Abstract
Background
A kidney recipient's urinary tract infection (UTI) can result in infectious problems and be a risk factor for less successful transplant outcomes. UTI risk factors are still controversial. The present study aimed to investigate the prevalence of UTI and its association with risk factors in kidney recipients.
Method
Twenty-six papers published between 2005 and 2022 were retrieved using keywords and searching Medlib, ScienceDirect, PubMed, and other databases. If possible, the pooled prevalence of UTI in kidney recipients and odds ratio (OR) with a 95% confidence interval for each risk factor were calculated. The data were analyzed using the random effects model in R and Stata 14.
Results
The total sample size was 72,600, with an average age of 48.7 years. The pooled prevalence of UTI was 35% (95% CI, 30–40%). The estimated risk factors for UTI were female (OR = 3.13; 95%CI: 2.35—4.17), older age (OR = 1.03; 95%CI: 1—1.05), history of UTI (OR = 1.31; 95%CI) CI: 1.05—1.63), receiving a kidney from a deceased donor (OR = 1.59; 95%CI: 1.23—2.35), long-term use of an indwelling catheter (OR = 3.03; 95%CI: 1.59—6.59), a ureteral stent (OR = 1.54; 95%CI: 1.16—2.06), diabetes (OR = 1.17; 95%CI: 0.97—1.41), hypertension (OR = 1.6; 95%CI: 1.26—2.28), acute rejection process (OR = 2.22; 95%CI: 1.45—3.4), and abnormal urinary tract anatomy (OR = 2.87; 95%CI 1.44—5.74).
Conclusion
This meta-analysis revealed that UTIs are a significant problem in kidney recipients. Factors such as female sex, old age, history of UTIs, deceased donor, long-term use of an indwelling catheter, diabetes, acute rejection process, use of ureteral stent, abnormal urinary tract anatomy, and hypertension were related to an increased risk of UTIs in kidney recipients.
Keywords: Urinary tract infection, Risk factors, Prevalence, Kidney transplant
Introduction
Kidney transplantation has gained popularity as the preferred medical procedure for the majority of patients in recent years with advanced and chronic kidney failure, which improves their quality of life and increases their life expectancy [1, 2]. Despite progress in this field, post-transplant infections remain a major cause of death in kidney recipients, including active infections preventing transplants and treatable chronic infections before transplantation [3]. Bacterial infections are among the most critical causes of transplant rejection and mortality in the early post-transplantation stages [4–81]. Around 80% of transplant recipients get infections within the first post-transplant year due to factors like potent immunosuppression, surgery, and continuous exposure to hospital-acquired pathogens [4–6]. Infection and dysfunction of the internal organs have a close and strong relationship with using immunosuppressive drugs post-transplant [7]. The most important risk factors that cause post-transplantation infection are the amount and initial dose of immunosuppressive drugs, the manner and degree of continuing immunosuppression during treatment, and the process of acute transplant rejection [8]. Prevention procedures, quick diagnosis, and treatment of this infection are vital [9]. Various studies have shown that UTIs are the most common infection among kidney recipients worldwide [10]. UTIs are one of the main causes of complications and hospitalization after kidney transplantation and seriously threaten successful transplantation outcomes [11, 12]. Almost one out of four kidney recipients will have a UTI within one-year post-transplantation, and these infections can negatively impact transplant outcomes if not well-treated [13, 14]. The prevalence of bacterial infections in different countries varies from 35 to 79%, and about 60% of nosocomial septicemias in kidney recipients are caused by UTIs [15, 16]. UTIs are usually expected in a short period post-transplantation [17]. The risk of getting an infection 3 to 6 months post-transplantation is equal to the general population, and this late infection has a better prognosis than early urinary infection [18, 19]. Since urinary infection in the first three months, post-transplantation is usually asymptomatic, in many cases [81], it can manifest itself with pyelonephritis, bacteremia, dysfunction of the transplanted organ, and a high risk of bacterial infection recurrence [20]. Correct diagnosis of UTI and appropriate treatment play a significant role in preventing transplant rejection and mortality. Risk factors related to the development of UTIs include sex, age, dose and duration of immunosuppression, co-morbidities such as diabetes mellitus (DM), aggressive urological maneuvers, and delay in transplant function as the most important parameters involved [23]. In addition, urinary tract instruments, including urinary catheters and ureteral stents, have also been identified as potential risk factors for UTIs post-transplantation [24]. Kidney recipients' most common pathogens leading to UTIs include Enterobacteriaceae, Enterococci, Staphylococci, and Pseudomonas. Other less prevalent microorganisms include Salmonella, Candida, and Corynebacterium uroliticum. Moreover, there is a possibility of infection by uncommon pathogens such as Mycoplasma hominis, Mycobacterium tuberculosis, or JC and BK viruses [25]. The most common symptoms of lower UTI are frequent urination and urgency due to cystitis. However, symptoms of more severe infection, such as fever, kidney allograft sensitivity, and sepsis due to acute pyelonephritis can also be seen [24]. Considering the importance of timely diagnosis and treatment to prevent life-threatening complications and transplant loss, it is necessary to identify the risk factors of UTI.
Given the importance of kidney transplants, we reviewed the data of different studies to identify the prevalence and influential risk factors for the development and progression of UTI in kidney recipients.
Method
Search strategy
This meta-analysis investigated the prevalence and risk factors for UTI in kidney recipients. Electronic documents and resources available until July 2022 were reviewed. Scientific journals and papers in PubMed, Medlib, ScienceDirect, ISI, Scopus, and Embase databases were retrieved. Articles were searched mainly using valid keywords such as kidney transplant, kidney transplantation, renal transplant, organ transplantation, organ transplant, urinary tract infection, UTI, infection, factors, and possible combinations in English. Keywords were standardized in MeSH and used for searching.
Inclusion and exclusion criteria
The inclusion criteria were: (1) studies that included adult patients receiving kidney transplants; (2) studies that investigated risk factors for UTI in patients after kidney transplantation; (3) studies in which immunosuppressant guidelines were similar after kidney transplantation; (4) the definition and diagnostic criteria of UTI were the same as the criteria of the Centers for Disease Control and Prevention (positive urine culture, i.e., ≥ 105 microorganisms per cc of urine) or clinical manifestations of fever > 38 °C, dysuria, urinary frequency, and urinary urgency, in the absence of pyelonephritis and the and criteria for cystitis).
The exclusion criteria were: (1) studies that included subjects with kidney transplant dysfunction caused by an acute disease other than UTI (e.g., myocardial infarction, acute intra-abdominal disorders, stroke); (2) studies that lacked risk factors for UTI or insufficient data to calculate the odds ratio (OR) of UT; (3) qualitative and descriptive studies; (4) abstract only, conference papers, reviews, systematic reviews, and meta-analyses; (5) studies published in languages other than English.
Study selection
Using Endnote X8, two researchers examined the titles and abstracts of the papers and then screened them according to the inclusion and exclusion criteria. Articles that met the requirements were further evaluated by reading their full text. In a disagreement between the two researchers, a third researcher passed the final judgment.
The selected documents were thoroughly reviewed, and all their information was entered into a data extraction form; then, the data were imported into Microsoft Excel. In the next step, the data were transferred from Excel to Review Manager 5.3 and Stata 14. The data collected in this study included the author's name, year of publication, location of research, number of patients, mean age, duration of follow-up, design, female/male, deceased donors/living donors, number of UTIs, risk factors of UTI including underlying disease (diabetes, hypertension), use of ureteral stents, days of catheterization, history of UTI, acute rejection process (ACR), abnormal anatomy of the urinary tract, and the abundance of UTI-causing bacteria. The primary objective was to investigate the prevalence of UTI in kidney recipients, and the main goal was to examine the risk factors of UTI in these patients.
