Abstract
Introduction
Heatstroke (HS) is a severe form of heat-related illness (HRI) associated with high morbidity and mortality, representing a condition that includes long-term multiorgan dysfunction and susceptibility to further heat illness.
Methods
In a systematic review searching Medline PubMed from the studies conducted between 2009 and 2020, 16 papers were identified.
Results
A hallmark symptom of heat stroke is CNS dysfunction (a hallmark sign of HS) which manifests as mental status changes, including agitation, delirium, epilepsy, or coma at the time of the collapse. Acute kidney injury (AKI), gut ischemia, blood clots in the stomach and small intestine, cytoplasmic protein clumps in the spleen, and injury of skeletal muscle (rhabdomyolysis) are all characteristics of peripheral tissue damage. Severe heat stroke tends to be complicated by rhabdomyolysis, especially in patients with exertional heat stroke. Rhabdomyolysis may lead to systemic effects, including the local occurrence of compartment syndrome, hyperkalemic cardiac arrest, and/or lethal disseminated intravascular coagulopathy. Untreated heat stroke might exacerbate psychosis, lactic acidosis, consumptive coagulopathy, hematuria, pulmonary edema, renal failure, and other metabolic abnormalities. Core body temperature and level of consciousness are the most significant indicators to diagnose the severity of heat stroke and prevent unfavorable consequences. Heatstroke is a life-threatening illness if not promptly recognized and effectively treated.
Discussion
This review highlighted that core body temperature and white blood cell count are significant contributing factors affecting heat stroke outcomes. Other factors contributing to the poor outcome include old age, low GCS, and prolonged hospital stay. The prevalence of both classic and exertional heatstroke can be reduced by certain simple preventive measures, such as avoiding strenuous activity in hot environments and reducing exposure to heat stress.
Keywords: Hajj, heat stroke, old age, pilgrimage, white blood cells
Introduction
Heat-related illnesses (HRIs) have a substantial impact on a considerable number of individuals annually and are emerging as a significant health-related issue in light of the notable increase in global temperatures.1 Based on the findings of the study, it has been observed that the occurrence of severe heat stroke poses a significant risk to the mental well-being of affected individuals. Prolonged exposure to elevated temperatures in the surrounding environment has the potential to induce hypothermia, a condition characterized by an abnormal decrease in body temperature. This physiological response can subsequently impact mental well-being and result in dehydration.2 The factors that contribute to an individual’s susceptibility to HRIs encompass a range of elements. These include a medical history that includes prior instances of illness or HRI, the presence of cardiovascular disease, individuals with a high body mass index (BMI), the use of certain medications, tobacco consumption, a low level of physical fitness, and the presence of the sickle cell trait (SCT) (Figure 1).3
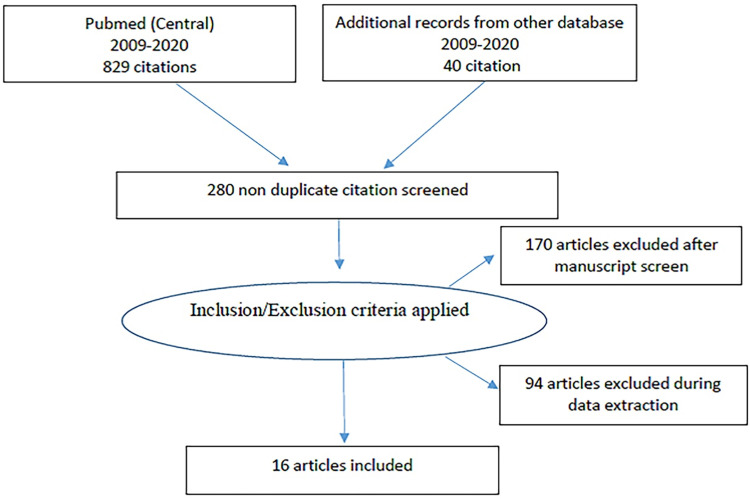
Figure 1.
Flow diagram for the searches and inclusion criteria in the study.
Heat exhaustion (HE) and heat stroke (HS) are considered to lie on the same heat spectrum with the former considered to be a milder form of HRI. It is an extremely important step to recognize heat exhaustion which has the potential to progress into more serious heat stroke.4 The condition of hyperthermia which is characterized by heat stroke causes the dysregulation of the nervous system. If physical treatment has not been provided for heat events this will significantly lead to morbidity, in most cases, cardiac arrest is the most common circumstance.
HS is categorized into two classes based on the presence or absence of exertion. Exertional HS is present in able-bodied individuals, such as athletes, soldiers, or laborers, or those performing rigorous physical activities, while non-exertional heat stroke is observed in people with low-level physical activities such as elderly, ambulatory individuals with co-morbidities such as diabetes, hypertension, heart disease, renal disease, dementia, and alcoholism.5
The research identifies that there are worse impacts of comorbid heat-related illness and common illnesses on that patient which are in more use of hospital resources. The factors which are the number of hours stayed in hospitals, length of stay, number of visits, discharge status or death condition, and having the symptom of the heat-related illness or common illness are all associated with the increase of disease. Many of them suffer from respiratory problems when heat stroke increases. The study reported that heat stroke has an indication of multiple health hazards like renal and diabetic problems are all linked with the illness of heat stroke. The multiple cases and the symptom of the HRI have a worse outcome and cause a higher risk of death among respiratory and cardiac disease patients.6 According to the climate report, it has been observed that for the last two decades, there had been reported record-breaking heat waves which have increased class heat stroke which affects the epidemic form of the globe and its facilities the heat-related illness to 9–37%, whereas external heat stroke badly affected young adults. The mortality reaches up to 26.5% in the intensive care units; however, 63.2% includes external and classic heat stroke. The survivor of heat stroke also suffers long-term damage in the cell injury and causes inflammation and thrombosis with the experience of neurological and cardiovascular complications. This leads to the persistent risk of death. No specific therapy or sure has been identified. The phenomena have proved that heat stroke contributes to physiological and morphological complications7 The significant effects caused by classical heat stroke and exertional heat stroke encompass a range of symptoms such as headache, weakness, dizziness, nausea and vomiting, diarrhea, irritability, coordination loss, tachycardia/hypotension, and preserved cognitive function. The primary demographic affected by this phenomenon consists of individuals who are particularly susceptible to its effects, such as street children who are regularly exposed to direct sunlight, as well as adults who remain inside sun-exposed enclosed vehicles during periods of intense heat.8
The facilities of the heat techniques which are immensely used and found effective are ice water immersion, augmentation of ice packs which can diffuse in the body easily, and provide the primary cooling supplement of chilled intravenous fluid. Applying the ice packs directly on the neck, axilla, and groin and cooling blankets are not recommended as the basic method of cooling to control heat stroke.6 The researchers define HS based on pathophysiology which stated
it as a form of hyperthermia accompanied by a systemic inflammatory response (SIR) resulting in multiorgan failure including rhabdomyolysis, renal failure, hepatitis, or coagulation disorder, particularly encephalopathy (Table 1 and Table 2).9
Table 1.
