Abstract
Objectives:
To investigate the pre-operative and post-operative characteristics of patients suffering from chronic back and radicular pain who had percutaneous hydrodiscectomy. Hydrodiscectomy is an advanced percutaneous discectomy technique that utilizes a concentrated, high flow water current for the cutting and simultaneous tissue aspiration of the intervertebral disc.
Methods:
Retrospective cohort study at a single center. We assessed the eligibility of all patients who had undergone hydrodiscectomy in the orthopedic department of our institution for four years period. Out of 40 eligible patients, a total of 22 patients consented to participate in the study. Study period from March 2017 to February 2022.
Results:
Fifteen patients were males (68.2%), seven were females (31.8%). Mean age was 45.46 years. Patients had symptoms for a mean of 46.36 months prior to the procedure, and the mean extent of disc bulge was 5.2 mm. 68.2% of the patients reported a reduction in or complete elimination of the back pain and the radicular lower limbs pain following hydrodiscectomy. 95.5% of the patients experienced no pre-, intra-, or post-operative complications.
Conclusion:
Results demonstrate that percutaneous hydrodiscectomy is safe and effective in patients with chronic back and radicular pain due to disc herniation.
There is no consensus on the definition of chronic lower back pain. There is no clear line to demarcate when acute back pain becomes chronic. Some authors define it as back pain that lasts more than 7-12 weeks. The pain is regarded as chronic when it lasts beyond the expected period of healing.1
Herniation of lumbar disc is one of the most common causes for lower back pain and lumbar radiculopathy, representing a leading indication for spinal surgery.2 The estimated incidence and prevalence of disc herniation in adults is 0.2 and 3% respectively. The condition is primarily observed between the ages of 30 to 50 years and occurs approximately twice as often in men as in women.3
Disc herniation happens due to a failure in the annulus fibrosis integrity, with the faiulure of the annulus fibrosis the contents of the nucleus leak into the neural canal.4 Disc herniation commonly happens due to age-related degeneration, which is associated with dehydration of the nucleus pulposus and weakening of the annulus fibrosis. These processes in turn lead to progressive, symptomatic disc herniation.
Management of disc herniation includes conservative and surgical treatments, although conservative strategies represent the first-line option given the natural history of disc herniation. Patients often exhibit good responses to pain management strategies and steroid injections, with some even experiencing spontaneous regression.5 When conservative management fails in controlling the symptoms, surgery is suggested.6 Traditional open surgery techniques are associated with complications such as epidural hematoma, dural tears, infection, instability, recurrence, and failed back syndrome.7 Historically, the success rates for surgical treatment of disc prolapse have ranged from 49-98%, varying based on several contributing factors. Thus, there is a need to develop surgical techniques that have higher success rates and lower rates of postoperative complications.
Percutaneous discectomy has become the preferred choice for many spine surgeons, given its minimal invasiveness and the increased likelihood of good outcomes when compared with other procedures. Since the introduction of the percutaneous lumbar discectomy procedure in 1989,8 numerous percutaneous discectomy techniques were successful in treating the pain and disability in patients with radiculopathy due to mild disc herniation. Such techniques include chymopapain treatment,9 automated percutaneous disc decompression,10 laser disc decompression,11 nuclear decompression,12 electrothermal ablation,13 and radiofrequency ablation.14
There are 2 types of disc herniation—contained and non-contained. Open discectomy is the preferred treatment for non-contained disc herniations.15 Success rate for percutaneous lumber discectomy are reported to be from 29-96%, while that for microdiscectomy ranges from 72-90%, based on the method of evaluation for the treatment of contained disc herniation that failed in the conservative treatment protocol.16 Recent literature showed that patients who had percutaneous lumbar discectomy for herniated discs experienced fewer post-operative complications such as blood loss or tissue damage and a shorter hospital stay.16 Hydrodiscectomy (i.e., “hydrocision”) has emerged as a novel treatment strategy for disc herniation, having been introduced at our institution in March 2013. This is an advanced percutaneous discectomy technique that utilizes a concentrated, high flow water current for the cutting and simultaneous tissue aspiration (Figure 1). One cadaver-based study reported that the procedure can be performed both quickly and precisely using this technique.17
Figure 1.
