Abstract
Artificial intelligence and machine learning are driving a paradigm shift in medicine, promising data-driven, personalized solutions for managing diabetes and the excess cardiovascular risk it poses. In this comprehensive review of machine learning applications in the care of patients with diabetes at increased cardiovascular risk, we offer a broad overview of various data-driven methods and how they may be leveraged in developing predictive models for personalized care. We review existing as well as expected artificial intelligence solutions in the context of diagnosis, prognostication, phenotyping, and treatment of diabetes and its cardiovascular complications. In addition to discussing the key properties of such models that enable their successful application in complex risk prediction, we define challenges that arise from their misuse and the role of methodological standards in overcoming these limitations. We also identify key issues in equity and bias mitigation in healthcare and discuss how the current regulatory framework should ensure the efficacy and safety of medical artificial intelligence products in transforming cardiovascular care and outcomes in diabetes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-023-01985-3.
Keywords: Machine learning, Artificial intelligence, Prediction, Personalized medicine, Digital health, Diabetes, Cardiovascular disease
Introduction
The rapid progress in artificial intelligence (AI) and machine learning (ML) has raised hopes for a more personalized, efficient, and effective approach to the management of diabetes mellitus and its cardiovascular sequelae [1, 2]. It is estimated that nearly 529 million people worldwide and 35 million Americans currently have diabetes, with cardiovascular disease (CVD) representing the leading cause of morbidity and mortality [3, 4]. Recognizing the need for improvement in the diagnosis, monitoring, and treatment of this growing patient population, AI and ML have already been applied to automate the screening of diabetes, detect macrovascular and microvascular complications [5–11], and enable multiomic phenotyping for personalized prevention and therapy recommendations [12, 13].
Unfortunately, most AI and ML-based tools fail to translate into improved outcomes for our patients and communities. This gap between evidence generation and clinical implementation is exemplified by the subpar real-world uptake of multiple therapies that reduce cardiovascular risk [14–17]. Furthermore, the current paradigm of medical AI heavily relies on existing data streams that reflect and thus perpetuate systemic biases. Acknowledging these limitations is necessary to prevent the misuse and overuse of AI and ML in medicine and further underscores the need for good research practices to ensure reproducibility [18] as well as guide the practical, ethical [19], and regulatory challenges that arise from the burgeoning use of these technologies [20, 21].
In this comprehensive review, we offer a broad overview of the various ML methods and how they may be leveraged in developing predictive models. This review focuses on these methods in the context of ML in the diagnosis, prognostication, phenotyping, and treatment of diabetes and its cardiovascular complications. In addition to discussing the properties of the models that enable their successful application in complex risk prediction, we define challenges that arise from the misuse of AI and ML, and the role of methodological standards in combating these challenges. We also identify key issues on equity and bias mitigation in healthcare and ways in which the regulatory framework can ensure the efficacy and safety of ML and AI in transforming cardiovascular care and outcomes in diabetes.
Developing and evaluating clinical machine learning models
An understanding of the principal tenets of model development and evaluation is essential for interpreting the evidence. These concepts are broad, applicable across a range of clinical conditions and ML tasks and represent the foundations of critical AI and ML appraisal.
Artificial intelligence (AI) and machine learning (ML)
Though AI and ML are inextricably linked, they are not identical terms [22, 23]. Artificial intelligence (AI) describes the ability of a machine to perform tasks that are typical of human intelligence, such as understanding natural language, problem-solving, or creative tasks like generating images and text. On the other hand, the process through which an AI system acquires this ability, learning and improving from experience and observed data to make predictions about new or unseen cases, is called machine learning (ML).
Model training
The specific step during which a model learns from data is also known as training, whereas the respective dataset is referred to as training set. Here, the model makes predictions and subsequently adjusts its parameters based on a metric that quantifies how good or bad the predictions are (loss function). It is typical that during training, the model will be applied to an unseen group of observations (validation set) to get a more reliable assessment on performance on unseen data. Further testing in external sets drawn from geographically and temporally distinct populations can serve to solidify claims about external model validity [24].
Supervised and unsupervised learning
The learning process can be supervised or unsupervised [22]. Supervised learning describes an iterative process that selects relevant input features and then assigns weights to link the input data to a given value (regression) or class (classification). Unsupervised learning, on the other hand, analyzes and clusters unlabeled datasets by identifying similarities and dissimilarities between data points, therefore uncovering hidden patterns in the data. These two approaches should be considered complementary and are often used in conjunction to address distinct problems. Supervised learning can be used to better predict future cardiovascular risk (regression), or the presence of diabetic retinopathy (classification), whereas unsupervised approaches can be used to identify distinct phenotypic clusters of patients with diabetes with differences in baseline risk, prognosis, and treatment response.
Building on these concepts, self-supervised learning (SSL) processes unlabeled data to create key representations that can facilitate downstream tasks [25]. In principle, SSL closely resembles unsupervised learning since it is applied to unlabeled data. However, instead of focusing on tasks like clustering, SSL attempts to solve tasks traditionally addressed through supervised learning, such as classification and regression [26]. We [27, 28], and others [29, 30], have shown that this is a powerful method to train clinical models, especially when there is a paucity of high-quality labels.
Machine learning algorithms
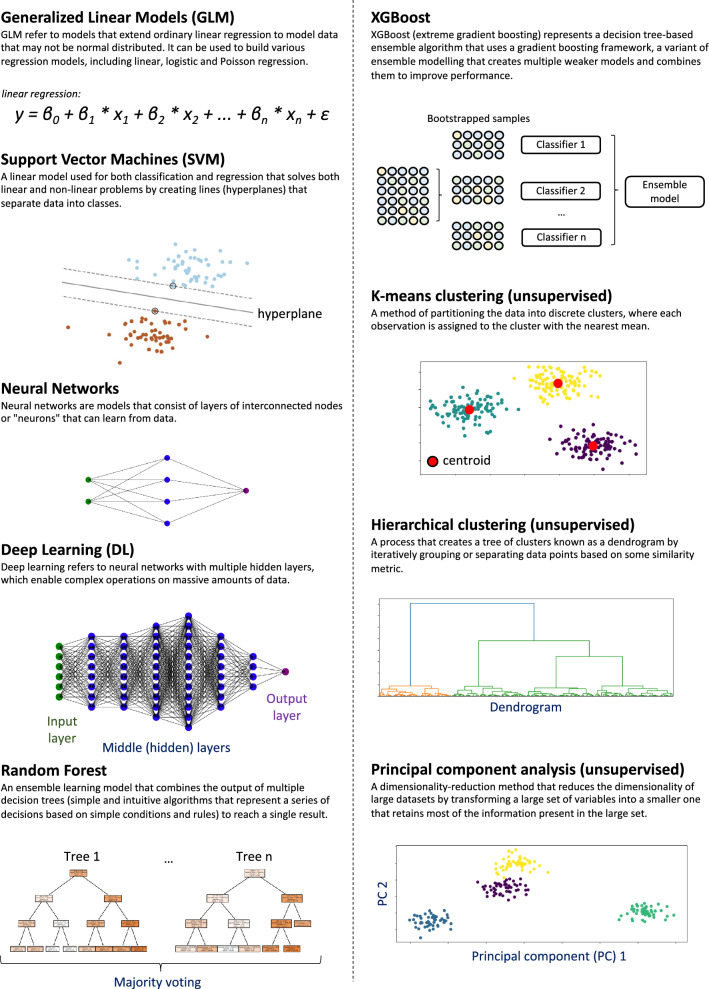
Whether supervised or unsupervised, the ML process requires a set of rules and statistical techniques that can learn meaningful patterns from data, known as algorithms. A representative list of ML algorithms used in medical applications is shown in Fig. 1. Ranging from linear regression to deep learning algorithms, these vary substantially in their ability to model complex data, interpretability, and performance [22]. Further, they can be adapted to model not only cross-sectional or short-term outcomes, as done with logistic regression, but also long-term predictions through survival analysis, similar to Cox regression modeling which has been widely used to estimate CVD risk in the US [31], UK [32], and Europe [33]. Some notable examples include (survival) random forests and deep learning algorithms, which have all been adapted to model long-term hazards [34–36].
Fig. 1.
Overview of commonly used algorithms in medical machine learning
Assessing model performance
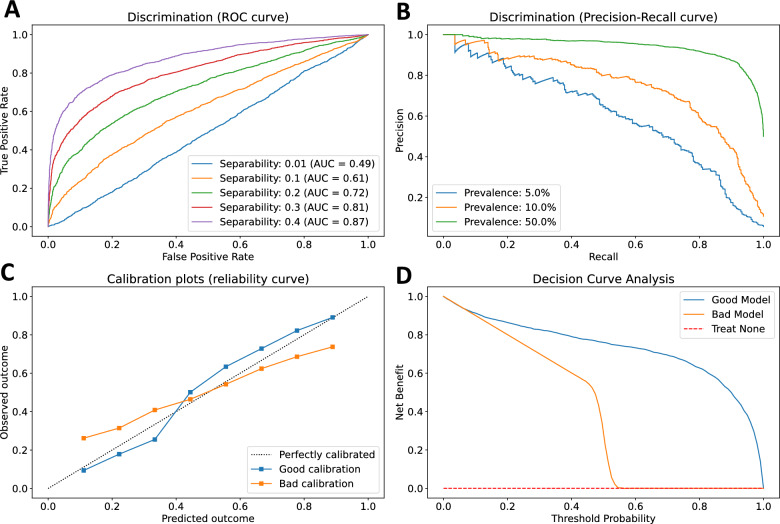
The comprehensive evaluation of the performance of a predictive ML model requires an integrated assessment of discrimination, calibration, and clinical benefit (Fig. 2; a detailed table of metrics used in classification and regression tasks, along with their strengths and weaknesses is also presented in Additional file 1: Table S1) [37]. Commonly used discrimination metrics, such as the Area Under the Receiver Operating Characteristic curve (AUROC) and the Area Under the Precision–Recall Curve (AUPRC) describe the model’s ranking of individual predictions and ability to discriminate between different classes. However, AUROC may not offer a complete description of the model’s performance, particularly in imbalanced datasets. For instance, a model with 95% sensitivity and specificity screening for a rare label (e.g., screening for type 1 diabetes mellitus in the community, prevalence ~ 0.55%), a positive prediction is more likely to be false positive than true positive. Calibration assesses the agreement between the predicted and observed outcomes across the entire range of predictions [38]. Two models may have a similar AUROC but may differ substantially in their calibration performance, a crucial difference that may often impact clinical decision-making if predictions consistently overestimate or underestimate risk. Guidelines on good research practices in prediction modeling suggest that for any given model both discrimination and calibration are reported [39]. Moreover, a complex model may have good discriminatory performance but lack incremental value beyond a simpler or established model, something that can be further evaluated by metrics such as the Net Reclassification Improvement (NRI) and Integrated Discrimination Improvement (IDI) [37]. Finally, good discrimination and calibration do not necessarily translate into net clinical benefit for a specific clinical application. In this setting, decision curve analysis (DCA) can be used to assess the net benefit of a model across a range of potential thresholds for action, weighing the benefit versus harm versus alternative risk stratification approaches [40].