The Outcome of HS Patients in Various Studies
| S. No | Author | Year | Study Design | Sample Size | Mean Age (Year) | Gender | Affected System | Findings | HS/HE/ HRI |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Wei-Ta Chen et al14 | 2012 | Case report | - | 39 | M | CVS | ST elevation, stress-induced cardiomyopathy | HS |
| 2 | Mimish et al27 | 2012 | Case-control | HS/HE/Control- 34/28/21 (n=83) | 59 | M/F | CVS | 1. Mean core temp: 41.7/38.7/37.1 | HS and HE |
| 2. HR: 120/97/74 | |||||||||
| 3.Mean BP:76/102/92 | |||||||||
| 4.Mean PR interval:158/152/159 | |||||||||
| 5. Mean QT interval: 314/326/364 | |||||||||
| 6. Pathological Q-waves: 0/2/0 | |||||||||
| 3 | Yang et al30 | 2017 | Retrospective cohort | 117 | 22 | M/F | CNS | Incidence of a neurologic sequel: 24.4% | EHS |
| GCS: 6 (4–9), GCS (3 in alive and 6 in expired) | |||||||||
| Deep coma: 37.6% | |||||||||
| 4 | Satirapoj et al33 | 2016 | Retrospective cohort | 66 | 22.1 | M | Renal | (Renal loss: potassium loss; 54.2%, phosphate loss; 86.7%, sodium loss; 64.7% and magnesium loss; 83.3%). | Nonexertional HS |
| AKI in 90.9% of cases, | |||||||||
| Expired: 3% | |||||||||
| Received dialysis: 16.7% | |||||||||
| 5 | Erarslan et al47 | 2012 | Case report | - | 63 | M | Hepatic | Acute liver failure: Total bilirubin (max): 7.8mg/dl on day 6 | |
| Direct bilirubin (max): 5.7mg/dl on day 6 | |||||||||
| AST (max): 3450 IU/L on day 5 | |||||||||
| ALT (max): 2600 IU/L | |||||||||
| Renal | Acute renal failure: Urea (max): 122mg/dl on day 3, creatinine: 7.7 mg/dl on day 7 | ||||||||
| 6 | Wu et al65 | 2015 | Case report | 35 | Male | Multiple organ failure | Urea nitrogen: 1.55 Serum creatinine:35.6 Prothrombin Ratio: 54 C-Reactive Protein 72 | Exertional heat stroke | |
| 7 | Abriat et al28 | 2014 | Retrospective study | 182 | 26 | Male | Multiple organ failure | Renal failure in 31.3% of the subjects, liver insufficiency in 12%, and disseminated intravascular coagulation in 1% | Exertional heatstroke |
| 8 | Li et al29 | 2015 | 59 | Male | Neurological problem | Remarkable symmetric lesions in the cerebellar peduncles, restricted water diffusion in the bilateral dentate nuclei |
Heat stroke | ||
| 9 | Jilma et al34 | 2012 | Retrospective study | 66 | 22.1 | Renal system failure | Hypokalemia in 71.2%, hypophosphatemia in 59.1%, hyponatremia in 53.0%, hypocalcemia in 51.5%, and hypomagnesemia in 34.9% of cases. 90.9% of patients suffered from AKI with 16.7% receiving acute dialysis | Exertional heatstroke | |
| 10 | Hifumi et al40 | 2018 | Randomized controlled study | 705 | 68 | Male | Coagulation system failure | Hospital mortality was significantly associated with the presence of DIC (odds ratio [OR], 2.16; 95% confidence interval [CI], 1.09–4.27; p=0.028) | Heat stroke |
| 11 | Carvalho et al48 | 2016 | Case report | 25 | Male | Acute liver failure | Acute kidney injury with creatinine 2.2 mg/ dL | Exertional heat stroke | |
| 12 | Salathé et al53 | 2015 | Case report | 36 | Male | Acute liver failure | Raised Aspartate aminotransferase [AST], Phosphate, and Factor V | Exertional heat stroke | |
| 13 | Castro et al57 | 2018 | Case report | 35 | Male | Fulminant liver failure | D-dimer (ng/mL): 8801 Activated partial thromboplastin time: 89, Total bilirubin (mg/dL):2.5, Creatinine: 1.7 |
Heat stroke | |
| 14 | Yoshizawa et al58 | 2016 | Case report | 34 | Male | Bimodal rhabdomyolysis | Creatinine phosphokinase (CPK) level increased to 8832 IU/L | Heat stroke | |
| 15 | Thongprayoon et al60 | 2020 | Cohort study | 3372 | 20–39 (median) | Male | Rhabdomyolysis | Rhabdomyolysis was significantly associated with an increased risk of hyponatremia, hypernatremia, hyperkalemia, hypocalcemia, serum phosphorus and magnesium derangement, metabolic acidosis, sepsis, ventricular arrhythmia or cardiac arrest, renal failure, respiratory failure, liver failure, neurological failure, hematologic failure, and in-hospital mortality | |
| 16 | Azzopardi et al47 | 2012 | Case report | 25 | Male | Acute liver impairment, Hypoxic Hepatitis, and Rhabdomyolysis | Glasgow Coma Score of 10. He had a temperature of 105.4°F on admission and he was sweaty, tachycardic (heart rate of 160 bpm), and had a systolic blood pressure of 90 mm Hg, creatinine phosphokinase (CPK) level (178,850 U/l) |
Table 2.
