Abstract
BACKGROUND/OBJECTIVES
Probiotics have been suggested as potent modulators of age-related disorders in immunological functions, yet little is known about sex-dependent effects of probiotic supplements. Therefore, we aimed to investigate sex-dependent effects of probiotics on profiles of the gut microbiota and peripheral immune cells in healthy older adults.
SUBJECTS/METHODS
In a randomized, double-blind, placebo-controlled, multicenter trial, healthy elderly individuals ≥ 65 yrs old were administered probiotic capsules (or placebo) for 12 wk. Gut microbiota was analyzed using 16S rRNA gene sequencing and bioinformatic analyses. Peripheral immune cells were profiled using flow cytometry for lymphocytes (natural killer, B, CD4+ T, and CD8+ T cells), dendritic cells, monocytes, and their subpopulations.
RESULTS
Compared with placebo, phylum Firmicutes was significantly reduced in the probiotic group in women, but not in men. At the genus level, sex-specific responses included reductions in the relative abundances of pro-inflammatory gut microbes, including Catabacter and unclassified_Coriobacteriales, and Burkholderia and unclassified Enterobacteriaceae, in men and women, respectively. Peripheral immune cell profiling analysis revealed that in men, probiotics significantly reduced the proportions of dendritic cells and CD14+ CD16- monocytes; however, these effects were not observed in women. In contrast, the proportion of total CD4+ T cells was significantly reduced in women in the probiotic group. Additionally, serum lipopolysaccharide-binding protein levels showed a decreasing tendency that were positively associated with changes in gut bacteria, including Catabacter (ρ = 0.678, P < 0.05) and Burkholderia (ρ = 0.673, P < 0.05) in men and women, respectively.
CONCLUSIONS
These results suggest that probiotic supplementation may reduce the incidence of inflammation-related diseases by regulating the profiles of the gut microbiota and peripheral immune cells in healthy elders in a sex-specific manner.
Keywords: Probiotics, gut microbiota, fluorescence-activated cell sorting, healthy aging, sex difference
INTRODUCTION
Aging is characterized by a progressive decline in biological functions of the organism. Many theories have been suggested to explain the cause of aging, such as programmed aging, telomeres, and redox theory. Another hallmark of aging is immunosenescence, with age-related changes in the immune system characterized by reduced phagocytic function of neutrophils, changes in B-cell populations, and diminished function and increased population of dendritic cells (DCs) [1]. As a result of immunosenescence, the immune-cell-mediated clearance of senescent cells is defective, which leads to a chronic low-grade inflammatory status called inflammaging [2]. Age-related disorders in immune surveillance are highly implicated in age-related chronic diseases, such as metabolic syndrome, cancer, and neurodegenerative diseases [1,2,3].
Studies have shown that dysbiosis of the gut microbiota is a major contributor to adverse health outcomes and development of age-related disorders [4,5,6]. Therefore, a few strategies for promoting health through manipulating the gut microbiota with probiotics, prebiotics, and fecal microbiota transplantation have been actively studied, with a special emphasis on the immune function of the host [4,7]. In particular, probiotics (live microorganisms that are beneficial to the host when consumed) act as immunoregulatory agents by modulating the gut microbiota. For example, some strains of Bifidobacteria and lactic acid bacteria enhanced immunity in elderly individuals with increased proportion of peripheral T cells and enhanced activity of circulating natural-killer (NK) cells [8,9]. In addition, supplementation with Lactobacillus in healthy elderly individuals changed the functional characteristics of resident microbes related to anti-inflammatory pathways. These findings provide evidence that probiotic microorganisms are promising agents for the deleterious effects of immunosenescence on cellular immunity via regulation of the gut microbiota. However, previous studies on the effects of probiotics on immunosenescence had a relatively short intervention period of less than 9 wk.
The effects of dietary intervention vary between sexes because of differences in biological and physiological characteristics between men and women, which are major factors contributing to inter-individual differences in response to dietary intervention [10]. Therefore, understanding the sex differences in response to dietary interventions is necessary to provide appropriate nutritional strategies for men and women. For example, it has been reported that insulin levels decreased in men but not in women after the 4-week intervention with a Mediterranean diet [11]. Without such a study evaluating sex differences, we would not be able to confirm that the Mediterranean diet is effective in lowering insulin levels in men but not in women. Therefore, it is essential to address sex-dependent differences in dietary intervention studies to provide sex-specific nutritional care [12]. However, little is known about the sex differences in the effects of probiotic supplementation. Therefore, we conducted a randomized, double-blind, placebo-controlled, multicenter trial to address the different effects of probiotic supplementation in men and women, with a focus on the profiles of gut microbiota and peripheral immune cells in community-dwelling elderly individuals.
SUBJECTS AND METHODS
Study design and participants
The study was a 12-wk randomized, double-blind, placebo-controlled, multicenter clinical trial examining the effects of probiotic consumption in healthy elderly individuals aged > 65 yrs, conducted at Seoul National University (Seoul, Republic of Korea) and Jesaeng Hospital (Seongnam, Republic of Korea) from March 2018 to March 2019. Details of the recruitment and eligibility of the participants have been previously described [13]. All participants involved in the study gave their informed consent for participation of the study. The study was conducted in accordance with the Declaration of Helsinki, and the study was approved and monitored by the Institutional Review Boards of Seoul National University (IRB No. 1801/002-015) and Bundang Jesaeng Hospital (IRB No. IMCN18-01). This study was registered with the Clinical Research Information Service (http://cris.nih.go.kr; registration ID: KCT0003929).
Probiotic intervention
Details of the probiotic intervention have been described previously [13]. Briefly, the participants were randomly assigned to one the study groups based on a random number that was generated by an independent study coordinator using GraphPad Prism (version 6.05; GraphPad Software, San Diego, CA, USA). The random sequence was stratified by sex with 1:1 allocation and was concealed from all participants and the researchers. Participants consumed either placebo or probiotic capsules after meals in the morning and evening. Participants in the placebo group took 4 capsules containing 500 mg of soybean oil without probiotics per day. Participants in the probiotics group consumed a total of 4 capsules (1 × 109 CFU of Bifidobacterium bifidum BGN4 and Bifidobacterium longum BORI in soybean oil) per day. These placebo and probiotic capsules cannot be distinguished by package, color, taste, or smell to keep the treatment allocation blind to participants and study staff.
Sample collection
Participants visited for the collection of blood and stool samples at baseline (wk 0) and wk 4, 8, and 12. Fasting (12 h) blood samples were collected into serum separator tubes for serum isolation, which were then aliquoted and immediately stored at −80°C for later analysis. Whole blood samples were collected for peripheral blood mononuclear cell (PBMC) isolation. PBMC isolation occurred within 2 h of blood collection. For stool sample collection, we provided stool collection kits and instructed participants to perform a manual stool collection. Participants were asked to collect fecal samples within a 48-h period before visiting, and stool samples were collected at each visit. Stool samples for gut microbiota analysis were collected with stool nucleic acid collection and preservation tubes (Norgen Biotek, Thorold, ON, Canada), and delivered to the laboratory at room temperature. Aliquots of 180–200 mg stool samples were immediately stored at −80°C until further analysis.
Outcome assessments
Gut microbiota analysis
Genomic DNA extraction: Total bacterial DNA was isolated from stool samples using the QIAamp® Fast DNA Stool Mini Kit (QIAGEN, Hilden, Germany) according to the manufacturer’s instructions and using the following additional steps. The extracted genomic DNA was confirmed by gel electrophoresis and quantified using a NanoDrop ND-2000 spectrophotometer (Thermo Scientific, Waltham, MA, USA).
