Abstract
This study evaluated the effects of comprehensive functional nursing on functional recovery and quality of life in patients with spinal cord injuries (SCIs). A total of 214 patients with SCIs treated in our hospital from October 2019 to October 2021 were included in the retrospective analysis and divided into a general care group (n = 107) and a comprehensive care group (n = 107), based on the care that they received. Patients in the general care group received general functional nursing, whereas those in the comprehensive care group received a comprehensive functional nursing intervention. The Rivermead Mobility Index (RMI), Barthel Index (BI), and Berg Balance Score (BBS) were used to evaluate patient neurobehavioral ability before and after nursing. Changes in cardiopulmonary function indexes, left ventricular end-diastolic dimension (LVEDD), left ventricular end-systolic dimension (LVESD), vital capacity (VC), forced expiratory volume in 1 second (FEV1), FEV1/FVC, and maximal voluntary ventilation (MVV) were measured before and after nursing. The number of micturition, maximum micturition volume, bladder volume, residual urine volume, and lower urinary tract symptom (LUTS) score were recorded, and the improvement in bladder function were measured before and after nursing. The Hamilton Anxiety Scale (HAMA) and Beck Depression Inventory (BDI) scores were used to evaluate patients’ emotional state. After nursing, the RMI, BI, BBS score, FEV1, FEV1/FVC, MVV, maximum micturition volume, bladder volume, and SF-36 scores of the comprehensive care group were significantly higher than those of the general care group, and the LVEDD, LVESD, micturition time, residual urine volume, and LUTS, HAMA, and BDI scores of the comprehensive care group were significantly lower than those of the general care group. In patients with SCIs, comprehensive functional nursing can promote the recovery of neurocognition, bladder function, and cardiorespiratory function, and improve their quality of life. Comprehensive functional nursing is worthy of clinical application.
Keywords: bladder function, cardiopulmonary function, comprehensive strengthening function intervention, intestinal function, spinal cord injury
1. Introduction
Spinal cord injury (SCI) is a serious, disabling trauma caused by car accidents, falls, and sports injuries. It mainly manifests as an impairment of normal functions, such as sensation, movement, reflexes, and autonomic nerve function.[1,2] Multiple clinical and animal experiments have established that in patients with incomplete SCIs, surgery, traditional Chinese medicine, acupuncture, and gene therapy can promote limited functional recovery, but more effective interventions are needed.[3–6]
In patients with SCIs, the main injury locations include the thoracic, lumbosacral, and cervical regions.[7,8] Corresponding strengthening function interventions are needed for injuries at different locations. In recent years, studies have confirmed that rehabilitation training interventions can effectively reduce secondary injury, restore spinal cord function, reduce the incidence of complications, and restore normal spinal cord function to the greatest extent.[9–11] Patients with thoracic and lumbosacral injuries rely only on their arms for relevant physical activities. The overall aerobic exercise ability of patients decreases, and their muscle and physical activity are relatively low, which leads to the loss of respiratory muscles and limits their autonomous activity ability.[11] Cardiopulmonary fitness assessment in patients with thoracolumbar SCIs and corresponding cardiopulmonary function training can effectively improve prognosis.[12] SCIs may lead to interruption of bladder innervation and loss of physiological function. Patients with bladder dysfunction are prone to complications, such as urinary retention, vesicoureteral reflux, and urinary tract infection, which can lead to renal failure and death in severe cases.[13,14] Recovery of bladder function in patients with SCIs plays an important role in reducing complications and mortality. SCIs slow intestinal peristalsis, lead to loss of automatic control of anal sphincter, and ability to voluntarily increase intra-abdominal pressure, resulting in neurogenic intestinal dysfunction, leading to constipation, abdominal distension, and other symptoms.[15,16] Approximately half of patients with SCIs have mild to severe intestinal dysfunction, and most of them occur in the early stage.[17] In the acute stage of SCI, patients can experience abdominal fullness and paralytic intestinal obstruction due to gastrointestinal peristalsis, which affects the movement of the diaphragm and causes respiratory distress in patients with quadriplegia. After this period, the spinal cord reflex recovers and there is passage of gas, but it is still difficult to defecate autonomously. If defecation difficulties persist, it affects digestion, absorption, and nutrition.[18] Therefore, strengthening intestinal function in patients with SCIs is important for their prognosis. Because patients with SCIs lose motor function and experience urinary incontinence, and it is difficult to recover their lives. The vast majority of patients cannot take care of themselves and need to be taken care of by others.[19] Due to long-term bed rest, a variety of complications can coexist, causing great pain and psychological obstacles for patients. Therefore, it is necessary to pay attention to the psychological state of patients to comprehensively strengthen their function.
Based on previous studies, we proposed 2 hypotheses: comprehensive functional nursing might promote the recovery of neurocognition, bladder function, and cardiorespiratory function in patients with SCIs and comprehensive functional nursing may improve quality of life in patients with SCIs. We conducted this study to explore the effect of comprehensive functional nursing on patients with SCIs.