Fig. 2.
Discrimination, calibration, and net clinical benefit. The comprehensive evaluation of a predictive model requires the simultaneous evaluation of its discrimination, calibration, and incremental value beyond the current standard-of-care. A The area under the receiver operating characteristic curve (AUROC) reflects the trade-off between sensitivity (true positive rate) and specificity (1-false positive rate) at different thresholds and provides a measure of separability, in other words the ability of the model to distinguish between classes (0.5 = no separation, 1 = perfect separation). B Models with similar AUROC may exhibit different behavior when the prevalence of the label varies. The precision–recall curve demonstrates the trade-off between the positive predictive value (precision) and sensitivity (recall), and illustrates how the area under the curve may vary substantially as the prevalence of the label of interest decreases from 50 to 5%. C Models with similar AUROC may also differ in their calibration. A model with good calibration (i.e. blue line) makes probabilistic predictions that match real world probabilities. On the other hand, the model shown in orange underestimates and overestimates risk at lower and higher prediction thresholds, respectively. D Finally, models should be compared against established standard-of-cares while incorporating clinical consequences and comparing the net clinical benefit across varying risk levels to established or no risk stratification approaches. Curves were generated using synthetic datasets for illustration purposes
Interpretability and explainability
Human end-users may feel reluctant to use what they cannot understand. Interpretability and explainability describe two closely linked yet slightly different concepts [41, 42]. Interpretability refers to the extent to which a human can understand how features are combined to make predictions. This is particularly desirable when training a model to understand its general behavior and identify potential sources of bias. Explainability is a property of ML models that describes the extent to which the inner workings of a model can be explained in human terms, that is, understanding why a model made a specific prediction (often on a case-by-case basis). This is important for the end-user and has practical and regulatory implications. A model can be interpretable without being explainable, and vice versa; however, ideally, a model should be both [43].
Data-driven advances in diabetes and cardiovascular disease
From continuous glucose monitoring devices to electronic health records (EHR), electrocardiograms (ECG), retinal images, and computed tomography images, the day-to-day monitoring, screening, and management of patients with diabetes have a constant stream of structured and unstructured data. The following section illustrates the breadth of tools that are being developed for use by individuals and their healthcare teams.
Targeted screening and risk stratification of prediabetes and diabetes
Both the American Diabetes Association (ADA) [44], and the United States Preventive Services Task Force (USPTF) [45] have emphasized the importance of early screening for pre-diabetes and diabetes among asymptomatic adults to ensure timely diagnosis and prevent downstream diabetes complications and its sequalae. Current guidelines recommend screening for pre-diabetes and type 2 diabetes with an informal assessment of risk factors or a validated risk calculator among all asymptomatic adults and testing among adults of any age who are overweight or obese and have one or more risk factors [44]. Several risk scores have been proposed for a more personalized risk assessment of type 2 diabetes, such as the American Diabetes Association questionnaire, a logistic regression model trained in National Health and Nutrition Examination Survey (NHANES), Atherosclerosis Risk in Communities (ARIC) and Cardiovascular Health Study (CHS) studies with a reported AUROC of 0.79 to 0.82 for undiagnosed diabetes among U.S. adults aged 20 years or older [46], the Australian type 2 diabetes risk Assessment Tool (AUSDRISK) to predict the incidence of type 2 diabetes over 5 years among participants 25 years or older (AUROC of 0.78) [47], and the Cambridge Risk score to detect cross-sectionally elevated HbA1c levels among individuals aged 45 years (AUROC of 0.84 for HbA1c 7% or greater) [48]. The moderate accuracy of these tools in addition to concerns about their external validity [49] has prompted researchers to explore whether targeted screening could be improved through ML of structured and unstructured data [5–11].
In NHANES, an XGBoost classifier based on 123 variables showed an AUROC of 0.86 in detecting the presence of an established diabetes diagnosis, though the performance dropped to 0.73 when detecting undiagnosed diabetes adjudicated based on abnormal laboratory findings [50]. In a retrospective analysis of 16 predictors from routine health check-up data of 277,651 participants from Japan, a light gradient boosting machine algorithm was able to predict the 3-year incidence of diabetes with an AUROC of 0.84, demonstrating significantly improved performance compared with a logistic regression model for large training populations of 10,000 patients or more [6]. Another ML algorithm built using EHR and administrative healthcare data from Canada reportedly identified type 1 diabetes cases with 87.2% sensitivity and 99.9% specificity [51].
Moving beyond EHR models relying on administrative datasets, an analysis of 1262 individuals from India showed that an XGBoost algorithm using ECG inputs had excellent performance (97.1% precision, 96.2% recall) and good calibration in detecting type 2 diabetes and pre-diabetes [7]. Furthermore, the integration of a genome-wide polygenic risk score and serum metabolite data with structured clinical parameters using a random forest model resulted in improved type 2 diabetes risk prediction in a Korean cohort of 1425 participants [8]. Several other studies have also defined metabolomic [52] and proteomic signatures for identifying diabetes or insulin resistance [9]. Integrative personal omics profiles (iPOP) that combine genomic, transcriptomic, proteomic, metabolomic, and autoantibody profiles from a single individual over several months can also be harnessed to connect genomic information with dynamic omics activity, describe host-microbiome interactions, and describe personal aging markers, thus risk stratifying various medical risks, including type 2 diabetes [53–57].
Finally, imaging-based biomarkers are also being studied, with the development of DL models that can automatically segment and output measurements of pancreatic attenuation, volume, fat content, fractal dimension, and parameters associated with visceral adiposity and muscle attenuation/volume. For instance, in a retrospective cohort of 8992 patients undergoing screening CT colonography, a DL model of the above phenotypes could predict the future incidence of diabetes with an AUROC of 0.81 to 0.85 [10].
Computable phenotypes of patients with diabetes
The traditional classification of diabetes into type 1 and type 2 does not fully capture the complex and highly heterogeneous nature of the condition. From the heterogeneity of the islet microenvironment to the diversity of pathophysiological endotypes that span multiple demographic groups, diabetes mellitus affects a diverse group of patients with distinct molecular underpinnings that require individualized approaches to therapy [58]. Multiomic signatures may provide insights into the interaction of a patient’s genome, phenome, and environment [53–57], but are often hard to measure at scale.
Unsupervised ML techniques using routinely available EHR computable phenotypes can provide valuable data-driven inference about distinct phenotypic clusters. In longitudinal DL-based clustering of 11,028 patients with type 2 diabetes using a kernelized autoencoder algorithm that mapped 5 years of data, there were seven phenotypic clusters with distinct clinical trajectories and varying prevalence of comorbidities (i.e., hypertension, hypercholesterolemia) or diabetic complications [13]. In a separate analysis of 8,980 patients with newly diagnosed diabetes from Sweden, k-means and hierarchical clustering revealed five replicable clusters with significant differences in the observed risk of diabetic complications [59]. A separate analysis of 175,383 patients with type 2 diabetes further identified 20 frequent comorbidity clusters, and using Bayesian nonparametric models demonstrated a complex and dynamic interrelationship between diabetes-related comorbidities and accelerated disease progression [60].
Despite this, computable definitions can vary significantly in their ability to capture the respective phenotypes. Such differences can have a substantial impact on model performance even within the same center. In an analysis of 173,503 adults from the Duke University Health System, the concordance of variable definitions of diabetes (with or without ICD-9-CM codes) ranged from 86% to as low as 50% [61].
Finally, DL approaches, such as natural language processing, can be used to screen large hospital registries to monitor the quality of care. As shown in an analysis of 33,461 patients with diabetes from 2014 to 2020 in Northern California, a natural language processing approach accurately identified statin nonuse (AUROC of 0.99 [0.98–1.00]) and highlighted patient- (side effects/contraindications), clinician- (guideline‐discordant practice), and system-centered reasons (clinical inertia) for statin nonuse, with notable variation by race and ethnicity [62].
Predicting CVD among patients with diabetes (from diagnosis to risk prediction)
Diabetes is associated with a range of micro- and macro-vascular complications [3]. Given their simplicity and wide availability, fundoscopic images were used in some of the earliest DL models in medicine, predicting diabetic retinopathy with performance matching that of expert readers [11, 63, 64]. This has opened the way for efficient screening of both diabetes, and diabetes-related chronic kidney disease and retinopathy in settings with limited resources, as demonstrated in real-world implementation studies in Thailand and India [65, 66].
While current guidelines endorse routine screening for microvascular complications, there is a paucity of data to support the routine screening for macrovascular complications in asymptomatic individuals [67]. Diabetes has traditionally been regarded as an atherosclerotic CVD (ASCVD) equivalent [44]. Non-invasive cardiovascular imaging approaches, such as measurement of coronary artery calcium (CAC) [68], coronary computed tomography angiography [69], or functional testing [67], are often used to further risk stratify patients with diabetes and diagnosed subclinical CVD. However, such approaches are costly and hard to implement for population-level screening.