HS Cases with Rhabdomyolysis
| No | Report | Year | Age | Sex | Trigger | Peak Day | CPK Max | HD | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Wu65 | 2015 | 27 | Male | Exercise | 2 | 55,650 | Yes | Survival |
| 2 | Asserraji66 | 2014 | 35 | Male | Marathon | 5 | 91,596 | Yes | Survival |
| 3 | Raj67 | 2013 | 11 | Male | Jog | 1 | 4326 | Yes | Death |
| 4 | Horseman47 | 2013 | 22 | Male | Walking | 1 | 649,530 | Yes | Survival |
| 5 | Azzopard68 | 2012 | 25 | Male | Marathon | 2 | 178,850 | No | Survival |
| 6 | Muriz74 | 2011 | 15 | Male | Football | 2 | 39,954 | No | Survival |
| 7 | Trujilo38 | 2011 | 14 | Female | Exercise | 3 | 36,243 | Yes | Survival |
| 8 | Lin22 | 2011 | 11 | Female | Jogging | 2 | 21,351 | No | Survival |
| 9 | Miura69 | 2010 | 38 | Male | Marathon | 3 | 84,612 | No | Death |
| 10 | Lee70 | 2010 | 57 | Male | Ko spring | 3 | 9565 | Yes | Death |
| 11 | Niu71 | 2009 | 47 | Male | Labor | 1 | 4682 | No | Survival |
A rise in the body temperature leads to sympathetic cutaneous vasodilation activation which causes thermal sweating but also results in a reduction in the intra-vascular volume leading to heat syncope. Several strategies are used by sports athletes which uses to reduce the risk factors of the dangers which come from exercise done in the heat condition. Nutritional intervention is one of the major sources to vasodilate the cutaneous process and also expand the plasma volume which will be helpful to improve cardiovascular activity and helps in optimizing the hydration status by fluid replacement beverages. The more consumption of sodium and glucose can improve and provide betterment water retention and absorption.10
The nonspecific symptom of heat exhaustion is headache, malaise, and nausea. All the first aid or treatment including the monitoring of liquid intake by the patient and the surrounding environment have cooling impacts. If heat exhaustion is not treated priory, it may lead to damage to the central nervous system like coma and heatstroke leading the cardiac arrest. Now the researcher is focusing more on physicians and the public health department.11
Several studies are associated with heat-related illnesses describing the risk factors and their illness symptoms with cardiovascular diseases. The association of heat stroke represents that the risk of cardiovascular diseases increases with the increased ratio of heat stroke. The symptom has equal control on the population in different comparisons of age, sex, and comorbidity-matched patients.12,13 The outcomes of HRIs include cause rhabdomyolysis, coma with acute and even permanent vital organ damage, and multiple organ failure (MOF).14,15
The heat waves have provoked the global warming condition, damaging the greenhouse effect which threatens the survival of human beings. The ability to absorb heat has deteriorated the skin of the body and led to skin problems. This thermal change has aided the sweating and the cutaneous flow in the body, although it also affects the physiological and pathological condition of the body. Thus, more identification is required to protect the skin of the body, and more care is required for the patient.16 In heat stroke, there is further impairment of thermoregulation due to a reduction in cutaneous vasodilation as a result of shunting of the blood from the central circulation to the muscles and skin, leading to MOF.17
Although previous studies have examined the associations between climate variability and the outcomes of patients with heatstroke and heat exhaustion, none of these studies have specifically investigated the impact of different climate zones on these outcomes. Consequently, we conduct a comprehensive and methodical examination of the existing epidemiological data about the impacts of heat exposure on patient outcomes. This is accomplished through a thorough and current review of the relevant literature, followed by an evaluation of the quality and robustness of the evidence.
Materials and Methods
This systematic review was executed to identify and extract all relevant and potential studies emphasizing the outcome of patients with heat stroke and exhaustion. The literature search was conducted using the “PubMed: MEDLINE” database. The search screened articles published from 2009 to 2020 and possibly qualified articles were searched manually through reference list screening. The preferred language for this research is English, while the keywords selected to search algorithms in the database are “Heatstroke” “Heat-related illness” “Heat exhaustion” or “Heat stress”. The inclusion criteria of this study were to enroll the adult population who have experience visiting hospitals in heat stroke or heat exhaustion conditions. This review considers the application domain including disease diagnosis and the outcome. International Classification of Diseases (ICD) was followed. The exclusion criteria were to reject the articles which were not in English, studies related to heat impact on the animal, and articles without full text.
Two researchers conducted initial screenings of articles, employing a double-blind and independent approach. These screenings encompassed the evaluation of titles, abstracts, and full texts. The relevant data from the chosen studies were recorded in a spreadsheet, which included details such as the author’s name, publication year, study design, sample size, age range, gender distribution, affected system, findings, and evaluation of health economics, health systems, and health research and innovation. This information was then reviewed and verified by the investigators.
The present study employed a systematic review methodology, thus statistical analysis was not performed. The data was synthesized using a narrative approach. The assessment of study quality and bias was conducted using a combination of the Downs and Black scale and the Newcastle-Ottawa Scale. These scales consist of 11 items, as described by Downs et al18 and Wells et al,19 and are organized into four themes: reporting, external validity, internal validity for bias, and internal validity for confounding. This approach was employed to encompass both observational and experimental study designs.
The data for each included study consisted of the following details author and year of publication.
Results
A total of 869 citations were identified through electronic searches. Titles and abstracts were screened for relevance (stage 1 screening), then study duplications were identified, resulting in 280 relevant citations being retained. The full texts of these articles were obtained. Then applying inclusion criteria to these full-text articles (stage 2 selection), 264 citations were excluded, which were not according to the inclusion criteria. Sixteen citations were therefore included in the systematic review.
Mortality
ICU mortality was due to MOF present early after admission to ICU, as reflected by circulatory shock, renal failure, hemostasis disorders, deep coma, and a high admission SAPS II score. Furthermore, it is very likely that neurologic sequelae largely contributed to death in the hospital after ICU discharge, as previously reported.19,20 Misset et al17 reported a mortality rate of 20% mortality (n = 58) of patients and these patients had much more severe heatstroke as reflected by the lower Glasgow Coma Scale score.21 Several factors independently associated with mortality, including high body temperature and prolonged prothrombin time, were present within the first 24 hrs after ICU admission. This is consistent with the current knowledge of the pathophysiology of heatstroke, including the diffuse cell damage induced by higher temperatures,22 the production of cytokines23 and nitric oxide,24 and endothelial cell injury.25 Although older age, cardiac, respiratory, or neurologic co-morbidity, preexisting use of neuroleptics or diuretics, and alcohol abuse commonly predispose to the occurrence of heatstroke,26 Misset et al19 observed none of these factors was an independent predictor of mortality in declared heatstroke.