Risk of bias assessment
Two reviewers independently evaluated the study's quality using the Newcastle–Ottawa checklist. Discussions with the third reviewer helped to resolve discrepancies. Scores under 3, under 6, and between 7 and 9 were regarded as low, moderate, and high-risk studies, respectively. The total score varied from 0 to 9. The discussion was used to settle any disagreements between the two investigators in each process. The details of risk of bias assessment are available in Table 1. Also, publication bias was evaluated by visual inspection of funnel plot asymmetry (Fig. 1).
Table 1.
Risk of bias assessment of the included studies
| Study (Ref) | Exposed representation | Nonexposed selection | Selection Ascertainment of obesity | Outcome absent at study start | Comparability | Outcome assessment | Outcome Follow-up length | Adequacy of follow-up | Overall score | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|
| Adjustment by age and nodal status or stage | ||||||||||
| Bonkat G [42] | 1 | 1 | - | 1 | 1 | 1 | 1 | 1 | 7 | Low |
| Alangaden G J [5] | - | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | Low |
| Sorto R [43] | 1 | 1 | - | 1 | 1 | 1 | 1 | 1 | 7 | Low |
| Golebiewska J [69] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Farr A [70] | 1 | 1 | - | 1 | 1 | 1 | 1 | 1 | 7 | Low |
| Papasotiriou M [23] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Vidal E [33] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Giullian JA [71] | 1 | 1 | - | 1 | - | 1 | 1 | 1 | 6 | Moderate |
| Dantas S [39] | 1 | - | 1 | 1 | - | 1 | 1 | 1 | 6 | Moderate |
| Chuang P [5] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Pellè G [72] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Memikoglu KO [73] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| ópez-Medrano F [74] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Safdar N [44] | 1 | - | 1 | 1 | 1 | 1 | 1 | 1 | 7 | Low |
| Wojciechowski D [10] | 1 | 1 | - | 1 | - | 1 | 1 | 1 | 6 | Moderate |
| Lee JR [12] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Espinar MJ [61] | - | 1 | - | 1 | 1 | 1 | 1 | 1 | 6 | Moderate |
| Bodro M [75] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Królicki T [76] | 1 | 1 | - | 1 | 1 | 1 | 1 | 1 | 7 | Low |
| Bodro M [45] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Britt NS [62] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Ariza-Heredia EJ [67] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Naik AS [77] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 | Low |
| Liu S [78] | - | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 | Low |
| Hazratullah E [63] | _ | 1 | 1 | 1 | _ | 1 | - | 1 | 5 | Moderate |
| Mansury D [79] | 1 | 1 | 1 | 1 | _ | 1 | 1 | 1 | 7 | Low |
Fig. 1.
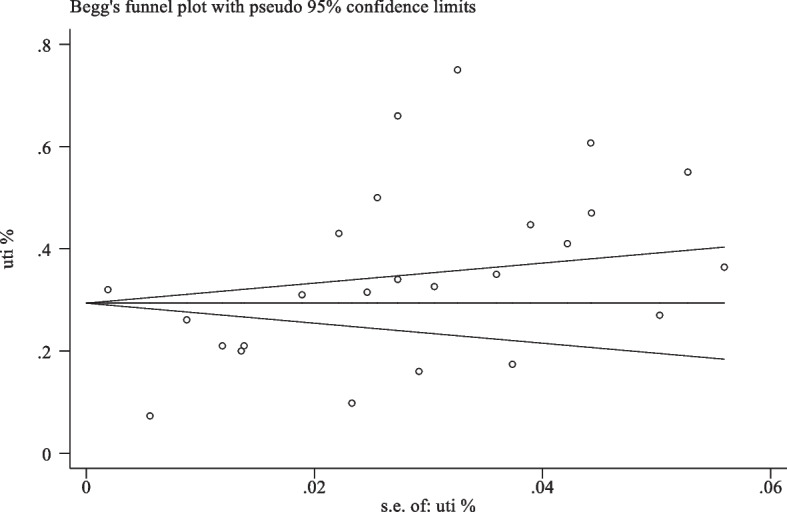
Publication bias test using Begg’s funnel plot test
Statistical analysis
The pooled prevalence of UTI in kidney recipients was calculated with a 95% confidence interval, and subgroup analysis was performed according to the geographical area of the studies and the type of antibiotic prophylaxis. The odds ratio (OR) with a 95% confidence interval for each risk factor was recorded or calculated when possible. Studies were pooled according to the sample size, mean, and standard deviation. Each study was weighted according to the inverse of its variance. The Q test and I2 index were tested for significance at the α error level of < 10% to investigate heterogeneity. In cases where the results of the studies were heterogeneous, they were analyzed using meta-analysis (random effects model). R and Stata 14 were used for data analysis. A random effects model calculated ORs and the corresponding 95% confidence intervals (CIs) for dichotomous outcomes.
Results
After removing duplicates and irrelevant studies, 205 studies were examined. The steps of study selection are shown in Fig. 2. Finally, 26 eligible papers published between 2005 and 2022 were included in this meta-analysis (Table 2) (Fig. 1). These studies were conducted on 72,600 participants, with an average age of 48.7 years. Moreover, 59.8% of the participants were men, and 40.2% were women. The follow-up periods in the included studies varied considerably, with the longest extended study period being 11 years and the shortest being three months.
Fig. 2.
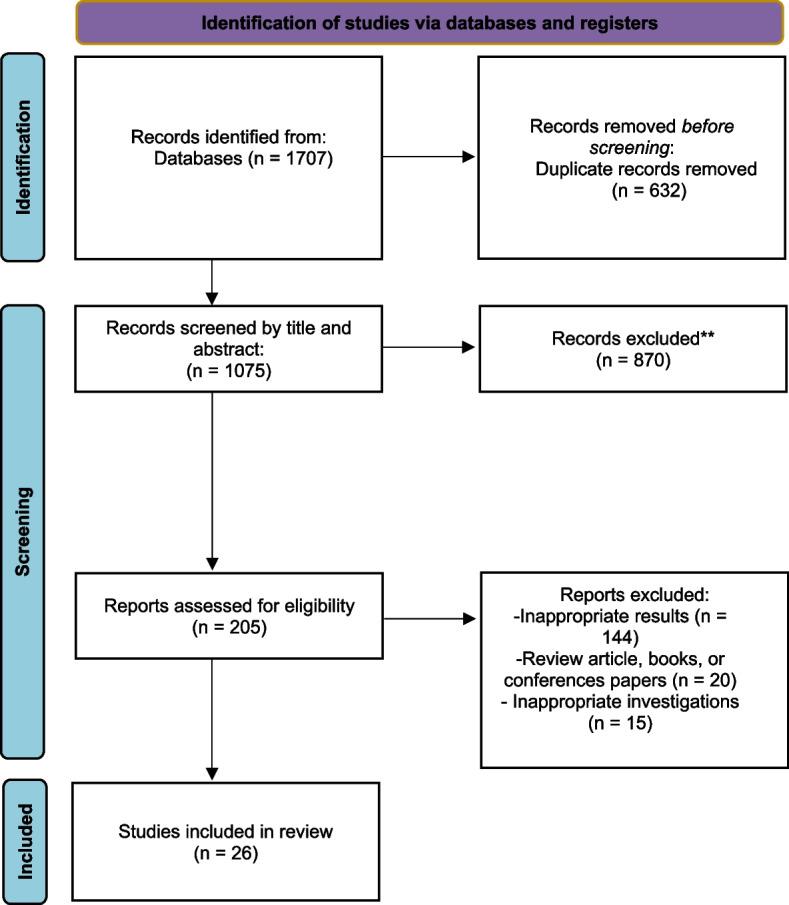
Flow diagram of studies identified in this study
Table 2.
