Abstract
Children who have been sexually abused may experience various short- and long-term psychological sequelae and behavioral problems. This study assessed the mental health of sexually abused children using the Korean-Child Behavior Checklist (K-CBCL) and examined differences from a control group. The participants were 97 children who had been sexually abused and who visited a local Sunflower Center, and 178 control participants. Data were collected via the K-CBCL and analyzed using SPSS version 25.0. T-tests, cross-tabulation, and logistic regression analyses were performed. Scores from the K-CBCL Problem Behavior Syndrome scale were compared between sexually abused children and the control participants. Significant differences were observed between the 2 groups in all the subscales. Compared to the control group, children who were sexually abused showed statistically significant differences in the total problem behavior, internalization, anxiety/depression, withdrawal/depression (withdrawn), somatic symptoms, externalization, rule-breaking behavior (delinquency), aggressive behavior, social immaturity, thought problems, attention problems, and other subscale scores. Sexual violence hurts the overall mental health of children who are abused, including their emotional, behavioral, and social factors. Our findings suggest that multidisciplinary assessment and treatment are required for children who have experienced sexual abuse.
Keywords: child behavior checklist, mental health, psychological sequelae, psychopathology, sexually abused children
1. Introduction
Sexual violence has a more significant impact on an individual’s physical and mental health than other types of crimes. The effects also persist for longer.[1–4] For children, the trauma of sexual violence can last until adolescence and even adulthood, resulting in negative life-long effects. Children who were sexually abused report symptoms such as depression, anxiety, post-traumatic stress, low self-esteem, self-harm, and inappropriate sexual behavior. Adolescents who have experienced childhood sexual abuse are more likely to run away from home, use alcohol, have suicidal thoughts, attempt suicide, and exhibit lower academic performance. Sexual abuse in childhood is associated with various psychopathologies and overall functional decline. Furthermore, minors who were sexually abused continue to experience depressive disorders, eating disorders, suicidal tendencies, sexual problems, high divorce rates, and low job performance even after they become adults.[5–8]
Sexual violence is an act in which 1 intentionally performs sexual acts without the consent of the other party or coerces or physically forces a person to engage in sexual acts against their will, and is classified as sexual harassment, sexual assault, or rape (Act on Special Cases Concerning the Punishment, etc of Sexual Crimes).
According to statistics from the United Nations Office on Drugs and Crime, the number of cases of sexual violence worldwide were: 44 countries/207,648 events in 2012 and 35 countries/308,482 events in 2021 in Europe; 25 and 21 countries/185,695 and 202,333 events in 2012 and 2021, respectively, in America; 2 and 2 countries/22,837 and 40,511 events in 2012 and 2021, respectively, in Oceania; 23 and 12 countries/131,790 and 39,486 cases in 2012 and 2021, respectively, in Asia; and 8 and 6 countries/21,017 and 19,753 events in 2012 and 2021, respectively, in Africa. Compared to 10 years ago, the number of countries that reported sexual violence decreased. However, sexual violence increased over the past 10 years in Europe, the Americas, and Oceania, although not in Asia and Africa where it was difficult to observe an increasing or decreasing trend.
The number of sexual assault cases in Korea continue to increase. According to a crime analysis in 2022,[9] there were 1210 sexual crimes against children aged under 13 years in 2021. Over the past 10 years, such sexual crimes have increased by 7.4%.[9] The actual incidence of sexual crimes against children was estimated to be much higher as it was difficult for children to make accurate statements and may under-report their victimization owing to social prejudice against sexual violence.[10,11] Of the sexually abused children, 88.7% were girls aged under 13 years. Regarding the specific types of sexual crimes, indecent assault accounted for 65.8% (796 cases), followed by rape (19.5%, 236 cases), and obscene acts using communication media (7.2%, 87 cases). Regarding the relationship between the perpetrator and victim, strangers accounted for 57.5%, followed by relatives (17.3%) and neighbors/acquaintances (13.8%).[9]
Children are inexperienced in expressing their psychological state or pain appropriately. Hence, their difficulties and the extent of their trauma may go unnoticed by those around them, which may intensify their aftereffects.[12] Therefore, it is important to evaluate the symptoms that appear after children have been sexually abused to provide appropriate treatment and intervention.
The Korean-child behavior checklist (K-CBCL), a parent-rated scale, has been used to measure the adaptation and problem behaviors of children and adolescents aged 6 to 18 years and their psychopathology. In particular, the CBCL Problem Behavior Syndrome scale is highly correlated with the diagnostic and statistical manual of mental disorders system diagnosis for hospitalized and outpatient children and adolescents who exhibit related problem behaviors. Its utility as a complementary tool for diagnostic and statistical manual of mental disorders diagnosis has been proven in clinical settings.[13–16]Most previous studies conducted in Korea on sexually abused children used only some subscales of the CBCL (such as total scores for problem behavior, internalization, and externalization). Only few compared the CBCL scores of victims of sexual violence with those of control groups. Kim et al[17] compared the CBCL scale results of 27 sexually abused children and adolescents who visited a local Sunflower Center (Sexual Violence Victims Integrated Support Center) and 27 control participants and found that the victims of sexual abuse showed significantly higher T-scores in withdrawal, social problems, delinquency, externalizing problems, and total problem behavior scales than the control group. They also had a statistical trend toward higher scores on the anxiety/depression and attention problems scales than did the control group. Similarly, Son et al[18] also found significant differences in social immaturity, thought problems, delinquency, and total problem behavior scales between the sexual assault victims and control groups.