Cardiovascular Damage
A case–control study conducted by Mimish27 observed that electrocardiographic abnormalities occur with a high frequency in patients with HS and HE, with sinus tachycardia and ischemic changes. In Group 1, 18 were females and 16 males with mean ages of 59 ± 11 years.27 Their mean heart rate was 120 ± 24 per minute. Only 5/34 ECGs were completely normal. Sinus tachycardia was present in 79% of patients, with ischemic changes in 9/34 ECGs. In group 2, 24 were males and four females with age 47 ± 15 years, mean heart rate was 97 ± 160 per minute. In group 2, 21/28 (75%) had some abnormalities. None had ischemic changes. The control group (group 3), was five females and 26 males, the mean age was 38 ± 15 years, and 22/31 (71%) had normal ECGs. All had normal sinus rhythm, and mean beats were 74 ± 11 per minute. Nine patients had some electrocardiographic abnormalities, but none of them had ischemic changes.
Findings on ECG described in patients with HRI include sinus tachycardia, conduction defects, QT interval prolongation, diffuse ST-T changes, as well as ST-T changes localized to the distribution of a coronary artery.27 Although previous research had attributed most of the ECG changes to electrolyte imbalances associated with heat stroke, subsequent studies done on a larger cohort have failed to evaluate any clear correlation.27
Previous studies reported conduction defects including non-specific intraventricular conduction delay, which have been attributed to multiple factors including a change in the conduction rate of the repercussions of the right bundle branch due to the potential involvement of heat shock proteins in ion channel trafficking in the cell membrane and elevated right ventricle pressure (resulting in incomplete RBBB).27
Neurological Damage
With the brain being sensitive to extremely high temperatures, the impairment of CNS is considered one of the most serious complications of HS. This impairment has been reported in 80.3 to 100% of HS patients admitted to ICUs during the heat waves in America and Europe and 100% of soldiers.28 Another important finding observed in HS patients is the presence of neurological sequelae such as cerebellar ataxia, dysarthria, cognitive disorders, and anterograde amnesia) in 20–30% of patients within a few days, weeks, or months of heat stroke even with timely aggressive clinical intervention initiation which includes lowering of core body temperature and support of organ function.29
The Glasgow Coma Scale (GCS) is the most commonly used clinical scoring system for the assessment of the severity of CNS deterioration severity, which ranges as follows: mild (GCS 13–15), moderate (GCS 9–12), or severe (GCS 3–8).30 Yang et al30 study reported HS patients were classified into 2 groups, ie, severe (GCS 3–8) and moderate (GCS 9–15) depending on CNS injury extent. The period of CNS injury spanned from the time of admission in the hospital until the point at which the patient’s condition had improved such that s/he could open the eyes in response to the speech, exhibit improved conversational ability, and attain a GCS score of at least 12. Since HS patients were discharged, neurological sequelae such as cerebellar ataxia, dysarthria, cognitive disorders, and/or anterograde amnesia that developed later were also observed.
Of one hundred and seventeen patients, for axillary temperature, 46 patients (39.3%), 44 (37.6%), 25 (21.3%), and 1 (0.8%) exhibited axillary temperatures between 39 and 40 °C; 40.1 and 41 °C; 41.1 and 42 °C; and greater than 42 °C, respectively. Forty-five (38.5%) patients exhibited signs of hypotension (mean arterial pressure <65 mm Hg). 79.5% had severe (GCS 3–8) CNS injuries, while 22.5% did not have severe (GCS 9–15) CNS injuries. Forty-four (37.6%) patients experienced deep coma (GCS = 3). The extent of CNS injury extent was significantly more severe in expired (median GCS-3; IQR 3–4.5) than in alive patients (median GCS: 6; IQR 4–9). Of the 21 patients with neurological sequelae, 42.9% patients were found to have developed cerebellar ataxia, 28.6% had dysarthria and 19.0% had cognitive disorders and anterograde amnesia.30
Another study conducted by Yamamoto et al31 retrospectively analyzed various predictive factors for hospitalization amongst patients who presented with mild to moderate heat illness in the emergency department (ED) of Yamaguchi Prefecture, Japan. It was found that a significant difference was observed in the GCS between inpatient and outpatient groups (inpatient GCS median 15 (IQR 14–15), outpatient GCS median 15 (IQR 15–15).
A case report was published about a Japanese man who collapsed due to non-exertional HS on a hot and humid day.32 On presentation, the patient had a GCS of 6/15, altered consciousness, and a core body temperature of 40.6°C. He had a deranged hepatic and renal profile with evidence of severe rhabdomyolysis (CPK – 1163 U/L). Due to low GCS, the patient was intubated and cooled aggressively with the intravascular balloon-catheter system. The patient was discharged on day 5 with no evidence of any neurological sequelae and a GCS of 15/15.33
Renal System Failure
A retrospective cohort study34 included 66 subjects (mean age 22.1 years) with EHS. Hypokalemia was observed in 71.2%, hypophosphatemia in 59.1%, hyponatremia in 53.0%, hypocalcemia in 51.5%, and hypomagnesemia in 34.9% of cases. Electrolyte depletion was confirmed as renal loss (potassium loss; 54.2%, phosphate loss; 86.7%, sodium loss; 64.7%, and magnesium loss; 83.3%). During hospitalization ranging from 2 to 209 days, 90.9% of patients suffered from AKI with 16.7% receiving acute dialysis, and 3% of patients died. At discharge, AKI and electrolyte abnormalities had dramatically improved. The prognosis factors for AKI receiving dialysis were identified as neurological status, renal function, and serum muscle enzyme at the time of admission.
