Abstract
Background:
Breast implant illness (BII) is a poorly understood heterogeneous disorder treated with implant removal; however, patient-reported symptoms and outcomes after treatment remain unclear.
Methods:
A retrospective review of patients undergoing bilateral breast implant removal related to BII by two surgeons at an academic medical center between 2018 and 2022 was conducted. Patients were surveyed using the BREAST-Q Reconstruction model with the American Society for Aesthetic Plastic Surgery BII survey extension. Outcomes were analyzed using multivariable logistic regression, adjusted for patient-associated factors.
Results:
Forty-seven patients were surveyed with a response rate of 51% (n = 24). Of the 20 patients who completed the survey, the majority were White (85%), with 45% (n = 9) having a documented history of psychiatric illness. Six (30%) patients had capsular contracture and four (20%) had documented implant rupture. Most implant removal procedures (n = 12, 60%) were not covered by insurance. Fourteen (70%) patients reported a net improvement in their symptoms after implant removal, most commonly chest discomfort, muscle pain, fever, and headaches. Capsular contracture was predictive of reduced psychosocial, sexual, and breast satisfaction scores (P = 0.015). Self-pay was predictive of increased breast satisfaction scores (P = 0.009), but had no impact on symptomatic improvement. A reduced time to implant removal was predictive of fewer residual symptoms (P = 0.032). Psychiatric illness had no significant impact on the outcomes.
Conclusions:
In the setting of suspected or diagnosed BII, a reduced time to implant removal may decrease the risk of residual symptoms and improve overall patient satisfaction. In patients with capsular contracture, preoperative counseling should emphasize that implant removal may only improve physical symptoms.
Takeaways
Question: In BII patients, what factors are associated with implant removal satisfaction and what is the impact on patient-reported quality of life?
Findings: Psychiatric illness had no significant impact on outcomes. Self-pay was predictive of increased breast satisfaction. Capsular contracture was predictive of reduced psychosocial, sexual, and breast satisfaction scores. Reduced time to implant removal was predictive of fewer residual symptoms.
Meaning: A reduced time to implant removal may decrease the risk of residual symptoms and improve overall patient satisfaction. However, patients with capsular contracture should be counseled that removal will likely improve physical discomfort only.
INTRODUCTION
Breast implant illness (BII) is a poorly understood, heterogeneous disorder that refers to patient-reported malaise as well as a constellation of systemic symptoms that researchers, physicians, and patients have attributed to the placement of silicone breast implants. The term itself has been popularized by media platforms owing to the increasing number of patients with breast implants who report systemic symptoms that are otherwise unexplainable.1 Although some hypothesize that these symptoms are caused by an immune response toward silicone or other chemical components of the implants, the pathophysiology of BII remains unknown, and no diagnostic tests currently exist.2–12
The notion that breast implants contribute to systemic illnesses remains controversial because there is an overwhelming amount of evidence supporting their safety. Few medical devices have undergone the degree of scrutiny and evaluation that silicone breast implants have throughout the course of their use in clinical practice.13 Despite this, numerous studies have reported improvement or total symptom resolution in patients with BII following implant removal,14–17 although the overall evidence remains equivocal.18,19 The most common critique of these studies is that they lack a validated, patient-reported outcome measuring tool to assess symptoms and outcomes following treatment.20 Therefore, the usefulness of explantation remains unclear.
Although more than 100 symptoms have been associated with BII, the plastic surgery division at Brigham and Women’s Hospital recently utilized an international panel and Delphi survey to reach a consensus on the top 19 BII symptoms reported by patients.20,21 Additionally, the American Society for Aesthetic Plastic Surgery (ASAPS) created a postexplantation questionnaire that efficiently collects patient-related factors, including patient-reported, subjective assessment of mammary, extra-mammary, and other systemic symptoms. The purpose of this study was to utilize the most comprehensive and validated BII survey to better understand and characterize patient experience, outcomes, and symptoms after seeking implant removal. We accomplished this by offering the BREAST-Q Reconstruction survey and providing the ASAPS BII questionnaire as a survey extension that included the top 19 BII symptoms to date. We hope that our findings can help better address patient concerns, provide more evidence-based care, and inform not only prospective patients, but also prospective surgeons about the potential risks of treatment in this patient population.
METHODS
Study Design and Covariates
This study was approved by the hospital institutional review board of the University of Pennsylvania (IRB# 851143). The surgical case logs of the senior authors (S. J.K and P. D. B.) were retrospectively reviewed from 2018 to 2022 for women aged 18 years or older with a history of breast augmentation who underwent bilateral breast implant removal for a diagnosis of or high suspicion of BII. Patients were excluded if they did not have at least 90 days of follow-up or had reinsertion of their breast implants.