ML approaches may support more efficient screening of CVD in this population. In an analysis of NHANES, logistic regression, SVM, XGBoost and random forest models, as well as an ensemble of the four, showed comparable performance in detecting CVD among all-comers with an AUROC of 0.81 to 0.83 [50]. In a separate single-center study from China, training a model to predict the co-occurrence of coronary heart disease and diabetes using 52 structured features in 1273 patients with type 2 diabetes resulted in an AUROC of 0.77–0.80; however, this dropped to 0.7 in an independent dataset, highlighting the challenges in the generalizability of such tools when trained in single-center cohorts [70]. In a retrospective analysis of administrative data from Australia, investigators combined ML techniques with a social network analytic approach to define the disease network for patients with diabetes with or without CVD and identify discriminatory features for CVD presence, with a reported overall AUROC of 0.83 for the random forest classifier, only dropping to 0.81 for a logistic regression model [71]. Overall, it appears that in most cohorts there were minimal gains from using more complex and less interpretable algorithms compared to standard logistic regression. Moreover, many studies do not report the incremental value beyond established risk scores such as the pooled cohort equations, which prevents a reliable assessment of their net clinical value.
Predictive models can further be customized for more specific cardiovascular conditions, such as congestive heart failure, and model survival analyses incorporating time-to-event outcomes. In a post hoc analysis of the ACCORD trial, a non-parametric random survival forest model predicted the risk of incident heart failure, with a C-statistic of 0.77 [72]. A parsimonious five-feature integer-based score based on this model maintained moderate discriminatory performance in both ACCORD (Action to Control Cardiovascular Risk in Diabetes) and an independent test set from Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) with an AUROC of 0.74 and 0.70, respectively. In a separate retrospective analysis of an EHR-based cohort of patients with diabetes undergoing cardiac testing, a deep neural network survival method resulted in an AUROC of 0.77 for incident heart failure [36].
Many of these studies should be interpreted with caution. First, as shown in a recent systematic review of predictive models for the detection of CVD among patients with diabetes, there is often a high risk of bias in several studies and poor adherence to standardized reporting guidelines [73–75]. Second, retrospective analyses of single-center cohorts and administrative claims are also prone to perpetuating biases and inequities in healthcare since patients who have better access to healthcare are more likely to utilize such resources and be represented in administrative claims datasets [76].
Digital health for diabetes care optimization and personalization through predictive algorithms
As the focus shifts from the secondary prevention of diabetes-related complications to earlier prevention in the community, various digital health technologies emerge that can be deployed at scale and minimal cost. Large language models (LLM) have already led to smart conversational agents (“chatbots”), such as ChatGPT, which are freely accessible to most individuals with internet access. Such models are task-agnostic and have been shown to provide “concise”, “well-organized” and easy-to-understand instructions to a series of questions regarding diabetes self-management, albeit with occasional factual inaccuracies [77]. Such tools could be incorporated into existing digital healthcare platforms that combine glucometer, bioelectrical impedance, blood pressure, activity, and AI-derived nutritional analysis data to improve glycemia and weight loss among patients with type 2 diabetes [78].
In the same vein, the rapid uptake in the use of wearable devices and smartwatches has led to AI-enabled solutions to optimize glycemic management. These applications have built on an expanding body of research highlighting the value of AI-ECG (both using 12-lead or 1-lead signals) in detecting subclinical forms of cardiomyopathy and arrhythmias [79–81]. Recent work from our lab has further expanded these approaches to the use of ECG images [82, 83] and single-lead wearable signals [84], enabling the scaling of such technologies to low-resource settings and to ubiquitous data streams.
In diabetes, AI-ECG-guided monitoring through customized DL models has shown promise in detecting hypoglycemic events [85, 86], and is currently being studied in prospective studies [87, 88]. In one of the pilot studies, investigators trained personalized models using a combination of convolutional (CNN) and recurrent neural networks (RNN) for each participant using data collected over the run-in period, followed by subsequent testing in the same patient. This combination of distinct model architectures takes advantage of the distinct strengths of each model type, with CNN learning hierarchical, abstract representations of the input space, whereas RNN learns sequence patterns across time [85]. Similar concepts have been applied to continuous glucose monitoring (CGM). Here, multi-modal data integration from CGM devices, meal or insulin entries and sensor wristbands has shown promise in detecting hypo- or hyperglycemic events in patients with type 1 diabetes in both simulation [89], as well as small real-world prospective studies [90]. While such technologies have the potential to democratize access to high-value care, we have shown that as of 2020 use patterns suggested disproportionately lower use among individuals with or at risk of CVD than those without CVD risk factors, with fewer than 1 in 4 using such devices [91, 92].
AI-driven innovation in clinical trials and evidence generation
Detecting heterogeneous treatment effects
Randomized controlled trials (RCTs) represent the methodological and regulatory gold-standard to test the efficacy and safety of new therapies [93]. However, RCTs traditionally report an average treatment effect (ATE) which does not adequately describe the individualized benefit for each unique patient profiles [94]. The detection of reliable heterogeneous treatment effects (HTE) is limited by the fact that in outcomes trials participants get assigned to one arm (thus the “counterfactual” is never observed). In addition, most trials lack statistical power to detect subgroup differences [95].
One way to explore such differences is through a priori or post hoc-defined clinical subgroups. For instance, it has been shown that sex and body mass index are associated with heterogeneity in the treatment and safety signal of thiazolidinediones and sulfonylureas [96], whereas insulin resistance has been associated with significant differences in the glycemic response to dipeptidyl peptidase 4 (DPP-4) inhibitors [97]. Such subgroups, however, rely on simplistic subgroup definitions, and may not accurately reflect the phenotypic diversity seen in clinical profiles and treatment response. Various statistical approaches have been employed to identify such complex effects, with methods ranging from unsupervised clustering [98] to causal forests and meta-learners (i.e. X-learners), algorithms that can use any supervised learning or regression method to estimate the conditional average treatment effect [94]. In applying this approach in ACCORD and Veteran Affairs Diabetes Trial (VADT), investigators described eight subgroups in which the differences in major adverse cardiovascular events ranged from as low as -5.1% to as high as 3.1% [99].
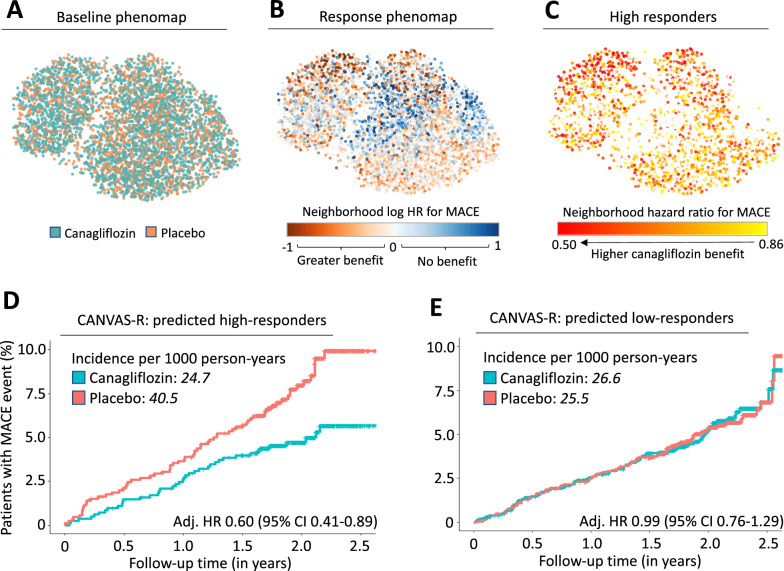
Most of these approaches focus on the absolute risk reduction of a therapy, which reflects both the relative treatment effect as well as a patient’s baseline risk. We previously developed and tested a phenomapping-based method that creates multidimensional representations of a population based on the full breadth of pre-randomization phenotypes. Over a series of in silico simulations that account for the unique phenotype of each participant relative to all other participants, an ML algorithm learns signatures that are consistently associated with a higher or lower relative treatment effect. In representative applications, our approach has reproduced a beneficial association between the use of anatomical as opposed to functional testing in patients with diabetes and chest pain [100, 101], and highlighted heterogeneity across phenotypes in the cardiovascular benefits of canagliflozin [12] as well as intensive systolic blood pressure control [102] (Fig. 3). However, prospective validation of any post-hoc comparisons is required to inform treatment decisions.
Fig. 3.
Phenomapping-derived tools for personalized effect estimates. Phenomaps enable a visual and topological representation of the baseline phenotypic variance of a trial population while accounting for many pre-randomization features. As shown in an analysis of the Canagliflozin Cardiovascular Assessment (CANVAS) trial [138], a phenomap representation of all enrolled patients shows that the study arms are randomly distributed in the phenotypic space (A). Through a series of iterative analyses centered around each patient’s unique phenotypic location, a machine learning model can learn phenotypic signatures associated with distinct responses to canagliflozin versus placebo therapy (B, C). An extreme gradient boosting algorithm trained to describe this heterogeneity in treatment effect in CANVAS successfully stratified the independent CANVAS-R population into high- (D) and low-responders (E). Panels reproduced with permission from Oikonomou et al. [12]
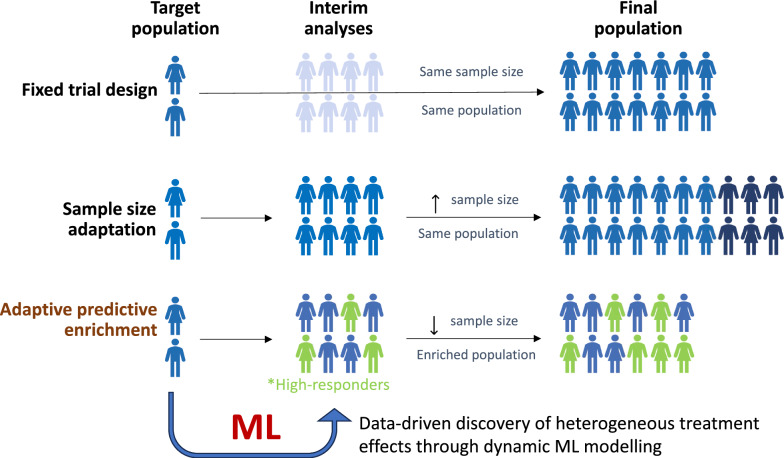
Towards smarter clinical trials
Furthermore, ML can be used to guide the design of adaptive clinical trials, guiding protocol modifications based on accumulating data [103] (Fig. 4). The need for methodological innovation in this space has been embraced by the United States Food and Drug Administration (FDA) [104]. For instance, ML-driven approaches of individualized predictive benefit could be integrated into interim analyses to prioritize randomization of patients with a higher expected net clinical benefit from the studied intervention [105]. In a simulation of real-world clinical trial data from Insulin Resistance in Stroke study (IRIS) [106], and Systolic Blood Pressure Intervention Trial (SPRINT) [107] an ML-informed strategy of adaptive, predictive enrichment enabled a consistent reduction in the number of enrolled participants, while preserving the original trial’s effect [105].