Coagulation System Failure
HS has also been reported to result in the activation of the coagulation pathway and fibrin formation which is manifested as disseminated intravascular coagulation (DIC).35 The occurrence of DIC in the case of HS has been reported in original research studies,36 three case series37,38 and numerous case reports6,9–41 over the past 50 years. Hifumi et al40 reported the DIC in 708 HS patients. The diagnosis of DIC was made according to JAAM DIC diagnostic criteria41 The score consisted of systemic inflammatory response syndrome, platelet counts, prothrombin time, and fibrinogen/fibrin degradation products or D-dimer levels, and a total score of ≥4 established the diagnosis of DIC. It was reported that patients with scores ≥4 had higher odds of mortality during hospital stay (OR, 2.16; 95% CI, 1.09–4.27; p = 0.028). Another important finding was the increase in the mortality rate to 10% in patients who had a DIC score of 2. It was further reported that anti-thrombin levels were found to be significantly reduced in expired patients in comparison to alive patients (median [IQR]: 77%38,42–63 vs 98%,47,64–71 p = 0.02).
A study conducted by Ward et al44 reported the time-resolved progression of clinical laboratory disturbances days following an exertional heat stroke (EHS) in 2216 patients experiencing a total of 2529 HS episodes. The study participants were US Active-Duty Service Members (US Army, Navy, Air Force, and Marine Corps) serving from 2008 to 2014. It was reported that prothrombin times were found to be elevated 4 days after injury and remained outside the reference range from days 1–16 days. Corresponding decreases in hemoglobin, hematocrit, and red blood cells were observed from day 1 after injury and then persisted below the lower levels of normal for 6 days. Thirty-five percent of patients were found to have platelets below the lower levels of normal on 2nd day.
Hepatic System Damage
Hepatocellular injury is a well-documented complication of heat stroke, but few case reports [45–52] have described an association with acute liver injury or failure (ALI/ALF). Weigand et al reported two cases of liver failure associated with EHS, suggesting that HS and exhaustion were underestimated causes of liver failure.52 Garcin et al52 concluded that 22.7% of 110 patients progressed with liver failure.53–57 Recently, the ALF Study Group identified eight patients with HS in a prospective American cohort of 2675 patients with ALI.56 Hepatocellular necrosis is consequent to thermal and circulatory shock, endotoxemia, and cytokines with increased concentration and acute-phase proteins.55 However, the only predictor for the occurrence of liver failure was hypophosphatemia.55–57 There must be no evidence that hypophosphatemia is the cause of liver dysfunction. A report from the Acute Liver Failure Study Group found that 25% of deaths in patients with liver failure secondary to heat stroke were diagnosed between January 1988 and April 2015 in the United States.10 Varghese et al58 followed 28 HS victims and concluded that the high mortality of these cases is due to multiple organic dysfunctions.
Rhabdomyolysis
Severe heat stroke tends to be complicated by rhabdomyolysis, especially in patients with exertional heat stroke.59 Rhabdomyolysis may lead to systemic effects, including the local occurrence of compartment syndrome, hyperkalemic cardiac arrest, and/or lethal disseminated intravascular coagulopathy.60
Yoshizawa et al61 reported a case of a 34 years old male patient, found lying unconscious (GCS of 10) on the road after participating in a half marathon in the spring with a temperature of 24.2°C. A sedative was administered, and tracheal intubation was performed. On the second day of hospitalization, a blood analysis was compatible with a diagnosis of acute hepatic failure; thus, he received fresh frozen plasma and a platelet transfusion was performed, following plasma exchange and continuous hemodiafiltration. The patient’s creatinine phosphokinase (CPK) level increased to 8832 IU/L on the fifth day of hospitalization and then showed a tendency to transiently decrease. The patient was extubated on the 8th day of hospitalization. On the 9th day, rehabilitation was initiated gradually. His CPK level increased with pain in his legs again. Despite the cessation of all drugs and rehabilitation, his CPK level increased from 105 to 945 IU/L on the 15th day.62
Systemic Inflammatory Response Syndrome (SIRS) Criteria
The preliminary cardiovascular reaction to heat exposure or heat stroke is an elevation in skin blood flow that increases heat loss and deteriorates the level of heat exposure from the surrounding. Elevated skin blood flow is convoyed by a reduced splanchnic blood flow as an alternative mechanism for maintaining blood pressure. Reduced cerebral blood flow is further correlated with hyperthermia, ac-counting for CNS impairments, and presyncopal indications.63 The SIRS is classified as a reply to bacterial infection that follows disruption to the gut and other organs, ensuing elevated mitigations in splanchnic blood flow. Nitrosative and oxidative stress are promoted through the resultant ischemic environment that results in stricter gut junctions becoming leaky. Gram-positive and -negative bacteria are then aided for freely crossing the stricter junction restriction and entering into the systemic circulation.24–38,40–64
Risk Factors
Previous studies have compared risk factors among survival and non-survival heat stroke cases and found prolonged hospital stay in non-survival cases (p-value <0.001), significantly low mean among non-survived patients (p-value = 0.001), high core body temperature, ie, 42.454 ± 1.082°C (p-value = 0.001), increased mean lactate, ie, 8.756 ± (p-value = 0.001, increased mean white blood cells (WBCs) values of 19.623 ± 7.612 (p-value = 0.001), increased mean creatinine (3.992 ± 2.263) and BUN (46.325 ± 27.940), increased AST (1445.125 ± 2829.278) and AST (810.174 ± 1566.975) among non-survival patients. While the heart rate (HR), respiratory rate (RR), systolic blood pressure (SBP), and diastolic blood pressure (DBP) had no significant effect on the prognosis of heat stroke patients. The results have shown no significant value in the outcome of the patients based on PT, PTT, INR, and CK-CPK.
Conclusion
This study concludes that HS is a life-threatening condition marked by neurological disorders, damage in the hepatic system, renal system, coagulation failure, muscular-skeletal system, and cardiovascular system. Untreated heat stroke might exacerbate psychosis, lactic acidosis, consumptive coagulopathy, haematuria, pulmonary edema, renal failure, and other metabolic abnormalities. This review elucidated that core body temperature and white blood cell count are pivotal determinants influencing the outcomes of heat stroke. Certain simple preventive measures can effectively reduce the prevalence of both classic and exertional heatstroke. These measures include refraining from engaging in strenuous physical activity in hot environments and minimizing exposure to heat stress. In contrast, there is a significant lack of understanding regarding the pathophysiology of heat stroke and its relationship to systemic inflammatory response syndrome (SIRS), which is crucial for comprehending the factors that contribute to mortality and morbidity. It is crucial to recognize the significance of novel biotechnologies in advancing our understanding of the pathophysiology of heat stroke. The utilization of these technologies will play a crucial role in enhancing comprehension of Systemic Inflammatory Response Syndrome (SIRS) and devising innovative approaches to mitigate the mortality and morbidity associated with heat stroke. This will be achieved through the integration of novel in vitro, in silico, and in vivo models. One of the limitations inherent in our study was the relatively brief duration of the study period, coupled with a predominance of case reports. However, it was observed through case presentations that males exhibited a higher susceptibility to heat stroke and were more significantly impacted by its associated complications.
