Abstract
Remodeling of the arterial wall occurs mainly as a consequence of increased wall stress caused by hypertension. In this issue of the JCI, Azizi et al. report that in humans with a kallikrein gene polymorphism that lowers kallikrein activity, the brachial artery undergoes eutrophic inward remodeling in the absence of hypertension or other hemodynamic changes. It has also been reported that alterations of the kallikrein-kinin system are associated with formation of aortic aneurysms. Conversely, after vascular injury, kinins mediate the beneficial effect of angiotensin-converting enzyme inhibitors that prevent neointima formation. These findings raise the intriguing possibility that decreased kallikrein-kinin system activity may play an important role in the pathogenesis of vascular remodeling and disease, while increased activity may have a beneficial effect.
Kallikrein-kinin system, vascular expression, and release
Kinins (bradykinin and lysyl-bradykinin) have been implicated in the regulation of renal function, blood flow, and blood pressure (1). The vasodilator, natriuretic, and diuretic effects of kinins are mediated by the release of autacoids such as eicosanoids, NO, and endothelium-derived hyperpolarizing factor. Kinins are released from kininogen by proteolytic enzymes known as kininogenases, the main kininogenases being plasma and tissue (glandular) kallikrein (hereafter referred to as kallikrein). Kinins are rapidly hydrolyzed by a group of peptidases known as kininases (Figure 1). In the blood, kinins circulate in the low picogram range (2–20 pg), a concentration 100 times lower than that needed to decrease blood pressure (2). Thus, if kinins participate in the regulation of blood flow, blood pressure, and renal function, they must act as autocrine hormones (at the site of release) or paracrine hormones (near the site of release) (3).
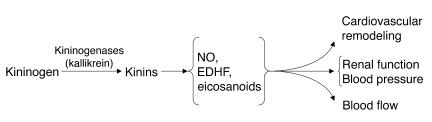
Figure 1.
Mechanism of kinin generation and effect of kinins via various intermediaries (NO, endothelium-derived hyperpolarizing factor [EDHF], and cyclooxygenase- and cytochrome P450–derived eicosanoids).
Kallikrein mRNA and protein are present in blood vessels, which indicates that kallikrein is synthesized in vascular tissue (4–6). Kallikrein is released from isolated arteries and into the perfusate of isolated rat hindquarters and kidneys (7–9). While the factors that control vascular kallikrein expression have not been studied in detail, arterial kallikrein is decreased in Goldblatt renovascular hypertensive rats (10). Conversely, in the acute phase of experimental mineralocorticoid/salt hypertension (2 weeks after administration of mineralocorticoid/salt is begun), arterial tissue kallikrein concentration and release are both increased. However, in the chronic phase (4–6 weeks) arterial kallikrein is decreased, while in the veins, tissue kallikrein is increased in both the acute and chronic phase (9). In humans and rats with mineralocorticoid/salt hypertension, renal kallikrein excretion is increased, while in essential hypertension and other types of hypertension, it is decreased (11). Thus expression of kallikrein in the vascular tissue may not necessarily parallel urinary kallikrein excretion.
