 0.75 | 0.54 | 1.03 | 0.074 | |
| Ethnicity | |||||||||
| Sundanese | 1.00 | (ref) | 1.00 | (ref) | |||||
| Aceh | 6.76 | 0.80 | 57.31 | 0.058 | 5.67 | 0.63 | 52.11 | 0.100 | |
| Bali | 1.55 | 0.98 | 2.44 | 0.057 | 1.40 | 0.85 | 2.26 | 0.179 | |
| Banjar | 1.68 | 1.01 | 2.73 | 0.040 | 1.70 | 0.99 | 2.88 | 0.051 | |
| Batak | 0.73 | 0.43 | 1.20 | 0.226 | 0.70 | 0.40 | 1.19 | 0.198 | |
| Betawi | 2.57 | 1.65 | 4.00 | < 0.001 | 1.62 | 1.00 | 2.61 | 0.048 | |
| Bima-dompu | 0.27 | 0.06 | 0.75 | 0.029 | 0.41 | 0.10 | 1.21 | 0.156 | |
| Bugis | 1.02 | 0.59 | 1.71 | 0.944 | 1.20 | 0.67 | 2.09 | 0.527 | |
| Chinese | 10.15 | 1.65 | 78.32 | 0.012 | 9.51 | 1.43 | 79.43 | 0.020 | |
| Javanese | 1.64 | 1.21 | 2.26 | 0.001 | 1.60 | 1.16 | 2.24 | 0.004 | |
| Komering | 1.04 | 0.16 | 3.90 | 0.958 | 1.36 | 0.20 | 5.37 | 0.696 | |
| Maduranese | 1.14 | 0.54 | 2.23 | 0.704 | 1.33 | 0.60 | 2.73 | 0.462 | |
| Makasar | 0.80 | 0.36 | 1.62 | 0.560 | 0.85 | 0.37 | 1.79 | 0.682 | |
| Melayu | 1.42 | 0.40 | 3.96 | 0.534 | 1.24 | 0.34 | 3.64 | 0.711 | |
| Minang | 1.37 | 0.86 | 2.14 | 0.175 | 1.12 | 0.69 | 1.80 | 0.650 | |
| Nias | 0.25 | 0.01 | 1.21 | 0.178 | 0.66 | 0.04 | 3.41 | 0.689 | |
| Palembang | 1.87 | 0.76 | 4.12 | 0.141 | 1.81 | 0.69 | 4.30 | 0.198 | |
| Sasak | 0.59 | 0.31 | 1.06 | 0.090 | 0.63 | 0.32 | 1.17 | 0.161 | |
| Sumbawa | 0.34 | 0.02 | 1.67 | 0.294 | 0.35 | 0.02 | 1.86 | 0.321 | |
| Other Southern Sumatrans | 0.87 | 0.50 | 1.46 | 0.598 | 1.09 | 0.61 | 1.90 | 0.755 | |
| Toraja | 1.27 | 0.29 | 3.96 | 0.712 | 1.14 | 0.25 | 3.83 | 0.850 | |
a Numerical data. Outcome variable: nutritional status of overweight/obese child (normal-weight child = reference). OR: odds ratio, CI: confidence interval
Discussion
This study revealed a childhood overweight/obesity rate of 17.5% among Indonesian children aged 6–12 years. This prevalence has increased in Indonesia since 2007 (12.8%) [17]. The increasing trend indicates a need to address and control Indonesia’s rate of overweight and obesity among children.
One personal factor we identified as being associated with a higher risk of childhood overweight and obesity was the child’s age. This study used BAZ to classify the child’s nutritional status. Although we adjusted BMI by age, it was associated with overweight and obesity, possibly because, as they age, children make more independent decisions [40]. In Indonesia, primary school students have a high exposure to less nutritious foods, [4, 17, 41] and are less physically active, [4] and it is challenging for children who have only begun to develop their own decision-making skills to make good food choices. Thus, high exposure to less nutritious food with less physical activity increases the likelihood that children will consume these foods, leading them to become overweight and obese.