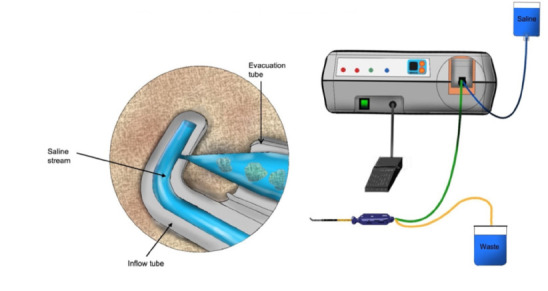
- The hydrocision machine and how it works.
The procedure is done percutaneously to treat patients suffering from contained disc herniations, thus reducing the need for in-patient surgical intervention. A posterolateral approach is utilized, which inflicts reduced trauma to muscles and ligaments.
Methods
We assessed the eligibility of all patients who underwent hydrodiscectomy in the orthopedic department of our institution for the duration of four years. Inclusion criteria: back pain and radiculopathy related to a specific nerve root, confirmed lumbosacral disc protrusion on mid-sagittal MRI series (Figure 2) corresponding to the dermatome/myotome identified clinically, and referral for decompression due to a lack of improvement after at least six months of commencement of symptoms, without response to conservative management techniques such as physiotherapy, modification of daily activities, weight control, and analgesics.
Figure 2.
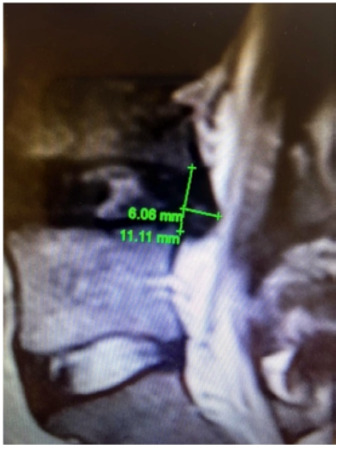
- Mid-Sagittal lumbar spine L4L5 disc protrusion, the protrusion measured at 6.06 mm and the disc height 11.11 mm.
Patients who had central stenosis, bone impingement or free-fragment herniation, and those who had undergone hydrodiscectomy at more than one level were excluded. Additional exclusion criteria were discogenic pain without nerve root compression (non-specific back pain), mechanical back pain, spondylolisthesis, and cervical or thoracic disc herniation.
We aimed to analyze pre-operative and post-operative data related to demographic characteristics, pain, complication rates, and the need for a revision surgery among patients with chronic symptoms undergoing percutaneous hydrodiscectomy at a single institution.
Prior related research was searched for using PubMed with the help of Endnote software using selected keywords.
Ethical approval for this study was obtained from the institutional review board of King Abdullah International Medical Research Center (KAIMRC). IRB approval number - SP17/048/J.
IBM Statistical Package for Social Sciences Software for Windows, v. 25 was utilized for statistical analysis. Descriptive analysis was done presenting the continuous variable as means and the categorial variables were presented as frequencies and percentages. No comparative analyses were carried out as this is a descriptive study.
In this study, we used a hydrodiscectomy device (Figure 1) that enables the removal of the nucleus pulposus by generating high levels of kinetic energy in a closed saline circuit.
The hydrodiscectomy procedure is performed using a transforaminal approach by inserting a spinal needle and then a guide wire using the Kambin’s triangle. A 4mm working channel is then inserted percutaneously with the help of an image intensifier. A dilator is used to dilate the annulus fibers rather than cutting through them, this allows them to shrink back into position thereafter, and so reducing the risk of re-herniations. The spine fluid-jet percutaneous resector is inserted through the working channel to simultaneously ablate, cut, and remove targeted tissue using a focused, high stream of water that enables precise tissue resection. The removed tissue is collected in a closed system which reduces the intradiscal pressure and allows the disc to shrink, reducing the compression on the nerve root(s). This system has the power density of a laser and uses radiofrequency technologies but does not cause thermal tissue damage.
