Abstract
This study aimed to elicit the preferences and willingness-to-pay for blood pressure (BP) telemonitoring programs. This study also investigated the different factors or participant characteristics that could influence preferences and choice behaviors. Participants with hypertension were identified from an online survey panel demographically representative of Singapore’s general population. Participants completed a discrete choice experiment (DCE) with 12 choice sets, selecting their preferred BP monitoring program differing on five attributes: mode of consultation, BP machine type (with Bluetooth or not), BP machine price, monthly fee, and program duration. The base reference population (male, married, higher income, more formal education years, full-time worker, aged 55 to <65 years, and digital skills score of 36) preferred teleconsultation over in-person consultation, Bluetooth feature, lower machine price, lower monthly fee, and shorter program duration. A subgroup of participants can be considered teleconsultation-resistant, and three demographic factors were associated with lower preference for teleconsultation: female, fewer formal education years, and lower income. Considering the reference population and Bluetooth attribute, participants were willing to pay 66 SGD (~49 USD) additional for the machine to obtain the Bluetooth feature. Considering the reference population and teleconsultation attribute, participants were willing to pay 6.80 SGD (~5.10 USD) extra monthly fee for a program using teleconsultation. Here we report that amongst participants with hypertension, there is strong preference for the use of teleconsultation and a BP machine with Bluetooth feature in a BP monitoring program. However, a subgroup of participants are teleconsultation-resistant and would prefer in-person consultation.
Subject terms: Health care economics, Health services
Introduction
The global disease burden continues to grow with ageing populations and rising prevalence of chronic diseases1–4. Health systems have immense pressures to cope with the increasing demand for health services5. Clinicians face increased workload and time stresses6,7, while patients face long wait times and low consultation time with their healthcare providers8,9. There is thus a need for health systems to optimize the use of healthcare manpower and resources and to improve patient care and experience.
Telehealth can help ease the increasing pressures of the health systems and be used to support chronic disease care management10–12. Patients require regular consultations with their chronic disease care provider to ensure the monitoring of disease progression and control, as well as for medication titration. In-person visits could be burdensome and inefficient, taking up patients’ time and causing potential income loss, with long wait times for a short consultation session10,13,14. The use of teleconsultation for regular reviews and check-ins could thus replace in-person visits without losing quality of care.
With the advent of COVID-19, the use of telehealth services has seen an increase in popularity and adoption15–18, as it reduces the risk of infection by leaving home and being near the care provider and other patients in the waiting area19. COVID-19 has also created a shift in knowledge, attitudes, and behaviors toward the use of telehealth services, and could thus provide a timely catalyst for new telehealth programs. In recent years, one such telehealth program that was piloted by the Ministry of Health Office for Healthcare Transformation (MOHT) in Singapore is the Primary Tech Enhanced Care (PTEC) home blood pressure (BP) monitoring program for those with hypertension20.
Singapore had a ratio of 2.4 doctors per 1000 persons in 201821, which is a marked improvement from the ratio of 1.7 from 7 years earlier22. However, this ratio for a city-state remains low compared to other high-income economies with larger populations and rural areas22,23. At the same time, hypertension has a high prevalence in Singapore, with about 1 in 5 residents aged 30–69 years with BP ≥ 140/90 mmHg (18.9% in 2010, 21.5% in 2017)24. This prevalence is expected to rise by over 60% by 204025. At public hospitals’ specialist outpatient clinics and polyclinics, which are large public primary care centers, waiting times have been on the rise due to the increasing patient load, particularly those seeking care in managing their chronic diseases. Time spent per patient is also low, with physicians in polyclinics spending less than 10 min of consultation time for 89% of chronic cases26.
Improved hypertension management is key in preventing disease worsening and complications, thereby decreasing the disease burden for the patient and the health system. From a health system and health policy perspective, the use of telehealth, be it with teleconsultations and/or telemonitoring, could significantly improve hypertension management. Understanding which attributes of such a telehealth program are preferred by patients with hypertension would thus be key in the design, implementation, and scaling up of such programs12.
Health preference research provides insights into trade-offs that help inform healthcare service providers on optimal design and pricing27. Using a discrete choice experiment (DCE) administered to participants with hypertension, this study aimed to elicit the preferences and willingness-to-pay for BP telemonitoring programs. In addition, patient populations are not homogenous, and different factors or characteristics of patient subgroups could influence the different preferences and choice behaviors. This study thereby aimed to investigate these subgroup differences.
In summary, this study demonstrates that overall, amongst participants with hypertension, there is a strong preference for the use of teleconsultation and a BP machine with Bluetooth feature in a BP monitoring program. Participants with hypertension are willing to pay about 5 SGD more monthly for teleconsultation and 66 SGD more for the Bluetooth feature as part of the BP telemonitoring program. However, there is a subgroup of participants (i.e., female, lower income, and fewer formal education years) who are teleconsultation-resistant, and would prefer in-person consultation instead. With the advent of COVID-19, there has been increased use of and exposure to telehealth services and programs, thereby strengthening the acceptance of and preferences for the use of teleconsultation.
Results
Of the 229 participants in the online research platform that were invited to participate in this online survey, 216 started the survey, and 9 of them (all completers) indicated “No” to the question of being diagnosed with hypertension by a doctor. Of the 207 remaining eligible participants, 193 participants completed the full survey with the DCE section consisting of 12 choice sets. Summary statistics of the participants are presented in Table 1. The number of females and males was similar. Close to 38% of participants were aged 65 years or above, which was the retirement age in Singapore. About three-quarters of the participants were married. Close to 39% had fewer formal education years (11 years or less), and close to 38% of participants had full-time employment. Over one-quarter of participants were classified as with lower income (income below 3000 SGD, or those living in a 1-room public housing). The digital skills score, which was calculated with a summation (reverse scored) of the 10 adapted28 5-point Likert scale questions on the mastery in the use of digital technologies (Supplementary Fig. 1), had a mean of 35.1 (higher the better).
