Abstract
The usage of silicon oil (SO) in vitreoretinal surgery is associated with potential complications. One such complication is the extravasation of SO into the subconjunctival space through open sclerotomies. Subconjunctival SO (SCSO) can cause irregularities in the ocular surface which predisposes to complications like corneal dellen. This corneal dellen can get infected in rare situations. SCSO needs to be removed to stabilize the ocular surface. We present a case of corneal dellen with infiltration which developed as a consequence of SCSO and its management.
Keywords: Corneal dellen, corneal infiltration, ocular surface, silicon oil tamponade, subconjunctival silicon oil
Introduction
Corneal dellen, first described by Ernst Fuchs are shallow, saucer-like excavations, usually of the peripheral cornea with intact overlying epithelium with no epithelial staining and no infiltration (1). They occur secondary to paralimbal elevations like filtering blebs, (2) after strabismus and scleral buckle surgery, (1,3) and have also been reported to occur after silicon oil (SO) leak from the vitreous cavity to the subconjunctival space (4). Subconjunctival SO (SCSO) following micro incisional vitreoretinal surgery (MIVS) is a known but rare complication (5). Despite better wound construction, extravasation of SO into the subconjunctival space can still occur through open sclerotomies (6). We describe a case of dellen with secondary infiltration following SCSO and its management.
Case Report
A 52-year-old male presented with complaints of redness, pain, photophobia, and blurring of vision in the right eye (OD) for 3 days. He had undergone uneventful manual small incision cataract surgery with posterior chamber intraocular lens (PCIOL) 6 months back in OD with good post-operative gain in vision. However, 3 months post cataract surgery he developed retinal detachment in OD for which he underwent pars plana vitrectomy (PPV) with a 23-gauge sutureless vitrectomy system, endophotocoagulation and intraocular 1000 centistokes silicone oil tamponade. One month later, the patient underwent re-surgery under SO for recurrent retinal detachment using a 23-gauge vitrectomy system. At present, his best corrected visual acuity was 0.02 in both eyes (OS). Slit lamp examination of OS showed a dense cataract and the fundus showed an epiretinal membrane at the macula. Slit lamp examination of OD showed conjunctival hyperemia with SO migration under the temporal conjunctiva forming multiple subconjunctival cysts (Fig. 1a). The temporal cornea at 9 o’clock position showed the presence of a 6×3 mm dellen associated with an infiltrate (Fig. 1b). The anterior chamber was quiet with PCIOL in situ. Intraocular pressure on Goldmann applanation tonometer was 14 mmHg in OS and was deferred in OD due to active infiltrate. Ocular tension was digitally normal. Fundus examination of OD showed that the retina was attached and well-lasered with SO in situ. Anterior segment optical coherence tomography showed the corneal dellen and multiple SCSO bubbles as well as subscleral SO bubble (Fig. 2). Surgical intervention to remove the SCSO in OD was deferred at this visit in view of active infective infiltrate and the patient was started on hourly topical antibiotic levofloxacin 1.5% eye drops, gatifloxacin 0.3% eye ointment and bedtime and frequent topical lubricants. He was placed under close observation and the infiltrate showed a reduction in size at 3 days follow-up and the patient was symptomatically better. One week later after the infiltrate had resolved, surgical intervention was planned for improving the ocular surface. Subconjunctival dissection of SCSO was performed and cyanoacrylate glue was applied at the site of the dellen with a bandage contact lens (BCL) to strengthen the thinned cornea and avoid perforation (Fig. 3). The patient was symptomatically better, and ocular findings were stable at the last follow-up, 2 months after the procedure.
Figure 1.
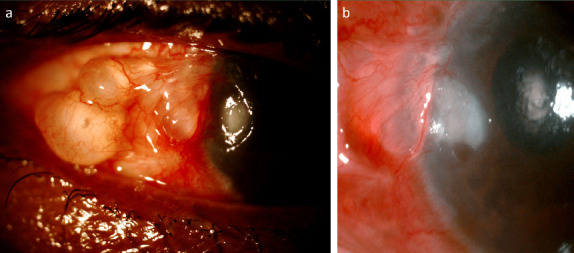
(a) Slit lamp image of the right eye showing multiple subconjunctival silicon oils along with a dellen at the temporal aspect of the cornea. (b) Slit lamp image of the right eye showing the dellen along with infiltration.
