Abstract
Background:
Nursing students are at higher risk for depression, suicide, and other mental health concerns as compared to the general college student population. Moral distress and other ethical issues may be a significant source of psychological harm within nursing student experiences and warrants further attention.
Purpose:
The purpose of this study was to understand the mediating effect of depression on the relationship between moral distress and suicide risk among undergraduate nursing students.
Methods:
This cross-sectional analysis was derived from a larger sequential mixed methods study. The first phase was an online survey completed by a national sample of N = 679 nursing students in the United States.
Findings:
The relationship between moral distress and suicide risk was fully mediated by depression and statistically significant at the alpha = 0.05 level.
Conclusion:
All three psychological variables (depression, moral distress, suicide risk) impact nursing students and require innovative solutions within nursing and educational programs.
Keywords: Moral distress, Depression, Suicide risk, Nursing students, Mental health
Suicide rates are steadily increasing across the youth of America (CDC, 2022) with suicide deaths the second leading cause of death for college-age youth (NIMH, 2022). Nursing students are no exception; with suicide rates steadily rising for women—the gender majority in the profession (CDC, 2022). Depressive symptomology is often a contributor for suicide risk (APA, 2013), but other factors, such as environmental stressors, may also contribute to this risk. Nursing students (as compared to other college-age youth) may experience morally distressing encounters in their undergraduate nursing programs, which may lead to negative psychological or emotional sequalae (Ulrich & Grady, 2018). What is unclear, however, is whether nursing students who experience moral distress in their undergraduate programs are at risk for depression and suicide risk. The purpose of this study is to examine the mediating effect of depression on the relationship between moral distress and suicide risk among undergraduate nursing students.
Background
Suicide is the second leading cause of death for 15- to 34-year-olds in the United States (NIMH, 2022). Youth suicide rates have steadily increased from 2000 to 2018 (CDC, 2022) with 5,954 suicide deaths (15–24 age group) and 8,059 suicide deaths (25–34 age group) in 2019 (NIMH, 2022). For females aged 15 to 24, rates increased 87% from 2007 through 2020 (CDC, 2022), and the leading means of suicide for females in 2020 was firearms-related, a change from previous years (CDC, 2022). On college campuses, studies suggest 8% to 18% of students think about suicide, and 1% to 11% of students report a lifetime suicide attempt (Macrynikola et al., 2018). These statistics are startling, especially when we consider the additional impact of the Covid-19 pandemic in recent years.
For undergraduate college students, nursing students may be at higher risk for depression (Chernomas & Shapiro, 2013; Xu et al., 2014), suicide (Aradilla-Herrero et al., 2014; Leal & Santos, 2016), and other mental health concerns, such as anxiety and sleep difficulties (Zhang et al., 2018) as compared to the general college student population. Nursing students often have demanding academic schedules, rigorous clinical and classroom expectations, and stressful encounters with life, death, and suffering, which may contribute to emotional or psychological distress and higher levels of mental health concerns. In fact, studies have reported depressive symptoms as high as 32.6% and 38.7% (Chen et al., 2015; Rezayat & Dehghan Nayeri, 2014).
Furthermore, moral distress may be a significant source of psychological and emotional harm within undergraduate nursing experiences (Krautscheid et al., 2017; Sasso et al., 2016; Wojtowicz et al., 2014). Moral distress is defined as “knowing or believing what the right thing to do is but feeling constrained to take the appropriate moral action” (Jameton, 2017). Nursing school often present students with ethical situations that can be traumatizing and fraught with conflict. This includes anxieties that may arise within hospitalized patients and their families, death and dying, distraught patients and families, emergency situations that require quick and clear thinking, and learning under stressful work conditions (Ulrich & Grady, 2018).
Previous literature suggests consequences of moral distress can include a range of emotional and psychological responses, such as frustration, sadness, guilt, anger, and hurt (Lachman, 2016). What is unclear, however, is whether nursing students experience clinical depression or depressive symptoms in the face of morally distressing encounters. Furthermore, it is unclear if moral distress contributes to suicide risk in the presence or absence of depressive symptomology. In preparing the next generation of nurses, it is imperative to understand their moral distress and the risks within academic and practice environments that may impact their mental health, including depression and suicide risk. To date, there have been no studies that explore the relationship between moral distress, depression, and suicide risk among nursing students. In response, the purpose of this study was to examine these relationships and to understand the mediating effect of depression on the relationship between moral distress and suicide risk among undergraduate nursing students.
