Abstract
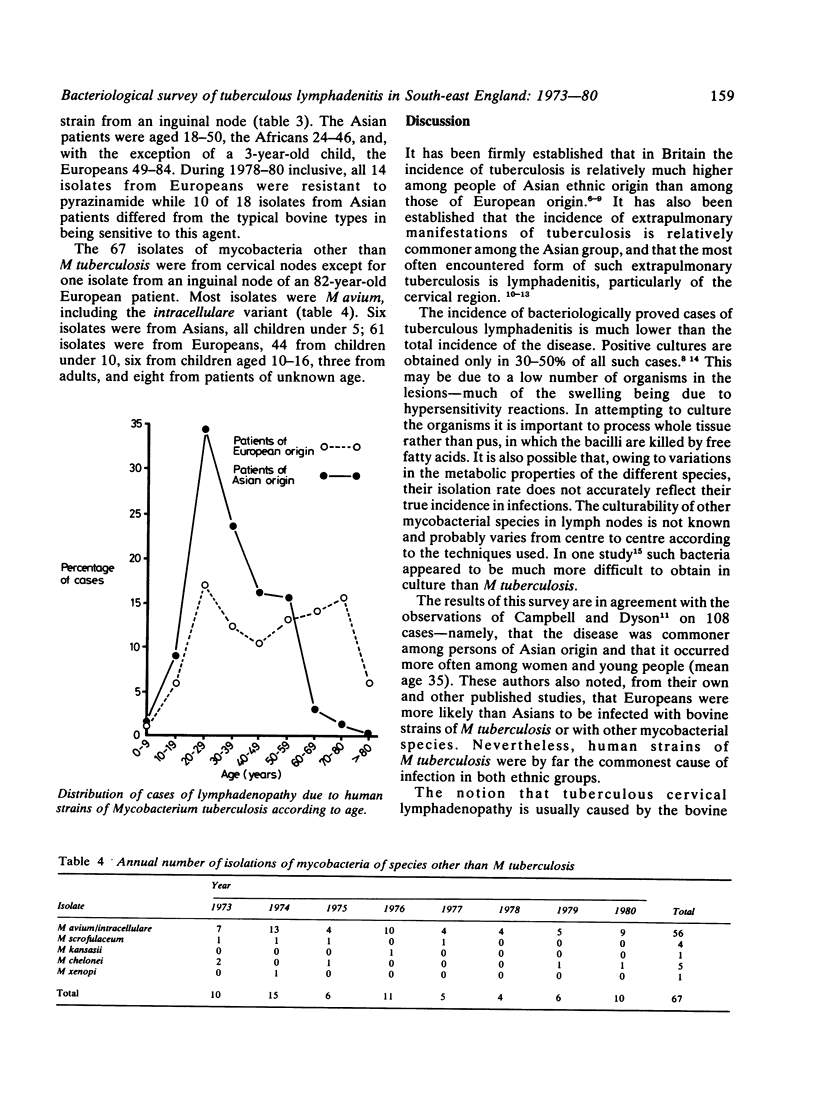
During the eight years 1973-80 the Public Health Laboratory Service Regional Centre for Tuberculosis Bacteriology received cultures of mycobacteria from 2339 patients with tuberculous lymphadenitis. Of these, 2272 were M tuberculosis (2207 human and 65 bovine strains) and 67 were other mycobacterial species, usually M avium and its intracellulare variant. Disease due to the human strains of M tuberculosis occurred most often in young women of Asian ethnic origin. Many bovine strains isolated from Asian patients differ from the classical bovine type in being sensitive to pyrazinamide: the origin of these strains, whether from other people or from cattle, is unknown. Lymphadenitis due to bovine strains tended to occur in an older age group than the human strains and probably include relatively more cases of reactivation diseases. Infection caused by the other mycobacterial species occurred mainly in young children of European origin. Tuberculosis, therefore, remains an important cause of lymphadenopathy in Britain.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Campbell I. A., Dyson A. J. Lymph node tuberculosis: a comparison of various methods of treatment. Tubercle. 1977 Dec;58(4):171–179. doi: 10.1016/0041-3879(77)90041-1. [DOI] [PubMed] [Google Scholar]
- Collins C. H., Yates M. D., Grange J. M. A study of bovine strains of Mycobacterium tuberculosis isolated from humans in South-East England, 1977-1979. Tubercle. 1981 Jun;62(2):113–116. doi: 10.1016/0041-3879(81)90018-0. [DOI] [PubMed] [Google Scholar]
- Grange J. M., Aber V. R., Allen B. W., Mitchison D. A., Mikhail J. R., McSwiggan D. A., Collins C. H. Comparison of strains of Mycobacterium tuberculosis from British, Ugandan and Asian immigrant patients: a study in bacteriophage typing, susceptibility to hydrogen peroxide and sensitivity to thiophen-2-carbonic acid hydrazide. Tubercle. 1977 Dec;58(4):207–215. doi: 10.1016/0041-3879(77)90045-9. [DOI] [PubMed] [Google Scholar]
- Grange J. M. Tuberculosis: the changing tubercle. Br J Hosp Med. 1979 Dec;22(6):540–548. [PubMed] [Google Scholar]
- Hooper A. A. Tuberculous peripheral lymphadenitis. Br J Surg. 1972 May;59(5):353–359. doi: 10.1002/bjs.1800590506. [DOI] [PubMed] [Google Scholar]
- Kent D. C. Tuberculous lymphadenitis: not a localized disease process. Am J Med Sci. 1967 Dec;254(6):866–874. [PubMed] [Google Scholar]
- MILLER F. J., CASHMAN J. M. Origin of peripheral tuberculous lymphadenitis in childhood. Lancet. 1958 Feb 8;1(7015):286–289. doi: 10.1016/s0140-6736(58)91030-4. [DOI] [PubMed] [Google Scholar]
- Newcombe J. Tuberculosis: tuberculous glands in the neck. Br J Hosp Med. 1979 Dec;22(6):553–555. [PubMed] [Google Scholar]
- Schuit K. E., Powell D. A. Mycobacterial lymphadenitis in childhood. Am J Dis Child. 1978 Jul;132(7):675–677. doi: 10.1001/archpedi.1978.02120320035007. [DOI] [PubMed] [Google Scholar]
- WILMOT T. J., JAMES E. F., REILLY L. V. Tuberculous cervical adenitis. Lancet. 1957 Dec 14;273(7007):1184–1187. doi: 10.1016/s0140-6736(57)90160-5. [DOI] [PubMed] [Google Scholar]
- Yates M. D., Collins C. H. Identification of tubercle bacilli. Ann Microbiol (Paris) 1979 Jul;130B(1):13–19. [PubMed] [Google Scholar]