Family factors that were associated with childhood overweight and obesity were having an overweight or obese father and parents’ perceptions of their children’s food consumption. In this study, children of overweight or obese fathers were two to four times more likely to be overweight or obese themselves, consistent with a systematic review and meta-analysis from HICs, middle-income countries, and one low-income country in which child obesity was associated with overweight or obesity among fathers [22]. The elevated risk is likely attributable to the combination of genetic predisposition and shared environmental factors. However, according to social learning theory, parents’ actions directly influence their children’s behaviors through experience and observations, [42] and some children likely imitate their parents’ obesity-promoting behaviors.
Whereas a significant association exists between paternal and childhood overweight/obesity, no such association has been found between maternal and childhood overweight/obesity. A qualitative study conducted in Indonesia [43] revealed that fathers have described themselves as more permissive, whereas mothers tend to be more overprotective. Meanwhile, a nine-year prospective cohort study found that authoritative parenting was perceived as more successful at preventing children from increased BMI than permissive parenting [44]. According to social learning theory, [42] children imitate each other’s behavior through a process known as reproduction. Indonesian fathers tend to have more permissive parenting styles, and they also tend to indulge their children by giving them everything they need. This may give children more opportunity to replicate their fathers’ obesity-promoting behavior in the reproduction process. In addition, Javanese fathers are expected to be imitation models for their children, [45] which made fathers the main models for the children’s behavior. This mechanism might explain why different studies have reached different results concerning the association between parental nutritional status and overweight/obesity among children in Indonesia.
We also found that parents who perceived their children as having less than adequate food consumption tended to have children with normal weight. Studies have demonstrated unique cultural perceptions; for example, Indonesian adults often found overweight children to be “cute[r],” “health[ier],” and “funn[ier]” [46, 47]. These culturally held beliefs may contribute to childhood overweight/obesity, as overweight children may be more appealing. Additionally, significant familial variation exists in the definition of a healthy diet [48].
We also found some environmental factors to be associated with childhood overweight/obesity, specifically, living in an urban area and being of Chinese or Javanese ethnicity. Understanding cultural differences in eating habits could elucidate this finding. Apart from providing sustenance, food plays a social and cultural role by establishing and maintaining interpersonal relationships. For example, Chinese mothers in China often use sweets and desserts as rewards for their children, [49] and excessive consumption of sweet foods potentially contributes to the increased overweight and obesity that we observed among Chinese children in Indonesia. Similarly, a nationwide health survey in Indonesia found that Javanese people (who live in Central Java province, East Java province, and the Special Region of DI Yogyakarta) consumed more sweets per day than did Sundanese people (who live in West Java province) [50]. Indeed, the cuisine of Central Java, where 70% of the inhabitants are ethnic Javanese, tends to be very sweet [51]. Meanwhile, findings from a cross-sectional study conducted in England corroborated possible associations between childhood overweight and obesity and ethnic and cultural factors [52].
We also found that children living in urban areas were 1.36 times more likely to be overweight or obese than were children living in rural areas, and this finding was consistent with findings from studies conducted in Indonesia and China [53, 54]. Urban areas are considered obesogenic environments with high access to less nutritious foods [25]. Additionally, data from the Indonesian National Health Survey revealed that people from urban environments more often had sedentary lifestyles than did people from rural environments [50].
Results of this study will afford better understanding of children, familial, and environmental characteristics in Indonesia, which public health nurses can use to provide health promotion and intervention programs for those who suffer from nutritional problems. Moreover, our study found that fathers play an important role in influencing overweight and obesity among children in Indonesia. While health education was traditionally provided only for women and children in Indonesia, future prevention strategies to overcome overweight and obesity among children must also include fathers. The implication of this study is that urban areas could become targeted areas for future intervention or prevention. However, Indonesia has regional disparities that lead to huge gaps in socioeconomic development between western Indonesia and central/eastern Indonesia. For a more targeted approach, future studies also need to capture socioeconomic differences at the regional level that might also contribute to childhood overweight and obesity.