Major statistics related to sexual violence against children in Korea are limited to surveys on the status and types of victims. Owing to difficulties in recruiting participants and managing data confidentiality, most studies on sexual violence victims are retrospective studies of adults, which has limitations as they may have distorted their memories of the traumatic events or have difficulties in reporting their psychological state at the time of the crime.[19] We used the K-CBCL and examined the difference in psychological sequelae between the sexual violence victim and control groups. We wanted to help design a treatment program in the field of psychotherapy by finding symptoms that were expected to be further aggravated by damage from sexual violence.
2. Methods
2.1. Study design
In total, 97 children aged 7 to 12 (20 boys, 77 girls, mean age 10.27 ± 2.28 years) who visited the Sunflower Center of Southern Gyeonggi from December 2014 to November 2020 participated in this study.
All abuses were sexual assault, not rape. Children and their guardians visited the Sunflower Center immediately after a sexual assault incident occurred, and the center collected evidence, confirmed the need for post-psychotherapy, and provided psychological treatment services with consent. Since the K-CBCL questionnaires were completed in the first step before the psychotherapy services, they were collected within approximately 1 month after the occurrence of the incident. As Korean sentiment is reluctant in asking for a child’s psychiatric treatment history, psychological treatment at the Sunflower Center is conducted internally, without going through the hospital registration process. Therefore, there was no information regarding the medical history of the children. As Korea’s personal information protection law was strengthened, information such as socioeconomic level was not considered essential information for treatment. Hence, in most cases it was collected and excluded from the treatment service process. Survey data collected through these procedures were coded anonymously after consent to participate in the research was obtained. Data were stored and managed in a database. Afterwards, the victim received psychological treatment within the Sunflower Center and hospital treatment if necessary.
For the control group, the study used data from 178 children (32 boys aged 9, 12 boys aged 11, 84 girls aged 9, 50 girls aged 11, average age 9.7 ± 0.96 years) among data collected by the Korea Institute of Child Care and Education at the Panel Study on Korean Children (panel.kicce.re.kr).
Both groups of elementary school students aged 7 to 12 years were assessed via the K-CBCL 6-18 scale, and had no intellectual/mental disabilities. This study was conducted in accordance with the Declaration of Helsinki and its future amendments. The study was approved by the Institutional Review Board of Dankook University (DKU 2022-10-059-003). Written informed consent was obtained according to the required procedures, after the study details were explained to the participants and their parents. Participants voluntarily partook in the study and were informed that they could withdraw at any time.
2.2. Measure
2.2.1. K-CBCL 6–18 behavior rating scale (Korean- child behavior checklist: K-CBCL)
The Korean version of the Child Behavior Checklist, a widely used caregiver report measure, was used to measure the emotions and problem behaviors of children and adolescents aged 6 to 18 years. In this study, the primary caregivers of the children who visited the Sunflower Center assessed their children. The Child Behavior Checklist (CBCL 6-18) developed by Achenbach and Edelbrock[20] was standardized into a Korean version by Oh et al[21]
This study used the Problem Behavior Syndrome Scale. The scale consisted of the total problem behavior score, internalization, anxiety/depression, withdrawal/depression, somatic symptoms, externalization, rule-breaking behavior, aggressive behavior, social immaturity, thought problems, attention problems, and other problems. Each item was rated on a 3-point Likert scale: Not True (0 points), Somewhat or Sometimes True (1 point), and Very True or Often True (2 points). The standard scores for each subscale were calculated. Datasets analyzed during the current study are not publicly available due to an ethical issue; however, they are available from the corresponding author on reasonable request.
2.3. Analysis
All statistical analyses were performed using the IBM SPSS version 25.0. The t test was used to examine the mean differences between sexual assault victims and non-victims (P < .05). A cross-analysis was conducted to investigate the correlation between the clinical and nonclinical groups according to the K-CBCL subscale scores between the 2 groups. Logistic regression was performed to compare the influence of specific problem behavior types on sexually abused children.
3. Results
3.1. Differences in the K-CBCL subscales between the 2 groups
Table 1 shows the differences in the K-CBCL subscale scores between the 97 victims of sexual violence and 178 control participants. There were significant differences between the 2 groups for all the subscales. We used partial eta squared to measure the effect size of each subscale and the order was internalization, total problem behavior score, anxiety/depression, externalization, withdrawal/depression, attention problems, thought problems, social immaturity, somatic symptoms, aggressive behavior, rule-breaking behavior, and other problems.