Fig. 4.
Machine learning for predictive enrichment of randomized control trials. Machine learning can be used to guide adaptive clinical trial design though data-driven inference and predictive enrichment. Traditional fixed trial designs do not allow modifications in the patient population, whereas sample size adaptations only allow interim revisions in the power calculations and target sample sizes based on the accumulating rate of primary outcome and safety events. In trials whereas there happens to be clinically meaningful heterogeneity in the treatment effect, a priori inclusion of machine learning, data-driven inference may provide early signals of heterogeneous benefit or harm and a reference for adaptive predictive enrichment. This approach can optimize the trial’s efficacy, shorten its duration, minimize its costs, maximize inference, and ultimately ensure safety for the study participants. ML machine learning
Causal inference from observational data
Modern RCTs are both resource and time-intensive [108], particularly when evaluating the effects of novel therapies on major clinical endpoints [109–111]. Federated analytic approaches that utilize large-scale, multinational, real-world databases, such as the Large-scale evidence generation and evaluation across a network of databases for type 2 diabetes mellitus (LEGEND-T2DM) initiative, are currently underway to enable comparative effectiveness analysis through both traditional and ML-driven big data approaches [112, 113].
Key methodological considerations when interpreting ML models
Finding the best algorithm
In the ML literature, it is widely recognized that a priori knowledge of an optimal algorithm is challenging for any given task. This often depends on the underlying dataset, the performance metric utilized, whereas for any given algorithm performance may still vary with tuning of model-specific hyperparameters (values used to control the training process that are external to the model and cannot be computed from the data). Second, there is a common misconception that for any given dataset, complex models will always outperform less complex ones. This may be true for tasks involving unstructured data, in particular biomedical images and videos, where DL models enable automatic learning and hierarchical combination of key spatial as well as temporal features (rather than relying on hand-engineered features), as well as models that are robust to variations, scalable and transferrable across tasks [114]. However, for structured datasets, such as databases of clinical information used for predictive modeling, the performance of easily interpretable models, such as logistic regression, is often comparable to that of complex extreme gradient boosting or neural network methods [115]. Third, complex models are susceptible to learning noise that may not generalize to a new dataset (overfitting) [116]. In this context, careful consideration of the available data and training plan (i.e., cross-validation), as well as strict separation of training and testing datasets, are warranted to maximize the external validity of new models.
Geographic and temporal drift in model performance
The training of any clinical model should not stop at the time of deployment but rather continue by incorporating real-time data and updating its parameters to prevent a drift in performance when used in a different clinical, geographical, or temporal setting [117]. A notable example here is a widely implemented and proprietary EHR-embedded sepsis prediction model whose external performance was substantially different from the one reported by the model’s creators (AUROC of 0.63 from 0.76–0.83) when deployed across independent hospitals with heterogeneous patient populations [118].
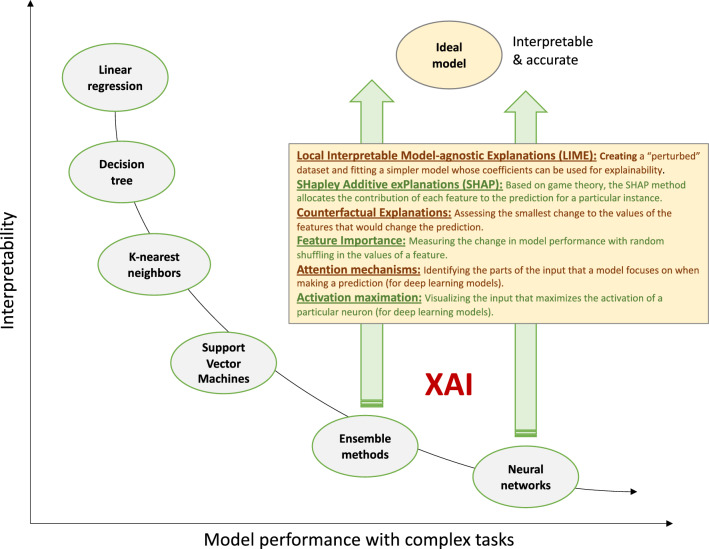
Promoting explainable AI
To bridge the interpretability gap of complex “black box” algorithms, various approaches have emerged including Local Interpretable Model-agnostic Explanations (LIME) and SHapley Additive exPlanations (SHAP) [119, 120] (Fig. 5). Though such approaches are often imperfect, ensuring model explainability is not only a regulatory recommendation, but also enhances the adoption of the model in the real world. In a survey of 170 physicians, greater explainability of ML risk calculators was significantly associated with greater physician understanding and trust of the algorithm [121].
Fig. 5.
Explainability and interpretability of medical machine learning. Broadly speaking, more complex algorithms demonstrate better performance when dealing with complex tasks and data inputs. For instance, the recognition of cardiomyopathy using echocardiographic videos may require a deep learning algorithm to model the full extent of temporal and spatial features that carry diagnostic value, whereas predicting the risk of re-admission using electronic health record data may be modelled using generalized linear models. Simpler models, such as decision trees and linear models are intuitive and interpretable, whereas ensemble and neural network-based methods are too complex for the human mind to fully understand. Explainable artificial intelligence (XAI) methods aim to bridge this interpretability gap by offering direct or indirect insights into the inner workings of complex algorithms
Statistical, ethical and regulatory concerns: promoting equitable and safe AI use
Ensuring good research practices
Clinical predictions rarely rely on a single factor and are most often multivariable by design. In 2015, to provide a standardized framework for the creation and reporting of such statistical models, the transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) statement was published [39]. This followed multiple reports, including systematic reviews of risk prediction models in type 2 diabetes, that showed widespread use of poor methods and reporting [122, 123] contributing to “avoidable waste” in research evidence [124]. Unfortunately, several subsequent reviews have shown poor adherence to these standards, particularly among studies using ML algorithms [125]. The increasing adoption of ML algorithms in clinical prediction modeling, despite the lack of clear incremental value beyond simpler methods such as logistic regression in most settings [115, 126], has prompted the original TRIPOD authors to update their statement (TRIPOD-AI, see [127]) researchers, clinicians, systematic reviewers, and policy-makers critically appraise ML-based studies. ML models should generally be used when processing large amounts of multi-dimensional or complex inputs (e.g. time-series from wearables, videos etc.), whereas head-to-head comparisons to traditional statistical models should be provided when feasible to assess the trade-off between performance, complexity, and interpretability.
Mitigating bias through AI
Since ML models learn from existing data and care patterns, they can perpetuate human and structural biases [128, 129] (Table 1). Careful evaluation of the historical training data for health care disparities, ensuring that historically disadvantaged subgroups have adequate representation, review of model performance across key subgroups, and incorporating feedback from key stakeholders and patient representatives are some approaches that can be taken to mitigate bias [76, 128]. This is not a straightforward task and requires caution when assessing for confounders [130], since ML models have shown the ability to identify features such as race even when blinded to such labels [131].
Table 1.
Types and examples of bias in medical artificial intelligence
| Bias type | Definition: “A bias arising from…” | Example |
|---|---|---|
| Confirmation bias | A tendency to interpret data in a way that confirms our prior beliefs | A machine learning model confirms existing assumptions about certain broad phenotypic groups benefiting from a given therapy, potentially leading to unequal treatment and misdiagnosis |
| Sampling bias | Non-random sampling which limits the generalizability of an algorithm | Enrolling patients who visit a particular clinic or location may not represent the broader diabetes population |
| Algorithmic bias | The design and implementation of an algorithms that systematically discriminates against a given group | A blood pressure monitoring system that may provide consistently inaccurate readings for a given demographic group |
| Aggregation bias | Drawing misleading conclusions about individuals from group data | Concluding all patients with type 2 diabetes and hypertension benefit from a given medication without considering individual variations |
| Longitudinal data fallacy | Poor analysis of temporal data | Assessing quality of diabetes control and performing long-term risk prognostication using a single laboratory reading rather than long-term patterns |
| Implicit bias | Unintentional embedding of underlying biases and prejudices in algorithms | A model that is trained using records from a specific racial or ethnic group may make inaccurate predictions and disproportionately misclassify individuals from other racial groups as having higher or lower risk of diabetic complications contributing to healthcare disparities |
| User interaction bias | Both the user interface and the user's behavior | A diabetes management digital health app only collects voluntary input data, thus not capturing all relevant patient information |
| Presentation bias | How information is displayed to users | A patient may miss important information on an app due to the information's placement at the bottom of the screen |
| Emergent bias | Longitudinal changes in population, societal habits, norms, and practices over time | An outdated diabetes therapy might persist due to long-standing cultural beliefs |
| Evaluation bias | The process of model evaluation | The effectiveness of a novel antihyperglycemic therapy is evaluated against a benchmark that favors a particular demographic |
| Population bias | Differences in user characteristics between the training and the intended population | A diabetes management application initially tested among tech-savvy young adults may not adequately address the needs of older adults |
Navigating the regulatory framework
While clinical decision support (CDS) tools used to assist with electronic patient records, administrative tasks, medical device data, and models aimed at supporting a healthy lifestyle fall outside the FDA’s definition of a “device” [132], most diagnostic and predictive clinical models and CDS are regulated under the “Software as Medicine Device (SaMD)” umbrella and categorized as class I (low-risk), II (moderate-risk), III (high-risk) [20]. In the US, the FDA mandates that class III devices generally undergo a longer and more in-depth review process, known as pre-market authorization. However, for lower or intermediate-risk devices (class I and II), alternative pathways exist [20]. The 510(k) pathway requires manufacturers to show that the risk presented by their device is no greater than that of a substantially equivalent predicate device [20], whereas the de novo pathway is designed for class I or II devices without predicates [133]. While built to accelerate the regulatory process, the latter two pathways have been criticized on certain occasions for facilitating the clearance of devices based on faulty predicates [134]. The regulatory process is different in Europe, where lowest risk devices (class I) are the responsibility of the manufacturer, whereas class II and III devices are processed in a decentralized way through private “Notified Bodies”. Of the 124 AI/ML-based devices approved in the USA and Europe between 2015 and 2020, 80 were first approved in Europe [20]. The European Union’s General Data Protection Regulation (GDPR) further lists explainability as a requisite for any medical AI application [135]. Despite the above, there is no clear consensus as to whether regulatory bodies should require RCT-level evidence to support the effectiveness and safety of their proposed AI tools, even though recent studies have demonstrated the feasibility of testing the net clinical benefit of AI-based ECG and echocardiographic models in the context of pragmatic RCTs [136, 137].
