Abstract
Introduction:
Spontaneous recanalization of an occluded internal carotid artery (ICA) is thought to be unlikely. However, there has been a growing number of reports describing this phenomenon. Despite this, the frequency, time course, and mechanism of spontaneous recanalization remain unknown. In this paper, we describe a patient with a symptomatic recanalization of an occluded left ICA.
Case Report:
A 70-year-old woman presented with transient speech arrest and right upper extremity weakness related to an occluded ICA. After 3 days, her weakness and aphasia reappeared and worsened transiently. A repeat computed tomography angiography revealed recanalization of the occluded ICA, as well as new ischemic changes in the previously hypoperfused left insular region. This finding changed the management from medical management to revascularization with a stent, after which the patient was discharged home with acetylsalicylic acid and clopidogrel.
Conclusions:
Although previously thought to be a rare occurrence, spontaneous recanalization is not uncommon. Further research into this phenomenon as proper identification and characterization of this phenomenon can influence follow-up and management.
Key Words: ischemic stroke, recanalization, internal carotid artery occlusion
Cervical internal carotid artery (ICA) stenosis is a risk factor for ischemic strokes through artery-to-artery embolization. Current recommendations indicate urgent carotid endarterectomy or stenting [carotid artery stenting (CAS)] in a recently symptomatic patient with >50% stenosis.1 Once completely occluded (ie, 100% stenosis), ICAs are typically not recommended for routine reimaging or revascularization, as it is assumed that the artery can no longer be a source of artery-to-artery embolization.2 However, there exist previously documented instances of symptomatic recanalization.3–6 Due to the relative paucity of recorded recanalization events outside of case series and individual case reports, the exact mechanism, time course, and prevalence of events are currently unclear. Nevertheless, these events may prove to be more common than originally estimated, particularly due to the lack of consensus regarding follow-up imaging. In this case report, we describe a patient who presented with a symptomatic recanalization of a previously occluded ICA. The patient consented to have her case published.
CASE REPORT
A 70-year-old woman with a past medical history significant for hypertension presented to the emergency department with a chief complaint of transient speech arrest and right upper extremity weakness lasting for 10 minutes. Her neurological assessment after symptom resolution was remarkable for decreased pin-prick appreciation over the right arm and leg. Upon imaging, her computed tomography head revealed left parietal lobe hypodensities in a watershed appearance. In addition, computed tomography angiography (CTA) revealed an occluded left ICA with distal reconstitution at the petrous segment (Fig. 1A). At the time of presentation, she was deemed not a candidate for tissue-type plasminogen activator or endovascular thrombectomy was given the mild nature of her deficits. She was administered acetylsalicylic acid (ASA) 160 mg and clopidogrel 300 mg (dual antiplatelet therapy) and admitted for further workup and monitoring. On her workup, the transthoracic echocardiogram was unremarkable, HbA1c was 5.0%, and low-density lipoprotein was 2.0 mmol/L, for which she was initiated on Rosuvastatin 20 mg PO daily.
FIGURE 1.
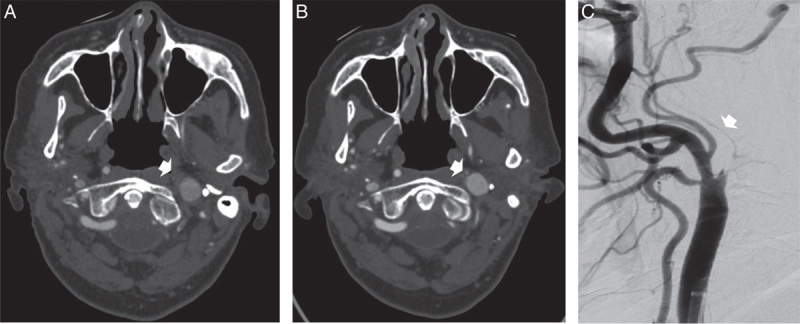
Brain computed tomography angiography (CTA) and angiography. (A) Arrowhead shows occluded left internal carotid artery (ICA) at initial presentation. (B) Arrowhead shows spontaneously recanalized ICA upon repeat CTA 3 days after initial presentation. (C) Arrow shows narrow channel of blood flow in recanalized ICA during angiography.
Three days after admission, the patient had another event of transient right upper extremity weakness and worsening aphasia. A repeat CTA was ordered, which revealed a small channel of recanalization in the left ICA (Fig. 1B), as well as new ischemic changes in the left insular region. She underwent a cerebral angiogram the same day and a stent was successfully placed in the left ICA (Fig. 1C). She was discharged home with ASA 81 mg and clopidogrel 75 mg for 3 months, followed by ASA indefinitely.
DISCUSSION
Although thought to be unlikely, spontaneous recanalization of an occluded ICA is not an uncommon event. The highest incidence found through a literature search was within a population of 30 patients with ICA occlusion, where 12 patients presented with recanalization (40%).7 Other reports cite slightly more conservative rates in their populations, ranging from 2.3% to 10.3%.6,8,9 Unfortunately, the exact incidence and timing of recanalization cannot be confirmed, as both are highly contingent on the degree of follow-up. Among reports, the length of time for follow-up varied widely, from days,8,10 to weeks,3,7,11,12 to years.5,6,9 Moreover, within these time periods, the true timeline of recanalization with respect to the timing of imaging is unknown. As the individual sampling methods were mostly arbitrary, the data would be more reliable if patients are followed for longer periods of time and/or in more regular intervals in future studies.
