Abstract
Intellectual capital is a scarce resource in the healthcare industry. Making the most of this resource is the first step toward achieving a completely intelligent healthcare system. However, most existing centralized and deep learning-based systems are unable to adapt to the growing volume of global health records and face application issues. To balance the scarcity of healthcare resources, the emerging trend of IoMT (Internet of Medical Things) and edge computing will be very practical and cost-effective. A full examination of the transformational role of intelligent edge computing in the IoMT era to attain health care equity is offered in this research. Intelligent edge computing-aided distribution and collaborative information management is a possible approach for a long-term digital healthcare system. Furthermore, IEC (Intelligent Edge Computing) encourages digital health data to be processed only at the edge, minimizing the amount of information exchanged with central servers/the internet. This significantly increases the privacy of digital health data. Another critical component of a sustainable healthcare system is affordability in digital healthcare. Affordability in digital healthcare is another key component of a sustainable healthcare system. Despite its importance, it has received little attention due to its complexity. In isolated and rural areas where expensive equipment is unavailable, IEC with AR / VR, also known as edge device shadow, can play a significant role in the inexpensive data collection process. Healthcare equity becomes a reality by combining intelligent edge device shadows and edge computing.
Keywords: internet of things, machine learning, distributed computing, equitable healthcare, digital health
Introduction
The healthcare sector is undergoing a major transformation as new technologies such as artificial intelligence (AI), the internet of things (IoT), and augmented reality/virtual reality (AR/VR) are enabling more efficient, effective, and personalized care delivery. However, these technologies also pose significant challenges in terms of data management, security, privacy, interoperability, and scalability. Moreover, there are persistent inequalities in healthcare access and outcomes across different regions, populations, and socioeconomic groups. Intelligent healthcare is one of the major components of a smart urban environment. Smart healthcare developed from the aim to improve the management of the health sector, make more efficient use of its capabilities, and reduce its cost while maintaining or even enhancing its quality. In contrast, non-consumable resources are items that do not expire with time. Human resources, including physicians, pharmacists, and nurse practitioners, as well as the entire human capital involved in the medical process, constitute non-consumable assets. Intellectual capital in the medical business is an extremely expensive resource, and using this resource effectively is a must for a fully intelligent medical system. A sophisticated healthcare system is necessary in modern society. The technologies of artificial intelligence, the internet of things, and big data, among others, are crucial to the development of a smart and intelligent healthcare system. The creation of an intelligent healthcare system not only provides diagnosis and care to a greater number of patients, but also minimizes the burden of health professionals. Smart medical systems may deliver more sophisticated and accessible services and programs as technology advances.
From establishing a diagnosis to giving treatments, healthcare has always been guided by statistics. Due to the capabilities of machine learning and the Internet of Things, the medical industry is making significant progress in the collecting and processing of high-quality data. IoT is a device (or group of sensors) that communicates to the internet, enabling data to be delivered to whoever needs it. On a broad scale, the IoT comprises millions of sensors and equipment that send a constant flow of data, for example in a distribution chain. Faster accessibility, more precise, and real-time data facilitate decision-making for decision-makers in every sector. The IoT in healthcare is also characterized by an increased reliance on big data, which combines internal as well as external data from multiple sources, to improve the decision-making process. “Healthcare’s Equitability” is self-explanatory; it attempts to ensure that every person has access to cost-effective, culturally relevant healthcare irrespective of Race, Ethnicity, Gender, Sexual orientation, Age, origin, location, and economic/social status. However, the difficulty persists in the appropriate implementation of an ideal strategy that will guarantee underprivileged individuals get equal healthcare services. The digital approach seems to promise in this regard. Teleconsultation and remote diagnostics may eliminate geographical constraints and give rural populations enough access. Health professionals refer to inequalities in healthcare as health disparities. A health disparity is a difference in health resulting from unfair socioeconomic or environmental inequality. Health disparities harm communities facing bigger social or economic issues. Regarding discrepancies in health care, race is not the only determinant. In addition, disadvantaged individuals may face other obstacles while attempting to get health care. This includes discrimination, a lack of affordable treatment options, and living far from treatment centers. Mobile medical centers consisting of vans furnished with medical equipment may assist in increasing access, hence promoting equality in rural areas.
Typically, establishing equity in healthcare coverage necessitates the elimination or lowering of barriers to a person’s economic and social resources that affect their health. Some specific ways to do this could include Expanding access to healthcare via the implementation of mobile health centers or telemedicine initiatives, including such virtual healthcare services. Rising healthcare translations is one way to promote culturally responsive care. Endorsing policies that mitigate the damage done by racial injustice, misogyny, and discrimination as well as other forms of injustice, which hinder medical outcomes. When quantifying healthcare accessibility, the socioeconomic factors of well-being are often considered. Using social determinants of the healthcare framework, healthcare providers may investigate the external factors that impact the health of a certain individual.
The pandemic forced global decision-makers, medical experts, and the public at large to consider digital healthcare more significantly. Currently, it is rapidly transitioning from a decision made by a tiny percentage of individuals to the most popular option for treatment. The solution to the world’s unequal access to healthcare lies in technological progress. Where a lack of knowledge, accessibility, and cost are the primary causes of this imbalance, the solution is becoming the method for addressing it. And over 75% of health personnel are present in metropolitan regions where less than 30% of the community resides to address the concerns. Moreover, 70% of the rural population suffers from a chronic shortage of primary healthcare services. And as a result, rural communities must rely on quacks and unskilled practitioners to treat their ailments and symptoms until they develop serious disorders. Discrimination against racial and ethical minorities causes a decline in their health, which is exacerbated if they reside in rural locations. Remote monitoring-based diagnostic provides patients with rapid, accurate vital checks and instantaneous findings, regardless of their location. Digital health not just offers clinicians a more comprehensive perspective of patient health via data access, but also significantly improves the prevention of disease, diagnosis, and administration, resulting in enhanced care delivery results.
By combining intelligent edge computing and AR/VR, we envision a smart healthcare system that can provide equitable care to all individuals, particularly those in remote or rural areas where conventional healthcare facilities may be scarce or inaccessible. This system would collect and analyze health data from various sources using edge devices equipped with AI capabilities. It would then provide timely and personalized feedback, guidance, and intervention to users through AR/VR devices connected to edge devices. Additionally, the system would enable remote collaboration and consultation among users, healthcare providers, and experts through AR/VR platforms supported by edge computing. Digital technologies may enhance equality by extending access to healthcare, solving unmet medical needs, customizing treatment for patients, and considering the historical background of the communities that they serve. Digital technology is transforming the healthcare business from a responsive to a proactive one, expanding the availability of high-quality treatment for previously disadvantaged or marginalized populations. All of these benefits extend beyond the fact that digital health enables it possible to serve previously subject-to-discrimination groups while maintaining the same grade of high-end health centers. Virtual health’s complete capacity resides in its capacity to progress race-related, sex, and age-social equality, to close gaps in health care, to improve productivity by easing doctors of basic activities so that they can focus on patient care and devote more time to them, and to progress personalized medicine. Digital technology is unquestionably leading us toward the future. In a society in which the horizon defines the possibilities. Technological innovations such as remote operations, robotic surgeries, undetectable sensors, etc., are outstanding steps toward creating a future where everyone is happy and well-served.
The primary motivation for this study is to explore how the potential of new technologies such as AI, IoT, and AR/VR can be leveraged to achieve healthcare equitability - the provision of fair and appropriate care to all individuals regardless of their circumstances. The introduction provides background and information relevant to the study and puts the rest of the paper into perspective by explaining its structure. The rest of the paper is organized as follows: Section 2 provides some background information on digital health, edge computing, edge intelligence, equitable healthcare, and related works. Section 3 discusses the problems and challenges of using edge computing and AR/VR for healthcare equitability. Section 4 presents the impact of intelligent edge computing and AR/VR for achieving healthcare equitability. Section 5 concludes the paper and outlines some future research directions.
