ABSTRACT
General primary care workers and family physicians are a crucial work force in managing the mental health of people in any given region. However, the barriers they face in low- and middle-income countries (LMICs) may be worsened by the pandemic. This review aims to bring together evidence about mental health treatment challenges experienced by people in LMICs in primary care settings. The review focuses on the shortage of essential mental healthcare services, stigma and lack of competent primary care professionals in establishing these services and their importance in the COVID-19 pandemic context. The systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and the search strategy included keyword search terms (MeSH) to perform a search across three electronic databases - Critical Appraisal Skills Program assessed PubMed, SpringerLink, and Cochrane and quality of the articles. The articles selected were analyzed through thematic analysis to identify the main themes and conclude our findings. Findings indicate that out of 1792 publications found, 14 studies matched the desired criteria for the studies. Endnotes, database search filters, and Covidence data extraction tools were used to generate the relevant articles in this study. This study shows that primary care institutions have financial and management issues in providing mental health services and a shortage of competent mental health experts in primary care, especially mental health–trained family physicians. The study also identifies community stigma as the most prevalent barrier to seeking mental health therapy, reflecting the lack of community health education in LMICs.
Keywords: Covid-19, mental health, primary care
Introduction
Mental health is a condition of well-being in which each person reaches their maximum capabilities, deals with daily problems, works effectively, and gives back to their community (Roberts, 2018). Mental health is a crucial element of total health, but healthcare institutions have not adequately addressed the issue.[1] Most of the population with mental health issues, such as anxiety disorders, behavioral and emotional disorders in children, bipolar affective disorder and depression in low- and middle-income countries (LMICs) do not receive their mental health support due to defined and undefined barriers.[2] This review refers to anxiety, depression, and psychiatric illness like schizophrenia, bipolar disorders, and substance abuse-related mental health disorders as mental health issues. These mental health problems increase the disease burden in LMICs. It is anticipated that by 2030, schizophrenia, depressive disorders, bipolar, and health-related issues in LMICs will account for 19.1% of the mental health disorders.[3] On the other hand, cultural and social factors such as stigmatization, discrimination and some beliefs in superstitions contribute significantly to the burden of mental health disease in the population. Our review demonstrates that LMICs receive inadequate resources, and there is a need to address funding issues for mental health education.
It is an understatement that COVID-19 has disrupted global activities as we know it (international travel, workplace ethics, food supply and distribution, and corporate protocols, among others) with its various impacts still unclear at this point.[4-6] It is more than ever important to improve and implement mental health services in primary care in LMICs as COVID-19 is having a significant impact on the mental health of our communities. Stress levels have increased significantly; people are in fear and uncertainty about their own and their loved ones’ health. Employment issues are rising, leading to increased poverty and substance abuse cases resulting from social isolation and depression.[7] This study will help identify the current obstacles as studies from the 2000s are included here.
Family physicians and primary care workers also have several impediments to effectively work within LMIC institutions. Some recent studies have reported several barriers (Kamvura et al., 2022)[8] but are still poorly understood. These professionals provide critical healthcare services to a range of patients regardless of resource shortages (Pokhrel et al., 2021).[9] The lack of existing literature on the primary care practitioners’ abilities and knowledge in mental health and competencies in LMICs can lead to severe impairment and a significant health burden on LMICs as a post-pandemic consequence, as recently posited in this review.[10] This submission uses the PCIO framework to assess this area of interest. It anticipates that LMIC governments and policymakers will take critical steps in a post-COVID world toward mitigating the adverse effects and increasing the productivity of primary care professionals.
Materials and Methods
Data collection and search strategy
The systematic review was done in June 2021, and the results were updated in November 2021 using a search strategy developed by the student and with the supervisor’s assistance. Three databases, namely, PubMed, Springer Link, and Cochrane, were .searched and the originality of the project was ensured [Appendix 1]. The search strategy was conducted using the following approach:
a. Identifying key terms and keywords
Keywords and key terms were identified in searching the identified databases following a previous study[11] [Table 1a]. Boolean operators were used in combining the search terms, and it was useful in combining specific search terms and broadening or narrowing them. For example, the search for MeSH terms [Table 1b] using search tools used the field section to identify the terms and search for title, abstract and keywords.
Table 1a.
Keyword identification for this study
| Concept 1 | Concept 2 |
|---|---|
| Various free tests and vocabularies | Low- and middle-income countries |
| In search terms such as: | Mental health treatment |
| Mental health, schizophrenia, anxiety, bipolar and depression | Substance abuse |
Table 1b.
Detailed search engine algorithms used in this review
| MeSH | Searches=Sn | |
|---|---|---|
| PubMed | Mental health illness, Mental health treatment, Primary care physicians, GP, Primary care, Doctors, Barriers, Low-income countries, Low middle-income countries | S11 S3 AND S6 AND S10 Search modes Boolean/Phrase |
| S10 S7 OR S8 OR S9 | ||
| S9 ((“mental health” n3 service*) OR counseling) | ||
| S8 (MH “Gaps, barriers, hurdles, issues faced+”) | ||
| S7 (MH “Mental Health Services+”) OR (MH “Community | ||
| Mental Health Services”) | ||
| S6 S4 OR S5 | ||
| S5 “overdose*” or “substance abuse” S4 (MH “Drug Abuse”) OR (MH “Substance Abuse, Intravenous”) OR (MH “Substance Abuse, Oral”) OR (MH | ||
| “Alcohol-Related Disorders”) S3 S1 OR S2 | ||
| S2 (“Primary care*” OR “GP*” OR “Family physician*”) | ||
| S1 (MH “Low Middle Income Countries, LMIC, Low Income, Middle income”) | ||
| Cochrane | Mental health illness, Mental health treatment, Primary care physicians, GP, Primary care, Doctors, Barriers, Low-income countries, Low middle income countries | S10 S7 OR S8 OR S9 |
| S9 ((“mental health” n3 service*) OR counseling) | ||
| S8 (MH “Counseling+”) | ||
| S7 (MH “Mental Health Services+”) OR (MH “Community Mental Health Services”) | ||
| S6 S4 OR S5 | ||
| S5 “overdose*” or “substance abuse” | ||
| S4 (MH “Drug abuse”) OR (MH “Substance Abuse, Oral”) OR (MH “Alcohol-Related Disorders”) | ||
| S3 S1 OR S2 | ||
| S2 (“Primary Care*” OR “Primary Care Providers*” OR “General Practitioners*”) | ||
| S1 (MH “Gaps, Barriers to Treatments, Hurdles”) | ||
| Springer Link | Mental health illness, Mental health treatment, Primary care physicians, GP, Primary care, Doctors, Barriers, Low-income countries, Low middle-income countries | S4 |
| S1 AND S2 AND S3 | ||
| S3 (DE “Mental Health Services” OR DE “Community Mental Health Services” OR DE “Psychological First Aid” OR DE “Counseling” OR DE “Community Counseling” OR DE “Cross Cultural Counseling” OR DE “Group Counseling” OR DE | ||
| “Multicultural Counseling” OR DE “Psychotherapeutic Counseling” OR DE “Rehabilitation Counseling”) OR ((“mental health” n3 service*) OR counseling) S2 (DE “South Asian Cultural Groups”) OR (“South Asian*” OR | ||
| “Asian American*” OR “Asian Canadian*”) S1 | ||
| ((DE “Substance Use Prevention” OR DE “Substance Abuse and Addiction Measures” OR DE “Drug Abuse” OR DE “Substance Use Treatment” OR DE “Drug Overdoses” OR DE “Alcoholism”) OR (overdose* OR “substance abuse” or alcohol*) |
The Boolean operator was used to differentiate the concepts or the search terms using “OR” and “AND”, combine all the individual search terms for concept 1 with OR other concepts; alternatively, combine all the individual search terms for concept 1 AND concept 2
Search filters
After identifying search terms, we applied additional search filters (inclusion and exclusion criteria) to narrow down the search and make it easier to locate relevant articles. We used the filter slide bar on the left side of the screen to refine our search in the PubMed database, such as article type, publication year, language, and so on. We narrowed our search by including and excluding criteria such as “qualitative studies”, “English publishing” from 2000 onwards, “mental health treatment gaps”, “primary care”, and so on [Table 2]. A similar filter using inclusion and exclusion strategy was also used for Springer Link and Cochrane database search. The inclusion and exclusion criteria that guided the filtering process was carried out following the method set by Patino and Ferreira.[12]
Table 2.