Characteristics of the articles reviewed in this study
| AUTHOR Ref | Year | No. of participants | Country | Mean age | Male/female (n) | % UTI | Deceased donor/ living donor | Antibiotic prophylaxis | Study design | Risk factors investigated | Mean follow-up (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bonkat G [42] | 2012 | 78 | Switzerland | 56 | 51/27 | 27 | 50/28 | Sulfanamid | Cohort | Age, female sex, previous history of UTI | 24 |
| Sorto R [43] | 2010 | 176 | Mexico | 37 | 96/80 | 35 | 38/138 | B lactam | Cohort | Age, female sex, deceased donor, duration of catheter, diabetes, use of ureteral stent, abnormal anatomy of urinary tract, antibiotic prophylaxis | 48 |
| Golebiewska J [69] | 2011 | 89 | Poland | 48.1 | 52/37 | 55 | 88/1 | B lactam | Cohort | Age, female gender, previous history of UTI, acute rejection, use of ureteral stent | 12 |
| Farr A [70] | 2014 | 598 | Austria | 54 | 389/209 | 31 | 57/521 | Sulfanamid | Cohort | Age, female gender | 18 |
| Papasotiriou M [24] | 2011 | 122 | Greece | 44 | 75/47 | 60.7 | Sulfanamid | Cohort | Female gender, diabetes, acute rejection | 68 | |
| Vidal E [33] | 2012 | 2172 | Spain | 52 | 1381/671 | 7.3 | Sulfanamid | Cohort | Age, female sex, previous history of UTI, diabetes, acute rejection | 18 | |
| Giullian JA [71] | 2008 | 158 | USA | 47 | 109/49 | 16 | 67/76 | Sulfanamid | Cohort | Female gender, deceased donor, Diabetes, abnormal anatomy of the urinary tract, antibiotic prophylaxis | 36 |
| Dantas S [39] | 2006 | 163 | Brazil | 42.5 | 98/65 | 44.7 | 110/53 | Sulfanamid | Cohort | Deceased donor, duration of catheter | 24 |
| Chuang P [6] | 2005 | 500 | USA | 44 | 331/169 | 43 | 105/195 | B lactam | Cohort | Age, female gender, deceased donor | 42 |
| Pellè G [72] | 2007 | 177 | France | 46.5 | 117/60 | 75 | 153/24 | B lactam | Cohort | Female gender, previous history of UTI, acute rejection, | 22 |
| Memikoglu KO [73] | 2007 | 136 | Turkey | 32 | 88/48 | 41 | 33/103 | B lactam | Cohort | Female gender, use of ureteral stents | 38 |
| ópez-Medrano F [74] | 2014 | 163 | Spain | 44.8 | 107/56 | 9.8 | 140/244 | Cohort | Female gender | 26 | |
| Safdar N [44] | 2005 | 385 | USA | 47 | 166/218 | 50 | 607/141 | Cohort | Female gender, previous history of UTI, duration of catheter, diabetes, use of ureteral stent, abnormal anatomy of urinary tract, antibiotic prophylaxis | 96 | |
| Wojciechowski D [11] | 2013 | 236 | USA | 51.6 | 145/91 | 32.6 | 95/141 | Sulfanamid | Cohort | Age, female gender, deceased donor, use of ureteral stent | 12 |
| Espinar MJ [61] | 2015 | 98 | Portugal | 53.8 | 35/63 | case control | Previous history of UTI, diabetes, antibiotic prophylaxis | 9 | |||
| Bodro M [75] | 2015 | 867 | Spain | 60 | 20 | Sulfanamid | Cohort | Age, female gender | 90 | ||
| Bodro M [45] | 2015 | 867 | Spain | 60 | 520/347 | 21 | 662/205 | Sulfanamid | Cohort | Female gender, deceased donor, diabetes, acute rejection | 90 |
| Ariza-Heredia EJ [67] | 2014 | 301 | USA | 56.7 | 177/124 | 34 | 123/132 | B lactam | Cohort | Female gender, use of ureteral stents, abnormal anatomy of the urinary tract | 24 |
| Naik AS [77] | 2015 | 60,702 | USA | 52 | 36,725/23977 | 32 | 44,616/16086 | Cohort | Age, female gender, deceased donor, diabetes | 132 | |
| Liu S [78] | 2016 | 103 | China | 35.4 | 79/24 | 17.4 | B lactam | RCT | Age, female sex, use of ureteral stent | 48 | |
| Hazratullah E [63] | 2022 | 74 | Pakistan | 62/12 | 36.4 | Sulfanamid | Cohort | Female gender, previous history of UTI, diabetes, acute rejection, abnormal anatomy of the urinary tract | 3 | ||
| Hazratullah E [63] | 2022 | 74 | Pakistan | 62/12 | 36.4 | Sulfanamid | Cohort | ||||
| Mansury D [79] | 2018 | 356 | Iran | 206/150 | 31.5 | 241/115 | Cohort | Female gender, deceased donor, | 48 |
Prevalence of UTIs
The pooled prevalence of UTIs was 35% (95% CI, 30%-40%; P < 0.01) in the entire population (Fig. 3). The prevalence of UTIs varied in the reviewed studies. The lowest prevalence of UTIs was 7.3%, and the highest prevalence was 75%. In the subgroup analysis based on the studied geographical region, the prevalence of UTIs was 34% in America based on 11 studies, 37% in Europe based on ten studies, and 31% in Asia based on four studies. Moreover, in the subgroup analysis based on antibiotic prophylaxis, the prevalence of UTIs was 41% in patients who received beta-lactam after kidney transplantation based on nine papers, and 29% in patients who received sulfonamide based on 11 articles (Table 3).
Fig. 3.
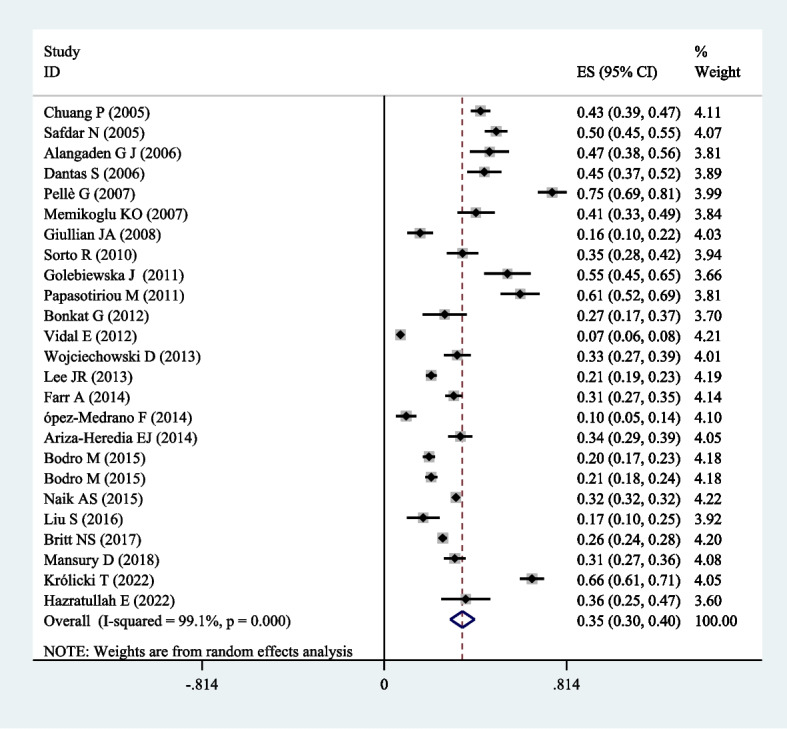
Forest plot of the prevalence of UTIs in renal transplant patients. The square represents the effect estimate of individual studies with their 95% confidence intervals with the size of squares proportional to the weight assigned to the study in the meta-analysis. In this chart, studies are stored in order of the year of publication and author’s names, based on a random effects model
Table 3.
