Abstract
Background
Birth pain affects women at a physical and psychological level. Pain is subjective, and perception will vary among individuals depending on their health status, pain tolerance, and psychological state. Labor pain can drastically affect the birth process and delivery outcomes if not managed well, ranging from poor maternal satisfaction and impaired maternal-newborn bonding to prolonged labor and fetal distress. Since pharmacological pain relief methods harm the fetus, non-pharmacological pain relief methods are gaining popularity among laboring women and healthcare professionals.
Objectives
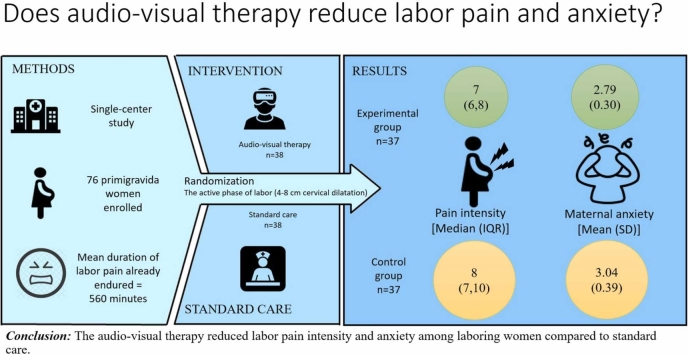
The study aimed to evaluate the effect of audio-visual therapy on labor pain and maternal anxiety.
Methods
A randomized, controlled, open-label, single-center trial was conducted among 76 primigravida women with no obstetrical complications during the active phase of labor (4–8 cm cervical dilatation). The participants were randomly assigned to an experimental group receiving 50 min of virtual reality intervention or a control group receiving standard care using a computer-generated random sequence. The data related to pain and anxiety were collected using the personal information form, anxiety assessment scale for pregnant women in labor, present behavioral intensity scale, numerical pain rating scale, and post-delivery birth satisfaction checklist.
Results
Groups were homogenous in terms of demographic and obstetric variables. The virtual reality intervention reduced the experimental group's reported pain intensity and anxiety score. However, no statistically significant difference was noted in maternal vital signs and labor and neonatal outcomes between the groups.
Conclusion
The virtual reality intervention reduced labor pain intensity and anxiety among laboring women compared to standard care.
Keywords: Virtual reality, Parturition, Complementary therapies, Pain management, Midwifery
Graphical Abstract
Highlights
-
•
Pharmacological methods of pain relief have side effects.
-
•
The effectiveness of non-pharmacological methods such as analgesics and anxiolytics needs more evidence.
-
•
Audio-visual therapy is a cost-effective, practical, and highly effective intervention.
-
•
Audio-visual therapy was effective in reducing labor pain and anxiety.
-
•
Audio-visual therapy is a practical and self-administered intervention that can be implemented in any setting for pain relief.
1. Introduction
Childbirth is one of the most critical events in a woman's life, and various physical and psychological factors determine the pain experienced during that period. Pain has traditionally been understood as a medical model that equates pain to tissue damage or disease, but various research on pain and its nature has driven a change towards a more holistic view of pain. [1] Pain perception is subjective and will vary among individuals depending on their health status, pain tolerance, and psychological state. [2].
Pain activates the respiratory system, causing increased minute ventilation and oxygen consumption, respiratory alkalosis, and reduced fetal blood flow. Furthermore, during delivery, pain, worry, and stress can trigger an increase in the release of catecholamines and cortisol into the bloodstream. [3], [4] Pain and anxiety during labor stimulate the sympathetic nervous system, which starts a series of physiological events due to which corticotropin-releasing hormone (CRH) is released. CRH further stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH). ACTH initiates the synthesis of stress hormones known as "glucocorticoids" from the adrenal cortex. The uterine contractions are negatively affected by the increasing amount of glucocorticoids, resulting in prolonged labor. [5].
Studies suggest excessive pain and anxiety during labor harm the newborn and maternal bonding and feeding behavior due to delayed lactation. [5], [6], [7] Various pharmacological options, including opioids and NSAIDs, are available for pain management during labor. However, these pharmacological pain relief methods have side effects ranging from nausea, vomiting, drowsiness, post-dural puncture headache, fetal heart rate abnormalities, and decreased and uncoordinated uterine tone. [4].
Various studies summarise that complementary pain relief techniques, such as music therapy, aromatherapy, and perineal massage, can help reduce pain and anxiolysis and also encourage women to have a vaginal delivery [3] which is less time-consuming, inexpensive, and satisfactory, with added physiological benefits of decreased incidence of prolonged labor and improved fetal well-being. [8], [9], [10], [11] Adding on to these findings, non-pharmacological pain relief methods significantly lower maternal systolic blood pressure (BP) and heart rate, and the babies had higher APGAR scores and less likelihood of being admitted to intensive care units at birth. [12], [13] Such complementary therapies also reduced the requirement for analgesics in the postpartum period [14] and the occurrence of postpartum depression rates. [11].
Virtual reality (VR) is a relatively recent concept in medicine. As VR stimulates multiple senses at the same time, it provides better relief from acute discomfort than other types of diversions. [15] Another study mentions that an MRI of the brain during VR use reveals that the pain alleviation provided by VR is comparable to that offered by narcotics and can also alleviate anxiety and acute and chronic pain. [16] Studies show that burn and wound treatment, needles/cannulation, dental operations, perioperative pain, and impact management have all been well-represented in VR pain research since its inception. [17], [18], [19], [20], [21] The cost-effectiveness of larger-scale VR installation is also gaining traction. [22].
VR's effectiveness in reducing acute pain perception has been mainly attributed to its distraction effect. [23] Another unified theory is the Gate Control theory, in which messages from the body converge on the spinal cord's dorsal horns and brain, which are integrated with other data to determine the neural response resulting in pain perception. The spinal cord's dorsal horns have been compared as a "gate" that can open or close to signals from the body depending on various criteria, such as previous experience, attention, and cognitive variables. [1].