This study is the first of its kind to provide data on personal, familial, and environmental factors associated with childhood overweight and obesity in Indonesia using national data. This study has several potential limitations. First, it used self-reported questionnaire data from IFLS, which may introduce bias. Questions in the survey addressing parents’ perceptions about their children’s food consumption may be biased. Parents were asked to subjectively qualify their children’s eating habits as less than adequate, just adequate, or more than adequate. It is unclear how parents who participated in this questionnaire define each category on perception about children’s food consumption that could lead to misclassification. Second, we were not able to determine causal relationships between childhood overweight and obesity and the factors we studied because of the cross-sectional study design. Third, although one ethnicity showed an association with childhood overweight/obesity, this association was present only in a small sample; thus, the result may not be replicated in other studies. Fourth, we were unable to include some potentially confounding variables (e.g., family income, physical activity, and sugar-beverage consumption) because they were either inconsistent or unavailable in the IFLS-5 data. Fifth, we did not incorporate sample weight in the analysis, which means that this study cannot clearly explain the extent to which its results represent the total Indonesian population. Although the baseline sample in the IFLS-1 represents 83% of the Indonesian population, decreasing the recontact rate of original households in 1993 [30] could lead to a decrease in representativeness. In addition, we included in the multivariate analysis only participants with complete data. Some characteristics significantly differed between data included in and excluded from the analysis (data not shown). Finally, differences in participants’ characteristics potentially led to selection bias.
Conclusions
Among children aged 6–12 years in Indonesia, overweight/obesity was associated with the following personal, familial, and environmental risk factors: age, overweight or obese father, ethnicity (i.e., Chinese and Javanese), and living in an urban area. Normal childhood weight was associated with parents’ perceptions that children’s food consumption was less than adequate. Targeting the different factors we identified as significant on multiple levels could be a critical first step in increasing community-wide insight and improving nursing approaches to preventing primary childhood overweight and obesity.
Acknowledgements
We are grateful to the participants who joined IFLS-5 in 2014/2015. We also would like to thank RAND Corporation for providing access to the IFLS data. This work is part of a master’s thesis submitted to Mie University Graduate School of Medicine, Japan.
Abbreviations
- BMI
body mass index
- IFLS
Indonesia Family Life Survey
- FCS
food consumption score
- WHO
World Health Organization
- OR
odds ratio
- AOR
adjusted odds ratio
- GVIF
generalized variance inflation factor
- CI
confidence interval
Authors’ contributions
SO, MM, RN, and ST contributed to conception and design. SO performed data cleaning. SO, MM, and ST conducted data analyses. SO, MM, RN, and ST interpreted the results. MM supervised the whole project. SO and MM drafted the manuscripts, and all authors revised it critically. All authors have read and approved the final manuscript.
Funding
This study did not receive any specific grant from a public or private organization.
Data availability
The datasets are available upon registration on the website of the RAND Corporation (https://www.rand.org/well-being/social-and-behavioral-policy/data/FLS/IFLS.html).
Declarations
Ethical approval and consent to participate
The IFLS-5 was reviewed and approved by the Institutional Review Boards of RAND Corporation in the United States (No. s0064-06-01-CR01). One or two household members were asked to provide information at the household level. The interviewers conducted an interview with every individual aged 11 and above. For children less than 11, interviewers interviewed their parent or caretaker. Informed consent was obtained from all subjects and/or their parents/guardians [30]. Ethical clearance for this study was received from the Clinical Research Ethics Review Committee of Mie University Hospital (No. U2021-011). The study procedure was performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zellner K, Ulbricht G, Kromeyer-Hauschild K. Long-term trends in body mass index of children in Jena, Eastern Germany. Econ Hum Biol. 2007;5:426–34. doi: 10.1016/j.ehb.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. doi: 10.1542/peds.101.S2.497. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Prevalence of overweight among children and adolescents, BMI > + 1 standard deviations above the median, crude. https://apps.who.int/gho/data/view.main.BMIPLUS1C05-19v?lang=en. Accessed 23 Sep 2023.