Patient data were collected from electronic medical records. These data included patient demographics, clinical comorbidities, and surgical histories. The presence of documented psychiatric illness was recorded from medical history and included major depressive disorder, generalized anxiety disorder, bipolar disorder, schizophrenia, and attention-deficit/hyperactivity disorder. The payment status for the index breast implant removal was determined from the encounter billing information and was characterized as self-pay or covered by insurance. The time to implant removal was defined as the time elapsed between the most proximal breast augmentation and the index explant. The presence of capsular contracture and implant rupture were noted along with perioperative complications, including seroma and hematoma, within 90 days.
Surgical Technique
All patients underwent an incision via the inframammary fold (IMF) to access the implant before undergoing standardized total capsulectomies that included the posterior wall. All breast pockets were irrigated with both antibiotic saline and betadine before the placement of closed suction drains and skin closure. None of the patients received fat grafting, mastopexy, or any other cosmetic or corrective procedures following explantation.
Electronic Survey
Patients who met the inclusion criteria were contacted via email with a customized electronic Qualtrics (Qualtrics LLC, Provo, Utah) survey, which comprised the validated BREAST-Q Reconstruction model instrument in addition to the ASAPS BII postexplantation survey as an extension. The questionnaire was also designed to include the top 19 symptoms reported in the recently published Delphi survey from Brigham and Women’s Hospital.20,21 Upon completing the BREAST-Q portion of the survey, the patients were asked to indicate the symptoms that they experienced both before and following the index explantation. Patients who did not initially respond to the electronic survey or did not complete the survey in its entirety were contacted via telephone to request survey completion no more than twice. Only the completed surveys were included in the analysis.
Statistical Analysis
Categorical variables were summarized as frequencies and percentages, and continuous variables were summarized as means with SDs. BII resolved symptoms were defined as those no longer reported following explantation, as noted by patient surveys, and residual symptoms were defined as those present in both the pre- and postexplantation portions of the survey. Net symptomatic improvement was defined as the number of improved symptoms minus the number of residual symptoms. Outcomes, including BREAST-Q modular scores as well as improved and residual symptom totals, were analyzed using multivariable linear regressions adjusted for patient-associated factors. The final regression models were adjusted for the following covariates: age, body mass index (BMI), history of psychiatric illness, prior number of breast procedures, documented capsular contracture, time to implant removal, implant rupture, and insurance status of explants. Statistical significance was set at an alpha level of 0.05. significance.
RESULTS
Forty-seven patients were surveyed with a response rate of 51% (n = 24). Of the 20 patients who completed the entire survey, the mean age was 44.9 ± 9.8 years, the majority were White (n = 17, 85%), and 45% (n = 9) had a documented history of psychiatric illness (Table 1). The most frequently reported psychiatric diagnoses were generalized anxiety disorder (n = 8) and major depressive disorder (n = 7). Eleven patients (55%) reported allergies at baseline. None of the patients had autoimmune disease, but two were actively immunosuppressed with corticosteroids for osteoarthritis. The majority of implant removal procedures (n = 12, 60%) were not covered by insurance and thus labeled as “self-pay.”