Conclusions
Rapid advances in AI and ML have revolutionized the field of medicine and have identified new ways to optimize the management of diabetes and its cardiovascular complications. Nevertheless, several challenges remain, ranging from standardizing the assessment of model performance along with model interpretability and explainability to mitigating bias during both development and deployment. Acknowledging these challenges and fostering a collaborative environment between clinicians, researchers, sponsors, and regulatory agencies is a prerequisite to harness the full potential of AI in catalyzing the transition towards a more patient-centered approach to the care of diabetes and CVD.
Supplementary Information
Additional file 1: Table S1. Strengths and weaknesses of commonly used metrics in machine learning.
Acknowledgements
Not applicable.
Abbreviations
- ADA
American Diabetes Association
- AI
Artificial intelligence
- AUROC
Area Under the Receiver Operating Characteristic Curve
- CDS
Clinical decision support
- CNN
Convolutional Neural Network
- CVD
Cardiovascular disease
- DL
Deep learning
- ECG
Electrocardiography
- EHR
Electronic health record
- FDA
U.S. Food and Drug Administration
- ML
Machine learning
- NHANES
National Health and Nutrition Examination Survey
- RCT
Randomized controlled trials
- RNN
Recurrent neural network
- XGBoost
EXtreme Gradient Boosting
Author contributions
Both authors contributed to the interpretation and discussion of the evidence. EKO performed the literature search and drafted the manuscript RK revised the manuscript. Both authors read and approved the final manuscript.
Funding
Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL153775 (to RK), as well as the Doris Duke Charitable Foundation (under award 2022060 to RK). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
E.K.O and R.K. are co-inventors of the U.S. Patent Applications 63/508,315 and 63/177,117 and co-founders of Evidence2Health, a health analytics company to improve evidence-based cardiovascular care. E.K.O. reports a consultancy and stock option agreement with Caristo Diagnostics Ltd (Oxford, U.K.), unrelated to the current work. R.K. received support from the National Heart, Lung, and Blood Institute of the National Institutes of Health (under award K23HL153775) and the Doris Duke Charitable Foundation (under award 2022060). R.K. further receives research support, through Yale, from Bristol-Myers Squibb and Novo Nordisk, unrelated to current work. He is a coinventor of U.S. Pending Patent Applications 63/428,569 and 63/346,610, unrelated to the current work. He is an Associate Editor at JAMA.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haug CJ, Drazen JM. Artificial intelligence and machine learning in clinical medicine, 2023. N Engl J Med. 2023;388(13):1201–1208. doi: 10.1056/NEJMra2302038. [DOI] [PubMed] [Google Scholar]
- 2.Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44–56. doi: 10.1038/s41591-018-0300-7. [DOI] [PubMed] [Google Scholar]
- 3.Joseph JJ, Deedwania P, Acharya T, Aguilar D, Bhatt DL, Chyun DA, et al. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation. 2022;145(9):e722–e759. doi: 10.1161/CIR.0000000000001040. [DOI] [PubMed] [Google Scholar]
- 4.Ong KL, Stafford LK, McLaughlin SA, Boyko EJ, Vollset SE, Smith AE, et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023 doi: 10.1016/S0140-6736(23)01301-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ravaut M, Harish V, Sadeghi H, Leung KK, Volkovs M, Kornas K, et al. Development and validation of a machine learning model using administrative health data to predict onset of type 2 diabetes. JAMA Netw Open. 2021;4(5):e2111315. doi: 10.1001/jamanetworkopen.2021.11315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seto H, Oyama A, Kitora S, Toki H, Yamamoto R, Kotoku J, et al. Gradient boosting decision tree becomes more reliable than logistic regression in predicting probability for diabetes with big data. Sci Rep. 2022;12(1):15889. doi: 10.1038/s41598-022-20149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kulkarni AR, Patel AA, Pipal KV, Jaiswal SG, Jaisinghani MT, Thulkar V, et al. Machine-learning algorithm to non-invasively detect diabetes and pre-diabetes from electrocardiogram. BMJ Innov. 2023 doi: 10.1136/bmjinnov-2021-000759. [DOI] [Google Scholar]
- 8.Hahn S-J, Kim S, Choi YS, Lee J, Kang J. Prediction of type 2 diabetes using genome-wide polygenic risk score and metabolic profiles: a machine learning analysis of population-based 10-year prospective cohort study. EBioMedicine. 2022;86:104383. doi: 10.1016/j.ebiom.2022.104383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrasco-Zanini J, Pietzner M, Lindbohm JV, Wheeler E, Oerton E, Kerrison N, et al. Proteomic signatures for identification of impaired glucose tolerance. Nat Med. 2022;28(11):2293–2300. doi: 10.1038/s41591-022-02055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tallam H, Elton DC, Lee S, Wakim P, Pickhardt PJ, Summers RM. Fully automated abdominal CT biomarkers for type 2 diabetes using deep learning. Radiology. 2022;304(1):85–95. doi: 10.1148/radiol.211914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316(22):2402–2410. doi: 10.1001/jama.2016.17216. [DOI] [PubMed] [Google Scholar]
- 12.Oikonomou EK, Suchard MA, McGuire DK, Khera R. Phenomapping-derived tool to individualize the effect of canagliflozin on cardiovascular risk in type 2 diabetes. Diabetes Care. 2022;45(4):965–974. doi: 10.2337/dc21-1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manzini E, Vlacho B, Franch-Nadal J, Escudero J, Génova A, Reixach E, et al. Longitudinal deep learning clustering of type 2 diabetes mellitus trajectories using routinely collected health records. J Biomed Inform. 2022;135:104218. doi: 10.1016/j.jbi.2022.104218. [DOI] [PubMed] [Google Scholar]
- 14.Hanna J, Nargesi AA, Essien UR, Sangha V, Lin Z, Krumholz HM, et al. County-level variation in cardioprotective antihyperglycemic prescribing among medicare beneficiaries. Am J Prev Cardiol. 2022;11:100370. doi: 10.1016/j.ajpc.2022.100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sangha V, Lipska K, Lin Z, Inzucchi SE, McGuire DK, Krumholz HM, et al. Patterns of prescribing sodium–glucose cotransporter-2 inhibitors for medicare beneficiaries in the United States. Circ Cardiovasc Qual Outcomes. 2021;14(12):e008381. doi: 10.1161/CIRCOUTCOMES.121.008381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nargesi AA, Clark C, Aminorroaya A, Chen L, Liu M, Reddy A, et al. Persistence on novel cardioprotective antihyperglycemic therapies in the United States. Am J Cardiol. 2023;196:89–98. doi: 10.1016/j.amjcard.2023.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nargesi AA, Jeyashanmugaraja GP, Desai N, Lipska K, Krumholz H, Khera R. Contemporary national patterns of eligibility and use of novel cardioprotective antihyperglycemic agents in type 2 diabetes mellitus. J Am Heart Assoc. 2021;10(13):e021084. doi: 10.1161/JAHA.121.021084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vollmer S, Mateen BA, Bohner G, Király FJ, Ghani R, Jonsson P, et al. Machine learning and artificial intelligence research for patient benefit: 20 critical questions on transparency, replicability, ethics, and effectiveness. BMJ. 2020;368:l6927. doi: 10.1136/bmj.l6927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Srikumar M, Finlay R, Abuhamad G, Ashurst C, Campbell R, Campbell-Ratcliffe E, et al. Advancing ethics review practices in AI research. Nat Mach Intell. 2022;4(12):1061–1064. [Google Scholar]
- 20.Muehlematter UJ, Daniore P, Vokinger KN. Approval of artificial intelligence and machine learning-based medical devices in the USA and Europe (2015–20): a comparative analysis. Lancet Digit Health. 2021;3(3):e195–203. doi: 10.1016/S2589-7500(20)30292-2. [DOI] [PubMed] [Google Scholar]
- 21.Gottlieb S, Silvis L. Regulators face novel challenges as artificial intelligence tools enter medical practice. JAMA Health Forum. 2023;4(6):e232300. doi: 10.1001/jamahealthforum.2023.2300. [DOI] [PubMed] [Google Scholar]
- 22.Sarker IH. Machine learning: algorithms, real-world applications and research directions. SN Comput Sci. 2021;2(3):160. doi: 10.1007/s42979-021-00592-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health. 2018;8(2):020303. doi: 10.7189/jogh.08.020303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Austin PC, van Klaveren D, Vergouwe Y, Nieboer D, Lee DS, Steyerberg EW. Validation of prediction models: examining temporal and geographic stability of baseline risk and estimated covariate effects. Diagn Progn Res. 2017;1:12. doi: 10.1186/s41512-017-0012-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jing L, Tian Y. Self-supervised visual feature learning with deep neural networks: a survey. IEEE Trans Pattern Anal Mach Intell. 2021;43(11):4037–4058. doi: 10.1109/TPAMI.2020.2992393. [DOI] [PubMed] [Google Scholar]
- 26.Huang S-C, Pareek A, Jensen M, Lungren MP, Yeung S, Chaudhari AS. Self-supervised learning for medical image classification: a systematic review and implementation guidelines. NPJ Digit Med. 2023;6(1):74. doi: 10.1038/s41746-023-00811-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holste G, Oikonomou EK, Mortazavi B, Wang Z, Khera R. Self-supervised learning of echocardiogram videos enables data-efficient clinical diagnosis. arXiv [cs.CV]. 2022. http://arxiv.org/abs/2207.11581.