The prevalence of UTIs in kidney transplant patients based on subgroup analysis of location and type of antibiotic
| Subgroup | Number of articles | UTI (% (95% CI) | |
|---|---|---|---|
| America | 11 | 34% (30% to 38%) | |
| Location | Europe | 10 | 37% (25% to 39%) |
| Asia | 4 | 31% (22% to 41%) | |
| Antibiotic | β-lactam | 9 | 41% (29% to 53%) |
| Sulfonamide | 11 | 29% (21% to 36%) |
Risk factors for UTIs in patients after kidney transplant
Twelve papers examined the association between the recipient's age and the occurrence of UTIs. The pooled OR for older age was 1.03 P = 0.11). The relationship between sex and UTIs was investigated in 23 papers. As shown in Table 4, the incidence of UTIs in women was significantly higher. The pooled OR for the female sex was 3.13 (P < 0.001). The relationship between a history of UTIs and UTIs post-transplant was discussed in eight papers. The pooled OR of a history of UTIs pre-transplantation was 1.31 ( P = 0.001). Pooled results from 11 papers demonstrated that the incidence of UTIs in patients who received a kidney from a deceased donor was 1.59 (P < 0.001) times higher than that of those who received a kidney from a living donor.
Table 4.
The pooled odds ratio for UTIs risk factors in kidney transplant patients
| Variable | Number of articles | Pooled odds ratio | P value |
|---|---|---|---|
| 95% Confidence interval (%) | |||
| Age | 12 | 1.03 (1 to 1.05) | 0.11 |
| Female sex | 23 | 3.13 (2.35 to 4.17) | 0 |
| previous UTI | 8 | 1.31 (1.05 to 1.63) | 0.001 |
| Deceased donor | 11 | 1.59 (1.23 to 2.35) | 0 |
| Duration of catheter | 4 | 3.03 (1.59 to 6.59) | 0 |
| Diabetes | 12 | 1.17 (0.97 to 1.41) | 0 |
| Acute rejection | 7 | 2.22 (1.45 to 3.4) | 0 |
| Ureteral stent | 10 | 1.54 (1.16 to 2.06) | 0 |
| Abnormal urinary | 5 | 2.87 (1.44 to 5.74) | 0 |
| anatomy | |||
| Hypertension | 3 | 1.6 (1.26 to 2.28) | 0.12 |
| Antibiotic prophylaxis | 6 | 1.67 (1.34 to 2.37) | 0.487 |
By comparing the data about the duration of catheterization and urinary infections from 4 papers, we concluded that the risk of developing a urinary infection in patients with a longer period of catheter use is higher; pooled OR was 3.03 (P < 0.001). Twelve papers investigated the association between diabetes and the occurrence of UTIs. Pooled OR results showed that the odds of developing a UTI in patients with diabetes compared to non-diabetic patients was 1.17 (P < 0.001). The association between aacute rejection process and UTI was investigated in 7 papers. The pooled OR was 2.22 (P < 0.001). We pooled data on ureteral stent use and UTIs from 10 papers and concluded that patients who used ureteral stents were more susceptible to UTIs; pooled OR was 1.45 (P < 0.001).
Five studies investigated the relationship between UTIs and abnormal anatomy of the urinary tract; a pooled OR of 2.87 (P < 0.001) was obtained. Three studies investigated the relationship between UTI and hypertension. The pooled OR for hypertension was 1.6 (P = 0.12). More statistical details are noted in Table 4.
Microbiology of UTIs:
The most common pathogens reported by urine culture in kidney recipients were Escherichia coli (39%), and Enterococcus spp. (16%), Klebsiella spp. (14%), Staphylococci spp. (12%), Enterobacter cloacae (8%), and Pseudomonas aeruginosa (6%) (Fig. 4).
Fig. 4.
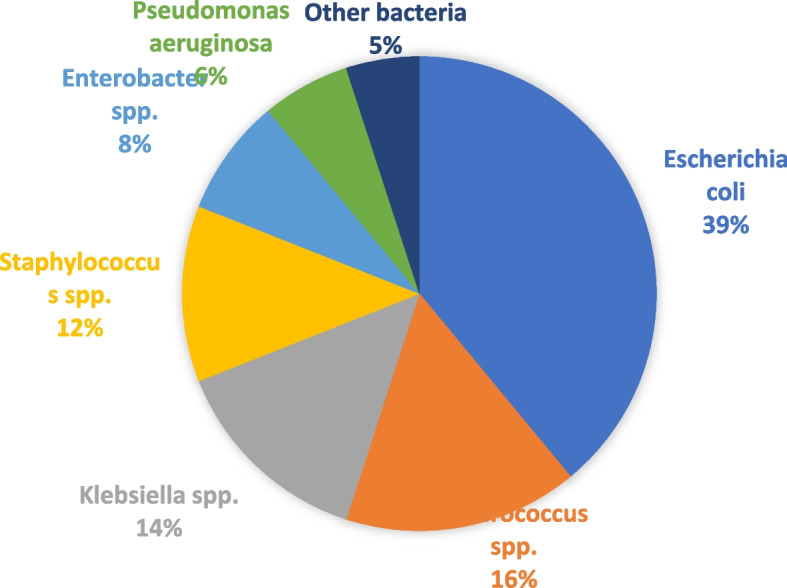
The most important bacteria causing UTIs in kidney transplant recipients
Discussion
UTIs are prevalent and serious infections after kidney transplantation [6, 26–28]. It has been reported that UTIs can be associated with increased complications and mortality [26, 6, 29] and, possibly, a decline in long-term transplant survival [5]. Studies have shown that the incidence of UTIs in kidney recipients is much higher than the rate observed in the general population [30]. Therefore, it is critical to treat and prevent UTIs in kidney recipients.
The present meta-analysis was conducted to identify and pool the findings of previous studies and meta-analyses investigating the prevalence and risk factors for UTIs in kidney recipients.
This meta-analysis collected data from 26 papers related to 72,600 kidney transplant recipients, in which risk factors for UTIs post-transplantation were examined. Due to the significant heterogeneity among studies, the random effects model was used in all stages. A key factor causing heterogeneity in the results of studies is the difference in procedures followed by different studies; the difference in follow-up time, the definition of UTI, and healthcare systems are among the factors that cause this heterogeneity.
Our study showed an overall prevalence of 35% for UTI in kidney recipients. Older age of the transplant recipient, female sex, previous history of UTI, deceased donor, prolonged use of a catheter, diabetes,acute rejection process, use of ureteral stent, abnormal urinary tract anatomy, and hypertension were associated with an increased risk of infection. E. coli was the most common bacterium causing UTI in patients after kidney transplants.
According to the studies conducted in different countries, the prevalence of UTI in patients after kidney transplant varies from 6 to 86% [24]. The explanation for this difference depends on several factors, including differences in surgical technique, the definition of UTI, immunosuppressive drugs, and treatment to prevent infection. Our study obtained an overall prevalence of 35% (30%-40%). In the meta-analysis by Wu et al., this rate was 38% [31]. Lo´pez-Medrano et al. [32] and Vidal et al. [33] reported a prevalence of less than 10% for UTIs. In contrast, Pellè et al. [34] and Papasotiriou et al. [24] showed a prevalence of about 70% for UTIs in kidney recipients. Factors including exposure to an intense immunosuppressive regimen, surgical trauma, long-term urinary tract catheterization, ureteral stents, and prolonged hospitalization can explain the higher percentage of infectious complications in these patients compared to the general population [4, 6].