Table 1.
Demographic and Clinical Characteristics of the Patients
| Characteristic | Value (N = 20) | Percent |
|---|---|---|
| Demographic | ||
| Age (y), mean ± SD | 44.9 ± 9.8 | — |
| Female sex | 20 | 100 |
| Race | ||
| African American/Black | 1 | 5 |
| White | 17 | 85 |
| Asian | 2 | 10 |
| Non-Hispanic/Latino | 20 | 100 |
| Body-mass index (kg/m2), mean ± SD | 26.16 ± 4.84 | — |
| Clinical | ||
| Documented history of: | ||
| Type II diabetes mellitus | 0 | 0 |
| Tobacco use | 8 | 40 |
| COPD | 1 | 5 |
| Hypertension | 4 | 20 |
| Chronic kidney disease | 1 | 5 |
| Documented psychiatric illness | ||
| Any psychiatric illness | 9 | 45 |
| Major depressive disorder | 7 | 35 |
| Generalized anxiety disorder | 8 | 40 |
| Bipolar disorder | 0 | 0 |
| Schizophrenia | 0 | 0 |
| ADHD | 2 | 10 |
| History of wound infection | 0 | 0 |
| Active immunosuppression | 2 | 10 |
| History of chemotherapy | 0 | 0 |
| History of chest wall radiation | 2 | 10 |
| Implant removal insurance status | ||
| Covered by insurance | 8 | 40 |
| Self-pay | 12 | 60 |
COPD, chronic obstructive pulmonary disease; ADHD, attention-deficit/hyperactivity disorder
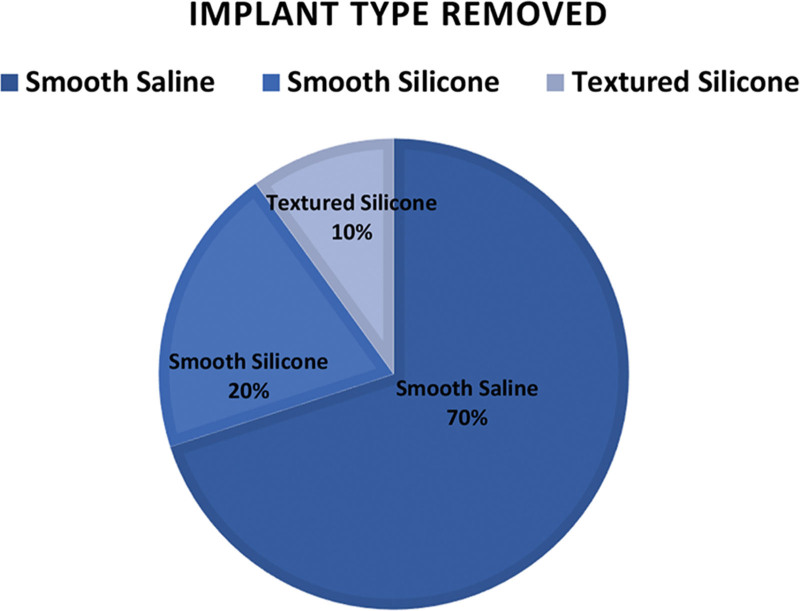
Breast prostheses were found in the submuscular plane in 15 patients (75%), whereas five patients had placement in the subglandular space (25%). Fourteen patients (70%) had smooth saline implants removed, four (20%) had smooth silicone implants, and two (10%) had textured silicone gel implants (Table 2, Fig. 1). There was no association between type of implant removed and symptomatic relief. Six (30%) patients had capsular contracture, and four (20%) had documented implant rupture at the time of explantation. Three of the four patients with implant rupture had silicone gel implants, with just one having bilateral saline implant rupture. The mean time to implant removal following the most recent breast augmentation was 13.2 ± 6.6 years. The mean time to survey completion after implant removal was 1.48 ± 0.74 years. Two patients (10%) experienced perioperative complications following explantation, and two patients (10%) required surgical revision.
Table 2.
Surgical Characteristics of the Patients
| Characteristic | Value (N = 20) | Percent |
|---|---|---|
| No. prior breast procedures, mean ± SD | 1.4 ± 0.6 | — |
| Last breast augmentation type | ||
| Submuscular | 15 | 75 |
| Subglandular | 5 | 25 |
| Time to implant removal from most recent augmentation (y), mean ± SD | 13.2 ± 6.6 | — |
| Implant type | ||
| Silicone | 6 | 30 |
| Saline | 14 | 70 |
| Textured | 2 | 10 |
| Smooth | 18 | 90 |
| Capsular contracture present | 6 | 30 |
| Implant rupture | 4 | 20 |
| Postoperative complications | ||
| Seroma | 1 | 5 |
| Surgical site infection | 1 | 5 |
| Revision after explant | 2 | 10 |
Fig. 1.
A summary of implant types removed. In a cohort of 20 patients, 20 pairs of implants (40 individual prostheses) were removed with the majority being smooth saline (70%, n = 14 pairs), four pairs being smooth silicone gel (20%), and only two pairs of implants being textured silicone gel (10%).
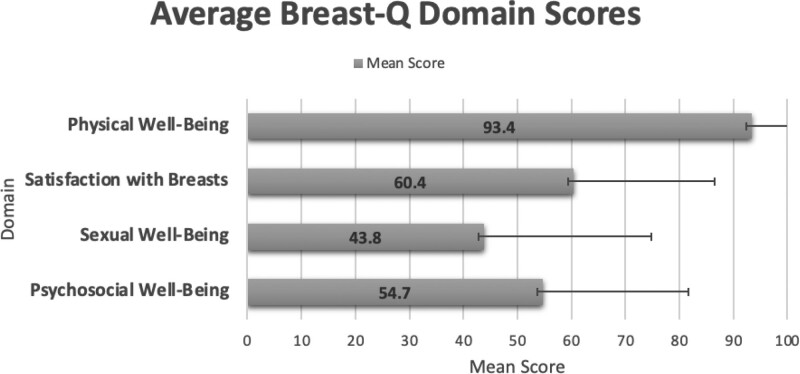
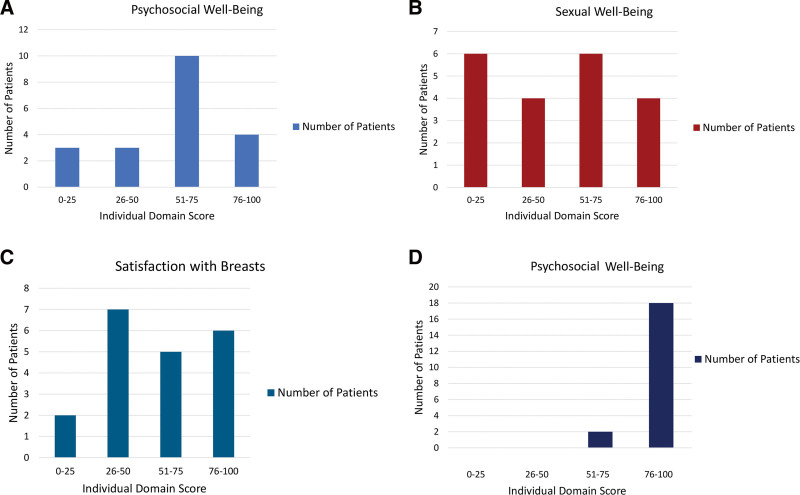