Kallikrein-kinin system, vascular remodeling, and disease
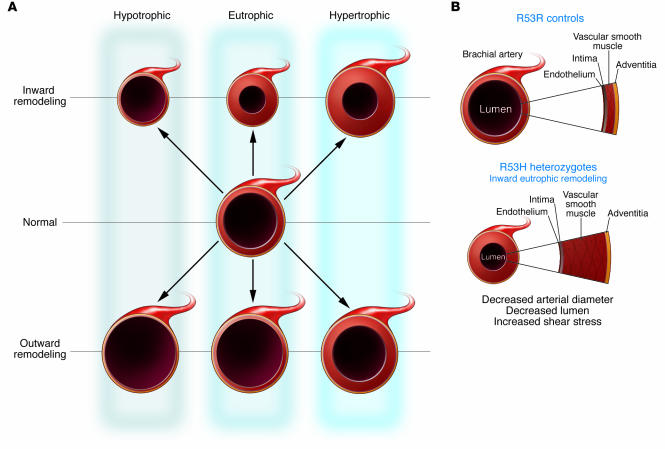
In this issue of the JCI, Azizi et al. (12) report that subjects with a polymorphism of the human kallikrein gene KLK (R53H) have lower urinary kallikrein excretion compared with that of control subjects (R53R). As a consequence of this polymorphism, the kallikrein expressed has decreased enzymatic activity. Thus, in affected subjects, kallikrein activity should also be decreased in the arterial wall and other tissues, since the polymorphism alters enzymatic activity, not kallikrein expression. In individuals carrying the polymorphism, compared with control subjects, there is a decrease in the internal diameter of the brachial artery but no change in cross-sectional area, a process referred to as eutrophic inward remodeling (Figure 2) (for review, see Mulvany et al.; ref. 13). In these subjects, the arterial wall did not adapt to a chronic increase in shear stress. Azizi et al. indicate that 5–7% of normotensive Caucasian subjects will have the R53H polymorphism and consequently will exhibit eutrophic inward remodeling of the brachial artery. Despite remodeling of the arterial wall and decreased urinary kallikrein enzymatic activity, the subjects had normal blood pressure; however, one of the criteria for inclusion in this study was normotension. Moreover, all of the subjects were young (18–35 years). As individuals with the polymorphism — both the heterozygous (R53H) and the rare homozygous (H53H) form — grow older, it will be extremely interesting to observe whether they develop hypertension or other vascular diseases.
Figure 2.
Arterial remodeling. (A) Diagram showing the manner in which remodeling can modify the cross-sectional area of arteries. The vessel in the center represents a normal artery. Remodeling can be hypotrophic, represented by reduced cross-sectional area of the vessel wall (left); eutrophic, with no change in cross-sectional area (center); or hypertrophic, characterized by increased cross-sectional area (right). These forms of remodeling can be inward, showing decreased lumen diameter (top); or outward, with increased lumen diameter (bottom). Modified with permission from Hypertension (13). (B) Diagram of a normal arterial wall (left) and an arterial wall with eutrophic inward remodeling, showing the decrease in both lumen and external diameter of the artery with normal wall area (right).
The authors recognize that the changes they observed in vascular remodeling could be caused by variations in another gene located at the same site as KLK, and this possibility cannot be ruled out. However, the assumption that the kallikrein-kinin system may play an important role in vascular remodeling and development of vascular disease is also supported by a recent report indicating that kininogen deficiency is associated with aortic aneurysm formation (14). Both kininogen-deficient Brown Norway Katholiek rats (which have a spontaneous mutation in the kininogen gene) and normal Brown Norway rats (which have normal kininogen) are susceptible to development of lesions in the internal elastic lamina of the aorta; however, in that study, a higher proportion of kininogen-deficient rats (50%) developed aneurysms than those with normal kininogen (32%). The aneurysms were associated with enhanced elastolysis, FasL- and caspase-3–mediated apoptosis, induction of MMP-2 and MMP-3 proteolytic cascades, and downregulation of tissue inhibitor of matrix metalloproteinase-4 protein (TIMP-4). Kininogen deficiency was also associated with changes in plasma concentrations of various cytokines. We have reported (15, 16) that carotid neointima formation after endothelial injury was prevented by an angiotensin-converting enzyme or kininase II inhibitor and this effect was mediated by kinins and NO. Furthermore, inactivation of the tissue kallikrein gene in mice induced endothelial dysfunction but not arterial remodeling. However, in these mice, the septum and posterior wall are thinned and left ventricular mass is reduced, while the heart tends to dilate (17–19). Collectively, these studies suggest that the cardiovascular kallikrein-kinin system may play a role in arterial and cardiac remodeling and pathology. However, it is very intriguing that these forms of vascular remodeling have a different pathogenesis: (a) eutrophic inward remodeling of the brachial artery, which may be due to restructuring of vascular smooth muscle cells around a smaller lumen as a result of chronic vasoconstriction (20); (b) aortic aneurysms, which may be due to enhanced elastolysis and apoptosis; and (c) neointima formation, which may be due to myofibroblast and vascular smooth muscle cell proliferation and migration to the neointima. Thus, further studies are needed to understand the mechanism by which changes in vascular kallikrein-kinin system activity cause a heterogeneous alteration in the arterial wall and establish whether these changes lead to vascular diseases and hypertension.