Inclusion and exclusion criteria for the study
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Published after 2000 | Published before 2000 |
| Published in the English Language | Published in other languages other than English |
| Qualitative Design | Quantitative design- Limit the number of articles due to lack of time |
| Peer-Reviewed Journals | Grey Literature, conferences proceedings, reports, Wikipedia. |
| Target population are people with mental disorders/Primary care providers | Target population are people with illness other than mental health-related/Tertiary care providers |
| The focus is on the LMICs | The focus is on the high-income countries |
| Relate to search questions and concepts | Does not relate to search questions and concepts. |
Adopted Inclusion and Exclusion Criteria (Patino and Ferreira, 2018)[12]
Search limits in the databases
Once the final search was done, the researcher combined all of the ideas with AND; we improved the search outcome further to focus on the date of publication and the study design.[13] The search was also limited to only studies about mental health and focusing on LMICs [Figure 1]. This study had other limitations, including only three databases (PubMed, Springer Link and Cochrane) being used and searched, leaving other credible and reliable databases such as Embase and MEDLINE due to lack of available resources and limited time available to conduct the research. Secondly, the articles were only limited to those published after 2000, which locks out recorded information before then due to focus on COVID-19 that required the latest study articles. Lastly, all of the pieces selected for this study were published in English to avoid the challenges that can occur because of translation.
Figure 1.

Medical subject headings and search database and search terms chart
Data extraction and synthesis
After applying screening filters through inclusion eligibility, the remaining articles were imported into EndNote. After further screening for duplicates and of abstracts and titles, the remaining articles were transported into Covidence software for data extraction purposes.[14] Research titles and types with the year of publication and where the study was conducted, along with population, barriers and challenges to mental health in LMICs were highlighted in the research studies for data extraction through the Covidence data extraction tool [Table 3].
Table 3.
Barriers to mental health treatment in family practice in LMICs. Characteristics of included studies with original text for data extraction from original articles with references
| Lead author, year, country, and setting | Study aim | Study design | Facility type | Participants/sample size | Data collection methods | Mental health type | Barriers (address barriers only) |
|---|---|---|---|---|---|---|---|
| Aggarwal (2020) (1) India (LMIC) | To examine perspectives and explanatory styles of youth with self- harm and their caregivers to inform the design of evidence-based PI in a non- Western, cultural setting. To enhance acceptability by recommending ways for the integration of local practices and traditions | Qualitative | Psychiatry department of a tertiary hospital located in Mumbai, India | 19 young adolescents and their caregivers | Interviews | Self-harm, suicide | This research identified barriers against self-harm reduction, which include scarcity of research-based evidence of self-harm reduction in LMICs; contextual, interpersonal, intrapersonal, and sociocultural self-harm, formulation and current sentiments; family members and friends as perceived determinants of self-harm possibility in the future; adverse treatment experiences and ineffective coping mechanisms |
| Bhat (2020) (2) India (LMIC) | a) To explore barriers to accessibility of mental health treatment b) To evaluate the reasons for poor adherence to follow-up and medication among women with MDD c) To assess barriers to accessibility of mobile mental health services | Cross-sectional study | Community rural mental health program | 69 rural women aged 18–85 enrolled in the community health program | Focus group discussions | Major depressive disorder (MDD) | Barriers to accessing mental health services using mobile phones identified in this study included culture-driven, faulty attribution of psychiatric disorders, e.g., to fate, problems with in-laws, alcohol abusive husbands, etc.; unwillingness or inability to identify depression in presence of physical symptoms; denial of the need despite acknowledgment of depression symptoms; lack of family support; fear of condescending mental health provider’s response leading to underreporting of medication side-effects; financial loss from unpredictable clinic wait and commute times, and unreliable public transportation; limited personal access to mobile phones; preference for an in-person clinical consultation; unfamiliarity with the use of mobile devices; inadequate literature on mental health service delivery in rural areas using mobile health platforms, workforce deficits; and systemic barriers such as poor transportation and infrastructure |
| Blixen (2020) (3) Tanzania (LMIC) | To identify real-time barriers to medication adherence, use of long-acting injectables, and management of chronic psychotic disorders | Qualitative cross-sectional study | Community | 44 participants (patients) with CPD, caregivers, mental healthcare providers | In-depth interviews and focus group discuss ions | Chronic psychotic disorders | This research revealed two inter-linked barriers to mental health treatment which included widespread poor medication adherence, and the resulting relapse that in turn reinforced poor medication adherence |
| Brown (2019) (4) (Lebanon and Jordan) (LMIC) | To reduce barriers to providing accessible, quality mental healthcare for young adolescents affected by mental health disorders through the WHO’s Early Adolescent Skills for Emotions (EASE) psychological intervention for young adolescents | Scope study | Community and regions containing vulnerable populations of refugees, minorities, and immigrants | 445 | Randomly sized group treatment trials | Early adolescent mental health disorders | Important barrier which was identified and dealt with elaborately in this research was psychological distress arising from internalization of feelings in young adolescents. Other barriers unique to countries with a majority of war-induced displacement included poverty, inadequate protection, community violence, inaccessibility to services, etc.; Existing mental health programs have been either too specific to certain disorders or require specialized mental health training and caregivers |
| S. Evans-Lacko (2018) (4) Colombia, Iraq, Nigeria, People’s Republic of China, Peru, Ukraine, Brazil, Bulgaria, Medellin Colombia, Lebanon, Mexico, Romania, South Africa (LMICs) | To examine the treatment gap between the number of people with mental disorders and the number treated, by socioeconomic status and service sector | Qualitative cross-sectional, interventional study | None | 16,753 | Community surveys and interviews | Adult separation anxiety disorder, agoraphobia, generalized anxiety disorder, panic disorder, post-traumatic stress disorder, social phobia, specific phobia, bipolar mood disorder I, bipolar mood disorder II, sub-threshold mood disorder, dysthymic disorder, major depressive episode (MDE), alcohol abuse or dependency, illicit drug abuse or dependency | This research concluded that obstacles to seeking specialized mental health treatment included poor socioeconomic status; inadequate healthcare spending on treatment services; the perception that low illness severity does not warrant access to specialized mental health treatments; a dearth of specialist mental health (SMH) treatment resources; and SMH treatment shelved for only severe-to-complex cases |
| Ezeanolue (2020) (6) Nigeria (LMIC) | To identify the challenges and opportunities related to integration of mental healthcare into existing HIV programs in Nigeria | Scope study | Nigeria Implementation Science Alliance (NISA) 2019 conference | N/A | N/A | Mental health in HIV patients | Stigma, policy and research gaps were concluded as the most critical barriers to seeking mental health treatment |