- 28.Holste G, Oikonomou EK, Mortazavi BJ, Coppi A, Faridi KF, Miller EJ, et al. Severe aortic stenosis detection by deep learning applied to echocardiography. Eur Heart J. 2023; Available from: 10.1093/eurheartj/ehad456. [DOI] [PMC free article] [PubMed]
- 29.Hu X, Zeng D, Xu X, Shi Y. Semi-supervised contrastive learning for label-efficient medical image segmentation. arXiv [cs.CV]. 2021. http://arxiv.org/abs/2109.07407.
- 30.Mehari T, Strodthoff N. Self-supervised representation learning from 12-lead ECG data. Comput Biol Med. 2022;141:105114. doi: 10.1016/j.compbiomed.2021.105114. [DOI] [PubMed] [Google Scholar]
- 31.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49–73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 32.Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ. 2017;357:j2099. doi: 10.1136/bmj.j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.SCORE2 Working Group and ESC Cardiovascular Risk Collaboration SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439–2454. doi: 10.1093/eurheartj/ehab309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ishwaran H, Kogalur UB, Blackstone EH, Lauer MS. Random survival forests. arXiv [stat.AP]. 2008. http://arxiv.org/abs/0811.1645.
- 35.Pickett KL, Suresh K, Campbell KR, Davis S, Juarez-Colunga E. Random survival forests for dynamic predictions of a time-to-event outcome using a longitudinal biomarker. BMC Med Res Methodol. 2021;21(1):216. doi: 10.1186/s12874-021-01375-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gandin I, Saccani S, Coser A, Scagnetto A, Cappelletto C, Candido R, et al. Deep-learning-based prognostic modeling for incident heart failure in patients with diabetes using electronic health records: a retrospective cohort study. PLoS ONE. 2023;18(2):e0281878. doi: 10.1371/journal.pone.0281878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128–138. doi: 10.1097/EDE.0b013e3181c30fb2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van Calster B, McLernon DJ, van Smeden M, Wynants L, Steyerberg EW. Topic group ‘evaluating diagnostic tests and prediction models’ of the STRATOS initiative. Calibration: the Achilles heel of predictive analytics. BMC Med. 2019;17(1):230. doi: 10.1186/s12916-019-1466-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162(1):55–63. doi: 10.7326/M14-0697. [DOI] [PubMed] [Google Scholar]
- 40.Fitzgerald M, Saville BR, Lewis RJ. Decision curve analysis. JAMA. 2015;313(4):409–410. doi: 10.1001/jama.2015.37. [DOI] [PubMed] [Google Scholar]
- 41.Ghassemi M, Oakden-Rayner L, Beam AL. The false hope of current approaches to explainable artificial intelligence in health care. Lancet Digit Health. 2021;3(11):e745–e750. doi: 10.1016/S2589-7500(21)00208-9. [DOI] [PubMed] [Google Scholar]
- 42.Reddy S. Explainability and artificial intelligence in medicine. Lancet Digit Health. 2022;4(4):e214–e215. doi: 10.1016/S2589-7500(22)00029-2. [DOI] [PubMed] [Google Scholar]
- 43.Rudin C. Stop explaining black box machine learning models for high stakes decisions and use interpretable models instead. Nat Mach Intell. 2019;1(5):206–215. doi: 10.1038/s42256-019-0048-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S19–S40. [Google Scholar]
- 45.US Preventive Services Task Force. Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement. JAMA. 2021;326(8):736–743. doi: 10.1001/jama.2021.12531. [DOI] [PubMed] [Google Scholar]
- 46.Bang H, Edwards AM, Bomback AS, Ballantyne CM, Brillon D, Callahan MA, et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med. 2009;151(11):775–783. doi: 10.1059/0003-4819-151-11-200912010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen L, Magliano DJ, Balkau B, Colagiuri S, Zimmet PZ, Tonkin AM, et al. AUSDRISK: an Australian type 2 diabetes risk assessment tool based on demographic, lifestyle and simple anthropometric measures. Med J Aust. 2010;192(4):197–202. doi: 10.5694/j.1326-5377.2010.tb03507.x. [DOI] [PubMed] [Google Scholar]
- 48.Thomas C, Hyppönen E, Power C. Type 2 diabetes mellitus in midlife estimated from the Cambridge risk score and body mass index. Arch Intern Med. 2006;166(6):682–688. doi: 10.1001/archinte.166.6.682. [DOI] [PubMed] [Google Scholar]
- 49.Stiglic G, Pajnkihar M. Evaluation of major online diabetes risk calculators and computerized predictive models. PLoS ONE. 2015;10(11):e0142827. doi: 10.1371/journal.pone.0142827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dinh A, Miertschin S, Young A, Mohanty SD. A data-driven approach to predicting diabetes and cardiovascular disease with machine learning. BMC Med Inform Decis Mak. 2019;19(1):1–15. doi: 10.1186/s12911-019-0918-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weisman A, Tu K, Young J, Kumar M, Austin PC, Jaakkimainen L, et al. Validation of a type 1 diabetes algorithm using electronic medical records and administrative healthcare data to study the population incidence and prevalence of type 1 diabetes in Ontario, Canada. BMJ Open Diabetes Res Care. 2020;8(1):e001224. doi: 10.1136/bmjdrc-2020-001224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carter TC, Rein D, Padberg I, Peter E, Rennefahrt U, David DE, et al. Validation of a metabolite panel for early diagnosis of type 2 diabetes. Metabolism. 2016;65(9):1399–1408. doi: 10.1016/j.metabol.2016.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen R, Mias GI, Li-Pook-Than J, Jiang L, Lam HYK, Chen R, et al. Personal omics profiling reveals dynamic molecular and medical phenotypes. Cell. 2012;148(6):1293–1307. doi: 10.1016/j.cell.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhou W, Sailani MR, Contrepois K, Zhou Y, Ahadi S, Leopold SR, et al. Longitudinal multi-omics of host-microbe dynamics in prediabetes. Nature. 2019;569(7758):663–671. doi: 10.1038/s41586-019-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Piening BD, Zhou W, Contrepois K, Röst H, Gu Urban GJ, Mishra T, et al. Integrative personal omics profiles during periods of weight gain and loss. Cell Syst. 2018;6(2):157–170.e8. doi: 10.1016/j.cels.2017.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ahadi S, Zhou W, Schüssler-Fiorenza Rose SM, Sailani MR, Contrepois K, Avina M, et al. Personal aging markers and ageotypes revealed by deep longitudinal profiling. Nat Med. 2020;26(1):83–90. doi: 10.1038/s41591-019-0719-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Schüssler-Fiorenza Rose SM, Contrepois K, Moneghetti KJ, Zhou W, Mishra T, Mataraso S, et al. A longitudinal big data approach for precision health. Nat Med. 2019;25(5):792–804. doi: 10.1038/s41591-019-0414-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cefalu WT, Andersen DK, Arreaza-Rubín G, Pin CL, Sato S, Verchere CB, et al. Heterogeneity of diabetes: β-cells, phenotypes, and precision medicine: proceedings of an international symposium of the Canadian Institutes of Health Research’s Institute of Nutrition, Metabolism and Diabetes and the U.S. National Institutes of Health’s National Institute of Diabetes and Digestive and Kidney Diseases. Diabetes. 2021 doi: 10.2337/db21-0777. [DOI] [Google Scholar]
- 59.Ahlqvist E, Storm P, Käräjämäki A, Martinell M, Dorkhan M, Carlsson A, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018;6(5):361–369. doi: 10.1016/S2213-8587(18)30051-2. [DOI] [PubMed] [Google Scholar]
- 60.Martinez-De la Torre A, Perez-Cruz F, Weiler S, Burden AM. Comorbidity clusters associated with newly treated type 2 diabetes mellitus: a Bayesian nonparametric analysis. Sci Rep. 2022;12(1):20653. doi: 10.1038/s41598-022-24217-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Richesson RL, Rusincovitch SA, Wixted D, Batch BC, Feinglos MN, Miranda ML, et al. A comparison of phenotype definitions for diabetes mellitus. J Am Med Inform Assoc. 2013;20(e2):e319–e326. doi: 10.1136/amiajnl-2013-001952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sarraju A, Zammit A, Ngo S, Witting C, Hernandez-Boussard T, Rodriguez F. Identifying reasons for statin nonuse in patients with diabetes using deep learning of electronic health records. J Am Heart Assoc. 2023;12(7):e028120. doi: 10.1161/JAHA.122.028120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bora A, Balasubramanian S, Babenko B, Virmani S, Venugopalan S, Mitani A, et al. Predicting the risk of developing diabetic retinopathy using deep learning. Lancet Digit Health. 2021;3(1):e10–e19. doi: 10.1016/S2589-7500(20)30250-8. [DOI] [PubMed] [Google Scholar]
- 64.Dai L, Wu L, Li H, Cai C, Wu Q, Kong H, et al. A deep learning system for detecting diabetic retinopathy across the disease spectrum. Nat Commun. 2021;12(1):3242. doi: 10.1038/s41467-021-23458-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ruamviboonsuk P, Tiwari R, Sayres R, Nganthavee V, Hemarat K, Kongprayoon A, et al. Real-time diabetic retinopathy screening by deep learning in a multisite national screening programme: a prospective interventional cohort study. Lancet Digit Health. 2022;4(4):e235–e244. doi: 10.1016/S2589-7500(22)00017-6. [DOI] [PubMed] [Google Scholar]
- 66.Nunez do Rio JM, Nderitu P, Raman R, Rajalakshmi R, Kim R, Rani PK, et al. Using deep learning to detect diabetic retinopathy on handheld non-mydriatic retinal images acquired by field workers in community settings. Sci Rep. 2023;13(1):1392. doi: 10.1038/s41598-023-28347-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Young LH, Wackers FJT, Chyun DA, Davey JA, Barrett EJ, Taillefer R, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes: the DIAD study: a randomized controlled trial. JAMA. 2009;301(15):1547–1555. doi: 10.1001/jama.2009.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Malik S, Zhao Y, Budoff M, Nasir K, Blumenthal RS, Bertoni AG, et al. Coronary artery calcium score for long-term risk classification in individuals with type 2 diabetes and metabolic syndrome from the multi-ethnic study of atherosclerosis. JAMA Cardiol. 2017;2(12):1332–1340. doi: 10.1001/jamacardio.2017.4191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blanke P, Naoum C, Ahmadi A, Cheruvu C, Soon J, Arepalli C, et al. Long-term prognostic utility of coronary CT angiography in stable patients with diabetes mellitus. JACC Cardiovasc Imaging. 2016;9(11):1280–1288. doi: 10.1016/j.jcmg.2015.12.027. [DOI] [PubMed] [Google Scholar]