Table 1.
Baseline demographic of participants.
| Frequency | Percentage | |
|---|---|---|
| Gender | ||
| Male | 100 | 51.8% |
| Female | 93 | 48.2% |
| Ethnicity | ||
| Chinese | 170 | 88.1% |
| Malay, Indian, and others | 23 | 11.9% |
| Age group | ||
| Below 55 years | 52 | 26.9% |
| 55 years to below 65 | 68 | 35.2% |
| 65 years and above | 73 | 37.8% |
| Marital status | ||
| Married | 142 | 73.6% |
| Single, divorced, or widowed | 51 | 26.4% |
| Education years | ||
| Fewer formal education years | 75 | 38.9% |
| More formal education years | 118 | 61.1% |
| Employment | ||
| Full-time | 73 | 37.8% |
| Part-time or not working | 120 | 62.2% |
| Income group | ||
| Lower income | 49 | 25.4% |
| Higher income | 144 | 74.6% |
| Mean (min, median, max) | SD | |
| Digital skills score | 35.1 (10, 36, 50) | 9.1 |
The baseline demographic of the participants in the study are presented as a frequency and percentage of the total number of participants. The mean and standard deviation (SD) of the digital skills score of all the participants are also presented, along with the minimum (min), median, and maximum (max) scores.
A tabulation of the attributes and levels of the DCE is presented in Table 2. These attributes of the DCE were all features of a program within MOHT’s control to optimize: the mode of consultation, BP machine type (with Bluetooth or not), BP machine price, monthly fee, and duration of the program. All the levels of these attributes had positive chances of being chosen when they were presented to the participants as hypothetical choices (Table 2), suggesting that participants had to consider the trade-offs across different attributes. In about 50% of the choice tasks, participants chose not to enroll in the selected program. For the price of the machine, the monthly fee, and the duration of the program, the percentage of selection decreased as the values of these attributes increased to become longer or more expensive. Furthermore, the pattern of the percentages suggested that these attributes should be entered into the model as continuous variables. For example, as the duration of the program increased from 1 to 2 years, and to 3 years, the percentage of selection dropped from 55 to 50%, and then to 45%.
Table 2.
Appearance and selection frequencies of the discrete choice experiment.
| Attributes and levels | Total no. of appearances | Total no. of selection | Percentage of selection |
|---|---|---|---|
| Consultation mode | |||
| Teleconsult | 2315 | 1096 | 47.3% |
| In-person | 2317 | 1220 | 52.7% |
| BP machine type | |||
| Bluetooth BP machine | 2312 | 1223 | 52.9% |
| Non-Bluetooth BP machine | 2320 | 1093 | 47.1% |
| BP machine price | |||
| $50 | 1544 | 930 | 60.2% |
| $100 | 1541 | 767 | 49.8% |
| $150 | 1547 | 619 | 40.0% |
| Monthly fee | |||
| $5 | 1551 | 1017 | 65.6% |
| $10 | 1540 | 791 | 51.4% |
| $20 | 1541 | 508 | 33.0% |
| Minimum duration | |||
| 1 year | 1534 | 846 | 55.1% |
| 2 years | 1552 | 782 | 50.3% |
| 3 years | 1546 | 688 | 44.5% |
| None | 2316 | 1149 | 49.6% |
The appearances and selection frequencies (as total number and percentage of the appearances) for the different levels of the attributes used in the discrete choice experiment are presented.
Table 3 shows the preference weights from the mixed logit model analysis. There was no evidence of left-and-right bias in choice selection. The reference population preferred teleconsultation over in-person consultation (coefficient = 1.12, 95% CI = 0.79 to 1.44, P < 0.001) and Bluetooth feature (coefficient = 0.92, 95% CI = 0.64 to 1.20, P < 0.001). Lower machine prices (coefficient = –0.01, 95% CI = –0.02 to –0.01, P < 0.001), lower monthly fee (coefficient = –0.16, 95% CI = –0.18 to –0.15, P < 0.001), and shorter duration of program (coefficient = –0.34, 95% CI = –0.44 to –0.25, P < 0.001) were preferred. The magnitude of the coefficient of the monthly fee was about 12 times that of the machine price, which suggests that the participants converted the monthly fee into yearly cost when they made their decisions. Random preference heterogeneity at the individual level was significant for all the levels.
Table 3.
Mixed logit model results.