Table 1.
Comparison of the mean score and effect size of problem behavior between the two groups.
| CBCL | Case group (N = 97) | Control group (N = 178) | t | P value | η2p |
|---|---|---|---|---|---|
| Total problem behavior | 65.64 ± 13.28 | 48.06 ± 10.37 | −11.3 | .000 | 0.47 |
| Internalization | 65.37 ± 13.18 | 48.07 ± 8.98 | −11.55 | .000 | 0.53 |
| Anxiety/depression | 63.19 ± 10.40 | 52.98 ± 5.42 | −9.03 | .000 | 0.41 |
| Withdrawal/depression | 62.40 ± 10.05 | 53.23 ± 5.42 | −8.35 | .000 | 0.39 |
| Somatic symptoms | 60.34 ± 8.40 | 52.63 ± 5.22 | −8.22 | .000 | 0.32 |
| Externalization | 62.87 ± 13.71 | 49.20 ± 10.07 | −8.63 | .000 | 0.40 |
| Rule-breaking behavior | 61.60 ± 8.94 | 54.01 ± 6.08 | −7.48 | .000 | 0.30 |
| Aggressive behavior | 60.86 ± 9.62 | 53.44 ± 6.13 | −6.87 | .000 | 0.31 |
| Social immaturity | 61.70 ± 9.60 | 53.50 ± 5.94 | −7.66 | .000 | 0.35 |
| Thought problems | 61.23 ± 8.42 | 54.23 ± 6.44 | −8.15 | .000 | 0.36 |
| Attention problem | 61.59 ± 10.82 | 52.85 ± 6.06 | −7.35 | .000 | 0.36 |
| Other problems | 61.07 ± 8.32 | 53.99 ± 6.00 | −7.39 | .000 | 0.27 |
3.2. Cross-analysis of problem behaviors by clinical standards in the victims and controls
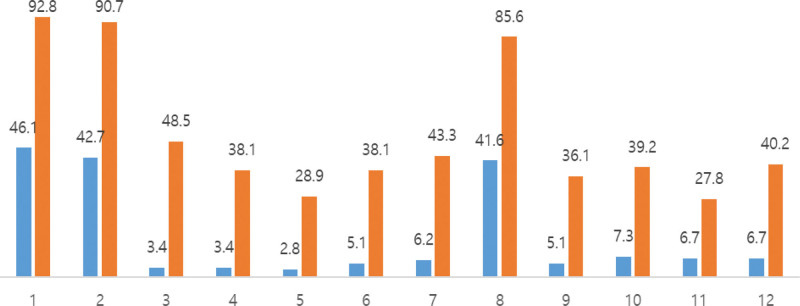
Cross-tabulation was conducted to verify the difference in the ratio between the risk and non-risk groups based on clinical values in victims and non-victims of sexual violence. Rates of the risk and non-risk groups based on clinical values showed a significant difference (P = .000) (Table 2). Figure 1 shows the proportions of victims and control participants based on their clinical values.
Table 2.
Chi-square analysis of CBCL problem behaviors in sexually abused children.
| CBCL Clinical classification | Control group (N = 178) | Case group (N = 97) | Total | x2 | P value | |
|---|---|---|---|---|---|---|
| Total problem behavior | Nonclinical | 96 (53.9) | 7 (7.2) | 103 (37.5) | 58.491 | .000 |
| Clinical | 82 (46.1) | 90 (92.8) | 172 (62.5) | |||
| Internalization | Nonclinical | 102 (57.3) | 9 (9.3) | 111 (40.4) | 60.158 | .000 |
| Clinical | 76 (42.7) | 88 (90.7) | 164 (59.6) | |||
| Anxiety/depression | Nonclinical | 172 (96.6) | 50 (51.5) | 222 (80.7) | 82.020 | .000 |
| Clinical | 6 (3.4) | 47 (48.5) | 53 (19.3) | |||
| Withdrawal/depression | Nonclinical | 172 (96.6) | 60 (61.9) | 232 (84.4) | 57.553 | .000 |
| Clinical | 6 (3.4) | 37 (38.1) | 43 (15.6) | |||
| Somatic symptoms | Nonclinical | 173 (97.2) | 69 (71.1) | 242 (88.0) | 40.369 | .000 |
| Clinical | 5 (2.8) | 28 (28.9) | 33 (12.0) | |||
| Social immaturity | Nonclinical | 169 (94.9) | 60 (61.9) | 229 (83.3) | 49.349 | .000 |
| Clinical | 9 (5.1) | 37 (38.1) | 46 (16.7) | |||
| Thought problems | Nonclinical | 167 (93.8) | 55 (56.7) | 222 (80.7) | 55.602 | .000 |
| Clinical | 11 (6.2) | 42 (43.3) | 53 (19.3) | |||
| Externalization | Nonclinical | 104 (58.4) | 14 (14.4) | 118 (42.9) | 49.605 | .000 |
| Clinical | 74 (41.6) | 83 (85.6) | 157 (57.1) | |||
| Attention problem | Nonclinical | 169 (94.9) | 62 (63.9) | 231 (84.0) | 44.970 | .000 |
| Clinical | 9 (5.1) | 35 (36.1) | 44 (16.0) | |||
| Rule-breaking behavior | Nonclinical | 165 (92.7) | 59 (60.8) | 224 (81.5) | 42.220 | .000 |
| Clinical | 13 (7.3) | 38 (39.2) | 51 (18.5) | |||
| Aggressive behavior | Nonclinical | 166 (93.3) | 70 (72.2) | 236 (85.8) | 22.953 | .000 |
| Clinical | 12 (6.7) | 27 (27.8) | 39 (14.2) | |||
| Other problems | Nonclinical | 166 (93.3) | 58 (59.8) | 224 (81.5) | 46.546 | .000 |
| Clinical | 12 (6.7) | 39 (40.2) | 51 (18.5) | |||
Figure 1.
