Abstract
This cohort study compares rates of hypertension among nonhypertensive patients with atrial fibrillation using JNC 8 vs ACC/AHA thresholds.
Introduction
The CHA2DS2-VASc score identifies patients with atrial fibrillation (AF) who are likely to derive net clinical benefit from oral anticoagulation (OAC).1 One component of CHA2DS2-VASc is hypertension, defined by contemporary clinical practice.1 The 2017 American College of Cardiology/American Heart Association (ACC/AHA) hypertension guidelines lowered the blood pressure (BP) threshold to diagnose hypertension from 140/90 to 130/80 mm Hg.2 Among nonhypertensive patients with AF, the new definition may result in earlier hypertension diagnoses, CHA2DS2-VASc up-scoring, and earlier OAC indications in those with previous scores of 0 or 1.
Methods
We performed a retrospective cohort study of nonhypertensive patients with AF using the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence (PINNACLE) outpatient quality improvement registry (cohort selection diagram in eFigure in Supplement 1).3 The first encounter on or after January 1, 2016, was the index encounter. Informed consent waiver and study authorization were granted by Advarra. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
We used 2 hypertension definitions: Eighth Joint National Committee (JNC 8) hypertension, defined as having 2 or more BP measurements with a systolic pressure of 140 mm Hg or higher and/or diastolic pressure of 90 mm Hg or higher within a 2-year span; or 2017 ACC/AHA hypertension, using BP cutoffs of 130 and 80 mm Hg, correspondingly. The primary outcome was CHA2DS2-VASc up-scoring (details of CHA2DS2-VASc calculation in eTable in Supplement 1), defined as receiving 1 point for hypertension with 2017 ACC/AHA hypertension but not JNC 8 hypertension, in patients with an initial score of 0 or 1. We used Kaplan-Meier product limit survival estimates to calculate the duration from the first encounter with CHA2DS2-VASc up-scoring until (1) JNC 8 hypertension diagnosis, (2) CHA2DS2-VASc score of 2 or higher from accumulating different comorbidities or increase in age, or (3) end of follow-up.
Results
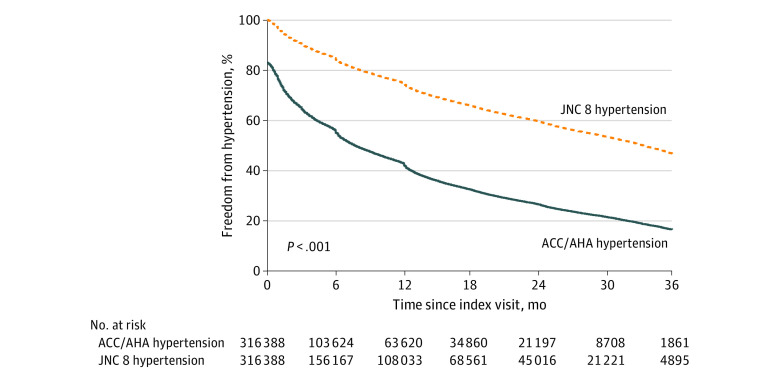
The analysis cohort comprised 316 388 patients (mean [SD] age, 68 [15] years; 42% female) with AF and outpatient encounters on or after January 1, 2016 (Table). At the index encounter, 53 920 patients (17.0%) met the 2017 ACC/AHA hypertension definition based on previous BP values, of whom 6420 (11.9%) had an index CHA2DS2-VASc score of 0 and 11 451 (21.2%) had a score of 1 (prior to new hypertension diagnosis). At 36 months, 83.5% of patients met the 2017 ACC/AHA hypertension definition, compared with 53.3% with the JNC 8 hypertension definition (Figure). At 36 months, 51.4% of patients with an index CHA2DS2-VASc score of 0 had JNC 8 hypertension compared with 86.6% with 2017 ACC/AHA hypertension; in patients with an index CHA2DS2-VASc score of 1, 50.0% had JNC 8 hypertension compared with 83.0% with 2017 ACC/AHA hypertension.