| Coefficient | 95% CI | P value | |
|---|---|---|---|
| Left | –0.12 | (–0.25 to 0.01) | 0.080 |
| Base reference population | |||
| None option | –0.37 | (–0. 85 to 0.11) | 0.134 |
| Teleconsultation | 1.12 | (0.79 to 1.44) | <0.001 |
| Bluetooth | 0.92 | (0.64 to 1.20) | <0.001 |
| Machine price | –0.01 | (–0.02 to –0.01) | <0.001 |
| Monthly fee | –0.16 | (–0.18 to –0.15) | <0.001 |
| Duration | –0.34 | (–0.44 to –0.25) | <0.001 |
| Impact of demographic factors | |||
| None option * female | –0.22 | (–0.65 to 0.21) | 0.319 |
| None option * age above 65 | 0.45 | (0.02 to 0.89) | 0.042 |
| None option * not married | 0.96 | (0.45 to 1.47) | <0.001 |
| None option * fewer education years | –0.70 | (–1.10 to –0.30) | <0.001 |
| None option * digital skills score | 0.06 | (0.03 to 0.08) | <0.001 |
| Teleconsultation * female | –0.62 | (–0.95 to –0.30) | <0.001 |
| Teleconsultation * age below 55 | 0.10 | (–0.23 to 0.42) | 0.560 |
| Teleconsultation * not married | –0.26 | (–0.61 to 0.10) | 0.158 |
| Teleconsultation * fewer education years | –0.89 | (–1.19 to –0.59) | <0.001 |
| Teleconsultation * not full-time employment | –0.07 | (–0.38 to 0.23) | 0.649 |
| Teleconsultation * lower income | –0.53 | (–0.88 to –0.19) | 0.003 |
| Bluetooth * age below 55 | –0.44 | (–0.78 to –0.10) | 0.011 |
| Bluetooth * age above 65 | –0.27 | (–0.61 to, 0.07) | 0.121 |
| Bluetooth * not full-time employment | –0.11 | (–0.41 to 0.19) | 0.456 |
| Machine price * age below 55 | –0.005 | (–0.009 to –0.001) | 0.008 |
| Monthly fee * lower income | 0.05 | (0.02 to 0.08) | <0.001 |
| Monthly fee * digital skills score | –0.002 | (–0.003 to 0) | 0.036 |
| Random preference heterogeneity at the individual level | |||
| None option | 4.78 | (4.27 to 5.28) | <0.001 |
| Teleconsultation | 2.48 | (2.22 to 2.74) | <0.001 |
| Bluetooth | 0.86 | (0.69 to 1.03) | <0.001 |
| Machine price | 0.005 | (0.004 to 0.007) | <0.001 |
| Monthly fee | 0.10 | (0.09 to 0.12) | <0.001 |
| Duration | 0.58 | (0.49 to 0.68) | <0.001 |
Mixed logit model results with control of demographic factors are presented, along with the 95% confidence intervals (95% CI) of the coefficient. The P values presented are for the t test for the significance of the coefficients in the mixed logit model. The base reference population were male; married; higher income; more formal education years; full-time worker; age at 55 years to below 65; and with a digital skills score of 36 (median). The interaction of demographic factors with the levels of the DCE attributes are denoted with an asterisk (*).
The coefficient for Bluetooth of participants aged below 55 years is –0.44 (95% CI = –0.79 to –0.10, P = 0.011), i.e., 0.44 lower compared to that of the reference population participants, which is 0.92, thereby equating to a preference weight of 0.48 (0.92 subtracting 0.44). Participants aged below 55 years had preference weight coefficients lower than that of the reference population participants for machine price. Participants with lower income and participants with lower digital skills score had preference weight coefficients lower in absolute terms than that of the reference population participants for monthly fee.
Comparing teleconsultation with in-person consultation, three factors were associated with lower preference for teleconsultation: being female, having fewer formal education years, and having a lower income. In our overall study sample, there is a significantly greater portion of females with fewer formal education years than males (P = 0.020). This difference was found between females and males that are 65 years old and above (P = 0.02), but not between females and males that are below 65 years old (P = 0.300). The preference weight coefficients for teleconsultation of female participants, participants with fewer formal education years, and lower-income participants, are 0.63, 0.89, and 0.53 lower, respectively, than that of the reference population participants, which is 1.12. The preference weights for teleconsultation of female participants, participants with fewer formal education years, and lower-income participants, thus equate to 0.49, 0.23, and 0.59, respectively. For participants with these three characteristics, their preference weight was –0.32 for teleconsultation. Hence, combining these three characteristics, this formed a subgroup of participants that were female, with fewer formal education years, and lower income, named “Low SES Female”, who preferred face-to-face consultation over teleconsultation.
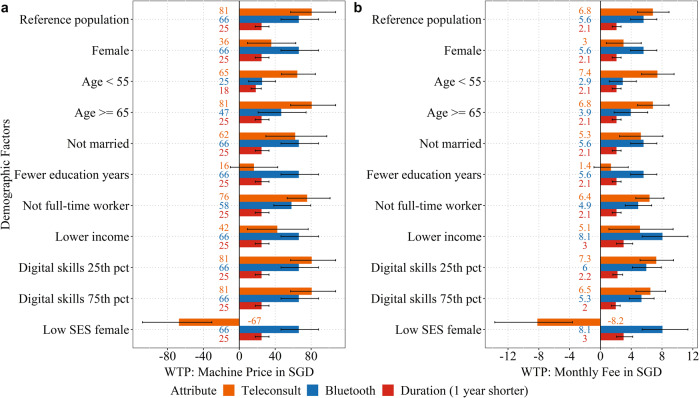
Willingness-to-pay, in 2020 values, with 95% confidence interval are presented in Fig. 1. Panel A uses the price of BP machine to calculate the willingness-to-pay. Considering the reference population and Bluetooth attribute, the participants were willing to pay 66 SGD (~49 USD) additional for the BP machine to obtain the Bluetooth feature. Panel B uses the monthly fee to calculate willingness-to-pay. Considering the reference population and teleconsultation attribute, the participants were willing to pay 6.80 SGD (~5.10 USD) additional for monthly fee for a program using teleconsultation. The bars for the different demographic factors show the willingness-to-pay by changing that demographic factor while all other demographic factors are held fixed like the reference population. For example, the bars for female show the willingness-to-pay of female participants that are also aged at 55 years to below 65 years, married, with more formal education years, full-time worker, with higher income, and with digital skills score at the median of the sample (score of 36). This is except for the combination subgroup “Low SES Female”, which is a combination of multiple demographic factors.
Fig. 1. Willingness-to-pay.