Graph of incidence rates based on clinical values in the two groups.
3.3. Logistic regression analysis based on the 2 group’s clinical values
Logistic regression analysis was conducted to compare the effect size of the subdivided problem behavior types of sexually abused children. All the sub-factors of problem behavior were statistically significant. We examined the significance of the regression coefficients and found that sexually abused children showed high odds ratio (OR) values in the order of anxiety/depression (OR 26.95, 95% confidence interval [CI] 10.89–66.69), withdrawal/depression (OR 17.68, 95% CI 7.11–43.97), total problem behavior score (OR 15.05, 95% CI 6.61–34.30), somatic symptoms (OR 14.04, 95% CI 5.21–37.85), internalization (OR 13.13, 95% CI 6.22–27.71), thought problems (OR 11.59, 95% CI 5.59–24.07), social immaturity (OR 11.58, 95% CI 5.28–25.41), and attention problems (OR 10.60, 95% CI 4.82–23.32) compared to non-abused children (Table 3).
Table 3.
Logistic regression analysis of CBCL problem behaviors in sexually abused children.
| Scale | OR | P value | 95% CI (range) | |
|---|---|---|---|---|
| Total problem behavior | Nonclinical | 1 | ||
| Clinical | 15.05 | .000 | 6.61–34.30 | |
| Internalization | Nonclinical | 1 | ||
| Clinical | 13.13 | .000 | 6.22–27.71 | |
| Anxiety/depression | Nonclinical | 1 | ||
| Clinical | 26.95 | .000 | 10.89–66.69 | |
| Withdrawal/depression | Nonclinical | 1 | ||
| Clinical | 17.68 | .000 | 7.11–43.97 | |
| Somatic symptoms | Nonclinical | 1 | ||
| Clinical | 14.04 | .000 | 5.21–37.85 | |
| Social immaturity | Nonclinical | 1 | ||
| Clinical | 11.58 | .000 | 5.28–25.41 | |
| Thought problems | Nonclinical | 1 | ||
| Clinical | 11.59 | .000 | 5.59–24.07 | |
| Externalization | Nonclinical | 1 | ||
| Clinical | 8.33 | .000 | 4.39–15.80 | |
| Attention problem | Nonclinical | 1 | ||
| Clinical | 10.60 | .000 | 4.82–23.32 | |
| Rule-breaking behavior | Nonclinical | 1 | ||
| Clinical | 8.18 | .000 | 4.07–16.40 | |
| Aggressive behavior | Nonclinical | 1 | ||
| Clinical | 5.336 | .000 | 2.56–11.13 | |
| Other problems | Nonclinical | 1 | ||
| Clinical | 9.30 | .000 | 4.56–18.97 | |
CI = confidence interval, OR = odds ratio.
4. Discussion
This study assessed the mental health of sexually abused children using the K-CBCL scale and examined how it differed from that of non-abused children. To compare scores under the same conditions, except for the presence or absence of damage, both groups were composed of elementary school children without intellectual/mental disabilities. In both groups, the male-to-female ratio was equal to approximately 1:3, and the average age was also configured equally in the 9 to 10 year old category. Scores of the K-CBCL Problem Behavior Syndrome scale were compared between the victims and non-victims of sexual violence. Significant differences were observed in all the subscales. Therefore, sexually abused children had significantly higher scores for internalization, total problem behavior, anxiety/depression, externalization, withdrawal/depression (withdrawn), attention problems, thought problems, social immaturity, somatic symptoms, aggressive behavior, rule-breaking behavior (delinquency), and other problems than those in the control group. These findings were partially consistent with the results of previous studies,[17,18,22] which suggested that sexually abused children reported various psychopathologies, which included psychological distress, compared with non-abused children. Furthermore, the K-CBCL could effectively assess them.