2. Materials and methods
2.1. Study design and participants
This study was a retrospective study. It was approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University (Ref. no. 2157/2021), and conformed to the Declaration of Helsinki. All patients with SCIs admitted to our hospital from October 2019 to October 2021 were selected for this study. The patients were divided into a general care group (n = 107) and a comprehensive care group (n = 107) based on the different care. Patients in the general care group received general functional nursing, whereas the comprehensive care group received a comprehensive functional nursing intervention.
2.2. Inclusion and exclusion criteria
Inclusion criteria: Patients were eligible for inclusion if they met the diagnostic criteria for SCI, the spinal cord shock period had ended, and their condition was stable. The patients and their families were required to be willing to participate and provide voluntarily written informed consent, and to be able to complete the 5-month follow-up. Exclusion criteria: Patients with severe liver or kidney dysfunction, coagulation disorders, cognitive impairment, intestinal or bladder dysfunction unrelated to the SCI, and those unwilling to participate were excluded. Patients lost during follow-up were also excluded.
2.3. Sample size
This was a retrospective study and the sample size was not based on statistical power calculations. All patients who met the inclusion criteria were included in the study.
2.4. Nursing methods
2.4.1. Rehabilitation training nursing.
The patients in the general care group received general rehabilitation training nursing. General rehabilitation training primarily includes limb joint activity maintenance, muscle strength enhancement, sensory stimulation, and sitting and standing balance. Patients were provided with strength training of the undamaged arm muscles; strength and coordination training of the connection between the lower back muscles and abdominal muscles; and the legs were mainly used to enhance motor control. Sensory stimulation included tactile stimulation with a soft bristle brush; temperature stimulation with brief local ice application; and proprioceptive stimulation with traction, tapping, or compression.
The patients in the comprehensive care group received intensive rehabilitation training nursing based on general rehabilitation training; early strength rehabilitation training at the bedside, which consisted mainly of active and passive movement of each joint of the affected limb, focusing on the shoulder, elbow, wrist, metacarpal, hip, and knee joints. The training was conducted twice a day for 30 minutes at a time. Sitting and standing balance training started using an inclined bed, and gradually progressed to sitting and standing balance, and finally, transitioned to walking practice. Daily life training mainly included eating, going to the toilet, putting on and taking off clothes.
2.4.2. Cardiopulmonary function training.
Patients with thoracic and lumbosacral injuries have cardiopulmonary dysfunction. Patients in the general care group received posture nursing, second stool management, joint activity training, muscle strength training, exercise transfer ability training, life activity ability training, and health education.
Patients in the comprehensive care group received cardiopulmonary function training based on general training. Patients in the comprehensive care group used the arm muscles for aerobic exercise training and a pulmonary function test system for the cardiopulmonary function exercise test. Based on the results of the cardiopulmonary function exercise test, 40% to 60% of the VO2peak was selected as the aerobic exercise intensity. The nurse assisted the patient with using a wheelchair, putting on a mask, connecting the exhalation tube, electrocardiogram, cuff blood pressure, and infrared blood oxygen saturation monitor, and used the symptom self-limiting exercise scheme to exercise to the maximum tolerance of the patient. The patients rested for 2 minutes, 30 minutes once a day, 5 days a week, before exercise. During exercise, the patient exhaled through a breath collection tube connected to an analyzer, oxygen uptake was measured through breath-by-breath mode, and the patient electrocardiogram and transcutaneous oxygen saturation were monitored in real time. Blood pressure was measured every 2 to 3 minutes to ensure patient safety. The exercise laboratory was equipped with an oxygen inhalation device, electric defibrillator, and first-aid drugs to prevent accidents. Based on the patient symptom self-limit, the exercise could not be maintained at more than 80 times/min with maximum effort. At this time, VO2max, peak energy metabolic equivalent, and other indicators were measured to determine whether the patient had reached their maximum exercise load. The exercise was terminated if the patient felt extremely tired and asked to stop the test; VO2max plateaued or began to decline; or if they experienced adverse cardiovascular events such as chest pain during exercise.
2.4.3. Bladder function training.
Patients with bladder dysfunction were treated for bladder dysfunction. Patients in the general care group were treated with bladder drainage. Patients in the comprehensive care group received intensive interventions for bladder function which included respiratory muscle training, abdominal muscle training, sitting and standing training, bladder training, intermittent clean catheterization, and application of pelvic floor muscle stimulation instruments.
2.4..4. Cognitive behavioral intervention.
The patients in the general care group were treated with hormone dehydration and nerve nutrition. In addition to conventional treatment methods, patients in the comprehensive care group were given cognitive behavioral therapy. First, the doctor asked the patient to explain their thoughts and understanding of their SCI, and then, under the guidance and direction of the doctor, patients were informed of their physical condition and prognosis. The doctor corrected misconceptions and unrealistic expectations and encouraged patients to rebuild a healthy, effective, and functional attitude, and improve their psychology and behavior. The patients were trained in psychological methods of regulating physical and mental comfort and accepting active treatment.