This is significant to the nursing student population as the experiences of moral distress, depression, and suicide risk—in isolation—or the cumulative effect of all three—may impact student mental health and wellness and contribute to further suicide rates in the young adult (and female) population. This is also significant to the future of nursing. As students enter the profession as novice nurses, the experiences of moral distress may exacerbate and without adequate attention and awareness to the impact of moral distress on mental health and well-being, nurses may suffer and leave the profession... or suffer in silence (Rushton & Boston-Leary, 2022). This study hopes to bring awareness and greater recognition to the impact of moral distress and other mental health concerns, such as depression and suicide risk, which are prevalent in the young adult population. Furthermore, this study has the potential to lead to the implementation of evidence-based interventions that identify and treat depression and suicide risk in nursing students.
Methods
Design and Conceptual Model
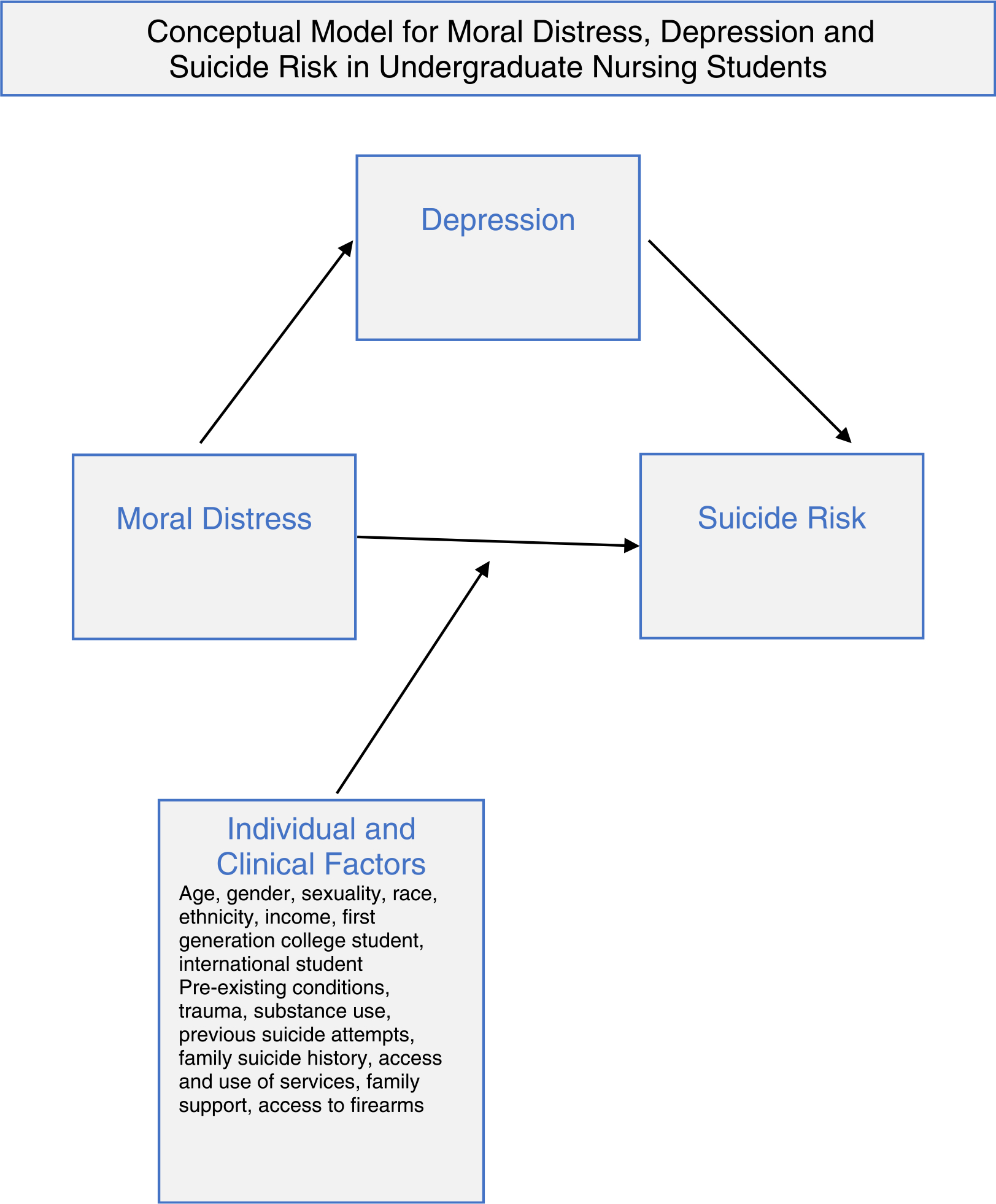
This cross-sectional analysis is derived from a larger sequential mixed methods study on moral distress, depression, and suicide risk among undergraduate nursing students. The primary aim of the study was to examine the mediating effect of depression on the relationship between moral distress and suicide risk in the presence of individual and clinical factors. The variable of depression was chosen as the mediator variable given its association with both moral distress and suicidality. Also, depression can easily be measured with highly reliable and valid instruments across multiple populations. The first phase of the study was a quantitative survey completed by a national sample of undergraduate nursing students in the United States. The conceptual model for this study (see Figure 1) is supported by bioethics literature on moral distress (Grady et al., 2008; Piers et al., 2011; Ulrich & Grady, 2018)—specifically related to the negative impact of moral distress on emotional and psychological health (including depressive symptomology). It is also supported by mental health literature that postulates a person’s suicide risk is influenced by individual and clinical factors and the extent of an individual’s risk exposure to depression is a significant predictor of suicide risk (Thapar et al., 2022).
Figure 1– Conceptual model for moral distress, depression, and suicide risk.
Sample and Setting
Participants in this study were undergraduate nursing students from the United States. The researchers partnered with the National Student Nurses Association (NSNA) to recruit a purposive sample of nursing students (NSNA, 2022). Eligible nursing students were: (a) at least 18 years old, (b) enrolled in an undergraduate nursing program at a college or university, (c) at the junior or senior level (or equivalent for those in accelerated or part-time programs) or completed at least one nursing clinical rotation, and (d) willing to provide informed consent. Survey responses were obtained from November 2018 to April 2019 with a final sample of N = 679 nursing students. The final sample was derived from over 800 survey responses (n = 802); duplicates and respondents with completely blank responses (n = 123) were excluded from the analysis. Partial and full survey responses were included, resulting in a study sample of 679 participants. Informed consent was implied when students agreed to participate in the online survey. All participants received a $10 Visa Gift Card for their time and effort in the study.