Methods
Search Strategy
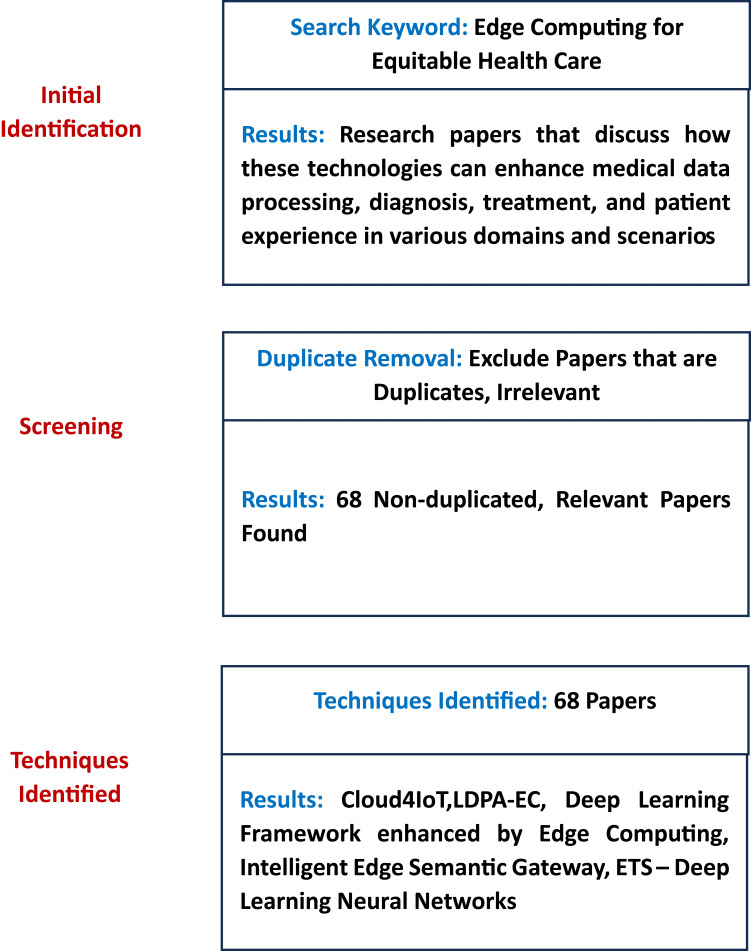
Our research on the topic of Health Care Equity Through Intelligent Edge Computing and AR/VR was conducted through a systematic review of recent publications from 2018 to 2022. We utilized a combination of keywords and topics related to equitable healthcare, edge computing, edge intelligence, AR/VR in healthcare, and health equity to ensure that our search was comprehensive. Our primary sources of information were research journals from IEEE Access and Google Scholar. We also employed referential retracing techniques to verify the inclusion of all relevant papers. Any publications with flawed methods or results were excluded from our analysis.
Search Terms
Our search for information on the topic of Health Care Equity Through Intelligent Edge Computing and AR/VR was conducted using a combination of intervention and application keywords. These included terms such as “edge computing”, “edge intelligence”, “AR/VR in healthcare”, “health equity”, and “equitable healthcare”. This approach allowed us to comprehensively explore the relevant literature and ensure that our research was thorough and up to date.
Search Eligibility Criteria
This research focuses on the role of intelligent edge computing and AR/VR in achieving health care equity in the era of the Internet of Medical Things (IoMT). Only papers that discussed the applications and challenges of these technologies in the context of IoMT and digital health were considered. We did not evaluate studies that examined other aspects of edge computing, AR/VR, or IoMT that were not related to health care equity. Also omitted was any research that used centralized or cloud-based systems, or that did not address the issues of data privacy, affordability, and accessibility. Purely peer-reviewed articles, conference proceedings and papers, and published works were included in this list of credible research. There were no limits on publishing country, research design, or results. Included are studies written in English and published between 2018 and 2022. In addition to removing duplicate data, unnecessary titles and contents were eliminated. Only those research that described the transformational role of intelligent edge computing and AR/VR in the IoMT era to attain health care equity were considered. The search and selection are clearly shown in Figure 1
Figure 1.
Review process.
Background
In this section we describe the main technologies in this study the edge computing, edge intelligence, health monitoring and HealthCare Equity.
Edge Computing
An efficient and cost-effective approach for extending cloud computing is edge computing. By placing computer resources close to the edge of an IoT-enabled network, it offers low-latency data services. The aim is to reduce the processing and traffic load from weak IoT devices to strong edge servers. Decentralization is aided by edge computing, which also helps with network response times and can address security issues. Since data is being created at the network’s edge more frequently, processing data there would be more effective. By enabling edge nodes to react to service requests, the edge computing platform lowers bandwidth usage and network delay.
The edge of the network will have access to edge resources such as mini data centers, routers, and storage arrays under the edge computing approach. These assets will be far less capable than their Cloud equivalents, but they will be situated much nearer to the end consumers. The Edge Module will enhance the global model’s overall learning process as local versions are updated for use with their Edge devices.
Edge computing is a rapidly expanding and crucially important technology in medicine. Internet of Things (IoT) consists of intelligent devices with minimal resources that can identify and analyze information, as well as transferring processed data across network members.1 IoT is the foundational technology in several fields, including patient monitoring,2,3 system infrastructure,4,5 and intelligent urbanization.6 In several nations, the notion of patient monitoring is constantly evolving, and the worldwide market for Internet of Things (IoT) medical equipment is expanding annually.7 Constantly developing new dangers to public health, like the new coronavirus epidemic,8 provide a continuing stimulus for the creation of innovative technology. Since intelligent data analysis necessitates the employment of neural networks and algorithms, the notion of edge devices9–14 is undergoing rapid development. In edge computing, a portion of the processing burden is dispersed across local devices with linked sensors. The processed data is subsequently sent to the edge node for further processing, and ultimately to the clouds and fog server for further worldwide registration and handling. If the Internet connection to the fog and cloud servers gets interrupted, sophisticated local intelligent systems aid in choosing to address the situation at the source of data. Edge computing improves resource utilization by decreasing the quantity of data transported between endpoints and central cloud infrastructure. It increases the connectivity and processing speed of IoT medical equipment.
Certain requirements cannot be met by cloud computing because most data centers are situated far from customers, which causes delays. Implementing cloud computing may result in severe unacceptable network delays for time-sensitive applications, in addition to limited available resources and bandwidth. Edge computing paradigms have been created as supporting technologies for cloud computing to overcome these issues. Edge computing’s main objective is to reduce the distance between consumers and data processing facilities (servers).
Edge computing is an infrastructure that merges cloud-based computation, memory, and communications networks at the network’s edge. By outsourcing some operations to edge devices, edge computation enhances processing performance, decreases storage, lowers latency throughput, increases information security, and eliminates geographical limitations in comparison to cloud computing capabilities. In edge computing, numerous sorts of devices will create vast quantities of data. Instead of transferring the data upstream to cloud computing, the data may be processed on edge services to decrease bandwidth and power costs. Furthermore, edge computing could extract and organize the essential data from the incoming raw data to lower the needed quantity of storage. Additionally, edge computing offers many consumers efficient and secure solutions. Within the framework of 5G communications systems, information technology has the benefit over cloud technology by exploiting the greater bandwidth and reduced latency to guarantee that data is processed and analyzed quickly and effectively.
Health Monitoring
The monitoring of health in IoMTs is essential for the development of ubiquitous healthcare systems. Three major types are described in the following sections.
Health Monitoring Provided by Cloud Computing: Given recent advancements in cloud technology, the framework cost may be cut tremendously by providing remote health monitoring. Conventional methods are very inefficient and difficult to apply in the actual world. Forkan et al15 offer a health surveillance system that can discriminate between emergency and regular scenarios. Pagán et al16 provide a methodology for remote monitoring of health that identifies movement. Using cloud computing, an adaptable sensing method is built to lower transmission costs.
Edge Computing enables Health Monitoring: Unlike most current offloading systems, health monitoring is particularly sensitive to delay. Underneath the delay limitation, distant cloud servers always can deliver appropriate support. Edge computing is used to decrease transmission delays to circumvent this impediment. Gu et al17 present a paradigm for cost-effective healthcare that integrates edge computing and healthcare applications. The researched framework covers server connection, allocation of healthcare analysis duties, and virtualized implementation. Based on linear regression, a heuristic technique for solving the specified optimization model is devised.
