Significance
Extreme air pollution events, like those from wildfires, negatively affect health through physiological responses but may also be salient enough to induce behavioral changes in individuals protecting their own health. The net impacts of these complex tradeoffs are poorly characterized. By joining the near-universe of emergency department visits in California from 2006 to 2017 with spatially and temporally resolved estimates of ambient wildfire smoke, we find total visits respond nonlinearly to increasing wildfire smoke concentrations, but that response differs by cause of visit. Total visits increase at lower concentrations but then decline at higher concentrations, suggesting that populations shift their behaviors following salient smoke periods. Whereas respiratory-related visits steadily increase, visits for accidental injuries and nonrespiratory symptoms like stomach pains decline at high smoke concentrations.
Keywords: wildfire, health, behavior, pollution
Abstract
Air pollution negatively affects a range of health outcomes. Wildfire smoke is an increasingly important contributor to air pollution, yet wildfire smoke events are highly salient and could induce behavioral responses that alter health impacts. We combine geolocated data covering all emergency department (ED) visits to nonfederal hospitals in California from 2006 to 2017 with spatially resolved estimates of daily wildfire smoke PM concentrations and quantify how smoke events affect ED visits. Total ED visits respond nonlinearly to smoke concentrations. Relative to a day with no smoke, total visits increase by 1 to 1.5% in the week following low or moderate smoke days but decline by 6 to 9% following extreme smoke days. Reductions persist for at least a month. Declines at extreme levels are driven by diagnoses not thought to be acutely impacted by pollution, including accidental injuries and several nonurgent symptoms, and declines come disproportionately from less-insured populations. In contrast, health outcomes with the strongest physiological link to short-term air pollution increase dramatically in the week following an extreme smoke day: We estimate that ED visits for asthma, COPD, and cough all increase by 30 to 110%. Data from internet searches, vehicle traffic sensors, and park visits indicate behavioral changes on high smoke days consistent with declines in healthcare utilization. Because low and moderate smoke days vastly outweigh high smoke days, we estimate that smoke was responsible for an average of 3,010 (95% CI: 1,760–4,380) additional ED visits per year 2006 to 2017. Given the increasing intensity of wildfire smoke events, behavioral mediation is likely to play a growing role in determining total smoke impacts.
Extreme weather and air pollution events are known to negatively affect a broad range of health outcomes. For instance, there is a large body of evidence documenting increases in emergency department (ED) visits for cardiovascular and respiratory conditions, injuries, infections, and other conditions exacerbated by environmental stressors during or following heat waves (1–5), hurricanes and other extreme weather (6–8), and intense pollution events (9–18).
However, when environmental conditions are sufficiently hazardous, people may purposefully or inadvertently alter their behavior in ways that shape health outcomes. Previous work has documented that changes in health seeking behavior lead to fewer ED visits on snowy days and during hurricanes (6, 19–21). In the case of air pollution, research from multiple settings has shown that when individuals are informed of high ambient pollution exposures, they alter their behavior in an effort to reduce exposures and that these efforts shape health outcomes (22–24). For wildfire smoke specifically, research shows that individual awareness of air quality appears to increase with ambient exposure levels and people are more likely to remain at home when wildfire smoke is high (25). They are perhaps less likely to seek health services on these days and also perhaps less likely to need to seek health services if, for example, as has been documented in other settings, spending more time at home reduces driving and leads to fewer car accidents and thus fewer ED visits for trauma (26). The impact of environmental stressors on changes in ED visits, or any health outcome, thus depends on a complex combination of factors that worsen health and factors that can be “protective” of health. Comprehensive assessment of the societal impacts of extreme environmental events, many of which are likely to become more frequent under future climate change (27), requires an accurate accounting of the net effect of these two counteracting influences as exposures vary.
Here, we focus on understanding health impacts of wildfire smoke, one of the fastest growing environmental health risk factors in the United States and in many other countries. Wildfire smoke events represent an increasingly common hazard faced by populations across the United States. Recent estimates suggest that over the past decade, the number of days with any smoke in the air has roughly doubled, the number of days with smoke fine particulate matter (PM has increased by a factor of 12, and the number of days with smoke PM has increased by a factor of more than 60 (28). Growing evidence has begun to establish the negative health effects of these exposures, especially for respiratory health (29). At the same time, wildfire events are often highly salient, inducing observable changes in information-seeking behavior regarding exposures and protective measures, mobility, and health-protective investments (25).
We combine data covering all ED visits to nonfederal hospitals in California from 2006 to 2017, representing 127 million individual visits, with recently developed spatially resolved estimates of daily surface PM concentrations from wildfire smoke. Over the study period, both the number (Fig. 1A) and rate (SI Appendix, Fig. S1) of total ED visits have increased, although spatial patterns vary for different primary diagnoses (SI Appendix, Fig. S2), including those diagnoses that are most common or relevant to wildfire smoke (Fig. 1B). Wildfire smoke has also been steadily increasing with substantial year-to-year variation (Fig. 1C). We aggregate our encounter-level data to the zipcode by day level based on the patient’s zipcode of residence and estimate the effect of wildfire smoke intensity (Fig. 1D) on ED visit rates using a panel fixed effects estimator that exploits local temporal variation in both exposure and outcome (Materials and Methods). While average wildfire smoke exposure is related to a suite of characteristics that could plausibly be correlated with ED visit rates (30), local-level variation in daily exposure is highly random, driven by idiosyncrasies in where and when fires start and how the wind blows on a given day. Panel estimators that exploit within-location variation over time—and which are commonly employed in related environmental settings—plausibly isolate the impact of variation in smoke exposure from other time-invariant and time-varying factors that could be correlated with both wildfire smoke exposure and ED visits. In addition to location and day-of-week fixed effects, our model includes county by month-of-year fixed effects to account for average regional seasonality in both ED visits (SI Appendix, Fig. S3) and wildfire smoke and wildfire-season by year fixed effects to control flexibly for trends over time and factors like bad flu seasons that occur primarily during nonsmoke months and may be negatively correlated with the intensity of the fire season that year. Because both health impacts and the decision to seek treatment can occur well after the time of exposure, we model ED visits as function of daily wildfire smoke on the day of visit and in the prior week. We include up to four weeks of daily lags in alternative models; that is, a wildfire exposure on a day in a given location is allowed to affect ED visits in that location for up to a month after the exposure. To understand how ED visits respond to different intensities of exposure, we estimate ED visits as flexible nonlinear functions of wildfire smoke PM using flexible polynomials and splines as well as nonparametric binned models (Materials and Methods).
Fig. 1.
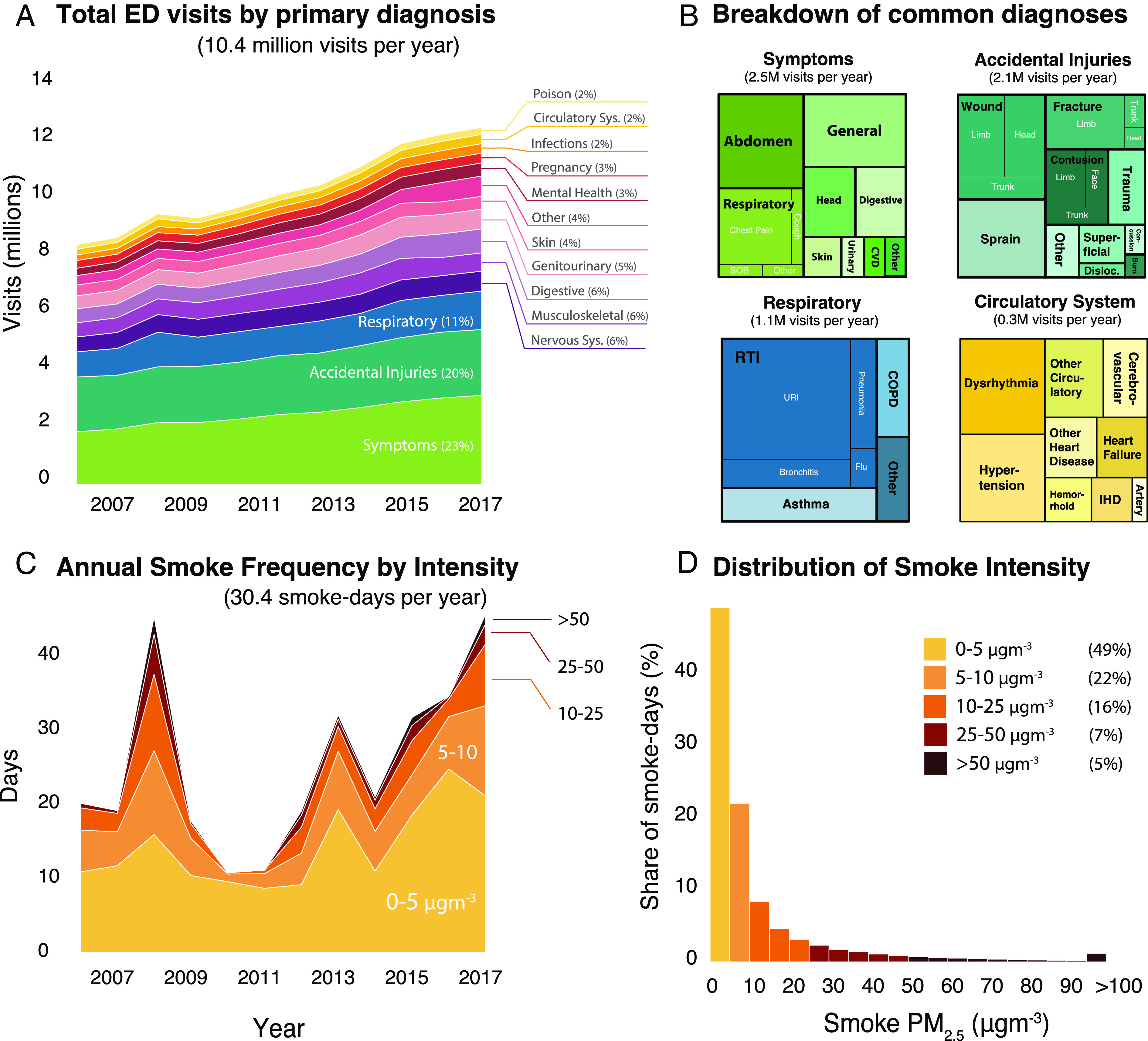
Data summary. (A) Annual total ED visits in California 2006-2017 broken down by primary diagnosis (SI Appendix for International Classification of Diseases (ICD) codes corresponding to each group). (B) Subgroup breakdown for relevant diagnoses. Black labels indicate broader categories, while white labels indicate subcategories. (C) Annual population-weighted average wildfire smoke days in California color coded by concentration of PM from smoke. (D) Histogram of smoke PM concentration on days with smoke present. Nearly half of smoky days 2006 to 2017 had smoke PM less than 5 while 5% of smoky days had smoke PM over 50 .