Data Collection Procedures
Survey responses were gathered using REDCap (Research Electronic Data Capture), a secure, web-based application designed to support data capture for research (Harris et al., 2009). The REDCap tool provides a secure way for participants to complete survey information while protecting their privacy and confidentiality. Only approved members of the project have access to the survey responses. Furthermore, all participants received their own unique participant ID to protect their anonymity. In the electronic survey, participants completed the demographic questionnaire (with questions eliciting information on individual and clinical factors), the Moral Distress Thermometer (MDT), Center for Epidemiologic Studies Depression Scale-Revised (CESD-R), Suicidal Affect-Behavior-Cognition Scale (SABCS), and the Brief Social Desirability Scale (BSDS). Study instruments pertinent to this analysis will be described further.
Ethical Considerations
This study was approved by the Institutional Review Board (IRB) at the first authors’ primary and secondary affiliations. Procedures for suicide safety and risk are detailed below. First, the research team flagged participants scores ≥11 on the SABCS (maximum score = 32)—the primary measure for suicidality on the survey (Harris et al., 2015). Then, suicide risk assessments using the Columbia Suicide Severity Rating Scale (C-SSRS) were completed with participants who endorsed suicidality on the survey (Posner et al., 2009, 2011; Lucas et al., 2015). Next, suicide safety and risk protocols were initiated for low, moderate, and high-risk students based on their responses from the C-SSRS suicide risk assessment. Protocols are included as supplementary. Finally, all participants received NIMH-approved information on depression and suicide risk for college students after completing the survey (NIMH, 2018).
Measurements
Individual and Clinical Factors
The online survey comprised of the eligibility screen, demographic questionnaire, and study instruments. The demographic questionnaire included individual and clinical factors, as depicted in the conceptual model. Individual factors included age (continuous), gender (male, female, other), sexuality (heterosexual, LGBTQ, other), race (White/Caucasian, Black/African American, Asian, Native Hawaiian or Pacific Islander, American Indian/Alaska Native, other), ethnicity (Hispanic/Latinx, non-Hispanic/Latinx), income—family of origin (five categories from less than $30,000 to over $100,000), first-generation college student status (yes/no), and international student (yes/no). Clinical factors included pre-existing medical or mental health conditions (yes, no), adverse childhood experiences (ACEs), substance use, personal history of suicide attempt (yes, no), family history of suicide (yes, no, unsure), access to mental health services (yes, no), currently receiving mental health services (yes, no), family support (yes, no), and access to guns or firearms (yes, no).