Amplification of the 16S ribosomal ribonucleic acid gene and sequencing: Hypervariable regions (V3-V4) of the 16S ribosomal ribonucleic acid (rRNA) gene were amplified using barcoded universal primers for each sample. Polymerase chain reaction (PCR) was performed using BioFact F-Star Taq DNA polymerase (BioFACT™, Seoul, Republic of Korea). Briefly, a final volume of 50 μL of PCR reaction contained about 20 ng of DNA template, 5 μL of 10X Taq buffer (20 mM Mg2+), 1 μL of 10 mM dNTP mix, 2 μL of forward and reverse barcoded primers (10 pmol/μL), and 0.25 μL of DNA polymerase. PCR reactions were performed using a GeneAmp® PCR system 9700 (Applied Biosystems, Foster City, CA, USA). The PCR program was as follows: initial denaturation for 5 min at 94°C, followed by 28 cycles of denaturation (30 s at 95°C), annealing (30 s at 60°C), and extension (30 s at 72°C), with a final extension step (10 min at 72°C), followed by holding at 4°C. The PCR product was confirmed by 1% agarose gel electrophoresis and visualized using a Gel Doc system (BioRad, Hercules, CA, USA). The amplified products were purified with the PureLink Quick Gel Extraction and PCR Purification Combo Kit (Invitrogen, Carlsbad, CA, USA) and quantified using a Qubit 2.0 fluorometer (Invitrogen). Library size was assessed using a BioAnalyzer (Agilent Technologies, Santa Clara, CA, USA). Amplicons were pooled and sequenced using an Illumina MiSeq sequencing system (Illumina, San Diego, CA, USA).
Bioinformatics analysis of sequencing data: Microbial sequences were processed using QIIME2 (version 2019.1) [14]. Briefly, sequences were denoised to remove sequences with low-quality scores and chimeras via DADA2. Then, the denoised sequences were clustered into operational taxonomic units (OTUs), and OTU representative sequences were aligned based on the SILVA database (version 132) at 99% sequence identity with the scikit-learn Naïve Bayes-based machine-learning classifier. A phylogenetic tree was generated using the MAFFT and FastTree methods for diversity analyses. Downstream analyses of alpha diversity were performed to measure dissimilarities in the richness and evenness of the microbial community. Comparisons of relative abundance between the groups were performed to identify differential features across the samples.
Fluorescence-activated cell sorting (FACS) analysis
PBMC were isolated from whole blood samples using Ficoll-Hystopaque (Sigma Diagnostics, Inc., Livonia, MI, USA). Isolated PBMC were resuspended in FACS buffer (1X phosphate-buffered saline, 0.1% bovine calf serum, and 0.05% sodium azide) and then stained with the following antibodies for 30 min at 4°C: BV711 conjugated anti-human CD3e, APC.Cy7 conjugated anti-human CD4, Alexa Fluor 700 conjugated anti-human CD8, APC conjugated anti-human CD11c, PE-conjugated anti-human CD14, FITC-conjugated anti-human CD16, V421 conjugated anti-human CD27, APC conjugated anti-human CD28, FITC conjugated anti-human CD45RA, PE conjugated anti-human CD197, PE.Cy5 conjugated anti-human HLA-DR (BD Pharmingen, San Jose, CA, USA), APC.eFluor 780 conjugated anti-human CD11b, PE.Cy7 conjugated anti-human CD19 (ThermoFisher, Carlsbad, CA, USA), and Brilliant Violet785 conjugated anti-human CD56 (BioLegend, San Diego, CA, USA). After sufficient washing with FACS buffer, the stained cells were analyzed with FACS LSRII (BD Biosciences, Franklin Lakes, NJ, USA) and FlowJo software (TreeStar, Ashland, OR, USA).
Serum biochemical markers
Serum C-reactive protein (CRP, DY1707; R&D Systems, Germany) and lipopolysaccharide-binding protein (LBP, ab279407; Abcam, UK) levels were measured using an enzyme-linked immunosorbent assay kit according to the manufacturer’s instructions.
Statistical analysis
Sample size was calculated considering a dropout rate of 20%, with a two-sided 5% significance level and a power of 80% to detect a statistical significance. The study variables were tested for normality and homogeneity of variance using the Kolmogorov–Smirnov test. Baseline values were compared between groups using independent t-tests, χ2 tests, or Fisher’s exact tests. Comparison analysis between groups for delta values (Δ(wk4-wk0), Δ(wk8-wk0), and Δ(wk12-wk0)) was conducted using the unpaired t-test or Mann–Whitney U test. Association analyses between variables were performed using the Spearman’s correlation or Spearman’s rank correlation method. The false discovery rate (FDR) was used for multiple testing correction. The P-value < 0.05 and FDR < 0.05 were considered statistically significant in all statistical analyses. All statistical analyses were conducted using SPSS (version 26.0; SPSS Inc., Chicago, IL, USA) or GraphPad Prism (version 9.4.0; GraphPad Software).
RESULTS
General characteristics of participants at baseline
To examine sex differences in the effects of probiotic consumption on the gut microbiota and peripheral immune cell population in healthy elderly individuals, we conducted a 12-wk randomized, double-blind, placebo-controlled, multicenter clinical trial. A total of 63 healthy elderly individuals participated in the study and were randomly assigned to either the placebo or probiotics group (Supplementary Fig. 1). In the present study, we conducted sex-stratified analyses to unravel the sex differences in probiotic intervention in the elderly population, resulting in a relatively uneven ratio of participants in the experimental group, but the difference was not significant (38.46% and 62.96% of participants in the probiotic group in the male and female populations, respectively; P = 0.07, Table 1). The demographic and clinical characteristics according to sex at baseline are summarized in Table 1. There was no significant difference in the average age across the groups in both men and women. Average age was 72.63 and 72.70 yrs old in the placebo and probiotics group, respectively, among men (P = 0.97); and 71.00 and 70.18 yrs in the placebo and probiotics group, respectively, among women (P = 0.62). Socioeconomic and clinical characteristics, including educational level, marital status, type of household, cigarette use, alcohol use, physical activity, and subjective health status, were not statistically different across groups in both men and women.
Table 1. General characteristics of participants at baseline by sex.
| Variables | Men | Women | P-value | |||||
|---|---|---|---|---|---|---|---|---|
| Placebo | Probiotics | P-value | Placebo | Probiotics | P-value | |||
| Participants | 16 (61.54) | 10 (38.46) | 10 (37.04) | 17 (67.96) | 0.07 | |||
| Age (yrs) | 72.63 ± 0.96 | 72.70 ± 1.58 | 0.97 | 71.00 ± 0.70 | 70.18 ± 1.20 | 0.62 | ||
| BMI (kg/m2) | 25.12 ± 0.58 | 23.88 ± 0.63 | 0.18 | 24.08 ± 1.18 | 22.79 ± 0.71 | 0.33 | ||
| Education | 0.49 | 0.33 | ||||||
| Elementary or less | 2 (12.50) | 0 (0) | 1 (10.00) | 6 (35.29) | ||||
| Junior-high school | 2 (12.50) | 3 (30.00) | 4 (40.00) | 3 (17.65) | ||||
| High school | 4 (25.00) | 3 (30.00) | 2 (20.00) | 5 (29.41) | ||||
| College or more | 8 (50.00) | 4 (40.00) | 4 (40.00) | 3 (17.65) | ||||
| Marital status | 0.99 | 0.21 | ||||||
| Divorced/separated | 1 (6.25) | 1 (10.00) | 0 (0) | 2 (11.77) | ||||
| Widowed | 0 (0) | 0 (0) | 1 (10.00) | 5 (29.41) | ||||
| Married | 15 (93.75) | 9 (90.00) | 9 (90.00) | 10 (58.82) | ||||
| Lives | 0.99 | 0.36 | ||||||
| Alone | 1 (6.25) | 5 (50.00) | 1 (10.00) | 8 (47.06) | ||||
| With others | 15 (93.75) | 5 (50.00) | 9 (90.00) | 9 (52.94) | ||||
| Smoking status | 0.22 | 0.37 | ||||||
| Never | 9 (56.25) | 7 (70.00) | 9 (90.00) | 17 (100.00) | ||||
| Ever | 3 (18.75) | 3 (30.00) | 0 (0) | 0 (0) | ||||
| Current | 4 (25.00) | 0 (0) | 1 (10.00) | 0 (0) | ||||
| Drinking status | 0.23 | 0.52 | ||||||
| Never | 6 (37.50) | 1 (10.00) | 7 (70.00) | 10 (58.82) | ||||
| Ever | 1 (6.25) | 2 (20.00) | 0 (0) | 2 (11.77) | ||||
| Current | 9 (56.25) | 7 (70.00) | 3 (30.00) | 5 (29.41) | ||||
| Physical activity | 0.99 | 0.52 | ||||||
| No | 1 (6.25) | 0 (0) | 0 (0) | 2 (11.77) | ||||
| Yes | 15 (93.75) | 10 (100.00) | 10 (100.00) | 15 (88.23) | ||||
| Health status | 0.22 | 0.20 | ||||||
| Excellent | 2 (12.50) | 4 (40.00) | 1 (10.00) | 6 (35.30) | ||||
| Good | 13 (81.25) | 5 (50.00) | 6 (60.00) | 9 (52.94) | ||||
| Fair | 1 (6.25) | 1 (10.00) | 3 (30.00) | 1 (5.88) | ||||
| Poor | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||||
| Very poor | 0 (0) | 0 (0) | 0 (0) | 1 (5.88) | ||||
| Energy intake (kcal/d) | 1,681.69 ± 93.34 | 1,673.84 ± 185.54 | 0.97 | 1,447.36 ± 122.96 | 1,425.08 ± 65.34 | 0.86 | ||
Data are presented as the mean ± SEM or number (%).