Figure 2.

Anterior segment OCT of the right eye showing the dellen and subconjunctival silicon oil and subscleral silicon oil bubble.
Figure 3.
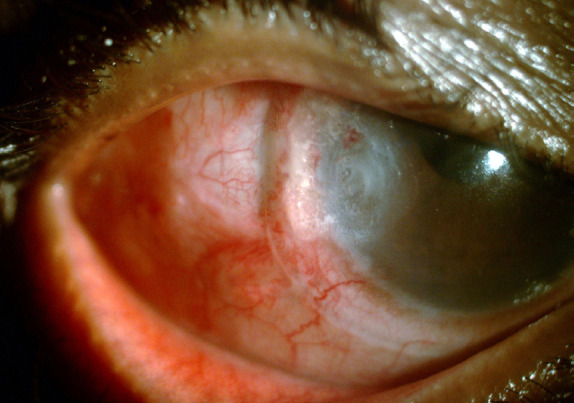
Slit lamp image of the right eye after removal of subconjunctival silicon oil showing bandage contact lens and glue in situ.
Discussion
SO is a common intraocular tamponade used in vitreoretinal surgery (6). MIVS has incisions that are smaller (0.51 mm for 25 G and 0.64 mm for 23 G), cause less disruption of conjunctiva and sclera, are self-sealing, and ideally do not require any suturing (7). Despite the better wound construction, extravasation of silicone oil into the SC space through open sclerotomies post-sutureless vitrectomies is a potential complication (6). Potential corneal complications secondary to intraocular SO tamponade are corneal edema, corneal opacity, band-shaped keratopathy, and the possible need for a corneal transplant. Dellen is the corneal complication of extraocular SO extravasation. Multiple studies have reported extraocular extravasation of SO like a migration of SO into the eyelid causing mechanical blepharoptosis, (8) optic chiasm and cerebral migration, (9) migration in the SC space through Molteno implant (10) or Ahmed glaucoma valve, (11) and formation of subconjunctival cysts (12). Egress of SO from the vitreous cavity to the subconjunctival space has been reported in 9.7% of cases treated with PPV and SO injection, which warranted second surgery to remove SO from the SC space (13). Formation of dellen secondary to SCSO is due to the elevation of the conjunctiva leading to an irregular ocular surface. Mahgoub et al. reported 20 eyes with SCSO following MIV, of which ten eyes had dellen formation also. They identified that the proximity of SCSO to the limbus is a risk factor for developing dellen, that is, the closer to the SCSO is to the limbus, the greater chance of developing dellen. None of the dellen had associated infiltration, which was seen in our case. All the dellen were noted to heal with scar formation after SCSO removal was done during the time of SO removal from the vitreous cavity (5). Hyung and Min also reported dellen’s disappearance after the removal of SCSO (10). Dellen can get secondarily infected leading to sight-threatening complications such as perforation and endophthalmitis (2,14). Dellen should be recognized and managed to avoid these complications. It is important to rapidly reestablish the mucin layer with copious lubricants, and patching of the eye which helps in faster healing and usage of large-diameter BCLs (15). Since dellen secondary to SCSO may be resistant to topical treatment, early SCSO evacuation will prevent disruption of the ocular surface tear film leading to major complications (5).
In conclusion, SO extravasation should be avoided by ensuring a tight sclerotomy at the end of MIV. In our case, the patient presented with a dellen with infiltrate which fortunately resolved on medical management.
Conclusion
Patients undergoing SO tamponade should be followed up for not only retinal status but also for early identification of SO associated complications and their appropriate management.
Footnotes
Disclosures
Informed consent: Written informed consent was obtained from the patient for the publication of the case report and the accompanying images.
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship Contributions: Concept – S.M.; Design – G.N.; Supervision – Sa.M.; Resource — S.M.; Materials – S.M.; Data collection and/or processing – G.N.; Analysis and/or interpretation –Sa.M.; Literature search – Sa.M., G.N.; Writing – G.N., Sa.M.; Critical review – Sa.M., S.M.