Table. Baseline Characteristics of Nonhypertensive Patients With AF With Outpatient Encounters On or After January 1, 2016.
| Characteristic | Patients, No. (%) (N = 316 388) |
|---|---|
| Age, mean (SD), y | 68.0 (14.5) |
| Sex | |
| Female | 134 055 (42.4) |
| Male | 182 333 (57.6) |
| Racea | |
| Black/African American | 9086 (4.3) |
| White | 197 100 (93.0) |
| Otherb | 5554 (2.6) |
| Multiracial | 192 (0.1) |
| Insurance | |
| None | 1774 (0.7) |
| Private | 176 120 (71.8) |
| Medicare | 59 320 (24.2) |
| Medicaid | 5794 (2.4) |
| Other | 2390 (1.0) |
| Height, mean (SD), cm | 172.4 (11.0) |
| Weight, mean (SD), kg | 86.1 (23.1) |
| BMI, mean (SD) | 28.9 (6.8) |
| Heart rate, mean (SD), beats/min | 74.0 (15.4) |
| Blood pressure, mean (SD), mm Hg | |
| Systolic | 122.6 (15.5) |
| Diastolic | 73.1 (10.1) |
| Diabetes | 33 892 (10.7) |
| Dyslipidemia | 96 942 (30.6) |
| Heart failure | 69 620 (22.0) |
| Stroke/TIA | 36 845 (11.6) |
| Coronary artery disease | 90 289 (28.5) |
| Peripheral vascular disease | 21 079 (6.7) |
| Stroke | 28 471 (9.0) |
| Myocardial infarction | 15 157 (4.8) |
Abbreviations: AF, atrial fibrillation; BMI, calculated as weight in kilograms divided by height in meters squared; TIA, transient ischemic attack.
Self-reported.
Includes American Indian or Alaska Native and Asian.
Figure. Kaplan-Meier Estimates of Freedom From New Hypertension Diagnoses by JNC 8 and 2017 ACC/AHA Definitions.
At the index encounter, 53 920 patients (17.0%) met the definition for 2017 American College of Cardiology/American Heart Association (ACC/AHA) hypertension. At 36 months, 83.5% of patients met 2017 ACC/AHA hypertension compared with 53.2% with Eighth Report of the Joint National Committee (JNC 8) hypertension.
In the 113 359 patients with a CHA2DS2-VASc score of 0 or 1 at the index encounter, 63.1% had up-scoring by 36 months. The mean (SD) duration of up-scoring was 23 (0.2) months and 20 (0.1) months in those with an index score of 0 and 1, accordingly. In up-scored patients with an index score of 0 or 1, 48% and 52% were receiving OAC within 12 months of up-scoring, accordingly.
Discussion
While the definition of hypertension has changed in response to landmark clinical trials,4 CHA2DS2-VASc was validated using an older hypertension definition1 with limited ambulatory BP monitoring and higher BP goals for treatment. Now, patients with AF will meet the CHA2DS2-VASc threshold for OAC earlier in their disease course. However, it is not known if patients with scores of 1 or 2 using the new hypertension definition have sufficient stroke risk to offset the bleeding risk of OAC and will receive net clinical benefit.5
Our study has limitations. PINNACLE cannot incorporate home BP measurements or those from unlinked health care systems. PINNACLE is also an outpatient quality improvement registry not suited to evaluate clinical end points. Our findings support the need to recalibrate AF stroke risk prediction to provide a stronger, contemporary evidence base and incorporate other comorbidities, AF severity and characteristics, and imaging features6 to facilitate nuanced patient counseling and shared decision-making.
eTable. CHA2DS2-VASc Score Definitions
eFigure. Cohort Selection Diagram
Data Sharing Statement
References
- 1.Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJGM. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137(2):263-272. doi: 10.1378/chest.09-1584 [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138(17):e426-e483. doi: 10.1161/CIR.0000000000000597 [DOI] [PubMed] [Google Scholar]
- 3.Messenger JC, Ho KKL, Young CH, et al. ; NCDR Science and Quality Oversight Committee Data Quality Workgroup . The National Cardiovascular Data Registry (NCDR) data quality brief: the NCDR Data Quality Program in 2012. J Am Coll Cardiol. 2012;60(16):1484-1488. doi: 10.1016/j.jacc.2012.07.020 [DOI] [PubMed] [Google Scholar]
- 4.James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. doi: 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 5.Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point: the decision to anticoagulate patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2011;4(1):14-21. doi: 10.1161/CIRCOUTCOMES.110.958108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turakhia MP. It’s time to rethink (and retrial) our framework for stroke prevention in atrial fibrillation. JAMA Cardiol. 2021;6(12):1370. doi: 10.1001/jamacardio.2021.3709 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. CHA2DS2-VASc Score Definitions
eFigure. Cohort Selection Diagram
Data Sharing Statement