- 4.Kementrian Kesehatan Republik Indonesia [Indonesian Ministry of Health]. Laporan nasional riskesdas 2018 [Basic health research report 2018]. 2019. https://repository.badankebijakan.kemkes.go.id/id/eprint/3514/. Accessed 23 Sep 2023.
- 5.Williams DP, Going SB, Lohman TG, Harsha DW, Srinivasan SR, Webber LS, et al. Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am J Public Health. 1992;82:358–63. doi: 10.2105/AJPH.82.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–82. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 7.Raj M, Sundaram KR, Paul M, Deepa AS, Kumar RK. Obesity in indian children: time trends and relationship with hypertension. Natl Med J India. 2007;20:288–93. [PubMed] [Google Scholar]
- 8.I’Allemand D, Wiegand S, Reinehr T, Muller J, Wabitsch M, Widhalm K, et al. Cardiovascular risk in 26,008 european overweight children as established by a multicenter database. Obes (Silver Spring) 2008;16:1672–9. doi: 10.1038/oby.2008.259. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell RB, Kelly J. Outcome of adenotonsillectomy for obstructive sleep apnea in obese and normal-weight children. Otolaryngol Head Neck Surg. 2007;137:43–8. doi: 10.1016/j.otohns.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 10.Nogueira-de-Almeida CA, Del Ciampo LA, Ferraz IS, Del Ciampo IRL, Contini AA, Ued FDV. COVID-19 and obesity in childhood and adolescence: a clinical review. J Pediatr (Rio J) 2020;96:546–58. doi: 10.1016/j.jped.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. 2021;4:e2111182. doi: 10.1001/jamanetworkopen.2021.11182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tripathi S, Christison AL, Levy E, McGravery J, Tekin A, Bolliger D, et al. The impact of obesity on disease severity and outcomes among hospitalized children with COVID-19. Hosp Pediatr. 2021;11:e297–e316. doi: 10.1542/hpeds.2021-006087. [DOI] [PubMed] [Google Scholar]
- 13.Guo SS, Chumlea WC. Tracking of body mass index in children in relation to overweight in adulthood. Am J Clin Nutr. 1999;70:145S–8S. doi: 10.1093/ajcn/70.1.145s. [DOI] [PubMed] [Google Scholar]
- 14.Lindberg L, Danielsson P, Persson M, Marcus C, Hagman E. Association of childhood obesity with risk of early all-cause and cause-specific mortality: a swedish prospective cohort study. PLoS Med. 2020;17:e1003078. doi: 10.1371/journal.pmed.1003078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Institute of Medicine (U.S.) Perspectives on the prevention of childhood obesity in children and youth. Washington (DC): National Academies Press; 2006. [Google Scholar]
- 16.Liberali R, Kupek E, Assis MAA. Dietary patterns and childhood obesity risk: a systematic review. Child Obes. 2020;16:70–85. doi: 10.1089/chi.2019.0059. [DOI] [PubMed] [Google Scholar]
- 17.Oddo VM, Maehara M, Rah JH. Overweight in Indonesia: an observational study of trends and risk factors among adults and children. BMJ Open. 2019;9: e031198. [DOI] [PMC free article] [PubMed]
- 18.Hadi H, Nurwanti E, Gittelsohn J, Arundhana AI, Astiti D, West KP Jr., et al. Improved understanding of interactions between risk factors for child obesity may lead to better designed prevention policies and programs in Indonesia. Nutrients. 2020;12:175. [DOI] [PMC free article] [PubMed]
- 19.Syahrul S, Kimura R, Tsuda A, Susanto T, Saito R, Ahmad F. Prevalence of underweight and overweight among school-aged children and it’s association with children’s sociodemographic and lifestyle in Indonesia. Int J Nurs Sci. 2016;3:169–77. [Google Scholar]
- 20.Lamerz A, Kuepper-Nybelen J, Wehle C, Bruning N, Trost-Brinkhues G, Brenner H, et al. Social class, parental education, and obesity prevalence in a study of six-year-old children in Germany. Int J Obes (Lond) 2005;29:373–80. doi: 10.1038/sj.ijo.0802914. [DOI] [PubMed] [Google Scholar]