Based on subgroup analysis, there was no significant difference in the prevalence of UTIs between Americans, Europeans (34% vs. 37%), and Americans and Asians (34% vs. 31%). Still, there was a significant difference between Europeans and Asians (37% vs. 31%). This difference can be caused by genetic differences and different individual characteristics in other countries of two continents. In the subgroup analysis based on antibiotic prophylaxis, the prevalence of UTIs in patients who used beta-lactam antibiotics was significantly higher than in those who used sulfonamide antibiotics (41% vs. 29%). The increase of antibiotic resistance among bacteria, including beta-lactamase-producing strains could cause this difference. A type of resistance occurs through the production of beta-lactamases and induces resistance to beta-lactam drugs. These bacteria have recently been discussed as emerging health problems worldwide [35, 36].
UTI is a common infection among both sexes, but due to physiological reasons, it is more common among women [37]. Several studies have shown that the female sex is a risk factor for UTIs after kidney transplantation [5, 6, 13, 38]. However, other studies have not found a significant relationship between increased urinary infection and the female sex [39, 40]. In the present study, a significant relationship between increased UTIs and the female sex was observed. Since UTIs and bacteriuria are generally more common in women than men due to the shorter urethra and the proximity of the urethral opening to the vagina and anus, this observation is justifiable.
Different studies have reported conflicting results about the relationship between recipients' age and the occurrence of UTIs. Some studies reported no association between the age of recipients and the occurrence of UTI [23, 39, 41]. In contrast, others have reported the recipients' old age as a risk factor for UTIs post-transplantation [33, 42, 43]. Our study showed that age is a weak risk factor in kidney transplant recipients. Factors such as increased incidence of benign prostatic hypertrophy, bladder atrophy, impaired mobility, impaired immune system, and poor personal hygiene are among the reasons for the higher risk of UTIs in the elderly compared to the young [24].
We found that using invasive devices such as urinary catheters and other stents was associated with an increased risk of UTI. This finding is consistent with several studies conducted in this field [5, 42–46], although some studies have presented different results [38, 47–49]. Since indwelling catheters and stents are placed during an invasive procedure, it can damage the urinary tract and, as a result, increase the possibility of urinary infection. Moreover, the urinary tract surgical process and technical errors that contaminate the catheter can increase the risk of infection [50]. Therefore, shortening the time or avoiding urethral catheterization, regular urine culture, and early diagnosis of UTIs are required to reduce the incidence of UTIs.
Conflicting results have been reported regarding acute rejection episodes and the occurrence of UTIs. Some studies have reported no association between acute rejection episodes and UTI incidence [23, 46, 51]. On the other hand, several studies have confirmed the relationship between the period of acute rejection and UTIs [52–54]. Similarly, our findings showed that the rate of UTIs rises in patients who had passed an acute rejection period. The treatment of acute rejection requires more intense immunosuppression, which leads to an increased risk of infectious complications post-transplantation; 60% of patients experience at least one infection during the first-year post-transplantation [55]. On the other hand, immunosuppressive treatments lead to the host's weak inflammatory response against bacteria and increase the risk of infection-related complications. When bacteria invade the urinary tract, certain cytokines, including tumor necrosis factor and interleukin 1, 6, and 8, are activated both locally and systemically [52].
Our results showed that UTIs were more common in kidney recipients from deceased donors than living donors. Several studies have reported similar results [52, 56, 57]. According to one study, the prevalence of UTI in patients who received a transplant from a deceased donor and those who received a kidney from a living donor was 70% and 28%, respectively [58]. On the other hand, in a study, a higher prevalence of UTI was reported in recipients of kidneys from living donors [41]. One of the reasons why UTI is more common in recipients of kidneys from deceased donors can be an asymptomatic infection in the kidney donor, and the occurrence of these infections due to the use of immunosuppressive drugs in the recipients while living donors are tested for disease before donation [30, 59]. Furthermore, patients receiving kidneys from deceased donors probably needed more immunosuppressive treatment compared to those receiving kidneys from living donors [32].
Underlying diseases such as diabetes and hypertension are risk factors for UTI in patients after kidney transplants [65]. Kidney recipients with diabetes are more exposed to bacterial and fungal infections [66]. In our study, diabetes and hypertension were associated with increased UTIs risk in kidney recipients. Diabetes can affect the anatomical and functional features of the urinary system and lead to abnormalities in this system. Such abnormalities are increased following the use of medical devices such as urinary catheters and, in turn, extend the infection [37]. Therefore, regular urine cultures and early diagnosis of urinary infections in these patients are necessary.
Our results showed that anatomical abnormalities of the urinary tract are one of the risk factors for UTIs in kidney recipients. Several studies have reported similar findings [6, 46]. In the study by Ariza-Heredia et al., the most common abnormalities leading to UTIs were benign prostatic hypertrophy, ureteral obstruction, bladder dysfunction, urinary incontinence, and vesicoureteral reflux, respectively [67].
In individuals with and without kidney transplants, the microorganisms that cause UTIs are similar. Over 70% of UTIs are caused by infections with gram-negative bacteria [42]. According to various research, E. coli has a frequency ranging from 21 to 73% in the general population and kidney transplants, making it the most prevalent UTI pathogen [24]. Pseudomonas, Staphylococcus, and Enterobacter species are the most common agents causing UTI within 3 to 5 weeks after transplantation, while E. coli and Enterococcus species mainly cause infection within 6 to 12 weeks post-transplantation [68]. In the present study, E. coli was the most common cause of UTI after kidney transplant in patients, followed by Enterococcus, Klebsiella, Staphylococcus, and Enterobacter species.
There are several limitations to this meta-analysis. The first limitation was the criteria based on which UTIs diagnosis is made. The diagnosis of UTIs is mainly based on positive urine culture, and some doctors argue that these patients only have bacteriuria and do not necessarily have UTIs. Second, despite our efforts to present all relevant variables, there is a possibility that not all UTIs risk factors were included in the results due to the presence of diverse variables and the limitations in the original data. For instance, although we aimed to pool the odds ratios for antibiotic prophylaxis as a risk factor, the wide array of variables prevented us from doing so. Third, there is always a risk of publication bias; the quantity of included papers and variations in sample sizes may had an impact on publication bias.
Conclusion
Kidney transplantation is a complex and important surgical procedure. Post-operative care, follow-up, and diagnosis and management of possible post-transplantation problems are of great significance. Treatment of infection as one of the most essential postoperative complications can reduce the mortality, complications, and costs imposed on patients. This meta-analysis revealed that UTIs are a significant problem in kidney recipients. Factors such as female sex, old age, history of UTIs, deceased donor, long-term use of an indwelling catheter, diabetes, acute rejection process, use of ureteral stent, abnormal urinary tract anatomy, and hypertensionwere related to an increased risk of UTIs in kidney recipients. To investigate the factors affecting UTIs in kidney recipients and to assess the impact of more recent immunosuppressive medications and prophylactic/therapeutic antimicrobial agents on the pattern of post-transplant infectious complications, prospective trials with a large sample size and a longer follow-up period would be beneficial.
Acknowledgements
Not applicable.
Authors’ contributions
M.H. and S.M. conceptualized the review and wrote the first draft. A.P. and M.H. supervised, reviewed, and improved the paper. A.P. and F.S. provided the figures and revised the paper. All authors finally approved this final version. All authors contributed to the article and approved the submitted version. All authors have read and agreed to the published version of the manuscript.
Funding
Not applicable.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Eggers pw. Effect of renal transplantation on the medical end- stage renal disease program. NEJ Med. 1988; 318223.
