Abstract
This study evaluates whether implementation of a content expert–developed clinical documentation tool can be beneficial to workflow by reducing time from patient arrival to encounter closure among pediatric patients receiving intestinal rehabilitation.
Intestinal failure is a complex, rare, morbid, and costly disorder occurring when gut function is insufficient to meet the growing body’s needs.1 Patients with a history of intestinal failure are often managed by a multidisciplinary, interprofessional intestinal rehabilitation team. Children with rare or medically complex conditions, such as intestinal failure, find themselves in an advanced health care system that has insufficient means of developing and providing evidence-based care.2,3 Learning health systems, which analyze routinely collected clinical data to generate new evidence and improve quality of care, do not simply appear with electronic health record adoption but require innovative methods for structured capture of clinical data.4 We have previously suggested content expert–developed tools for clinical documentation could capture data discretely, generating granular digital phenotypes and enabling health care professionals to learn from each clinical encounter.5 We hypothesized that such tools will be most effective if use is not mandated or burdensome, as their engaged use is the engine of a learning health system. In this study, we aimed to investigate whether implementation of a content expert–developed clinical documentation tool can be beneficial to workflow by reducing time from patient arrival to encounter closure among pediatric patients receiving intestinal rehabilitation.
Methods
This single-institution quality improvement project was conducted from January 2017 to March 2023. Interventions involved modifications to the clinic note template (intervention 1; implemented May 2019) and development and testing of a custom-built documentation toolset. The toolset was built from a list of approximately 1000 data elements by an intestinal rehabilitation professional with input from colleagues at 3 other centers. Tools were made available in the local electronic health record (intervention 2; implemented May 2021), and patient notes were transitioned from free text over subsequent months. Clinicians were informally trained, and support was provided by the builder. Tools were updated for formatting and grammar (intervention 3; implemented November 2021). The balancing measure was characters per note, as there was concern that planned interventions may add characters without content. X-bar process control charts were used to examine process stability and assess improvement of continuous variables. These charts displayed the mean encounter value per month. Commonly accepted rules for shifting the process stage mean were applied using the Healthcare–IHI rules of the QI Macros Process Change Wizard version 2020.10 (KnowWhere International). The Nationwide Children’s Hospital Institutional Review Board reviewed this study, and approval was not required as this was not human subjects research. This study was reported under the Standards for Quality Improvement Reporting Excellence (SQUIRE) 2.0 reporting guideline.
Results
During the study period, 272 patients were seen by 9 health care professionals across 4809 ambulatory encounters. A total of 120 patients (44.1%) were female, and the median (range) age at study conclusion was 10.5 (0.8-37.2) years. A total of 249 patients (91.5%) were diagnosed with short-bowel syndrome. The median (range) visits per patient was 11 (1-105). Mean time from arrival to encounter closure fell from 31 to 25 hours following availability of previsit medical record recording, then to 14 hours with toolset use (Figure 1). After toolset implementation, the process stage mean decreased from 14 787 characters to 9723 characters (Figure 2), and a median (range) of 152 (0-281) disease-specific data elements were captured per visit.
Figure 1. X-Bar Statistical Process Control Chart of Mean Monthly Time From Patient Arrival to Encounter Closure in an Intestinal Rehabilitation Clinic Over a 63-Month Period.