Acknowledgments
The author is very thankful to all the associated personnel in any reference that contributed to/for this research.
Disclosure
The author declares no competing interest.
References
- 1.Sankoff J. Environmental: heat illnesses: a hot topic in the setting of global climate change. Aust Fam Physician. 2015;44(1/2):22–26. [PubMed] [Google Scholar]
- 2.Higareda-Basilio AE, Trujillo-Narvaez FA, Jaramillo-Ramirez HJ. Mortality and functional disability in heat stroke. Salud Publica Mex. 2019;61(12):99–100. doi: 10.21149/9849 [DOI] [PubMed] [Google Scholar]
- 3.Nelson DA, Deuster PA, O’Connor FG, Kurina LM. Timing and predictors of mild and severe heat illness among new military enlistees. Med Sci Sports Exerc. 2018;50(8):1603. doi: 10.1249/MSS.0000000000001623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician. 2005;71(11):2133–2140. [PubMed] [Google Scholar]
- 5.Parsons IT, Stacey MJ, Woods DR. Heat adaptation in military personnel: mitigating risk, maximizing performance. Front Physiol. 2019;10:1485. doi: 10.3389/fphys.2019.01485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li S, Feng L, Liu Z, Li T, Wang Y. Emergent treatment and physical cooling for older adults with nonexertional heatstroke: a retrospective analysis of 24 cases. Acta Clin Croat. 2021;60(4). [Google Scholar]
- 7.Bouchama A, Abuyassin B, Lehe C, et al. Classic and exertional heatstroke. Nat Rev Dis Primers. 2022;8(1). doi: 10.1038/s41572-021-00334-6 [DOI] [PubMed] [Google Scholar]
- 8.Laitano O, Leon LR, Roberts WO, Sawka MN. Controversies in exertional heat stroke diagnosis, prevention, and treatment. J Appl Physiol. 2019;127(5):1338–1348. doi: 10.1152/japplphysiol.00452.2019 [DOI] [PubMed] [Google Scholar]
- 9.Kushimoto S, Yamanouchi S, Endo T, et al. Body temperature abnormalities in non-neurological critically ill patients: a review of the literature. J Intensive Care. 2014;2:1–6. doi: 10.1186/2052-0492-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hymczak H, Gołąb A, Mendrala K, et al. Core temperature measurement—principles of correct measurement, problems, and complications. Int J Environ Res Public Health. 2021;18(20):10606. doi: 10.3390/ijerph182010606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiran AA, Khichar JP. Clinico-physiological manifestations of heat stroke in exotic and crossbred cattle. Pulse. 2022;62(1.2792a):113–169. [Google Scholar]
- 12.Wang JC, Chien WC, Chu P, Chung CH, Lin CY, Tsai SH. The association between heat stroke and subsequent cardiovascular diseases. PLoS One. 2019;14(2):e0211386. doi: 10.1371/journal.pone.0211386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmeltz MT, Marcotullio PJ, Himmelstein DU, Woolhandler S, Sembajwe G. Outcomes of hospitalizations for common illnesses associated with a comorbid heat-related illness in the United States, 2001–2010. Clim Change. 2016;138:567–584. doi: 10.1007/s10584-016-1747-5 [DOI] [Google Scholar]
- 14.Chen WT, Lin CH, Hsieh MH, Huang CY, Yeh JS. Stress-induced cardiomyopathy caused by heat stroke. Ann Emerg Med. 2012;60(1):63–66. doi: 10.1016/j.annemergmed.2011.11.005 [DOI] [PubMed] [Google Scholar]
- 15.Tustin AW, Cannon DL, Arbury SB, Thomas RJ, Hodgson MJ. Risk factors for heat-related illness in US workers: an OSHA case series. J Occup Environ Med. 2018;60(8):e383–9. doi: 10.1097/JOM.0000000000001365 [DOI] [PubMed] [Google Scholar]
- 16.Williams ML. Global warming, heat-related illnesses, and the dermatologist. Int J Womens Dermatol. 2021;7(1):70–84. doi: 10.1016/j.ijwd.2020.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Misset B, De Jonghe B, Bastuji-Garin S, et al. Mortality of patients with heatstroke admitted to intensive care units during the 2003 heat wave in France: a national multiple-center risk-factor study. Indian J Crit Care Med. 2006;34(4):1087–1092. [DOI] [PubMed] [Google Scholar]
- 18.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomized studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–1988. doi: 10.1056/nejmra011089 [DOI] [PubMed] [Google Scholar]
- 20.Douma MJ, Aves T, Allan KS, et al. First aid cooling techniques for heat stroke and exertional hyperthermia: a systematic review and meta-analysis. Resuscitation. 2020;148:173–190. doi: 10.1016/j.resuscitation.2020.01.007 [DOI] [PubMed] [Google Scholar]
- 21.Bynum GD, Pandolf KB, Schuette WH, Goldman RF, Lees DE, Bull JM. Induced hyperthermia in sedated humans and the concept of critical thermal maximum. Am J Physiol Regul Integr Comp Physiol. 1978;235(5):R228–R236. doi: 10.1152/ajpregu.1978.235.5.R228 [DOI] [PubMed] [Google Scholar]
- 22.Lin MT, Liu HH, Yang YL. Involvement of interleukin-1 receptor mechanisms in the development of arterial hypotension in rat heatstroke. Am J Physiol Heart Circ Physiol. 1997;273(4):H2072–7. doi: 10.1152/ajpheart.1997.273.4.H2072 [DOI] [PubMed] [Google Scholar]
- 23.Lu KC, Wang JY, Lin SH, Chu P, Lin YF. Role of circulating cytokines and chemokines in exertional heatstroke. Indian J Crit Care Med. 2004;32(2):399–403. [DOI] [PubMed] [Google Scholar]
- 24.Bouchama A, Bridey F, Hammami MM, et al. Activation of coagulation and fibrinolysis in heatstroke. Thromb Haemost. 1996;76(12):15. doi: 10.1055/s-0038-1650685 [DOI] [PubMed] [Google Scholar]
- 25.Jones TS, Liang AP, Kilbourne EM, et al. Morbidity and mortality associated with the July 1980 heat wave in St Louis and Kansas City. JAMA. 1982;247(24):3327–3331. doi: 10.1001/jama.1982.03320490025030 [DOI] [PubMed] [Google Scholar]