The procedure is performed in an outpatient setting under local anesthesia, it lasts around 30 minutes. Being done under local anaesthesia can help closely monitor for nerve root irritation during the insertion of the spinal needle and allows patients to go home the same day.
Using consecutive sampling, we reviewed our medical records and identified 40 patients meeting the above-mentioned eligibility criteria. All these patients had undergone hydrodiscectomy in the orthopedic department of our hospital. Study period extended from March 2017 to February 2022.
Results
Among the 40 eligible patients, 22 (mean age: 45.46 years) consented to participate in the study. Fifteen were males (68.2%), while the remaining 7 were females (31.8%) (Table 1). The mean symptoms duration prior to the procedure was 46.36 months, ranging from 9 months to 7 years (Table 2). The extent of disc bulge was calculated based on the most prominent area revealed on an MRI, averaging 5.2 mm measured in midsagittal MRI T2 weighted image (Figure 2).
Table 1.
- Distribution of the cohort into males and females.
| Valid | Frequency | Percentage | Cumulative percentage |
|---|---|---|---|
| Male | 15 | 68.2 | 68.2 |
| Female | 7 | 31.8 | 100.0 |
| Total | 22 | 100 |
Table 2.
- Distribution of the cohort according to the duration of symptoms (in months) prior to intervention.
| Valid | Frequency | Percentage | Cumulative percentage |
|---|---|---|---|
| 12 or less | 7 | 31.8 | 31.8 |
| 12–24 | 3 | 13.6 | 45.4 |
| 24–36 | 1 | 4.6 | 50 |
| 36–48 | 3 | 13.6 | 63.6 |
| 48–60 | 3 | 13.6 | 77.2 |
| 60-72 | 1 | 4.6 | 81.8 |
| 72-84 | 4 | 18.2 | 100.0 |
| Total | 22 | 100 |
Seven of the 22 selected patients (31.8%) participated in a rehabilitation program after the procedure, while the remaining 15 (68%) did not attend any physiotherapy sessions post-operatively.
Regarding post-operative back pain, nine patients (40.9%) reported reduced pain following hydrodiscectomy, while 6 (27.3%) reported experiencing no pain at all. However, 2 patients (9.1%) reported that their pain had increased following surgery, and 5 patients reported that there was no change in pain pre- and post-operatively (Table 3).
Table 3.
- Back pain following hydrodiscectomy.
| Valid | Frequency | Percent | Cumulative percentage |
|---|---|---|---|
| No pain | 6 | 27.3 | 27.3 |
| Better than before | 9 | 40.9 | 68.2 |
| Same as before | 5 | 22.7 | 90.1 |
| Worse than before | 2 | 9.1 | 100.0 |
| Total | 22 | 100.0 |
Regarding radicular lower limb pain, 10 patients (45.5%) reported a postoperative reduction in radiating pain, while 5 (22.7%) reported experiencing no radiating pain following the procedure. However, 2 patients (9.1%) reported that their radiating pain had increased following surgery, and 5 patients (22.7%) reported no changes in radiating pain (Table 4).
Table 4.
- Radicular pain following hydrodiscectomy.
| Valid | Frequency | Percent | Cumulative percentage |
|---|---|---|---|
| No pain | 5 | 22.7 | 22.7 |
| Better than before | 10 | 45.5 | 68.2 |
| Same as before | 5 | 22.7 | 90.9 |
| Worse than before | 2 | 9.1 | 100.0 |
| Total | 22 | 100.0 |
The mean follow-up period for the study population was 12 months (7-108 months). For the purpose of the study, all patients were assessed for pain during their first visit to the outpatient department 2 weeks after the procedure. The improvement experienced during the acute post-operative period was sustainable in the study population. None of the participants in the studied group required further intervention(s).
Only one patient experienced postoperative complications (i.e., dural puncture) and suffered from headache, as a consequence. The patient was treated with an injection of Epidural Blood Patch under local anesthesia. This was done as an outpatient procedure; the patient responded very well to it and had a complete resolution of the symptoms.
