Introduction
The COVID-19 pandemic created physical and emotional burdens on healthcare workers (HCWs) and impacted them on both personal and professional levels. The increase in HCW responsibilities included the adoption of new safety and treatment protocols, higher patient acuities, and overcoming severe patient care staffing shortages. We reflect on healthcare worker burnout, patient safety, and infection prevention during the COVID-19 pandemic and propose the prioritization of healthcare worker wellness and resilience, on both individual and organizational levels, as an important driver of health system safety.
Healthcare worker burnout: from bad to worse
Healthcare worker burnout is associated with symptoms of exhaustion, depression, insomnia, post-traumatic stress disorder (PTSD), or other mental health symptoms and is considered a national crisis and priority by the United States Surgeon General. 1 About 50% of physicians reported symptoms of burnout prepandemic and burnout increased as the pandemic evolved. 1,2 Burnout drives turnover in healthcare professions. 2,3 The American Nurses Foundation reported that 31% of nurses under 35 expressed the intent to leave and 35 to 45% of all nurses are experiencing burnout. 3,4 There are several factors that led to increased burnout during the pandemic. Healthcare workers were afraid of infecting family members and were challenged by ongoing changes in pandemic-driven patient care protocols. 5 Healthcare workers faced an increase in workloads and inadequate supplies. 6 Other reported drivers of burnout include decrease in social support, increased periods of isolation, and inadequate rest. 6 Nurses reported moral distress from the poor prognosis of their patients. An increase in stress occurred from nurses who reported inadequate support from leaders and a lack of teamwork. 7 There is a direct correlation between burnout and patient outcomes. This extreme level of stress and psychological pressure resulted in PTSD, anxiety, insomnia, and depression symptoms among healthcare workers. COVID-19 aggravated burnout that already existed within the healthcare systems prepandemic. 8 Providers are not exempt. Physicians experiencing burnout can suffer substance abuse, depression, suicidal ideation, decreased self-care, and increased risk for motor vehicle crashes. 9 All healthcare disciplines suffered the negative consequences of the pandemic.
Healthcare worker burnout impacts patient care and further demoralizes them. Patients experience longer recovery times when providers suffer from depersonalization. 9 Medical errors increase stress on healthcare workers worsening burnout symptoms. 9 Moral injury from errors deepens the existing symptoms of burnout. 4 Thus, burnout causes a decrease in quality care, an increase in medical errors, increased recovery times for patients, and lower patient satisfaction scores. Burnout is associated with lower healthcare productivity. 9 Healthcare workers are more effective when burnout is minimized.
COVID-19, patient safety and healthcare infection prevention
Patient safety is the top priority in patient care as first, do no harm is the primary tenet of medicine. Healthcare workers suffering from burnout pose an increased risk of accidental harm to patients. 4,9 Failure to minimize avoidable harm increases the risk of patient and family suffering caused by death, disability, increased cost, and longer length of stay. 10 Healthcare organizations maximize patient safety through targeted processes of care measures, technologies, and desired behaviors to mitigate the risk of adverse events. 10 Healthcare workers experiencing burnout may suffer from greater depersonalization, be less connected with a safety mission, and may be more prone to errors and breaks in safety protocols (Table 1).
Table 1.
Key Factors for Healthcare Worker Wellness, Resilience, Patient Safety, and Infection Prevention
| Theme | Comments |
|---|---|
| HCW burnout and patient safety |
|
| HCW burnout and infection prevention |
|
| Individual level interventions |
|
| System level interventions |
|
| HCW wellness as the primary factor in patient safety |
|
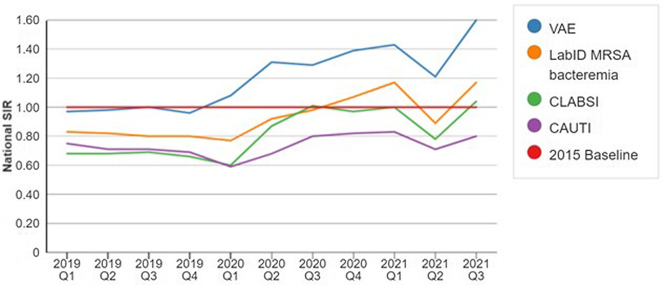
The Centers for Disease Control and Prevention reported a surge in healthcare-associated infection (HAI) during the COVID-19 pandemic (Figure 1). 11 These include a higher incidence of ventilator-associated events (VAE), central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), and methicillin-resistant Staphylococcus aureus (MRSA) bacteremia when comparing pandemic years to the most recent year prior to the pandemic.