P-value was based on the t-test, χ2 test, or Fisher’s exact test.
BMI, body mass index.
Different effects of probiotic supplementation on the gut microbial community depending on sex
To investigate whether there was a sex difference in the gut microbiota in response to probiotic supplementation, we conducted 16S rRNA gene sequencing analysis before and after probiotic intervention. First, we found that the baseline values of diversity indices were not significantly different between the placebo and probiotics groups in both men and women (Supplementary Fig. 2), and changes in diversity indices were compared between the placebo and probiotics groups in men and women. In the male population, the changes in diversity indices, including Pielou’s evenness index, Faith’s phylogenetic diversity, number of observed OTUs, and Shannon’s diversity index, which were measured at weeks 4, 8, and 12, were not significantly different between the two groups (Supplementary Fig. 2A–D). The results were similar in the female population, as the changes in diversity indices showed no statistical differences between the two groups at any time point (Supplementary Fig. 2A–D).
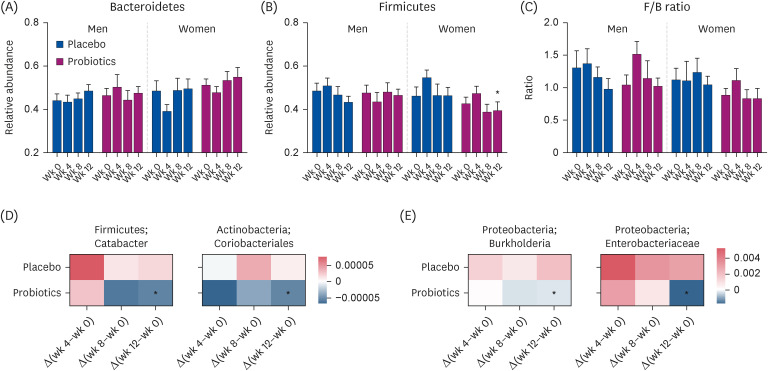
Next, we examined the changes in the bacterial community at various taxonomic levels. At the phylum level, baseline levels of relative abundance of the two most abundant phyla, Bacteroidetes and Firmicutes, were not significantly different between the placebo and probiotics groups in both men and women (Fig. 1), and the changes in relative abundance during the intervention were compared between the placebo and probiotics groups in each sex. In the male population, the relative abundance of Bacteroidetes showed a tendency to increase during the intervention in both the placebo and probiotic groups, with no statistical difference (Fig. 1A). In the female population, the relative abundance of Bacteroidetes was dramatically decreased at week 4 in the placebo group, but it returned to the baseline level at the end of the intervention. The probiotic group in the female population showed a similar pattern in the change of relative abundance of Bacteroidetes during the intervention. Therefore, in the female population, there was no significant difference in the relative abundance of Bacteroidetes between the two groups (Fig. 1A). Next, when comparing the change in relative abundance of Firmicutes, men showed no marked difference between the two groups; however, in the female population, the relative abundance of Firmicutes was significantly reduced at week 12 in the probiotics group compared to the placebo group (P < 0.05, Fig. 1B). In addition, the change in the Firmicutes to Bacteroidetes (F/B) ratio in the male population was compared between the two groups (Fig. 1C). The change in the F/B ratio was elevated at week 4 in the probiotic group, but the change was not statistically different from that in the placebo group. In the female population, the F/B ratio increased in the probiotics group, while it remained unchanged in the placebo group, but the difference between the two groups showed no statistical significance (Fig. 1C).
Fig. 1. Changes in gut microbial community by sex. Relative abundances of the phyla (A) Bacteroidetes, (B) Firmicutes, and (C) the F/B ratio measured over the course of the intervention are shown as bar graphs. Data are presented as the mean (SEM). (D-E) Heatmap showing the changes in the relative abundances of the gut bacteria that were significantly shifted by probiotic supplementation over the course of the intervention in (D) men and (E) women. The color keys indicate the relative abundances.
F/B, Firmicutes to Bacteroidetes.
*P < 0.05, based on Mann–Whitney U test for the comparison of changes from baseline between the two groups in each sex group.
In addition, we compared changes in the relative abundance of the gut microbiota at the genus level. Baseline levels of relative abundances of genera were not significantly different between the placebo and probiotics groups in both men and women (data not shown), and the changes in relative abundances of genera during the intervention were compared between the placebo and probiotic groups. In the male population, the genera Catabacter and unclassified Coriobacteriales were significantly reduced at week 12 in the probiotic group compared with the placebo group (P < 0.05, Fig. 1D). In the female population, the genera Burkholderia and unclassified Enterobacteriaceae showed significant reductions in their relative abundances at week 12 in the probiotic group compared with the placebo group (P < 0.05, Fig. 1E). Taken together, the gut microbial composition showed sex-dependent changes in response to probiotic supplementation, although the baseline composition did not differ between men and women.
Different effects of probiotic supplementation on peripheral immune cell profiles depending on sex
To investigate whether there was a sex difference in peripheral immune cell profiles after probiotic intervention in the elderly, we performed a flow cytometry assay for PBMCs. First, the changes in lymphocytes, including NK, B, CD4+ T, and CD8+ T cells, and their subpopulations, were compared between the placebo and probiotic groups in each sex group. We confirmed that none of the parameters differed between the two groups in either men or women at baseline (data not shown). Over the course of the intervention, in the male population, the proportion of CD19+ B cells tended to increase in the probiotics group, while it remained unchanged in the placebo group (Table 2). In addition, the proportion of total CD 8+ T cells showed an increasing tendency in men who consumed probiotics, whereas it was reduced in the placebo group. In the female population, a similar pattern was observed in the proportion of CD19+ B cells in the probiotic group, with an increasing tendency. Moreover, the proportion of total CD4+ T cell significantly reduced at week 8 in the probiotics group compared with the placebo in women population (−0.73 ± 2.15 vs. 8.78 ± 1.50; P < 0.05, Table 2).