Moral Distress: Predictor of Interest
Moral distress, the predictor variable for this study, was captured using the Moral Distress Thermometer (MDT) by Wocial and Weaver (2013). The MDT is a single item visual-analog scale from 0 (none) to 10 (worst possible) with verbal descriptors to help anchor the degree of the distress in a meaningful way. The MDT provides a definition of moral distress and asks respondents to reflect on their clinical practice in the last 2 weeks and identify on the thermometer their level of moral distress. The instrument has acceptable construct validity with convergent validity with the Moral Distress Scale (MDS)—a commonly used measure for moral distress among health care professionals (Giannetta et al., 2020; Sonis et al., 2022; Wocial & Weaver, 2013) and concurrent validity with those wanting to leave turnover groups (those wanting to leave or not leave a position) (Wocial & Weaver, 2013).
Depression: Mediator
The mediator variable was depression quantified by the Center for Epidemiologic Studies Depression Scale-Revised (CESD-R) by Eaton et al. (2004). The CESD-R is frequently used in clinical practice and research to capture depressive symptoms. Nine different symptom groups are measured in the CESD-R, including sadness/dysphoria, loss of interest/anhedonia, appetite, sleep, thinking/concentration, guilt/worthlessness, tired/fatigue, movement/agitation, and suicidal ideation. These correspond with the symptoms of depression in the Diagnostic and Statistical Manual for Mental Disorders, 5th edition (DSM-5) (APA, 2013). This 20-item Likert scale includes response ranges from 0 (not at all or less than a day) to 3 (nearly every day for 2 weeks). Total summative scores range from 0 to 60, with higher scores indicating greater depressive symptomology. Categories of determination based upon a designated algorithm for depression is associated with the instrument. The scale is well-known with good psychometric properties and remains one of the most widely used instruments in psychiatric epidemiology (Center for Innovative Public Health Research, 2022). In a recent study, researchers analyzed 19 English version and 11 other language articles using the CESD-R from 2004 to 2018 and found high internal consistency (Cronbach’s α = 92) and robust convergent, factorial, and diagnostic validity (Kimong et al., 2022).
Suicide Risk: Outcome
The Suicidal Affect-Behavior-Cognition Scale (SABCS) by Harris et al. (2015) was used to measure suicide risk, the outcome variable for this study. The SABCS is a six-item measure that captures the affective, behavioral, and cognitive attributes of suicidality. Items may include recent suicide ideation (e.g., “How often have you thought about killing yourself in the past year?”) with responses ranging from “Never” (0) to “Very Often” (5) and future suicide behavior (e.g., “How likely is it that you will attempt suicide someday?” with responses ranging from “Not at all” (0) to “Very Likely” (5). Items are totaled with higher scores indicating greater suicide risk. The SABCS has strong psychometric properties with excellent internal reliability estimates and construct and convergent validity (Harris et al., 2015).
Statistical Analyses
Missing Data
At the participant level, 18.26% had missing data for at least one variable of interest. Multiple imputation was used to maximize utilization of the complete available data. This imputation method was chosen given the rate of missingness exceeded 5% for the primary variables of interest. Subsequent regression results for all analyses averaged estimates over 1,000 iterations of multiple imputation (MICE) using a classification and regression tree (CART) model to nonlinearly predict each missing value from the available covariate data.
Descriptive Statistics
Preliminary analyses for both the raw data and the imputed data included descriptive statistics—that is, means, standard deviations, minimums, medians, and maximums for continuous variables; counts and percentages for categorical variables.
Stepwise Linear Regression
To determine the set of control variables to include in the mediation modeling, stepwise linear regression was carried out for each of the 1,000 imputed datasets using the methods proposed by Brand (1999). Separate sets of models regressing suicide risk and depression on moral distress and all other independent variables were performed. The union of the set of predictors selected in the two step-wise procedures for suicide risk and depression defined the set of control variables included for mediation analyses. Moral distress was retained as an independent variable in the final models as a variable of interest to the study.