- 2.Fishman JA, Rubin RH. Infection in organ-transplant recipients. N Engl J Med. 1998;338:1741–1751. doi: 10.1056/NEJM199806113382407. [DOI] [PubMed] [Google Scholar]
- 3.Bretan PN, Malone MJ. Renal transplantation. In: Tanagho EA, McAninch JW, editors. Smith's General Urology. 15. New York: Lange Medical/McGraw-Hill; 2000. pp. 614–627. [Google Scholar]
- 4.Maraha B, Bonten H, van Hooff H, Fiolet H, Buiting AG, Stobberingh EE. Infectious complications and antibiotic use in renal transplant recipients during a 1-year follow-up. ClinMicrobiol Infect. 2001;7:619–625. doi: 10.1046/j.1198-743x.2001.00329.x. [DOI] [PubMed] [Google Scholar]
- 5.Alangaden GJ, Thyagarajan R, Gruber SA, Morawski K, Garnick J, El-Amm JM. Infectious complications after kidney transplantation: current epidemiology and associated risk factors. Clin Transplant. 2006;20:401–409. doi: 10.1111/j.1399-0012.2006.00519.x. [DOI] [PubMed] [Google Scholar]
- 6.Chuang P, Parikh CR, Langone A. Urinary tract infections after renal transplantation: a retrospective review at two US transplant centers. Clin Transplant. 2005;19:230–235. doi: 10.1111/j.1399-0012.2005.00327.x. [DOI] [PubMed] [Google Scholar]
- 7.Rubin RH. Infectious disease complications of renal transplantation. Kidney Int. 1993;44:221–236. doi: 10.1038/ki.1993.234. [DOI] [PubMed] [Google Scholar]
- 8.Jamil B, Nicholls K, Becker GJ, Walker RG. Impact of acute rejection therapy on infections and malignancies in renal transplant recipients. Transplantation. 1999;68:1597–1603. doi: 10.1097/00007890-199911270-00027. [DOI] [PubMed] [Google Scholar]
- 9.Charfeddine K, Zahden S, Kharrat M. Infectious complications in kidney transplant recipients. Transplant Proc. 2005;37:2823. doi: 10.1016/j.transproceed.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Joseph R. Masci, Gary P. Wormser. Mandell, Douglas, Bennett's. principles and practice of infectious Diseases. Sixth ed. Philudelphia, Pennsylvania: Elsevir; 2005: 3503.
- 11.Wojciechowski D, Chandran S. Effect of ciprofloxacin combined with sulfamethoxazole-trimethoprim prophylaxis on the incidence of urinary tract infections after kidney transplantation. Transplantation. 2013;96:400–405. doi: 10.1097/TP.0b013e3182962cab. [DOI] [PubMed] [Google Scholar]
- 12.Karuthu S, Blumberg EA. Common infections in kidney transplant recipients. Clin J Am Soc Nephrol. 2012;7:2058–2070. doi: 10.2215/CJN.04410512. [DOI] [PubMed] [Google Scholar]
- 13.Lee JR, Bang H, Dadhania D. Independent risk factors for urinary tract infection and for subsequent bacteremia or acute cellular rejection: A single-center report of 1166 kidney allograft recipients. Transplantation. 2013;96:732–738. doi: 10.1097/TP.0b013e3182a04997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shin DH, Kim EJ, Lee S, Kim SJ, Oh J. Early-onset graft pyelonephritis is predictive of long-term outcome of renal allografts. Tohoku J Exper Med. 2015;236:175–183. doi: 10.1620/tjem.236.175. [DOI] [PubMed] [Google Scholar]
- 15.Abbott KC, Oliver JD, Hypolite I, Lepler LL, Kirk AD, Ko CW. Hospitalizations for bacterial septicemia after renal transplantation in the United States. Am J Nephrol. 2001;21:120–127. doi: 10.1159/000046234. [DOI] [PubMed] [Google Scholar]
- 16.Brayman KL, Stephanian E, Matas AJ, Schmidt W, Payne WD, Sutherland DE. Analysis of infectious complications occurring after solid-organ transplantation. Arch Surg. 1992;127:38–47. doi: 10.1001/archsurg.1992.01420010044007. [DOI] [PubMed] [Google Scholar]
- 17.Ramsey D E, Finch W T. Birteh A G. Urinary tract infection in kidney transplant recipients. Arch Surg. 1979;114: 1022–5. [DOI] [PubMed]
- 18.Rao KV, Andersen RC. Long-term results and complications in renal transplant recipients. Observations in the second decade Transplantation. 1988;45:45. doi: 10.1097/00007890-198801000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Grekas D, Thanos V, Dioudis C. Treatment of urinary tract infections with ciprofloxacin after renal transplantation. Int J Clin Pharmacol Ther Toxicol. 1993;31:309. [PubMed] [Google Scholar]
- 20.Gargah T, Labessi A, Ounissi M, Derouiche A, Chokri Z, Trabelsi M. Early infections in children following renal transplantation. Tunis Med. 2011;89:26–30. [PubMed] [Google Scholar]
- 21.Viale P, Scudeller L. Infectious complications after renal transplantation. G Ital Nefrol. 2004;26:48–52. [PubMed] [Google Scholar]
- 22.Kawecki D, Kwiatkowski A, Michalak G, Sawicka- Grzelak A, Mlynarczyk A, Sokol-Leszczynska B. Etiologic agents of bacteremia in the early period after simultaneous pancreas-kidney transplantation. Transplant Proc. 2009;41:3151–3153. doi: 10.1016/j.transproceed.2009.07.064. [DOI] [PubMed] [Google Scholar]
- 23.Takai K, Tollemar J, Wilczek HE, Groth CG. Urinary tract infections following renal transplantation. Clin Transplant. 1998;12:19–23. [PubMed] [Google Scholar]
- 24.Papasotiriou M, Savvidaki E, Kalliakmani P, Papachristou E, Marangos M, Fokaefs E. Predisposing factors to the development of urinary tract infections in renal transplant recipients and the impact on the long-term graft function. Ren Fail. 2011;33:405–410. doi: 10.3109/0886022X.2011.568137. [DOI] [PubMed] [Google Scholar]
- 25.Miranda C, Carazo C, Bañón R, Mendoza J, Montes A, de la Rosa M. Mycoplasma hominis infection in three renal transplant patients. Diagn Microbiol Infect Dis. 1990;13:329–331. doi: 10.1016/0732-8893(90)90025-Q. [DOI] [PubMed] [Google Scholar]
- 26.Abbott KC, Swanson SJ, Richter ER. Late urinary tract infection after renal transplantation in the United States. Am J Kidney Dis. 2004;44:353. doi: 10.1053/j.ajkd.2004.04.040. [DOI] [PubMed] [Google Scholar]
- 27.Di Cocco P, Orlando G, Mazzotta C, et al. Incidence of urinary tract infections caused by germs resistant to antibiotics commonly used after renal transplantation. Transplant Proc. 2008;40:1881. doi: 10.1016/j.transproceed.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 28.Lyerova L, Viklicky O, Nemcova D. The incidence of infectious diseases after renal transplantation: a single-centre experience. Int J Antimicrob Agents. 2008;31:S58. doi: 10.1016/j.ijantimicag.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 29.Abbott KC, Oliver JD, Hypolite I. Hospitalizations for bacterial septicemia after renal transplantation in the United States. Am J Nephrol. 2001;21:120. doi: 10.1159/000046234. [DOI] [PubMed] [Google Scholar]