Table 2. Changes in peripheral lymphocyte population by sex over the course of intervention.
| Cell type | Men | Women | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Placebo (n = 9) | Probiotics (n = 4) | P for Δ (wk 4–wk 0) | P for Δ (wk 8–wk 0) | P for Δ (wk 12–wk 0) | Placebo (n = 5) | Probiotics (n = 7) | P for Δ (wk 4–wk 0) | P for Δ (wk 8–wk 0) | P for Δ (wk 12–wk 0) | |||||||||||
| Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | |||||||||
| NK cell | ||||||||||||||||||||
| % CD56high NK cell/lymphocytes | −0.20 ± 0.33 | 1.46 ± 0.41 | −0.35 ± 0.26 | −0.54 ± 0.24 | 1.40 ± 0.46 | −0.60 ± 0.37 | 0.50 | 0.94 | 0.59 | 0.02 ± 0.35 | 1.47 ± 0.52 | −0.34 ± 0.26 | 0.11 ± 0.12 | 2.01 ± 0.41 | 0.04 ± 0.17 | 0.77 | 0.44 | 0.23 | ||
| % CD56low NK cell/lymphocytes | −2.33 ± 5.77 | −15.32 ± 4.10 | −7.49 ± 4.17 | −4.94 ± 4.48 | −22.04 ± 3.89 | −11.70 ± 3.37 | 0.77 | 0.30 | 0.51 | 1.80 ± 2.83 | −11.23 ± 4.44 | −5.43 ± 2.45 | −2.77 ± 6.16 | −11.10 ± 5.06 | −5.43 ± 5.81 | 0.61 | 0.99 | 0.99 | ||
| B cell | ||||||||||||||||||||
| % CD19+/total live cells | 0.05 ± 1.51 | 0.53 ± 0.97 | 0.15 ± 1.06 | 1.88 ± 1.15 | 1.90 ± 1.55 | 3.76 ± 1.55 | 0.42 | 0.44 | 0.07 | 2.86 ± 1.51 | −0.81 ± 0.90 | 0.01 ± 1.22 | 2.08 ± 1.53 | 4.01 ± 1.97 | 3.13 ± 1.59 | 0.75 | 0.11 | 0.21 | ||
| CD4 T cell | ||||||||||||||||||||
| % CD4+/lymphocytes | −4.25 ± 1.92 | 6.41 ± 1.70 | 1.68 ± 1.07 | −6.87 ± 5.26 | 0.94 ± 5.96 | −1.66 ± 5.01 | 0.58 | 0.28 | 0.41 | −4.05 ± 2.58 | 8.78 ± 1.50 | 4.10 ± 2.30 | −7.09 ± 4.35 | −0.73 ± 2.15 | −2.43 ± 2.19 | 0.64 | 0.01 | 0.09 | ||
| % Naïve CD4 T cell/CD4+ | −3.69 ± 5.65 | −2.06 ± 7.46 | 3.32 ± 6.65 | −9.92 ± 6.62 | −13.1 ± 5.65 | −5.28 ± 4.34 | 0.51 | 0.33 | 0.39 | 4.58 ± 7.39 | −0.68 ± 6.02 | 5.40 ± 6.45 | −1.08 ± 5.10 | 4.68 ± 4.80 | 9.31 ± 4.88 | 0.53 | 0.51 | 0.64 | ||
| % CD4 TCM/CD4+ | 1.57 ± 2.41 | 1.90 ± 2.67 | 3.94 ± 2.72 | 1.40 ± 1.53 | −0.18 ± 3.19 | 1.56 ± 2.39 | 0.96 | 0.64 | 0.57 | 2.45 ± 2.83 | 3.78 ± 2.44 | 5.03 ± 3.91 | 1.87 ± 3.86 | 1.06 ± 3.04 | 2.36 ± 2.84 | 0.92 | 0.56 | 0.59 | ||
| % CD4 TEM/CD4+ | 0.06 ± 4.35 | −0.87 ± 4.88 | −7.05 ± 4.46 | 9.46 ± 5.49 | 11.70 ± 4.89 | 3.66 ± 3.35 | 0.21 | 0.12 | 0.13 | −6.08 ± 5.65 | −1.93 ± 4.76 | −8.08 ± 6.17 | −2.61 ± 6.53 | −6.30 ± 6.57 | −11.37 ± 5.39 | 0.73 | 0.66 | 0.71 | ||
| % CD4 TEMRA/CD4+ | 2.09 ± 1.04 | 1.09 ± 0.70 | −0.19 ± 0.93 | −0.94 ± 2.12 | 1.56 ± 1.03 | 0.03 ± 0.77 | 0.17 | 0.70 | 0.88 | −0.97 ± 1.29 | −1.16 ± 1.54 | −2.35 ± 1.38 | 1.85 ± 1.20 | 0.59 ± 0.54 | −0.27 ± 0.60 | 0.17 | 0.22 | 0.14 | ||
| CD8 T cell | ||||||||||||||||||||
| % CD8+/lymphocytes | −2.07 ± 3.26 | −3.07 ± 1.93 | −1.96 ± 2.45 | 4.58 ± 5.41 | 3.78 ± 5.01 | 1.36 ± 4.03 | 0.28 | 0.15 | 0.47 | −7.45 ± 2.26 | −8.90 ± 2.05 | −8.00 ± 2.38 | −3.10 ± 3.68 | −8.31 ± 3.49 | −6.11 ± 3.46 | 0.43 | 0.91 | 0.71 | ||
| % Naïve CD8 T cell/CD8+ | −3.69 ± 5.65 | −2.06 ± 7.46 | 3.32 ± 6.65 | −9.92 ± 6.62 | −13.10 ± 5.65 | −5.28 ± 4.34 | 0.51 | 0.33 | 0.39 | 4.58 ± 7.39 | −0.68 ± 6.02 | 5.40 ± 6.45 | −1.08 ± 5.10 | 4.68 ± 4.80 | 9.31 ± 4.88 | 0.53 | 0.51 | 0.64 | ||
| % CD8 TCM/CD8+ | 1.57 ± 2.41 | 1.90 ± 2.67 | 3.94 ± 2.72 | 1.40 ± 1.53 | −0.18 ± 3.19 | 1.56 ± 2.39 | 0.96 | 0.64 | 0.57 | 2.45 ± 2.83 | 3.78 ± 2.44 | 5.03 ± 3.91 | 1.87 ± 3.86 | 1.06 ± 3.04 | 2.36 ± 2.84 | 0.92 | 0.56 | 0.59 | ||
| % CD8 TEM/CD8+ | 0.06 ± 4.35 | −0.87 ± 4.88 | −7.05 ± 4.46 | 9.46 ± 5.49 | 11.70 ± 4.89 | 3.66 ± 3.35 | 0.21 | 0.12 | 0.13 | −6.08 ± 5.65 | −1.93 ± 4.76 | −8.08 ± 6.17 | −2.61 ± 6.53 | −6.30 ± 6.57 | −11.37 ± 5.39 | 0.73 | 0.66 | 0.71 | ||
| % CD8 TEMRA/CD8+ | 2.09 ± 1.04 | 1.09 ± 0.70 | −0.19 ± 0.93 | −0.94 ± 2.12 | 1.56 ± 1.03 | 0.03 ± 0.77 | 0.17 | 0.70 | 0.88 | −0.97 ± 1.29 | −1.16 ± 1.54 | −2.35 ± 1.38 | 1.85 ± 1.20 | 0.59 ± 0.54 | −0.27 ± 0.60 | 0.17 | 0.22 | 0.14 | ||
Data are presented as the mean ± SEM.
P-value from the t-test for between-group comparisons. The cell surface markers for subsets of T cells were as follows: CD45RA+ CD197+ for naïve, CD45RA- CD197+ for TCM, CDRA45- CD197- for TEM, and CD45RA+ CD197- for TEMRA.
NK cells, natural killer cells; TCM, central memory T cell; TEM, effector memory T cell; TEMRA, effector memory-RA T cell.