Willingness-to-pay for the program using teleconsultation, Bluetooth feature of BP machine, or 1 year shorter duration of the program measured by a the price of blood pressure (BP) machine and b the monthly fee. The base “reference population” comprise of those who were male, married, with higher income, with more formal education years, full-time worker, aged at 55 years to below 65 years, and with a digital skills score of 36 (median). Digital skills score was calculated with a summation (reverse scored) of the 10 adapted 5-point Likert scale questions on the mastery in the use of digital technologies, and a higher score is indicative of having higher mastery. Digital skills score at the 25th percentile (“digital skills 25th pct”) and at the 75th percentile (“digital skills 75th pct”) have a 6- and 5-point difference from the median score. The “low SES female” comprise of subgroup of participants that were female, with fewer formal education years, and lower income. Error bars indicate the 95% confidence intervals of the willingness-to-pay.
Willingness-to-pay for Bluetooth and the duration of the program were similar across different groups. However, willingness-to-pay for teleconsultation was different across different groups; and notably, participants with lower income and fewer formal education years had a lower preference weight for teleconsultation. The “Low SES Female” group could be considered to be teleconsultation-resistant. This group was willing to pay 67 SGD (~50 USD) more for the machine, or 8.20 SGD (~6.10 USD) more for the monthly fee, if they could switch from teleconsultation to in-person consultation.
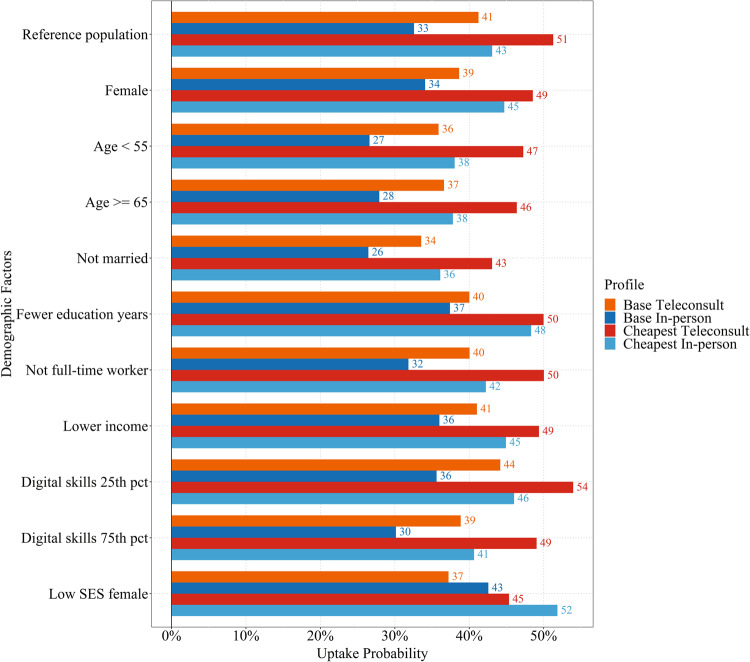
Program uptake probabilities are presented in Fig. 2. We considered the following program profiles: (1) Base Teleconsult: teleconsultation, Bluetooth machine, machine price at 100 SGD, monthly fee at 10 SGD, mandatory program duration of 2 years; (2) Base In-Person: in-person consultation, Bluetooth machine, machine price at 100 SGD, monthly fee at 10 SGD, mandatory program duration of 2 years; (3) Cheapest Teleconsult: teleconsultation, Bluetooth machine, machine price at 50 SGD, monthly fee at 5 SGD, mandatory program duration of 1 year; (4) Cheapest In-Person: in-person consultation, Bluetooth machine, machine price at 50 SGD, monthly fee at 5 SGD, mandatory program duration of 1 year.
Fig. 2. Program uptake probability.
Uptake probability for the four different program profiles across the different demographic factors and participant subgroups. The base “reference population” comprised of those who were male, married, with higher income, with more formal education years, full-time worker, aged at 55 years to below 65 years, and with a digital skills score of 36 (median). Digital skills score was calculated with a summation (reverse scored) of the 10 adapted 5-point Likert scale questions on mastery in the use of digital technologies, and a higher score is indicative of having higher mastery. Digital skills score at the 25th percentile (“digital skills 25th pct”) and at the 75th percentile (“digital skills 75th pct”) have a 6- and 5-point difference from the median score. The “low SES female” comprised a subgroup of participants that were female, with fewer formal education years, and lower income.
The bars for the different demographic factors show the uptake probability by changing one demographic factor at a time, except again for the combination subgroup “Low SES Female”. For the first two program profiles, the uptake probability ranged between 26 and 44%. In general, participants had higher chances of participating in the program if it was teleconsultation. For the Low SES Female group, however, the uptake probability is higher by around 6–7% for a program with in-person consultation. The third and fourth program profiles achieved the highest uptake probabilities, ranging between 36 and 56%. Overall, comparing the different program profiles, when the machine price decreases by 50 SGD, the monthly fee decreases by 5 SGD, and the program duration decreases by 1 year, the uptake probability consistently increased by 8–11%.
Discussion
The main finding that the base reference population preferred teleconsultation to in-person consultation, and valued having a Bluetooth feature in the BP machine, supports a large-scale adoption of a BP telemonitoring program for patients with hypertension. This finding corroborates recent findings on the positive receptivity for the use of teleconsultation and telemonitoring after the advent of COVID-1915–18, which has led to more prominent widespread use of teleconsultation and a strong demonstration of its utility. Previous studies conducted before COVID-19 have also found positive attitudes for the use of BP telemonitoring in stroke patients29,30. Unsurprisingly, this study found that a lower BP machine price, lower monthly fee, and shorter duration of commitment to the program was preferred over more expensive and longer programs.