Identification and diagnosis of ICA stenosis and recanalization can be achieved with magnetic resonance imaging, CTA, and ultrasound (US). Currently, CTA is the gold standard to confirm occlusion, identify a small channel, and offer intervention. However, US modalities have high diagnostic sensitivity, with the additional advantage of being nonionizing and cost-effective compared with magnetic resonance imaging or CTA.13,14 In the context of recanalization, where the exact time course is not yet known, US may be the easier and more resource-friendly method of diagnosis. In addition, it may offer a further advantage in imaging real-time flow to identify “trickle flow” in near-occluded vessels.
Currently, there are no recommendations or consensus guidelines for management after recanalization. Reported cases have been treated with both medical interventions, such as ASA, antiplatelets, and anticoagulants, and surgical interventions such as carotid endarterectomy and CAS. An acute symptomatic recanalized ICA would warrant consideration of revascularization and ideally needs to occur within 2 weeks of initial presentation.1 This timeline further emphasizes the importance of being able to identify recanalization soon after the presentation. In our case, the patient underwent CAS with follow-up medical management. Although the patient recovered well with no short-term complications, it is unclear whether surgical interventions would improve long-term morbidity and mortality outcomes in this population.
CONCLUSIONS
In summary, we describe a case of spontaneous recanalization of a recently occluded symptomatic ICA. This finding changed the management of the patient from medical management to revascularization. Although previously thought to be a rare occurrence, spontaneous recanalization is not uncommon and has been described in multiple reports. Prospective studies are required to establish the prevalence, time course, and optimal investigation modality for follow-up, and management.
Footnotes
The authors declare no conflict of interest.
Contributor Information
Sarah Y. Zhang, Email: sarah.zhang3@mail.mcgill.ca.
Dylan Blacquiere, Email: dblacquiere@toh.ca.
Brian Dewar, Email: bdewar@toh.ca.
Grant Stotts, Email: gstotts@toh.ca.
Dar Dowlatshahi, Email: ddowlat@toh.ca.
REFERENCES
- 1. Gladstone DJ, Lindsay MP, Douketis J, et al. Canadian stroke best practice recommendations: secondary prevention of stroke update 2020. Can J Neurol Sci. 2021;49:315–337. [DOI] [PubMed] [Google Scholar]
- 2. Gomensoro J, Maslenikov V, Azambuja N, et al. Joint study of extracranial arterial occlusion: VIII. Clinical-radiographic correlation of carotid bifurcation lesions in 177 patients with transient cerebral ischemic attacks. J Am Med Assoc. 1973;224:985–991. [DOI] [PubMed] [Google Scholar]
- 3. Nguyen-Huynh MN, Lev MH, Rordorf G. Spontaneous recanalization of internal carotid artery occlusion. Stroke. 2003;34:1032–1034. [DOI] [PubMed] [Google Scholar]
- 4. Fieschi C, Bozzao L. Transient embolic occlusion of the middle cerebral and internal carotid arteries in cerebral apoplexy. J Neurol Neurosurg Psychiatry. 1969;32:236–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Markwalder TM, Starrett RW, Mumenthaler M. Spontaneous bilateral recanalization in bilateral internal carotid artery occlusion. Stroke. 1980;11:95–98. [DOI] [PubMed] [Google Scholar]
- 6. Morris-Stiff G, BCh M, Teli M, et al. Internal carotid artery occlusion: its natural history including recanalization and subsequent neurological events. Vasc Endovascular Surg. 2013;47:603–607. [DOI] [PubMed] [Google Scholar]
- 7. Bogousslavsky J, Despland PA, Regli F. Spontaneous carotid dissection with acute stroke. Arch Neurol. 1987;44:137–140. [DOI] [PubMed] [Google Scholar]
- 8. Meves SH, Muhs A, Federlein J, et al. Recanalization of acute symptomatic occlusions of the internal carotid artery. J Neurol. 2002;249:188–192. [DOI] [PubMed] [Google Scholar]
- 9. Camporese G, Labropoulos N, Verlato F, et al. Benign outcome of objectively proven spontaneous recanalization of internal carotid artery occlusion. J Vasc Surg. 2011;53:323–329. [DOI] [PubMed] [Google Scholar]
- 10. Calleja S, De La Vega V, Llaneza JM, et al. Spontaneous recanalization of acute internal carotid artery occlusion. Ann Vasc Surg. 2004;18:490–492. [DOI] [PubMed] [Google Scholar]
- 11. Lehrer GM. Arteriographic demonstration of collateral circulation in cerebrovascular disease. Neurology. 1958;8:27–32. [DOI] [PubMed] [Google Scholar]
- 12. Parenti G, Marconi F, Canapicchi R, et al. Spontaneous recanalization of carotid artery occlusion following non traumatic dissection. Ital J Neurol Sci. 1989;10:361–367. [DOI] [PubMed] [Google Scholar]
- 13. Sturzenegger M, Mattle HP, Rivoir A, et al. Ultrasound findings in carotid artery dissection: analysis of 43 patients. Neurology. 1995;45:691–698. [DOI] [PubMed] [Google Scholar]
- 14. Nederkoorn PJ, Van Der Graaf Y, Hunink MGM. Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis: a systematic review. Stroke. 2003;34:1324–1332. [DOI] [PubMed] [Google Scholar]