According to Kim et al[23], of the 84 children aged < 13 years who visited a local Sunflower Center, 46.43% reported significant internalizing problems (which included depression, anxiety, and withdrawal), and 36.9% reported significant externalizing problems (which included delinquency, aggression, and hyperactivity). This suggested that sexually abused children could have higher total problem behavior scores than the control participants. Son et al[18] compared the symptoms of sexually abused and non-abused children using the trauma symptom checklist for children and found statistically significant group differences in all the clinical scales. Compared to the control group, sexually abused children reported higher rates of anxiety (fear of men, fear, worry about everything), depression (“I feel like no 1 likes me,” “I am not sad or happy”), anger (frequently get into fights, often yell, or smash things), post-traumatic stress and dissociation (“I try not to think about anything,” “try not to feel anything”), and sexual problems (“I touch my private parts too much,” “get scared or angry when I think of sex”), which indicated that they experienced related difficulties.
Kwon and Lee investigated the effects of sexual abuse on psychological maladjustment among 126 female adolescents who lived in juvenile detention homes.[24] The results showed statistically significant differences between the sexual abuse victims and control participants on the total Symptom Checklist-90-Revision score, somatization, hostility, depression, and anxiety. Sexually abused adolescents also had higher scores in all the areas than the control participants, except obsession, interpersonal sensitivity, and paranoia. In addition, 66% of the girls reported experience of sexual abuse. Sexually abused teenagers experienced severe depression, anxiety, and low self-esteem, and felt alienated. They could turn to drugs or alcohol use to cope with their psychological anxiety or lead to ease engagement in sexual activities (e.g., promiscuous sex, prostitution, etc.). Through these mechanisms, sexually abused teens were also more likely to engage in various delinquent or criminal behaviors, such as violence, theft, robbery, and drug abuse.[25–27]
The somatic symptoms scale consisted of items related to complaints of various physical symptoms, even though they were not medically confirmed. Previous studies reported that somatic symptoms, such as chronic pelvic pain, irritable bowel syndrome, non-epileptic seizures, and back pain, were associated with child sexual abuse.[28–31] Physical symptoms caused by psychological trauma could be explained by a shared vulnerability model in which physical symptoms occur because of increased anxiety sensitivity due to trauma. When experiences that involved somatic symptoms occurred, anxiety sensitivity, fear, anxiety, and avoidance reactions increased, which resulted in a gradual increase in and persistence of pain.[32,33]
In this study, sexually abused children had significantly higher scores for withdrawal/depression (“I like being alone,” refusing to talk, too shy or timid) and social immaturity (“I do not get along with other children,” “rely too much on adults”) than the control group. These results suggested that sexually abused children experienced difficulties in their peer relationships and social adjustment. According to Shin, children aged 12 to 15 years kept their distance from their friends as they believed their friends would judge them if they found out of their past, based on the experiences of 15 sexually abused children. They also believed that their friends avoided them and judged them.[1]
Our results showed that sexual violence had a negative impact on children’s emotional, behavioral, and social domains. Many previous studies in Korea covered the emotional and behavioral symptoms of victims of sexual violence; however, research that evaluated the social aspects was lacking.[34] Therefore, further research is required to identify the impact of sexual violence on an individual’s social and interpersonal domains. In addition, organizations that support sexually abused children and adolescents should provide interventions to help them maintain safe social relationships without being isolated in addition to physical and psychological trauma treatment. Currently, the method of supporting victims of sexual violence is somewhat individualized and focuses on physical and psychological treatment, such as obstetrics and gynecology care, psychiatric care, and psychotherapy. Interventions should help victims stay and remain within their social systems rather than being separated and protected from them. Furthermore, they should help create safe social support systems for child and adolescent victims with weak support systems.
Children experience difficulties in recognizing themselves as victims of sexual abuse and disclosing the trauma inflicted on them.[35] Sexual crimes usually have no witnesses as most cases occur behind closed doors. Parents experience difficulties recognizing child sexual abuse because perpetrators often use secret-keeping to manipulate children and adolescents. In addition, unlike victims of other traumatic incidents, victims of sexual violence tend to feel guilt, shame, and self-blame,[36] which makes it additionally difficult for them to report such crimes. Therefore, providing sexual violence education to children and adolescents so that they can understand various types of sexual violence and disclose such crimes without self-judgment is necessary.
5. Limitations
First, it was difficult to generalize the results as this study was only conducted on children who visited a center dedicated to sexual abuse in 1 region in Korea.