- 21.Muthuri SK, Onywera VO, Tremblay MS, Broyles ST, Chaput JP, Fogelholm M, et al. Relationships between parental education and overweight with childhood overweight and physical activity in 9–11 year old children: results from a 12-country study. PLoS ONE. 2016;11:e0147746. doi: 10.1371/journal.pone.0147746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JS, Jin MH, Lee HJ. Global relationship between parent and child obesity: a systematic review and meta-analysis. Clin Exp Pediatr. 2022;65:35–46. doi: 10.3345/cep.2020.01620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tang D, Bu T, Dong X. Are parental dietary patterns associated with children’s overweight and obesity in China? BMC Pediatr. 2020;20:12. doi: 10.1186/s12887-020-1910-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson JA 3rd, Johnson AM. Urban-rural differences in childhood and adolescent obesity in the United States: a systematic review and meta-analysis. Child Obes. 2015;11:233–41. [DOI] [PubMed]
- 25.Nurwanti E, Hadi H, Chang JS, Chao JC, Paramashanti BA, Gittelsohn J, et al. Rural-urban differences in dietary behavior and obesity: results of the Riskesdas study in 10-18-year-old indonesian children and adolescents. Nutrients. 2019;11:2813. doi: 10.3390/nu11112813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arcan C, Culhane-Pera KA, Pergament S, Rosas-Lee M, Xiong MB. Somali, latino and Hmong parents’ perceptions and approaches about raising healthy-weight children: a community-based participatory research study. Public Health Nutr. 2018;21:1079–93. doi: 10.1017/S1368980017001719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oktaviani S, Mizutani M, Nishide R, Tanimura S. Prevalence of obesity and overweight stratified by age group of the 34 provinces in Indonesia: local empirical bayesian estimation. Asian Community Health Nursing Research. 2021;3:15–21. [Google Scholar]
- 28.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child. 1995;73:25–9. doi: 10.1136/adc.73.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strauss J, Witoelar F, Sikoki B. The fifth wave of the Indonesia Family Life Survey: overview and field report. 2016. https://www.rand.org/pubs/working_papers/WR1143z1.html. Accessed 12 Oct 2020.
- 31.Koplan JP, Liverman CT, Kraak VI, editors. Preventing childhood obesity: health in the balance. Washington (DC): National Academies Press (US); 2005. [PubMed] [Google Scholar]
- 32.World Food Program. Meta data for the food consumption score (FCS) indicator. 2015. https://www.wfp.org/publications/meta-data-food-consumption-score-fcs-indicator. Accessed 13 Jan 2021.
- 33.Isaura ER, Chen YC, Yang SH. The association of food consumption scores, body shape index, and hypertension in a seven-year follow-up among indonesian adults: a longitudinal study. Int J Environ Res Public Health. 2018;15:175. doi: 10.3390/ijerph15010175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization. Body mass index (BMI). https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index. Accessed 1 Oct 2021.
- 35.Badan Pusat Statistik [the Central Bureau of Statistics]. Kewarganegaraan, suku bangsa, agama, dan bahasa sehari-hari penduduk Indonesia: hasil sensus penduduk 2010 [Nationality, ethnicity, religion, and daily language of Indonesian population: the 2010 people census result]. 2011. https://www.bps.go.id/website/pdf_publikasi/watermark%20_Kewarganegaraan%2C%20Suku%20Bangsa%2C%20Agama%20dan%20Bahasa_281211.pdf. Accessed 30 Jan 2022.
- 36.World Health Organization. BMI-for-age (5–19 years). https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age. Accessed Nov 2022.
- 37.World Health Organization. WHO 2007 R macro package. https://www.who.int/docs/default-source/child-growth/growth-reference-5-19-years/readme-r.pdf?sfvrsn=6155b518_2. Accessed 9 Jun 2021.