Additionally, the changes in DC and monocytes were compared across sex groups (Table 3). In the male population, the changes in the proportion of CD11c+ HLA-DR+ DC were significant between the two groups (Table 3). Probiotic consumption significantly reduced the proportion of DC in men at week 4 and 12 compared with the placebo group (−1.32 ± 0.40 vs. 1.27 ± 0.58 at wk 4; −2.90 ± 0.64 vs. 0.29 ± 0.49 at wk 12; P < 0.05, Table 3). Also, there were significant reductions in the proportion of CD14+ CD16- classical monocytes at week 8 in the probiotics group compared with the placebo in men population (−14.88 ± 6.91 vs. 2.00 ± 3.80 at wk 8; P < 0.05, Table 3). However, these effects were not observed in the female population. Overall, these results indicate that there is a sex-related differential response to probiotic supplementation in the immune cell profiles of healthy elderly individuals.
Table 3. Changes in peripheral dendritic cell and monocyte population by sex during the intervention.
| Cell type | Men | Women | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Placebo (n = 9) | Probiotics (n = 4) | P for Δ (wk 4–wk 0) | P for Δ (wk 8–wk 0) | P for Δ (wk 12–wk 0) | Placebo (n = 5) | Probiotics (n = 7) | P for Δ (wk 4–wk 0) | P for Δ (wk 8–wk 0) | P for Δ (wk 12–wk 0) | ||||||||||
| Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | Δ (wk 4–wk 0) | Δ (wk 8–wk 0) | Δ (wk 12–wk 0) | ||||||||
| Dendritic cell | |||||||||||||||||||
| % CD11c+ HLA-DR+ cell/CD14− CD16− | 1.27 ± 0.58 | 2.18 ± 1.11 | 0.29 ± 0.49 | −1.32 ± 0.40 | −0.93 ± 1.14 | −2.09 ± 0.64 | < 0.01 | 0.10 | 0.01 | 1.54 ± 0.62 | 0.20 ± 0.59 | −0.66 ± 0.14 | 0.51 ± 0.98 | 1.28 ± 0.71 | −0.36 ± 0.24 | 0.48 | 0.33 | 0.40 | |
| Monocyte | |||||||||||||||||||
| % CD14− CD16+/monocytes | −4.25 ± 0.87 | −3.63 ± 1.16 | −3.76 ± 0.66 | −2.55 ± 1.56 | −0.13 ± 0.42 | −2.48 ± 1.32 | 0.32 | 0.02 | 0.35 | −5.89 ± 3.27 | −6.26 ± 3.30 | −5.53 ± 3.08 | −3.77 ± 2.29 | −2.46 ± 2.63 | −4.27 ± 1.33 | 0.60 | 0.40 | 0.67 | |
| % CD14+ CD16−/monocytes | −3.38 ± 2.46 | 2.00 ± 3.80 | 0.47 ± 1.78 | −9.48 ± 3.60 | −14.88 ± 6.91 | −2.88 ± 2.15 | 0.18 | 0.04 | 0.27 | −5.70 ± 6.73 | 6.55 ± 7.78 | 1.93 ± 6.94 | −7.73 ± 4.41 | −4.16 ± 6.77 | −2.71 ± 2.03 | 0.80 | 0.35 | 0.44 | |
Data are presented as the mean ± SEM.
P-value from the t-test for between-group comparisons.
The significant effects of probiotic supplementation on the proportion of peripheral immune cells and the profiles of the gut microbiota prompted us to measure the levels of markers of systemic inflammation. In men, the change in serum CRP was dramatically reduced at week 12 in the probiotics group but a statistical significance was not observed (−215.02 ± 172.11 vs. −302.27 ± 204.57 at week 12, Supplementary Table 1). Serum LBP was also decreased in the probiotics group, but it was not significant in men (−1,074.49 ± 292.15 vs. 37.94 ± 387.83 at wk 12, Supplementary Table 1). In women, the change in serum CRP levels was significantly different between the two groups at week 12 (Supplementary Table 1). However, serum LBP was reduced in the probiotics group in women although it was not significant (−107.80 ± 344.44 vs. 1,068.63 ± 810.43 at week 12, Supplementary Table 1). Overall, there were no significant changes in systemic inflammatory markers throughout the intervention across the sex groups.
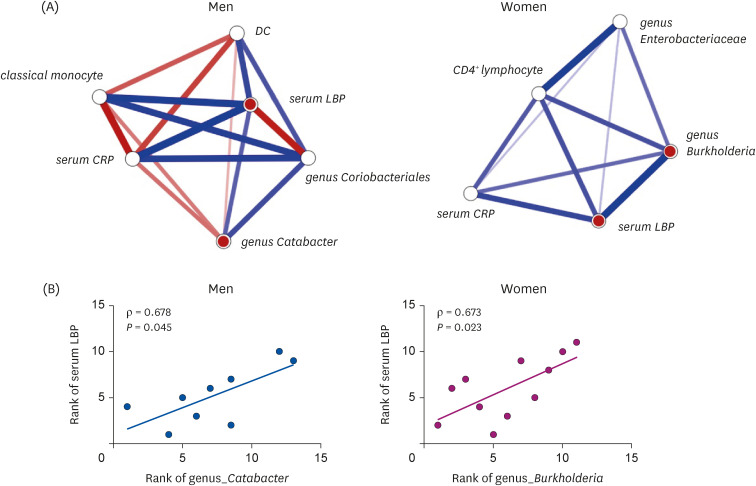
We conducted a network meta-analysis to examine changes in the association between the gut microbiota and immune markers across sex groups. As shown in Fig. 2A, the change in the genus Catabacter and the change in serum LBP levels showed a statistically significant positive correlation in men (ρ = 0.678, P < 0.05, Fig. 2B). In addition, there was a significant positive correlation between the change in the genus Burkholderia and the change in serum LBP in women (ρ = 0.673, P < 0.05, Fig. 2A and B). Therefore, our results suggest that probiotic supplementation reduced circulating LBP, possibly by reshaping the gut microbiota in healthy elderly individuals in a sex-specific manner.
Fig. 2. Network meta-analysis on association between the gut microbiota and immune markers by sex. (A) Network meta-analysis results for the delta values of variables by sex. The thickness of the solid line indicates the strength of association. Blue and red colors of the solid line indicate the positive and negative correlation, respectively. Node with red colors indicates significant results. (B) Spearman’s rank correlation analysis between the rank of variables by sex.
CRP, C-reactive protein; DC, dendritic cell; LBP, lipopolysaccharide-binding protein.
DISCUSSION
Lifestyle factors, including diet, nutrient intake, and physical exercise, play crucial roles in maintaining a healthy immune system and promoting resistance to infection or immune-related diseases [15,16]. There has been much interest in dietary strategies to improve immunity in elderly individuals because immune function itself and the impact of nutrition on immune function are significantly altered during aging [17,18]. Of particular interest is the use of dietary factors, including zinc, vitamin E, and probiotics, which have immunomodulatory effects [15]. For example, one study reported that zinc supplementation increased the number of activated CD4+ T cells in institutionalized healthy elderly individuals [17]. Several studies have reported beneficial effects of dietary supplementation with probiotics in the healthy elderly population [9,18,19]. Studies have shown that certain probiotics increase the frequency and activity of NK cells in healthy older adults [9,19]. However, previous studies on the effects of probiotics on immunosenescence had a relatively short period of intervention (< 9 wk) and the lack of consideration for sex difference, which is a crucial factor affecting the subjects’ responses to dietary intervention. To the best of our knowledge, this is the first study showing that there is a sex-related differential response to probiotic supplementation in terms of age-related phenotypes of immune cell profiles and gut microbiota in healthy elderly individuals.