2.5. Outcome indicators
2.5.1. Neurobehavioral assessment.
The Rivermead Mobility Index (RMI), Barthel Index (BI), and Berg Balance Score (BBS) were used to evaluate neurobehavioral ability.[20–22] RMI is an intuitive evaluation of a patient motor function. The evaluation is divided into 15 items. According to the scoring standard, options that met the condition were assigned 1 point, and those that could not be completed were recorded as 0 points. The maximum possible score was 15. The BI was used to evaluate the living ability of the patients, with a maximum possible score of 100. The trunk balance function of the patients was evaluated according to the BBS scoring standard; The BBS consists of a total of 14 items, with a maximum possible score of 56. The lower the score, the more serious the balance dysfunction, and a score <40 points suggested a risk of falling.
2.5.2. Detection of cardiopulmonary function indexes.
Doppler echocardiography was used to guide the patients to lie still in the left position, control their respiratory rate, and stabilize it. The left ventricular end-diastolic dimension (LVEDD) and left ventricular end-systolic dimension (LVESD) were compared before and after the intervention. The lung function of the patients was measured using the MasterScope lung function detection system and analysis software (eResearchTechnology GmbH, Estenfeld, Germany), including vital capacity (VC), forced expiratory volume in 1 second (FEV1), FEV1/FVC, and maximum voluntary ventilation (MVV). The pulmonary function levels before and after the intervention were compared.
2.5.3. Bladder function evaluation.
From 7 days before treatment to 7 days after treatment, the daily micturition times, maximum micturition volume, bladder volume, residual urine volume, quality of life score affected by micturition symptoms, and international lower urinary tract symptoms (LUTS) were recorded to evaluate the therapeutic effect.[23]
2.5.4. Cognitive assessment.
The Hamilton Anxiety Scale (HAMA) and Beck Depression Inventory (BDI) were used to evaluate the patients’ emotional state,[24,25] and the SF-36 score was used to evaluate their quality of life. The HAMA cutoff value was 14 points, with more than 21 points indicating obvious anxiety and more than 29 points indicating serious anxiety. The cutoff value of the BDI was 17 points; with 17 to 20 points indicating borderline depression, and more than 20 points indicating severe depression. The SF-36 score includes items on overall health, physical pain, physiological function, social function, vitality, and mental health.
2.6. Data collection and statistical analysis
Relevant clinical data were collected from the hospital electronic medical record system. All data were analyzed using SPSS version 26.0 (IBM Corp., Armonk, NY). Continuous data were described using the mean ± standard deviation and the groups were compared using t tests. Categorical data were described using frequencies and proportions, and the groups were compared using chi-square tests. P values < .05 was considered statistically significant.
3. Results
3.1. Comparison of clinical data of patients
This study included 132 male and 82 female patients, with a mean age of 44.4 ± 9.9 years. The general care group comprised 64 male patients and 43 female patients, aged from 21 to 74 years, with a mean age of 43.8 ± 8.9 years, of whom 76 had an incomplete injury and 31 had a complete injury. The SCI location included 58 cases of thoracic injury, 31 cases of lumbosacral injury, and 18 cases of cervical injury. The comprehensive care group comprised 68 male patients and 39 female patients, aged from 23 to 75 years, with a mean age of 45.1 ± 9.6 years, of whom 73 had an incomplete injury and 34 had a complete injury. The SCI location included 52 cases of thoracic injury, 28 cases of lumbosacral injury, and 27 cases of cervical injury. There were no significant differences between the 2 groups.
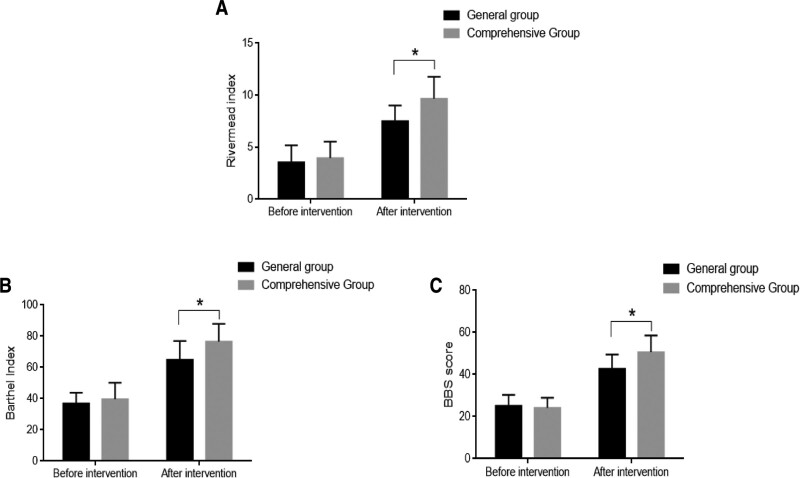
3.2. Neurobehavioral assessment
Before the intervention, there were no significant differences in RMI, BI, and BBS scores between the comprehensive care and general care groups. After the intervention, the RMI (Fig. 1A), BI (Fig. 1B), and BBS scores (Fig. 1C) were significantly higher in the comprehensive care group than in the general care group.
Figure 1.
Comparison of neurobehavioral between the comprehensive care and general care groups. (A) Rivermead Mobility Index (RMI); (B) Barthel Index (BI); and (C) Berg Balance Score (BBS). *P < .05.