Role of the kallikrein-kinin system in sodium and water excretion
Azizi et al. (12) also conclude that despite a 50% deficiency in urinary kallikrein activity in R53H-heterozygous individuals compared with control individuals (R53R), the kidney adapts to large variations in sodium and potassium intake. Although the subjects reach a sodium balance 7 days after being placed on either a low-sodium/high-potassium or high-sodium/low-potassium diet, this is not a very sensitive indicator of whether or not the renal kallikrein-kinin system plays an important role in the regulation of sodium and water excretion. We and others have produced evidence that the renal kallikrein-kinin system contributes to both acute and chronic regulation of water and sodium excretion as well as regulation of renal vascular resistance and medullary blood flow (21–23). For example, mice lacking kinin B2 receptors develop hypertension and increased renal vascular resistance after at least 6 weeks of a very high-sodium diet (3.15% Na+ in food plus 1% saline in drinking water) (24). It is beyond the scope of this commentary to discuss the possible role of the renal kallikrein-kinin system in the regulation of renal function (for a review, see ref. 1).
In conclusion, the interesting studies by Azizi et al. (12), reporting remodeling of the brachial artery in human subjects with a polymorphism of the kallikrein gene; Unger’s group (14), reporting increased aneurysm formation in rats deficient in kininogen; and Meneton et al. (17), reporting decreased flow-induced dilatation in kallikrein gene–deficient mice, as well as previous publications regarding vascular kallikrein alterations in hypertension (9, 10), raise the possibility that the genetic association between the genotype R53H and inward remodeling of the brachial artery is causally linked to kallikrein deficiency. These findings also raise the possibility that alterations of the arterial kallikrein-kinin system may play an important role in the pathogenesis of vascular diseases.
Footnotes
See the related article beginning on page 780.
Conflict of interest: The author has declared that no conflict of interest exists.
References
- 1.Carretero, O.A., Yang, X.-P., and Rhaleb, N.-E. 2005. The kallikrein-kinin system as a regulator of cardiovascular and renal function. In Hypertension: a companion to Brenner and Rector’s The kidney. S. Oparil and M. Weber, editors. Elsevier. Philadelphia, Pennsylvania, USA. 203–218.
- 2.Salgado MCO, Rabito SF, Carretero OA. Blood kinin in one-kidney, one clip hypertensive rats. Hypertension. 1986;8(Suppl. I):I110–I113. [Google Scholar]
- 3.Carretero OA, Scicli AG. Kinins paracrine hormone. Kidney Int. 1988;34(Suppl. 26):S52–S59. [PubMed] [Google Scholar]
- 4.Nolly H, Scicli AG, Scicli G, Carretero OA. Characterization of a kininogenase from rat vascular tissue resembling tissue kallikrein. Circ. Res. 1985;56:816–821. doi: 10.1161/01.res.56.6.816. [DOI] [PubMed] [Google Scholar]
- 5.Nolly H, et al. Kininogenase from rat vascular tissue. Adv. Exp. Med. Biol. 1986;198A:11–17. doi: 10.1007/978-1-4684-5143-6_2. [DOI] [PubMed] [Google Scholar]
- 6.Saed GM, Carretero OA, MacDonald RJ, Scicli AG. Kallikrein messenger RNA in rat arteries and veins. Circ. Res. 1990;67:510–516. doi: 10.1161/01.res.67.2.510. [DOI] [PubMed] [Google Scholar]
- 7.Nolly H, Carretero OA, Scicli AG. Kallikrein release by vascular tissue. Am. J. Physiol. 1993;265:H1209–H1214. doi: 10.1152/ajpheart.1993.265.4.H1209. [DOI] [PubMed] [Google Scholar]
- 8.Vio CP, et al. Renal kallikrein in venous effluent of filtering and non-filtering isolated kidneys. Adv. Exp. Med. Biol. 1983;156B:897–905. [PubMed] [Google Scholar]
- 9.Nolly H, Carretero OA, Lama MC, Miatello R, Scicli AG. Vascular kallikrein in deoxycorticosterone acetate-salt hypertensive rats. Hypertension. 1994;23(Suppl. I):I185–I188. doi: 10.1161/01.hyp.23.1_suppl.i185. [DOI] [PubMed] [Google Scholar]
- 10.Nolly H, Carretero OA, Scicli G, Madeddu P, Scicli AG. A kallikrein-like enzyme in blood vessels of one-kidney, one-clip hypertensive rats. Hypertension. 1990;16:436–440. doi: 10.1161/01.hyp.16.4.436. [DOI] [PubMed] [Google Scholar]
- 11.Carretero, O.A., and Scicli, A.G. 1995. The kallikrein-kinin system as a regulator of cardiovascular and renal function. In Hypertension: physiology, diagnosis, and management. J.H. Laragh and B.M. Brenner, editors. Raven Press. New York, New York, USA. 983–999.