Immunosenescence is characterized by a decline in the population of B cells [20] and diminished function of B cells but an increased population of DCs [21], which leads to defects in innate and adaptive immune functions. These age-related alterations result in a chronic low-grade inflammatory status [2,22], which is highly implicated in age-associated diseases such as metabolic syndrome, cancer, and neurodegenerative diseases [1,2,3]. Therefore, it is imperative to manage immunosenescence in the elderly to ensure successful aging. Notably, we showed that the age-related decrease in the peripheral CD19+ B-cell population was modulated by probiotic supplementation in men. We assumed that the increased number of CD19+ B cells might reflect the B-1 cell population, which has anti-inflammatory effects by producing natural antibodies [23]. Since we did not measure the subsets of B cells in the present study, further studies are required to identify the effects of probiotic consumption on the changes in the populations of B cell subsets. Additionally, the proportion of peripheral CD11c+ HLA-DR+ DC was found to be reduced during the intervention in the probiotic group in men. Moreover, among the male population, there was a reduction in the proportion of CD14+ CD16- classical monocytes. Classical monocytes, which account for 95% of monocytes, are a major contributor to age-related chronic inflammatory status [24]. Previous studies have demonstrated that classical monocytes in older adults exhibit mitochondrial dysfunction, which may increase basal inflammation [25]. Our results suggest that probiotic supplementation in men specifically target the aged monocytes, which may ameliorate age-related chronic inflammation. The possible mechanistic bases underlying these findings can be supported by our findings on the changes in the gut microbial composition in the probiotic group. In fact, the gut microbiota and its metabolites have regulatory roles in the host immune system and inflammatory signals [2,26]. Several studies reported that administration of probiotic Bifidobacteria reduces the pro-inflammatory intestinal bacteria which could result in improved intestinal barrier function and integrity [27,28]. As a result of increased intestinal barrier function and integrity, translocation of gut bacteria and bacterial components may be decreased, thereby contributing to the amelioration of systemic inflammation in association with changes in the immune cell population. In the present study, men who consumed probiotics showed a reduced abundance of the genus Catabacter, which is known to increase in inflammation-associated diseases, including colonic inflammation in Crohn’s disease [29] and local inflammation in the brain, followed by aggregation of α-synuclein in Parkinson’s disease [30]. In addition, a reduction in unclassified Coriobacteriales may also be implicated in the amelioration of inflammation in men who consume probiotics. Coriobacteriales has been reported to decrease with the suppression of inflammation in a murine model of psoriasis [31]. Overall, these results indicate that probiotic supplementation in elderly men ameliorates age-related changes in immune cell profiles by reducing the levels of bacteria that are known to be responsible for inflammation.
We also observed that probiotic intervention lowered the frequency of CD4+ T cells only in women, which may be due to a dramatic reduction in the number of effector memory CD4+ T cells among the subsets of the CD4+ T cell population. It is well established that a shift in populations of peripheral T cells is found in the elderly population, showing that memory T cells predominate over naïve T cells [32,33]. This is because of lifelong exposure to antigens, age-related chronic inflammatory environment, and reduction in newly generated naive T cells due to thymic involution [34]. Cumulative evidence indicates that such naïve-memory imbalance of CD4+ T cells contributes to chronic inflammation and accelerates system-wide deterioration of the organism during ageing [35]. Collectively, our results suggest that probiotic supplementation in women has beneficial effects on the homeostasis of CD4+ T cells, which may have protective effects against age-related diseases by reducing memory CD4+ T cells. Overall, the present study showed significant sex differences in the immunomodulatory role of dietary supplementation with probiotics. In line with these findings, a significant reduction in the abundance of Firmicutes, Enterobacteriaceae, and Burkholderia was observed in women who consumed probiotics. One of the aging-associated changes in the gut microbiota is the increased abundance of Firmicutes, which leads to an immune response towards the activation of Th17 cells [36,37]. Moreover, Burkholderia species have been reported to cause inflammatory pulmonary disease by stimulating pro-inflammatory cytokines such as interleukin (IL)-8 and IL-6 in the respiratory epithelium [38]. Such increases in inflammatory cytokines are associated with a decrease in the efficacy of immune function, thereby elevating the risk of chronic inflammation and diseases [7]. Interestingly, Enterobacteriaceae, which is known to cause severe infectious diseases [39], was reduced in women by probiotic supplementation and positively correlated with the proportion of CD4+ T cells. Several studies reported that CD4+ T cells can recognize commensal bacteria under homeostatic and inflammatory conditions [40,41]. A recent study also showed the characteristics of Enterobacteriaceae-reactive CD4+ T cells in healthy individuals [41], which supports our results that reductions in pro-inflammatory gut microbes in women may positively affect the homeostasis of immune function and inflammation-associated diseases via the regulation of the gut microbiota.
LBP is a well-known biomarker of systemic exposure to intestinal bacteria that are translocated into the bloodstream [42]. LBP is increased in the blood in response to the leakage of endotoxin (LPS) derived from gram-negative bacteria via the altered intestinal barrier, which is a key signal for inducing low-grade inflammation [42]. Thus, the increase in LBP in the blood is used as a relevant marker of gut-related pro-inflammatory status [42]. LBP has also been reported to be a biomarker of frailty and age-related diseases in older adults [43,44,45]. There have been attempts to regulate the concentration of LBP by dietary intervention, and many studies have shown that diets have the potential to decrease the level of circulating LBP in animals and humans [46,47,48]. In the present study, we also identified a moderate increase in LBP in both men and women in the placebo group, but not in the probiotic group. Moreover, a decrease in LBP was positively associated with reductions in the inflammation-causing gut bacteria Burkholderia [49]. These results suggested that probiotic consumption may have protective effects against chronic endotoxemia.
The mechanisms underlying the sex-dependent effects of dietary supplements remain unclear. Studies have suggested that gut microbiota may be a mediator of sex differences in dietary effects [50] because both diet and sex are factors that influence the gut microbiota [50]. For example, diet affects the nutritional environment and composition of the gut microbiota [50,51]. Sexes also affect the gut microbiota differently, partially because of sex hormones and sex-specific immune responses [52]. Therefore, our findings showing sex-specific responses in the gut microbiota may explain the different immunomodulatory effects of probiotics in men and women. However, further studies are required to elucidate the mechanisms of the microbiota-mediated sex-specific effects of probiotics and how sex and diet interactively control the gut microbiota.
The composition of the gut microbiota varies between individuals, which requires a larger sample size than other biological markers [53]. However, since it is difficult to recruit older adults, randomized controlled trials with older adults have small sample sizes. For example, an open-label intervention trial of omega-3 polyunsaturated fatty acids was conducted on 12 older adults in each group of control and intervention [54]. A double-blind, cross-over intervention trial with a modified Mediterranean-ketogenic diet compared gut microbial changes in 11 older subjects with mild cognitive impairment to 6 cognitively normal participants [55]. Although the sample size in the sex-stratified analysis was relatively small in the present study, which may have reduced statistical power, we still found significant results. Therefore, we argue that the sample size is sufficiently large to monitor significant changes. In addition, there was an uneven distribution in the sex-stratified analysis which could influence the findings of the study, although the sex ratio was not statistically different between men and women. Despite these limitations, this is the first study to examine the different effects of probiotic supplementation on the profiles of the gut microbiota and peripheral immune cells in healthy elderly individuals.
In conclusion, the present study demonstrated that probiotic supplementation may reduce the incidence of inflammation-related diseases by regulating the profiles of the gut microbiota and peripheral immune cells in healthy elderly individuals. Moreover, our findings highlight that dietary intervention targeting the gut microbiota, including probiotics, requires a tailored strategy in consideration of the host sex.
Footnotes
Funding: This research was supported by the Technology Innovation Program (No. 20014744) funded by the Ministry of Trade, Industry & Energy (MOTIE, Republic of Korea).
Conflict of Interest: The authors declare no potential conflicts of interests.
- Conceptualization: Kim CS, Shin DM.
- Data curation: Kim CS.
- Formal analysis: Kim CS.
- Funding acquisition: Kim CS.
- Investigation: Kim CS, Jung MH, Choi EY.
- Methodology: Shin DM.
- Software: Kim CS.
- Supervision: Choi EY, Shin DM.
- Visualization: Kim CS.
- Writing - original draft: Kim CS.
- Writing - review & editing: Shin DM.
SUPPLEMENTARY MATERIALS
Systemic inflammatory markers by sex before and after the intervention
CONSORT flow diagram.