5G-Enabled Monitoring: 5G is a potential technology for future sophisticated healthcare systems that may increase spectrum utilization and facilitate high-speed connectivity. System stability, energy loss, and communications delay are considered while allocating the wireless channel’s capabilities. Yi et al18 investigate the randomized arrival of medical analysis jobs and develop a transmission management solution for 5G-enabled medicine. To reduce communication latency, a strategy based on a waiting game is created.19,20
Edge Intelligence
Edge intelligence creates intelligence at the network’s edge. It refers to the capacity to analyze data locally rather than transmitting it to the cloud for examination. Although machine learning methods have been employed in the communications sector, there is still a lot to learn regarding edge intelligence, which will be a vital enabler for the realization of a future with billions of intelligent, interconnected IoT devices. Edge intelligence involves intelligent offloading from terminals to edge servers, intelligent collaboration among edge servers, analyzing service behavior patterns locally at the edge, analyzing data locally at the edge rather than in the cloud to recognize a world of a trillion smart IoT devices, and utilizing machine learning at the edge network to recognize interactive and friction - free Tactile Internet experiences, etc.
Edge Intelligence is a result of the integration of Edge Computing with AI, which is functionally required for the speedy analysis of massive volumes of data and the extraction of insights. Edge Intelligence is more complex than just combining AI and edge computing. The topic of edge intelligence is vast and extremely complicated, encompassing numerous ideas and technologies that are intricately intertwined together. Some studies investigate the idea from the standpoint of building Intelligent Wireless Networks on Edge. To improve the quality and speed of data processing and to safeguard the security and privacy of data, edge intelligence entails a group of interconnected systems and devices that are used for data gathering, caching, processing, and analysis close to the point of collection.
Pushing the AI frontier from the cloud to the network edge is imperative since both AI and IoT are flourishing. Edge computing has long been acknowledged as a potential way to serve computation-intensive AI applications in contexts with limited resources, which satisfies this trend. The unique paradigm of EI is the result of the interaction between edge computing and AI. Intelligent health monitoring paradigms and automatically generated medical diagnosis frameworks offer services in various surroundings and circumstances, including health facilities, places of work, and residences, as well as public transit support, to drastically reduce the cost of doctor visits and enhance the quality of care overall. Utilizing AI approaches, edge intelligence is progressing toward intelligent healthcare frameworks with human-like intellect and intelligent systems. Edge intelligent systems may be completely or partly taught at the edge level, further while computation can be dispersed across edge and fog nodes or performed in the cloud in computationally intensive applications.
In the healthcare industry, edge intelligence can be used to enable a range of applications and services, such as:
Real-time monitoring and analysis of patient data from wearable devices, such as smartwatches and fitness trackers, to detect early signs of illness or disease.
Remote monitoring and diagnosis from remote monitoring devices, such as telemedicine devices, to diagnose and treat patients remotely.
Predictive maintenance of medical equipment to analyze data from medical equipment to predict when it is likely to fail or require maintenance.
Clinical decision support to analyze patient data and provide healthcare providers with real-time recommendations and decision support, helping them to make more informed treatment decision.
Digital Health
With both the government and public health response towards the novel COVID-19 outbreak shutting down conventional healthcare delivery globally, initiatives to reduce obstacles to digital healthcare provision demonstrate the potential to redefine conventional care models into digital and distance methods.21 Technology-supported programs have helped many nations preserve methods of health care without social distance.5,22 As world leaders consider policies that could increase access to innovative health services in reaction to the COVID-19 pandemic, it has become increasingly critical to comprehend how identified and evolving IoT/ ML/ AR/VR technologies can assist healthcare systems to produce safe and efficient care during crises or epidemics.23
In the frame of reference of the ongoing transitions of health and social care systems to enhance this same safety and quality of patient treatment and public health, as well as the effectiveness and efficiency of care delivery companies under the well-known restrictions, adequate organizational and epistemological paradigm shifts, supported by technological advancements, are unavoidable. Concerning the organizational paradigm, there has been a shift from organization-centric healthcare to disorder procedure care to person-centered care. This procedure is accompanied by technological advances, such as the shift from centrally controlled to a distributed network and mobile platforms, the deployment of the healthcare internet of things, also known as the internet of medical things, smart infrastructure, information retrieval, and management, as well as the emergence of a new enterprise. In addition, big data and analytics, training technologies and machine intelligence, and automated vehicles facilitated by cloud, and edge computing, in addition to quantum computing today, must be considered. Concerning the methodological framework, care emerges from the empirical application of basic care addressing health issues with a one-size-fits-all remedy to the proof medicine approach of devoted care for a stratification population to specific, clinically significant conditions and, in conjunction with the mentioned previously technological advances, comprehensive or genomic medicine.
Electronic Health (eHealth)
E-health is an emerging topic at the confluence of traditional health and Information and Communications Technology (ICT), such as the usage of Electronic Medical Records that contain patients’ health records. People, procedures, and technologies are the three pillars of the eHealth revolution. While technology and procedures may alter people, the stronger impact routes are those that involve people modifying technologies and processes - through ingenuity, invention, and creativity. People’s creative talent is responsible for the advances that may revolutionize health systems. eHealth is also redefining the role of the public in health care by providing individuals access to health-related information and so shifting them from passive spectators to actively participating in the process of care. In certain instances, people come to the hospital with greater knowledge about their disease than healthcare professionals. In every region of the globe, health equality and social justice pose a formidable obstacle for society. Health-related resources are a crucial component of the ability to use eHealth and are among the areas with the highest demand. Many healthcare systems in poor nations are at risk of failing to reach the health MDGs due to a shortage of personnel to offer even the most basic services. Due to their requirement for highly skilled personnel, hospitals are at the forefront of this dilemma. As the amount and complexity of data and knowledge have exceeded the capacity of health professionals to perform properly without the help of information management tools, telecommunications, and information technology have become crucial in health care. The citizen is significant but, according to some, often ignored asset in the healthcare system. In a particular month, the ecosystem of medical treatment indicates that up to as 20% of persons serviced by the health-care system exhibit no symptoms of illness. Investing in disease prevention would provide substantial returns in the form of reduced healthcare costs. Recent data indicates that preventative health is the key arena in which the user information systems in health lead to improvement and that lower care usage is the main efficiency advantage obtained. Currently, the citizen is transforming from a passive participant inside the caregiving process – confined by the long-standing information imbalance between patient and care provider – to an active collaborator in the mending or well-being processes. Consumers may have more knowledge about their ailments than their physicians do today, but they still want the healthcare system professional to convert this information into actionable steps. Undoubtedly, an educated patient is a benefit in the treatment process. Perhaps the most noteworthy thing about eHealth is that it is facilitating the transition of the healthcare system: from one that is focused specifically on disease treatment in health facilities by healthcare professionals to a system with a broader focus on wellness and enabling citizens by supplying them with data to take care of their well-being wherever and whenever that there is a need arises.
Mobile Health (m-Health)
Smartphones have lately been recognized as being of considerable use in the healthcare industry, resulting in the development of mobile healthcare. Previously known as mhealth. M-health is a subset of e-health and is characterized as
Medical and public training supported by mobile, including such mobiles, patient monitoring equipment, digital assistants, as well as other digital connectivity24
By WHO in cooperation with the Global Observation deck for eHealth. The contact between patients and careers is facilitated through M-health apps. Additionally, they permit monitoring systems in real time.
Smart Health (s-Health)
Context-aware settings, like smart homes and smart towns, are constructed with advanced detecting, analyzing, and decision-making abilities, because of the continuous development of ICT. The adoption of context-aware settings in conjunction with e-health and m-health has spawned the phrase smart health. In terms of core architecture, S-health and m-health are unlike. According to,25 “the idea of s-health might be regarded as an extension of m-health with the sensor devices of smart cities”, and sums up the distinctions in two points; distinctions in sources of information even as data could originate from various sources other than patients, which exceeds m-health, and distinctions in information flow as the obtained information may be analyzed by multiple parties, thereby surpassing the user-centric strategy and m-health.
Smart healthcare arose from the desire to enhance the administration of the healthcare industry, better use its capabilities, and decrease its costs while preserving or even increasing its quality. Consumable assets and non-consumable assets may be broadly categorized within the medical industry. Consumable resources are those that degrade and expire over time, such as all healthcare equipment and instruments. On the opposite hand, non-consumable resources are items that do not diminish with time. Human resources including doctors, nurses, and nurse practitioners, as well as all the intellectual resources that go into the healthcare system, are non-consumable assets. Intellectual capital in the healthcare industry is a highly costly resource, and employing this resource effectively is a step toward a fully intelligent healthcare system.