In our study, three demographic factors were associated with a lower preference for teleconsultation: being female, having a lower income, and having fewer years of formal education. In our overall study sample, there was a significantly greater portion of females with fewer formal education years than males. This difference was driven by those that are 65 years old and above, which is expected as education opportunities were lower for females in the older generations. The demographic factor of older age group of 65 years and above alone was not found to influence the willingness-to-pay. As such, the teleconsultation-resistant group remains this intersection of the three demographic factors of being female, having a lower income, and having fewer years of formal education.
Some studies have found that the factor of female alone have higher preference31 or did have higher actualization14,32–34 of teleconsultation appointments, likely because they found teleconsultation convenient and time-saving. However, earlier studies have also shown that the combination of female, lower income, and with fewer formal education years were associated with lower access to the use of technology35,36. In our study, we found that the subgroup with this combination of these factors was willing to pay 67 SGD (~50 USD) more for the machine, or 8.20 SGD (~6.10 USD) more for the monthly fee if they could switch from teleconsultation to in-person consultation. Perhaps this particular subgroup has lesser access and exposure to teleconsultation, and thus less likely to discover the potential benefits that teleconsultation could bring. Nonetheless, the uptake probability for the cheapest Teleconsult program is similar to that of the base In-person program in this subgroup, indicating cost playing a more crucial role than just the mode alone.
A major implication from the findings is that equitable considerations have to be made in the care and management of patients with hypertension. The population of those with hypertension is not homogenous, with clear preferential differences differing for those of different demographic profiles. Even though this study elucidates an optimized design of a BP telemonitoring program that will maximize program uptake given the budget constrain from the government, the reality is that variations will have to exist to cater to those who would prefer a BP monitoring program with in-person consultation. Furthermore, the random preference heterogeneities at the individual level were significant for all the levels. These individual level heterogeneities could capture other factors affecting people’s preference but were not controlled in this study. Identifying all these factors can be costly and not feasible. In practice, the government could design a program which allows personal customization by patients themselves.
The program design being tested in our study has two financial components: machine price and monthly fee. While machine price is straightforward to consider, the monthly fee needs another step of calculations to understand the total cost. Our results showed that participants with lower digital skills score and participants with lower income were less sensitive (had lower disutility) to an increase in monthly fee. Participants with higher digital skills score may have experience with many free digital services online, and hence were more sensitive to the monthly fee. For participants with lower income, they had lower sensitivity to monthly fees but not machine price. This could be influenced by how clearly the participants understood the DCE task with the preamble (Supplementary Methods). Participants with lower income might have lower financial literacy and require additional steps to understand the full financial implication of such monthly fees. The correlation of low financial literacy with ineffective spending and financial planning has been well documented37. Numeracy in some population groups in the United States and other countries is low and these people have been found to make mistakes in financial decisions requiring simple calculations38. Hence, assisting patients in the understanding of the full financial implication of such health programs with complex cost components is important.
One of the key strengths of this study was the use of a DCE, which elicits preferences indirectly through choice selection, as opposed to direct reporting or ranking. Participants might not always declaratively know which factors they prefer or be able to quantify how important each factor is to them. Through the use of a DCE, how strongly the various attributes are as preferences can be elicited, and a quantifiable utility value generated. Another strength of this study was the timely investigation into preferences for telehealth programs as they become more mainstream after increased use and exposure due to COVID-19.
One of the limitations of this study was that the participants from the SPHS Online Panel were all able to read English, had access to the internet via a computer or smartphone and could use it to complete the survey. This meant that the participant pool would not have represented those unable to read English, and had no access or ability to use a computer or smartphone. However, it should be noted that the Singapore population has a high English literacy rate39 and a high percentage with access to the internet40, and so this limitation does not severely limit the generalizability of the participant cohort, although the findings may not generalize to other settings where internet access may act as a barrier to uptake of telemedicine. We also did a comparison of the demographic profile of our study sample (Supplementary Table 1) with that of a separate published study in Singapore that investigated the demographic profiles of those with hypertension using a multi-ethnic cohort in Singapore41. Compared to this cohort, our study sample has a smaller proportion with fewer years of formal education, smaller proportion with lower income, and are older. However, we cannot identify which sample is more representative of the patients with hypertension in Singapore, since the multi-ethnic cohort has a much lower proportion of Chinese than that in the general Singapore population.
Another limitation was that the participant pool was selected based on self-reporting of hypertension, with no additional verification or use of medical records. However, participants reported this diagnosis of hypertension as part of reporting on the chronic diseases that they have, without knowing that there would be a follow-up survey with hypertension as a criterion for selection. Therefore, there was a very low likelihood of false reporting in order to participate in this study. Those without an official clinical diagnosis of hypertension or had wrongly reported so before proceeded with this study survey and were identified with verification questions to filter their data out from analyses.
Methods
Study design and participants
The study was a cross-sectional online survey administered through the Singapore Population Health Studies (SPHS) Online Panel, approved by the National University of Singapore Institutions Review Board (NUS-IRB; Ref No.: H-18-011). This panel served as an online research platform that facilitated public health research on a diverse range of topics, through monthly surveys related to public health. When the survey was conducted, the panel was made up of 2413 active participants who were demographically representative of the general population of Singapore. Participants had already been recruited into the SPHS Online Panel and provided informed consent, hence no further recruitment was conducted. This study obtained a waiver for documented informed consent from the NUS-IRB (Ref No.: NUS-IRB-2020-82).