- 12.Azizi M, et al. Arterial and renal consequences of partial genetic deficiency in tissue kallikrein activity in humans. J. Clin. Invest. 2005;115:780–787. doi:10.1172/JCI200523669. doi: 10.1172/JCI23669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mulvany MJ, et al. Vascular remodeling. Hypertension. 1996;28:505–506. [PubMed] [Google Scholar]
- 14.Kaschina E, et al. Genetic kininogen deficiency contributes to aortic aneurysm formation but not to atherosclerosis. Physiol. Genomics. 2004;19:41–49. doi: 10.1152/physiolgenomics.00035.2004. [DOI] [PubMed] [Google Scholar]
- 15.Farhy RD, Carretero OA, Ho K-L, Scicli AG. Role of kinins and nitric oxide in the effects of angiotensin converting enzyme inhibitors on neointima formation. Circ. Res. 1993;72:1202–1210. doi: 10.1161/01.res.72.6.1202. [DOI] [PubMed] [Google Scholar]
- 16.Ellenby MI, Ernst CB, Carretero OA, Scicli AG. Role of nitric oxide in the effect of blood flow on neointima formation. J. Vasc. Surg. 1996;23:314–322. doi: 10.1016/s0741-5214(96)70276-8. [DOI] [PubMed] [Google Scholar]
- 17.Meneton P, et al. Cardiovascular abnormalities with normal blood pressure in tissue kallikrein-deficient mice. Proc. Natl. Acad. Sci. U. S. A. 2001;98:2634–2639. doi: 10.1073/pnas.051619598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bergaya S, et al. Decreased flow-dependent dilation in carotid arteries of tissue kallikrein-knockout mice. Circ. Res. 2001;88:593–599. doi: 10.1161/01.res.88.6.593. [DOI] [PubMed] [Google Scholar]
- 19.Bergaya S, Matrougui K, Meneton P, Henrion D, Boulanger CM. Role of tissue kallikrein in response to flow in mouse resistance arteries. J. Hypertens. 2004;22:745–750. doi: 10.1097/00004872-200404000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Bakker ENTP, et al. Inward remodeling follows chronic vasoconstriction in isolated resistance arteries. J. Vasc. Res. 2002;39:12–20. doi: 10.1159/000048989. [DOI] [PubMed] [Google Scholar]
- 21.Tomiyama H, Scicli AG, Scicli GM, Carretero OA. Renal effects of Fab fragments of kinin antibodies on deoxycorticosterone acetate-salt-treated rats. Hypertension. 1990;15:761–766. doi: 10.1161/01.hyp.15.6.761. [DOI] [PubMed] [Google Scholar]
- 22.Fenoy FJ, Scicli AG, Carretero O, Roman RJ. Effect of an angiotensin II and a kinin receptor antagonist on the renal hemodynamic response to captopril. Hypertension. 1991;17:1038–1044. doi: 10.1161/01.hyp.17.6.1038. [DOI] [PubMed] [Google Scholar]
- 23.Saitoh S, Scicli AG, Peterson E, Carretero OA. Effect of inhibiting renal kallikrein on prostaglandin E2, water, and sodium excretion. Hypertension. 1995;25:1008–1013. doi: 10.1161/01.hyp.25.5.1008. [DOI] [PubMed] [Google Scholar]
- 24.Alfie ME, Sigmon DH, Pomposiello SI, Carretero OA. Effect of high salt intake in mutant mice lacking bradykinin-B2receptors. Hypertension. 1997;29:483–487. doi: 10.1161/01.hyp.29.1.483. [DOI] [PubMed] [Google Scholar]