- 26.Akhtar MJ, Al-Nozha M, Al-Harthi S, Nouh MS. Electrocardiographic abnormalities in patients with heat stroke. Chest. 1993;104(2):411–414. doi: 10.1378/chest.104.2.411 [DOI] [PubMed] [Google Scholar]
- 27.Mimish L. Electrocardiographic findings in heat stroke and exhaustion: a study on Makkah pilgrims. J Saudi Heart Assoc. 2012;24(1):35–39. doi: 10.1016/j.jsha.2011.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abriat A, Brosset C, Brégigeon M, Sagui E. Report of 182 cases of exertional heatstroke in the French Armed Forces. Mil Med. 2014;179(3):309–314. doi: 10.7205/MILMED-D-13-00315 [DOI] [PubMed] [Google Scholar]
- 29.Li J, Zhang XY, Zou ZM, Wang B, Xia JK. Heat stroke: typical MRI and 1H-MRS features. Clin Imaging. 2015;39(3):504–505. doi: 10.1016/j.clinimag.2014.12.011 [DOI] [PubMed] [Google Scholar]
- 30.Yang M, Li Z, Zhao Y, et al. Outcome and risk factors associated with the extent of central nervous system injury due to exertional heat stroke. Medicine. 2017;96(44):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamamoto T, Todani M, Oda Y, et al. Predictive factors for hospitalization of patients with heat illness in Yamaguchi, Japan. Int J Environ Res Public Health. 2015;12(9):11770–11780. doi: 10.3390/ijerph120911770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamaya H, Hifumi T, Kawakita K, et al. Successful management of heat stroke associated with multiple-organ dysfunction by active intravascular cooling. Am J Emerg Med. 2014;33(1):124–e5. [DOI] [PubMed] [Google Scholar]
- 33.Satirapoj B, Kongthaworn S, Choovichian P, Supasyndh O. Electrolyte disturbances and risk factors of acute kidney injury patients receiving dialysis in exertional heat stroke. BMC Nephrol. 2016;17:1–6. doi: 10.1186/s12882-016-0268-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jilma B, Derhaschnig U. Disseminated intravascular coagulation in heat stroke: a hot topic. Indian J Crit Care Med. 2012;40(4):1370–1372. [DOI] [PubMed] [Google Scholar]
- 35.Bouchama A, Al-Mohanna F, Assad L, et al. The tissue factor/factor VIIa pathway mediates coagulation activation in induced-heat stroke in the baboon. Indian J Crit Care Med. 2012;40(4):1229–1236. [DOI] [PubMed] [Google Scholar]
- 36.Huisse MG, Pease S, Hurtado-Nedelec M, et al. Leukocyte activation: the link between inflammation and coagulation during heatstroke. A study of patients during the 2003 heat wave in Paris. Indian J Crit Care Med. 2008;36(8):2288–2295. [DOI] [PubMed] [Google Scholar]
- 37.Sonkar SK, Soni D, Sonkar GK. Heat stroke presented with disseminated intravascular coagulation and bilateral intracerebral bleed. Case Rep. 2012; 2012:bcr2012007027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trujillo MH, Fragachán G. Rhabdomyolysis and acute kidney injury due to severe heat stroke. Case Rep Crit Care. 2011;2011:1–4. doi: 10.1155/2011/951719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wells GA, Shea B, O’Connell DA, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandom studies in meta-analyses; 2000.
- 40.Hifumi T, Kondo Y, Shimazaki J, et al. Prognostic significance of disseminated intravascular coagulation in patients with heat stroke in a nationwide registry. J Crit Care. 2018;44:306–311. doi: 10.1016/j.jcrc.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 41.Ward MD, King MA, Gabrial C, Kenefick RW, Leon LR. Biochemical recovery from exertional heat stroke follows a 16-day time course. PLoS One. 2020;15(3):e0229616. doi: 10.1371/journal.pone.0229616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wakino S, Hori S, Mimura T, et al. Heat stroke with multiple organ failure treated with cold hemodialysis and cold continuous hemodiafiltration: a case report. Ther Apher Dial. 2015;9(5):423–428. doi: 10.1111/j.1744-9987.2005.00321.x [DOI] [PubMed] [Google Scholar]
- 43.Miyake Y. Pathophysiology of heat illness: thermoregulation, risk factors, and indicators of aggravation. Japan Med Assoc J. 2013;56(3):167–173. [Google Scholar]
- 44.Gando S, Saitoh D, Ogura H, Mayumi T, Koseki K, Ikeda T; and Japanese Association for Acute Medicine Disseminated Intravascular Coagulation (JAAM DIC) Study Group. Disseminated intravascular coagulation (DIC) diagnosed based on the Japanese Association for Acute Medicine criteria is a dependent continuum to overt DIC in patients with sepsis. Thromb Res. 2009;123:715–718. doi: 10.1016/j.thromres.2008.07.006 [DOI] [PubMed] [Google Scholar]
- 45.Singh RK, Baronia AK, Sahoo JN, et al. Prospective comparison of new Japanese Association for Acute Medicine (JAAM) DIC and International Society of Thrombosis and Hemostasis (ISTH) DIC score in critically ill septic patients. Thromb Res. 2012;129:e119–e125. doi: 10.1016/j.thromres.2011.11.017 [DOI] [PubMed] [Google Scholar]
- 46.Erarslan E, Yüksel Í, Haznedaroğ Lu S. Acute liver failure due to non-exertional heatstroke after sauna. Ann Hepatol. 2012;11:138–142. doi: 10.1016/S1665-2681(19)31499-1 [DOI] [PubMed] [Google Scholar]
- 47.Azzopardi N, Chetcuti S, Sant J, Pocock J. Acute liver impairment in a young, healthy athlete: hypoxic hepatitis and rhabdomyolysis following heat stroke. Case Rep Gastroenterol. 2012;6(2):563–568. doi: 10.1159/000338838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carvalho AS, Rodeia SC, Silvestre J, Póvoa P. Exertional heat stroke and acute liver failure: a late dysfunction. Case Rep. 2016; 2016:bcr2016214434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carter R, Cheuvront SN, Williams JO, et al. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc. 2005;37:1338. doi: 10.1249/01.mss.0000174895.19639.ed [DOI] [PubMed] [Google Scholar]