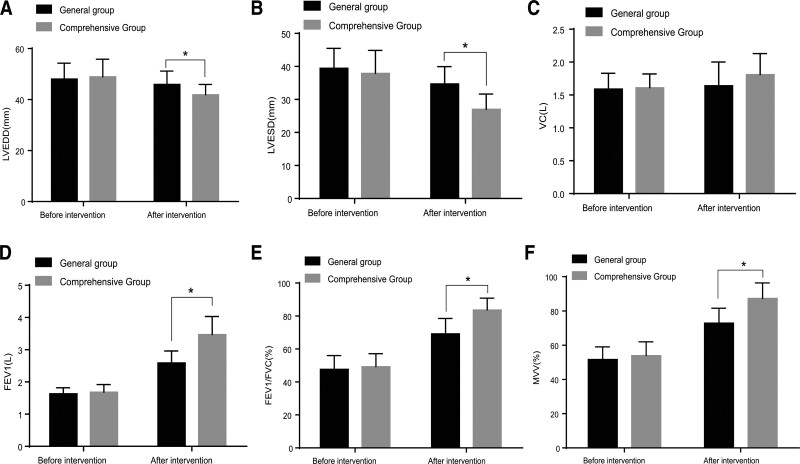
3.3. Detection of cardiopulmonary function indexes
We recorded the LVEDD (Fig. 2A), LVESD (Fig. 2B), VC (Fig. 2C), FEV1 (Fig. 2D), FEV1/FVC ratio (Fig. 2E), and MVV (Fig. 2F) indexes of the 2 groups before and after the intervention to evaluate changes in cardiopulmonary function. Before the intervention, there were no significant differences in the various indexes of cardiopulmonary function between the comprehensive and general care groups. After the intervention, the indexes of LVEDD (Fig. 2A) and LVESD (Fig. 2B) in the comprehensive care group were significantly lower than those in the general care group, and the indexes of FEV1, FEV1/FVC, and MVV in the comprehensive care group were significantly higher than those in the general care group.
Figure 2.
Comparison of cardiorespiratory function indexes between the comprehensive care and general care groups. (A) Left ventricular end-diastolic dimension (LVEDD); (B) left ventricular end-systolic dimension (LVESD); (C) vital capacity (VC); (D) forced expiratory volume in 1 second (FEV1); (E) FEV1/FVC; and (F) maximal voluntary ventilation (MVV). *P < .05.
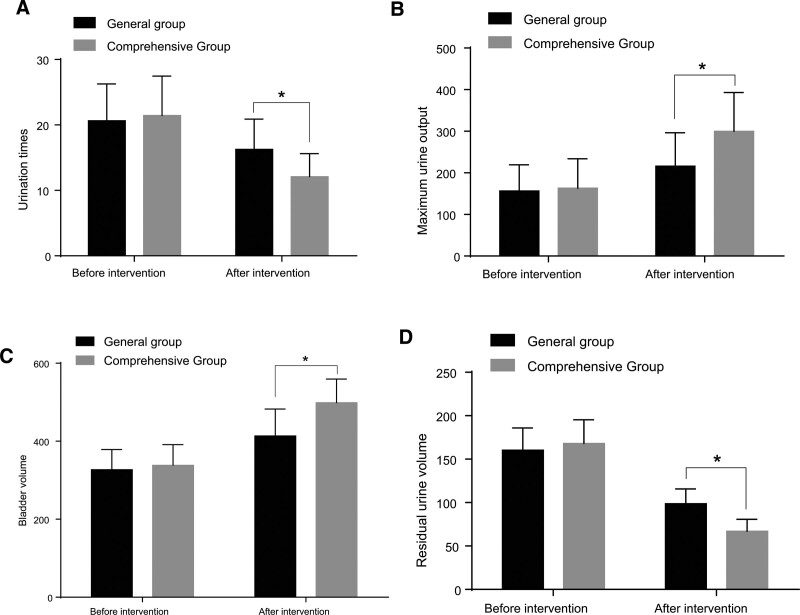
3.4. Bladder function evaluation
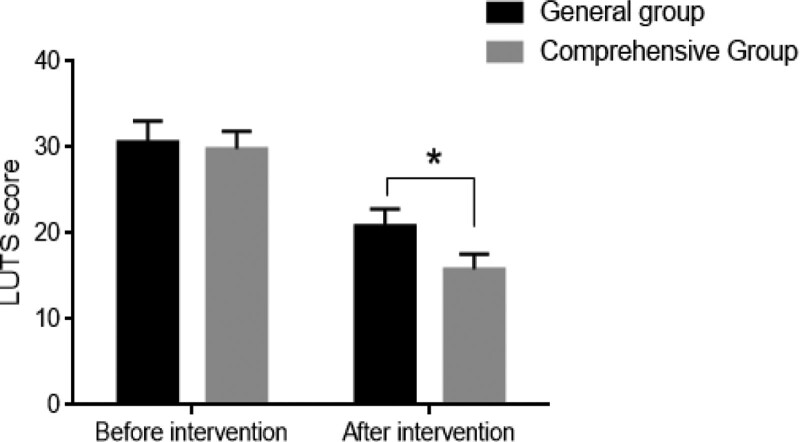
In order to explore the recovery of bladder function in the 2 groups, we compared micturition times (Fig. 3A), maximum micturition volume (Fig. 3B), bladder volume (Fig. 3C), residual urine volume (Fig. 3D), and LUTS scores (Fig. 4) between the 2 groups. Before the intervention, there were no significant differences in urination time, maximum urination volume, bladder volume, residual urine volume, and LUTS score between the general and comprehensive care groups. After the intervention, the number of micturition, residual urine volume, and LUTS scores in the comprehensive care group were significantly lower than those in the general care group, and the maximum micturition and bladder volumes were significantly higher than those in the general care group.