Based on the survey results, the most common symptom reported among patients before explantation was fatigue (n = 17, 85%), followed by chest discomfort (n = 14, 70%) and joint pain (n = 14, 70%). Fourteen patients (70%) experienced a net improvement in their symptoms after implant removal, most commonly improving chest discomfort, muscle pain, fever, and headaches (Table 3, Fig. 2). Patients were least likely to experience improvements in weight problems, joint pain, and insomnia. Patients were moderately satisfied regarding their satisfaction with their breasts and psychosocial scores, whereas the lowest satisfaction scores pertained to their sexual well-being (Table 4, Figs. 3 and 4). Scores were consistently high among the physical well-being domain, revealing that patients were most satisfied with the relief they felt from decreased muscle pain, tightness, and overall discomfort experienced during physical activity.
Table 3.
Symptomatic Presentation of Breast Implant-associated Illness and Subsequent Improvement after Removal
| Symptom | No. Patients with Symptom | Improvement after Removal, n (%) |
|---|---|---|
| Fatigue | 17 | 11 (64.7) |
| Chest discomfort | 14 | 13 (92.8) |
| Joint pain | 14 | 8 (57.1) |
| Anxiety/depression/panic attacks | 13 | 8 (61.5) |
| Poor sleep/insomnia | 12 | 7 (58.3) |
| Acid reflux | 11 | 7 (63.6) |
| Cognitive dysfunction | 11 | 7 (63.6) |
| Hair loss | 11 | 7 (63.6) |
| Muscle pain/weakness | 11 | 9 (81.8) |
| Fever/night sweats | 9 | 7 (77.8) |
| Headaches | 9 | 7 (77.8) |
| Pain around implant/underarm | 9 | 6 (66.7) |
| Weight problems | 9 | 2 (22.2) |
Fig. 2.
A summary of symptom improvement after breast implant removal. The graph displays the total number of patients reporting each symptom before intervention (light blue), and the number of patients who reported improvement in those symptoms post intervention (dark blue). Chest discomfort, muscle pain/weakness, headache, and fever were the least prevalent and most improved following implant removal.
Table 4.
BREAST-Q Results
| Characteristic | Value (N = 20) |
|---|---|
| Psychosocial well-being score, mean ± SD | 54.6 ± 26.9 |
| Sexual well-being score, mean ± SD | 43.8 ± 31.0 |
| Satisfaction with breasts score, mean ± SD | 60.4 ± 26.2 |
| Physical well-being score, mean ± SD | 93.4 ± 12.7 |
| Net improvement in symptoms? | 14 |
| No residual symptoms | 5 |
Fig. 3.
Average BREAST-Q domain scores. The scores for each domain of the reconstruction BREAST-Q survey are displayed as mean values, along with SD, to represent the entire cohort.
Fig. 4.
Scoring breakdown of individual BREAST-Q components. The domain scores for psychosocial well-being (A), sexual well-being (B), satisfaction with breasts (C), and physical well-being (D) are broken down into four quartiles to represent lowest satisfaction, moderately low satisfaction, moderate satisfaction, and highest satisfaction, to accurately depict how many patients scored similarly for each component.
The results of multivariable linear regression modeling of the BREAST-Q modular scores and residual/persistent symptom totals are summarized in Table 5 and Table 6. Capsular contracture was predictive of reduced psychosocial, sexual, and breast satisfaction scores (P = 0.02, P = 0.02, and P = 0.01, respectively). Self-pay was predictive of increased breast satisfaction scores (β = 32.0, P = 0.01), but had no impact on symptomatic improvement or other BREAST-Q scores. Implant rupture was also predictive of increased breast satisfaction scores after removal (β = 33.0, P = 0.02). The average time to implant removal in these patients was 13.2 years, with a reduced time to implant removal being predictive of fewer residual symptoms (β = −0.8, P = 0.03). Psychiatric illness had no significant impact on the outcomes. Only two patients (10%) reported that they had never undergone implant removal surgery.
Table 5.