| Hanlon (2017) (7) (LMIC) | To address evidence-based gaps in task-sharing mental healthcare for patients of SMI | Policy review | N/A | N/A | N/A | Severe mental illness | This study observed that the rural population relatively preferred mental health treatment much less than the urban population. Another reason for reduced access to mental health treatment was the lack of primary care services and professionals in mental health services |
| Knapp (2006) (20) Ethiopia, Zambia, Nepal, Mongolia, Tanzania, West Bank and Gaza, and Malawi (LMIC) | To discuss economic barriers to improving the availability , accessibility, efficiency and equity of mental healthcare in LMICs | Policy review | N/A | N/A | N/A | Depression, schizophrenia, Alzheimer’s disease, child behavioral disorders, chronic anxiety disorders | This study was able to bring to light several barriers to mental health treatment access. These included the inapplicability of mental treatment evidence collected from high- income countries to LMICs; failure to benefit from existing research activities due to clinical and system-level decision-makers’ unawareness and perceived lack of value of such activities; the resulting poor quality of practice and finance allocation to more common, prevalent, severe or emergent disorders; highly centralized fund collection and allocation, tedious administrative procedures in fund redirection; restrictions to flow of finance from the less necessary in-patient psychiatric facilities to the more effective community-based options; poor resource management within LMICs; unequal urban/rural resource distribution; highly institutionalized facilities such as asylums are far removed from population lefts or that access to highly institutionalized mental health resources depend on policy decisions approved by clinicians/managers in charge; existing facilities non-conducive to mental health improvement due to overcrowding, poor quality care and human rights abuse; overfunding of costly technology; disincentivizing schemes where the improvement in mental disorder translates into a loss of social security or welfare benefits; poor coordination across agencies; delayed resource timing; and training delays |
| Kola (2020) (9) Nigeria (LMIC) | To identify factors influencing health service utilization for adolescent perinatal depression in Nigeria to inform new strategies of care delivery | Qualitative | Primary healthcare facilities | 42 participants | Purposive sampling; data collected using focus group discussions (FGDs); semi-structured interview | Perinatal depression | Disablers of mental health access detected in this research were the all-too-common social stigma from family and neighbors, self-blame, poor behavior of and disdain from healthcare providers toward young mothers; unawareness of depression symptoms; lack of mother’s autonomy, long wait times at the healthcare facilities; and absent parental support of mothers |
| Luitel (2020) (18) Nepal (LMIC) | To assess service users’ and caregivers’ perceptions of mental health services provided by trained primary healthcare workers in Nepal | Qualitative | Primary care-based mental health facilities | 81 | Semi-structured interview | Depression, psychosis, alcohol use disorder | This study cataloged numerous impedances to accessing mental health treatment which included distance to mental health service; transportation expenses; servicing by private hospitals more inconvenient than that by primary care; the frequent transfer of trained health workers; eventual non-availability of the same healthcare provider at follow-ups; frequent unavailability of medicines or non-availability of required medicines or irregular supply; lack of a confidential space for consultation and counseling in health facilities; demoralizing behavior, failure to value confidentiality, lack of punctuality, and no counseling by some health workers; assurance of job security of healthcare providers, irrespective of performance; stigmatizing to the extent of human rights violation in family or community; and patient’s inability to afford the treatment cost |
| Qin (2020) (17) China (LMIC) | To investigate potential causes of treatment gap from the perspective of economics: (1) Why so many people with mental illness go untreated; (2) How to bridge the treatment gap for them | Economic review - Evaluation | N/A | N/A | N/A | N/A | Obstacles to the use of mental health treatment as noted in this research included high non-monetary cost due to stigma; insufficient public funds devoted to mental health; the resulting out-of-pocket fees of mental healthcare; time wastage in seeking already scarce mental health services in traveling, waiting, and receiving treatment; insufficient mental healthcare personnel and services available due to inadequate training; unfair geographic distribution of mental health resources; distrust in treatment effectiveness due to outdated treatment; slow integration (up to 7 years) into the practice of new medical knowledge and technology resulting from underfunding and administrative steps; underpaid healthcare providers; and eventual drug prescription determined by profit margins |
| Trop J (2018) (12) Mongolia (LMIC) | To elucidate perspectives and experiences of Mongolian healthcare providers regarding PPD | Qualitative | Tertiary hospital | 15 including nurses, midwives, family clinic nurses, ob-gyn physicians, family physicians, psychologist, monk, traditional healer | The interview was focused groups discuss ions | Postpartum depression | This study recognized mental healthcare providers’ lack of confidence in identifying and treating PPD; lack of training and time constraints |
| Woods-Jaeger (2017) (13) Tanzania & Kenya (LMICs) | To explore facilitators, barriers, and strategies used to deliver child mental health evidence-based treatment (EBT), trauma-focused cognitive behavioral therapy (TF- CBT), in a culturally responsive manner | Qualitative | Large, randomized, controlled trial of TF-CBT | 12 TF-CBT lay counselors | Semi-structured interviews | General mental health | This study re-emphasized and revealed barriers to mental health services unique to children which included the culturally intrinsic disregard for the existence of negative feelings and insecurity in children; the paling of mental healthcare importance in the setting of families unaffordability of basic school supplies; shortage of mental health professionals and the oft-ignored lack of emotional sustainability tools for counselors to deliver quality mental healthcare (EBT-TF- CBT) |
| Wood (2021) (14) India (LMIC) | To understand the barriers and facilitators that lay health workers (LHWs) face in delivering mental healthcare | Qualitative | Non-governmental organizations | 32 | Semi-structured interview | General mental health | This research made note of inhibitors of mental health access which included the treatment gap for mental disorders common to all LMICs, and deficient research into task-sharing experiences of lay mental healthcare providers |
Data analysis strategy
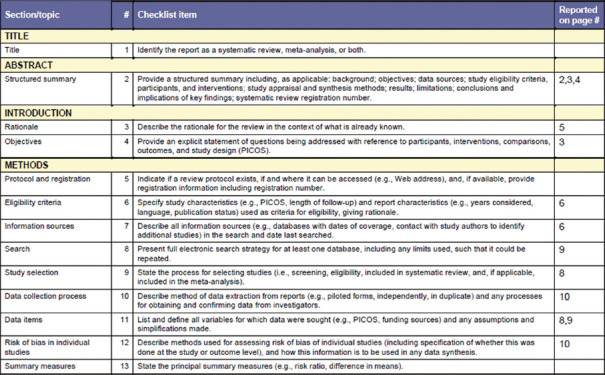
The data was analyzed using the “best fit” framework synthesis and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [Figure 2]. The steps in the best fit framework are a systematic identification of relevant primary research studies, the identification of relevant publications using search strategy, the extraction of data based on characteristics identified in the appraisal for quality, coding of the evidence, creation of new themes by conducting thematic analysis on the evidence and producing a new framework composed of a prior and new themes supported by the evidence. The key study also used main articles selected in the scanning search and created an all-inclusive search strategy that involved appropriate text-word and therapeutic subject[15] [Figure 1].