Figure 3.
Comparison of bladder function between the comprehensive care and general care groups. (A) Micturition times; (B) maximum micturition volume; (C) bladder volume; and (D) residual urine volume. *P < .05.
Figure 4.
Comparison of lower urinary tract symptom (LUTS) score between the comprehensive care and general care groups. *P < .05.
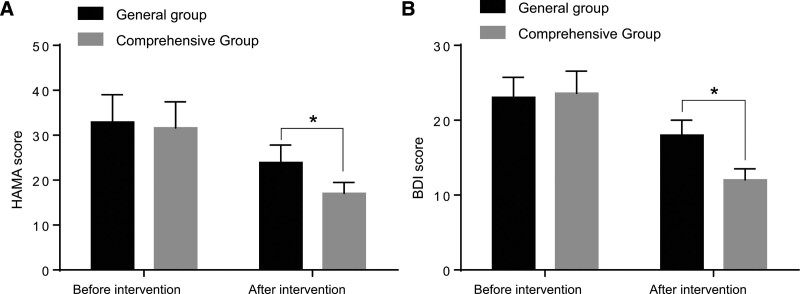
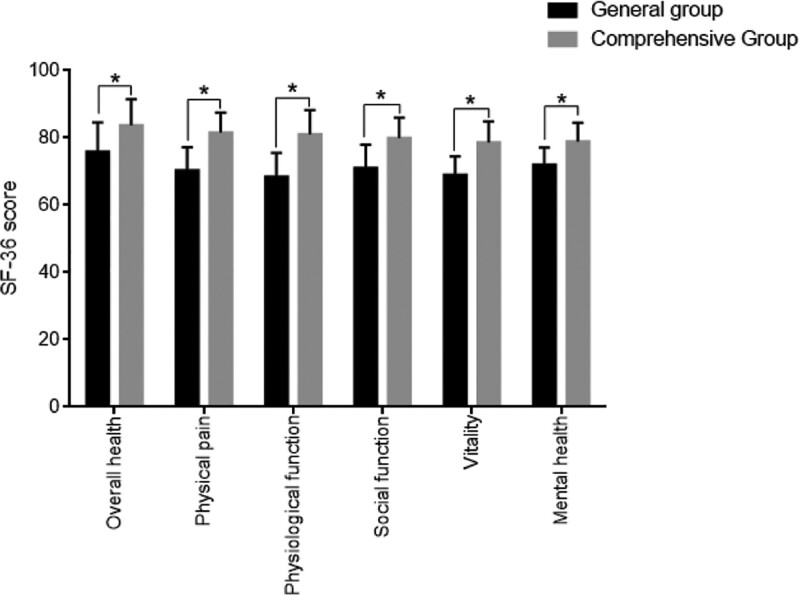
3.5. Assessment of patients’ emotional state and quality of life
Patients’ emotional status was assessed using the HAMA (Fig. 5A) and BDI scores (Fig. 5B), and their quality of life was assessed using the SF-36 score (Fig. 6). The HAMA and BDI scores of patients in the comprehensive care group were significantly lower than those of patients in the general care group, whereas the SF-36 scale was significantly higher than those in the general care group.
Figure 5.
Comparison of patients’ emotional state between the comprehensive care and general care groups. (A) Hamilton Anxiety Scale (HAMA) score and (B) Beck Depression Inventory (BDI) score. *P < .05.
Figure 6.
Comparison of SF-36 score between the comprehensive care and general care groups. *P < .05.
4. Discussion
SCI refers to damage to the structure and function of the spinal cord caused by trauma or disease, resulting in spinal cord nerve dysfunction. After SCI, patients develop paraplegia, quadriplegia, and other symptoms that mostly cause motor dysfunction, loss of their ability to work, and reduced quality of life.[26,27] Only the restoration of limb function and reconstruction can improve patients’ quality of life, but the etiology of SCI is complex, with a high morbidity, and is often complicated buy other diseases.[28] The results of this study showed that patients who received a comprehensive intensive functional intervention had a significantly greater improvement than those who received a general functional intervention.