Multivariable Linear Regressions for BREAST-Q Scores after Implant Removal
| Psychosocial Well-being Score | Sexual Well-being Score | Satisfaction with Breasts Score | Physical Well-being Score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariate | β | P | 95% CI | β | P | 95% CI | β | P | 95% Confidence Interval | β | P | 95% Confidence Interval |
| Age | −1.3 | 0.32 | −3.9 to 1.4 | −1.1 | 0.38 | −3.8 to 1.6 | −1.0 | 0.20 | −2.6 to 0.61 | −0.7 | 0.31 | −2.0 to 0.7 |
| BMI | 1.4 | 0.38 | −2.0 to 4.8 | 1.2 | 0.44 | −2.2 to 4.6 | 2.0 | 0.06 | −0.1 to 4.0 | −0.3 | 0.74 | −2.0 to 1.4 |
| Any psychiatric diagnosis | −9.5 | 0.46 | −36.9 to 24.3 | −9.2 | 0.48 | −36.7 to 18.3 | −12.8 | 0.11 | −29.1 to 3.6 | 8.5 | 0.20 | −5.2 to 22.2 |
| Prior number of breast procedures | −5.9 | 0.68 | −36.1 to 24.3 | −18.0 | 0.22 | −48.3 to 12.3 | −17.2 | 0.06 | −35.1 to 0.8 | −4.1 | 0.56 | −19.1 to 11.0 |
| Capsular contracture | −38.5 | 0.02 | −67.4 –−9.6 | −52.4 | 0.01 | −87.7 –−17.1 | −38.6 | 0.01 | −66.9 –−10.4 | 2.4 | 0.81 | −19.3 –24.0 |
| Time to implant removal | 1.3 | 0.48 | −2.5 to 5.1 | −0.5 | 0.79 | −4.3 to 3.3 | −0.4 | 0.72 | −2.6 to 1.9 | 0.5 | 0.60 | −1.4 to 2.4 |
| Implant rupture | 26.7 | 0.21 | −17.4 to 70.8 | 39.9 | 0.07 | −4.4 to 84.1 | 33.0 | 0.02 | 6.7 to 59.3 | 7.6 | 0.46 | −14.4 to 29.6 |
| Removal covered by insurance | 15.2 | 0.39 | −21.9 to 52.3 | 29.6 | 0.11 | −7.6 to 66.8 | 32.0 | 0.01 | 9.9 to 54.1 | 1.2 | 0.89 | −17.3 to 19.7 |
Values in boldface indicate statistical significance. BMI, body-mass index; CI, confidence interval.
Table 6.
Multivariable Linear Regressions for Residual and Improved BII Symptoms after Implant Removal
| Total No. Residual Symptoms | Total No. Improved Symptoms | |||||
|---|---|---|---|---|---|---|
| Covariate | β | p | 95% CI | β | p | 95% CI |
| Age | −0.5 | 0.08 | −1.1 to 0.1 | 0.7 | 0.01 | 0.2 to 1.2 |
| BMI | −0.2 | 0.65 | −0.9 to 0.6 | −0.2 | 0.41 | −0.8 to 0.4 |
| Any psychiatric diagnosis | 1.2 | 0.68 | −4.5 to 7.2 | −1.2 | 0.59 | −6.2 to 3.7 |
| Prior number of breast procedures | −0.1 | 0.98 | −6.8 to 6.6 | −2.8 | 0.28 | −8.2 to 2.6 |
| Capsular contracture | −2.1 | 0.62 | −11.4 to 7.2 | −3.4 | 0.35 | −11.0 to 4.2 |
| Time to implant removal | 0.6 | 0.15 | −0.2 to 1.5 | −0.8 | 0.03 | −1.4 to −0.1 |
| Implant rupture | 0.2 | 0.96 | −9.5 to 9.9 | −1.9 | 0.62 | −9.8 to 6.1 |
| Removal covered by insurance | −1.5 | 0.68 | −9.7 to 6.6 | −2.1 | 0.51 | −8.7 to 4.6 |
Values in boldface indicate statistical significance. BMI, body-mass index; CI, confidence interval.
DISCUSSION
The importance of continued research on breast implants and BII cannot be understated, as breast augmentation procedures only increase with each passing year.22 Although the association of breast implants with autoimmune or systemic symptoms remains an ongoing and highly debated topic, their effect on lowering feelings of self-reported general health and physical functioning has been found to be very real.16 This is further supported by literature reporting improved symptoms with implant removal and capsulectomy,14–17 including a recent study where an astounding 96% reported improvement or complete resolution of their symptoms after explantation.23 The reporting of these data, combined with a growing public concern, has resulted in a 30.7% increase in breast implant removal since 2006.24 Plastic surgery is already a unique surgical specialty, with many procedures having a profound effect on a patient’s psychiatric well-being.13 If the aim is to truly improve well-being through surgery that addresses both form and function, then the specialty should collectively strive for continued clarity on BII, particularly for the purpose of caring for these patients with a more optimized, multi-faceted approach. Unfortunately, there is a paucity of knowledge available on how to optimize this approach and refine expectant management for both the patient and surgeon.