Second, the study did not fully consider the characteristics (event, personal, cognitive, etc.) found to affect the symptoms of sexually abused children. Not all survivors of sexual violence experienced the same psychological symptoms and difficulties, and 30% to 40% of children reported no symptoms or only mild mental health problems.[37,38] Many researchers thought that cognitive factors (e.g., victim attribution and perception) were a primary mechanism of post-traumatic stress symptoms represented by the psychological sequelae of sexually abused children and teens.[39–41] Researchers reported empirical evidence that when individuals were overwhelmed by negative experiences, they underwent changes in their attributions to the event and their perceptions of themselves and the world. These changes directly affected their psychological adaptation.[42–44] In particular, as logical and rational thinking did not fully develop during childhood and adolescence, traumatic experiences were more likely to distort perceptions or attributional styles of oneself and others.[45] Cognitive factors such as attributional styles and coping methods for sexual violence were changeable, and it was anticipated that interventions that targeted them would be highly effective in reducing the aftereffects of sexual violence and assisting victims in their recovery.[46]
Third, this study used a parent report scale to assess the symptoms of sexually abused children. However, assessing both the child and caregiver would have provided further clinical information regarding the child’s symptoms and prevented respondents from either under- or overreporting the child’s distress. Among the scales designed to assess symptoms following a traumatic event, the trauma symptom checklist for children and Trauma Symptom Checklist for Young Children are particularly useful in measuring the psychopathology of sexually abused children because they have items that can measure sexual problems, a characteristic aftereffect of sexual violence, and psychological pain caused by the trauma.[18,47]
Fourth, this study did not examine the differences in symptoms over time. Crossley[48] suggested that interventions for victims of sexual violence should be differentiated over time. Crisis interventions, such as medical and psychological treatment, should be conducted from the victim’s perspective until 6 months after sexual abuse. Interventions to improve resource utilization skills and coping abilities should be provided from a survivor’s perspective for up to 2 years after the incident. True healing occurs when victims can set new directions and goals in life without dwelling on their past from an experiencer’s point of view. Therefore, follow-up studies are required to reflect these perspectives.
Despite these limitations, this study was significant in that it investigated the psychological aftereffects experienced by sexually abused children and compared the scores of the K-CBCL Problem Behavior Syndrome scale between the victims of sexual violence and the control participants. We found that sexual violence harms children’s overall mental health, which includes emotional, behavioral, and social factors. These findings suggest that multidisciplinary assessment and treatment are vital for children with sexual abuse.
Yoo study predicted that family environmental variables, such as parental support and family function, would affect the recovery of victimized children.[49] In particular, in Spaccarelli and Kim study, parents supportive responses after exposure to sexual abuse incidents had the greatest impact on the adaptation of victimized children. Furthermore, children who perceived that they had been supported by their parents were social, academic, and interpersonal, and showed a high degree of adaptation.[50] Therefore, implementing parenting skills improvement programs for parents and communication skills programs with children could be another effective measure along with direct support for victimized children.
Author contributions
Conceptualization: Sam Sik Choi, Myung Ho Lim, Hyoung Yoon Chang.
Data curation: Sam Sik Choi, Saet Byeol Yang, Ja Young Lim, Hyoung Yoon Chang.
Formal analysis: Saet Byeol Yang, Ja Young Lim, Kyoung Min Kim, Youngil Lee, Min Sun Kim, Myung Ho Lim, Hyoung Yoon Chang.
Investigation: Sam Sik Choi, Saet Byeol Yang, Ja Young Lim, Hyoung Yoon Chang.
Methodology: Sam Sik Choi, Saet Byeol Yang, Kyoung Min Kim, Youngil Lee, Se-Hoon Shim, Min Sun Kim, Myung Ho Lim.
Supervision: Kyoung Min Kim, Youngil Lee, Se-Hoon Shim, Min Sun Kim, Myung Ho Lim, Hyoung Yoon Chang.
Validation: Sam Sik Choi, Saet Byeol Yang, Ja Young Lim, Kyoung Min Kim, Youngil Lee, Se-Hoon Shim, Min Sun Kim, Myung Ho Lim, Hyoung Yoon Chang.
Visualization: Se-Hoon Shim, Myung Ho Lim.
Writing – original draft: Sam Sik Choi.
Writing – review & editing: Myung Ho Lim, Hyoung Yoon Chang.
Abbreviations:
- CI
- confidence interval
- K-CBCL
- Korean-child behavior checklist
- OR
- odds ratio
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Choi SS, Yang SB, Lim MH, Lim JY, Kim KM, Lee Y, Shim S-H, Kim MS, Chang HY. Psychological aftereffects experienced by sexually abused children: Psychopathological characteristics revealed by the K-CBCL. Medicine 2023;102:38(e34699).
Contributor Information
Sam Sik Choi, Email: css37733@daum.net.
Saet Byeol Yang, Email: mindstar@dankook.ac.kr.
Myung Ho Lim, Email: paperose@dankook.ac.kr.
Ja Young Lim, Email: paperose@dankook.ac.kr.
Kyoung Min Kim, Email: 12191720@dankook.ac.kr.
Youngil Lee, Email: anat104@dku.edu.
Se-Hoon Shim, Email: shshim2k@hanmail.net.