- 50.Weigand K, Riediger C, Stremmel W, Flechtenmacher C, Encke J. Are heat stroke and physical exhaustion underestimated causes of acute hepatic failure? World J Gastroenterol. 2007;13:306. doi: 10.3748/wjg.v13.i2.306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garcin JM, Bronstein JA, Cremades S, Courbin P, Cointet F. Acute liver failure is frequent during heat stroke. World J Gastroenterol. 2008;14:158. doi: 10.3748/wjg.14.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davis BC, Tillman H, Chung RT, Stravitz RT, Reddy R, Fontana RJ; Acute Liver Failure Study Group. Heat stroke leading to acute liver injury and failure: a case series from the Acute Liver Failure Study Group. Liver Int. 2007;37:509–513. doi: 10.1111/liv.13373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Salathé C, Pellaton C, Carron PN, Coronado M, Liaudet L. Acute liver failure complicating exertional heat stroke: possible role of hypophosphatemia. Curr Sports Med Rep. 2015;14:49–50. doi: 10.1249/JSR.0000000000000113 [DOI] [PubMed] [Google Scholar]
- 54.Varghese GM, John G, Thomas K, Abraham OC, Mathai D. Predictors of multi-organ dysfunction in heatstroke. Emerg Med J. 2005;22:185–187. doi: 10.1136/emj.2003.009365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brown J, Mitchell S. A complicated case of exertional heat stroke in a military setting with persistent elevation of creatine phosphokinase. Mil Med. 1992;157:101–103. doi: 10.1093/milmed/157.2.101 [DOI] [PubMed] [Google Scholar]
- 56.Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis–an overview for clinicians. Crit Care. 2004;9:1–12. doi: 10.1186/cc2978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Castro T, D. RRT, Costa Filho R, Nóbrega ACLD. Fulminant liver failure in a street runner: effects of heat stroke. Rev Assoc Med Bras. 2018;64:208–221. doi: 10.1590/1806-9282.64.03.208 [DOI] [PubMed] [Google Scholar]
- 58.Yoshizawa T, Omori K, Takeuchi I, et al. Heat stroke with bimodal rhabdomyolysis: a case report and review of the literature. J Intensive Care. 2016;4:1–5. doi: 10.1186/s40560-016-0193-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nyb L. Exercise, and heat stress: cerebral challenges and consequences. Prog Brain Res. 2007;162:29–43. [DOI] [PubMed] [Google Scholar]
- 60.Thongprayoon C, Petnak T, Kanduri SR, et al. Impact of rhabdomyolysis on outcomes of hospitalizations for heat stroke in the United States. Hosp Pract. 2020;48:276–281. doi: 10.1080/21548331.2020.1792214 [DOI] [PubMed] [Google Scholar]
- 61.Bradfield JB. Control of spillover: the importance of Kupffer-cell function in clinical medicine. Lancet. 1974;304:883–886. doi: 10.1016/S0140-6736(74)91213-6 [DOI] [PubMed] [Google Scholar]
- 62.Szold O, Reider-Groswasser II, Abraham RB, et al. Gray–white matter discrimination—a possible marker for brain damage in heat stroke? Eur J Radiol. 2002;43:1–5. doi: 10.1016/S0720-048X(01)00467-3 [DOI] [PubMed] [Google Scholar]
- 63.Patel DR, Gyamfi R, Torres A. Exertional rhabdomyolysis and acute kidney injury. Phys Sportsmed. 2009;37:71–79. doi: 10.3810/PSM.2009.04.1685 [DOI] [PubMed] [Google Scholar]
- 64.Wu B, Gong D, Ji D, Xu B, Liu Z. Clearance of myoglobin by high cutoff continuous venovenous hemodialysis in a patient with rhabdomyolysis. Hemodial Int. 2015;19:135–140. doi: 10.1111/hdi.12172 [DOI] [PubMed] [Google Scholar]
- 65.Asserraji M, Benameur I, Maoujoud O, El Kharras A, Hajbi H, Filali K. Late care in marathon runs leads to exertional heat stroke with multiple organ failure. Asian J Sports Med. 2014;5:136. [PMC free article] [PubMed] [Google Scholar]
- 66.Raj VMS, Alladin A, Pfeiffer B, et al. Therapeutic plasma exchange in the treatment of exertional heat stroke and multiorgan failure. Pediatr Nephrol. 2013;28:971–974. doi: 10.1007/s00467-013-2409-8 [DOI] [PubMed] [Google Scholar]
- 67.Horseman MA, Rather-Conally J, Saavedra C, Surani S. A case of severe heatstroke and review of pathophysiology, clinical presentation, and treatment. Intern Med J. 2013;28:334–340. [DOI] [PubMed] [Google Scholar]
- 68.Shiota M, Kusakabe H, Izumi Y, et al. Heat shock cognate protein 70 is essential for Akt signaling in endothelial function. Arterioscler Thromb Vasc Biol. 2010;30:491–497. doi: 10.1161/ATVBAHA.109.193631 [DOI] [PubMed] [Google Scholar]
- 69.Lee CW, Perng CL, Huang YS, Luo JC, Hung CL, Lin HC. Multiple organ failure caused by non-exertional heat stroke after bathing in a hot spring. J Chin Med Assoc. 2010;73:212–215. doi: 10.1016/S1726-4901(10)70044-7 [DOI] [PubMed] [Google Scholar]
- 70.Niu Z, Liu F, Yan Q, Li L. Effects of different levels of selenium on growth performance and immunocompetence of broilers under heat stress. Arch Anim Nutr. 2009;63:56–65. doi: 10.1080/17450390802611610 [DOI] [PubMed] [Google Scholar]
- 71.Latten GH, Spek M, Muris JW, Cals JW, Stassen PM. Accuracy and interobserver-agreement of respiratory rate measurements by healthcare professionals, and its effect on the outcomes of clinical prediction/diagnostic rules. PLoS One. 2019;14:e0223155. doi: 10.1371/journal.pone.0223155 [DOI] [PMC free article] [PubMed] [Google Scholar]