Our study provides an objective assessment of patients’ perceptions of their outcomes following explantation for suspected or diagnosed BII. The aim was not only to evaluate patient-reported satisfaction and the effect of explant on systemic complaints, but also to better characterize what symptoms may be more likely to improve with surgery, as well as what patient-related factors may affect that improvement. The symptoms experienced by patients in our cohort were similar to those reported in other large BII studies.23,25 before explantation, most patients reported fatigue (n = 17, 85%), chest discomfort (n = 14, 70%), and joint pain (n = 14, 70%). None of the patients had lupus, connective tissue disease, or any other type of autoimmune condition that may have contributed to their fatigue and arthralgia.
Expectation Management
All patients in this study were treated with standardized implant removal via an IMF incision, followed by total capsulectomy that included the posterior capsule wall. Fourteen patients (70%) showed net improvement in their symptoms after undergoing the procedure. The symptoms that most frequently improved included chest discomfort, muscle pain, fever, and headaches. With much of the cohort having breast implant placement in the submuscular plane (75%, n = 1%) and the most improved symptoms being chest discomfort and muscle pain, this could suggest that the need for mechanical relief is very much significant in the etiology of BII. The relationship between cause and effect in the development of BII is complex. Although it is possible that the psychological symptoms of BII contribute to the development of physical symptoms, it can also be bidirectional, with women having difficulty coping with the physical symptoms and thereby contributing to the emotional symptoms.26,27 Patients were least likely to see improvements in joint pain, weight problems, and insomnia. Explicitly reviewing expected outcomes such as these helps set realistic surgical goals for the patient and allows them to seek alternative treatments for symptoms less likely to be alleviated by implant removal. Most importantly, we believe it is imperative to discuss the individual components of the BREAST-Q, as this may provide patients with a clearer perspective on what their outcome and experience may resemble following explantation.
The majority of women in the study were found to have moderate satisfaction with their psychosocial well-being, but moderately low satisfaction with their breasts and even lower satisfaction with sexual well-being. Physical well-being was the only domain that received consistently high scores across the cohort and contradicted previous literature that found physical well-being to remain lower for patients with BII, even after implant removal.28 In theory, bringing these topics to discussion enables counseling to become more than just a debate about whether implant removal will result in the complete resolution of symptoms. When fixated on a constellation of symptoms that may or may not be related to their breasts, patients might not give themselves the chance to truly consider their satisfaction with their breast appearance and overall body image, how their breasts will feel, or their resultant sexual confidence. This conversation may also help bridge the gap between the discussion on implant removal and considerations regarding adjunctive cosmetic procedures.
Patients seeking the removal of their breast implants can often become hyper-focused on explantation, leaving it up to the surgeon to redirect some of their focus on the topic of secondary revision. Although the topic may initially be deferred by the patient, it is important that they understand how both time and the implant itself can cause structural changes in the breast footprint and overlying soft tissue.14,29 Although not utilized in any patients in this study, preoperative in-office implant deflation is one way to accurately depict a postexplantation breast appearance, for those with saline implants who are committed to removal but unsure about the need for mastopexy. Recently, an algorithm and discussion has also been published on the utility of postexplantation mastopexy in BII patients desiring cosmetic revision of the affected breasts.30,31 Using such literature may be useful in assisting both the surgeon and patient collaboratively in selecting the ideal breast lift and implant removal approach. In our cohort, only two patients reported wishing that they had never had their breast implants removed at all, with both attributing their feelings to too little education and ultimately dissatisfaction with the end appearance of their breasts. Thus, taking a firm stance in having a more in-depth discussion about secondary revision and staging procedures may help prevent such patient-reported outcomes. Additionally, showing before and after pictures of other patients can also be an effective way to educate BII patients on their presumed aesthetic result and help aid their decision on whether to undergo implant removal.
Patient-related Factors
A unique aspect of caring for BII patients is understanding how patient-related characterizations play a role in not only the portrayal of their symptoms but also how they affect outcomes after surgery. It has been previously found that women with BII, regardless of whether they have undergone explant surgery, report experiencing more severe somatic symptoms, higher depression and anxiety, and poorer physical health than women without BII.32 With nearly half (40%) of our BII cohort having a generalized anxiety disorder and 35% having a major depressive disorder, one would expect these conditions to have some causal link or key role in how they affect symptoms and quality of life in the postoperative setting. However, the presence of psychiatric illnesses had no statistically significant effect on the outcomes of our patients.
Upon embarking on this study, one psychological tendency that we expected to find was the presence of some level of confirmation bias in our outcomes, especially in those who paid for their own implant removal. Due to their being a financial event and/or investment, we believe it could have a significant effect on their belief that explantation would cure their systemic symptoms, despite contrary evidence. However, although we did not find a significant correlation between self-pay and impact on symptoms, we did find that those who self-paid had increased breast satisfaction scores (P = 0.009), attributing to the idea that those who get their explant covered by insurance may be more likely to be unsatisfied and critical of the cosmetic appearance of their breasts.