The survey was designed as a follow-up for participants who had indicated having hypertension in a separate survey by the research team administered four months prior (229 out of 1975). Of the 229 participants invited to participate in this survey, 216 started it, and 202 completed it. Nine participants (all completers) indicated “No” to the question on being diagnosed with hypertension by a doctor, and so their data were removed.
Procedures
Participants in the panel who met the above criteria for this survey received a notification by email and/or SMS about the survey in December 2020. Participants accessed the survey via the provided link and completed the survey on the Research Electronic Data Capture platform. The survey had an expiration date for completion within 10 days and was no longer accessible once it had expired. Before proceeding, participants were provided a participant information sheet. The survey had two parts: an initial 45 questions covering demographics, healthcare use, digital use, digital skills, and their hypertension management, followed by the DCE with 12 choice sets.
Selection of attributes for DCE
The use of DCEs is common in health preference research42,43 and has been found to have moderate predictive value of real-world choice behaviors44. MOHT was developing and implementing the PTEC home BP monitoring program for those with hypertension20, and was a key stakeholder for this study. MOHT was interested in investigating the optimal combinations of controllable attributes to roll out a sustainable scaled-up program.
The program by design would use teleconsultation in combination with a BP machine that has Bluetooth capabilities to automatically synchronize the readings for remote monitoring. For the program to be cost-effective and for the impact of the program to take hold, the design of the program would require patients’ commitment to enroll in the program for a fixed duration. Thus, the price of the BP machine and the monthly fee of the program were factors that MOHT was interested in investigating. The attributes chosen for the DCE were all features of such a program within MOHT’s control to optimize: the mode of consultation, BP machine type (with Bluetooth or not), BP machine price, monthly fee, and duration of the program.
DCE design
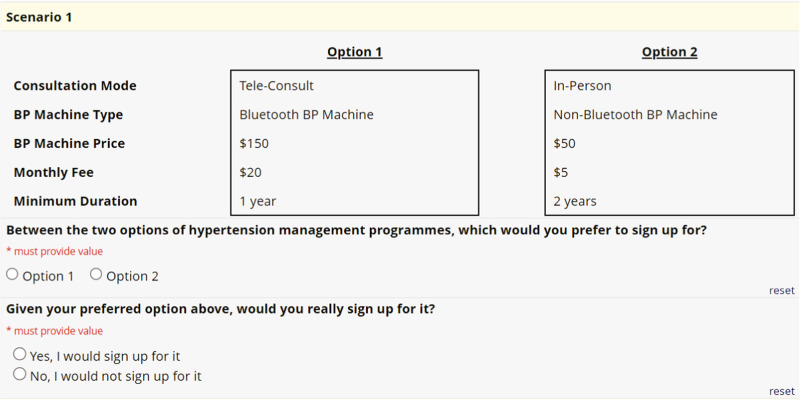
The final set of five attributes and levels is presented in Table 2. The DCE questionnaire was designed using Sawtooth Software Inc.’s Lighthouse Studio version 9.8. A two-stage design was used. The questionnaire was designed using the Balanced Overlap option provided by Lighthouse Studio, with only the main effects considered. Twenty blocks were used, with twelve tasks per block. A simulation exercise was conducted to examine the coverage matrix of the design and test the sample size required. An example of a DCE choice task is presented in Fig. 3.
Fig. 3. DCE choice task.
An example of one of the choice task questions in the discrete choice experiment.
Statistical analysis
Mixed logit model was used in the analysis to incorporate two types of preference heterogeneities: (1) preference heterogeneity that the demographic factors can explain and (2) random preference heterogeneity at the individual level. Equation (1) is the formula for the random utility of individual , for a program , where is a vector describing the details of the consultation program and is the idiosyncratic error term assumed to follow a type 1 extreme value distribution. Equation (2) is the formula for the term in Eq. (1). The term is a vector including the demographic factors in the analysis. The term shows the preference heterogeneity that is affected by demographic factors. The term follows multivariate normal distribution representing the random preference heterogeneity which includes all unobserved factors that affect individuals’ preferences.
| 1 |
| 2 |
Consultation mode and BP machine type were entered into the model as discrete variables. BP machine price, monthly fee, and minimum duration were entered into the model as continuous variables based on the tabulation pattern of the levels of each attribute and the percentage of selection. Bayesian information criterion (BIC) was compared between the model using continuous values and the model using discrete values for the three attributes of BP machine price, monthly fee, and minimum duration, one variable at a time. Smaller BICs were obtained for all models using continuous values compared to models using discrete values, confirming that these three attributes should be entered into our models as continuous variables.
Demographic factors that were entered into the model included gender, age group, marital status, education years, employment, income group, and digital skills score measuring the mastery that participants have with use of digital technologies such as smartphones. Age was classified into three categories: 65 years and above (the retirement age in Singapore), 55 years to below 65 years, and below 55 years. The choice of 55 years was chosen to ensure enough participants were in the lower age group for estimation. Marital status was classified into two categories: married and not married (single, divorced, or widowed).
Participants with education levels at secondary school or below were considered as having fewer formal education years (11 years or less), while participants with education levels above secondary school were considered as with more formal education years (more than 11 years). Employment status was classified into two categories: full-time and not full-time (part-time or not working). Information on household income and housing type were considered together to generate the two categories of income level: lower income and higher income. Participants with monthly household income below 3000 SGD, or those living in a 1-room public housing were categorized as lower income. The digital skills score was derived from a set of ten questions adapted from ref. 28, with participants rating on a 5-point Likert scale their mastery with regards to various uses of digital technology (Supplementary Fig. 1). The score was calculated with a summation of the ten questions (reversed scored) and a higher score is indicative of having higher mastery. The digital skills score was modeled as continuous, but with the score rescaled with the subtraction of the median to allow for ease of interpretation.