References
- [1].Shin KS. Sexually abused children’s victimized experience. Kor J Psychol. 2011;30:1255–87. [Google Scholar]
- [2].Park Y, Lee J. Mobile application contents development for the information accessibility and mental health promotion to recover from sexual violence. J Digital Contents Soc. 2022;23:191–202. [Google Scholar]
- [3].Madriz E. Nothing Bad Happens to Good Girls: Fear of Crime in Women’s Lives. Berkeley: University of California Press; 1997. [Google Scholar]
- [4].Stanko EA. Everyday Violence: How Women and Men Experience Sexual and Physical Danger. Pandora; 1990. [Google Scholar]
- [5].Mullen PE, Martin JL, Anderson JC, et al. The effect of child sexual abuse on social, interpersonal and sexual function in adult life. Br J Psychiatry. 1994;165:35–47. [DOI] [PubMed] [Google Scholar]
- [6].Luster T, Small SA. Sexual abuse history and problems in adolescence: Exploring the effects of moderating variables. J Marriage Family. 1997;59:131–42. [Google Scholar]
- [7].Tyler K. Social and emotional consequences of childhood sexual abuse: a review of recent research. Aggr Violent Beha. 2002;7:567–89. [Google Scholar]
- [8].Buckle SK, Lancaster S, Powell MB, et al. The relationship between child sexual abuse and academic achievement in a sample of adolescent psychiatric inpatients. Child Abuse Negl. 2005;29:1031–47. [DOI] [PubMed] [Google Scholar]
- [9].Supreme Prosecuters’ Office. Crime analysis. Seoul, supreme prosecuters. Office. 2022:2022. [Google Scholar]
- [10].Kim SN. The problem of military sexual violence by hierarchy: focusing on the contents of media articles. J Converg Culture Technol. 2022;8:85–92. [Google Scholar]
- [11].Song SH, Kim SY, Chung YK, et al. A study of sexual assaults on children and adolescents: based on data from a one-stop service center. J Kor Acad Child Adolesce Psychiatr. 2008;19:162–7. [Google Scholar]
- [12].Perrin S, Smith P, Yule W. Practitioner review: the assessment and treatment of post-traumatic stress disorder in children and adolescents. J Child Psychol Psychiatry. 2000;41:277–89. [PubMed] [Google Scholar]
- [13].Lee SA, Kim KH, Yook KH. Utility of K-CBCL and MMPI-A in evaluation and diagnosis of adolescents with internalizing or externalizing disorders. Kor J Clin Psychol. 2012;31:391–9. [Google Scholar]
- [14].Kim MS, Ha EH, Oh KJ. A cluster analysis of K-CBCL for outpatient children. Kor J Clin Psychol. 2014;33:675–96. [Google Scholar]
- [15].Achenbach TM, Rescorla L. Manual for the Aseba School-Age Forms & Profiles: an Integrated System of Multi-Informant Assessment. University of Vermont; 2001. [Google Scholar]
- [16].Morgan CJ, Cauce AM. Predicting DSM-III-R disorders from the youth self-report: analysis of data from a field study. J Am Acad Child Adolesc Psychiatry. 1999;38:1237–45. [DOI] [PubMed] [Google Scholar]
- [17].Kim HY, Hwang JW, Choi SM, et al. Impact of trauma due to sexual violence on psychopathology and quality of life in children and adolescents. J Kor Acad Child Adolesc Psychiatr. 2014;25:217–23. [Google Scholar]
- [18].Son SY, Kim TK, Shin YJ. The effectiveness of traumatic symptom checklist for children (TSCC): comparisons of sexually abused children and nonabused normal children. J Kor Acad Child Adolesc Psychiatr. 2007;18:49–57. [Google Scholar]
- [19].Kim KY, Lee NH, Cheon KA, et al. A cohort study of children and adolescents victims with sexual abuse in Korea and their initial assessment results. Kor J Psychos Med. 2019;27:13–24. [Google Scholar]
- [20].Achenbach TM, Edelbrock CS. Manual for the Child: Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont; 1983. [Google Scholar]
- [21].Oh KJ, Lee HR, Hong KE, et al. K-CBCL Child and Adolescent Behavior Assessment Scale. Seoul: Central aptitude publishing house; 1997. [Google Scholar]
- [22].Mannarino AP, Cohen JA, Smith JA, et al. Six-and twelve-month follow-up of sexually abused girls. J Interpers Violence. 1991;6:494–511. [Google Scholar]
- [23].Kim TK, Kim SH, Choi KS, et al. Psychopathology of sexually abused children in Korea. J Kor Neuropsychiatr Assoc. 2006;45:165–73. [Google Scholar]
- [24].Kweon HS, Lee JC. The influence of sexually abused adolescents’ attribution style and coping strategies on psychological maladjustment. KJYC. 2003;11:22–31. [Google Scholar]
- [25].Beitchman JH, Zucker KJ, Hood JE, et al. A review of the short-term effects of child sexual abuse. Child Abuse Negl. 1991;15:537–56. [DOI] [PubMed] [Google Scholar]
- [26].Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: a review and synthesis of recent empirical studies. Psychol Bull. 1993;113:164–80. [DOI] [PubMed] [Google Scholar]