Figure 2.
PRISMA Checklist
In the analysis, we employed two approaches, the SURE and COM-B models, as complementary frameworks to achieve the study’s aims. The Seemingly Unrelated Regression Equations (SURE) model is used to validate the identification of barriers to mental health treatment, but it fails to offer procedures for addressing those barriers.
On the other hand, the Capability, Opportunity, and Motivation Model of Behavior (COM-B) offers a model of understanding the behavior of the communities and primary healthcare providers. Therefore, we used this model [Figure 3], which connected the two frameworks and enabled the identification of the barriers previously used in another similar study [Additional File 2] Wakida et al. 2018.[10] Shows classification of the barriers in line with the COM-B attributes and actionable options, which makes sense compared to when looked only with the SURE framework. In this approach, we found a comparable survey to identify challenges to mental healthcare services in LMICs.
Figure 3.
SURE/COM-B hybrid framework developed by the authors
Result
Study selection
The internet and database search resulted a total of 1,792 studies from PubMed (n = 1,120), Cochrane (n = 457), and Springer Link (n = 215). Other additional materials from the World Health Organization (WHO) (n = 13) and grey sources were included (n = 23). Therefore, the total number of articles searched in this process were 1,828. A total of 109 articles were removed because of duplication and the remaining (n = 1719) were screened.
Further screening of the 34 articles after database filters was based on the abstract and the title through Covidence data extraction, which yielded in the removal of 20 articles; the primary reason for elimination was that these articles were not directly related to mental health issues or mental health treatment or its barriers, or its studies were not conducted in a primary healthcare setting. The research remained with only 14 articles that met all of the inclusion criteria. The selection is explained in the PRISMA flowchart [Figure 4].
Figure 4.

Developed PRISMA flowchart
Study characteristics
Finally, 14 articles were selected for the analysis, and it included qualitative and cross-sectional studies, which combined both the qualitative and quantitative design. The analysis of the qualitative studies was done using a descriptive approach and thematic analysis[16] [Figure 4]. These studies were from LMICs, including India, Tanzania, Nigeria, Mongolia, China, South Africa, Nepal, Lebanon, and Jordan. These articles described the primary care providers, social, economic, and cultural barriers to mental health issues treatment in LMICs. These articles were published after 2000 to provide the most relevant information, including our interest in the COVID-19 context.
Quality of articles included
All of the articles included in the study were quality and were assessed using the Critical Appraisal Skills Programme (CASP) Systematic Review checklist [Additional File 1]. They had clear research objectives and research designs, and the strategies used in the recruitment were appropriate in addressing the aims of the research. In these studies, the most common method was qualitative, and others used cross-sectional data analysis methods, except two articles that had no specific target population or a country and one article from the WHO that focused on general LMICs.[17] The primary community obstacle in mental health was stigma and a lack of community health education (n = 7) [Figure 3].[18] Affordable and cost-effective mental health therapies may be offered via collaborative care interventions in primary care, resulting in improved overall health outcomes and cost-effectiveness (n = 8). The WHO designed the SURE framework, containing 28 areas, to achieve health reforms in Africa (World Health Organization, n.d.). These areas are divided into five categories: (a) care recipients, (b) care providers, (c) other stakeholders, (d) health system restrictions, and (e) social and political restrictions[19]; these areas complimented with COM-B to find the desired objectives of this study.
Discussion
The studies were reviewed to investigate the challenges and the measures that should be implemented to increase access to mental health treatment.[10,20,21] From this systematic review process, it was also established that several studies that examined the challenges to mental healthcare services[22-25] and the importance of addressing these problems had been done. However, it was also evident that some gaps in the barriers needed to be explored, especially for LMICs.[10] Hence, we focused on the main factors that affected access to mental healthcare services, specifically in LMICs. The identified barriers to a community’s access to mental healthcare include the attitude toward mental health issues, the acceptance of the problem’s existence, and the credibility of the healthcare centers. Again, it was established that knowledge and skills concerning mental health contribute significantly; a lack of sufficient knowledge about mental health issues results in stigmatization. The motivation to change, the financial resources and management and leadership are the main themes. These barriers and facilitators are discussed below.
Social-cultural factors
The main barriers to accessing mental healthcare treatment under the sociocultural community context are community mental health knowledge, attitudes toward the mental health program, and motivation to change. These factors are closely related to each other and are critical in behavioral change. The barriers under the healthcare systems are also grouped as those that relate to financial resource allocation; and leadership and management.[18,26,27] The community responses regarding appropriateness, acceptability, and credibility toward mental health services in primary health centers (PHCs) were identifiable in all of the eligible studies except in one[17] [Figure 5]. The barriers within the community context include (a) beliefs about mental illness as a punishment from God or the ancestors and not a disease (most of the communities lack knowledge on mental health and do not know that people living with the disorder should be taken for treatment) [Figure 5][10,22,28,29]; (b) cultural beliefs about the dangers of people with mental illness has caused stigmatization and avoidance of these people [Figure 5].[18,20,25-27] It was also established that most people avoid seeking medication because it looks shameful. After all, they will be labelled as mad or crazy.[8,15,18] The communities are also not satisfied with the level of knowledge possessed by the family physicians. They are, therefore, discouraged to continue seeking treatment. Additionally, it was found that negative attitudes toward mental health in primary care settings in LMICs is a big hurdle against achieving maximum care[8,19,21,22,26,28] [Figure 4]. Primary care physicians (PCPs) responded that mental healthcare services are not part of primary care practices, demonstrating a lack of knowledge and limited consultation skills.[8,17,26,28]
Figure 5.

COVID-19 effects and need for further assessment of mental health services in LMIC
In this systematic review, the barriers associated with acceptability, credibility, and appropriateness in the SURE model were categorized as “Motivation” in COM-B and classified under the theory of behavior change since they all concern intentions and beliefs, and they can be barriers or facilitators. The barriers associated with appropriateness, acceptability, and credibility of mental healthcare settings, seven developing countries had the highest challenges and six developed states [Table 3].
Knowledge and skills
In all of the studies, barriers associated with knowledge and skills were identified[18,21,30-33] [Figure 5]. The significant issues include low level of diagnosis and treatment of mental illness because of lack of adequate facilities that results in many referrals and inability to recognize an antipsychotic medication, insufficient knowledge about psychosocial intervention,[18] lack of training and awareness concerning mental health issues, lack of enough screening tools,[10,25,28,33] lack of education and skills related to health structures and processes in the management of mental health [Figure 5]. These factors were classified as “Capability” in the SURE framework and behavioral factors under COM-B because they involve knowledge, skills, and strength. When examining the primary care setting in the context of knowledge and skills, these issues were identifiable in all LMICs [Figure 4].