Our primary analysis examines how total (i.e., all-cause) ED visits respond to wildfire smoke events. To distinguish the health impacts of wildfire smoke from the impacts of being close to a fire, we control for the distance to the nearest active fire. As an additional check, we reestimate responses for the subsample of zipcodes far from active fires that are still affected by wildfire smoke. To better disentangle direct physiologic responses to smoke from indirect impacts induced by behavioral changes, we then estimate cause-specific responses where ED visits are grouped by the principal diagnosis associated with each visit (based on International Classification of Disease (ICD) groupings) (SI Appendix).
We also evaluate whether different age and demographic subgroups respond differently to wildfire smoke. In particular, we observe that baseline ED visit rate varies by both age and health insurance status and posit that these features may influence physiological or behavioral responses to smoke pollution. Children under 5 y of age visit the ED at the highest rate of any age group in our sample (136.9 per 100K), 60% higher than the next highest group (83.5 per 100K for people over 65). While we do not observe individual insurance status, zipcodes in the lowest tercile of average insurance coverage rates in our data (those with less insured populations) have 60% higher ED visit rates than those in the highest tercile of coverage (mean rates of 101.1 and 63.6 per 100K). To assess how ED visits among these subgroups respond to wildfire smoke events, we estimate separate analogous regressions for each subgroup (Materials and Methods).
To probe whether behavioral changes shape observed ED visit responses, we examine behavioral responses that are plausibly relevant to ED visits. We assemble location- and time-resolved data on internet search activity for air quality information, vehicular traffic volumes from in-road sensors, and administrative data on visits to national parks in California (Materials and Methods) and merge each with daily smoke data. Search activity is a proxy for the salience of smoke exposure and for whether individuals are informed when air quality worsens. Vehicular traffic volumes and national park visits provide insight on whether individuals change their mobility patterns, especially motor vehicle use, in response to varying ambient smoke conditions.
Finally, to evaluate the overall impact of wildfire smoke on ED visits, which includes the combined impact of both low-intensity and high-intensity exposures, we estimate the annual number of excess ED visits attributable to wildfire smoke during our sample period. We do this by applying our estimated ED-smoke dose–response curve to observed daily smoke PM concentrations and then scaling the predicted rates by the relevant population in the exposed zipcodes (Materials and Methods).
Results
We find that total (all-cause) ED visit rates increase in response to low or moderate intensity wildfire smoke but decline in response to heavy smoke (Fig. 2A). We estimate the largest positive effects on total ED visits when wildfire smoke PM is in the 5 to 15 range (for context, average nonsmoke PM in California is 9 , and the EPA 24-h standard for total PM is 35 ). At this intensity, total ED visits increase by an average of 0.9 additional daily visits per 100,000 (95% CI: 0.6–1.2) in the week following wildfire smoke. This change represents a 1.1% increase over the sample baseline rate of 75.3 ED visits per 100,000. The response of total ED visits to wildfire smoke peaks at 10 of smoke PM (88th percentile in our data) and declines thereafter becoming negative for smoke PM20 (95th percentile smoke intensity). At smoke PM = 50 (99th percentile), we estimate that total ED visits are lower by 7.3 visits per 100,000 (95% CI: 5.6–9.1) relative to a day in the same zipcode without wildfire smoke, a 9.8% decline in ED visits. The general shape of the all-cause ED visits response is remarkably robust to modeling choices with respect to functional form, lag structure, fixed effects, controls, modeling approach, and level of temporal aggregation (SI Appendix, Figs. S4–S7). However, certain choices, such as whether to control for temperature and the number of daily lags included, affect the relative magnitudes of estimated positive and negative responses and thus have implications for our attribution estimates.
Fig. 2.
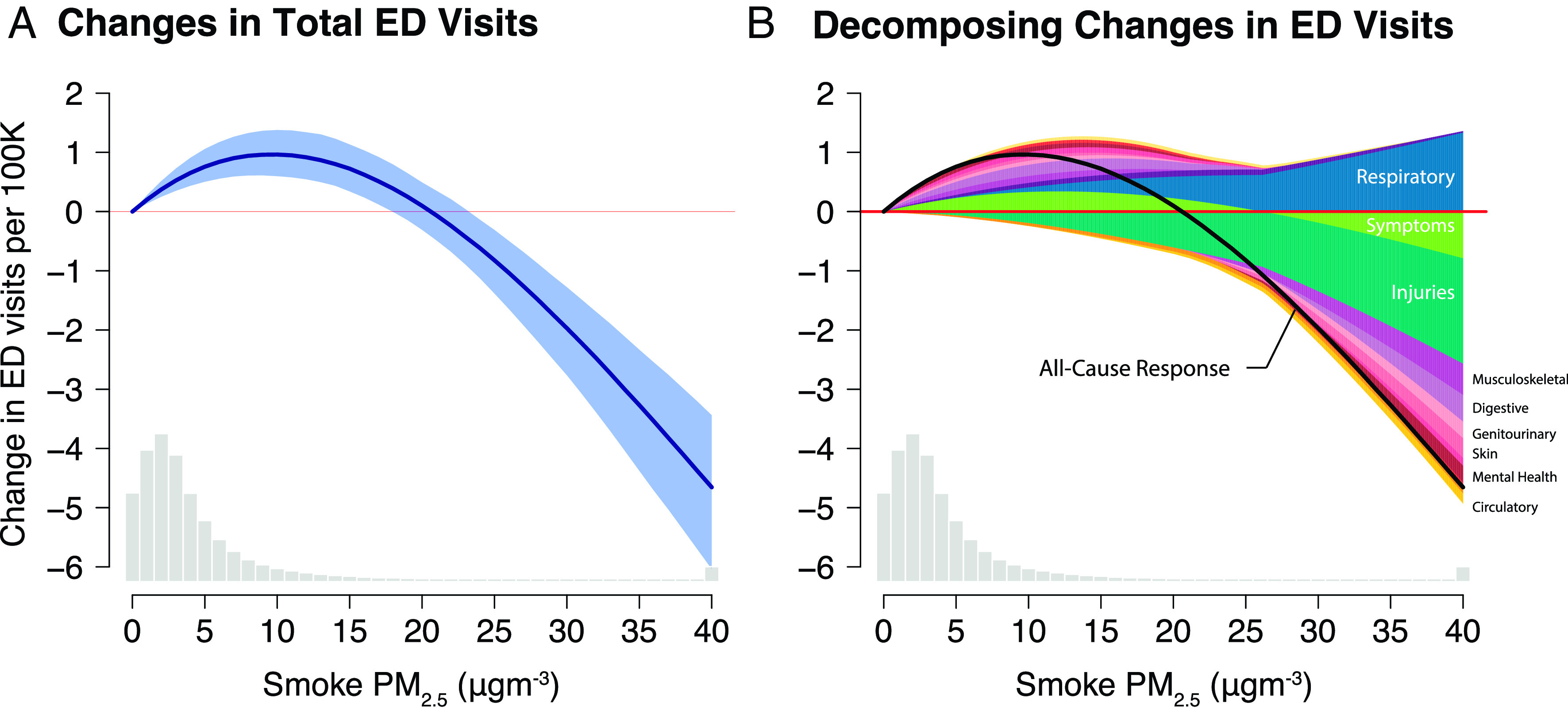
All-cause ED visits increase with additional exposure to moderate levels of smoke pollution but decline dramatically on the most extreme days. (A) The estimated all-cause response is derived from a zipcode-level distributed lag regression model of daily ED visit rates on a 4th-degree polynomial of wildfire smoke intensity measures for the 7 d prior through day-of visit Eq. 2. Coefficient estimates at each level of smoke intensity were summed across lags to estimate the total effect of an additional day at a given exposure intensity on ED visits in the following week. The shaded area indicates bootstrapped 95% CI (Materials and Methods). The histogram at the bottom shows the distribution of smoke intensity across smoke days. (B) Responses separated out by primary ICD grouping associated with the principal visit diagnosis. Each response comes from a different regression with that group of ED visits as the outcome in Eq. 2. The all-cause response estimated from a separate regression and shown in panel A is plotted in black and reflects the net effect of positive and negative impacts associated with different diagnoses (SI Appendix, Fig. S12, for further decomposition).