- 70.Fan R, Zhang N, Yang L, Ke J, Zhao D, Cui Q. AI-based prediction for the risk of coronary heart disease among patients with type 2 diabetes mellitus. Sci Rep. 2020;10(1):14457. doi: 10.1038/s41598-020-71321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hossain ME, Uddin S, Khan A. Network analytics and machine learning for predictive risk modelling of cardiovascular disease in patients with type 2 diabetes. Expert Syst Appl. 2021;164:113918. [Google Scholar]
- 72.Segar MW, Vaduganathan M, Patel KV, McGuire DK, Butler J, Fonarow GC, et al. Machine learning to predict the risk of incident heart failure hospitalization among patients with diabetes: the WATCH-DM risk score. Diabetes Care. 2019;42(12):2298–2306. doi: 10.2337/dc19-0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kee OT, Harun H, Mustafa N, Abdul Murad NA, Chin SF, Jaafar R, et al. Cardiovascular complications in a diabetes prediction model using machine learning: a systematic review. Cardiovasc Diabetol. 2023;22(1):13. doi: 10.1186/s12933-023-01741-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stevens LM, Mortazavi BJ, Deo RC, Curtis L, Kao DP. Recommendations for reporting machine learning analyses in clinical research. Circ Cardiovasc Qual Outcomes. 2020;13(10):e006556. doi: 10.1161/CIRCOUTCOMES.120.006556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Luo W, Phung D, Tran T, Gupta S, Rana S, Karmakar C, et al. Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J Med Internet Res. 2016;18(12):e323. doi: 10.2196/jmir.5870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Parikh RB, Teeple S, Navathe AS. Addressing bias in artificial intelligence in health care. JAMA. 2019;322(24):2377–2378. doi: 10.1001/jama.2019.18058. [DOI] [PubMed] [Google Scholar]
- 77.Sng GGR, Tung JYM, Lim DYZ, Bee YM. Potential and pitfalls of ChatGPT and natural-language artificial intelligence models for diabetes education. Diabetes Care. 2023;46(5):e103–e105. doi: 10.2337/dc23-0197. [DOI] [PubMed] [Google Scholar]
- 78.Lee Y-B, Kim G, Jun JE, Park H, Lee WJ, Hwang Y-C, et al. An integrated digital health care platform for diabetes management with AI-based dietary management: 48-week results from a randomized controlled trial. Diabetes Care. 2023;46(5):959–966. doi: 10.2337/dc22-1929. [DOI] [PubMed] [Google Scholar]
- 79.Attia ZI, Kapa S, Lopez-Jimenez F, McKie PM, Ladewig DJ, Satam G, et al. Screening for cardiac contractile dysfunction using an artificial intelligence-enabled electrocardiogram. Nat Med. 2019;25(1):70–74. doi: 10.1038/s41591-018-0240-2. [DOI] [PubMed] [Google Scholar]
- 80.Attia ZI, Noseworthy PA, Lopez-Jimenez F, Asirvatham SJ, Deshmukh AJ, Gersh BJ, et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction. Lancet. 2019;394(10201):861–867. doi: 10.1016/S0140-6736(19)31721-0. [DOI] [PubMed] [Google Scholar]
- 81.Cohen-Shelly M, Attia ZI, Friedman PA, Ito S, Essayagh BA, Ko W-Y, et al. Electrocardiogram screening for aortic valve stenosis using artificial intelligence. Eur Heart J. 2021;42(30):2885–2896. doi: 10.1093/eurheartj/ehab153. [DOI] [PubMed] [Google Scholar]
- 82.Sangha V, Mortazavi BJ, Haimovich AD, Ribeiro AH, Brandt CA, Jacoby DL, et al. Automated multilabel diagnosis on electrocardiographic images and signals. Nat Commun. 2022;13(1):1583. doi: 10.1038/s41467-022-29153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sangha V, Nargesi AA, Dhingra LS, Khunte A, Mortazavi BJ, Ribeiro AH, et al. Detection of left ventricular systolic dysfunction from electrocardiographic images. Circulation. 2023 doi: 10.1161/CIRCULATIONAHA.122.062646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Khunte A, Sangha V, Oikonomou EK, Dhingra LS, Aminorroaya A, Mortazavi BJ, et al. Detection of left ventricular systolic dysfunction from single-lead electrocardiography adapted for portable and wearable devices. NPJ Digit Med. 2023;6(1):124. doi: 10.1038/s41746-023-00869-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Porumb M, Stranges S, Pescapè A, Pecchia L. Precision medicine and artificial intelligence: a Pilot study on deep learning for hypoglycemic events detection based on ECG. Sci Rep. 2020;10(1):170. doi: 10.1038/s41598-019-56927-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lehmann V, Föll S, Maritsch M, van Weenen E, Kraus M, Lagger S, et al. Noninvasive hypoglycemia detection in people with diabetes using smartwatch data. Diabetes Care. 2023;46(5):993–997. doi: 10.2337/dc22-2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Andellini M, Haleem S, Angelini M, Ritrovato M, Schiaffini R, Iadanza E, et al. Artificial intelligence for non-invasive glycaemic-events detection via ECG in a paediatric population: study protocol. Health Technol. 2023;13(1):145–154. doi: 10.1007/s12553-022-00719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cisuelo O, Stokes K, Oronti IB, Haleem MS, Barber TM, Weickert MO, et al. Development of an artificial intelligence system to identify hypoglycaemia via ECG in adults with type 1 diabetes: protocol for data collection under controlled and free-living conditions. BMJ Open. 2023;13(4):e067899. doi: 10.1136/bmjopen-2022-067899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shahid S, Hussain S, Khan WA. Predicting continuous blood glucose level using deep learning. In: Proceedings of the 14th IEEE/ACM international conference on utility and cloud computing companion. New York: Association for Computing Machinery; 2022. p. 1–5. (UCC ’21).
- 90.Zhu T, Uduku C, Li K, Herrero P, Oliver N, Georgiou P. Enhancing self-management in type 1 diabetes with wearables and deep learning. NPJ Digit Med. 2022;5(1):78. doi: 10.1038/s41746-022-00626-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dhingra LS, Aminorroaya A, Oikonomou EK, Nargesi AA, Wilson FP, Krumholz HM, et al. Use of wearable devices in individuals with or at risk for cardiovascular disease in the US, 2019 to 2020. JAMA Netw Open. 2023;6(6):e2316634. doi: 10.1001/jamanetworkopen.2023.16634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Aminorroaya A, Dhingra LS, Nargesi AA, Oikonomou EK, Krumholz HM, Khera R. Use of smart devices to track cardiovascular health goals in the United States. JACC Adv. 2023;2(7):100544. doi: 10.1016/j.jacadv.2023.100544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bothwell LE, Podolsky SH. The emergence of the randomized, controlled trial. N Engl J Med. 2016;375(6):501–504. doi: 10.1056/NEJMp1604635. [DOI] [PubMed] [Google Scholar]
- 94.Künzel SR, Sekhon JS, Bickel PJ, Yu B. Metalearners for estimating heterogeneous treatment effects using machine learning. Proc Natl Acad Sci USA. 2019;116(10):4156–4165. doi: 10.1073/pnas.1804597116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rekkas A, Paulus JK, Raman G, Wong JB, Steyerberg EW, Rijnbeek PR, et al. Predictive approaches to heterogeneous treatment effects: a scoping review. BMC Med Res Methodol. 2020;20(1):264. doi: 10.1186/s12874-020-01145-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dennis JM, Henley WE, Weedon MN, Lonergan M, Rodgers LR, Jones AG, et al. Sex and BMI alter the benefits and risks of sulfonylureas and thiazolidinediones in type 2 diabetes: a framework for evaluating stratification using routine clinical and individual trial data. Diabetes Care. 2018;41(9):1844–1853. doi: 10.2337/dc18-0344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dennis JM, Shields BM, Hill AV, Knight BA, McDonald TJ, Rodgers LR, et al. Precision medicine in type 2 diabetes: clinical markers of insulin resistance are associated with altered short- and long-term glycemic response to DPP-4 inhibitor therapy. Diabetes Care. 2018;41(4):705–712. doi: 10.2337/dc17-1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zou X, Huang Q, Luo Y, Ren Q, Han X, Zhou X, et al. The efficacy of canagliflozin in diabetes subgroups stratified by data-driven clustering or a supervised machine learning method: a post hoc analysis of canagliflozin clinical trial data. Diabetologia. 2022;65(9):1424–1435. doi: 10.1007/s00125-022-05748-9. [DOI] [PubMed] [Google Scholar]
- 99.Edward JA, Josey K, Bahn G, Caplan L, Reusch JEB, Reaven P, et al. Heterogeneous treatment effects of intensive glycemic control on major adverse cardiovascular events in the ACCORD and VADT trials: a machine-learning analysis. Cardiovasc Diabetol. 2022;21(1):58. doi: 10.1186/s12933-022-01496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Oikonomou EK, Van Dijk D, Parise H, Suchard MA, de Lemos J, Antoniades C, et al. A phenomapping-derived tool to personalize the selection of anatomical vs. functional testing in evaluating chest pain (ASSIST) Eur Heart J. 2021;42(26):2536–2548. doi: 10.1093/eurheartj/ehab223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sharma A, Coles A, Sekaran NK, Pagidipati NJ, Lu MT, Mark DB, et al. Stress testing versus CT angiography in patients with diabetes and suspected coronary artery disease. J Am Coll Cardiol. 2019;73(8):893–902. doi: 10.1016/j.jacc.2018.11.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Oikonomou EK, Spatz ES, Suchard MA, Khera R. Individualising intensive systolic blood pressure reduction in hypertension using computational trial phenomaps and machine learning: a post-hoc analysis of randomised clinical trials. Lancet Digit Health. 2022;4(11):e796–805. doi: 10.1016/S2589-7500(22)00170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pallmann P, Bedding AW, Choodari-Oskooei B, Dimairo M, Flight L, Hampson LV, et al. Adaptive designs in clinical trials: why use them, and how to run and report them. BMC Med. 2018;16(1):29. doi: 10.1186/s12916-018-1017-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Center for Drug Evaluation, Research. Adaptive design clinical trials for drugs and biologics guidance for industry. U.S. Food and Drug Administration. FDA. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/adaptive-design-clinical-trials-drugs-and-biologics-guidance-industry. Accessed 1 June 2022.