To examine how demographic factors affected preferences, the demographic factors were entered into the model by interacting with the levels of the DCE attributes. There are 48 possible interaction terms with full interaction, which could lead to multi-collinearity issues given the sample size. Therefore, in the selection of the final model, to achieve a parsimonious specification, one demographic factor at a time was considered, as well as its full interaction with the levels. Only interaction terms with P lower than 0.10 were kept in the final model.
The preference weights coefficients of the interaction terms indicate the preference weight differences between the reference population and the population with that demographic factor switched (i.e., all other factors remaining the same as the reference population except for that demographic factor). The base reference population comprised of those who were male, married, with higher income, with more formal education years, full-time worker, aged at 55 years to below 65 years, and with a digital skills score of 36 (median). Latent Class Analyses were also conducted but not included in the main results (Supplementary Note 1 and Supplementary Table 2).
Willingness-to-pay was calculated and presented in SGD, and can be taken to be December 2020 values. The USD values presented were calculated using the historical exchange rate on 1 December 202045. Krinsky and Robb’s method was used to generate the confidence intervals46. Uptake probability was calculated by considering a few desired program profiles. All statistical analyses were carried out using R47.
Supplementary information
Acknowledgements
This study was funded by the Singapore Ministry of Health Office for Healthcare Transformation. This study was conducted using the Singapore Population Health Studies Online Panel, which was funded through the Singapore Ministry of Health’s National Medical Research Council Centre Grant Programme (grant number NMRC/CG/C026/2017_NUHS) for Singapore Population Health Improvement Centre (SPHERiC). We would like to thank Shumian Yeo, Mark Salloway, and the rest of the Singapore Population Health Studies Online Panel team for supporting the setup, testing, and execution of the survey in this study. We would like to thank Satvinder Singh Dhaliwal for his inputs on the design and analyses approach of the discrete choice experiment. We would also like to thank Sharon Quaye, Jerrald Lau, and Chuan De Foo for their inputs on the design of the study, as well as Bob Xian Yi Ng and Clarence Ong for their inputs on the analyses of the data. We thank all the participants who took part in this study.
Author contributions
I.Y.H.A. and Y.W. contributed to this work equally and are co-first authors. I.Y.H.A., Y.W., S.T., and G.C.H.K. were responsible for the concept and design of the study. I.Y.H.A., S.T., G.C.H.K., and A.R.C. were responsible for obtaining funding for this study. I.Y.H.A. and A.R.C. were responsible for the recruitment of participants and data collection. Y.W. and I.Y.H.A. were responsible for the analysis of data. G.C.H.K. and A.R.C. provided supervision and administrative support. I.Y.H.A. and Y.W. wrote the first draft of the manuscript. All authors were involved in the interpretation of the data and worked on critical revisions of the manuscript. All authors read and approved the final manuscript.
Data availability
The data collected and analyzed in this study are only available from the corresponding author upon reasonable request and with permission of the institution review board.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41746-023-00919-3.
References
- 1.Song P, et al. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: a systematic review, meta-analysis, and modelling study. Lancet Glob. Health. 2020;8:e721–e729. doi: 10.1016/S2214-109X(20)30117-0. [DOI] [PubMed] [Google Scholar]
- 2.Roth GA, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J. Am. Coll. Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray CJL, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 4.Lozano R, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bodenheimer T, Chen E, Bennett HD. Confronting the growing burden of chronic disease: can the U.S. health care workforce do the job? Health Aff. 2009;28:64–74. doi: 10.1377/hlthaff.28.1.64. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, et al. Burnout and satisfaction with work-life balance among us physicians relative to the general US population. Arch. Intern. Med. 2012;172:1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt TD, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin. Proc. 2015;90:1600–1614. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Lee AA, James AS, Hunleth JM. Waiting for care: chronic illness and health system uncertainties in the United States. Soc. Sci. Med. 2020;264:113296. doi: 10.1016/j.socscimed.2020.113296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irving G, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7:e017902. doi: 10.1136/bmjopen-2017-017902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bashshur RL, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed. e-Health. 2014;20:769–800. doi: 10.1089/tmj.2014.9981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polisena J, Coyle D, Coyle K, McGill S. Home telehealth for chronic disease management: a systematic review and an analysis of economic evaluations. Int. J. Technol. Assess. Health Care. 2009;25:339–349. doi: 10.1017/S0266462309990201. [DOI] [PubMed] [Google Scholar]
- 12.Chua V, Koh JH, Koh CHG, Tyagi S. The willingness to pay for telemedicine among patients with chronic diseases: systematic review. J. Med. Internet Res. 2022;24:e33372. doi: 10.2196/33372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sayani S, et al. Addressing cost and time barriers in chronic disease management through telemedicine: an exploratory research in select low- and middle-income countries. Ther. Adv. Chronic Dis. 2019;10:2040622319891587. doi: 10.1177/2040622319891587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reed ME, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw. Open. 2020;3:e205873. doi: 10.1001/jamanetworkopen.2020.5873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Imlach F, et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam. Pract. 2020;21:269. doi: 10.1186/s12875-020-01336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ebbert, J. O. et al. Patient preferences for telehealth services in a large multispecialty practice. J. Telemed. Telecare 1357633X20980302. 10.1177/1357633X20980302 (2021). [DOI] [PubMed]
- 17.Chua, C. H., Seow, F. C., Tang, F. M. & Lim, L. M. Factors affecting telepractice use in COVID-19. Proc. Singapore Healthcare 20101058221074120. 10.1177/20101058221074120 (2022).