Changes in diversity of gut microbiota by sex. (A) Pielou’s evenness index, (B) Faith’s phylogenetic diversity, (C) the number of observed OTUs, and (D) Shannon’s diversity index measured during the intervention are shown. Data are presented as a box and whisker plot. The lowest and highest point are the minimum and maximum of the data set, respectively, and a horizontal line in the middle of the box indicates the mean value.
References
- 1.Nikolich-Žugich J. The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol. 2018;19:10–19. doi: 10.1038/s41590-017-0006-x. [DOI] [PubMed] [Google Scholar]
- 2.Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A. Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat Rev Endocrinol. 2018;14:576–590. doi: 10.1038/s41574-018-0059-4. [DOI] [PubMed] [Google Scholar]
- 3.Deleidi M, Jäggle M, Rubino G. Immune aging, dysmetabolism, and inflammation in neurological diseases. Front Neurosci. 2015;9:172. doi: 10.3389/fnins.2015.00172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marchesi JR, Adams DH, Fava F, Hermes GD, Hirschfield GM, Hold G, Quraishi MN, Kinross J, Smidt H, Tuohy KM, et al. The gut microbiota and host health: a new clinical frontier. Gut. 2016;65:330–339. doi: 10.1136/gutjnl-2015-309990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rooks MG, Garrett WS. Gut microbiota, metabolites and host immunity. Nat Rev Immunol. 2016;16:341–352. doi: 10.1038/nri.2016.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma R, Padwad Y. Probiotic bacteria as modulators of cellular senescence: emerging concepts and opportunities. Gut Microbes. 2020;11:335–349. doi: 10.1080/19490976.2019.1697148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaiserman AM, Koliada AK, Marotta F. Gut microbiota: a player in aging and a target for anti-aging intervention. Ageing Res Rev. 2017;35:36–45. doi: 10.1016/j.arr.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Gill HS, Rutherfurd KJ, Cross ML, Gopal PK. Enhancement of immunity in the elderly by dietary supplementation with the probiotic Bifidobacterium lactis HN019. Am J Clin Nutr. 2001;74:833–839. doi: 10.1093/ajcn/74.6.833. [DOI] [PubMed] [Google Scholar]
- 9.Gill HS, Rutherfurd KJ, Cross ML. Dietary probiotic supplementation enhances natural killer cell activity in the elderly: an investigation of age-related immunological changes. J Clin Immunol. 2001;21:264–271. doi: 10.1023/a:1010979225018. [DOI] [PubMed] [Google Scholar]
- 10.Leblanc V, Hudon AM, Royer MM, Corneau L, Dodin S, Bégin C, Lemieux S. Differences between men and women in dietary intakes and metabolic profile in response to a 12-week nutritional intervention promoting the Mediterranean diet. J Nutr Sci. 2015;4:e13. doi: 10.1017/jns.2015.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bédard A, Riverin M, Dodin S, Corneau L, Lemieux S. Sex differences in the impact of the Mediterranean diet on cardiovascular risk profile. Br J Nutr. 2012;108:1428–1434. doi: 10.1017/S0007114511006969. [DOI] [PubMed] [Google Scholar]
- 12.Yaqoob P. Ageing alters the impact of nutrition on immune function. Proc Nutr Soc. 2017;76:347–351. doi: 10.1017/S0029665116000781. [DOI] [PubMed] [Google Scholar]
- 13.Kim CS, Cha L, Sim M, Jung S, Chun WY, Baik HW, Shin DM. Probiotic supplementation improves cognitive function and mood with changes in gut microbiota in community-dwelling older adults: a randomized, double-blind, placebo-controlled, multicenter trial. J Gerontol A Biol Sci Med Sci. 2021;76:32–40. doi: 10.1093/gerona/glaa090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Peña AG, Goodrich JK, Gordon JI, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maijó M, Clements SJ, Ivory K, Nicoletti C, Carding SR. Nutrition, diet and immunosenescence. Mech Ageing Dev. 2014;136-137:116–128. doi: 10.1016/j.mad.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Pae M, Meydani SN, Wu D. The role of nutrition in enhancing immunity in aging. Aging Dis. 2012;3:91–129. [PMC free article] [PubMed] [Google Scholar]
- 17.Fortes C, Forastiere F, Agabiti N, Fano V, Pacifici R, Virgili F, Piras G, Guidi L, Bartoloni C, Tricerri A, et al. The effect of zinc and vitamin A supplementation on immune response in an older population. J Am Geriatr Soc. 1998;46:19–26. doi: 10.1111/j.1532-5415.1998.tb01008.x. [DOI] [PubMed] [Google Scholar]
- 18.Arunachalam K, Gill HS, Chandra RK. Enhancement of natural immune function by dietary consumption of Bifidobacterium lactis (HN019) Eur J Clin Nutr. 2000;54:263–267. doi: 10.1038/sj.ejcn.1600938. [DOI] [PubMed] [Google Scholar]
- 19.Dong H, Rowland I, Thomas LV, Yaqoob P. Immunomodulatory effects of a probiotic drink containing Lactobacillus casei Shirota in healthy older volunteers. Eur J Nutr. 2013;52:1853–1863. doi: 10.1007/s00394-012-0487-1. [DOI] [PubMed] [Google Scholar]
- 20.Cancro MP, Hao Y, Scholz JL, Riley RL, Frasca D, Dunn-Walters DK, Blomberg BB. B cells and aging: molecules and mechanisms. Trends Immunol. 2009;30:313–318. doi: 10.1016/j.it.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panda A, Arjona A, Sapey E, Bai F, Fikrig E, Montgomery RR, Lord JM, Shaw AC. Human innate immunosenescence: causes and consequences for immunity in old age. Trends Immunol. 2009;30:325–333. doi: 10.1016/j.it.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Franceschi C, Garagnani P, Vitale G, Capri M, Salvioli S. Inflammaging and ‘Garb-aging’. Trends Endocrinol Metab. 2017;28:199–212. doi: 10.1016/j.tem.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 23.Aziz M, Holodick NE, Rothstein TL, Wang P. The role of B-1 cells in inflammation. Immunol Res. 2015;63:153–166. doi: 10.1007/s12026-015-8708-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pence BD. Fanning the flames of inflammaging: impact of monocyte metabolic reprogramming. Immunometabolism. 2020;2:e200025. doi: 10.20900/immunometab20200025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hearps AC, Martin GE, Angelovich TA, Cheng WJ, Maisa A, Landay AL, Jaworowski A, Crowe SM. Aging is associated with chronic innate immune activation and dysregulation of monocyte phenotype and function. Aging Cell. 2012;11:867–875. doi: 10.1111/j.1474-9726.2012.00851.x. [DOI] [PubMed] [Google Scholar]
- 26.Brestoff JR, Artis D. Commensal bacteria at the interface of host metabolism and the immune system. Nat Immunol. 2013;14:676–684. doi: 10.1038/ni.2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schroeder BO, Birchenough GM, Ståhlman M, Arike L, Johansson ME, Hansson GC, Bäckhed F. Bifidobacteria or fiber protects against diet-induced microbiota-mediated colonic mucus deterioration. Cell Host Microbe. 2018;23:27–40.e7. doi: 10.1016/j.chom.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bergmann KR, Liu SX, Tian R, Kushnir A, Turner JR, Li HL, Chou PM, Weber CR, De Plaen IG. Bifidobacteria stabilize claudins at tight junctions and prevent intestinal barrier dysfunction in mouse necrotizing enterocolitis. Am J Pathol. 2013;182:1595–1606. doi: 10.1016/j.ajpath.2013.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quince C, Ijaz UZ, Loman N, Eren AM, Saulnier D, Russell J, Haig SJ, Calus ST, Quick J, Barclay A, et al. Extensive modulation of the fecal metagenome in children with Crohn’s disease during exclusive enteral nutrition. Am J Gastroenterol. 2015;110:1718–1729. doi: 10.1038/ajg.2015.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sampson T. The impact of indigenous microbes on Parkinson’s disease. Neurobiol Dis. 2020;135:104426. doi: 10.1016/j.nbd.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 31.Zákostelská Z, Málková J, Klimešová K, Rossmann P, Hornová M, Novosádová I, Stehlíková Z, Kostovčík M, Hudcovic T, Štepánková R, et al. Intestinal microbiota promotes psoriasis-like skin inflammation by enhancing Th17 response. PLoS One. 2016;11:e0159539. doi: 10.1371/journal.pone.0159539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Linton PJ, Dorshkind K. Age-related changes in lymphocyte development and function. Nat Immunol. 2004;5:133–139. doi: 10.1038/ni1033. [DOI] [PubMed] [Google Scholar]