Figure 1.
Quarterly National SIRs for select HAI types, 2019-Q1–2021-Q311.
The proportionate impact of HCW burnout on HAI outcomes remains undefined, though Cimiotti et al reported that nurse burnout was significantly associated with an increased risk for urinary tract infections and surgical site infections. 12 Various studies demonstrate that burnout is associated with heightened risks for patient safety incidents, though not specifically HAIs. 13–15 We argue that the unique HCW burnout experienced during the COVID-19 pandemic, coupled with factors outlined below, created a “perfect storm” of conditions that made patients increasingly vulnerable to HAIs during this period.
Various forces potentially drove the HAI increase during the COVID-19 pandemic. Hospital-associated infections likely heightened secondary to changes in hospital procedures resulting in increasing intravenous (IV) tubing length. 16 This was done so IV medications could be changed outside of patient rooms, and to allow nurses to bundle care to decrease overall personal protective equipment (PPE) usage. Staffing shortages played a role in increasing HAIs rates secondary to staff fatigue and burnout, resulting in greater reliance on third-party agency staffing. 17,18 Agency nurses may be less knowledgeable of institution-specific safety culture awareness and hospital-specific HAI prevention techniques. 19,20
Individual and organizational wellness and the path toward resiliency
No single intervention exists to minimize burnout and heighten healthcare worker wellness. There are various individual and organizational strategies to promote resiliency and decrease burnout. 5 Individuals can use self-guided coping mechanisms to reduce signs and symptoms of stress. This includes mindful activities, physical activity, meditation, and reflection. 21–23 Organizational strategies are more impactful at reducing the overall signs and symptoms of burnout within systems. 23,24 Organizational strategies include improving and reducing workloads, workflows, increasing flexibilities of schedules to improve work-life integration, provide opportunities for advancement, to bring meaning in work, promote collegiality within the organization to increase social support, and to decrease the stress of the organization as a whole. 2,23 For example, a positive work environment for front-line providers includes supportive leadership, the ability to balance a work schedule, professional autonomy, adequate resources, and opportunities to professionally advance. 8
Various professional and government organizations endorse wellness enhancement tools. The American Hospital Association published a Well-Being Playbook 2.0 to serve as an executive guide for hospital leaders. 25 The Institute for Healthcare Improvement toolkit, titled, Guide to Promoting Health Care Workforce Well-Being During and After the COVID-19 Pandemic serves a similar purpose. 26 The Office of the Assistant Secretary for Preparedness and Response that serves under the Health and Human Services published tips for resiliency strategies and workforce retention, Creating a Caring Workforce Culture: Practical Approaches for Hospital Executives. 27 The U.S. Surgeon General made HCW burnout top five priorities. 28 Additional research is needed on the direct impact of hospital-acquired infections and burnout.
A multi-path approach is required to minimize HCW burnout, maximize resilience of the workforce, and maximize patient safety. First, healthcare systems must prioritize the recognition of burnout including depersonalization, emotional exhaustion, and personal lack of accomplishment, and prepare for future pandemics and global health crises. 6,29 Healthcare workers must be aware that their organization is working to improve and provide a healthy professional environment to feel supported. 30 Addressing burnout cannot be done on the individual level alone. 2,3 Organizations must assess HCWs regularly to identify dimensions of burnout and well-being. 2,29 Professional engagement or worker motivation is a healthy way to reduce burnout and increase safety within an organization. 29,31 Healthcare organizations must also consistently provide mental health support to their workforce. 1
Conclusion
Healthcare worker burnout worsened during the COVID-19 pandemic, deteriorating from bad to worse. The COVID-19 pandemic also resulted in increased HAIs. Although the proportionate impact of healthcare worker burnout on HAI outcomes is not well defined, burnout likely increases depersonalization and decreases safety practices across an organization, including infection prevention protocols. This may result in decreased fidelity with standard, horizontal infection prevention protocols and heighten device-associated infection risk.
Patient safety outcomes are a general reflection of organizational safety culture and overall institutional performance, this includes healthcare worker engagement and wellness. First and foremost, in the safety mission, is the wellness of the healthcare workforce. Institutions with established wellness programs are committed to healthcare worker engagement, regularly measure wellness, and use targeted interventions to minimize burnout. Top institutions are also committed to the study of drivers and mitigators of healthcare worker burnout. Individual resilience is also valuable. Examples and guidance for maximizing HCW resilience exist in the published literature. Collectively, these individual and system-level interventions impact healthcare worker wellness greater than when instituted in isolation.
It is time to focus on HCW wellness as the primary factor in patient safety. Infection prevention leaders should be aware of institutional wellness initiatives and relentlessly advocate for their ongoing implementation and expansion. This is both for the wellness of the infection prevention team, which drives infection prevention practice, but also for heightened, global patient safety, which further impacts patient-centered outcomes. Advocating for healthcare worker wellness, much like advocating for improvements in hand hygiene and safety checklists, is critical for the desired safety outcomes and gets us closer to the shared goal of minimal preventable harm to patients.
Acknowledgments
None.
Financial support
None reported.
Competing interests
All authors report no conflicts of interest relevant to this article.
References
- 1. Murthy V. Confronting healthcare burnout and well-being. NEJM. 2022. 10.1056/NEJMp2207252 [DOI] [PubMed]
- 2. Shanafelt TD, Noseworthy JH. Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clinic proceedings. 2017;92(1):129-146. doi: 10.1016/j.mayocp.2016.10.004 [DOI] [PubMed]
- 3. Pulse of the nation’s nurses survey series: Mental health and wellness. American Nurses Foundation Mental Health and Wellness Survey Report. American Nurses Foundation website »https://www.nursingworld.org/»4aa484/globalassets/docs/ancc/magnet/mh3-written-report-final.pdf. Published 2021. Accessed February 19, 2023
- 4. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington, DC: The National Academies Press. National Academies of Sciences, Engineering, and Medicine website. https://nam.edu/publications/the-future-of-nursing-2020-2030/). Published 2021. Accessed January 30, 2023. 10.17226/25982 [DOI] [PubMed]
- 5. Lluch C, Galiana L, Doménech P, Sansó N. The Impact of the COVID-19 Pandemic on Burnout, Compassion Fatigue, and Compassion Satisfaction in Healthcare Personnel: A Systematic Review of the Literature Published during the First Year of the Pandemic. Healthcare (Basel). 2022;10(2):364-. doi: 10.3390/healthcare10020364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–3302. doi: 10.1111/jan.14839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Guttormson JL, Calkins K, McAndrew N, Fitzgerald J, Losurdo H, Loonsfoot D. Critical Care Nurses’ Experiences During the COVID-19 Pandemic: A US National Survey. Am J Crit Care. 2022;31(2):96–103. doi: 10.4037/ajcc2022312 [DOI] [PubMed] [Google Scholar]
- 8. Copanitsanou P, Fotos N, Brokalaki H. Effects of work environment on patient and nurse outcomes. Br J Nurs. 2017;26(3):172–176. doi: 10.12968/bjon.2017.26.3.172 [DOI] [PubMed] [Google Scholar]
- 9. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. doi: 10.1111/joim.12752 [DOI] [PubMed] [Google Scholar]
- 10. Safety Patient. World Health Organization (WHO) website. https://www.who.int/news-room/fact-sheets/detail/patient-safety. Published September 13, 2019. Accessed January 30, 2023.
- 11. COVID-19 Impact on HAIs. Centers for Disease and Control and Prevention. Website. https://www.cdc.gov/hai/data/portal/covid-impact-hai.html. Published 2022. Accessed January 30, 2023.
- 12. Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012. Aug;40(6):486-90. doi: 10.1016/j.ajic.2012.02.029. Erratum in: Am J Infect Control. 2012 Sep;40(7):680. PMID: ; PMCID: PMC3509207. [DOI] [PMC free article] [PubMed]
- 13. Hall LH, Johnson J, Watt I, Tsipa A, Healthcare Staff Wellbeing O’Connor DB., Burnout, and Patient Safety: A Systematic Review. PLoS One. 2016. Jul 8;11(7):e0159015. doi: 10.1371/journal.pone.0159015. PMID: ; PMCID: PMC4938539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, Collicott P, Novotny PJ, Sloan J, Freischlag J. Burnout and Medical Errors Among American Surgeons. Annals of Surgery 251(6):p 995-1000, June 2010. doi: 10.1097/SLA.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- 15. Garcia CL, Abreu LC, Ramos JLS, Castro CFD, Smiderle FRN, Santos JAD, Bezerra IMP. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina (Kaunas). 2019. Aug 30;55(9):553. doi: 10.3390/medicina55090553. PMID: ; PMCID: PMC6780563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Blake JWC, Giuliano KK, Butterfield RD, Vanderveen T, Sims NM. Extending tubing to place intravenous smart pumps outside of patient rooms during COVID-19: an innovation that increases medication dead volume and risk to patients. BMJ innovations. 2021;7(2):379–386. doi: 10.1136/bmjinnov-2020-000653 [DOI] [Google Scholar]
- 17. McVey C, von Wenckstern T, Mills C, et al. Nurse-Sensitive Indicator Quality Improvement Toolkit: A Scalable Solution to Improve Health Care–Associated Infections. Journal of nursing care quality. 2022;37(4):295–299. doi: 10.1097/NCQ.0000000000000634. [DOI] [PubMed] [Google Scholar]
- 18. Zhou Q, Lai X, Wan Z, Zhang X, Tan L. Impact of burnout, secondary traumatic stress and compassion satisfaction on hand hygiene of healthcare workers during the COVID-19 pandemic. Nurs Open. 2021;8(5):2551–2557. doi: 10.1002/nop2.786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stone PW, Pogorzelska M, Kunches L, Hirschhorn LR. Hospital staffing and health care-associated infections: a systematic review of the literature. Clin Infect Dis. 2008. Oct 1;47(7):937–44. doi: 10.1086/591696. PMID: ; PMCID: PMC2747253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mitchell BG, Gardner A, Stone PW, Hall L, Pogorzelska-Maziarz M. Hospital Staffing and Health Care-Associated Infections: A Systematic Review of the Literature. Jt Comm J Qual Patient Saf. 2018. Oct;44(10):613–622. doi: 10.1016/j.jcjq.2018.02.002. Epub 2018 Jun 13. PMID: . [DOI] [PubMed] [Google Scholar]
- 21. Maresca G, Corallo F, Catanese G, Formica C, Lo Buono V. Coping Strategies of Healthcare Professionals with Burnout Syndrome: A Systematic Review. Medicina (Kaunas, Lithuania). 2022;58(2):327-. doi: 10.3390/medicina58020327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Green AA, Kinchen EV. The Effects of Mindfulness Meditation on Stress and Burnout in Nurses. J Holist Nurs. 2021;39(4):356–368. doi: 10.1177/08980101211015818 [DOI] [PubMed] [Google Scholar]
- 23. De Simone S, Vargas M, Servillo G. Organizational strategies to reduce physician burnout: a systematic review and meta-analysis. Aging Clin Exp Res. 2021;33(4):883–894. doi: 10.1007/s40520-019-01368-3 [DOI] [PubMed] [Google Scholar]
- 24. Naegle MA, Kelly LA, Embree JL, et al. American academy of nursing consensus recommendations to advance system level change for nurse well-being. Nurs Outlook. 2023;71(2):101917–101917. doi: 10.1016/j.outlook.2023.101917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Well-being Playbook 2.0 A COVID-19 Resource for Hospital and Health System Leaders. American Hospital Association website. https://www.aha.org/system/files/media/file/2021/02/alliance-playbook-2021_final.pdf Published 2021. Accessed February 19, 2023
- 26. A Guide to Promoting Health Care Workforce Well-Being During and After the COVID-19 Pandemic. Boston, Massachusetts: Institute for Healthcare Improvement; 2020. (Available at www.ihi.org)
- 27. Creating a Caring Workforce Culture: Practical Approaches for Hospital Executives. Public Health Emergency website. https://www.phe.gov/Preparedness/planning/abc/Pages/hospital-exec-practical-approaches.aspx Published 2021. Accessed February 19, 2023
- 28. The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. Current Priorities of the U.S. Surgeon General. Addressing Health Worker Burnout website. https://www.hhs.gov/sites/default/files/health-worker-wellbeing-advisory.pdf Published 2022. Accessed February 19, 2023
- 29. James TT, Hudon R, Merrick T, Olson L, Hanes D, Scanlan JM. Creating a Comprehensive Pandemic Response to Decrease Hospitalist Burnout During COVID-19: Intervention vs Control Results in 2 Comparable Hospitals (HOSP-CPR). J Gen Intern Med. Published online 2023:1–8. doi: 10.1007/s11606-023-08041-6 [DOI] [PMC free article] [PubMed]
- 30. Reitz KM, Terhorst L, Smith CN, et al. Healthcare providers’ perceived support from their organization is associated with lower burnout and anxiety amid the COVID-19 pandemic. PloS one. 2021;16(11):e0259858–e0259858. doi: 10.1371/journal.pone.0259858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mossburg SE, Dennison Himmelfarb C. The Association Between Professional Burnout and Engagement With Patient Safety Culture and Outcomes: A Systematic Review. J Patient Saf. 2021;17(8):e1307–e1319. doi: 10.1097/PTS.0000000000000519 [DOI] [PubMed] [Google Scholar]