- 18.Ang IYH, et al. A personalized mobile health program for type 2 diabetes during the COVID-19 pandemic: single-group pre–post study. JMIR Diabetes. 2021;6:e25820. doi: 10.2196/25820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6:e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teo, V. H. et al. Effects of technology-enabled blood pressure monitoring in primary care: a quasi-experimental trial. J. Telemed. Telecare 1357633X211031780 10.1177/1357633X211031780 (2021). [DOI] [PMC free article] [PubMed]
- 21.MOH | Health Manpower. https://www.moh.gov.sg/resources-statistics/singapore-health-facts/health-manpower (2023).
- 22.OECD/World Health Organization. Health at a Glance: Asia/Pacific 2014: Measuring Progress towards Universal Health Coverage. 10.1787/health_glance_ap-2014-en (2014).
- 23.OECD. Health at a Glance 2017: OECD Indicators. 10.1787/health_glance-2017-en (2017).
- 24.Prevalence of hypertension, diabetes, high total cholesterol, obesity and daily smoking. Data.gov.sghttps://data.gov.sg/dataset/prevalence-of-hypertension-diabetes-high-total-cholesterol-obesity-and-daily-smoking (2019).
- 25.Ansah JP, Inn RLH, Ahmad S. An evaluation of the impact of aggressive hypertension, diabetes and smoking cessation management on CVD outcomes at the population level: a dynamic simulation analysis. BMC Public Health. 2019;19:1105. doi: 10.1186/s12889-019-7429-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Health Information Division, Ministry of Health. Primary Care Survey 2014. https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/reports/moh-primary-care-survey-2014-report.pdf?sfvrsn=6e773b6d_0 (2014).
- 27.Marsh K, et al. Health preference research in Europe: a review of its use in marketing authorization, reimbursement, and pricing decisions—report of the ISPOR stated preference research special interest group. Value Health. 2020;23:831–841. doi: 10.1016/j.jval.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Poli A, Kelfve S, Motel-Klingebiel A. A research tool for measuring non-participation of older people in research on digital health. BMC Public Health. 2019;19:1487. doi: 10.1186/s12889-019-7830-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jenkins C, et al. Stroke patients and their attitudes toward mHealth monitoring to support blood pressure control and medication adherence. Mhealth. 2016;2:24. doi: 10.21037/mhealth.2016.05.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nichols M, et al. Post-intervention qualitative assessment of mobile health technology to manage hypertension among Ghanaian stroke survivors. J. Neurol. Sci. 2019;406:116462. doi: 10.1016/j.jns.2019.116462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Polinski JM, et al. Patients’ satisfaction with and preference for telehealth visits. J. Gen. Intern. Med. 2016;31:269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fischer SH, Ray KN, Mehrotra A, Bloom EL, Uscher-Pines L. Prevalence and characteristics of telehealth utilization in the United States. JAMA Netw. Open. 2020;3:e2022302. doi: 10.1001/jamanetworkopen.2020.22302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eberly LA, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw. Open. 2020;3:e2031640. doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Latulippe K, Hamel C, Giroux D. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J. Med. Internet Res. 2017;19:e6731. doi: 10.2196/jmir.6731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hilbert M. Digital gender divide or technologically empowered women in developing countries? A typical case of lies, damned lies, and statistics. Women’s Stud. Int. Forum. 2011;34:479–489. doi: 10.1016/j.wsif.2011.07.001. [DOI] [Google Scholar]
- 36.Chilukuri N, et al. Information and communication technology use among low-income pregnant and postpartum women by race and ethnicity: a cross-sectional study. J. Med Internet Res. 2015;17:e163. doi: 10.2196/jmir.3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lusardi A. Financial literacy and the need for financial education: evidence and implications. Swiss J. Econ. Stat. 2019;155:1. doi: 10.1186/s41937-019-0027-5. [DOI] [Google Scholar]
- 38.Lusardi, A. Numeracy, financial literacy, and financial decision-making. Numeracy5, 10.5038/1936-4660.5.1.2 (2012).
- 39.Department of Statistics, Ministry of Trade & Industry, Republic of Singapore. Singapore Census of Population 2020, Statistical Release 1: Demographic Characteristics, Education, Language and Religion. Basehttp://www.singstat.gov.sg/publications/reference/cop2020/cop2020-sr1/census20_stat_release1 (2021).
- 40.Müller, J. Internet usage in Singapore - statistics & facts. Statistahttps://www.statista.com/topics/5852/internet-usage-in-singapore/ (2023).
- 41.Liew SJ, et al. Sociodemographic factors in relation to hypertension prevalence, awareness, treatment and control in a multi-ethnic Asian population: a cross-sectional study. BMJ Open. 2019;9:e025869. doi: 10.1136/bmjopen-2018-025869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21:145–172. doi: 10.1002/hec.1697. [DOI] [PubMed] [Google Scholar]
- 43.Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32:883–902. doi: 10.1007/s40273-014-0170-x. [DOI] [PubMed] [Google Scholar]
- 44.Quaife M, Terris-Prestholt F, Di Tanna GL, Vickerman P. How well do discrete choice experiments predict health choices? A systematic review and meta-analysis of external validity. Eur. J. Health Econ. 2018;19:1053–1066. doi: 10.1007/s10198-018-0954-6. [DOI] [PubMed] [Google Scholar]
- 45.Currency Converter | Foreign Exchange Rates | OANDA. https://www.oanda.com/currency-converter/en/ (2023).
- 46.Krinsky I, Robb AL. On approximating the statistical properties of elasticities. Rev. Econ. Stat. 1986;68:715–719. doi: 10.2307/1924536. [DOI] [Google Scholar]
- 47.R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data collected and analyzed in this study are only available from the corresponding author upon reasonable request and with permission of the institution review board.