- 38.Fox J, Monette G. Generalized collinearity diagnostics. J Am Stat Assoc. 1992;87:178–83. doi: 10.1080/01621459.1992.10475190. [DOI] [Google Scholar]
- 39.R Core Team. The R project for statistical computing. https://www.R-project.org/. Accessed 16 Nov 2022.
- 40.Malik F, Marwaha R. Developmental stages of social emotional development in children. Treasure Island (FL). StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK534819/#!po=95.4545.
- 41.Febriani D, Sudarti T. Fast food as drivers for overweight and obesity among urban school children at Jakarta, Indonesia. J Gizi Pangan. 2019:99–106.
- 42.Bandura A. Social learning theory. New Jersey: Prentice-Hall; 1977. [Google Scholar]
- 43.Setiawan JL, Widhigdo JC, Teonata A, Indriati L, Engel MM. Understanding the issues of co-parenting in Indonesia. J Educational Health Community Psychol. 2022;11:588–607. doi: 10.12928/jehcp.v11i3.24574. [DOI] [Google Scholar]
- 44.Lane SP, Bluestone C, Burke CT. Trajectories of BMI from early childhood through early adolescence: SES and psychosocial predictors. Br J Health Psychol. 2013;18:66–82. doi: 10.1111/j.2044-8287.2012.02078.x. [DOI] [PubMed] [Google Scholar]
- 45.Geertz H. The javanese family: a study of kinship and socialization. Glencoe (IL): Free Press; 1961. [Google Scholar]
- 46.Leonita EN. Persepsi ibu terhadap obesitas pada anak sekolah dasar [Perception of mothers about obesity in elementary school students] Jurnal Kesehatan Komunitas. 2010;1:39–48. doi: 10.25311/keskom.Vol1.Iss1.9. [DOI] [Google Scholar]
- 47.Rachmi CN, Hunter CL, Li M, Baur LA. Perceptions of overweight by primary carers (mothers/grandmothers) of under five and elementary school-aged children in Bandung, Indonesia: a qualitative study. Int J Behav Nutr Phys Activity. 2017;14:101. doi: 10.1186/s12966-017-0556-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adamo KB, Brett KE. Parental perceptions and childhood dietary quality. Matern Child Health J. 2014;18:978–95. doi: 10.1007/s10995-013-1326-6. [DOI] [PubMed] [Google Scholar]
- 49.Ma Gs Food, eating behavior, and culture in chinese society. J Ethnic Foods. 2015;2:195–9. doi: 10.1016/j.jef.2015.11.004. [DOI] [Google Scholar]
- 50.Kementerian Kesehatan Republik Indonesia [Indonesian Ministry of Health]. Riset kesehatan dasar 2013 [Basic health research 2013]. 2013. https://repository.badankebijakan.kemkes.go.id/id/eprint/4467/. Accessed 23 Sep 2023.
- 51.Wijaya S. Indonesian food culture mapping: a starter contribution to promote indonesian culinary tourism. J Ethnic Foods. 2019;6:1–10. doi: 10.1186/s42779-019-0009-3. [DOI] [Google Scholar]
- 52.Murphy M, Rebbeca J, Parsons NR, Robertson W. Understanding local ethnic inequalities in childhood BMI through cross-sectional analysis of routinely collected local data. BMC Public Health. 2019;19:1–15. doi: 10.1186/s12889-019-7870-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sandjaja S, Budiman B, Harahap H, Ernawati F, Soekatri M, Widodo Y, et al. Food consumption and nutritional and biochemical status of 0.5-12-year-old indonesian children: the SEANUTS study. Br J Nutr. 2013;110(Suppl 3):11–20. doi: 10.1017/S0007114513002109. [DOI] [PubMed] [Google Scholar]
- 54.Dong YH, Ma YH, Dong B, Zou ZY, Hu PJ, Wang ZH et al. Geographical variation and urban-rural disparity of overweight and obesity in chinese school-aged children between 2010 and 2014: two successive national cross-sectional surveys. BMJ Open. 2019;9: e025559. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets are available upon registration on the website of the RAND Corporation (https://www.rand.org/well-being/social-and-behavioral-policy/data/FLS/IFLS.html).