The originality of this study resides in the lack of similar studies examining the impact of immersive VR on maternal and fetal outcomes beyond managing pain and anxiety, unlike previous studies [15], [16]. No research in this area is reported from Low and Middle-Income Countries (LMICs) like India. Additionally, there is still a shortage of data on how VR affects labor outcomes, maternal vital signs, neonatal outcomes, labor pain, anxiety [4], and other aspects of labor. Additionally, it is a novel concept to evaluate the impact of simple, two-dimensional virtual reality content and Indian Raga on labor pain, which is non-pharmacological and cost-effective.
It advocates the need for a cutting-edge, easy-to-use, safe, and economic midwife-led labor pain and anxiety management intervention, which can enhance the caliber of midwifery care and the satisfaction of women's birthing experiences. Hence, this research aimed to generate evidence on the effect of audio-visual therapy (AVT) on maternal pain, anxiety, and vital signs and a few selected maternal and neonatal outcomes.
2. Materials and methods
2.1. Trial design and study setting
This randomized controlled trial (RCT) was conducted between October 01, 2021, and December 30, 2021, in the observation room of the labor theatre of a District secondary-level health facility, in Khorda district, Odisha, India, where trained midwives conducted approximately 200–300 vaginal deliveries per month. The study began after obtaining permission from the Institute's ethical committee with a code number IEC/AIIMS BBSR/PG Thesis/2021–22/02 and registering in the Clinical Trials Registry India vide code number CTRI/2021/09/036285.
2.2. Participants:
Sample size estimation: A priori sample size calculation was done using G*Power software, 3.1.9.7 version. Based on the effect size from a similar study done by Gur EY et al. (Post-test VAS pain scores; Group A=4.98 ± 1.69, Group E = 6.38 ± 1.86) [2] among laboring women and keeping the level of statistical significance as 5% and power as 95%, the total sample size calculated was 36 in each arm.
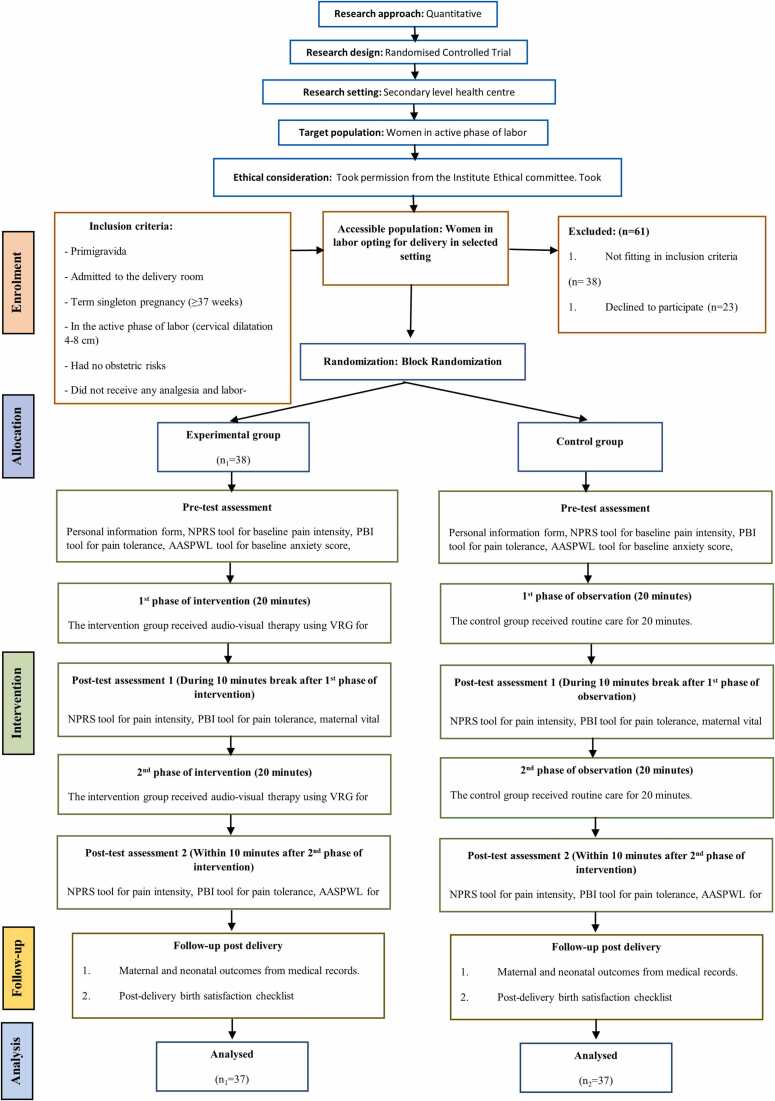
Approximately 587 vaginal deliveries took place during the research period, of which 76 primigravida term singleton pregnancies were admitted to the labor room in the active phase of labor (4–8 cm) with no obstetrical risks and had received no analgesia and labor-enhancing drugs like oxytocin were recruited to the study. Written informed consent was obtained from all the participants.
2.3. Randomization and masking
Women were randomized to either of the groups by computer-generated random sequence with a block size of 4. Allocation concealment was done by sealed opaque envelopes, which were serially numbered and had C or E written on the paper kept inside as the control and experimental group codes, respectively. The women were allocated to either of the groups in a 1:1 ratio based on the pre-assigned codes in the envelopes they picked.
2.4. Tools
The data was collected using a Personal Information form, an Anxiety assessment scale for pregnant women in labor (AASPWL), a Present Behavioural Intensity scale (PBI), a Numerical Pain rating scale (NPRS), and a "Post-delivery birth satisfaction checklist.".
Personal Information Proforma: It involved two sections: Socio-demographic and obstetric characteristics. There were, in total, 22 questions that the participant had to answer.
Present Behavioral Intensity Scale (PBI)[24]: This tool measured pain tolerance. It is an assessor-rated, five-category behavioral observation scale for tolerance of labor pain. The assessor observed the participant during a uterine contraction and rated the pain accordingly. In this study, Cohen's Kappa for this tool was 0.74.
Numerical Pain Rating Scale (NPRS): This tool measured pain intensity. The participant was asked to mark the severity of pain they felt during contraction on a 10-point scale, with '0' signifying "no pain" and '10' representing "worst pain." The participant marked the pain after the contraction stopped.
Anxiety: AASWPL Anxiety Assessment Scale for Pregnant Women in Labor[25]: This questionnaire consists of nine items on a five-point scale: the higher the mean score, the higher the anxiety. In this study, Cronbach's alpha for this tool was 0.81.