The observed dose–response of total ED visits to wildfire smoke is the net of diagnosis-specific increases and decreases. Both the magnitude of the diagnosis-specific responses and the baseline frequency of visits for that diagnosis influence each diagnosis’s contribution to the overall response. SI Appendix, Fig. S8, shows the frequency of ED diagnoses across our entire sample. The most common reasons people visit the ED include accidental injuries, general symptoms not associated with a specific diagnosis such as cough or stomach pain, and respiratory conditions including respiratory tract infections and asthma.
The response of ED visits to wildfire smoke differs substantially by diagnosis (Fig. 2B and SI Appendix, Fig. S9). For most acute respiratory conditions, ED visits monotonically increase with wildfire smoke intensity (SI Appendix, Fig. S10). The strongest responses are observed for asthma, COPD, and respiratory symptoms without a specific diagnosis (e.g., shortness of breath and cough), all of which increase by more than 30% in the week after an extreme smoke day, relative to a day without smoke (Fig. 3A). In contrast, for the most common diagnoses in the ED, most of which are not thought to be directly exacerbated by pollution exposure, visits decline at increasingly extreme smoke exposures; these declines more than offset respiratory increases and lead to an overall decline in total ED visits at extreme daily smoke concentrations. This is true even after limiting our sample to zipcodes far from active fires (SI Appendix, Fig. S11) and controlling for ED closures (SI Appendix, Fig. S4D), suggesting that the observed changes are driven by responses to smoke rather than responses to nearby fires or changes in the supply of available care. Results are also robust to including up to a month of lags of our smoke variable (SI Appendix, Fig. S4C), reducing the likelihood that an extreme smoke day is simply displacing non-smoke-related visits to a later day. Our results for ED visits with principal diagnoses related to the circulatory system have wide CIs, and we observe no clear response of ED visits for these causes to wildfire smoke (Fig. 3B).
Fig. 3.
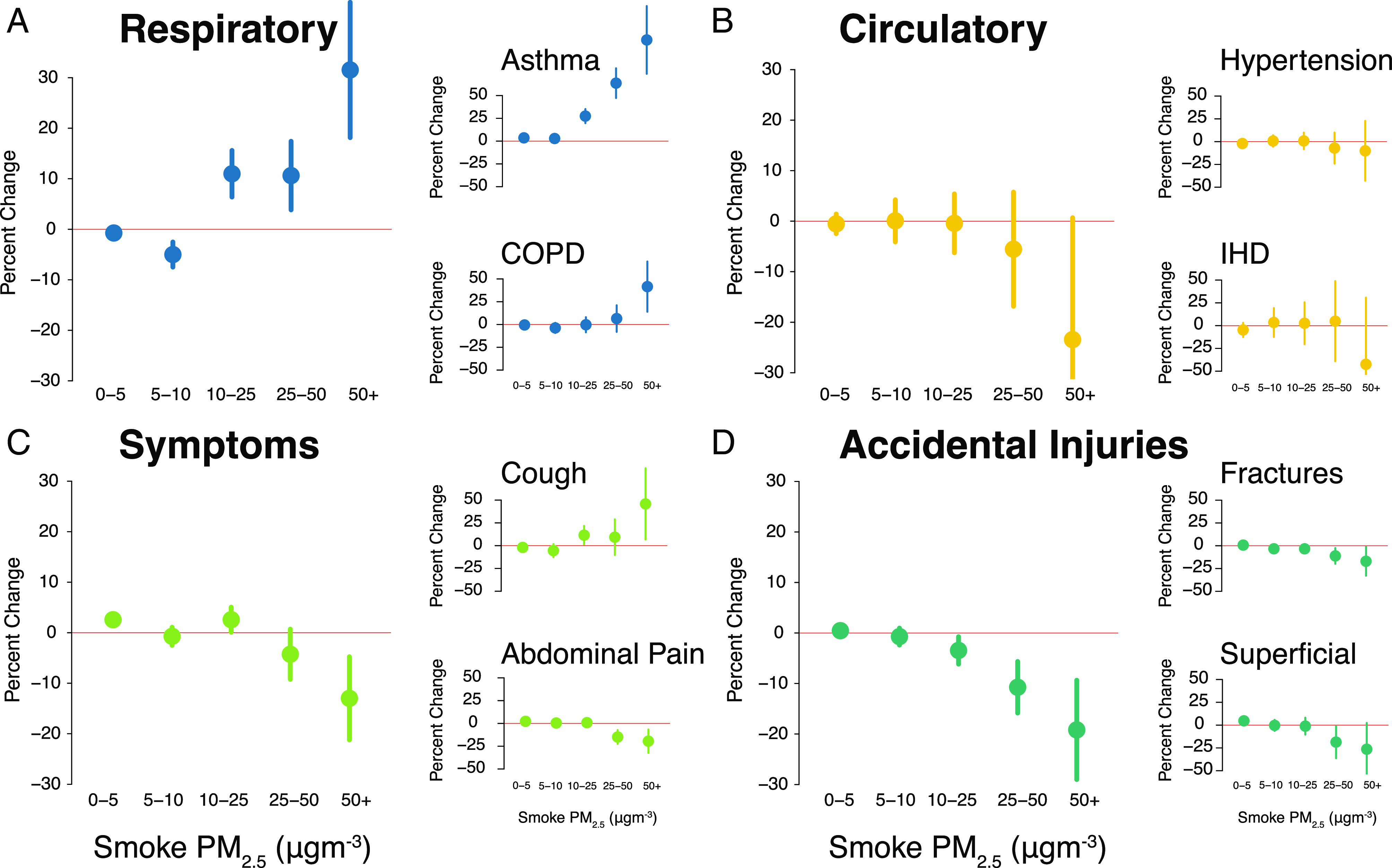
Responses to wildfire smoke vary by smoke intensity, whether diagnosis is directly exacerbated by pollution, and behavioral mechanism. Responses for visits to the ED for respiratory (A), circulatory (B), symptoms (C), and accidental injuries (D) and emblematic cause-subgroups shown in terms of percentage change relative to base rate for select diagnoses. Large panels correspond to primary ICD groupings and small panels correspond to select subcategory groupings. The response in each panel comes from a separate regression estimation of Eq. 3 where ED visits with a given diagnosis grouping are the outcome. Acronyms in labels: COPD = chronic obstructive pulmonary disease, IHD = ischemic heart disease.
In absolute terms, the most common ED visit diagnoses see the largest declines in response to heavy wildfire smoke. However, the relative contribution of different diagnoses varies by smoke intensity (SI Appendix, Fig. S12). This pattern is seen both in aggregate and on a smaller scale within the most frequent principal diagnosis category, “symptoms.” Within this diagnosis grouping, ED visits for nonrespiratory symptoms like abdominal pain or digestive discomfort decline in response to smoke while ED visits for respiratory related symptoms (classified as symptoms because they are not diagnosed to have a specific cause like asthma or COPD), including cough and shortness of breath, increase with wildfire smoke intensity (Fig. 3C and SI Appendix, Fig. S13). At lower smoke intensities, the increases in visits for respiratory symptoms generate an increase in the overall symptoms category, but as smoke intensity increases, the decline in visits for nonrespiratory symptoms dominates. As a result, fewer visits for issues like stomach pain become a large part of the decline in ED visits for symptoms and, in turn, total ED visits.
The largest contributor to the estimated decline in total ED visits at high wildfire smoke intensities is fewer visits for accidental injuries (SI Appendix, Fig. S12), with declines observed for several different types of injuries (SI Appendix, Fig. S14) including both more-urgent (fractures) and less-urgent (superficial injuries) conditions (Fig. 3D). We estimate that in the week following a day with 50 of wildfire smoke (99th percentile exposure), ED visits for accidental injuries decline by 19% (95% CI: 9–30%) with visits for sprains, contusions, fractures, wounds, and superficial injuries each estimated to decline by 15 to 25%.
Responses also differ by age and by health insurance coverage, both of which influence baseline ED utilization (young children and uninsured populations visit the ED at relatively higher rates in our data; see SI Appendix, Figs. S15 and S16). First, while the increases in total ED visits in response to low and moderate smoke levels are driven largely by additional visits for children under 5, the reduction in ED visits at high smoke intensities is driven primarily by reductions in visits among adults 18 to 64 and, to a lesser extent, people over 65 (SI Appendix, Fig. S15). Second, we find that the reduction in ED visits for diagnoses that drive the observed decline at high smoke intensities, such as accidental injuries and general symptoms, is largest in the least-insured zipcodes. For example, we estimate that among less insured populations, ED visits for symptoms strongly decline in response to high-intensity wildfire smoke while populations with high levels of insurance coverage exhibit no changes (Fig. 4A). In contrast, for diagnoses with the most clear physiological linkages to wildfire smoke like asthma, we find that ED visits increase similarly across groups regardless of zipcode-level insurance coverage (Fig. 4B).
Fig. 4.