In the last century, the enormous growth in the number of individuals suffering from chronic illnesses has greatly raised the need to identify creative techniques to manage the healthcare process in a manner that is efficient and cost-effective.26 The structure of the medical industry necessitates a dependable and effective method for constantly managing vast quantities of data. It is now feasible to design and create smart healthcare owing to the edge and cloud-based computing because it has been shown that the cloud is more dependable than traditional servers. Furthermore, cloud computing companies continue to protect patients’ privacy.27 The advantages and disadvantages of implementing new technologies are analyzed in,28 as are the advantages of migrating from conventional healthcare central systems to decentralized cloud-fog-based medical systems, as well as the requirement for allocation of resources, direction, and strategy. In addition, with the assistance of mobile computing, WAN may be upgraded for the implementation of healthcare devices.29 Cloud/edge computing can offer a safe and secure foundation for intelligent healthcare. In a subsequent study, Tuan et al30 emphasized and illustrated the significance of the IoT and computing in delivering more dependable health services. Intelligent healthcare studies may be roughly divided into two groups: patient-related and process-related. The patient-related group includes, but is not limited to, studies available on wearable technology to gather patient information for medical institutions. Applications of Big data, Artificial Intelligence methods such as deep learning, Decentralized technologies such as Blockchain technology, and such processes, would focus on extracting knowledge which is termed as “process mining” from medical records, which can lead to more automated solutions.
Equitable HealthCare
Equitable healthcare resource allocation may not always address disparities in healthcare demands. While there are disparities in gender, education, wealth, and racial and ethnic disparities that prohibit people from having access to health care, the availability of high-quality care may also be constrained. Since most modern medical facilities are found in urban regions, those who live there are likely to have access to the greatest medical care possible, but thousands of people in rural areas lack access to affordable healthcare. The idea of equitable healthcare emerged from the idea that people with different social and economic backgrounds have varied levels of accessibility to quality healthcare. To put it another way, groups of people who are already socially marginalized due to poverty, gender, race, ethnicity, or religion also have healthcare accessibility challenges. Distribution of resources and other procedures to address health inequalities are necessary for the equitable delivery of healthcare.
Inequities in healthcare are referred to by medical practitioners as health disparities. A health disparity is a variation in health that is associated with an unjust socioeconomic or environmental imbalance. Health inequalities are detrimental to communities that face larger social or economic challenges. Regarding health care disparities, race is not the sole determinant. Mobile health clinics, comprised of vans outfitted with medical devices, may aid in expanding healthcare access, hence enhancing equality in remote regions. Usually, achieving equality in healthcare coverage requires the elimination or reduction of economic and social constraints that impact a person’s health. Some means to do this may include:
Increasing healthcare access by introducing mobile medical centers or telemedicine programs, such as virtual health services or training. Increasing medical translations would be one method of fostering culturally sensitive care. Advocating for policies that alleviate the harms caused by racial inequality, sexism, class discrimination and other types of injustice, which impede healthcare outcomes. The socioeconomic determinants of wellness are often included when measuring healthcare accessibility. Using the social determinant of health, healthcare professionals may examine the external influences that influence the health of any specific person. The Centers for Disease Control and Prevention describe health-related social determinants as “conditions in the locations where individuals live, study, work, and play that influence a broad spectrum of health-related and life-quality risks and outcomes.18 Among the social factors that influence health are:
Education: languages and literacy rates, the greatest level of education, and educational quality.
Health care: primary healthcare accessibility and health literacy.
Economic stability comprises jobs, food security, and housing security.
Environment: dwelling quality, proximity to criminal activity and violence, and environmental risks.
Related Works
Edge Computing in Healthcare
The security of the e-healthcare surveillance services is proposed using an Edge of Things (EoT) computing platform. When real-time computation and storage functions are performed on the EoT framework, fully homomorphic encryption is utilized to perverse privacy. Large-scale heterogeneous data analysis also uses a distributed cluster-based methodology. However, as devices and heterogeneous sensors are added to meet high demand, the model’s security is reduced. An e-healthcare model based on edge computing is proposed, where the edge computing layer minimizes latency and reaction time. Most of the data is processed at the edge computer layer, making this viable. At the cloud storage, a suitable access control system is put in place to preserve security and prevent unauthorized users from accessing the data.31 For higher-level healthcare services like local storage, quick computing power, and real-time data interpretation, a smart e-healthcare doorway is set up at the network’s edge.32 An Edge computing platform for IoT-enabled healthcare systems that is secure and Software Defined Networking (SDN) based. All IoT devices are authorized at the edge server using a simple authentication method. All the data are then submitted for storage, processing, and analysis. In IoT-enabled healthcare systems, the edge server is connected to the SDN controller, which oversees load balancing, network optimization, and effective resource use.
Developments in areas like the Internet of Things, smart cities, and intelligent healthcare systems are being driven by edge computing. The significant use of edge computing in Smart healthcare systems includes a healthcare domain. Such is the management of healthcare resources, and medical equipment, in addition to 3D remote CT imaging and the automation of healthcare.33 The healthcare industry begins using edge computing to enhance healthcare services. The medical platform installed in a smart home allows the use of sensors and portable devices, as well as the scalability of information storage and processing capacity, for distinct types of healthcare analysis. It allows the exchange of analytical findings and accessibility to the storage and processing facilities with improved reaction time and resource efficiency.34 In a typical healthcare situation, for instance, aided individuals are watched by several sensors collecting data and analyzing the data on edge workstations (ie, servers) or the hospital-managed private cloud data center. Using these data processing findings, physicians may diagnose and make judgments. Inferring complex human actions and diagnosing potential diseases such as dementias,35 multiple sclerosis prognosis,36 fall detection,37 breathing failure in the elderly,38 Alzheimer’s disease,39 and coronary heart condition and cnacer40–43 is facilitated by computing duties on having to process recorded information. Additionally, this healthcare platform offers an environment for big data analytics for global and community health. Existing systems, their issues and probable solutions are listed in Table 1.
Table 1.
Edge Computing for Healthcare Systems: Problems in Existing Systems and Techniques Used to Solve
| Reference | Problem | Technique Used |
|---|---|---|
| Edge computing in IoT context: Horizontal and vertical Linux container migration42 | The increasing IoT devices pose challenges to data privacy and network performance. |
|
| A framework for edge-assisted healthcare data analytics using federated learning43 | Existing machine learning (ML) algorithms that were developed and validated on a single central data store will no longer work. |
|
| Edge computing-based secure health monitoring framework for electronic healthcare system44 | The Quality of Services (QoS) parameter in the cloud-based healthcare system is lowered by high latency and response times. |
|
| Health-Fog: An ensemble deep learning-based Smart Healthcare System for Automatic Diagnosis of Heart Diseases in integrated IoT and fog computing environments45 | The present edge models have significant drawbacks and are only concerned with either results precision or response time reduction, not both. |
|
| A secured framework for SDN-based edge computing in IoT-enabled healthcare systems18 | The associated data (patients’ personal, sensitive information) and low-powered technologies are vulnerable to several security risks. |
|
| An effective training scheme for deep neural networks in edge computing enabled Internet of medical things (IoMT) systems46 | The main problem in deploying an efficient latency-aware health monitoring system is that DL inference is embedded into an edge device, which has limited computational power. |
|
| Analysis of Privacy-Preserving Edge Computing and Internet of Things Models in the Healthcare Domain47 | Healthcare systems acquire and manage sensitive information, and the misuse of this data by malicious attackers can have disastrous effects. |
|
| An intelligent edge computing-based semantic gateway for healthcare systems interoperability and collaboration48 | Due to a lack of cooperation and information sharing among healthcare systems (clinics, hospitals, and pharmacies), compatibility with these systems is still an issue. |
|
| Edge computing health model using P2P-based deep neural networks.19 | Deep learning algorithms are hampered by the over-fitting issue in a neural network and increased computing costs related to elevated levels of time complexity. Response delays are common in large data learning processes and deep neural network-based data extraction procedures because of these issues, which exponentially raise the cost of data extraction. |
|
Edge Computing with AR/VR for Healthcare Systems
AR refers to an interactive experience in which computer-generated material and features are merged into the actual world. Various sensors, including haptic devices, cameras, microphones, and GPS, are used to construct the computer-generated information’s virtual content. In contrast to AR, virtual reality (VR) occurs in an artificial environment, and participants may choose to immerse themselves completely or partly in this world. In a virtual world, individuals may interact with and control computer-generated objects using haptic devices and other technologies.