Discussion
This study aims to investigate the preoperative characteristics and postoperative outcomes of patients who underwent percutaneous hydrodiscectomy after experiencing chronic back and radicular pain due to clinically and radiologically specific reasons. Our results indicated that 68.2% of the patients reported a reduction in or complete elimination of back pain and radicular lower limb pain following hydrodiscectomy. This result is in accordance with the clinical outcomes observed among patients who had undergone similar procedures.18–21 They required no further intervention(s) during the subsequent follow-up period, which extended from 7 months to 108 months. For patients who stayed in follow-up for the longest period, twelve months was the mean follow-up period considered. This result is in accordance with the literature for the short term.22 However, in the long term, revision surgeries were required.18,23 Apart from a single patient who had a dural puncture, 95.5% of the patients experienced no pre-, intra-, or post-operative complications. Hydrodiscectomy may be advantageous in comparison to other similar procedures, as it does not rely on the use of heat or chemical agents, which potentially reduces the risk of complications.
Despite appropriate referral to rehabilitation programs, only 31.8% of the patients participated in such programs following hydrodiscectomy. Physiotherapy might help in decreasing pain and encourage patient mobilization post-surgery. This might be the reason why some patients did not feel it necessary to attend these physiotherapy sessions, as they did not feel that they needed them.
Given that this procedure is relatively new, additional large-scale studies and clinical trials are recommended to measure the efficacy of hydrodiscectomy on functional status and quality of life.
Extensive training and reliance on experienced surgeons can further improve the patients’ experience and reduce the duration of hospitalization, thereby reducing medical costs for institutions and families.
Limitations
Retrospective design and limited number of cases are the two major limitations of this study.
Recommendations
Further prospective studies/RCTs involving a larger numbers of patients facing this issue for a longer period of time are recommended.
Conclusion
Our results demonstrate that minimally invasive percutaneous hydrodiscectomy is safe and effective to manage patients with chronic back and radicular pain due to disc herniation. This treatment strategy represents another option prior to referral for decompression surgery when conservative management strategies have proven to be ineffective even in chronic cases. This procedure might help improve patient outcomes and reduce the length of hospitalization.
Acknowledgment
We would like to thank Paper True (http://www.papertrue.com/) for English language editing.
Footnotes
References
- 1.Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999; 354: 581–585. [DOI] [PubMed] [Google Scholar]
- 2.Martin BI, Mirza SK, Flum DR, Wickizer TM, Heagerty PJ, Lenkoski AF, et al. Repeat surgery after lumbar decompression for herniated disc: The quality implications of hospital and surgeon variation. Spine J. 2012; 12: 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grotle M, Smastuen MC, Fjeld O, Grovle L, Helgeland J, Storheim K, et al. Lumbar spine surgery across 15 years: Trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open 2019; 9: e028743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Creer WS. Appearance of protruded disks. Lancet 1947; 2: 70. [DOI] [PubMed] [Google Scholar]
- 5.Turk O, Antar V, Yaldiz C.. Spontaneous regression of herniated nucleus pulposus: The clinical findings of 76 patients. Medicine (Baltimore) 2019; 98: e14667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozer AF, Keskin F, Oktenoglu T, Suzer T, Ataker Y, Gomleksiz C, et al. A novel approach to the surgical treatment of lumbar disc herniations: Indications of simple discectomy and posterior transpedicular dynamic stabilization based on carragee classification. Adv Orthop 2013; 2013:270565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joaquim AF, Botelho RV, Mudo ML, de Almeida AS, Bernardo WM.. Lumbar herniated disc - endoscopic discectomy treatment. Rev Assoc Med Bras (1992) 2018; 64: 397–407. [DOI] [PubMed] [Google Scholar]