- 33.Goronzy JJ, Weyand CM. Immune aging and autoimmunity. Cell Mol Life Sci. 2012;69:1615–1623. doi: 10.1007/s00018-012-0970-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weksler ME, Hütteroth TH. Impaired lymphocyte function in aged humans. J Clin Invest. 1974;53:99–104. doi: 10.1172/JCI107565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mittelbrunn M, Kroemer G. Hallmarks of T cell aging. Nat Immunol. 2021;22:687–698. doi: 10.1038/s41590-021-00927-z. [DOI] [PubMed] [Google Scholar]
- 36.Vaiserman A, Romanenko M, Piven L, Moseiko V, Lushchak O, Kryzhanovska N, Guryanov V, Koliada A. Differences in the gut Firmicutes to Bacteroidetes ratio across age groups in healthy Ukrainian population. BMC Microbiol. 2020;20:221. doi: 10.1186/s12866-020-01903-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Magrone T, Jirillo E. The interaction between gut microbiota and age-related changes in immune function and inflammation. Immun Ageing. 2013;10:31. doi: 10.1186/1742-4933-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fink J, Steer JH, Joyce DA, McWilliam AS, Stewart GA. Pro-inflammatory effects of Burkholderia cepacia on cystic fibrosis respiratory epithelium. FEMS Immunol Med Microbiol. 2003;38:273–282. doi: 10.1016/S0928-8244(03)00169-X. [DOI] [PubMed] [Google Scholar]
- 39.Shrivastava SR, Shrivastava PS, Ramasamy J. World health organization releases global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. J Med Soc. 2018;32:76. [Google Scholar]
- 40.Hegazy AN, West NR, Stubbington MJ, Wendt E, Suijker KI, Datsi A, This S, Danne C, Campion S, Duncan SH, et al. Circulating and tissue-resident CD4+ T cells with reactivity to intestinal microbiota are abundant in healthy individuals and function is altered during inflammation. Gastroenterology. 2017;153:1320–1337.e16. doi: 10.1053/j.gastro.2017.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cassotta A, Goldstein JD, Durini G, Jarrossay D, Baggi Menozzi F, Venditti M, Russo A, Falcone M, Lanzavecchia A, Gagliardi MC, et al. Broadly reactive human CD4+ T cells against Enterobacteriaceae are found in the naïve repertoire and are clonally expanded in the memory repertoire. Eur J Immunol. 2021;51:648–661. doi: 10.1002/eji.202048630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Djuric Z. Obesity-associated cancer risk: the role of intestinal microbiota in the etiology of the host proinflammatory state. Transl Res. 2017;179:155–167. doi: 10.1016/j.trsl.2016.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kavanagh K, Hsu FC, Davis AT, Kritchevsky SB, Rejeski WJ, Kim S. Biomarkers of leaky gut are related to inflammation and reduced physical function in older adults with cardiometabolic disease and mobility limitations. Geroscience. 2019;41:923–933. doi: 10.1007/s11357-019-00112-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roberts LM, Buford TW. Lipopolysaccharide binding protein is associated with CVD risk in older adults. Aging Clin Exp Res. 2021;33:1651–1658. doi: 10.1007/s40520-020-01684-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stehle JR, Jr, Leng X, Kitzman DW, Nicklas BJ, Kritchevsky SB, High KP. Lipopolysaccharide-binding protein, a surrogate marker of microbial translocation, is associated with physical function in healthy older adults. J Gerontol A Biol Sci Med Sci. 2012;67:1212–1218. doi: 10.1093/gerona/gls178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Everard A, Lazarevic V, Gaïa N, Johansson M, Ståhlman M, Backhed F, Delzenne NM, Schrenzel J, François P, Cani PD. Microbiome of prebiotic-treated mice reveals novel targets involved in host response during obesity. ISME J. 2014;8:2116–2130. doi: 10.1038/ismej.2014.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.González-Sarrías A, Núñez-Sánchez MA, Ávila-Gálvez MA, Monedero-Saiz T, Rodríguez-Gil FJ, Martínez-Díaz F, Selma MV, Espín JC. Consumption of pomegranate decreases plasma lipopolysaccharide-binding protein levels, a marker of metabolic endotoxemia, in patients with newly diagnosed colorectal cancer: a randomized controlled clinical trial. Food Funct. 2018;9:2617–2622. doi: 10.1039/c8fo00264a. [DOI] [PubMed] [Google Scholar]
- 48.Pei R, DiMarco DM, Putt KK, Martin DA, Gu Q, Chitchumroonchokchai C, White HM, Scarlett CO, Bruno RS, Bolling BW. Low-fat yogurt consumption reduces biomarkers of chronic inflammation and inhibits markers of endotoxin exposure in healthy premenopausal women: a randomised controlled trial. Br J Nutr. 2017;118:1043–1051. doi: 10.1017/S0007114517003038. [DOI] [PubMed] [Google Scholar]
- 49.Wiersinga WJ, de Vos AF, de Beer R, Wieland CW, Roelofs JJ, Woods DE, van der Poll T. Inflammation patterns induced by different Burkholderia species in mice. Cell Microbiol. 2008;10:81–87. doi: 10.1111/j.1462-5822.2007.01016.x. [DOI] [PubMed] [Google Scholar]
- 50.Bolnick DI, Snowberg LK, Hirsch PE, Lauber CL, Org E, Parks B, Lusis AJ, Knight R, Caporaso JG, Svanbäck R. Individual diet has sex-dependent effects on vertebrate gut microbiota. Nat Commun. 2014;5:4500. doi: 10.1038/ncomms5500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Markle JG, Frank DN, Mortin-Toth S, Robertson CE, Feazel LM, Rolle-Kampczyk U, von Bergen M, McCoy KD, Macpherson AJ, Danska JS. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science. 2013;339:1084–1088. doi: 10.1126/science.1233521. [DOI] [PubMed] [Google Scholar]
- 53.Moore RJ, Stanley D. Experimental design considerations in microbiota/inflammation studies. Clin Transl Immunology. 2016;5:e92. doi: 10.1038/cti.2016.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xyda SE, Vuckovic I, Petterson XM, Dasari S, Lalia AZ, Parvizi M, Macura SI, Lanza IR. Distinct influence of omega-3 fatty acids on the plasma metabolome of healthy older adults. J Gerontol A Biol Sci Med Sci. 2020;75:875–884. doi: 10.1093/gerona/glz141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nagpal R, Neth BJ, Wang S, Craft S, Yadav H. Modified Mediterranean-ketogenic diet modulates gut microbiome and short-chain fatty acids in association with Alzheimer’s disease markers in subjects with mild cognitive impairment. EBioMedicine. 2019;47:529–542. doi: 10.1016/j.ebiom.2019.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Systemic inflammatory markers by sex before and after the intervention
CONSORT flow diagram.
Changes in diversity of gut microbiota by sex. (A) Pielou’s evenness index, (B) Faith’s phylogenetic diversity, (C) the number of observed OTUs, and (D) Shannon’s diversity index measured during the intervention are shown. Data are presented as a box and whisker plot. The lowest and highest point are the minimum and maximum of the data set, respectively, and a horizontal line in the middle of the box indicates the mean value.