Augmented reality augments the actual world with individual or collective virtual components using the cameras on mobile devices. Real-time services around augmented reality technology make possible the application of such solutions in a variety of sectors across the globe and the construction of modern virtual systems that are made real. VR/AR technology continues to evolve rapidly. The software is becoming more complex, quicker, and its graphical representation is more detailed. Hardware is shrinking and becoming less costly. The least of these technological advancements is the enhancement of the user experience. It has become clear that providing the necessary low latency with cloud computing and the transfer of massive amounts of data to the data centers may not be feasible or may not be financially viable in the light of the recently emerging AR/VR applications and many other delay-sensitive applications in 5G. The idea of edge computing appears as a promising technique to get beyond these limitations. Proxy servers are a component of edge computing, also known as fog computing, which is based on the network’s edge. Edge computing’s primary goals are reduced latency and location awareness.
There are numerous uses for tactile internet and augmented reality in healthcare. One of the fundamental uses, for instance, is remote surgery for patients in remote areas where specialized doctors cannot travel or in circumstances like war zones. In addition to using AR/VR for remote surgery, patients with multiple sclerosis have seen a considerable improvement in their walking ability because of visual feedback from VR equipment.
There have been significant changes in health because of the advancement of technology. This category is being changed by some technologies, like Fitbit, diabetes meters, and other telemedicine tools. These devices’ data processing and storage capabilities were used to update patient records. However, the volume of data generated for millions of patients is too much for the cloud of these advances to handle and store. Edge Intelligence computers, especially in crises, can help in this situation by combining these technological capabilities with the availability of dependable clinicians and medical professionals, and near-patient information. Its proximity provides essential features such as low latency, scalability, and high-speed resulting in an unparalleled VR / AR experience.
Edge Computing for Equitable Healthcare Systems
Equitable access to healthcare necessitates addressing the varied needs of individuals but does not need publicly provided healthcare access. Some places may be suited for long-lasting to-lasting business, while others may need more focused assistance for epidemic or public health care.44
There is a perception that the delivery of healthcare equity is essential to the growth of any society. Health disparities in status, health care usage, and health care finance need population health. The notion of health equality developed from the assumption that variations in people’s social and economic origins affect their access to medical care. In other terms, groups of individuals that are already marginalized in society owing to income, gender, ethnic, regional, or religious origin are even further disadvantaged in terms of their health. To comprehend the notion of health equality, it is essential to recognize that health encompasses both physical and psychological well-being, with crucial social factors including home living circumstances, community, and employment environments, including healthcare access. About the ethical component, equitable healthcare does not necessitate that everybody should have equal access to medical care, but rather that individuals should be allowed to live lives that are of value. There is the perception that health equality encompasses more than ensuring that as many individuals as feasible in a society have access to care. The allocation of healthcare resources equitably may not always resolve disparities in healthcare demands. In addition to gender, education, income, and racial/ethnic disparities that impede individuals from accessing health care, the availability of excellent treatment could also be limited. This implies that if a government with restricted medical resources had to spread these resources among a relatively large number of people who need healthcare, some individuals would be unable to get treatment. People would not be able to attain health due to the lack of medical resources accessible to them.
Given the discrepancies in their socioeconomic situations, it seems that poor or underprivileged individuals require more and better treatment, as well as maybe early access to health care to achieve equivalent results to those with money or easy access. Inside this sense, equality in health may include preventative healthcare initiatives that provide early access to those in need within underserved areas. How can society guarantee that healthcare results benefit the well-being of individuals, organizations, and societies? This is a difficulty that arises when seeking to provide healthcare to everyone. The next section explores the challenge of providing affordable healthcare for as many individuals as feasible while maintaining treatment quality.
Problems
Problems in Utilizing Edge-Computing
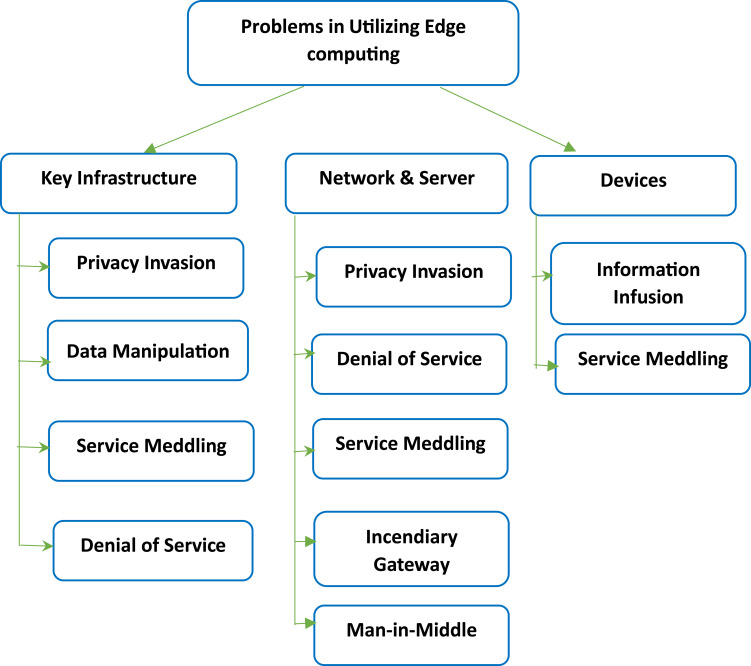
Key Infrastructure
It makes network access, centrally controlled edge computing services, and edge device function control easier. To store huge amounts of data, the edge computing infrastructure comprises an edge device network and edge nodes connected to IoT devices or cloud data centers. It is controlled by edge servers and cloud data centers, which causes data leakage, theft, unlawful replication, publication, and distribution.
Network and Server
The edge devices offer real-time data processing and storage solutions and cross-virtualization. Adversaries may take over these processing units internally or externally or interfere with the system’s operation. These data centers work in tandem and maintain constant connectivity to the conventional cloud. The techniques used to connect Internet-enabled IoT devices with sensors and rough gateways make it dangerous which leads to compromising data security. Edge computing modifies the security footprint, necessitating that distant servers use the same networking and security frameworks to account for position and traffic conditions. Edge computing may necessitate access for users across a substantially higher number of devices, necessitating that IT teams sketch out access permissions in detail.
Devices
To offer the facility to the end-users, these devices are connected to the network’s edge. Edge devices perform data gathering, data processing, and decision-making tasks. Because of hostile and corrupted devices, it has various security risks. In Figure 1, the key problems faced while utilizing edge computing for healthcare are highlighted.
Problems with Edge Computing
Cost and Storage
Even if the costs of cloud storage are reduced, there is an extra expenditure on the local ends. This is mostly due to the creation of storage capability for edge devices. Also, there is a financial component to edge computing since outdated IT network infrastructure must be replaced or modernized to support edge devices and storage. Some businesses may discover that the price of migrating to an edge network is comparable to the price of constructing and maintaining a conventional IT architecture.
Lost Data
The benefit of edge computing is accompanied by a danger. To prevent data loss during implementation, the system should be meticulously designed and developed. Several edge computing devices remove useless data after gathering, as they ought to. However, if the data destroyed is important, it is lost, and the cloud assessment will be inaccurate.
Security
There is a security issue on the local scale, just as there is a security benefit at the cloud and corporate levels. It serves little use for a corporation to choose a cloud-based service with exceptional security if its local network is vulnerable to intrusion. IT departments have wrestled with this issue for years, but awareness, or lack thereof, goes to the new edge network as well. Though cloud-based security is improving, human mistakes, locally installed programs, and weak passwords are the most common causes of security breaches.