Motivation to change
The motivation to change is a barrier yet a facilitator to mental healthcare services. Out of all of the eligible studies [Figure 4], only one did not provide specific motivation[33] [Figure 5]. In the review, the critical motivation-related barriers to accessing mental healthcare services include:
Little interest in delivering mental health treatment
Huge workload with little time
Low support from the community and at the district level
Few resources to provide sufficient treatment
The ramification of charting a diagnosis of mental healthcare issues or caring for the mental health patients [Figure 4]
All the barriers related to the SURE model were categorized as the “Opportunity” in COM-B since they involve resources, time, cues, location, interpersonal influence, physical affordance, and social and cultural factors [Figure 4].
Health management and leadership
Eight research studies [Figure 5] identified barriers to mental healthcare services related to management and leadership.[10,27,28,31,34] These barriers include lack of proper planning, organization and coordination between primary healthcare providers and the government to design legislation and policies[10]; lack of adequate training in mental healthcare services, particularly of the family physician; lack of enough support from the government to develop knowledge and skills in PCPs; lack of prioritization of mental healthcare issues; little knowledge on system structure and work processes; the inability of the healthcare system to respond to the increase in mental health issues; and lack of interest by the government and institutions to develop responsive mental health services. In this study, the barriers related to leadership and management were categorized as the “Opportunity” domain under the SURE model and COM-B, and the management and leadership barriers were found in 9 studies [Figures 4 and 5].
Financial resources
Five of the selected studies [Figure 5] pointed out the finance and resource-related challenges that primary care settings face in integrating mental healthcare services.[20,21,25,27,35] These barriers include inadequate allocation of resources, lack of employee benefits and motivation; no hiring and support staff to reduce the cost of mental health at the community level; and uncertainty regarding the continuation of funding. The barriers associated with financial resources in the SURE framework were categorized under the “Motivation” domain [Figure 4].
COVID-19: An enhancer of barriers to mental health treatment in LMICs
Many people suffer severe mental stress due to indiscriminate spread of COVID-19 worldwide. This includes job loss, food hardship, and the inability to manage existing medical conditions and maintain preventive measures like social distancing and use of personal preventative equipment (PPE)[7] [Figure 5]. People with chronic illness and other autoimmune disorders are among the most vulnerable in the COVID-19 period.[23] According to recent studies, stress levels have risen by 30% because of the pandemic.[7] This necessitates enhancing primary healthcare in the community for people and families acceptance for affordable mental health services. Here we can refer to the WHO[24,32] that formally adopted the concept of primary healthcare as the preferred method for providing comprehensive mental health services in LMICs. This will help reduce stigma, improve access and quality of primary care, reduce chronicity of mental illness and improve social integration in LMICs[24] [Figure 4].
Implications and future directions
Stigma, human resource shortages, fragmented service delivery models and lack of research capacity for implementation and policy change contribute to the current mental health treatment gap (Qureshi et al., 2021,[36] Tausch et al., 2022).[37] This review describes how health systems in LMICs can address this mental health gap and further identify challenges and priority areas, particularly after the coronavirus pandemic, for future research. General medicine and mental health treatments are accessed via family medicine in communities (Johnson et al., 2022).[38] Thus, primary care is the first stop for most individuals with mental symptoms (Goel et al., 2022).[39] Using our complimentary analysis framework, the obstacles and promoters that influence the primary care practitioner’s activities offer a practical strategy to overcome hurdles linked to mental healthcare services in primary care to improve the health outcomes of LMICs. Our review shows that some eligible studies used secondary data for their analysis, so we have recommended that primary data be the target as they are more credible information sources. In addition, we have attempted to use a combined framework to assess the eligible studies and the post-Covid effects on dealing with mental health management by primary care workers and family practitioners. Future studies should focus on specific countries and also use primary data.
Conclusion
The analysis in this review provides evidence of the lack of existing healthcare policies on the identified barriers to mental health services. If not considered, the key barriers will continue to compromise care for those with mental diseases. We observe that obstacles to the availability of mental healthcare services in primary care settings reflect these communities’ underlying social and financial issues. We were able to identify stigma as the prime barrier to the social context in 8 out of 14 studies, followed by religious and spiritual values influencing decision-making in seeking mental health treatment in LMICs. By understanding the inadequate policymaking and health models of LMICs that lack mental health services, we found a reflection of healthcare organizations’ low interest in mental health services. We also conclude that corruption in LMICs deviated the available global funds to other health issues and did not prioritize mental health in these communities. This study notes that the COVID-19 pandemic has exacerbated social determinants to health and reinteraties that community stigma significantly impedes mental healthcare treatment in LMICs. We conclude that the low adoption of mental healthcare is due to a lack of family physicians’ knowledge and of mental health services. Keeping in mind that the present COVID-19 pandemic has led to an increase of mental illnesses, we urge further post-pandemic mental health research to identify context-specific obstacles to mental health services in primary care that LMICs encounter. Appropriate interventions may be advised to improve mental health treatment globally.
Authors’ contribution statement
SR conceived the study and analyzed the data. AN developed the draft. Both authors approved the final draft of this study.
Declaration
The manuscript has been read and approved by both authors, who certify it to be honest work that is not being considered elsewhere for publication
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Additional File 1.