- [27].Stern AE, Lynch DL, Oates RK, et al. Self esteem, depression, behaviour and family functioning in sexually abused children. J Child Psychol Psychiatry. 1995;36:1077–89. [DOI] [PubMed] [Google Scholar]
- [28].Friedrich WN, Schafer LC. Somatic symptoms in sexually abused children. J Pediatr Psychol. 1995;20:661–70. [DOI] [PubMed] [Google Scholar]
- [29].Lampe A, Sölder E, Ennemoser A, et al. Chronic pelvic pain and previous sexual abuse. Obstet Gynecol. 2000;96:929–33. [DOI] [PubMed] [Google Scholar]
- [30].Reilly J, Baker GA, Rhodes J, et al. The association of sexual and physical abuse with somatization: characteristics of patients presenting with irritable bowel syndrome and non-epileptic attack disorder. Psychol Med. 1999;29:399–406. [DOI] [PubMed] [Google Scholar]
- [31].Linton SJ. A population-based study of the relationship between sexual abuse and back pain: establishing a link. Pain. 1997;73:47–53. [DOI] [PubMed] [Google Scholar]
- [32].Asmundson GJ, Coons MJ, Taylor S, et al. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47:930–7. [DOI] [PubMed] [Google Scholar]
- [33].Muris P, Vlaeyen JW, Meesters C, et al. Anxiety sensitivity and fear of pain in children. Percept Mot Skills. 2001;92:456–8. [DOI] [PubMed] [Google Scholar]
- [34].Lee AR, Kim JS. The research trends of sexual assault victim studies and meta analysis on the effects of group counseling programs. Kor J Health Psychol. 2022;27:533–61. [Google Scholar]
- [35].Johnson CF. Child sexual abuse. Lancet. 2004;364:462–70. [DOI] [PubMed] [Google Scholar]
- [36].Kim JY, Choi JH. Impact of the experience of sexual abuse on depression in female adolescents and mediation effect of distorted sex-related belief. Kor J Child Stud. 2009;30:231–47. [Google Scholar]
- [37].Finkelhor D, Berliner L. Research on the treatment of sexually abused children: a review and recommendations. J Am Acad Child Adolesc Psychiatry. 1995;34:1408–23. [DOI] [PubMed] [Google Scholar]
- [38].Putnam FW. Ten-year research update review: child sexual abuse. J Am Acad Child Adolesc Psychiatry. 2003;42:269–78. [DOI] [PubMed] [Google Scholar]
- [39].Feiring C, Taska L, Chen K. Trying to understand why horrible things happen: attribution, shame, and symptom development following sexual abuse. Child Maltreat. 2002;7:26–41. [DOI] [PubMed] [Google Scholar]
- [40].Quas JA, Goodman GS, Jones D. Predictors of attributions of self-blame and internalizing behavior problems in sexually abused children. J Child Psychol Psychiatry. 2003;44:723–36. [DOI] [PubMed] [Google Scholar]
- [41].Daigneault I, Tourigny M, Hébert M. Self-attributions of blame in sexually abused adolescents: a mediational model. J Trauma Stress. 2006;19:153–7. [DOI] [PubMed] [Google Scholar]
- [42].Foa EB, Steketee G, Rothbaum BO. Behavioral/cognitive conceptualizations of post-traumatic stress disorder. Behav Ther. 1989;20:155–76. [Google Scholar]
- [43].Lee Y, Han A, Kim J. Effects of childhood emotional trauma on juvenile delinquency: mediating roles of early maladaptive schemas. Kor J Human Ecol. 2022;31:15–22. [Google Scholar]
- [44].Sin S. Analysis on the decisions of the constitutional courts on special provisions on the evidence admissibility of video recorded statement of minor victims in sexual assault cases. Asian Women law. 2022;25:1–16. [Google Scholar]
- [45].Browne C, Winkelman C. The effect of childhood trauma on later psychological adjustment. J Interpers Violence. 2007;22:684–97. [DOI] [PubMed] [Google Scholar]
- [46].Shim HS, Chun JS, Kim JH. The mediating effects of coping strategies on the relationship between attributional styles and post-traumatic stress disorder among sexual assault victims. Kor Inst Health Soc Affairs. 2015;35:287–314. [Google Scholar]
- [47].Lanktree CB, Gilbert AM, Briere J, et al. Multi-informant assessment of maltreated children: convergent and discriminant validity of the TSCC and TSCYC. Child Abuse Negl. 2008;32:621–5. [DOI] [PubMed] [Google Scholar]
- [48].Crossley ML. Narrative psychology, trauma and the study of self/identity. Theory Psychol. 2000;10:527–46. [Google Scholar]
- [49].You S-J. Study on the Effects of Childhood Sexual Abuse on Mental Health among University Female Students: Focusing on the Abuse-Related Characteristics, Coping Strategies and Parental Support [master’s thesis]. Seoul: Ewha Womans University Graduate; 2003. 88. [Google Scholar]
- [50].Spaccarelli S, Kim S. Resilience criteria and factors associated with resilience in sexually abused girls. Child Abuse Negl. 1995;19:1171–82. [DOI] [PubMed] [Google Scholar]