Implant-related Factors
Capsular contracture was one factor that played a significant role in our outcomes. Although we already noted that many of our patients scored moderate to moderately low in terms of satisfaction on the BREAST-Q, capsular contracture was statistically significant and predictive of reduced psychosocial, sexual, and breast satisfaction scores (P = 0.01). When counseling patients who have both BII and a history of capsular contracture preoperatively, with regard to implant removal, additional precautions should be taken to warn the patient of this clinical prediction so that the necessary measures can be taken to achieve a more optimal-appearing breast.
Finally, the time to implant removal unsurprisingly played a role in patient satisfaction in our study, similar to previously published literature.1,23 Although some believe that BII develops between years seven and ten, it makes sense that one particular study showed that the reduction in systemic symptoms was significantly higher in women who removed their implants within 10 years after implantation.1 The average time to implant removal was 13.2 years, but the analysis showed that reduced time to implant removal was predictive of fewer residual symptoms (P = 0.032). This finding supports the idea that early recognition of these systemic symptoms is pivotal in leading to quicker implant removal, thus attributing to a greater reduction in systemic symptoms, fewer residual symptoms, and, in turn, increased patient satisfaction.
This study has the following limitations: First, the overall power due to our patient population only encompassed those who underwent breast augmentation, and not reconstruction. However, there may be benefits to individually characterizing these two groups, as those who experience cancer, cancer-related treatment, and reconstruction can have many different types of pain and symptoms. Additionally, patients were not surveyed at the same time following removal, allowing for the presence of other possible sequelae that could affect their symptom profile. Although a validated BREAST-Q tool was provided to each subject, along with the ASAPS attachment and other innovative components, the retrospective nature of this cohort study may be subject to recall bias and response bias, as the symptoms reported by patients in the survey may not represent all symptoms associated with BII, and those reported may be from more enthusiastic patients who had symptomatic improvement. Furthermore, even if poorly understood, we acknowledge that the presence of psychiatric disorders in this patient population play a role in symptom recall, despite having no statistical significance in our outcomes.
CONCLUSIONS
In the setting of suspected or diagnosed BII, a reduced time to implant removal may decrease the risk of residual symptoms and improve overall patient satisfaction. The vast majority (70%) of patients who underwent implant removal reported improvement in their symptoms, regardless of the implant type. However, for patients with a history of capsular contracture, preoperative counseling should emphasize that implant removal may only improve physical symptoms and discomfort related to submuscular placement.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 25 September 2023.
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Spit KA, Scharff M, de Blok CJ, et al. Patient-reported systemic symptoms in women with silicone breast implants: a descriptive cohort study. BMJ Open. 2022;12:e057159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watad A, Rosenberg V, Tiosano S, et al. Silicone breast implants and the risk of autoimmune/rheumatic disorders: a real-world analysis. Int J Epidemiol. 2018;47:1846–1854. [DOI] [PubMed] [Google Scholar]
- 3.Caravantes-Cortes M-I, Roldan-Valadez E, Zwojewski-Martinez R-D, et al. Breast prosthesis syndrome: pathophysiology and management algorithm. Aesthetic Plast Surg. 2020;44:1423–1437. [DOI] [PubMed] [Google Scholar]
- 4.Breiting VB, Hölmich LR, Brandt B, et al. Long-term health status of Danish women with silicone breast implants. Plast Reconstr Surg. 2004;114:217–26; discussion 227–228. [DOI] [PubMed] [Google Scholar]
- 5.Lipworth L, Holmich LR, McLaughlin JK. Silicone breast implants and connective tissue disease: No association. Semin Immunopathol. 2011;33:287–294. [DOI] [PubMed] [Google Scholar]
- 6.Maijers MC, de Blok CJ, Niessen FB, et al. Women with silicone breast implants and unexplained systemic symptoms: a descriptive cohort study. Neth J Med. 2013;71:534–540. [PubMed] [Google Scholar]
- 7.Tugwell P, Wells G, Peterson J, et al. Do silicone breast implants cause rheumatologic disorders? A systematic review for a court-appointed national science panel. Arthritis Rheum. 2001;44:2477–2484. [DOI] [PubMed] [Google Scholar]