Critical Appraisal Skills Programme (CASP). CASP Qualitative Checklist. Oxford; 2014
YES (Y), Can't tell (X), NO (N) and Not Applicable (N/A)
| Question | Aggarwal (2020) | Bhat (2020) | Blixen (2020) | Brown (2019) | Evans-Lacko (2018) | Ezeanolue (2020) | Hanlon (2017) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Was there a clear statement of the aims of the research? | Y | Y | Y | Y | Y | Y | Y | ||||||
| Is a qualitative methodology appropriate? | Y | Y | Y | Y | N/A | N | Y | ||||||
| Was the research design appropriate to address the aims of the research? | Y | Y | Y | Y | Y | Y | Y | ||||||
| Was the recruitment strategy appropriate to the aims of the research? | Y | Y | Y | Y | Y | Y | N/A | ||||||
| Were the data collected in a way that addressed the research issue? | Y | Y | Y | Y | Y | Y | Y | ||||||
| Has the relationship between the researcher and participants been adequately considered? | Y | Y | Y | Y | N/A | Y | N/A | ||||||
| Have ethical issues been taken into consideration? | Y | Y | Y | Y | N/A | N/A | Y | ||||||
| Was the data analysis sufficiently rigorous? | Y | Y | Y | Y | Y | Y | Y | ||||||
| Is there a clear statement of findings? | Y | Y | Y | Y | Y | Y | Y | ||||||
| Value of the research? (Contribution, new research areas, etc.) | Y | Y | Y | N | Y | Y | Y | ||||||
| Critical appraisal for quantitative studies | |||||||||||||
| A. Selection bias | |||||||||||||
| 1. Are the individuals selected to participate in the study likely to be representative of the target population? | Y | Y | Y | Y | Y | Y | Y | ||||||
| 2. Percentage of selected individuals agreed to participate indicated | Y | Y | Y | N/A | Y | Y | N/A | ||||||
| B. Study design | |||||||||||||
| 1. Indicate the study design | Qualitative | Qualitative | Qualitative | Scope | Qualitative cross section al-interventional | Scope | Policy review | ||||||
| 2. Was the study described as randomized? If NO, go to component C | N | N | N | N | N | N | N | ||||||
| 3. If yes, was the method of randomization described? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||||||
| 4. If YES, was the method appropriate? | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||||||
| C. Confounders | |||||||||||||
| 1. Were there important differences between groups prior to the intervention? | N | N | N/A | N/A | N | N/A | N/A | ||||||
| 2. If YES, indicate the percentage of relevant confounders that were controlled (either in the design (e.g., stratification, matching) or analysis) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||||||
| D. Blinding | |||||||||||||
| 1. Was (were) the outcome assessor (s) aware of the intervention or exposure status of participants? | N | Y | Y | N/A | N | Y | Y | ||||||
| 2. Were the study participants aware of the research question? | N/A | Y | Y | Y | Y | Y | N/A | ||||||
| E. Data collection methods | |||||||||||||
| 1. Were data collection tools shown to be valid? | Y | Y | Y | Y | Y | Y | Y | ||||||
| 2. Were data collection tools shown to be reliable? | Y | Y | Y | Y | Y | Y | Y | ||||||
| F. Withdrawals and drop-outs | |||||||||||||
| 1. Were withdrawals and drop-outs reported in terms of numbers and/or reasons per group? | N | N | Y | Y | N/A | N | N/A | ||||||
| 2. Indicate the percentage of participants completing the study (if the percentage differs by group, record the lowest) | N | N/A | N/A | N/A | N/A | N/A | Y | ||||||
| G. Intervention integrity | |||||||||||||
| 1. Percentage of participants who received the allocated intervention or exposure of interest | 100% | N/A | N/A | N/A | N/A | N/A | N/A | ||||||
| 2. Was the consistency of the intervention measured? | N | N | N | N | N | N/A | N/A | ||||||
| 3. Is it likely that subjects received an unintended intervention (contamination or co-intervention) that may influence the results? | N | N/A | Y | N | N | N | N/A | ||||||
| H. Analyses | |||||||||||||
| 1. Indicate the unit of allocation | |||||||||||||
| 2. Indicate the unit of analysis | |||||||||||||
| 3. Are the statistical methods appropriate for the study design? | Y | Y | Y | Y | Y | Y | Y | ||||||
| 4. Is the analysis performed by intervention allocation status (i.e., intention to treat) rather than the actual intervention received? | Y | Y | Y | Y | Y | Y | Y | ||||||
|
| |||||||||||||
| Question | Knap P (2006) | Kola (2020) | Luitel (2020) | Mkabile (2020) | Qin (2020) | Trop (2018) | |||||||
|
| |||||||||||||
| Was there a clear statement of the aims of the research? | Y | Y | Y | Y | Y | Y | |||||||
| Is a qualitative methodology appropriate? | N/A | Y | Y | Y | N/A | Y | |||||||
| Was the research design appropriate to address the aims of the research? | Y | Y | Y | Y | Y | Y | |||||||
| Was the recruitment strategy appropriate to the aims of the research? | N/A | Y | Y | Y | N/A | Y | |||||||
| Were the data collected in a way that addressed the research issue? | N/A | Y | Y | Y | Y | Y | |||||||
| Has the relationship between researcher and participants been adequately considered? | N/A | Y | Y | Y | N/A | Y | |||||||
| Have ethical issues been taken into consideration? | N/A | Y | Y | Y | N/A | Y | |||||||
| Was the data analysis sufficiently rigorous? | N/A | Y | Y | Y | Y | Y | |||||||
| Is there a clear statement of findings? | Y | Y | Y | Y | Y | Y | |||||||
| Value of the research? (Contribution, new research areas, etc.) | Y | Y | Y | Y | Y | Y | |||||||
| Critical appraisal for quantitative studies | |||||||||||||
| A. Selection bias | |||||||||||||
| 1. Are the individuals selected to participate in the study likely to be representative of the target population? | N/A | Y | N | Y | N/A | Y | |||||||
| 2. Percentage of selected individuals agreed to participate indicated | N/A | N/A | N/A | N/A | N/A | N/A | |||||||
| B. Study design | |||||||||||||
| 1. Indicate the study design | Policy review | Qualitative | Qualitative | Qualitative | Economic review | Qualitative | |||||||
| 2. Was the study described as randomized? If NO, go to component C | N/A | N | N | N | N/A | N | |||||||
| 3. If yes, was the method of randomization described? | N/A | N/A | N/A | N/A | N/A | N/A | |||||||
| 4. If yes, was the method appropriate? | N/A | N/A | N/A | N/A | N/A | ||||||||
| C. Confounders | |||||||||||||
| 1. Were there important differences between groups prior to the intervention? | N/A | N | N | N | N/A | N | |||||||
| 2. If yes, indicate the percentage of relevant confounders that were controlled (either in the design (e.g., stratification, matching) or analysis)? | N/A | N/A | N/A | N/A | N/A | N/A | |||||||
| D. Blinding | |||||||||||||
| 1. Was (were) the outcome assessor (s) aware of the intervention or exposure status of participants? | N/A | Y | N/A | Y | N/A | Y | |||||||
| 2. Were the study participants aware of the research question? | N/A | Y | Y | Y | N/A | Y | |||||||
| E. Data collection methods | |||||||||||||
| 1. Were data collection tools shown to be valid? | N/A | Y | Y | Y | N/A | Y | |||||||
| 2. Were data collection tools shown to be reliable? | N/A | Y | Y | Y | N/A | N | |||||||
| F. Withdrawals and drop-outs | |||||||||||||
| 1. Were withdrawals and drop-outs reported in terms of numbers and/or reasons per group? | N/A | N | N | Y | N/A | N/A | |||||||
| 2. Indicate the percentage of participants completing the study (if the percentage differs by groups, record the lowest) | N/A | N/A | N/A | N/A | N/A | N/A | |||||||
| G. Intervention integrity | |||||||||||||
| 1. Percentage of participants who received the allocated intervention or exposure of interest | N/A | N/A | N/A | N/A | N/A | N/A | |||||||
| 2. Was the consistency of the intervention measured? | N/A | N | N | N | N/A | N | |||||||
| 3. Is it likely that subjects received an unintended intervention (contamination or co-intervention) that may influence the results? | N/A | Y | Y | N | N/A | N | |||||||