Problems in Digital Healthcare
Bias in Medical Data
There are human biases across every branch of research, but in medicine, these biases are more pronounced and contribute to diagnostic mistakes and medical blunders. Doctors face largely common illnesses and rarely, rare disorders. In many instances, people with the same condition respond differently to the same medication, and clinicians’ efforts to make sense of and diagnose based on such unclear and inaccurate data may result in inappropriate treatment recommendations. Similarly, doctors apply revolutionary medical processes or therapies to their patients, given most of the evidence for such treatments has been created in carefully controlled study contexts. These new medical treatments and therapies may have varying effects on patients’ health due to differences such as standard of living, gender, wealth, geographical area, education level, and handicap conditions. Any prediction algorithm which uses data and statistical techniques to discover trends is susceptible to the same biases. For instance, machine-learning algorithms learn from basic training data by analyzing their patterns and generate predictions about fresh data by identifying patterns that are comparable to the original training data. If such systems learn the incorrect signal from training examples, the following predictions will be incorrect.
Problems in Edge Computing in Healthcare
Government Policies
Policy support is among the most crucial environmental facilitators for the Internet of Things. Numerous nations have previously enacted policies for eHealth45 and also have or are currently implementing policies regarding IoT infrastructure, funding, and deployment in healthcare coverage. Currently, many nations have appropriate IoT policies. Some governments have implemented specific policies and initiatives to support the growth of edge computing. For example, the United States Federal Communications Commission (FCC) has established a task force to explore the potential of edge computing and identify regulatory barriers to its deployment. The European Union has also supported the development of edge computing through initiatives such as the 5G PPP Edge Computing Working Group, which aims to accelerate the deployment of edge computing technologies in the EU.
It is important to note that while governments may support the development of edge computing, they may also impose regulations and standards to ensure the safe and responsible deployment of these technologies.
Cyber Security and Privacy
Cybersecurity is a significant barrier to the widespread acceptance of IoT.46 Individuals’ privacy should be protected to avoid illegal identification and monitoring. From this vantage point, the higher autonomy and intelligence of objects, the greater the difficulties in protecting identities and confidentiality.
The Internet of Things may provide the potential for hacks and unlawful data collection. IoT-based systems are susceptible to assaults in two fundamental ways: (1) most connections are wireless, therefore enabling eavesdropping relatively simply, and (2) the majority of IoT components have low energy, allowing them to implement complicated security systems on their own. National Institute of Standards and Technology has recently published a draft security guidance as well as suggestions for Internet of Things (IoT) devices, with a focus on data confidentiality in IoT;47 nevertheless, it is uncertain if such a guideline will be imposed all over IoT health devices.
Transparency and imposed rules of practice about where central cloud datasets are kept and who controls the data must be addressed for IoT-based healthcare coverage to advance. The exchange of data between states or regions and globally is an additional significant factor to consider. Confidentiality, protection, and privacy of information storage and management should be regulated at the federal level, but overseas hosts and providers might not be obligated to comply. To design and execute comprehensive IoT-based healthcare policies, the utilization of these systems needs strategic planning and open rules.
Confidence and Acceptability
A lack of public knowledge and comprehension exists about the security of health data kept on the internet. This is cause for worry since it represents the greatest danger to the social acceptance of IoT. The concept of IoT is understood by society; nevertheless, the real benefit IoT provides to individuals from a healthcare viewpoint is not well understood.48,49 For customers to reliably participate in IoT-supported healthcare systems, the perceived benefit must balance the possibility of a violation of confidentiality. Requirements are to ensure the trust and acceptance of IoT by medical professionals. The evaluation of innovation programs by clinicians is influenced by a variety of factors, along with the features of advanced technologies, patients’ beliefs and knowledge, external strategic factors, and organizational readiness.50
Standardization Protocols
Interoperability and standards issue between IoT with health care systems provide a significant barrier to the widespread deployment of IoT in healthcare systems. Even as industry and manufacturers have not yet reached an agreement on wireless transmission protocols and requirements for communication, a lack of standardization poses a danger to the growth of IoT in healthcare settings. Without even a single, standard, and interoperable infrastructure, the implementation of IoT for healthcare coverage would be significantly hampered and its worldwide reach is doubtful.51 Interoperability standards do exist; thus, the development and full capability of IoT-enabled healthcare coverage depend on solving interoperability.52 Interoperability among IoT platforms may give physicians and patients a safer, more affordable, efficient, and beneficial environment.
Financial Benefits
Traditionally, compensation for technology-assisted medical services has been difficult53 and varies substantially across nations. This is expected to be significantly more complicated for IoT-delivered health, for which payment concerns have not yet been defined. As global healthcare systems define robust principles and regulations on cybersecurity and deal with the issues encompassing interoperability and normalization procedures, remuneration and regulatory considerations should be a top priority to ensure the effective, beneficial, and cost-effective implementation of IoT healthcare models. The problems faced are given in Figure 2.
Figure 2.
Problems faced while utilizing edge computing.
Impact of Intelligent Edge Computing in Equitable Healthcare
In this section, we discuss how intelligent edge computing and AR/VR can have a positive impact on achieving healthcare equitability for all people, especially those who face challenges in accessing conventional healthcare facilities or services. We present some examples of existing or emerging applications that use these technologies to provide equitable healthcare in various domains, such as remote diagnosis and treatment, patient education and empowerment, medical training and simulation, and mental health therapy. We also highlight some of the challenges and limitations that these applications may encounter, such as technical issues, ethical concerns, or user acceptance. We aim to show how intelligent edge computing and AR/VR can offer innovative solutions that can overcome some of the barriers and gaps in healthcare delivery, while also acknowledging the need for further research and development in this domain.
Accessible Primary Healthcare
The Internet of Things does have the potential to enhance public health and shift our healthcare paradigm to a real hybrid version of basic and secondary care, in which the healthcare system can utilize its current personnel in faster and more effective ways. Changing health care in this manner is essential for enhancing self-management for persons with chronic diseases since even among heavy healthcare clients, over 90% of lifestyle self-management was performed by individuals outside of facilities and medical centers.
There is a definite desire for readily available health data. ML has also increased the accessibility of health data at the point of treatment, including chatbots that provide health opinions. These well-established AI bots include Woebot, and Health Tap, in which a client may enter their symptoms and get rapid recommendations.54 Nevertheless, more than 50% of the highest-rated apps make unapproved health claims,55 there is no official procedure for licensing applications or informing customer choice,56 and there is still much to learn about the possibilities of chatbots to enhance health. Consequently, a credible evidence foundation for digital health is required.57 If healthcare providers have ready access to evidence-based internet materials, gadgets, and mobile applications, digital prescriptions might allow a broader adoption of IoT in healthcare coverage and a greater public emphasis on illness prevention.
Individually, IoT provides the chance to integrate and probably learn from non-health IoT technology to track everyday activities, give informational assistance, and encourage behavior adjustments. IoT and data linking can provide fair, proof-based decision-making, that may be capable of influencing the shift of illness patterns and improving the well-being of residents on a large scale. The combination of urban infrastructures, IoT, and edge computing permits the collecting and analysis of a massive amount of diversity of both human and non-human information. Such data can provide crucial data regarding population-level monitoring of illnesses and accidents, health conditions, and climatic circumstances, which is difficult to obtain through the conventional human-reported disease monitoring system and can be especially useful in pandemic reactions. With IoT and data integration, lawmakers are expected to be able to make choices based on evidence to promote healthier cultural and built environments, efficient transport networks, high-quality public services, and intelligent medical services and systems for emergency responses.12,58,59
Proactive Secondary Healthcare
An Internet - of - things system for health care allows the total medical systems to transition from a responsive, inconsistent, and uncoordinated method of service supply to a proactive, continuous, and agreement. This strategy is advantageous because it allows for the provision of high-quality treatment that is less intrusive and more attractive to patients and healthcare providers. This transformation in the scenery of the medical system is also going to appeal to decision-makers as it can significantly improve the health system’s efficiency and will provide the medical system with the flexibility to adjust its frameworks of care and support delivery as needed on a personal or population-wide scale.