The RMI, BI, BBS score, FEV1, FEV1/FVC, MVV, maximum micturition volume, bladder volume, and SF-36 scores of the comprehensive care group were significantly higher than those of the general care group, and the LVEDD, LVESD, micturition times, residual urine volume, LUTS, HAMA, and BDI scores of the comprehensive care group were significantly lower than those of the general care group. After systematic rehabilitation training and nursing, the motor function and quality of life of patients with SCIs can significantly improve.[29] Rehabilitation training should be carried out as soon as possible after surgical treatment of SCI, and the intervention mode of rehabilitation training should be determined according to the location and degree of injury. The time, intensity, and content of rehabilitation training should be gradually increased according to the patient condition.[30,31] Rehabilitation training intervention plays an important role in the functional recovery of patients with SCIs. In the early stages of an SCI, the limbs show flaccid paralysis owing to spinal cord shock. It is necessary to maintain a good functional position of the paralyzed limbs, perform passive joint activity training every day, and change the body position regularly to prevent joint contracture, pressure ulcers, and osteoporosis to lay a foundation for the next phase of the rehabilitation training.[32,33] Patients with SCI can experience a variety of complications, which has adverse effects on their cure and process of rehabilitation.[34] Therefore, active prevention and treatment of complications are important for the rehabilitation of SCI. This study showed that the RMI, BI, and BBS scores of patients receiving comprehensive strengthening function interventions were significantly higher than those of patients in the general care group, indicating that the neurological and motor function recovery of patients who received the comprehensive intensive functional intervention was significant, which is consistent with the results of previous studies.[32,33]
The sudden decrease in exercise in patients with SCIs reduces their physical fitness and tolerance and then increases the burden on the heart and lungs, leading to heart- and lung-related complications. In addition, the nerves of patients with SCIs are also damaged, which limits their motor function and physical activity, thus increasing the incidence of cardiovascular and pulmonary diseases.[35,36] In the resting state, the heart rate of patients with SCIs is significantly accelerated, which indicates that in the case of reduced body activity, the patient autonomic nerve function is damaged, the response of systolic blood pressure to exercise stimulation is significantly reduced, and the reactivity of blood vessels to exercise is reduced, resulting in related cardiovascular diseases.[37,38] Our study showed that the indexes of cardiopulmonary function FEV1, FEV1/FVC, and MVV of patients receiving comprehensive functional nursing were significantly higher than those of patients receiving general nursing, and the indexes of LVEDD and LVESD were significantly lower than those of patients receiving general nursing, which indicates that comprehensive functional nursing has a good recovery effect on cardiopulmonary function in patients with SCIs, which is consistent with the results of previous studies.[35–38]
SCI can lead to bladder emptying disorders. Although indwelling catheters can solve the problem of urinary retention, long-term indwelling catheters have many complications, and can lead to urinary tract infections, kidney stones, and epididymitis, and adversely affect rehabilitation training.[39,40] In injuries above the spinal cord cone, the detrusor muscle has no inhibitory contraction, and the internal pressure of the bladder increases, which can lead to ureteral reflux and hydronephrosis. Repeated urinary tract infection, stones, and hydronephrosis gradually cause deterioration in renal function. Renal failure is the primary cause of late death in patients with SCIs.[41–43] Therefore, scientific bladder management and training important for reducing urinary complications and improving the quality of life of patients with SCIs. This study showed that the number of micturition, residual urine volume, and LUTS score in the comprehensive care group were significantly lower than those in the general care group, and maximum urine and bladder volumes in the comprehensive care group were significantly higher than those in the general care group, suggesting that comprehensive functional nursing can promote the recovery of bladder function in patients with SCI.
This study has several limitations. First, the small sample size is a major limitation. Second, the study was the single-center study and was conducted in a Chinese population, so the findings might not be generalizable to other populations.
5. Conclusion
In conclusion, comprehensive functional nursing for patients with SCIs can significantly restore their neurobehavioral, cardiopulmonary, intestinal, and bladder functions; improve their emotional state; and improve their quality of life. However, the follow-up period was limited, and the results need to be verified by conducting larger multicenter studies.
Author contributions
Conceptualization: Qing Dai.
Data curation: Qing Dai, Zhen Li.
Formal analysis: Qing Dai, Chenxia Liao, Xin Gao.
Funding acquisition: Xixuan Jiang, Lunlan Li, Qing Dai, Jing Liu, Jing Wang.
Investigation: Xixuan Jiang, Qing Dai, Lei Tao, Xin Gao.
Methodology: Xixuan Jiang, Qing Dai, Jing Liu, Zhen Li, Jing Wang, Chenxia Liao.
Project administration: Yang Ding, Xixuan Jiang, Qing Dai, Xin Gao.
Resources: Yang Ding, Xixuan Jiang, Qing Dai, Lei Tao, Jing Liu, Jing Wang.
Software: Yang Ding, Xixuan Jiang, Chenxia Liao.
Supervision: Yang Ding, Xixuan Jiang, Jing Liu, Zhen Li, Jing Wang, Xin Gao.
Validation: Yang Ding, Lei Tao.
Visualization: Yang Ding, Xin Gao.
Writing – original draft: Yang Ding, Zhen Li, Chenxia Liao.
Writing – review & editing: Yang Ding, Lei Tao.