| H. Analyses | |||||||||||||
| 1. Indicate the unit of allocation | |||||||||||||
| 2. Indicate the unit of analysis | |||||||||||||
| 3. Are the statistical methods appropriate for the study design? | Y | Y | Y | Y | Y | Y | |||||||
| 4. Is the analysis performed by intervention allocation status (i.e., intention to treat) rather than the actual intervention received? | Y | Y | Y | Y | Y | Y | |||||||
| Question | Woods-Jaeger (2017) | Wood (2021) |
|---|---|---|
| Was there a clear statement of the aims of the research? | Y | Y |
| Is a qualitative methodology appropriate? | Y | Y |
| Was the research design appropriate to address the aims of the research? | Y | Y |
| Was the recruitment strategy appropriate to the aims of the research? | Y | Y |
| Were the data collected in a way that addressed the research issue? | Y | Y |
| Has the relationship between researcher and participants been adequately considered? | Y | Y |
| Have ethical issues been taken into consideration? | Y | Y |
| Was the data analysis sufficiently rigorous? | Y | Y |
| Is there a clear statement of findings? | Y | Y |
| Value of the research? (Contribution, new research areas, etc.) | Y | Y |
| Critical appraisal for quantitative studies | ||
| A. Selection bias | ||
| 1. Are the individuals selected to participate in the study likely to be representative of the target population? | N | Y |
| 2. Percentage of selected individuals agreed to participate indicated | N/A | N/A |
| B. Study design | ||
| 1. Indicate the study design | Qualitative | Qualitative |
| 2. Was the study described as randomized? If NO, go to component C | N | N/A |
| 3. If yes, was the method of randomization described? | N/A | N/A |
| 4. If yes, was the method appropriate? | N/A | N/A |
| C. Confounders | ||
| 1. Were there important differences between groups prior to the intervention? | N | N |
| 2. If yes, indicate the percentage of relevant confounders that were controlled (either in the design (e.G., Stratification, matching) or analysis) | N/A | N/A |
| D. Blinding | ||
| 1. Was (were) the outcome assessor (s) aware of the intervention or exposure status of participants? | N/A | Y |
| 2. Were the study participants aware of the research question? | N/A | N/A |
| E. Data collection methods | ||
| 1. Were data collection tools shown to be valid? | Y | Y |
| 2. Were data collection tools shown to be reliable? | Y | Y |
| F. Withdrawals and drop-outs | ||
| 1. Were withdrawals and drop-outs reported in terms of numbers and/or reasons per group? | N/A | N |
| 2. Indicate the percentage of participants completing the study (If the percentage differs by group, record the lowest). | N/A | N/A |
| G. Intervention integrity | ||
| 1. Percentage of participants who received the allocated intervention or exposure of interest | N/A | N/A |
| 2. Was the consistency of the intervention measured? | N/A | N |
| 3. Is it likely that subjects received an unintended intervention (contamination or co-intervention) that may influence the results? | N | N/A |
| H. Analyses | ||
| 1. Indicate the unit of allocation | ||
| 2. Indicate the unit of analysis | ||
| 3. Are the statistical methods appropriate for the study design? | Y | Y |
| 4. Is the analysis performed by intervention allocation status (i.e., intention to treat) rather than the actual intervention received? | Y | Y |
Additional File 2.
Prior SURE (Coding) Framework- Best Fit Framework
Note: Chart for reference from previous study titled “Barriers and facilitators to the integration of mental health services into primary health care: a systematic review”
https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-018-0882- 7#Sec23
| Level | Factors affecting implementation |
|---|---|
| Recipients of care | Knowledge and skills |
| Attitudes regarding program acceptability, appropriateness and credibility | |
| Motivation to change or adapt the new behavior | |
| Providers of care | Knowledge and skills |
| Attitudes regarding program acceptability, appropriateness and credibility | |
| Motivation to change or adapt to the new behavior | |
| Other stakeholders (including other healthcare providers, community health committees, community leaders, program managers, donors, policy makers, and opinion leaders) | Knowledge and skills |
| Attitudes regarding program acceptability, appropriateness and credibility | |
| Motivation to change or adapt to the new behavior | |
| Health system constraints | Accessibility of care |
| Financial resources | |
| Human resources | |
| Educational system | |
| Clinical supervision | |
| Internal communication | |
| External communication | |
| Allocation of authority | |
| Accountability | |
| Management and or leadership | |
| Information systems | |
| Facilities | |
| Patient flow processes | |
| Procurement and distribution systems | |
| Incentives | |
| Bureaucracy | |
| Relationship with norms and standards | |
| Social and political constraints | Ideology |
| Short-term thinking |
Appendix 1: Declaration of originality
University of Edinburgh – Own Work Declaration
This sheet must be filled in (each box ticked to show that the condition has been met), signed and dated, and included with all assessments - work will not be marked unless this is done
Name:…………B136127……………………………
Matriculation Number:………B136127…………
Exam No.…………B136127………….
Course/Programme:……Family Medicine Research Project -
Title of work: Barriers to mental health treatment in
Primary Care Practice in Low Middle
Income countries: A Systematic Review
I confirm that all this work is my own except where indicated, and that I have:
Clearly referenced/listed all sources as appropriate □
Referenced and put in inverted commas all quoted text (from books, web, etc.) □
Given the sources of all pictures, data, etc., that are not my own □
Not made any use of the report(s) or essay(s) of any other student(s) either past or present □
Not sought or used the help of any external professional academic agencies for the work □
Acknowledged in appropriate places any help that I have received from others (e.g., fellow students, technicians, statisticians, external sources) □
Complied with any other plagiarism criteria specified in the course handbook □
I understand that any false claim for this work will be penalised in accordance with the University regulations □
Signature ……B 136127……………………………….
Date …………25/11/2021……………………………….
References
- 1.Roberts ST, Flaherty BP, Deya R, Masese L, Ngina J, McClelland RS, et al. Patterns of gender-based violence and associations with mental health and HIV risk behavior among female sex workers in Mombasa, Kenya: A latent class analysis. AIDS and behavior. 2018;22:3273–86. doi: 10.1007/s10461-018-2107-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts AJ, Bao H, Qu P, Moss A, Kim G, Joyce P, Malik F. Mental health comorbidities in adolescents and young adults with type 2 diabetes. Journal of Pediatric Nursing. 2021;61:280–3. doi: 10.1016/j.pedn.2021.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rathod S, Pinninti N, Irfan M. Mental health service provision in low- and middle-income countries. Health Serv Insights. 2017;10:1178632917694350. doi: 10.1177/1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383:510–2. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 5.Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–24. doi: 10.1016/S2215-0366(20)30307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Erinle KO, Ogwu MC, Evivie SE, Zaheer MS, Ogunyemi SO, Adeniran SO. Impacts of COVID-19 on agriculture and food security in developing countries: Potential mitigation strategies. South Asia. 2021;30:13. [Google Scholar]
- 7.Canadian Association of Mental Health, 2021. Menatl Health and the COVID 19 Pandemic. [Last accessed on 2021 Jul 15]. Available from: https://www.camh.ca/en/health-info/mental-health-and-covid-19 .