- 105.Oikonomou EK, Thangaraj PM, Bhatt DL, Ross JS, Young LH, Krumholz HM, et al. An explainable machine learning-based phenomapping strategy for adaptive predictive enrichment in randomized controlled trials. medRxiv. 2023 doi: 10.1101/2023.06.18.23291542v1.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, et al. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374(14):1321–1331. doi: 10.1056/NEJMoa1506930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.SPRINT Research Group. Wright JT, Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fogel DB. Factors associated with clinical trials that fail and opportunities for improving the likelihood of success: s review. Contemp Clin Trials Commun. 2018;11:156–164. doi: 10.1016/j.conctc.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bentley C, Cressman S, van der Hoek K, Arts K, Dancey J, Peacock S. Conducting clinical trials-costs, impacts, and the value of clinical trials networks: s scoping review. Clin Trials. 2019;16(2):183–193. doi: 10.1177/1740774518820060. [DOI] [PubMed] [Google Scholar]
- 110.Moore TJ, Zhang H, Anderson G, Alexander GC. Estimated costs of pivotal trials for novel therapeutic agents approved by the US Food and Drug Administration, 2015–2016. JAMA Intern Med. 2018;178(11):1451–1457. doi: 10.1001/jamainternmed.2018.3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Moore TJ, Heyward J, Anderson G, Alexander GC. Variation in the estimated costs of pivotal clinical benefit trials supporting the US approval of new therapeutic agents, 2015–2017: a cross-sectional study. BMJ Open. 2020;10(6):e038863. doi: 10.1136/bmjopen-2020-038863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Khera R, Dhingra LS, Aminorroaya A, Li K, Zhou JJ, Arshad F, et al. Multinational patterns of second-line anti-hyperglycemic drug initiation across cardiovascular risk groups: a federated pharmacoepidemiologic evaluation in LEGEND-T2DM. medRxiv. 2022 doi: 10.1101/2022.12.27.22283968v1.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Khera R, Schuemie MJ, Lu Y, Ostropolets A, Chen R, Hripcsak G, et al. Large-scale evidence generation and evaluation across a network of databases for type 2 diabetes mellitus (LEGEND-T2DM): a protocol for a series of multinational, real-world comparative cardiovascular effectiveness and safety studies. BMJ Open. 2022;12(6):e057977. doi: 10.1136/bmjopen-2021-057977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Djolonga J, Yung J, Tschannen M, Romijnders R, Beyer L, Kolesnikov A, et al. On robustness and transferability of convolutional neural networks. In: 2021 IEEE/CVF conference on computer vision and pattern recognition (CVPR). 2021. p. 16453–63.
- 115.Khera R, Haimovich J, Hurley NC, McNamara R, Spertus JA, Desai N, et al. Use of machine learning models to predict death after acute myocardial infarction. JAMA Cardiol. 2021;6(6):633–641. doi: 10.1001/jamacardio.2021.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Volovici V, Syn NL, Ercole A, Zhao JJ, Liu N. Steps to avoid overuse and misuse of machine learning in clinical research. Nat Med. 2022;28(10):1996–1999. doi: 10.1038/s41591-022-01961-6. [DOI] [PubMed] [Google Scholar]
- 117.Guo LL, Pfohl SR, Fries J, Posada J, Fleming SL, Aftandilian C, et al. Systematic review of approaches to preserve machine learning performance in the presence of temporal dataset shift in clinical medicine. Appl Clin Inform. 2021;12(4):808–815. doi: 10.1055/s-0041-1735184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wong A, Otles E, Donnelly JP, Krumm A, McCullough J, DeTroyer-Cooley O, et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern Med. 2021;181(8):1065–1070. doi: 10.1001/jamainternmed.2021.2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lundberg SM, Erion G, Chen H, DeGrave A, Prutkin JM, Nair B, et al. From local explanations to global understanding with explainable AI for trees. Nat Mach Intell. 2020;2(1):56–67. doi: 10.1038/s42256-019-0138-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Linardatos P, Papastefanopoulos V, Kotsiantis S. Explainable AI: a review of machine learning interpretability methods. Entropy. 2020;23(1):18. doi: 10.3390/e23010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Diprose WK, Buist N, Hua N, Thurier Q, Shand G, Robinson R. Physician understanding, explainability, and trust in a hypothetical machine learning risk calculator. J Am Med Inform Assoc. 2020;27(4):592–600. doi: 10.1093/jamia/ocz229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Collins GS, Mallett S, Omar O, Yu L-M. Developing risk prediction models for type 2 diabetes: a systematic review of methodology and reporting. BMC Med. 2011;9:103. doi: 10.1186/1741-7015-9-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Collins GS, de Groot JA, Dutton S, Omar O, Shanyinde M, Tajar A, et al. External validation of multivariable prediction models: a systematic review of methodological conduct and reporting. BMC Med Res Methodol. 2014;14:40. doi: 10.1186/1471-2288-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. 2009;374(9683):86–89. doi: 10.1016/S0140-6736(09)60329-9. [DOI] [PubMed] [Google Scholar]
- 125.Wynants L, Van Calster B, Collins GS, Riley RD, Heinze G, Schuit E, et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Christodoulou E, Ma J, Collins GS, Steyerberg EW, Verbakel JY, Van Calster B. A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. J Clin Epidemiol. 2019;110:12–22. doi: 10.1016/j.jclinepi.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 127.Collins GS, Dhiman P, Andaur Navarro CL, Ma J, Hooft L, Reitsma JB, et al. Protocol for development of a reporting guideline (TRIPOD-AI) and risk of bias tool (PROBAST-AI) for diagnostic and prognostic prediction model studies based on artificial intelligence. BMJ Open. 2021;11(7):e048008. doi: 10.1136/bmjopen-2020-048008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rajkomar A, Hardt M, Howell MD, Corrado G, Chin MH. Ensuring fairness in machine learning to advance health equity. Ann Intern Med. 2018;169(12):866–872. doi: 10.7326/M18-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mehrabi N, Morstatter F, Saxena N, Lerman K, Galstyan A. A survey on bias and fairness in machine learning. arXiv [cs.LG]. 2019. http://arxiv.org/abs/1908.09635.
- 130.Duffy G, Clarke SL, Christensen M, He B, Yuan N, Cheng S, et al. Confounders mediate AI prediction of demographics in medical imaging. NPJ Digit Med. 2022;5(1):188. doi: 10.1038/s41746-022-00720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gichoya JW, Banerjee I, Bhimireddy AR, Burns JL, Celi LA, Chen L-C, et al. AI recognition of patient race in medical imaging: a modelling study. Lancet Digit Health. 2022;4(6):e406–e414. doi: 10.1016/S2589-7500(22)00063-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Center for Devices, Radiological Health. Clinical decision support software—guidance. U.S. Food and Drug Administration. FDA; 2022. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-decision-support-software. Accessed 21 July 2023.
- 133.Johnston JL, Dhruva SS, Ross JS, Rathi VK. Clinical evidence supporting US Food and Drug Administration clearance of novel therapeutic devices via the de novo pathway between 2011 and 2019. JAMA Intern Med. 2020;180(12):1701–1703. doi: 10.1001/jamainternmed.2020.3214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kadakia KT, Dhruva SS, Caraballo C, Ross JS, Krumholz HM. Use of recalled devices in new device authorizations under the US Food and Drug Administration’s 510(k) pathway and risk of subsequent recalls. JAMA. 2023;329(2):136–143. doi: 10.1001/jama.2022.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Amann J, Blasimme A, Vayena E, Frey D, Madai VI, Precise4Q Consortium Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak. 2020;20(1):310. doi: 10.1186/s12911-020-01332-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yao X, Rushlow DR, Inselman JW, McCoy RG, Thacher TD, Behnken EM, et al. Artificial intelligence-enabled electrocardiograms for identification of patients with low ejection fraction: a pragmatic, randomized clinical trial. Nat Med. 2021;27(5):815–819. doi: 10.1038/s41591-021-01335-4. [DOI] [PubMed] [Google Scholar]
- 137.He B, Kwan AC, Cho JH, Yuan N, Pollick C, Shiota T, et al. Blinded, randomized trial of sonographer versus AI cardiac function assessment. Nature. 2023;616(7957):520–524. doi: 10.1038/s41586-023-05947-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–657. doi: 10.1056/NEJMoa1611925. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Strengths and weaknesses of commonly used metrics in machine learning.
Data Availability Statement
Not applicable.