Abbreviations:
- BBS
- Berg balance score
- BDI
- beck depression inventory
- BI
- Barthel Index
- FEV1
- forced expiratory volume in 1 second
- HAMA
- Hamilton Anxiety
- LUTS
- lower urinary tract symptoms
- LVEDD
- left ventricular end-diastolic dimension
- LVESD
- left ventricular end-systolic dimension
- MVV
- maximal voluntary ventilation
- RMI
- Rivermead Mobility Index
- SCI
- spinal cord injury
- VC
- vital capacity
YD and XJ contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Ding Y, Jiang X, Li L, Dai Q, Tao L, Liu J, Li Z, Wang J, Liao C, Gao X. Effects of comprehensive functional nursing on functional recovery and quality of life in patients with spinal cord injury. Medicine 2023;102:38(e35102).
Contributor Information
Yang Ding, Email: 15056068084@163.com.
Xixuan Jiang, Email: jiangxixuan@aliyun.com.
Qing Dai, Email: daiqing@163.com.
Lei Tao, Email: taolei1226@163.com.
Jing Liu, Email: wangjing@163.com.
Zhen Li, Email: lizhen@163.com.
Jing Wang, Email: wangjing@163.com.
Chenxia Liao, Email: 15855127626@163.com.
Xin Gao, Email: gaoxin@163.com.
References
- [1].Zipser CM, Cragg JJ, Guest JD, et al. Cell-based and stem-cell-based treatments for spinal cord injury: evidence from clinical trials. Lancet Neurol. 2022;21:659–70. [DOI] [PubMed] [Google Scholar]
- [2].Kirshblum S, Snider B, Eren F, et al. Characterizing natural recovery after traumatic spinal cord injury. J Neurotrauma. 2021;38:1267–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Gong D, Wang Y, Zhong L, et al. Excretory dysfunction and quality of life after a spinal cord injury: a cross-sectional study. J Clin Nurs. 2021;30:1394–402. [DOI] [PubMed] [Google Scholar]
- [4].Chay W, Kirshblum S. Predicting outcomes after spinal cord injury. Phys Med Rehabil Clin. 2020;31:331–43. [DOI] [PubMed] [Google Scholar]
- [5].Fan Q, Cavus O, Xiong L, et al. Spinal cord injury: how could acupuncture help? J Acupunct Meridian Stud. 2018;11:124–32. [DOI] [PubMed] [Google Scholar]
- [6].Bo X, Wu D, Yeh J, et al. Gene therapy approaches for neuroprotection and axonal regeneration after spinal cord and spinal root injury. Curr Gene Ther. 2011;11:101–15. [DOI] [PubMed] [Google Scholar]
- [7].Shortiss C, Howard L, McMahon SS. Lentiviral vectors delivered with biomaterials as therapeutics for spinal cord injury. Cells. 2021;10:2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Abu-Baker NN, Al-Zyoud NH, Alshraifeen A. Quality of life and self-care ability among individuals with spinal cord injury. Clin Nurs Res. 2021;30:883–91. [DOI] [PubMed] [Google Scholar]
- [9].Anjum A, Yazid MD, Fauzi Daud M, et al. Spinal cord injury: pathophysiology, multimolecular interactions, and underlying recovery mechanisms. Int J Mol Sci. 2020;21:7533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bender AA, Burgess EO. Constructing recovery narratives: experiences and expectations following spinal cord injury. Rehabil Nurs J. 2020;45:254–62. [DOI] [PubMed] [Google Scholar]
- [11].Pryor J, Haylen D, Fisher M. Problems people with spinal cord injury experience accessing help with bowel care when hospitalised outside a specialist spinal injury service. J Clin Nurs. 2021;30:1633–44. [DOI] [PubMed] [Google Scholar]
- [12].Selph SS, Skelly AC, Wasson N, et al. Physical activity and the health of wheelchair users: a systematic review in multiple sclerosis, cerebral palsy, and spinal cord injury. Arch Phys Med Rehabil. 2021;102:2464–2481.e33. [DOI] [PubMed] [Google Scholar]
- [13].Li Q-P, Li J, Pan H-Y. Effects of online home nursing care model application on patients with traumatic spinal cord injury. Risk Manag Healthc Policy. 2021;14:1703–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ahuja CS, Mothe A, Khazaei M, et al. The leading edge: Emerging neuroprotective and neuroregenerative cell-based therapies for spinal cord injury. Stem Cells Transl Med. 2020;9:1509–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].van Diemen T, van Nes IJ, van Laake-Geelen CC, et al. Learning self-care skills after spinal cord injury: a qualitative study. BMC Psychol. 2021;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Liu C-H, Zhao B-L, Li W-T, et al. Changes in depressive-like behaviors induced by spinal cord injury based on the hypothalamic-pituitary-adrenal axis and hippocampal neurogenesis. J Integr Neurosci. 2021;20:635–44. [DOI] [PubMed] [Google Scholar]
- [17].Sharif S, Ali MYJ. Outcome prediction in spinal cord injury: myth or reality. World Neurosurg. 2020;140:574–90. [DOI] [PubMed] [Google Scholar]
- [18].Cox A, Capone M, Matzelle D, et al. Nanoparticle-based estrogen delivery to spinal cord injury site reduces local parenchymal destruction and improves functional recovery. J Neurotrauma. 2021;38:342–52. [DOI] [PubMed] [Google Scholar]
- [19].Lee S, Wilkins N, Schmit BD, et al. Relationships between spinal cord blood flow measured with flow-sensitive alternating inversion recovery (FAIR) and neurobehavioral outcomes in rat spinal cord injury. Magn Reson Imaging. 2021;78:42–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Collen FM, Wade DT, Robb GF, et al. The Rivermead Mobility Index: a further development of the rivermead motor assessment. Int Disabil Stud. 1991;13:50–4. [DOI] [PubMed] [Google Scholar]
- [21].Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5. [PubMed] [Google Scholar]
- [22].Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27:27–36. [PubMed] [Google Scholar]
- [23].Roehrborn CG. Male lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Med Clin. 2011;95:87–100. [DOI] [PubMed] [Google Scholar]
- [24].Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–5. [DOI] [PubMed] [Google Scholar]
- [25].Lee NY, Lee DK, Song HS. Effect of virtual reality dance exercise on the balance, activities of daily living, and depressive disorder status of Parkinson’s disease patients. J Phys Ther Sci. 2015;27:145–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Guérout N. Plasticity of the injured spinal cord. Cells. 2021;10:1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Li J, Li Q-P, Yang B-H. Participatory continuous nursing using the WeChat platform for patients with spinal cord injuries. J Int Med Res. 2021;49:3000605211016145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Vázquez-Fariñas M, Rodríguez-Martin B. “Living with a fragmented body”: a qualitative study on perceptions about body changes after a spinal cord injury. Spinal Cord. 2021;59:855–64. [DOI] [PubMed] [Google Scholar]
- [29].Chen Q, Zhao Z, Yin G, et al. Identification and analysis of spinal cord injury subtypes using weighted gene co-expression network analysis. Ann Transl Med. 2021;9:466–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hosseini M, Sarveazad A, Babahajian A, et al. Effect of vitamins C and E on recovery of motor function after spinal cord injury: systematic review and meta-analysis of animal studies. Nutr Rev. 2020;78:465–73. [DOI] [PubMed] [Google Scholar]
- [31].Pryor J, Haylen D, Fisher MJ. The usual bowel care regimes of people living in the community with spinal cord injury and factors important for integrating bowel care into everyday life. Disabil Rehabil. 2022;44:6401–7. [DOI] [PubMed] [Google Scholar]
- [32].Aarabi B, Akhtar-Danesh N, Simard JM, et al. Efficacy of early (≤ 24 hours), Late (25–72 hours), and Delayed (> 72 hours) surgery with magnetic resonance imaging-confirmed decompression in American spinal injury association impairment scale grades C and D acute traumatic central cord syndrome caused by spinal stenosis. J Neurotrauma. 2021;38:2073–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Prang P, Schuld C, Rupp R, et al. Influence of patient isolation due to colonization with multidrug-resistant organisms on functional recovery after spinal cord injury. PLoS One. 2021;16:e0249295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rao J-S, Zhao C, Bao S-S, et al. MRI metrics at the epicenter of spinal cord injury are correlated with the stepping process in rhesus monkeys. Exp Anim. 2022;71:139–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Vasudevan D, Liu Y-C, Barrios JP, et al. Regenerated interneurons integrate into locomotor circuitry following spinal cord injury. Exp Neurol. 2021;342:113737. [DOI] [PubMed] [Google Scholar]
- [36].Inanici F, Brighton LN, Samejima S, et al. Transcutaneous spinal cord stimulation restores hand and arm function after spinal cord injury. IEEE Trans Neural Syst Rehabil Eng. 2021;29:310–9. [DOI] [PubMed] [Google Scholar]
- [37].Marquez-Chin C, Popovic MR. Functional electrical stimulation therapy for restoration of motor function after spinal cord injury and stroke: a review. Biomed Eng Online. 2020;19:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Fouad K, Popovich PG, Kopp MA, et al. The neuroanatomical–functional paradox in spinal cord injury. Nat Rev Neurol. 2021;17:53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Weber L, Voldsgaard NH, Holm NJ, et al. Exploring the contextual transition from spinal cord injury rehabilitation to the home environment: a qualitative study. Spinal Cord. 2021;59:336–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Majidpoor J, Mortezaee K, Khezri Z, et al. The effect of the “segment” of spinal cord injury on the activity of the nucleotide-binding domain-like receptor protein 3 inflammasome and response to hormonal therapy. Cell Biochem Funct. 2021;39:267–76. [DOI] [PubMed] [Google Scholar]
- [41].Wood C, Cutshall SM, Lawson DK, et al. Music therapy for anxiety and pain after spinal cord injury: a pilot study. Glob Adv Health Med. 2021;10:21649561211058697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Kim Y, Cho MH, Do K, et al. Incidence and risk factors of urinary tract infections in hospitalised patients with spinal cord injury. J Clin Nurs. 2021;30:2068–78. [DOI] [PubMed] [Google Scholar]
- [43].Van Broeckhoven J, Sommer D, Dooley D, et al. Macrophage phagocytosis after spinal cord injury: when friends become foes. Brain. 2021;144:2933–45. [DOI] [PubMed] [Google Scholar]