- 8.Kamvura TT, Dambi JM, Chiriseri E, Turner J, Verhey R, Chibanda D. Barriers to the provision of non-communicable disease care in Zimbabwe: A qualitative study of primary health care nurses. BMC Nurs. 2022;21:1–12. doi: 10.1186/s12912-022-00841-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pokhrel P, Karmacharya R, Taylor Salisbury T, Carswell K, Kohrt BA, Jordans MJD, et al. Perception of healthcare workers on mobile app-based clinical guideline for the detection and treatment of mental health problems in primary care: A qualitative study in Nepal. BMC Medical Inform Decis Mak. 2012;21:1–12. doi: 10.1186/s12911-021-01386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wakida EK, Talib ZM, Akena D, Okello ES, Kinengyere A, Mindra A. Barriers and facilitators to the integration of mental health services into primary health care: A systematic review. Syst Rev. 2018;7:211. doi: 10.1186/s13643-018-0882-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong SJ, Wilczynski NL, Haynes RB. Optimal CINAHL search strategies for identifying therapy studies and review articles. J Nurs Scholarsh. 2006;38:194–9. doi: 10.1111/j.1547-5069.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- 12.Patino CM, Ferreira JC. Inclusion and exclusion criteria in research studies: definitions and why they matter. Jornal Brasileiro de Pneumologia. 2018;44:84–4. doi: 10.1590/S1806-37562018000000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper C, Booth A, Varley-Campbell J, Britten N, Garside R. Defining the process to literature searching in systematic reviews: A literature review of guidance and supporting studies. BMC Med Res Methodol. 2018;18:85. doi: 10.1186/s12874-018-0545-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munn Z, Tufanaru C, Aromatiris E. JBI'S systematic reviews: Data extraction and synthesis. Am J Nurs. 2014;114:49–54. doi: 10.1097/01.NAJ.0000451683.66447.89. [DOI] [PubMed] [Google Scholar]
- 15.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324:819–23. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nowell LS, Norris JM, White DE. Thematic analysis: Striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16 doi: 10.1177/1609406917733847. [Google Scholar]
- 17.Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Benjet C, bruffaerts R, et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: Results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48:1560–671. doi: 10.1017/S0033291717003336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blixen C, Lema I, Mbwambo J, Kaaya S, Levin JB, Sajatovic M. Community perception of barriers to management of chronic psychotic disorders and knowledge and attitudes about long-acting injectable antipsychotic medication: Qualitative study in Dar es Salaam, Tanzania. BJPsych Open. 2020;6:e27. doi: 10.1192/bjo.2020.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chol C, Negin J, Garcia-Basteiro A, Gebrehiwot TG, Debru B, Chimpolo M. Health system reforms in five Sub-Saharan African countries that experienced major armed conflicts (Wars) during 1990-205: A literature review. Glob Health Action. 2018;11:1517931. doi: 10.1080/16549716.2018.1517931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanlon C. Next steps for meeting the needs of people with severe mental illness in low-and middle-income countries. Epidemiol Psychiatr Sci. 2017;26:348–54. doi: 10.1017/S2045796016001013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown FL, Steen F, Taha K, Aoun M, Bryant R, Jordans MJD, et al. Early adolescent skills for emotions (ease) intervention for treatment of psychological distress in adolescents: Study protocol for randomized controlled trials in Lebanon and Jordan. Trials. 2019;20:500–45. [Google Scholar]
- 22.Trop J, Gendenjamts B, Bat-Erdene U, Doripurev D, Ganbold S, Bayalag M, et al. Postpartum depression in Mongolia: A qualitative exploration of health care providers'perspectives. Midwifery. 2018;65:18–25. doi: 10.1016/j.midw.2018.06.020. [DOI] [PubMed] [Google Scholar]
- 23.Waterfield KC, Shah GH, Etheredge GD, Ikhile O. Consequences of COVID-19 crisis for persons with HIV: The impact of social determinants of health. BMC Public Health. 2021;21:299. doi: 10.1186/s12889-021-10296-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO, n.d. Integrating Mental Health into Primary Care. [Last accessed on 2022 Jan 20]. Available from: https://www.who.int/publications/i/item/9789241563680 .
- 25.Qin X, Hsieh CR. Understanding and addressing the treatment gap in mental healthcare: Economic perspectives and evidence from China. Inquiry. 2020;57:46958020950566. doi: 10.1177/0046958020950566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knapp M, Funk M, Curran C, Prince M, Grigg M, McDaid D. Economic barriers to better mental health practice and policy. Health Policy Planning. 2006;21:157–70. doi: 10.1093/heapol/czl003. [DOI] [PubMed] [Google Scholar]
- 28.Wood-Jaeger B, Kava C, Akiba CF, Lucid L, Dorsey S. The art and skill of delivering culturally responsive trauma-focused cognitive behavioral therapy in Tanzania and Kenya. Psychol Trauma. 2017;9:230–8. doi: 10.1037/tra0000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luitel NP, Jordans MJD, Subba P, Komproe IH. Perception of service users and their caregivers on primary care-based mental health services: A qualitative study in Nepal. BMC Fam Pract. 2020;21:202. doi: 10.1186/s12875-020-01266-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kola L, Bennett LM, Bhat A, Ayinde OO, Oladeji BD, Abiona D, et al. Stigma and utilization of treatment for adolescent perinatal depression in Ibadan Nigeria. BMC Pregnancy Childbirth. 2020;20:294. doi: 10.1186/s12884-020-02970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhat A, Goud RB, Pradeep JR, Jayaram G, Radhakrishnan R, Srinivasan K. Can mobile health improve depression treatment access and adherence among rural India Women?A qualitative study. Cult Med Psychiatry. 2020;44:461–78. doi: 10.1007/s11013-019-09664-3. [DOI] [PubMed] [Google Scholar]
- 32.Aggarwal S, Patton G, Bahl D, Shah N, Berk M, Patel V. Explanatory style in youth self-harm: An Indian qualitative study to inform intervention design. Evid Based Ment Health. 2020;23:100–6. doi: 10.1136/ebmental-2020-300159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mkabile S, Swartz L. 'I Waited for it until Forever': Community barriers to accessing intellectual disability services for children and their families in Cape Town, South Africa. Int J Environ Res Public Health. 2020;17:8504. doi: 10.3390/ijerph17228504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whitaker R, Hendry M, Booth A, Carter B, Charles JM, Craine N, et al. Intervention Now to Eliminate Repeat Unintended Pregnancy in Teenagers (INTERUPT): A systematic review of intervention effectiveness and cost-effectiveness, and qualitative and realist synthesis of implementation factors and user engagement. Health Technology Assessment (Winchester, England) 2016;20:1. doi: 10.3310/hta20160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ezeanolue EE, Iheanacho T, Adedeji IA, Itanyi IU, Olakunde B, Patel D, et al. Opportunities and Challenges to Integrating Mental Health into HIV Programs in a Low-and Middle-income Country: Insights from the Nigeria Implementation Science Alliance. BMC Health Serv Res. 2020;20:800–904. doi: 10.1186/s12913-020-05750-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qureshi O, Endale T, Ryan G, Miguel-Esponda G, Iyer SN, Eaton J, et al. Barriers and drivers to service delivery in global mental health projects. Int J Ment Health Syst. 2021;15:1–13. doi: 10.1186/s13033-020-00427-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tausch A, E Souza RO, Viciana CM, Cayetano C, Barbosa J, Hennis AJ. Strengthening mental health responses to COVID-19 in the Americas: A health policy analysis and recommendations. Lancet Reg Health Am. 2022;5:100118. doi: 10.1016/j.lana.2021.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson JK, Terry AL, Vingilis E. Providing healthcare and fitness to drive assessments for long-haul truck drivers: A qualitative study of family physicians and nurse practitioners. J Transp Health. 2022;24:101324. [Google Scholar]
- 39.Goel NJ, Thomas B, Boutté RL, Kaur B, Mazzeo SE. “What will people say?”: Mental health stigmatization as a barrier to eating disorder treatment-seeking for South Asian American women. Asian Am J Psychol. 2022 doi: 10.1037/aap0000271. doi: 10.1037/aap0000271. [DOI] [PMC free article] [PubMed] [Google Scholar]