- 30.Memikoğlu KO, Keven K, Sengul S, Soypacaci Z, Erturk S, Erbay B. Urinary tract infections following renal transplantation: a single-center experience. Transplant Proc. 2007;39:3131–3134. doi: 10.1016/j.transproceed.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Wu X, Dong Y, Liu Y, Li Y. The prevalence and predictive factors of urinary tract infection in patients undergoing renal transplantation: A meta-analysis. Am J Infect Control. 2016;44:1261–1268. doi: 10.1016/j.ajic.2016.04.222. [DOI] [PubMed] [Google Scholar]
- 32.Lopez-Medrano F, Garcia-Bravo M, Morales JM. Urinary tract infection due to Corynebacterium urealyticum in kidney transplant recipients: an underdiagnosed etiology for obstructive uropathy and graft dysfunction-results of a prospective cohort study. Clin Infect Dis. 2008;46:825–830. doi: 10.1086/528713. [DOI] [PubMed] [Google Scholar]
- 33.Vidal E, Torre-Cisneros J, Blanes M. Bacterial urinary tract infection after solid organ transplantation in the RESITRA cohort. Transpl Infect Dis. 2012;14:595–603. doi: 10.1111/j.1399-3062.2012.00744.x. [DOI] [PubMed] [Google Scholar]
- 34.Pelle G, Vimont S, Levy PP, Hertig A, Ouali N, Chassin C. Acute yelonephritis represents a risk factor impairing long-term kidney graft function. Am J Transplant. 2007;7:899–907. doi: 10.1111/j.1600-6143.2006.01700.x. [DOI] [PubMed] [Google Scholar]
- 35.Alevizakos M, Nasioudis D, Mylonakis E, Diseases DI. Urinary tract infections due to ESBL-producing Enterobacteriaceae in renal transplant recipients: A systematic review and meta-analysis. Transpl Infect Dis. 2017;19:12759. doi: 10.1111/tid.12759. [DOI] [PubMed] [Google Scholar]
- 36.Hossein Zadegan H, Hassani A, Azadpour M, Suleiman NS. Identification of beta-lactamase-producing gram-negative bacilli of a wide range of bacteria isolated from clinical cases. Laboratory Science Journal. 2007;2:21–25. [Google Scholar]
- 37.Vasudevan R. Urinary tract infection: an overview of the infection and the associated risk factors. Microbiol Exp. 2014;1:42–54. [Google Scholar]
- 38.Osman Y, li-El-Dein B, Shokeir AA, Kamal M, El-Din AB. Routine insertion of ureteral stent in live-donor renal transplantation: is it worthwhile? Urology. 2005; 65: 867–71. [DOI] [PubMed]
- 39.Dantas SR, Kuboyama RH, Mazzali M, Moretti ML. Nosocomial infections in renal transplant patients: risk factors and treatment implications associated with urinary tract and surgical site infections. J Hosp Infect. 2006;63:117–123. doi: 10.1016/j.jhin.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 40.Pourmand G, Salem S, Mehrsai A, Taherimahmoudi M, Ebrahimi R, Pourmand MR. Infectious complications after kidney transplantation: a single-center experience. Transpl Infect Dis. 2007;9:302–309. doi: 10.1111/j.1399-3062.2007.00229.x. [DOI] [PubMed] [Google Scholar]
- 41.Sqalli TH, Laboudi A, Arrayhani M. Urinary tract infections in renal allograft recipients from living related donors. Saudi J Kidney Dis Transpl. 2008;19:551–553. [PubMed] [Google Scholar]
- 42.Bonkat G, Rieken M, Siegel FP, Frei R, Steiger J, Groschl I. Microbial ureteral stent colonization in renal transplant recipients: frequency and influence on the short-time functional outcome. Transpl Infect Dis. 2012;14:57–63. doi: 10.1111/j.1399-3062.2011.00671.x. [DOI] [PubMed] [Google Scholar]
- 43.Sorto R, Irizar SS, Delgadillo G, Alberu J, Correa-Rotter R, Morales-Buenrostro LE. Risk factors for urinary tract infections during the first year after kidney transplantation. Transplant Proc. 2010;42:280–281. doi: 10.1016/j.transproceed.2009.11.029. [DOI] [PubMed] [Google Scholar]
- 44.Safdar N, SlatteryWR, Knasinski V. Predictors and outcomes of candiduria in renal transplant recipients. Clin Infect Dis. 2005; 40: 1413–21. [DOI] [PubMed]
- 45.Bodro M, Sanclemente G, Lipperheide I, Allali M. Impact of Urinary tract infections in short-term kidney graft outcome. Clin Microbiol Infect. 2015;21:1104.e8. doi: 10.1016/j.cmi.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 46.Tavakoli A, Surange RS, Pearson RC, Parrott NR, Augustine T, Riad HN. Impact of stents on urological complications and health care expenditure in renal transplant recipients: results of a prospective, randomized clinical trial. J Urol. 2007;177:2260–2264. doi: 10.1016/j.juro.2007.01.152. [DOI] [PubMed] [Google Scholar]
- 47.Mathe Z, Treckmann JW, Heuer M, Zeiger A, Sauerland S, Witzke O. Stented ureterovesical anastomosis in renal transplantation: does it influence the rate of urinary tract infections? Eur J Med Res. 2010;15:297. doi: 10.1186/2047-783X-15-7-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dominguez J, Clase CM, Mahalati K, MacDonald AS, McAlister VC, Belitsky P, et al. Is routine ureteric stenting needed in kidney transplantation? A randomized trial Transplantation. 2000;70:597–601. doi: 10.1097/00007890-200008270-00011. [DOI] [PubMed] [Google Scholar]
- 49.Giakoustidis G, Diplaris K, Antoniadis N, Papagianis A, Ouzounidis N, Fouzas I, et al. Impact of double-J ureteric stent in kidney transplantation: single-centre experience. Transplant Proc. 2008;40:3173–3175. doi: 10.1016/j.transproceed.2008.08.064. [DOI] [PubMed] [Google Scholar]
- 50.Tolkoff-Rubin NE, Rubin RH. Urinary tract infection in the immunocompromised host: lessons from kidney transplantation and the AIDS epidemic. Infect Dis Clin North Am. 1997;11:707–717. doi: 10.1016/S0891-5520(05)70381-0. [DOI] [PubMed] [Google Scholar]
- 51.Schmaldienst S, Horl WH. Bacterial infections after renal transplantation. Nephron. 1997;75:140–153. doi: 10.1159/000189523. [DOI] [PubMed] [Google Scholar]
- 52.Kamath NS, John GT, Neelakantan N, Kirubakaran MG, Jacob CK. Acute graft pyelonephritis following renal transplantation. Transpl Infect Dis. 2006;8:140–147. doi: 10.1111/j.1399-3062.2006.00148.x. [DOI] [PubMed] [Google Scholar]
- 53.Rabkin DG, Stifelman MD, Birkhoff J, Richardson KA, Cohen D, Nowygrod R. Early catheter removal decreases incidence of urinary tract infections in renal transplant recipient. Transplant Proc. 1998;30:4314–4316. doi: 10.1016/S0041-1345(98)01423-7. [DOI] [PubMed] [Google Scholar]
- 54.Gołe˛biewska J, De˛bska-S´ lizien´ A, Komarnicka J, Samet A, Rutkowski B. Urinary tract infections in renal transplant recipients. Transplant Proc. 2011; 43:2985- 90. [DOI] [PubMed]
- 55.Veroux M, Giuffrida G, Corona D, Gagliano M, Scriffignano V, Vizcarra D. Infective complications in renal allograft recipients: epidemiology and outcome. Transplant Proc. 2008;40:1873–1876. doi: 10.1016/j.transproceed.2008.05.065. [DOI] [PubMed] [Google Scholar]