An immersive VR system was developed using a 'Procus ONE Virtual reality headset 40 mm lenses- For IOS and Android', a head-mounted display powered by a Galaxy J7 prime, two phones, and headphones.
The post-delivery birth satisfaction checklist consists of 5 items to assess the maternal birth experience. In this study, Cronbach's alpha for this tool was 0.75.
A calibrated automated blood pressure measuring device measured the participant's blood pressure and pulse rate during contraction.
2.5. Description of intervention
The intervention included showing the woman a slideshow of images of pregnant women or breastfeeding mothers and playing Raga Desi Todi for an hour in two 30-minute cycles (20 min intervention + 10 min break). The researcher used the Procus ONE VR Headset with 40MM Lenses and a Samsung Galaxy J7 Prime 2 smartphone to show the 20-minute video and the audio was heard using a Samsung wired headset. The intervention was given at two points with a 10-minute break during the active phase of labor (4–8 cm of cervical dilatation).
The images for the video were made by compiling the pictures clicked of mothers with their newborn babies after obtaining their written consent. (Fig. 1) The faces were visible in the intervention video because the happy expression of the mother and child could generate a positive response in the woman in labor watching the video.
Fig. 1.
Few of the images clicked for the video purpose. The identity of the women and their babies has been concealed for the journal only.
Experts from Obstetrics and Gynaecology, Psychiatry, and Music departments ascertained the suitability of the video. The link to the prepared video was sent to the experts. Subsequently, the video was modified according to the comments. The intervention was pretested on ten pregnant women, and their views regarding the images, music, and virtual reality glass were recorded, which were positive. The intervention was also pretested and pilot-tested on ten pregnant women for feasibility and effectiveness.
Youtube Link of the selected music: https://www.youtube.com/watch?v=Wjyiv4hwdm0.
Orientation to the device and instructions took 15 min. Each patient viewed the same videos of images of mothers with their newborns simultaneously with the music of Raga Desi Todi played on flute by renowned Indian music director and classical flutist Hari Prasad Chaurasia. The intervention was given when the participant was in the observation room in the labor theatre during labor with the cervix dilatation between 4 and 8 cm. The women in this ward are allowed to be with their family members and are shifted to the labor room when cervical dilatation crosses 8 cm. The participant was asked to continue watching and focusing on the video and music during the contraction during the two cycles.
2.6. Intervention
Primary outcomes comprised pain relief, pain tolerance, and reduced anxiety. Secondary outcomes were maternal vitals, complications, analgesic-seeking frequency, and neonatal outcomes.
Post-randomization, the researcher collected baseline socio-demographic and obstetric data. The primary outcomes of interest, labor pain intensity, and pain tolerance were measured using the Numerical Pain Rating scale (NPRS) and Present Behavioural Intensity scale (PBI) [24], respectively, measured at three time points. Maternal anxiety during labor was measured using an anxiety assessment scale for pregnant women in labor (AASPWL) 25 at two time points. The reliability and validity of the tools were established for the study population.
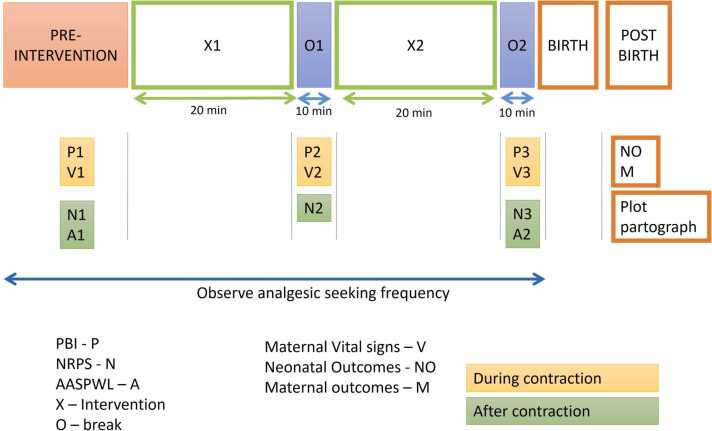
At three points, the researcher measured secondary outcomes related to maternal outcomes like pulse, respiration, and BP during labor pain. Data related to complications like prolonged labor, postpartum hemorrhage, analgesic-seeking frequency, and neonatal outcomes such as meconium-stained liquor, APGAR score, and admission to the neonatal intensive care unit were collected from the medical records after delivery. Post-delivery birth Satisfaction was measured using a five-item checklist. The data collection points are shown in Fig. 2.
Fig. 2.
Schematic representation of research design.
The figure depicts the multiple data collection points and the intervention duration.
The flow of participants is depicted in Fig. 3. The collected data were coded and entered in an Excel spreadsheet, cleaned, and checked for missing values. The Excel data sheet was uploaded into SPSS Version 28.0.1.1 (14).
Fig. 3.
CONSORT flow diagram. NPRS, Numerical Pain Rating Scale; PBI, Present Behavioural Intensity; AASPWL, Anxiety assessment scale for pregnant women in labor; BP, Blood pressure; VRG, Virtual Reality Glasses; CONSORT, Consolidated Standards of Reporting Trials.
3. Results
A sum of 76 expecting mothers was eligible for the study, 38 in each group with one drop-out from each group. In total, the data of 37 participants were analyzed for both groups. The Kolmogorov-Smirnov test assessed the normality for all the continuous variables, and the P-value was significant for all variables except the pain intensity score. Generalized estimating equations (GEE) were used to determine the difference in pain intensity and tolerance among two groups across three time points. Two-way repeated measures (RM) ANOVA was used to determine the difference in maternal anxiety, vital signs, and APGAR score between the two groups across the time points. Independent t-test, chi-square, and Mann-Whitney U tests were used to compare the groups' variables.
Table 1 shows the socio-demographic and obstetric variables of 74 participants in experimental and control groups. The mean (SD) age (in years) was 23.49 (3.66) in the control group and 23.08 (3.84) in the experimental group, and the P value was 0.64. A majority of the women were educated up to the secondary level [control group (70.27%), experimental group (51.35%)], and almost all of them were unemployed in both the groups [control group (97.30%), experimental group (97.30%)]. The P value for all variables was more than 0.05; hence, the groups were comparable. The income status was based on the Below Poverty Line (BPL) card issued by the government of India. Most participants (>80%) of both groups belonged to the 'below-poverty-line' income category.