- 8.Karlson EW, Lee IM, Cook NR, et al. Comparison of self-reported diagnosis of connective tissue disease with medical records in female health professionals: the women’s health cohort study. Am J Epidemiol. 1999;150:652–660. [DOI] [PubMed] [Google Scholar]
- 9.Hennekens CH, Lee IM, Cook NR, et al. Self-reported breast implants and connective-tissue diseases in female health professionals: a retrospective cohort study. JAMA. 1996;275:616–621. [PubMed] [Google Scholar]
- 10.Sánchez-Guerrero J, Colditz GA, Karlson EW, et al. Silicone breast implants and the risk of connective-tissue diseases and symptoms. N Engl J Med. 1995;332:1666–1670. [DOI] [PubMed] [Google Scholar]
- 11.Gabriel SE, O’Fallon WM, Kurland LT, et al. Risk of connective-tissue diseases and other disorders after breast implantation. N Engl J Med. 1994;330:1697–1702. [DOI] [PubMed] [Google Scholar]
- 12.Peters W, Keystone E, Snow K, et al. Is there a relationship between autoantibodies and silicone-gel implants? Ann Plast Surg. 1994;32:1–5; discussion 57. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan J, Rohrich R. Breast implant illness: a topic in review. Gland Surg. 2021;10:430–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katsnelson JY, Spaniol JR, Buinewicz JC, et al. Outcomes of implant removal and capsulectomy for breast implant illness in 248 patients. Plast Reconstr Surg Glob Open. 2021;9:e3813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Boer M, Colaris M, van der Hulst RRWJ, et al. Is explantation of silicone breast implants useful in patients with complaints? Immunol Res. 2017;65:25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rohrich RJ, Kenkel JM, Adams WP, et al. A prospective analysis of patients undergoing silicone breast implant explantation. Plast Reconstr Surg. 2000;105:2529–37; discussion 2538–2543. [DOI] [PubMed] [Google Scholar]
- 17.Wee CE, Younis J, Isbester K, et al. Understanding breast implant illness, before and after explantation: a patient-reported outcomes study. Ann Plast Surg. 2020;85(S1 Suppl 1):S82–S86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slavin SA, Goldwyn RM. Silicone gel implant explantation: reasons, results, and admonitions. Plast Reconstr Surg. 1995;95:63–69. [DOI] [PubMed] [Google Scholar]
- 19.Godfrey PM, Godfrey NV. Response of locoregional and systemic symptoms to breast implant replacement with autologous tissues: experience in 37 consecutive patients. Plast Reconstr Surg. 1996;97:110–116. [DOI] [PubMed] [Google Scholar]
- 20.Kaur M, Pusic AL, Cornacchi S, et al. Development of new BREAST-Q scales to measure the experience of breast implant illness. Plast Reconstr Surg Global Open. 2022;10:7–7. [Google Scholar]
- 21.de Vries CEE, Kaur MN, Klassen AF, et al. Understanding breast implant–associated illness: a delphi survey defining most frequently associated symptoms. Plast Reconstr Surg. 2022;149:p 1056e–p 1061e. [DOI] [PubMed] [Google Scholar]
- 22.The Aesthetic Society. Procedural Statistics. Available at https://www.theaestheticsociety.org/media/procedural-statistics.
- 23.Metzinger SE, Homsy C, Chun MJ, et al. Breast implant illness: treatment using total capsulectomy and implant removal. Eplasty. 2022;22:e5. [PMC free article] [PubMed] [Google Scholar]
- 24.Tian WM, Rames JD, Blau JA, et al. Contextualizing breast implant removal patterns with google trends: big data applications in surgical demand. Plast. Reconstr. Surg.—Glob. Open 2022;10:e4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee M, Ponraja G, McLeod K, et al. Breast implant illness: a biofilm hypothesis. Plast Reconstr Surg Global Open. 2020;8:e2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berben JA, Miseré RML, Schop SJ, et al. The Influence of personality on health complaints and quality of life in women with breast implants. Aesthet Surg J. 2023;43:245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bresnick S. Understanding breast implant illness: the important role of nocebo and placebo-like effects. Aesthet Surg J. 2023:43:399–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dinis J, Junn A, Allam O, et al. Patient-reported outcomes following implant removal for breast implant illness. Plast Reconstr Surg Global Open. 2021;9:35–36. [Google Scholar]
- 29.Rohrich RJ, Beran SJ, Restifo RJ, et al. Aesthetic management of the breast following explantation: evaluation and mastopexy options. Plast Reconstr Surg. 1998;101:827–837. [DOI] [PubMed] [Google Scholar]
- 30.Mowlavi A, Asghari A, Heydarlou D, et al. Breast lift algorithm for the treatment of breast implant illness requiring implant removal. Aesth Plast Surg. 2022;47:934–943. [DOI] [PubMed] [Google Scholar]
- 31.Parsa FD, Singh D. Invited discussion on: aesthetic plastic surgery breast lift algorithm for the treatment of breast implant illness requiring implant removal. Aesth Plast Surg. 2022;47:944–945. [DOI] [PubMed] [Google Scholar]
- 32.Newby JM, Tang S, Faasse K, et al. Commentary on: understanding breast implant illness. Aesthet Surg J. 2021;41:1367–1379. [DOI] [PubMed] [Google Scholar]