References
- 1.Tessler HH, Urist MJ. Corneal dellen in the limbal approach to rectus muscle surgery. Br J Ophthalmol. 1975;59:377–9. doi: 10.1136/bjo.59.7.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Narita A, Seguchi J, Shiraga F. Paecilomyces lilacinus-induced scleritis following bleb-associated endophthalmitis after trabeculectomy. Acta Med Okayama. 2015;69:313–8. doi: 10.18926/AMO/53678. [DOI] [PubMed] [Google Scholar]
- 3.Biedner BZ, Rothkoff L, Friedman L, Geltman C. Colchicine suppression of corneal healing after strabismus surgery. Br J Ophthalmol. 1977;61:496–7. doi: 10.1136/bjo.61.7.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Federman JL, Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology. 1988;95:870–6. doi: 10.1016/s0161-6420(88)33080-0. [DOI] [PubMed] [Google Scholar]
- 5.Mahgoub MM, Roshdy MM, Wahba SS. Dellen formation as a complication of subconjunctival silicone oil following microincision vitrectomy. Clin Ophthalmol. 2017;11:2215–9. doi: 10.2147/OPTH.S149531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byeon SH, Chu YK, Lee SC, Koh HJ, Kim SS, Kwon OW. Problems associated with the 25-gauge transconjunctival sutureless vitrectomy system during and after surgery. Ophthalmologica. 2006;220:259–65. doi: 10.1159/000093081. [DOI] [PubMed] [Google Scholar]
- 7.Warrier SK, Jain R, Gilhotra JS, Newland HS. Sutureless vitrectomy. Indian J Ophthalmol. 2008;56:453–8. doi: 10.4103/0301-4738.43364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mustafa TA, Al-Zuoby KM, Alawneh AM. Mechanical blepharoptosis and eyelid swelling caused by silicone oil. J Optom. 2009;2:27–8. [Google Scholar]
- 9.Kiilgaard JF, Milea D, Løgager V, la Cour M. Cerebral migration of intraocular silicone oil:An MRI study. Acta Ophthalmol. 2011;89:522–5. doi: 10.1111/j.1755-3768.2009.01793.x. [DOI] [PubMed] [Google Scholar]
- 10.Hyung SM, Min JP. Subconjunctival silicone oil drainage through the Molteno implant. Korean J Ophthalmol. 1998;12:73–5. doi: 10.3341/kjo.1998.12.1.73. [DOI] [PubMed] [Google Scholar]
- 11.Nazemi PP, Chong LP, Varma R, Burnstine MA. Migration of intraocular silicone oil into the subconjunctival space and orbit through an Ahmed glaucoma valve. Am J Ophthalmol. 2001;132:929–31. doi: 10.1016/s0002-9394(01)01144-8. [DOI] [PubMed] [Google Scholar]
- 12.Biswas J, Bhende PS, Gopal L, Parikh S, Badrinath SS. Subconjunctival cysts following silicone oil injection:A clinicopathological study of five cases. Indian J Ophthalmol. 1999;47:177–80. [PubMed] [Google Scholar]
- 13.Siqueira RC, Gil AD, Jorge R. Retinal detachment surgery with silicone oil injection in transconjunctival sutureless 23-gauge vitrectomy. Arq Bras Oftalmol. 2007;70:905–9. doi: 10.1590/s0004-27492007000600004. [DOI] [PubMed] [Google Scholar]
- 14.González Gomez A, González de Gor Crooke JL, García-Ben A, García-Campos JM. Dellen and corneal perforation after bilateral pterygium excision in a patient with no risk factors. BMJ Case Rep. 2015;2015:bcr2015213319. doi: 10.1136/bcr-2015-213319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kymionis GD, Plaka A, Kontadakis GA, Astyrakakis N. Treatment of corneal dellen with a large diameter soft contact lens. Cont Lens Anterior Eye. 2011;34:290–2. doi: 10.1016/j.clae.2011.07.002. [DOI] [PubMed] [Google Scholar]