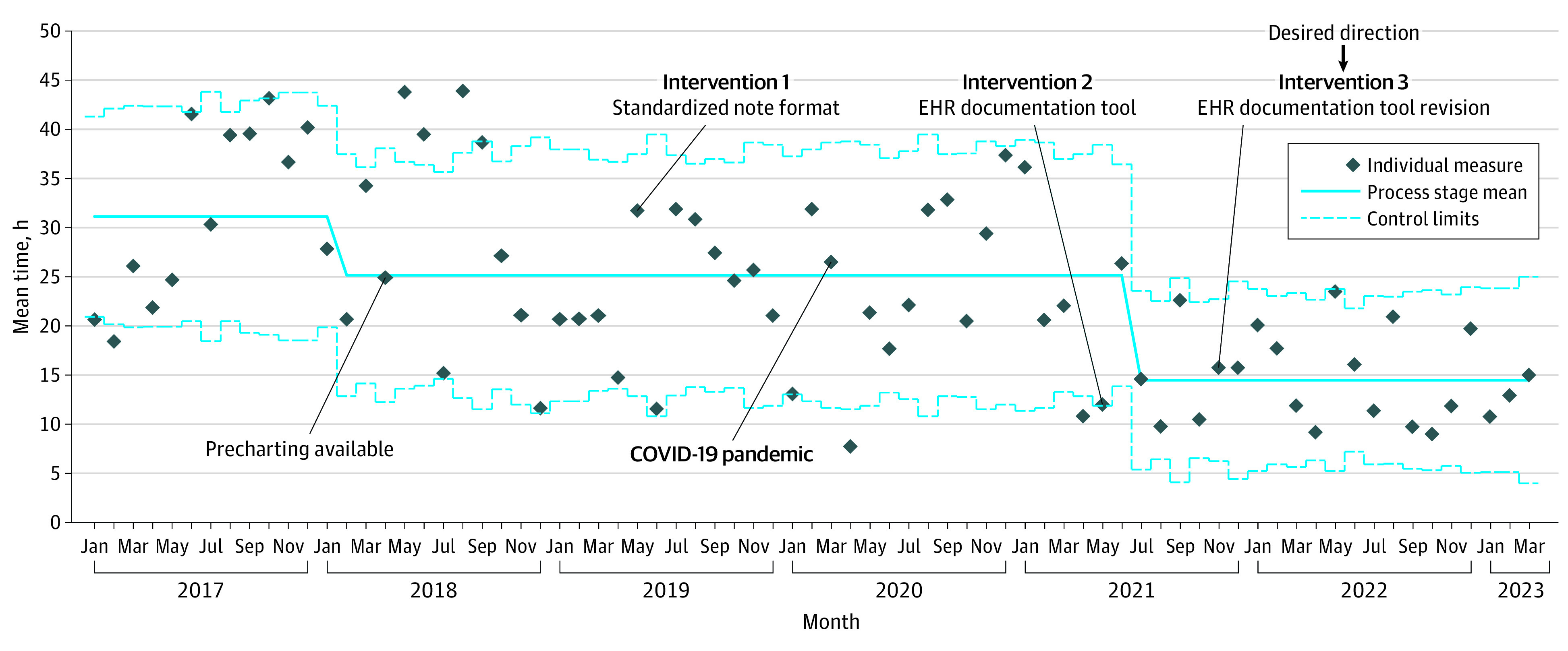
EHR indicates electronic health record.
Figure 2. X-Bar Statistical Process Control Chart of Mean Monthly Characters per Note in an Intestinal Rehabilitation Clinic Over a 63-Month Period.