- 8.Kafadar A, Kahraman S, Akboru M.. Percutaneous endoscopic transforaminal lumbar discectomy: a critical appraisal. Minim Invasive Neurosurg 2006; 49: 74–79. [DOI] [PubMed] [Google Scholar]
- 9.Dabezies EJ, Langford K, Morris J, Shields CB, Wilkinson HA. Safety and efficacy of chymopapain (Discase) in the treatment of sciatica due to a herniated nucleus pulposus. Results of a randomized, double-blind study. Spine (Phila Pa 1976) 1988; 13: 561–565. [DOI] [PubMed] [Google Scholar]
- 10.Chatterjee S, Foy PM, Findlay GF.. Report of a controlled clinical trial comparing automated percutaneous lumbar discectomy and microdiscectomy in the treatment of contained lumbar disc herniation. Spine (Phila Pa 1976) 1995; 20: 734–738. [DOI] [PubMed] [Google Scholar]
- 11.Casper GD, Mullins LL, Hartman VL.. Laser-assisted disc decompression: A clinical trial of the holmium:YAG laser with side-firing fiber. J Clin Laser Med Surg 1995; 13: 27–32. [DOI] [PubMed] [Google Scholar]
- 12.Derby R, Baker RM, Lee CH.. Evidence-informed management of chronic low back pain with minimally invasive nuclear decompression. Spine J 2008; 8: 150–159. [DOI] [PubMed] [Google Scholar]
- 13.Freeman BJ, Fraser RD, Cain CM, Hall DJ, Chapple DC.. A randomized, double-blind, controlled trial: intradiscal electrothermal therapy versus placebo for the treatment of chronic discogenic low back pain. Spine (Phila Pa 1976) 2005; 30: 2369–2377; discussion 2378. [DOI] [PubMed] [Google Scholar]
- 14.Barendse GA, van Den Berg SG, Kessels AH, Weber WE, van Kleef M.. Randomized controlled trial of percutaneous intradiscal radiofrequency thermocoagulation for chronic discogenic back pain: Lack of effect from a 90-second 70 C lesion. Spine (Phila Pa 1976) 2001; 26: 287–292. [DOI] [PubMed] [Google Scholar]
- 15.Gibson JN, Waddell G.. Surgical interventions for lumbar disc prolapse: Updated Cochrane review. Spine (Phila Pa 1976) 2007; 32: 1735–1747. [DOI] [PubMed] [Google Scholar]
- 16.Cristante AF, Rocha ID, Marcon RM, Filho TE.. Randomized clinical trial comparing lumbar percutaneous hydrodiscectomy with lumbar open microdiscectomy for the treatment of lumbar disc protrusions and herniations. Clinics (Sao Paulo) 2016; 71: 276–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huh HY, Ji C, Ryu KS, Park CK.. Comparison of SpineJet™ XL and conventional instrumentation for disk space preparation in unilateral transforaminal lumbar interbody fusion. J Korean Neurosurg Soc 2010; 47: 370–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klessinger S. The frequency of re-surgery after lumbar disc nucleoplasty in a ten-year period. Clin Neurol Neurosurg 2018; 170: 79–83. [DOI] [PubMed] [Google Scholar]
- 19.Patel N, Singh V.. Percutaneous lumbar laser discectomy: Literature review and a retrospective analysis of 65 cases. Photomed Laser Surg 2018; 36: 518–521. [DOI] [PubMed] [Google Scholar]
- 20.Liu C, Zhou Y.. Percutaneous endoscopic lumbar discectomy and minimally invasive transforaminal lumbar interbody fusion for massive lumbar disc herniation. Clin Neurol Neurosurg. 2019; 176: 19–24. [DOI] [PubMed] [Google Scholar]
- 21.Lee JH, Lee SH.. Clinical efficacy of percutaneous endoscopic lumbar annuloplasty and nucleoplasty for treatment of patients with discogenic low back pain. Pain Med 2016; 17: 650–657. [DOI] [PubMed] [Google Scholar]
- 22.Choi KC, Kim JS, Park CK.. Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Physician 2016; 19: E291–E300. [PubMed] [Google Scholar]
- 23.Eun SS, Lee SH, Sabal LA.. Long-term follow-up results of percutaneous endoscopic lumbar discectomy. Pain Physician 2016; 19: E1161–E1166. [PubMed] [Google Scholar]