Table 1.
Socio-demographic and obstetric characteristics of laboring women in the experimental and control group (n = 74).
| S.no. | Variables | Control group (n1=37) |
Experimental group (n2=37) |
P-value |
|---|---|---|---|---|
| Frequency (%) | Frequency (%) | |||
| Socio-demographic characteristics | ||||
| 1. | Age (in years)a | 23.49 (3.66) | 23.08 (3.84) | 0.64b |
| 2. |
Education No formal education Primary school Secondary school High school |
2 (5.40) 7 (18.93) 26 (70.27) 2 (5.40) |
1 (2.70) 14 (37.84) 19 (51.35) 3 (8.11) |
0.27c |
| 3. |
Husband's education No formal education Primary school Secondary school High school University education |
1 (2.70) - 17 (45.95) 16 (43.25) 3 (8.10) |
- 1 (2.70) 13 (35.15) 20 (54.05) 3 (8.10) |
0.56c |
| 4. |
Occupation NIL Working |
36 (97.30) 1 (2.70) |
36 (97.30) 1 (2.70) |
1.00c |
| 5. |
Husband's occupation Self-employed Private Job |
19 (51.35) 18 (48.65) |
22 (59.46) 15 (40.54) |
0.48c |
| 6. |
Place of residence Urban Rural |
6 (16.22) 31 (83.78) |
9 (24.32) 28 (75.68) |
0.49c |
| 7. |
Income status Above poverty line Below poverty line |
6 (16.22) 31 (83.78) |
5 (13.51) 32 (86.49) |
0.58c |
| 8. |
Family structure Nuclear family Joint family Extended family |
2 (5.40) 11 (29.73) 24 (64.87) |
3 (8.12) 11 (29.73) 23 (62.16) |
0.57c |
| 9. | Duration of marriage (in years)a | 1.92 (0.95) | 1.83 (0.81) | 0.66b |
| Obstetric characteristics | ||||
| 10. | Gestational age (in weeks)a |
38.74 (0.92) | 38.86 (1.32) | 0.66b |
| 11. | Duration of labor pain: baseline (in minutes)a | 546.49 (214.91) | 572.70 (274.69) | 0.64b |
| 12. |
Case status Booked Un-booked |
31 (83.78) 6 (16.22) |
32 (86.48) 5 (13.52) |
1.00c |
| 13. | Number of ANC visits ≤ 2 3–4 ≥ 5 |
13 (35.14) 22 (59.46) 2 (5.4) |
16 (43.24) 21 (56.76) - |
0.71c |
| 14. | Previous history of abortion | 2 (5.40) | 2 (5.40) | 0.71c |
| 15. |
Planned pregnancy Yes No |
30 (81.08) 7 (18.92) |
29 (78.38) 8 (21.62) |
0.78c |
| 16. |
Fear regarding labor Yes No |
10 (27.03) 27 (72.97) |
12 (32.43) 25 (67.57) |
0.61c |
| 17. |
Reason of fear Being alone in labor and childbirth Medical procedures Long-term implications of damage from childbirth Lack of knowledge |
(n = 10) - 8 (80) 2 (40) - |
(n = 12) 3 (25) 4 (33) 3 (25) 2 (16) |
0.15c |
| 18. | Cervical dilatation (at baseline) 4–5 cm 6–7 cm 8 cm |
21 (56.76) 8 (21.62) 8 (21.62) |
17 (45.94) 16 (43.25) 4 (10.81) |
0.15c |
aMean (Standard deviation) were reported
b – t test,
c - χ2
The mean (SD) gestational age (in weeks) of the participants of the control group was 38.74 (0.92), and of the experimental group was 38.86 (1.32), with a P value of 0.66. The mean (SD) duration of labor (in minutes) that the participants had already undergone before enrolment in the control group was 546.49 (214.91), and of the experimental group was 572.70 (274.69), with the P value of 0.64. Most cases were booked cases, with 83.78% in the control group and 86.48% in the experimental group. Most of the participants in both groups had only 3–4 antenatal visits [control group (59.46%), experimental group (56.76%)]. A majority of the participants had planned their current pregnancy, and most of them reported no fear regarding labor [control group (72.97%), experimental group (67.51%)]. The most common fear reported by participants was the fear of medical procedures. A majority of 56.76% of participants from the control group and 45.94% from the experimental group were recruited at the cervical dilatation of 4–5 cm. The P value of all the obstetrical variables was more than 0.05; hence, both groups were comparable concerning obstetrical variables.
3.1. Primary outcomes
Table 2 compares the pain tolerance measured by the PBI scale at three time points between the groups. GEE was used to determine the statistically significant change between the groups from baseline to 50 min after intervention. A P value of 0.15 suggests no significant difference in maternal pain tolerance throughout the intervention in both groups.
Table 2.
GEE to determine the change in pain tolerance at three-time points between the groups (n = 74).
| Groups | PBI value | At baseline |
At 20 min |
At 50 min |
Wald chi square value | P-value |
|---|---|---|---|---|---|---|
| Frequency (%) | Frequency (%) | Frequency (%) | ||||
| Experimental group (n2 =37) | 1 | 6 (16.22) | 5 (13.51) | 5 (13.51) | 3.760 | 0.15 |
| 2 | 20 (54.05) | 20 (54.05) | 21 (56.76) | |||
| 3 | 10 (27.02) | 11 (29.73) | 10 (27.02) | |||
| 4 | 1 (2.71) | 1 (2.71) | 1 (2.71) | |||
| (Control group (n1 =37) |
1 | 10 (27.02) | 11 (29.73) | 8 (21.62) | ||
| 2 | 15 (40.54) | 12 (32.43) | 13 (35.14) | |||
| 3 | 12 (32.43) | 14 (37.84) | 14 (37.84) | |||
| 4 | - | - | 2 (5.40) |
*P value < 0.05 is significant.
Table 3 compares the pain intensity reported by participants using the NPRS at three time points. GEE was used to determine the statistically significant change between the groups from baseline to 50 min after intervention. A P value of 0.004 suggests a significant decrease reported in maternal pain intensity throughout the intervention period in the experimental group. Bonferroni pairwise comparison between the groups at different time points revealed that the difference was statistically significant only after 50 min of intervention. (P value = 0.019).
Table 3.
GEE to determine the change in pain intensity at three-time points between the experimental and control group (n = 74).
| Groups | Pain intensity during labor (NPRS) Median [IQR] |
Wald chi square value | P-value | ||
|---|---|---|---|---|---|
| Baseline | At 20 min | At 50 min | |||
| Experimental group (n2 =37) | 7 (6,8) | 7 (6,8) | 7 (6,8) | 10.88 | 0.004 * |
| Control group (n1 =37) |
7 (6,8) | 7 (6,8) | 8 (7,10) | ||
| Bonferroni pairwise comparison between groups at different time points (P-value) | 0.532 | 0.214 | 0.019 * | ||
*P value < 0.05 is significant.
Table 4 shows the mean maternal anxiety scores for both groups at baseline and after 50 min of intervention. Two-way RM ANOVA was used to determine the change in mean anxiety scores between the groups at baseline and after two intervention cycles. A P-value of 0.003 showed a statistically significant difference in anxiety scores between the groups.
Table 4.
Two-way RM ANOVA to compare the effect of audio-visual therapy on maternal and neonatal outcomes at different time points between the groups (n = 74).
| Variable | Group | Mean (SD) |
df | F | P-value | ||
|---|---|---|---|---|---|---|---|
| At baseline | At 20 min | At 50 min | |||||
| Maternal outcomes | |||||||
| Maternal anxiety | Control group (n1 =37) |
3.00 (0.39) | - | 3.04 (0.39) | 1 | 9.245 | 0.003 *a |
| Experimental group (n2 =37) | 2.97 (0.40) | - | 2.79 (0.30) | ||||
| Systolic Blood Pressure | Control group (n1 =37) |
114.45 (6.43) | 115.79 (5.46) | 115.63 (5.36) | 2 | 2.242 | 0.11a |
| Experimental group (n2 =37) | 113.5 (6.4) | 113.18 (5.46) | 113.79 (4.66) | ||||
| Diastolic Blood pressure | Control group (n1 =37) |
73.63 (5.11) | 73.71 (4.76) | 74.29 (4.94) | 2 | 0.440 | 0.64a |
| Experimental group (n2 =37) | 72.11 (5.19) | 72.61 (4.29) | 72.37 (4.04) | ||||
| Pulse rate | Control group (n1 =37) |
81.58 (6.28) | 81.84 (6.08) | 83.08 (5.70) | 2 | 2.695 | 0.07a |
| Experimental group (n2 =37) | 81.24 (7.21) | 82.42 (5.33) | 81.18 (5.75) | ||||
| Respiratory rate | Control group (n1 =37) |
16.42 (3.39) | 17.19 (4.33) | 17.47 (3.53) | 2 | 0.791 | 0.45a |
| Experimental group (n2 =37) | 17.05 (3.50) | 17.42 (4.02) | 17.47 (3.83) | ||||
| Neonatal outcome | |||||||
| At birth | After 5 min | ||||||
| APGAR score | Control group (n1 =37) |
9.38 (1.32) | - | 9.84 (0.73) | 1 | 1.997 | 0.16a |
| Experimental group (n2 =37) | 9.78 (0.63) | - | 10.00 (0.00) | ||||
*P value < 0.05 is significant, a - Two-way RM ANOVA tes
3.2. Secondary outcomes
No statistically significant difference was noted between the groups regarding maternal vital signs and other maternal and neonatal outcomes.
Table 4 shows changes in maternal vital signs and the mean APGAR score at birth and 5 mins. Two-way repeated-measures ANOVA was used to determine the difference in mean Systolic Blood pressure, Diastolic Blood pressure, pulse rate, and respiratory rate at 3-time points between the groups. The results showed no statistically significant change in mean Systolic Blood pressure, Diastolic Blood pressure, pulse rate, and respiratory rate at 3-time points between the groups. (P > 0.05).
The change in mean APGAR score at birth and 5 min between groups was assessed using the two-way repeated-measures ANOVA. The results showed no statistically significant difference between the groups' mean APGAR score at birth and 5 mins.
Table 5 compares maternal and neonatal outcomes (MSL and admission to NICU) among the experimental and control groups. Independent samples t-test was used to determine whether there is a significant difference on average in the duration of labor in stages 1, 2, and 3 between the two groups. The results show that the labor duration is not significantly different between the groups in various stages of labor. Fisher's exact test was used to determine the effect of audio-visual therapy on maternal outcomes. (Prolonged labor, retained placenta, postpartum hemorrhage). The results show no statistically significant impact of AVT on maternal outcomes.
Table 5.
Comparison of maternal and neonatal outcomes in the experimental and control group (n = 74).
| S.no. | Variables | Control group (n1=37) |
Experimental group (n2=37) |
P-value |
|---|---|---|---|---|
| Frequency (%) | Frequency (%) | |||
| Maternal outcomes | ||||
| 1. | Duration of stages of labor (in minutes)a Stage I Stage II Stage III |
747.97 (200.77) 47.46 (26.74) 7.70 (2.12) |
762.14 (231.67) 54.43 (24.53) 7.62 (2.31) |
0.78b 0.24b 0.87b |
| 2. | Prolonged labor | 1 (2.7) | - | 0.99c |
| 3. | Retained placenta | 1 (2.7) | - | 0.99c |
| 4. | Postpartum Hemorrhage | 4 (10.8) | 4 (10.8) | 0.99c |
| 5. | Analgesia seeking frequency | 14 (37.8) | 7 (18.9) | 0.232c |
| 6. |
Mode of delivery Normal Vaginal Delivery Cesarean delivery |
36 (97.3) 1 (2.7) |
37 (100) - |
p = d,e |
| 7. |
Post-delivery birth satisfaction tool items Felt no requirement for further pain relief intervention Did not require more help to reduce stress Felt her birth experience was as per her expectations The labor was not longer than her expectations. This childbirth was one of the most beautiful experiences of her life |
17 (45.9) 10 (27) 22 (59.5) 14 (37.8) 23 (62.2) |
22 (59.5) 18 (48.6) 28 (75.7) 17 (45.9) 22 (59.5) |
0.24d 0.05d 0.13d 0.48d 0.81d |
| Neonatal outcomes | ||||
| 8. | Meconium-stained liquor | 3 (8.1) | 2 (5.4) | 0.99c |
| 9. | Admission to NICU | 2 (5.4) | - | 0.49c |
*P-value < 0.05 is significant.
aMean (Standard deviation) were reported
b – t-test
c – Fisher exact test
d - χ2
eStatistics not computed due to an insufficient number of counts in one category.
The post-delivery birth satisfaction between the groups was compared using the Chi-square test, and no significant difference was noted. The effect of audio-visual therapy on neonatal outcomes - MSL and admission to NICU was assessed using the Fisher exact test. The results show no statistically significant impact of audio-visual therapy on neonatal outcomes in MSL and NICU.
The findings suggest that the VR intervention reduced the experimental group's reported pain intensity and anxiety scores. The difference in the groups was statistically significant, with a P-value < 0.05. However, no statistically significant difference was noted between the groups regarding maternal vital signs and maternal and neonatal outcomes.
4. Discussion
Severe pain is reported by most women in labor; hence, pain control is essential to improve patient satisfaction. Epidural analgesia, considered the gold standard in labor analgesia, is not widely practiced in LMICs like India. Pain relief in labor is a primary responsibility of all midwives by minimizing medical interventions and offering non-pharmacological ways to cope with labor pain.
Our study evaluated the effectiveness of AVT on labor pain and anxiety. We found that the AVT successfully lowered pain and anxiety among the women in the experimental group. Secondary outcomes, on the other hand, did not differ substantially in both groups. Pain distraction appears to be aided by AVT. VR is beneficial as a pain distraction that can be used alone or in conjunction with established pharmacotherapies. Pain perception is based on a patient's ability to pay attention to a specific stimulus. [26].
4.1. Strengths of the study
Our findings on the efficiency of VR in pain management are consistent with earlier research. [15], [16] These studies were also open-label RCTs with solely nulliparous women as subjects, much like ours.
Elsewhere, prior studies indicated decreased pain intensity in the experimental arm. [2], [15], [16] In contrast, the pain intensity in the experimental group remained consistent during the intervention in our investigation, although typically, the intensity of labor pain increases as the labor progresses.
Despite the similarity in results, it was noted that different tools were used to assess labor pain. Most previous investigations have utilized the Visual analog scale (VAS) to measure pain. [15], [16] In a scoping review, many studies mentioned using the NPRS tool. [28] The NPRS is a more specific and better tool for measuring pain intensity than the VAS because it includes 11 possible responses, as an iterative study recommends. [29] The crossover design was employed in the Virtual reality analgesia in labor pilot trial, with interrupted intervention, each lasting 10 min. [15] The benefit is that the subjects acted as their controls, but the intervention's carryover effect should not be overlooked. Hence, we preferred keeping a separate control group.
In the current study, the decrease in anxiety with AVT was similar to previous studies. [22], [27] The previous research looked at the effectiveness of VR in lowering anxiety during episiotomy repair and first-trimester dilatation and curettage in tertiary care centers in Iran and the United States, respectively. The VAS and State trait anxiety inventory (STAI) tools were used in previous studies to assess anxiety. [22], [27] In our study, we used the AASPWL for evaluating anxiety, designed exclusively for women in labor [28], which has fewer items, making it user-friendly compared to the 40-item STAI scale. In addition, the AASPWL tool was pretested for its validity and reliability for the target population.
In contrast, a study testing the effectiveness of a VR-based intervention in 97 women opting for cesarean delivery at a tertiary care center in the Netherlands found that women in the VR group had a higher anxiety level. [30] This discrepancy in results could be attributed to differences in VR applications. The use of VR to provide information on cesarean birth might have led to an increase in anxiety. Our VR visualization featured photographs of happy mothers and newborns, which provided women with a positive stimulus.
A strength of our research is that the VR intervention was given considerably longer (40 min), with all participants undergoing the intervention for the same period. A computer-generated randomized sequence with an opaque sealed envelope was used for randomization. Our study had a control group that received standard routine care. Also, there were multiple time points of measurement.
Our research also adheres to the scientific framework that supports optimal practices in clinical VR trial techniques, [29] under which the VR content was created with the help of expectant and postnatal mothers, and their feedback on the photos and music utilized was taken into account (VR1 phase). The pilot research assessed acceptance, feasibility, tolerability, and initial clinical efficacy, including eight participants, and appropriate adjustments were made (VR2 phase). Finally, an RCT was conducted to determine the effectiveness of the intervention (VR3 phase).
4.2. Limitations
This research is not free from limitations. Firstly, we could not rule out the possibility of the Hawthorne effect, as the laboring women were aware of being studied. Second, the experiment does not use blinded behavioral observation tools, a source of measurement bias. Third, because the intervention strategy was implemented during the active phase of labor, we could not measure participants' music listening habits and prior music preferences. Women's choices are limited because our study because they couldn't decide what they wanted to see and hear. Furthermore, the women who declined to participate were not probed to find out why they refused.
The previous studies were conducted in tertiary care centers, and the participants were informed about the study during their prenatal visits [15], possibly leading to increased acceptance of the VR. We could not brief about VR intervention during prenatal visits because most women presented to the labor room directly with labor pain. Following up with the expectant mother from the antenatal period to the delivery time was difficult. This study failed to continue the intervention until delivery because intervention implementation at this stage was not feasible during the pilot study as women were more agitated and uncooperative and needed some time to assess the VR glasses and familiarize themselves. Also, the women in the research setting stayed in a room adjacent to the labor room when the cervical dilatation was less than 8 cm (the intervention period) and were taken to the labor room once the cervical dilatation reached more than or equal to 8 cm. This sudden change in the environment could have acted as a confounding variable; hence, the intervention was stopped once the participant was shifted to the labor room.
One of the critical drawbacks of the VR intervention is that the effect of pain reduction could be attributable to distraction rather than "distraction due to VR." The effectiveness of the intervention may be attributed to the novelty effect, as VR was a first-time experience for most participants.
Previous research has offered several VR material options, including labor procedure visualization, [16], and nature-related visualization depicting Iceland, beach, and dolphins. [22], [27] were more immersive and provided a 360° view. Due to financial constraints, we could not create three-dimensional, more immersive, labor-specific VR content.
VR intervention did not affect maternal BP, heart rate, or respiration rate. These findings are not in congruence with previous research. [9], [10], [12], [13], [16], [31] A study reported a lower post-intervention heart rate in the experimental arm. [16] The findings may be different because they had more immersive VR visualization.
Our study did not examine the extent of VR's effectiveness in lowering pain after a few hours of use. We had three points of pain measurement, each 20–25 min apart. The pain scores were examined at 2 and 4 h based on the intervention in a previous study [16]; however, there was no significant difference between the groups in the latter. We did not include this because the intervention's length was insufficient to have an effect lasting 2–4 h after application. These additional assessments can be completed while the VR is used during labor. However, short-term assessments may not establish an intervention's genuine clinical value. [29].
Another flaw of our study was that there was no control over "noise" around the subjects of the control group. They have used their smartphones to listen to songs or talk to their relatives to distract themselves from pain. As a researcher, we could not restrict this. Also, the control group was more likely to change positions, affecting pain coping. The experimental group was incapable of changing position due to the blocking of visual sense by the VR headset. Equipoise can be created by exposing patients to headsets in both groups while altering the headset's content on the aspects of its immersive quality or user interface. [29].
VR presents a beneficial non-pharmacological pain relief method with minimal side effects, although the subjects may report nausea. [26] Cybersickness, a side effect of VR, occurs due to a discrepancy between reality and the virtual environment perceived by the vestibular and oculomotor systems, manifested as eyestrain, nausea, fatigue, headache, blurred vision, and postural instability. [29] A previous study used the Simulator Sickness Questionnaire (SSQ) to check for the symptoms of VR sickness. [30] None of our study participants complained of such symptoms, which may be due to the two-dimensional AVT content. We failed to assess the cybersickness aspect of our study. The intervention was designed for 40 min only, whereas primigravida's active phase of labor may extend between 12 and 18 h. [32] Hence, a diverse content could be created to maintain the women's interest throughout the active phase of labor. However, research also highlights that using VR for longer has discomfort like sweating, pressure over the nose and under the eyes, and fogging lenses. [15].
5. Conclusion
The findings of this RCT support the use of VR with custom-designed content in labor rooms. However, the subjects should be sensitized about the VR technology during their prenatal sessions for future research. The cost-effectiveness and feasibility of implementing this intervention in a given situation should also be evaluated. More research is needed in economically disadvantaged populations, particularly in India, where few studies investigate VR's impact on pain management during labor. A mixed study technique might explore the elements driving VR acceptance or rejection and the accompanying myths, anxieties, and side effects. More labor-specific VR content should be created and made available online so that researchers can use and further test it for its effectiveness in healthcare settings, and women can benefit from it.
Ethical issues
None to be declared.
Data accessibility
The datasets generated during and analyzed during the current study are available from the corresponding author upon reasonable request.
Funding
Nil.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We sincerely thank all women who participated in this research work.
Financial support and sponsorship
Nil.
References
- 1.Penlington C., Urbanek M., Barker S. Psychological theories of pain. Prim Dent J. 2019;7(4):24–29. [PubMed] [Google Scholar]
- 2.Gür E.Y., Apay S.E. The effect of cognitive behavioral techniques using virtual reality on birth pain: a randomized controlled trial. Midwifery [Internet] 2020;91 doi: 10.1016/j.midw.2020.102856. (Available from:) [DOI] [PubMed] [Google Scholar]
- 3.Czech I., Fuchs P., Fuchs A., Lorek M., Tobolska-Lorek D., Drosdzol-Cop A., et al. Pharmacological and non-pharmacological methods of labour pain relief—establishment of effectiveness and comparison. Int J Environ Res Public Health. 2018;15(12) doi: 10.3390/ijerph15122792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koyyalamudi V., Sidhu G., Cornett E.M., Nguyen V., Labrie-Brown C., Fox C.J., et al. New labor pain treatment options. Curr Pain Headache Rep. 2016;20(2):1–9. doi: 10.1007/s11916-016-0543-2. [DOI] [PubMed] [Google Scholar]
- 5.Karakoyunlu Ö., Ejder Apay S., Gürol A. The effect of pain, stress, and cortisol during labor on breastfeeding success. Dev Psychobiol. 2019;61(7):979–987. doi: 10.1002/dev.21873. [DOI] [PubMed] [Google Scholar]
- 6.Dimitraki M., Tsikouras P., Manav B., Gioka T., Koutlaki N., Zervoudis S., et al. Evaluation of the effect of natural and emotional stress of labor on lactation and breastfeeding. Arch Gynecol Obstet. 2016;293(2):317–328. doi: 10.1007/s00404-015-3783-1. [DOI] [PubMed] [Google Scholar]
- 7.Chen D.C., Nommsen-rivers L., Dewey K.G., Lönnerdal B. Stress Labor Deliv Early Lact Perform. 2018;1(April):2. [Google Scholar]
- 8.Bashiri M., Akçalı D., Coşkun D., Cindoruk M., Dikmen A., Cifdalöz B.U. Evaluation of pain and patient satisfaction by music therapy in patients with endoscopy/colonoscopy. Turk J Gastroenterol. 2018;29(5):574–579. doi: 10.5152/tjg.2018.18200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jisha C., Pillai S.G. Effect of empowered female labour companion on anxiety, birth outcome, and maternal satisfaction among primiparturients. Manipal J Nurs Heal Sci. 2021;7(1):47–53. [Google Scholar]
- 10.Neiman E., Austin E., Tan A., Anderson C.M., Chipps E., Neiman E. Outcomes of Waterbirth in a US Hospital-Based Midwifery Practice: A Retrospective Cohort Study of Water Immersion During Labor and Birth. 2019;1–8. [DOI] [PubMed]
- 11.Simavli S., Kaygusuz I., Gumus I., Usluogullari B., Yildirim M., Kafali H. Effect of music therapy during vaginal delivery on postpartum pain relief and mental health. J Affect Disord. 2014;156:194–199. doi: 10.1016/j.jad.2013.12.027. [DOI] [PubMed] [Google Scholar]
- 12.Simavli S., Gumus I., Kaygusuz I., Yildirim M., Usluogullari B., Kafali H. Effect of music on labor pain relief, anxiety level and postpartum analgesic requirement: A randomized controlled clinical trial. Gynecol Obstet Invest. 2014;78(4):244–250. doi: 10.1159/000365085. [DOI] [PubMed] [Google Scholar]
- 13.Sidebottom A.C., Vacquier M., Simon K., Wunderlich W., Fontaine P., Dahlgren-roemmich D., et al. Maternal and Neonatal Outcomes in Hospital-Based Deliveries With Water Immersion. 2020;136(4):707–15. [DOI] [PMC free article] [PubMed]
- 14.Er C., Burns E., Cuthbert A. Immersion in water during labour and birth ( Review). 2018; [DOI] [PMC free article] [PubMed]
- 15.Frey D.P., Bauer M.E., Bell C.L., Low L.K., Hassett A.L., Cassidy R.B., et al. Virtual Reality Analgesia in Labor: The VRAIL Pilot Study - A Preliminary Randomized Controlled Trial Suggesting Benefit of Immersive Virtual Reality Analgesia in Unmedicated Laboring Women. Anesth Analg. 2019;128(6):E93–E96. doi: 10.1213/ANE.0000000000003649. [DOI] [PubMed] [Google Scholar]
- 16.Wong M.S., Spiegel B.M.R., Gregory K.D. Virtual reality reduces pain in laboring women: a randomized controlled trial. Am J Perinatol. 2021;38:E167–E172. doi: 10.1055/s-0040-1708851. [DOI] [PubMed] [Google Scholar]
- 17.Gohari S.H., Gozali E., Kalhori S.R.N. Virtual reality applications for chronic conditions management: a review. Med J Islam Repub Iran. 2019;33(1):1–9. doi: 10.34171/mjiri.33.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baeza-Barragán M.R., Labajos Manzanares M.T., Vergara C.R., Casuso-Holgado M.J., Martín-Valero R. The use of virtual reality technologies in the treatment of duchenne muscular dystrophy: Systematic review. JMIR mHealth uHealth. 2020;8(12) doi: 10.2196/21576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan E., Foster S., Sambell R., Leong P. Clinical efficacy of virtual reality for acute procedural pain management: a systematic review and meta-analysis. PLoS One. 2018;13(7):1–13. doi: 10.1371/journal.pone.0200987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patterson D.R., Drever S., Soltani M., Sharar S.R., Wiechman S., Meyer W.J., et al. A comparison of interactive immersive virtual reality and still nature pictures as distraction-based analgesia in burn wound care. Burns. 2022;4179(22):1–2. doi: 10.1016/j.burns.2022.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith V., Warty R.R., Sursas J.A., Payne O., Nair A., Krishnan S., et al. The effectiveness of virtual reality in managing acute pain and anxiety for medical inpatients: systematic review. J Med Internet Res. 2020;22(11) doi: 10.2196/17980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sridhar A., Shiliang Z., Woodson R., Kwan L. Non-pharmacological anxiety reduction with immersive virtual reality for first-trimester dilation and curettage: a pilot study. Eur J Contracept Reprod Heal Care [Internet] 2020;25(6):480–483. doi: 10.1080/13625187.2020.1836146. (Available from:) [DOI] [PubMed] [Google Scholar]
- 23.Trost Z., France C., Anam M., Shum C. Virtual reality approaches to pain: toward a state of the science. Pain. 2021;162(2):325–331. doi: 10.1097/j.pain.0000000000002060. [DOI] [PubMed] [Google Scholar]
- 24.Bonnel A.M., Boureau F. Labor pain assessment: Validity of a behavioral index. Pain. 1985;22(1):81–90. doi: 10.1016/0304-3959(85)90150-2. [DOI] [PubMed] [Google Scholar]
- 25.Durat G., Çulhacik G.D., Doğu Ö., Turan Z., Atasoy I., Toker E. The development of an anxiety assessment scale for pregnant women in labor. Saudi Med J. 2018;39(6):609–614. doi: 10.15537/smj.2018.6.22266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dascal J., Reid M., Ishak W.W., Spiegel B., Recacho J., Rosen B. Icns_14_1–2_14. 2017;14(1):14–21. [PMC free article] [PubMed]
- 27.Shourab N., Zagami S., Golmakhani N., Mazlom S., Nahvi A., Pabarja F., et al. Virtual reality and anxiety in primiparous women during episiotomy repair. Iran J Nurs Midwifery Res. 2016;21(5):521–526. doi: 10.4103/1735-9066.193417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hajesmaeel-Gohari S., Sarpourian F., Shafiei E. Virtual reality applications to assist pregnant women: a scoping review. BMC Pregnancy Childbirth. 2021;21(1):1–8. doi: 10.1186/s12884-021-03725-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Birckhead B., Khalil C., Liu X., Conovitz S., Rizzo A., Danovitch I., et al. Recommendations for methodology of virtual reality clinical trials in health care by an international working group: Iterative study. JMIR Ment Heal. 2019;6(1):1–20. doi: 10.2196/11973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noben, Goossens L., Truijens S.M.T.A., Berckel S.E.M., van M.M.G., Perquin C.W., Slooter G.D., et al. A virtual reality video to improve information provision and reduce anxiety before cesarean delivery: randomized controlled trial. JMIR Ment Heal [Internet] 2019;6(12) doi: 10.2196/15872. [cited 2021 October 16]; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith C.A., Levett K.M., Collins C.T., Armour M., Dahlen H.G., Suganuma M. Relaxation techniques for pain management in labour. Cochrane Database Syst Rev. 2018;2018(3) doi: 10.1002/14651858.CD009514.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raul Artal-Mittelmark. Management of Normal Labor [Internet]. Place unknown]: MSD Manual Professional Version; May 2021 [updated 2021 May; cited date - 2022 April 06]. Available from: https://www.msdmanuals.com/en-in/professional/gynecology-and-obstetrics/normal-labor-and-delivery/management-of-normal-labor#:∼:text=In%20a%20first%20pregnancy%2C%20labor,averaging%206%20to%208%20hours.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and analyzed during the current study are available from the corresponding author upon reasonable request.