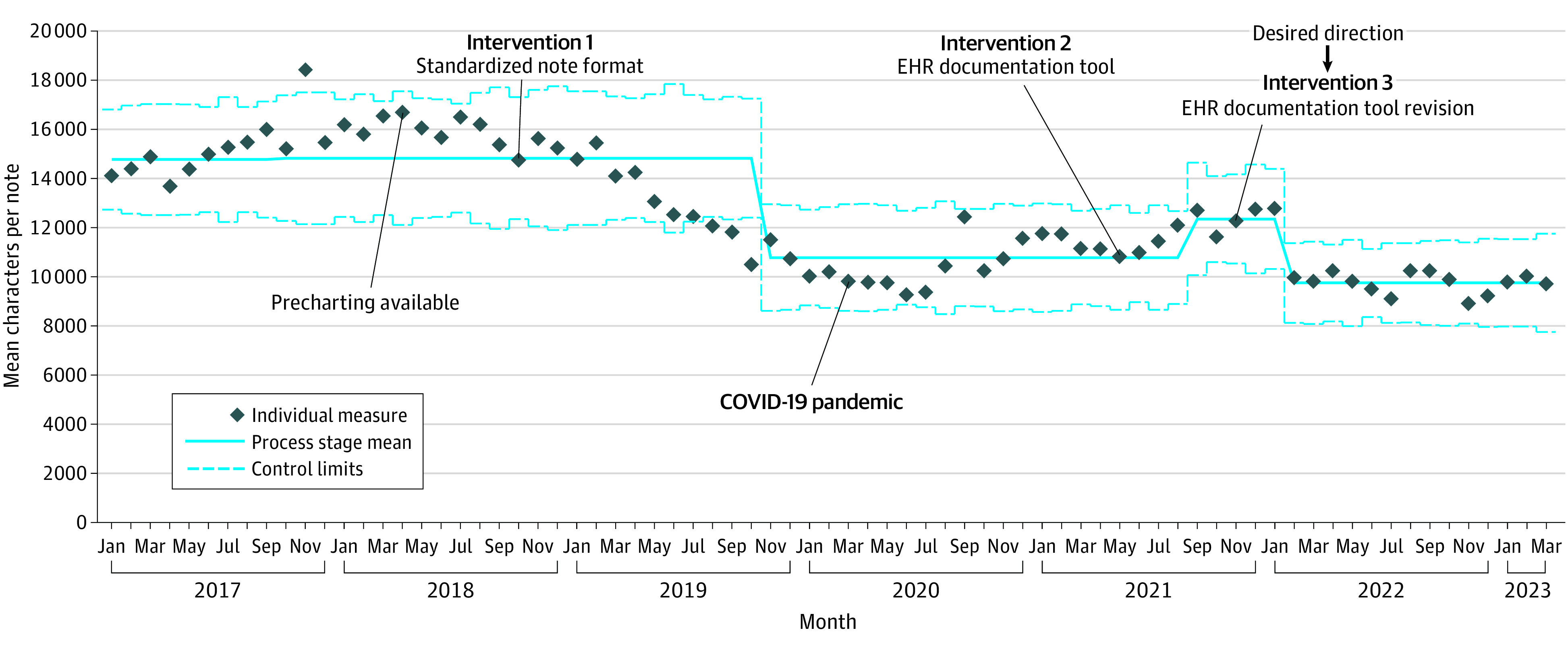
EHR indicates electronic health record.
Discussion
In this study, a disease-specific documentation toolset built by content experts improved time to encounter closure while collecting more than 150 disease-specific data points per encounter. Portability and interoperability of this toolset may permit creation of a multisite digital platform that can facilitate a comprehensive description of natural disease history, clinical improvement efforts, and comparative effectiveness studies. This work can serve as a model for creating complex disease-specific tools for data acquisition to learn from each clinical encounter. A limitation to the study was use of time to encounter closure instead of time spent in note. Broader limitations include data quality in the absence of required fields and ability to generalize efficiency gains to intestinal rehabilitation programs not participating in tool development.
Data Sharing Statement
References
- 1.Flahive CB, Goldschmidt M, Mezoff EA. A review of short bowel syndrome including current and emerging management strategies. Curr Treat Options Pediatr. 2021;7:1-16. doi: 10.1007/s40746-020-00218-z [DOI] [Google Scholar]
- 2.Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357(15):1515-1523. doi: 10.1056/NEJMsa064637 [DOI] [PubMed] [Google Scholar]
- 3.Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529-538. doi: 10.1542/peds.2010-0910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Capurro D, Yetisgen M, van Eaton E, Black R, Tarczy-Hornoch P. Availability of structured and unstructured clinical data for comparative effectiveness research and quality improvement: a multisite assessment. EGEMS (Wash DC). 2014;2(1):1079. doi: 10.13063/2327-9214.1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mezoff EA, Minneci PC, Hoyt RR, Hoffman JM. Toward an electronic health record leveraged to learn from every complex patient encounter: health informatics considerations with pediatric intestinal rehabilitation as a model. J Pediatr. 2019;215:257-263. doi: 10.1016/j.jpeds.2019.07.047 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement