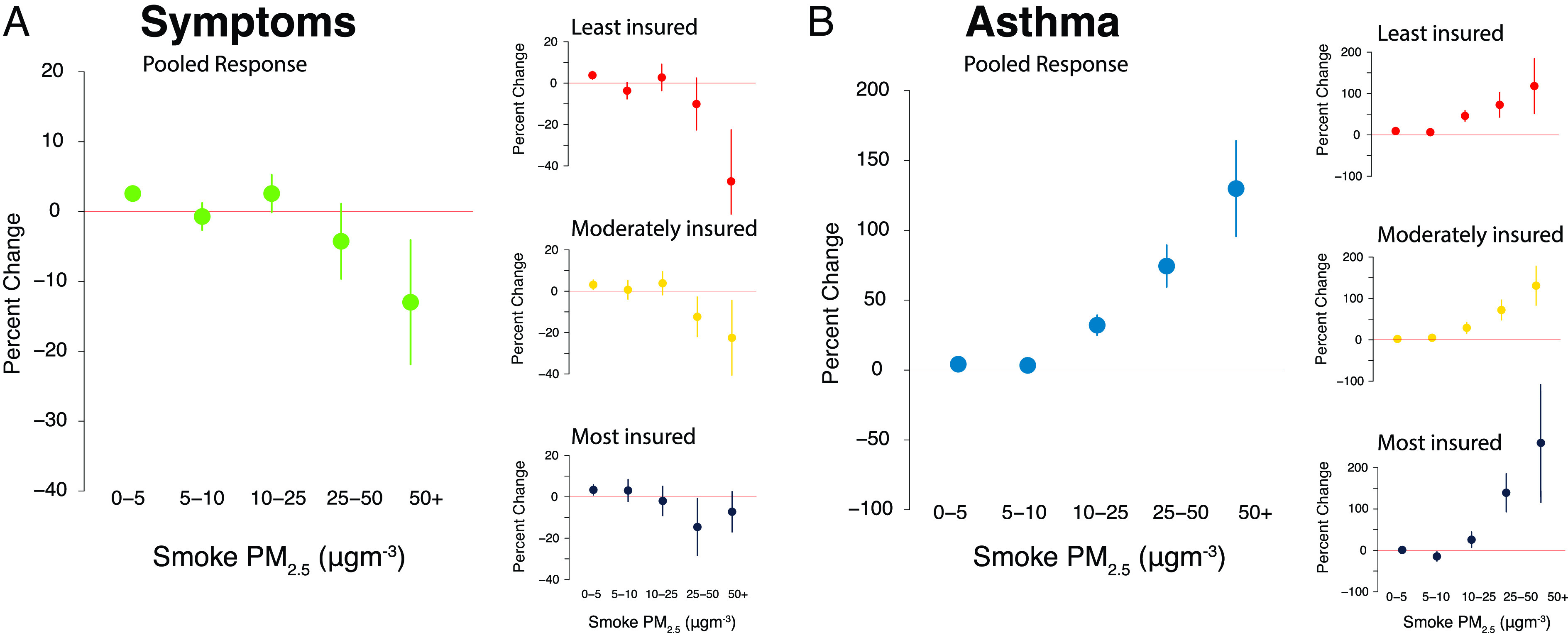
Declines in ED visits for general symptoms (A) at high smoke PM come primarily from reductions in visits among less insured populations whereas increases in ED visits for respiratory conditions (B) occur regardless of insurance coverage. Large panels show pooled responses for that condition, and small panels show responses estimated in separate regressions subsetting by tercile of zipcode-level average insurance coverage rate. All responses shown are estimated with Eq. 3. Responses are plotted as percentage changes from group-specific base rates.
We find evidence that ambient smoke exposure shapes human behavior in a manner consistent with our ED visit results. Internet searches for “air quality” during smoke events in CA rise linearly with ambient smoke levels, indicating that individuals are aware when ambient concentrations are worsening (Fig. 5A). At lower ambient smoke levels (25 ), we observe no change in vehicular traffic on urban highways in CA or visitation to CA national parks or monuments. However, at higher ambient smoke levels (25 ), we find clear evidence of declines in traffic volumes, with the magnitude of the response similar in magnitude to the decline in all-cause ED visits (Fig. 5B); results are robust to inclusion of additional lags of smoke concentrations. We also find evidence that visitation to national parks and monuments in CA decline on days when smoke levels in those parks are high (Fig. 5C), consistent with existing work (24, 31); results are robust to controlling for park closures and proximity to active fires. Taken together, these results are consistent with earlier US-wide results that indicate declining mobility at high ambient smoke levels (25) and suggest that individuals adjust their behavior during periods of high ambient concentrations in ways that could shape both smoke- and non-smoke-relevant health outcomes.
Fig. 5.
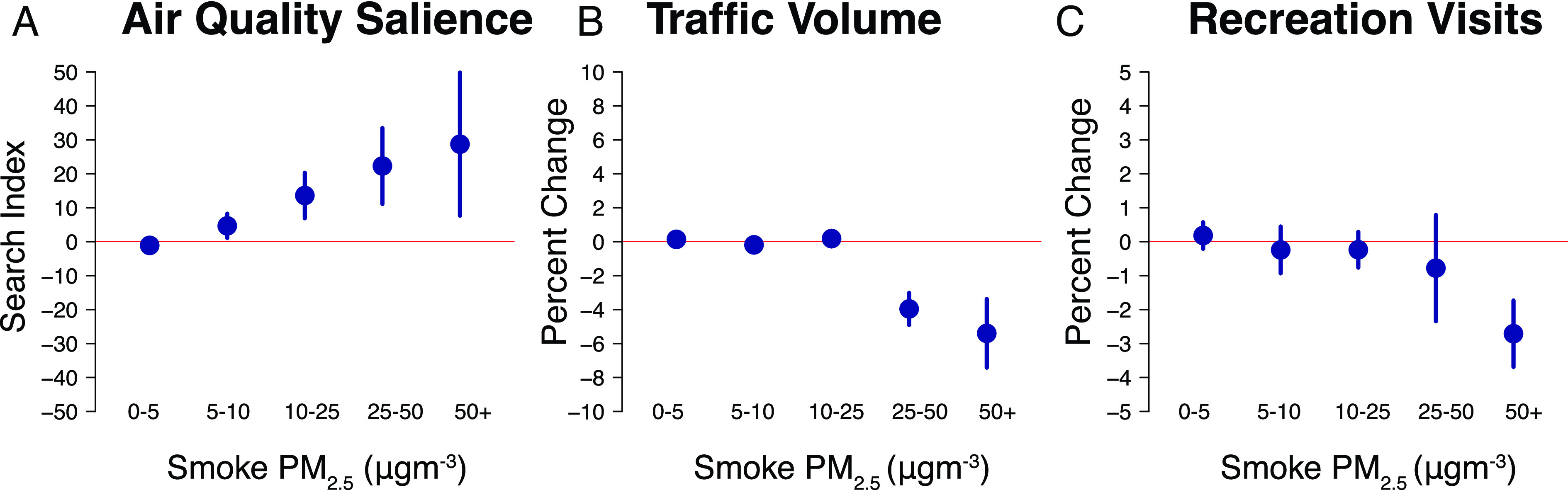
Evidence of wildfire smoke salience and behavioral changes at high smoke PM concentrations. (A) The number of Google searches for the term “Air Quality” increases with smoke PM concentrations; searches are measured using a normalized 0-100 index measuring relative popularity of a search term. (B and C) While the volume of traffic recorded by the California Department of Transportation on urban highways and the number of recreation visits to national parks in California do not change in response to low or moderate smoke levels, they decline in response to higher smoke PM concentrations.
The overall net impact of wildfire smoke on ED visits is a combination of increasing visits on low- and medium-smoke-intensity days and declining visits on the highest-intensity days. Because we find that total ED visits increase with smoke PM across most of the smoke intensity distribution, our estimates suggest that wildfire smoke in California increased total ED visits in every year of our sample (SI Appendix, Fig. S17). Estimated annual increases attributable to wildfire smoke range from a low of 975 additional visits in 2010 (95% CI: 727–1,270) to a high of 6,195 additional visits in 2016 (95% CI: 2,566–8,615). On average across our sample, we estimate that wildfire smoke is responsible for 3,010 additional annual ED visits across California (95% CI: 1,760–4,380). This estimate is generally robust to the use of response curves estimated from different model specifications (SI Appendix, Fig. S18).
Discussion
Our results are broadly consistent with previous findings that ED visits for acute respiratory conditions increase following exposure to wildfire smoke (9–18). In addition, we find evidence that ED visits for other conditions, including general symptoms, increase under low or moderate intensities of wildfire smoke. Taken together, we find that total ED visits increase in the week following low or moderate exposure. However, when ambient wildfire smoke concentrations exceed 20 (95th percentile smoke intensity in our sample), we find ED visit rates actually decline for many causes not typically directly linked to air pollution exposure, such as accidental injuries, abdominal pain, and digestive discomfort. While directly impacted conditions like respiratory symptoms steadily increase at higher wildfire intensities, these ailments represent a small fraction of total ED visits. For example, all respiratory and cardiovascular diagnoses combined account for less than 1 in 5 principal diagnoses in our sample, and thus, any increases in the rates of these diagnoses at high smoke intensities are dominated by the accompanying decreases in more common conditions, resulting in a net decline in total ED visits. These competing effects are not well understood, although short-term reductions in hospitalizations have been noted in response to wildfire smoke (32) and following exposure to other environmental stressors such as hurricanes and snowstorms (6, 19–21).
There are several potential mechanisms that could explain our observation of fewer ED visits under extreme wildfire smoke conditions. Individual decisions to visit the ED balance tradeoffs of the perceived benefits from a visit to the ED (which grow with more acute conditions such as severe asthma) and the costs, including the perceived cost of exposure to extreme smoke. Within this framework, wildfire smoke could induce behavioral responses that alter the decision to visit the ED through at least three different channels. First, behavioral responses could modify exposures. For example, people may remain indoors and turn on air purifiers, which is likely to ameliorate negative health impacts and reduce the number of ED visits for conditions exacerbated by air pollution (33, 34). Second, environmental conditions could impact decisions to seek care in the ED (35). People may opt not to visit the ED because they prefer to stay home (or are encouraged to stay at home by public officials), which could reduce ED visits regardless of how health is impacted. Third, behavioral responses may affect the probability of an injury occurring, even if that injury is unrelated to air pollution. For example, when people remain home, there is less opportunity to get into a car accident (36). Overall impacts on ED visits will therefore depend on how individual health risks shift with these behavioral changes.
Our evidence on traffic volumes and park visits suggests limited behavioral change at low smoke levels. These limited changes are consistent with the observed positive overall effects of smoke on ED visits at these levels, with increases in plausibly smoke-related health outcomes (e.g., respiratory visits) outweighing small observed declines in accidental injuries and general symptoms. Conversely, at high smoke levels, observed avoidance behavior is likely contributing to reductions in non-smoke-related ED visits, and these decreases dominate observed increases in smoke-related outcomes. These effects are likely driven by a combination of alterations to health-seeking behavior and behaviorally induced changes in risks for non-pollution-related injuries. ED visits for superficial injuries and nonacute symptoms decline following intense wildfire smoke and do not rebound over the next month, suggesting that individuals are often foregoing treatment for nonurgent conditions. Similarly, ED visits for fractures, traumatic injuries, and other severe injuries also decline following heavy smoke days and do not rebound, suggesting that reduced opportunity for injury also plays an important role. These findings are consistent with earlier evidence that found that on days with wildfire smoke PM, the number of people who never leave their homes increases by approximately 10% (25). More broadly, our findings are consistent with research from a number of settings demonstrating that avoidance behavior in response to air pollution can shape observed health outcomes (22–24).
We find limited evidence that proximity to fire amplifies the response of ED visits to smoke, suggesting that alterations to the supply of medical services are unlikely to be driving our results. Similarly, we do not find strong evidence that behavioral changes are effectively limiting smoke exposures: ED visits for respiratory conditions increase steadily as ambient smoke concentrations worsen. This increase is consistent with earlier findings of substantial infiltration of wildfire smoke into indoor residential environments (25), suggesting that staying at home is not sufficiently protective to completely avoid health impacts.
Available evidence regarding which age groups are most vulnerable to respiratory impacts from wildfire smoke is mixed (29). Consistent with our hypothesis that responses are strongest among subgroups that utilize the ED more frequently, our age-specific results suggest that children under 5 comprise the largest portion of observed increases in ED visits following smoke exposure. Our results across insurance terciles finding similar magnitude increases in ED visits for asthma but differential decreases in ED visits for symptoms and injuries suggest that while population-wide health, particularly among children, is negatively impacted by wildfire smoke, the overall decline in ED visits at high smoke intensities is driven at least in part by changes in behaviors among populations for whom the ED may play a more prominent role as a healthcare service provider. While we focus here on insurance coverage, which may directly influence ED utilization (share of population with insurance coverage is negatively correlated with ED visit rates in our data), this measure is also highly correlated with other factors that might influence the relationship between wildfire smoke and ED visit rates including income, share of population that speaks English less than “very well,” and frequency of ED visits, and we are not able to disentangle the effects of being insured from other covarying factors (SI Appendix, Fig. S16).
Despite the declines in ED visits at high smoke intensities, we find that wildfire smoke increases total ED visits overall. Given that there are more than 10 million ED visits per year in California, the 3,010 estimated smoke-induced ED visits per year represent a small fraction of total ED visits. However, the contribution of wildfire to ED visits for certain diagnoses such as asthma is likely to be substantially higher. Moreover, the totals for all-cause ED visits would be higher absent the behaviorally induced declines under the most extreme conditions. Our estimated attributed increase in ED visits in CA due to wildfire smoke in an average year represents about a fifth as many excess ED visits as have been attributed to an extreme heat wave (5).
While precise quantitative statements about the welfare impact of estimated changes in ED visits in response to wildfire smoke are difficult given existing data—e.g., we do not have data with which to price or value the avoidance behavior—qualitative analysis suggests overall welfare losses but perhaps ambiguous effects on very bad smoke days. Individuals derive many benefits from days with no smoke in the air, including less need to protect themselves with purifiers or masks, increased enjoyment of outdoor spaces, and relative ease in seeking medical care. However, seeking medical care can also create negative externalities if individuals only pay a portion of the cost of their ED visit and if visits for nonurgent conditions—which can make up a substantial portion of total visits (37, 38)—make treatment of urgent conditions more difficult. At low levels of smoke exposure, we find little obvious evidence of avoidance behavior and clear evidence of an increase in ED visits, relative to a day with no smoke; on these days, welfare effects are likely negative. On very high smoke days, however, we see a decline in injuries and a reduction in treatment-seeking behavior for a range of nonurgent symptoms; we also see a substantial increase in respiratory-related visits. The net effect of these competing channels depends on the relative size of the harm from the increased respiratory visits and any long-term harm from medical treatment foregone, relative to the benefits of a less-crowded ED and a reduction in the so-called “inappropriate-use” ED visits. While it seems plausible that harms from the former outweigh benefits from the latter, further work is needed to precisely quantify these tradeoffs.
There are a number of potential limitations to our approach. First, our unit of analysis is the zipcode day, and thus, our exposure metric could be subject to mismeasurement, particularly for zipcodes whose residents typically spend substantial time outside of their home zipcode. The extent and impact of mismeasurement on parameter estimates depend on the spatial covariance of exposure and whether work-related mobility is systematically related to daily wildfire exposure. As earlier work demonstrates strong spatial covariance in exposure (i.e., nearby areas are exposed similarly) and that individuals are more likely to remain in their residence on smoky days (25), we believe that the impact of this mismeasurement is likely small. Second, autocorrelation in daily wildfire smoke concentrations could affect estimated coefficients on individual lags in our distributed lag model (39). However, previous work in other settings shows that the sum of the lags is unbiased and low variance (40). Moreover, our finding that the shape of the estimated response is similar when we aggregate to the weekly level suggests that this issue is not driving our main results. Third, our exposure measure reflects ambient conditions and thus does not account for variation in how much ambient pollution filters indoors. Observed differential effects across zipcodes could be partially explained by systematic variations in the extent to which ambient wildfire smoke enters homes (25), which could itself be further correlated with ED visit rates, although the direction and magnitude of these differences is difficult to predict and a critical area for future work. Fourth, our wildfire smoke measure is modeled, and we do not have uncertainty measures to propagate through our statistical analysis, and thus, CIs in our outcomes models might be too small; this is a common challenge in the rapidly growing set of studies that use modeled pollution exposure data to estimate dose–response functions. Fifth, our exposure metric characterizes PM from wildfire smoke, not total PM, and marginal effect of smoke PM may differ across levels of nonsmoke PM. Sixth, while we observe detailed individual-level ED visit data, we do not observe direct measurements of injury severity which could allow us to better assess which behavioral mechanisms drive the observed reduction in visits at high smoke intensities. Seventh, we also do not observe visits to urgent care centers or drop-in clinics and thus cannot assess the extent of substitution from ED utilization to other types of healthcare providers.
Wildfire smoke pollution is an increasingly important environmental hazard throughout much of the United States and globally. Our work contributes to an increasingly large body of evidence on the negative impacts of wildfire smoke on health. As our ED data end in 2017, we are unable to measure the impacts of the more widespread extreme smoke exposures that occurred in 2018, 2020, and 2021. Further tracking the impact of these exposures will be critical to understanding and adapting to a warming climate, which is expected to make such exposures increasingly common throughout much of the United States in coming years.
Materials and Methods
Data.
ED visits.
ED visit data (41) come from California’s Department of Health Care Access and Information (HCAI) (known as the Office of Statewide Health Planning and Development prior to 2021). Our sample of the ED patient visit level dataset covers all of the approximately 127 million ED visits that occurred in the 353 nonfederal EDs in California between January 1, 2006, and December 31, 2017. Our data do not include visits to federally run EDs such as the 8 Veterans Affairs EDs in the state. A summary of total ED visits and visits by ICD grouping is shown in Fig. 1A.
Each record within the data consists of a single visit, also referred to as an outpatient encounter. Reported ED encounters include only those patients who had face-to-face contact with a provider. If a patient left without being seen, the patient did not have a face-to-face encounter with a provider, and therefore, the ED encounter does not constitute a visit and thus is not included in the data. The data do include patients that were admitted to the hospital through the ED but do not include visits to Urgent Care centers or other service outlets not classified as EDs.
For each visit, we observe the date of admission, patient characteristics (zipcode of residence, age at the time of service, self-reported race and ethnicity, and sex), primary diagnosis, up to 20 secondary diagnoses, and hospital identifier.
For the main analysis, we calculated daily zipcode-level rates by zipcode of residence for total ED visits and separately for ED visits by primary diagnosis ICD grouping. To calculate daily rates, we divided the total zipcode count of visits in a given grouping on that service date by the zipcode population from the American Community Survey (ACS) in that year (see below for additional details).
USPS zipcodes were mapped to Zipcode Tabulation Areas (ZCTAs), and ZCTAs with 0 population were omitted from our sample. In total, 2,710 unique zipcodes of residence appear in our data. After dropping out-of-state zipcodes and mapping to ZCTAs, we were left with 2,101 unique zipcodes. Of these, 543 additional zipcodes were dropped because they were determined to be PO Boxes and thus did not correspond to an individual’s place of residence. This left us with 6,811,182 zipcode (now ZCTA, but we use the terms interchangeably elsewhere in the paper) by day observations corresponding to 1,554 zipcodes and 4,383 d spanning January 1, 2006, through December 31, 2017.
In addition to all-age all-cause rates and all-age rates by primary diagnosis, we also calculated all-cause rates by age group (0–4, 5–17, 18–34, 35–64, and 65). To calculate daily age-specific rates for all-cause ED visits, we summed the number of visits by age group in each zip day and then divided by the age-group specific annual population derived from the ACS. We do not calculate diagnosis-specific rates by age group because the number of visits within each diagnosis by age group bin is too small to be stable.
We calculated the distance traveled for each visit as the distance from the centroid of the patient’s residential zipcode to the centroid of the zipcode where the ED was located. To identify ED closures, we calculated the total number of visits per day at each ED and then assumed any ED with 0 visits on a given date was closed. Distance to nearest open ED was then calculated at the zip-day level as the distance from residential zipcode centroid to the centroid of the zipcode where the nearest ED open on that date was located.
This work was approved by the Stanford University Institutional Review Board and the California State Committee for the Protection of Human Subjects (IRB 2018-255).
Grouping ED visits by cause.
Each visit in our dataset is associated with a primary diagnosis, which corresponds to a single ICD code as well as up to 20 secondary diagnoses that each corresponds to separate ICD codes. Over the course of our sample, all EDs in California transitioned from ICD-9 to ICD-10 codes. The transition occurred at different times for different hospitals. The groupings used here are based on ICD-9 groupings that were then mapped to ICD-10 codes relying primarily on the Centers for Medicare & Medicaid Services General Equivalence Mappings (42).
However, for some outcomes, there are no 1-to-1 mappings between ICD-9 and ICD-10. In these cases, we assigned additional ICD-10 codes to match the ICD-9 categories used in an effort to avoid discrete jumps in diagnosis-specific rates of ED visits across the ICD-9 to ICD-10 transition. The ICD-9 and ICD-10 codes corresponding to each grouping used in the analysis are linked to in SI Appendix.
Note that our main finding that all-cause ED visits increase at moderate smoke levels and decline at high smoke levels does not rely on the patient’s diagnosis and thus is not influenced by ICD code groupings.
Population.
Single-year annual zipcode population estimates are not available, so we rely on the 5-y averages derived from the American Community Survey (ACS) with the middle year in the running 5-y period corresponding to the year of the ED visit. For example, we estimate 2012 population for a given zipcode as the 5-y average population corresponding to that zipcode from 2010 to 2014 derived from the ACS. In addition to time-varying zipcode populations, average all-age and age group–specific zipcode populations across the sample period were calculated and used as regression weights for the corresponding regressions.
Wildfire smoke concentrations.
Estimates of smoke exposures come from a recent effort to estimate daily wildfire smoke PM concentrations for 10 10 km grid cells across the contiguous United States. These daily wildfire-driven PM concentrations were derived with a machine learning model that used a combination of ground, satellite, and reanalysis data sources as inputs and was trained on daily estimates of wildfire smoke PM concentrations at EPA pollution monitors (28). The model was optimized to predict within-location variation in smoke over time which is important given that our empirical approach relies on temporal rather than spatial variation in smoke exposures to estimate impacts. One limitation of the estimated smoke PM concentrations is that there are no associated uncertainty estimates, so we are unable to formally incorporate uncertainty in exposure measurement into our statistical models of impacts.
To assign exposures to each zipcode (ZCTA) day from 2006 to 2017, we calculated the population-weighted average smoke PM concentration across grid cells using population data from the Gridded Population of the World (GPW), v4 (43). A summary of the data is shown in Fig. 1 C and D. On average, zipcodes in our sample experienced 30.4 d with smoke per year. Among those smoke days, nearly half were associated with low smoke PM concentrations (0 to 5 ). Another 38% of smoke days were associated with moderate smoke PM concentrations (5 to 25 , and 12% of smoke days were associated with smoke PM concentrations above 25 .
Weather.
In our main specifications, we include daily temperature and daily rainfall as covariates. Daily temperature and rainfall were derived from PRISM (44) which estimate daily min and max temperature and total rainfall for 4 km grid cells across the United States. Following the procedure used to process smoke PM data, we calculated daily population-weighted averages across grid cells to derive zipcode by day averages. Population weights were derived from population data from the GPW, v4 (43) by resampling populations to the PRISM grid and taking pop-weighted averages of daily temperature and rainfall at the zipcode by day level.
Distance to fire.
Our estimates for distance to active fire come from previous work (30) and are calculated as the distance from zipcode centroid to the center of the nearest active fire point cluster each day. Fire point clusters are spatially concentrated groups of pixels identified using remotely sensing data from MODIS as having ongoing burning on that day. The purpose of clustering identified fire pixels rather than using every individual pixel identified as having fire is to distinguish active wildfires from other events that look similar in the MODIS fire data. See ref. 30 for details on the clustering algorithm used to identify groups of pixels found to best represent active wildfires.
Community-level characteristics.
Five-year averages from the American Community Survey covering 2011 to 2015 were used to represent average community-level characteristics across our 2006 to 2017 sample (45).
Zipcode-level average insurance coverage rates and income were derived from ACS variable B27015: “Health insurance coverage status and type by household income in the past 12 mo”). This variable provides population counts by insurance status and income group. To derive population counts by health insurance coverage status, we summed across income groups, and to derive population counts by income group, we summed across health insurance coverage status. Population counts were then used to derive population shares for each subgroup.
A similar approach was used to characterize the population not speaking English (ACS variable B06007: “Place of birth by language spoken at home and ability to speak English in the United States”). This variable provides population counts for people who speak English “less than ‘very well”’ separately by the primary language spoken at home and origin (native/non-native). To estimate the share of the population that speaks English less than “very well,” subpopulations were summed across places of birth and languages spoken at home to derive the total number of people that “speaks English less than ‘very well.”’ These totals were then used to calculate the proportion of the zipcode population.
These zipcode-level average community characteristics were used either to stratify regressions (in the case of health insurance) or merely in a descriptive manner (language ability, income) to help characterize the populations stratified by health insurance coverage rates as shown in SI Appendix, Fig. S16.
Measuring salience, traffic, and recreation activities.
We measure salience using public search query data from Google Trends (46). The data are accessed using the R package gtrendsR version 1.4.8.9 and are provided as location-, term- and period-normalized indices ranging from 0 to 100, where 0 is the lowest search volume for that term in that location during the chosen period, and 100 is the highest search volume. The data are available at the Designated Marketing Area (DMA) level (referred to as “metro” areas by Google Trends), which are geographic regions encompassing television media markets as defined by Nielsen. We collected data on searches for the term “Air Quality” in English for all 12 DMAs in California. We use weekly data between January 2016 and December 2020 resulting in a total of 3,132 DMA-week observations.
Traffic volumes come from the California Department of Transportation (Caltrans) Performance Measurement System (47). We utilize daily vehicle counts measured at vehicle detection stations located on state highways throughout California. We include stations with 90% nonmissing daily observations for the years in our main study sample (2006 to 2017). In total, the data include 5,670 stations across 4,383 d corresponding to 25,246,080 station-day observations. To test our hypothesis that people reduce local driving activities in response to high smoke PM concentrations, we focus our analysis on the 4,838 vehicle stations (85% of sample) located within cities as determined by nonmissing values for the “city” variable in the station metadata. These restrictions result in an analysis dataset with 20,994,570 station-day observations. As a robustness check, we also estimate this analysis on the full sample of stations including those with more than 10% missing observations and stations deployed on remote portions of highways.
Monthly recreation visits to areas managed by the National Parks Service (NPS) come from the NPS Visitor Use Statistics Database (48). We utilize visits to all parks with reported visitation statistics in California for the months corresponding to our main analysis study sample (January 2006 to December 2017). In total visits are reported for 23 parks in California resulting in 3,232 park-month observations. Visitations are reported for all parks managed by the NPS including National Parks, National Seashores, National Monuments, and National Recreation Areas. Visitation counts are estimated by NPS based on deployed traffic counters. In addition to providing recreation visitor counts, NPS also publishes monthly visitation comments that provide additional information on factors that may affect visitations. Commonly comments report issues related to partial or full park closures. They also occasionally directly mention nearby fire activity keeping visitors away. We utilize these comments by generating a dummy variable that indicates for each park month whether any portion of the park was reported closed. We also generate a separate indicator for whether fires were noted in the comments. Including these covariates accounts for the effect on visitations of park closures due to fires that we may otherwise conflate with visitation reductions due to smoke.
Modeling ED Visits as a Function of Wildfire Smoke.
We model daily zipcode ED visit rates as a function of wildfire smoke on the day of visit and on days leading up to the ED visit. Specifically, we estimate ED visit rates per 100,000 people () in zipcode on date as a function of wildfire smoke and controls.
| [1] |
Fixed effects at the zipcode level account for time-invariant differences across space (). Fixed effects at the year by season level account for differential trends in exposure and outcomes by season over time (). Fixed effects at the county by month-of-year level account for regional seasonality in exposure and outcomes (), and fixed effects at the day-of-week level account for weekly cycles in ED visits (). The motivation for allowing time trends to vary separately by wildfire season (May to October) and nonwildfire season is that we observe for both exposures and outcomes summer time trends differ from winter time trends. The motivation for allowing seasonality to vary by county is that we see clear regional differences in seasonality in both exposure and outcomes. In our main specification, includes daily maximum temperature, daily rainfall, and the calculated distance from the zipcode centroid to the nearest active fire on that day (see SI Appendix for further discussion of model specification choices).
Effects are calculated from OLS regression estimates of Eq. 1 using average zipcode population weights. To understand the shape of the response, we utilize various nonlinear functional forms for including binned specifications, splines, and higher-order polynomials.
Nonlinear, polynomial response of ED visits to ambient wildfire smoke.
Our main specification (shown in Fig. 2) is a 4th-degree polynomial with 7 lags (day of visit plus seven additional daily lags for a total of 8 d), which corresponds to Eq. 1 taking the following form:
| [2] |
To derive the cumulative response of wildfire smoke, we sum the coefficients for each polynomial degree across the day of visit and seven additional lags. For example, is estimated as , is estimated as , and so on. The interpretation of the cumulative effect at, for example, a smoke PM concentration of 25 is the effect of a day of smoke PM at 25 on the total number of additional ED visits in the following 8 d (day of smoke plus seven additional days) relative to a day with no smoke PM.
The responses shown in Fig. 2 corresponds to through evaluated at smoke PM concentrations ranging from 0 to 40 (the 98th percentile of wildfire smoke in our data). In other words, for each value of S = smoke PM from 0 to 40, we plot (S, *S + + + ).
CIs for the polynomial specification shown in Fig. 2A (and used for the attribution calculations) are derived by bootstrapping our estimation sample 1,000 times where we sample zipcodes with replacement with probability proportional to their population. For each draw of the data, we reestimate Eq. 2, sum polynomial degree coefficients across lags, and evaluate at every of smoke PM concentration from 0 to 40. 95% CIs are then estimated by taking the 2.5th and 97.5th percentile estimate across bootstrap runs for each smoke PM concentration. To ensure that 1,000 is a sufficiently large sample size, we confirm that estimated CIs are similar when calculated from 500, 750, and 1,000 samples, respectively.
The decomposition by diagnosis shown in Fig. 2B is derived using the same approach described above but from separate regressions for each of the 14 diagnoses. For each smoke PM concentration responses for individual diagnoses are then divided into positive or negative effects, sorted by magnitude, and plotted on top of each other.
To account for multiple hypothesis testing in our diagnosis-specific regressions, we apply the Bonferroni correction. For example, because we analyze 14 different primary ICD groupings, the estimated 95% CIs for diagnosis specific estimates (SI Appendix, Fig. S9) correspond to .
Binned response of ED visits.
The nonparametric binned version of Eq. 1 estimates nonlinearities by dividing daily smoke PM concentrations into discrete bins and then estimating separate coefficients for each bin. This binned specification takes the form:
| [3] |
where is a dummy for whether smoke PM in zip and date falls into the range of bin and fixed effects and controls are the same as Eq. 1.
The main binned specification divides smoke PM concentrations into five bins corresponding to smoke PM ranges of 0 to 5 (not inclusive of 0), 5 to 10, 10 to 25, 25 to 50, and 50 . These cutoffs were selected to correspond to approximately the 50th, 75th, 90th, 95th, and 99th percentile of the smoke PM distribution (Fig. 1D). Additional versions of Eq. 3 are also estimated by alternatively dividing smoke PM into 6 equally spaced 10 bins (0–10, 10–20, 20–30, 30–40, 40–50, and 50) or by dividing smoke PM into equally spaced 25 bins (0–25, 25–50, and 50). Results for all versions of the binned specifications are shown in SI Appendix, Fig. S5.
To derive the cumulative response across multiple days for the binned models, we sum the coefficients for each bin across all lags. Unlike the polynomial cases, because the binned specification is linear in each bin, we can calculate analytical standard errors for the sum of the lags. These estimated standard errors, clustered at the zipcode level, are then used to calculate the 95% CIs.
Because of the substantial computational requirements associated with estimating bootstrapped CIs for the polynomial specifications, we estimated the main binned specification for all regressions other than the main all-cause specification shown in Fig. 2. With the exception of the robustness evaluation shown in SI Appendix, Fig. S4, all other figures reflect results from regression estimates of Eq. 3 with the 0 to 5 (not inclusive of 0), 5 to 10, 10 to 25, 25 to 50, and 50 bins.
Weekly responses.
To assess whether our results depend on the level of temporal aggregation, we reestimate our daily model at a weekly level. To do so, we first sum ED visit counts and recalculate weekly zipcode-level ED visit rates. For exposure, we sum the number of days in each smoke PM bin occurring that week. For controls, we calculate mean temperature, rainfall, and distance to fire. We then reestimate Eq. 3 using our main bin cutoffs and include analogous fixed effects (zip, county by month of year, season year, and week of year).
We include the contemporaneous week and an additional lag to account for week-of exposure as well as exposure from the previous week. As with the daily analysis, we then calculate cumulative effects as the sum of the coefficients, and we calculate the analytical standard errors clustered at the zipcode level. Because we expect less autocorrelation between weekly smoke PM than for daily smoke PM, this exercise allows us to evaluate the shape of the estimated response curve in a lower collinearity setting. The total ED visit response estimated at the weekly level is shown in SI Appendix, Fig. S7.
Stratified responses.
For cause- and age-specific regressions, we estimate Eq. 3 separately for each ED visit rate. For the cause-specific analysis, we evaluate the hypothesis that wildfire smoke increases ED visits separately for each of the many diagnoses of interest. To account for these multiple hypotheses, we implement a Bonferroni correction to calculate adjusted 95% CIs corresponding to Eq. 3. Namely, we first estimate the standard errors for the sum of each bin’s coefficients across lags (clustered at the zipcode level), and then, we use these standard errors to calculate CIs with where reflect the number of outcomes. We then refer to the CIs as Bonferroni-adjusted 95% CIs. For example, the 95% CIs shown in SI Appendix, Fig. S9 are calculated as .
Because we do not observe insurance status at the individual level, we cannot calculate ED visit rates specific to the insured (or uninsured) population. Instead, we divide zipcodes into terciles based on the average percentage of the population that has health insurance during our sample as reported in the American Community Survey. We then estimate Eq. 3 separately for each subset of zipcodes. This approach allows us to estimate separate responses by insurance coverage status. However, average health insurance coverage rates are correlated with a suite of other factors (SI Appendix, Fig. S16) that we cannot empirically disentangle. Thus, we interpret the stratification by insurance coverage as a measure of vulnerability that includes insurance coverage and correlated factors.
Estimating ED Visits Attributable to Ambient Wildfire Smoke.
To estimate the number of ED visits attributable to wildfire smoke, we utilize the response curve shown in Fig. 2 (which corresponds to a regression estimate of Eq. 2) and apply the coefficients to historical smoke PM concentrations for each zipcode day. Evaluating the estimated coefficients at observed smoke PM levels produces estimates of the change in all-cause ED visit rates for each zipcode and day. We then scale these estimated rate changes by the population in each zipcode at the time and sum across zipcodes and days in each year. The output of this calculation is an annual estimate of additional ED visits statewide encompassing visits on the day of and in the 7 d following every observed smoke event 2006 to 2017. To estimate 95% CIs on estimated attributable ED visits, we utilize the CIs on the response curve shown in Fig. 2. Annual estimated excess ED visits attributable to wildfires smoke are shown in SI Appendix, Fig. S17. To assess the sensitivity of these estimates, we also reestimate attributable ED visits using the different response functions produced by different model specification choices shown in SI Appendix, Fig. S4. Estimated attributable ED visits under different model choices are shown in SI Appendix, Fig. S18.
Estimating Behavioral Responses to Wildfire Smoke.
To directly assess whether we detect behavioral changes in response to wildfire smoke, we incorporate data on air quality salience, traffic volume, and recreation visits and estimate how each outcome responds nonlinearly to concentrations of PM from wildfire smoke. Air quality salience, as measured by the frequency of Google searches for the term “air quality,” is observed at the DMA-week level (see above for details), traffic volume is observed at the vehicle detection station by day level, and recreation visits are observed at the park by month level.
For each outcome, we apply Eq. 3 adapted to the relevant unit of analysis. For air quality salience, smoke exposure is measured as the count of days within a smoke bin range in that DMA week. We include date and DMA by month fixed effects and weekly mean temperature and total precipitation as controls. Because traffic volume is observed at the station-day level, we utilize the construction of smoke bins used in the ED analysis but measured at the station locations. We also include analogous fixed effects (station ID, season by year, county by month of year, day of year, and day of week) as well as temperature and precipitation controls and estimate the model with and without the inclusion of lagged-day smoke exposures. For recreation visits which are observed at the park-month, smoke bins indicate the number of days in the month that smoke concentrations at that park fell into the particular range. For this model, we include park, year, and park by month-of-year fixed effects. In addition to monthly mean temperature and total rainfall, we also include controls for whether there were park closures and whether the NPS noted that wildfires affected visitation counts in that month (see Materials and Methods, Data for details on how these variables were constructed).
Because we model outcomes as a function of daily smoke PM concentration bins for all three models (aggregated to counts of days for the weekly and monthly analysis), the interpretation of the estimated coefficients is the effect on the outcome of an additional day at a given smoke concentration. Because of the way search frequencies are reported by Google, we cannot calculate percent changes and therefore report effects in terms of changes in search index. For traffic volume and recreation visits, we report results as percent changes relative to the baseline mean.
Supplementary Material
Appendix 01 (PDF)
Acknowledgments
We thank Iván Higuera-Mendieta, Ayako Kawano, Hunt Allcott, members of the Environmental Change and Human Outcomes lab, and seminar participants at Stanford, University of California Berkeley, University of California Santa Barbara, Columbia, and Montana State for helpful comments.
Author contributions
S.H.-N., C.F.G., E.B., and M.B. designed research; S.H.-N., C.F.G., M.L.C., M.V.K., M.D., E.B., and M.B. performed research; S.H.-N., C.F.G., and M.B. analyzed data; and S.H.-N., C.F.G., M.L.C., M.V.K., K.C.N., M.D., E.B., and M.B. wrote the paper.
Competing interests
The authors declare no competing interest.
Footnotes
This article is a PNAS Direct Submission. S.L. is a guest editor invited by the Editorial Board.
Data, Materials, and Software Availability
Code and nonprivate data used in the analysis have been made available at https://github.com/echolab-stanford/pnas-ed-smoke-2023 (49). Due to privacy concerns and our data use agreement with the California Department of Health Care Access and Information we cannot share ED visit data. We have provided code and instructions for reconstructing our analysis dataset from the ED visit encounter data which researchers can apply for access to at: https://datarequest.hcai.ca.gov/csm?id=csm_login (50).
Supporting Information
References
- 1.Zhang K., Chen T.-H., Begley C. E., Impact of the 2011 heat wave on mortality and emergency department visits in Houston, Texas. Environ. Health 14, 2015 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen T., et al. , Time-series analysis of heat waves and emergency department visits in Atlanta, 1993 to 2012.. Environ. Health Perspect. 125, 057009 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schaffer A., Muscatello D., Broome R., Corbett S., Smith W., Emergency department visits, ambulance calls, and mortality associated with an exceptional heat wave in Sydney, Australia, 2011: A time-series analysis. Environ. Health 11, 1–8 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schramm P. J., et al., Heat-related emergency department visits during the northwestern heat wave—United States, June 2021. Morb. Mortal. Wkly. Rep. 70, 1020 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knowlton K., et al. , The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ. Health Perspect. 117, 61–67 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parks R. M., et al. , Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat. Commun. 12, 1–12 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramesh B., et al. , Emergency department visits associated with satellite observed flooding during and following Hurricane Harvey. J. Expo. Sci. Environ. Epidemiol. 31, 832–841 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geehr E. C., et al. , Emergency health impact of a severe storm. Am. J. Emerg. Med. 7, 598–604 (1989). [DOI] [PubMed] [Google Scholar]
- 9.Heaney A., et al. , Impacts of fine particulate matter from wildfire smoke on respiratory and cardiovascular health in California. GeoHealth 6, e2021GH000578 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stieb D. M., Szyszkowicz M., Rowe B. H., Leech J. A., Air pollution and emergency department visits for cardiac and respiratory conditions: a multi-city time-series analysis. Environ. Health 8, 1–13 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reid C. E., et al. , Associations between respiratory health and ozone and fine particulate matter during a wildfire event. Environ. Int. 129, 291–298 (2019). [DOI] [PubMed] [Google Scholar]
- 12.Stowell J. D., et al. , Associations of wildfire smoke PM exposure with cardiorespiratory events in Colorado 2011–2014. Environ. Int. 133, 105151 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wettstein Z. S., et al. , Cardiovascular and cerebrovascular emergency department visits associated with wildfire smoke exposure in California in 2015. J. Am. Heart Assoc. 7, e007492. (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alman B. L., et al. , The association of wildfire smoke with respiratory and cardiovascular emergency department visits in Colorado in 2012: A case crossover study. Environ. Health 15, 64 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reid C. E., et al. , Differential respiratory health effects from the 2008 northern California wildfires: A spatiotemporal approach. Environ. Res. 150, 227–235 (2016). [DOI] [PubMed] [Google Scholar]
- 16.Johnston F. H., et al. , Air pollution events from forest fires and emergency department attendances in Sydney, Australia 1996–2007: A case-crossover analysis. Environ. Health 13, 1–9 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rappold A. G., et al. , Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ. Health Perspect. 119, 1415–1420 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tham R., Erbas B., Akram M., Dennekamp M., Abramson M. J., The impact of smoke on respiratory hospital outcomes during the 2002–2003 bushfire season, Victoria, Australia. Respirology 14, 69–75 (2009). [DOI] [PubMed] [Google Scholar]
- 19.Shah S., Murray J., Mamdani M., Vaillancourt S., Characterizing the impact of snowfall on patient attendance at an urban emergency department in Toronto, Canada. Am. J. Emerg. Med. 37, 1544–1546 (2019). [DOI] [PubMed] [Google Scholar]
- 20.Weinberger K. R., et al. , Association between Hurricane Sandy and emergency department visits in New York City by age and cause. Am. J. Epidemiol. 190, 2138–2147 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Platz E., Cooper H. P., Silvestri S., Siebert C. F., The impact of a series of hurricanes on the visits to two central Florida emergency departments. J. Emerg. Med. 33, 39–46 (2007). [DOI] [PubMed] [Google Scholar]
- 22.Neidell M., Information, avoidance behavior, and health the effect of ozone on asthma hospitalizations. J. Hum. Resour. 44, 450–478 (2009). [Google Scholar]
- 23.Barwick P. J., Li S., Lin L., Zou E., From fog to smog: The value of pollution information (National Bureau of Economic Research, 2019). [Google Scholar]
- 24.Keiser D., Lade G., Rudik I., Air pollution and visitation at us national parks. Sci. Adv. 4, eaat1613 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burke M., et al. , Exposures and behavioural responses to wildfire smoke. Nat. Hum. Behav., 6, 1351–1361 (2022). [DOI] [PubMed] [Google Scholar]
- 26.F. Shilling, D. Waetjen, Special report (2): Impact of COVID19 mitigation on numbers and costs of California traffic crashes (Tech. Rep. 2, 2020).
- 27.Seneviratne S. I., et al. , Chapter 11: Weather and climate extreme events in a changing climate (IPCC Sixth Assessment Report, 2021).
- 28.Childs M., et al. , Daily local-level estimates of ambient wildfire smoke PM for the contiguous US. Environ. Sci. Technol., (2022). [DOI] [PubMed] [Google Scholar]
- 29.Reid C. E., et al. , Critical review of health impacts of wildfire smoke exposure. Environ. Health Perspect. 124, 1334–1343 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burke M., et al. , The changing risk and burden of wildfire in the United States. Proc. Natl. Acad. Sci. U.S.A. 118, e2011048118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gellman J., Walls M., Wibbenmeyer M., Wildfire, smoke, and outdoor recreation in the western united states. Forest Policy Econ. 134, 102619 (2022). [Google Scholar]
- 32.Hutchinson J. A., et al. , The San Diego 2007 Wildfires and Medical Emergency Department presentations, inpatient hospitalizations, and outpatient visits: An observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med. 15, e1002601 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Henderson D. E., Milford J. B., Miller S. L., Prescribed burns and wildfires in colorado: Impacts of mitigation measures on indoor air particulate matter. J. Air Waste Manag. Assoc. 55, 1516–1526 (2005). [DOI] [PubMed] [Google Scholar]
- 34.Kunzli N., et al. , Health effects of the 2003 southern california wildfires on children. Am. J. Respir. Crit. Care Med. 174, 1221–1228 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hahn M. B., Kuiper G., O’Dell K., Fischer E. V., Magzamen S., Wildfire smoke is associated with an increased risk of cardiorespiratory emergency department visits in alaska. GeoHealth 5, e2020GH000349 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Law R. K., et al. , Injury-related emergency department visits during the covid-19 pandemic. Am. J. Prev. Med. 63, 43–50 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uscher-Pines L., Pines J., Kellermann A., Gillen E., Mehrotra A., Emergency department visits for nonurgent conditions: systematic literature review. Am. J. Manag. Care 19, 47–59 (2013). [PMC free article] [PubMed] [Google Scholar]
- 38.Carret M. L. V., Fassa A. G., Kawachi I., Demand for emergency health service: factors associated with inappropriate use. BMC Health Serv. Res. 7, 1–9 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Basagaña X., Barrera-Gómez J., Reflection on modern methods: visualizing the effects of collinearity in distributed lag models. Int. J. Epidemiol. 51, 334–344 (2022). [DOI] [PubMed] [Google Scholar]
- 40.McGuirk E., Burke M., The economic origins of conflict in africa. J. Polit. Econ. 128, 3940–3997 (2020). [Google Scholar]
- 41. HCAI, Nonpublic emergency department data. Individual Emergency Department Encounters. https://hcai.ca.gov/data-and-reports/healthcare-utilization/emergency-department/. Deposited 23 July 2019.
- 42.Centers for Medicare & Medicaid Services. Icd-9-cm to and from icd-10-cm and icd-10-pcs crosswalk or general equivalence mappings (2010). https://www.nber.org/research/data/icd-9-cm-and-icd-10-cm-and-icd-10-pcs-crosswalk-or-general-equivalence-mappings. Accessed 19 May 2022.
- 43.Columbia University. Center for International Earth Science Information Network (CIESIN). Gridded population of the world, version 4 (GPWv4): Population density adjusted to match 2015 revision of un wpp country totals, revision 10 (2017). 10.7927/H49884ZR. Accessed 19 May 2022. [DOI]
- 44.Oregon State University PRISM Climate Group, https://prism.oregonstate.edu. Accessed 16 December 2020.
- 45.American Community Survey (ACS), ACS demographic and housing estimates. ACS 5-year estimates. https://data.census.gov/. Deposited 5 August 2022.
- 46.Google, Google Trends. Query Trends. https://trends.google.com/trends/. Deposited 12 September 2021.
- 47.Caltrans, Daily Vehicle Traffic. Station Day Vehicle Totals. https://pems.dot.ca.gov/. Deposited 27 April 2023.
- 48.National Parks Service, Visitor use statistics. Recreation Visits by Month. Deposited 5 May 2023.
- 49.Heft-Neal S., et al., Emergency department visits respond nonlinearly to wildfire smoke. Replication Materials (Version 1). https://github.com/echolab-stanford/pnas-ed-smoke-2023. Deposited 12 July 2023. [DOI] [PMC free article] [PubMed]
- 50.California Department of Health Care Access and Information, Nonpublic emergency department data. Individual Emergency Department Encounters. https://datarequest.hcai.ca.gov/csm?id=csm_login. Accessed 23 July 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 01 (PDF)
Data Availability Statement
Code and nonprivate data used in the analysis have been made available at https://github.com/echolab-stanford/pnas-ed-smoke-2023 (49). Due to privacy concerns and our data use agreement with the California Department of Health Care Access and Information we cannot share ED visit data. We have provided code and instructions for reconstructing our analysis dataset from the ED visit encounter data which researchers can apply for access to at: https://datarequest.hcai.ca.gov/csm?id=csm_login (50).