- 56.Glazier DB, Jacobs MG, Lyman NW, Whang MI, Manor E, Mulgaonkar SP. Urinary tract infection associated with ureteral stents in renal transplantation. Can J Urol. 1998;5:462–466. [PubMed] [Google Scholar]
- 57.Goya N, Tanabe K, Iguchi Y, et al. Prevalence of urinary tract infection duringoutpatient follow-up after renal transplantation. Infection. 1997;25:101–105. doi: 10.1007/BF02113586. [DOI] [PubMed] [Google Scholar]
- 58.Rivera-Sanchez R, Delgado-Ochoa D, Flores-Paz RR, et al. Prospective study of urinary tract infection surveillance after kidney transplantation. BMC Infect Dis. 2010;10:245. doi: 10.1186/1471-2334-10-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Midtvedt K, Hartmann A, Midtvedt T, Brekke IB. Routine perioperative antibiotic prophylaxis in renal transplantation. Nephrol Dial. 1998;13:1637–1641. doi: 10.1093/ndt/13.7.1637. [DOI] [PubMed] [Google Scholar]
- 60.Munoz P. Management of urinary tract infection and Lymphocele in renal transplant recipients. Clin infect Dis. 2001;33:53–57. doi: 10.1086/320905. [DOI] [PubMed] [Google Scholar]
- 61.Espinar MJ, Miranda IM, osta-de-Oliveira S, Rocha R. Urinary Tract Infections in Kidney Transplant Patients Due to Escherichia coli and Klebsiella pneumoniae-Producing Extended-Spectrum β-Lactamases: Risk Factors and Molecular Epidemiology. PLOS ONE. 2015; 10: e0134737. [DOI] [PMC free article] [PubMed]
- 62.Britt N, Hagopian JC, Brennan DB. Effects of recurrent urinary tract infections on graft and patient outcomes after kidney transplantation. Nephrol Dial Transplant. 2017;32:1758–1766. doi: 10.1093/ndt/gfx237. [DOI] [PubMed] [Google Scholar]
- 63.Ullah H, Khan N, Malik A, Raman AU. Frequency of urinary tract infections in renal transplant recipients with common bacteria and its sensitivity. Pak-Euro J Med Life Sci. 2022;5:223–228. doi: 10.31580/pjmls.v5i2.2552. [DOI] [Google Scholar]
- 64.Kasiske BL, Zeier MG, Chapman GR. KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney Int. 2010;77:299–311. doi: 10.1038/ki.2009.377. [DOI] [PubMed] [Google Scholar]
- 65.Hewitt IK, Pennesi M, Morello W. Antibiotic Prophylaxis for Urinary Tract Infection-Related Renal Scarring: A Systematic Review. Pediatrics. 2017;139:e20163145. doi: 10.1542/peds.2016-3145. [DOI] [PubMed] [Google Scholar]
- 66.Gaston RS, Basadonna G, Cosio FG, Davis CL, Kasiske BL, Larsen J. Transplantation in the diabetic patient with advanced chronic kidney disease: a task force report. Am J Kidney Dis. 2004;44:529–542. doi: 10.1016/S0272-6386(04)00821-2. [DOI] [PubMed] [Google Scholar]
- 67.Ariza-Heredia EJ, Beam EN, Lesnick TG, Cosio FG. Impact of urinary tract infection on allograft function after kidney transplantation. Clin Transplant. 2014;28:683–690. doi: 10.1111/ctr.12366. [DOI] [PubMed] [Google Scholar]
- 68.Saemann M, Horl WH. Urinary tract infection in renal transplant recipients. Eur J Clin Invest. 2008;38:58–65. doi: 10.1111/j.1365-2362.2008.02014.x. [DOI] [PubMed] [Google Scholar]
- 69.Gołe˛biewska J, De˛bska-S´ lizien´ A, Komarnicka J, Samet A, Rutkowski B. Urinary tract infections in renal transplant recipients. Transplant Proc. 2011; 43:2985- 90. [DOI] [PubMed]
- 70.Farr A, Gyori G, Muhlbacher F, Husslein P, Bohmig GA, Margreiter M. Gender has no influence on VUR rates after renal transplantation. Transpl Int. 2014;27:1152–1158. doi: 10.1111/tri.12397. [DOI] [PubMed] [Google Scholar]
- 71.Giullian JA, Cavanaugh K, Schaefer H. Lower risk of urinary tract infection with low-dose trimethoprim/sulfamethoxazole compared to dapsone prophylaxis in older renal transplant patients on a rapid steroid-withdrawal immunosuppression regimen. Clin Transplant. 2010;24:636–642. doi: 10.1111/j.1399-0012.2009.01129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pelle G, Vimont S, Levy PP, Hertig A, Ouali N, Chassin C, et al. Acute yelonephritis represents a risk factor impairing long-term kidney graft function. Am J Transplant. 2007;7:899–907. doi: 10.1111/j.1600-6143.2006.01700.x. [DOI] [PubMed] [Google Scholar]
- 73.Memikoğlu KO, Keven K, Sengul S, Soypacaci Z, Erturk S, Erbay B. Urinary tract infections following renal transplantation: a single-center experience. Transplant Proc. 2007;39:3131–3134. doi: 10.1016/j.transproceed.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 74.Lopez-Medrano F, Garcia-Bravo M, Morales JM, et al. Urinary tract infection due to Corynebacterium urealyticum in kidney transplant recipients: an underdiagnosed etiology for obstructive uropathy and graft dysfunction-results of a prospective cohort study. Clin Infect Dis. 2008;46:825–830. doi: 10.1086/528713. [DOI] [PubMed] [Google Scholar]
- 75.Bodro M, Sanclemente G, Lipperheide I. Impact of Antibiotic Resistance on the Development of Recurrent and Relapsing Symptomatic Urinary Tract Infection in Kidney Recipients. Am J Transplant. 2015;15:1021–1027. doi: 10.1111/ajt.13075. [DOI] [PubMed] [Google Scholar]
- 76.Królicki T, Bardowska K, Kudla T, Królicka A. Acute kidney injury secondary to urinary tract infection in kidney transplant recipients. Sci Rep. 2022;12:10858. doi: 10.1038/s41598-022-15035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Naik A, Dharnidharka VR. Schnitzler MA, Brennan DB. Clinical and economic consequences of first-year urinary tract infections, sepsis, and pneumonia in contemporary kidney transplantation practice. Transplant International. 2016; 29: 241–52. [DOI] [PMC free article] [PubMed]
- 78.Liu S, Luo G, Sun B, Lu J, Zu Q. Early Removal of Double-J Stents Decreases Urinary Tract Infections in Living Donor Renal Transplantation: A Prospective, Randomized Clinical Trial. Transplantation Proceedings. 2017; 49: 297e302. [DOI] [PubMed]
- 79.Mansury D, Khaledi A, Ghazvini K, Ghorban SM. Study of Bacterial Infections Among Patients Receiving Kidney Transplant in Mashhad. Iran Experimental and Clinical Transplantation. 2018;3:282–286. doi: 10.6002/ect.2016.0311. [DOI] [PubMed] [Google Scholar]
- 80.Simsek C, Karatas M, Tatar E, Tercan IC, TasliAlkan F, Uslu A. Acute Allograft Pyelonephritis: Vague Symptoms, Indeterminate Laboratory Results, and the Necessity of Indication Biopsy. Exp Clin Transplant. 2022;20(Suppl 1):117–124. doi: 10.6002/ect.MESOT2021.P51. [DOI] [PubMed] [Google Scholar]
- 81.Pacaud M, Colas L, Kerleau C, Le Borgne F, Giral M, Brouard S, Dantal J. Impact of Late and Recurrent Acute Graft Pyelonephritis on Long-Term Kidney Graft Outcomes. Front Immunol. 2022 Mar 2;13:824425. doi: 10.3389/fimmu.2022.824425. PMID: 35418982; PMCID: PMC8998071. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.