Privacy
An integration of IoT with edge computing not only offers users flexible, efficient services and also fosters consumer confidence by protecting their privacy. The more decentralized the architecture of a healthcare system, the greater its ability to avoid the leaking of confidential information. Blockchain technology can provide high tamper resistance and health data from various sources stored on these decentralized networks need not rely on a single storage facility, hence healthcare organizations would be liberated from the liability of handling enormous amounts of medical records.60 Whereas decentralization eliminates a single point of failure and benefits differential privacy mechanisms, it also contributes additional complexity to the overall performance of the system. Edge computing’s heterogeneity and decentralization make it more challenging to scale up services in a safe and efficient manner.
Conclusion
Emerging innovations provide a significant potential for healthcare organizations to proactively identify, treat, and follow - up care outside of the facility. As the use of tech medical services expands to allow health systems to provide flexible support systems, a growing variety of conventional healthcare delivery techniques will be enhanced or replaced by IoT. Nevertheless, the deployment of IoT in health care will be contingent upon a clear and rigorous code of conduct for the handling of data, privacy, transparency, and security regarding the supply and utilization of IoT systems in health care. By leveraging the power of edge computing and AR/VR, healthcare professionals can provide fair and appropriate care to all individuals regardless of their circumstances. The review also sheds light on the challenges faced by existing centralized and deep learning-based healthcare systems and how intelligent edge computing and AR/VR can help overcome these challenges. Overall, this review provides valuable insights for healthcare professionals and policymakers to develop and implement intelligent healthcare systems that prioritize equity and accessibility. Further research in this area can help unlock the full potential of intelligent edge computing and AR/VR in transforming the healthcare industry.
The review’s findings emphasize the need to understand and overcome technological barriers to properly employ intelligent edge computing and augmented/virtual reality in healthcare. These technologies can improve healthcare delivery by enabling new applications and services. We acknowledge that healthcare equity has trumped technological problems. To increase paper coherence, future study should focus more on healthcare technology and fairness. Recognizing and tackling barriers to accessing and benefiting from cutting-edge technologies will help us keep healthcare equality at the forefront of innovation.
Since healthcare equity is essential to the adoption of intelligent edge computing and augmented reality/virtual reality, researchers, lawmakers, and healthcare providers must work together to provide inclusive, affordable, and accessible solutions. To ensure that these technologies satisfy the healthcare needs of disadvantaged and marginalized people, they should be actively involved in their design and deployment. Technical challenges are necessary to understand healthcare technology’s promise, but justice must be considered. By doing this, we may create a healthcare system that prioritizes patient needs and is more egalitarian, leveraging intelligent edge computing and augmented/virtual reality for everyone, regardless of background or circumstance.
Overall, edge computing has the potential to improve the efficiency and effectiveness of healthcare delivery, as well as enabling new applications and services that were not previously possible. However, it is important to ensure that the deployment of these technologies is done in a responsible and ethical manner, considering the privacy and security of patient data.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kuo AMH. Opportunities and challenges of cloud computing to improve health care services. J Med Internet Res. 2011;13(3):e67. doi: 10.2196/jmir.1867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Otoum S, Ahmed M, Mouftah HT. Sensor Medium Access Control (SMAC)-based epilepsy patients monitoring system. In: 2015 IEEE 28th Canadian Conference on Electrical and Computer Engineering (CCECE); 2015:1109–1114. [Google Scholar]
- 3.Gia TN, Jiang M, Rahmani AM, Westerlund T, Liljeberg P, Tenhunen H. Fog computing in healthcare internet of things: a case study on ECG feature extraction. In: 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing; 2015:356–363. [Google Scholar]
- 4.Kumar S, Tiwari P, Zymbler M. Internet of Things is a revolutionary approach for future technology enhancement: a review. J Big Data. 2019;6(1):111. doi: 10.1186/s40537-019-0268-2 [DOI] [Google Scholar]
- 5.Deepthi S, Ravikumar A. A study from the perspective of nature-inspired metaheuristic optimization algorithms. IJCA. 2015;113(9):53–56. doi: 10.5120/19858-1810 [DOI] [Google Scholar]
- 6.Korzun D, Meigal A. Multi-source data sensing in mobile personalized healthcare systems: semantic linking and data mining. In: 2019 24th Conference of Open Innovations Association (FRUCT); 2019:187–192. [Google Scholar]
- 7.Al-Turjman F, Nawaz MH, Ulusar UD. Intelligence in the Internet of Medical Things era: a systematic review of current and future trends. Comput Commun. 2020;150:644–660. doi: 10.1016/j.comcom.2019.12.030 [DOI] [Google Scholar]
- 8.Pătru II, Carabaş M, Bărbulescu M, Gheorghe L. Smart home IoT system. In: 2016 15th RoEduNet Conference: Networking in Education and Research; 2016:1–6. [Google Scholar]
- 9.Ahmed WS, Karim AA. The impact of filter size and number of filters on classification accuracy in CNN. In: 2020 International Conference on Computer Science and Software Engineering (CSASE); 2020:88–93. [Google Scholar]
- 10.Saeed SA, Khan FZ, Iqbal Z, et al. An IoT-Based Network for Smart Urbanization. Wirel Commun Mob Comput. 2021;2021:1–14. doi: 10.1155/2021/558466735573891 [DOI] [Google Scholar]
- 11.Rahman MM, Davis DN. Addressing the class imbalance problem in medical datasets. IJMLC. 2013;3:224–228. doi: 10.7763/IJMLC.2013.V3.307 [DOI] [Google Scholar]
- 12.Li J, Cai J, Khan F, et al. A secured framework for SDN-based edge computing in IoT-enabled healthcare system. IEEE Access. 2020;8:135479–135490. doi: 10.1109/ACCESS.2020.3011503 [DOI] [Google Scholar]
- 13.Chung K, Yoo H. Edge computing health model using P2P-based deep neural networks. Peer-to-Peer Netw Appl. 2020;13(2):694–703. doi: 10.1007/s12083-019-00738-y [DOI] [Google Scholar]
- 14.Hartmann M, Hashmi US, Imran A. Edge computing in smart health care systems: review, challenges, and research directions. Trans Emerg Telecommun Technol. 2022;33(3):e3710. doi: 10.1002/ett.3710 [DOI] [Google Scholar]
- 15.Shi W, Cao J, Zhang Q, Li Y, Xu L. Edge Computing: vision and Challenges. IEEE Internet Things J. 2016;3(5):637–646. doi: 10.1109/JIOT.2016.2579198 [DOI] [Google Scholar]
- 16.Pagán J, Fallahzadeh R, Pedram M, et al. Toward ultra-low-power remote health monitoring: an optimal and adaptive compressed sensing framework for activity recognition. IEEE Trans Mob Comput. 2019;18(3):658–673. doi: 10.1109/TMC.2018.2843373 [DOI] [Google Scholar]
- 17.Gu L, Zeng D, Guo S, Barnawi A, Xiang Y. Cost efficient resource management in fog computing supported medical cyber-physical system. IEEE Trans Emerg Top Comput. 2017;5(1):108–119. doi: 10.1109/TETC.2015.2508382 [DOI] [Google Scholar]
- 18.Yi C, Cai J. Transmission management of delay-sensitive medical packets in beyond wireless body area networks: a queueing game approach. IEEE Trans Mob Comput. 2018;17(9):2209–2222. doi: 10.1109/TMC.2018.2793198 [DOI] [Google Scholar]
- 19.Ravikumar A, Sriraman H. Real-time pneumonia prediction using pipelined spark and high-performance computing. PeerJ Comput Sci. 2023;9:e1258. doi: 10.7717/peerj-cs.1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ravikumar A. Non-relational multi-level caching for mitigation of staleness & stragglers in distributed deep learning. In: Proceedings of the 22nd International Middleware Conference: Doctoral Symposium; 2021:15–16. [Google Scholar]
- 21.Kitaria D, Mwadulo M. Adoption of Augmented Reality (AR) and Virtual Reality (VR) in healthcare systems. African J Sci Technol Soc Sci. 2022;1(1). doi: 10.58506/ajstss.v1i1.70 [DOI] [Google Scholar]
- 22.Baby K. Big data: an ultimate solution in health care. Int J Comput Appl. 2014;975:8887. [Google Scholar]
- 23.Schneider M, Rambach JR, Stricker D. Augmented reality based on edge computing using the example of remote live support. 2017 IEEE International Conference on Industrial Technology (ICIT); 2017:1277–1282. [Google Scholar]
- 24.Torous J, Myrick KJ, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Mental Health. 2020;7(3):e18848. doi: 10.2196/18848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisk M, Livingstone A, Pit SW. Telehealth in the Context of COVID-19: changing Perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res. 2020;22(6):e19264. doi: 10.2196/19264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan N, Efthymiou M. The use of biometric technology at airports: the case of customs and border protection (CBP). Int J Inf Manag Data Insights. 2021;1(2):100049. doi: 10.1016/j.jjimei.2021.100049 [DOI] [Google Scholar]
- 27.World Health Organization, 2022. Indicator metadata registry details. Available from: https://www. who. int/data/gho/indicator-metadata-registry/imr-details/158. Accessed 19 September, 2023.
- 28.Solanas A, Patsakis C, Conti M, et al. Smart health: a context-aware health paradigm within smart cities. IEEE Commun Mag. 2014;52(8):74–81. doi: 10.1109/MCOM.2014.6871673 [DOI] [Google Scholar]
- 29.Kim J. The effect of patient participation through physician’s resources on experience and wellbeing. Sustainability. 2018;10(6):2102. doi: 10.3390/su10062102 [DOI] [Google Scholar]
- 30.Aloqaily M, Kantarci B, Mouftah HT. Multiagent/multiobjective interaction game system for service provisioning in vehicular cloud. IEEE Access. 2016;4:3153–3168. doi: 10.1109/ACCESS.2016.2575038 [DOI] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Social determinants of health at CDC. Available from: https://www.cdc.gov/about/sdoh/index.html#:~:text=They%20are%20the%20conditions%20in,climate%20change%2C%20and%20political%20systems. Accessed 19 September, 2023.
- 32.Alabdulatif A, Khalil I, Yi X, Guizani M. Secure edge of things for smart healthcare surveillance framework. IEEE Access. 2019;7:31010–31021. doi: 10.1109/ACCESS.2019.2899323 [DOI] [Google Scholar]
- 33.Singh A, Chatterjee K. Securing smart healthcare system with edge computing. Comput Secur. 2021;108(C):102353. doi: 10.1016/j.cose.2021.102353 [DOI] [Google Scholar]
- 34.Rahmani AM, Gia TN, Negash B, et al. Exploiting smart e-Health gateways at the edge of healthcare Internet-of-Things: a fog computing approach. Future Gener Comput Syst. 2018;78:641–658. doi: 10.1016/j.future.2017.02.014 [DOI] [Google Scholar]
- 35.Dave R, Seliya N, Siddiqui N. The benefits of edge computing in healthcare, smart cities, and IoT. JCSA. 2021;9(1):23–34. doi: 10.12691/jcsa-9-1-3 [DOI] [Google Scholar]
- 36.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011;1(1):53–71. doi: 10.1007/s13142-011-0021-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Axelrod YK, Diringer MN. Temperature management in acute neurologic disorders. Neurol Clin. 2008;26(2):585–603. doi: 10.1016/j.ncl.2008.02.005 [DOI] [PubMed] [Google Scholar]
- 38.Gong, Goldman, Lach. Deepmotion: a deep convolutional neural network on inertial body sensors for gait assessment in multiple sclerosis. In: 2016 IEEE Wireless Health (WH); 2016:1–8. [Google Scholar]
- 39.Li Q, Stankovic JA, Hanson MA, Barth AT, Lach J, Zhou G. Accurate, fast fall detection using gyroscopes and accelerometer-derived posture information. In: 2009 Sixth International Workshop on Wearable and Implantable Body Sensor Networks; 2009:138–143. [Google Scholar]
- 40.Ray P, Birolleau S, Lefort Y, et al. Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Critical Care. 2006;10(3):R82. doi: 10.1186/cc4926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gong J, Rose KM, Emi IA, et al. Home wireless sensing system for monitoring nighttime agitation and incontinence in patients with Alzheimer’s disease. In: Proceedings of the Conference on Wireless Health. ACM; 2015:1–8. [Google Scholar]
- 42.John J, Ravikumar A, Abraham B. Prostate cancer prediction from multiple pretrained computer vision model. Health Technol. 2021;11(5):1003–1011. doi: 10.1007/s12553-021-00586-y [DOI] [Google Scholar]
- 43.Robin M, Ravikumar A, John J. Classification of Histopathological Breast Cancer Images using Pretrained Models and Transfer Learning. In: Saraswat M, Sharma H, Balachandran K, Kim JH, Bansal JC, editors. Congress on Intelligent Systems. Springer Nature Singapore; 2022:587–597. [Google Scholar]
- 44.Almusallam N, Alabdulatif A, Alarfaj F. Analysis of privacy-preserving edge computing and internet of things models in healthcare domain. Comput Math Methods Med. 2021;2021:e6834800. doi: 10.1155/2021/6834800 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45.Sigwele T, Hu YF, Ali M, Hou J, Susanto M, Fitriawan H. An intelligent edge computing based semantic gateway for healthcare systems interoperability and collaboration. In: 2018 IEEE 6th International Conference on Future Internet of Things and Cloud (FiCloud); 2018:370–376. [Google Scholar]
- 46.Qureshi S, Xiong J. The role of mobile phones in the provision of equitable health care for human development; 2017:23.
- 47.Islam SMR, Kwak D, Kabir MDH, Hossain M, Kwak KS. The internet of things for health care: a comprehensive survey. IEEE Access. 2015;3:678–708. doi: 10.1109/ACCESS.2015.2437951 [DOI] [Google Scholar]
- 48.Jalali MS, Kaiser JP, Siegel M, Madnick S. The internet of things promises new benefits and risks: a systematic analysis of adoption dynamics of IoT products. IEEE Secur Priv. 2019;17(2):39–48. doi: 10.1109/MSEC.2018.2888780 [DOI] [Google Scholar]
- 49.NIST. NIST releases draft security feature recommendations for IoT devices. NIST; 2019. [Google Scholar]
- 50.Lee H, Park YR, Kim HR, et al. Discrepancies in demand of internet of things services among older people and people with disabilities, their caregivers, and health care providers: face-to-face survey study. J Med Internet Res. 2020;22(4):e16614. doi: 10.2196/16614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Verloo H, Kampel T, Vidal N, Pereira F. Perceptions about technologies that help community-dwelling older adults remain at home: qualitative study. J Med Internet Res. 2020;22(6):e17930. doi: 10.2196/17930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.S. Rubí JN, Gondim PR. IoMT platform for pervasive healthcare data aggregation, processing, and sharing based on OneM2M and OpenEHR. Sensors. 2019;19(19):4283. doi: 10.3390/s19194283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rubí JNS, Gondim PR. Interoperable internet of medical things platform for e-health applications. Int J Distrib Sens Netw. 2020;16(1):1550147719889591. doi: 10.1177/1550147719889591 [DOI] [Google Scholar]
- 54.Milosevic Z, Bond A. Digital health interoperability frameworks: use of RM-ODP standards. In: 2016 IEEE 20th International Enterprise Distributed Object Computing Workshop (EDOCW). IEEE; 2016:1–10. [Google Scholar]
- 55.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585–1592. doi: 10.1056/NEJMsr1503323 [DOI] [PubMed] [Google Scholar]
- 56.Nadarzynski T, Miles O, Cowie A, Ridge D. Acceptability of artificial intelligence (AI)-led chatbot services in healthcare: a mixed-methods study. Digit Health. 2019;5:2055207619871808. doi: 10.1177/2055207619871808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wisniewski H, Liu G, Henson P, et al. Understanding the quality, effectiveness and attributes of top-rated smartphone health apps. Evid Based Ment Health. 2019;22(1):4–9. doi: 10.1136/ebmental-2018-300069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Borycki E. Quality and safety in eHealth: building the evidence-base (Preprint). J Med Internet Res. 2019;2019:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lai Y, Yeung W, Celi LA. Urban intelligence for pandemic response: viewpoint. JMIR Public Health Surveill. 2020;6(2):e18873. doi: 10.2196/18873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wray A, Olstad DL, Minaker LM. Smart prevention: a new approach to primary and secondary cancer prevention in smart and connected communities. Cities. 2018;79:53–69. doi: 10.1016/j.cities.2018.02.022 [DOI] [Google Scholar]