Mediation Analysis
To examine the mediation model, general linear modeling was employed using Baron and Kenny’s (1986) four step mediation analysis plan. Each of the following models were examined in succession. This process started with (1) The association between moral distress and suicide risk by regressing suicide risk on moral distress and all control variables. Having found a statistically significant association between suicide risk and moral distress, (2) the association between moral distress and depression was examined by regressing depression on moral distress and all control variables. Having found a statistically significant association between depression and moral distress, an examination was performed on (3) the association between depression and suicide risk while controlling for moral distress by regressing suicide risk on moral distress, depression, and all control variables. Finally, using the results of models (1), (2), and (3), an examination was undertaken to determine whether or not complete or partial mediation exists by controlling for the mediator variable, depression.
The determination of mediation was made using four derived statistics: average direct effects (ADE) of moral distress on suicide risk, average causal mediated effects (ACME) of moral distress on suicide risk by depression, total effects of moral distress on suicide risk, and percent of total effects of moral distress mediated by depression. The percent of total effects mediated was derived from the absolute value of the estimate for the controlled mediated effects divided by the sum of the absolute value of the estimate for the controlled mediated and direct effects, or total effect. Because the percent mediated was derived from multiple parameters from different models, bootstrapping was used to obtain an empirical 95% quantile-based confidence interval for percent mediated.
According to Baron and Kenny, mediation can be inferred when two conditions are satisfied. First, moral distress is found to be statistically significantly associated with both suicide risk and depression after adjusting for covariates (model 1 and model 2). Second, the proportion of the total effect of moral distress accounted for by the controlled mediated effect of depression (ACME) is statistically significantly different from zero (model 3). Additionally, mediation can be described as either full or partial. Partial mediation would be found if moral distress remains statistically significantly associated with suicide risk while controlling for the mediating effects of depression in the model 3; full mediation would be found if moral distress is no longer statistically significant. Statistical significance was taken at the 0.05 level. All analysis was performed in R (R Core Team, 2021).
Findings
Descriptive Statistics
A comparison of the raw vs. imputed data is illustrated in Table 1. Note. Counts for the imputed data are not exact integers as these counts are weighted. Looking across the rows, the imputed data is not dissimilar from the raw data. Additionally, both data sets show that the sample is mostly female (91%), White (75%), and self-identified as heterosexual (91%). The rest of the table can be interpreted in a similar manner. More than a third (36.1%) of participants were first generation college students and about a quarter reported a pre-existing mental health condition (24.3%). Almost 85% of the sample reported access to mental health services whereas 21.8% reported receiving mental health services. Alcohol use on weekends was as high as 57% and 21% on weekdays and almost a third (31.7%) had access to guns or firearms. Approximately 16% of the sample reported ≥4 adverse childhood experiences, and 13% had a family history of suicide. The average moral distress score was 2.14, and the median depression score was 12.0.
Table 1 –
Individual and Clinical Factors for Nursing Students (N = 679 Students*; Imputations = 1,000)
| Variable | Unimputed Data | Imputed Data (Imputations = 1,000; N = 679) |
|---|---|---|
|
| ||
| Individual factors | ||
| Age (years) | n = 661 | |
| Mean (SD) | 24.86 (6.42) | 24.86 (6.42) |
| Median [Min, Max] | 22.00 [18.00, 57.00] | 22.00 [18.00, 57.00] |
| Gender, n (%) | ||
| Female | 613 (90.68%) | 615.72 (90.68%) |
| Male | 61 (9.02%) | 61.27 (9.02%) |
| Other | 2 (0.30%) | 2.01 (0.30%) |
| Sexuality, n (%) | ||
| Heterosexual | 618 (91.02%) | 618.00 (91.02%) |
| LGBTQ | 50 (7.36%) | 50.00 (7.36%) |
| Other | 11 (1.62%) | 11.00 (1.62%) |
| Race, n (%) | ||
| White/Caucasian | 510 (75.11%) | 510.00 (75.11%) |
| Black/African American | 54 (7.95%) | 54.00 (7.95%) |
| Asian | 94 (13.84%) | 94.00 (13.84%) |
| Native Hawaiian or Pacific Islander | 6 (0.88%) | 6.00 (0.88%) |
| American Indian/Alaska Native | 14 (2.06%) | 14.00 (2.06%) |
| Other | 34 (5.01%) | 34.00 (5.01%) |
| Ethnicity, n (%) | ||
| Hispanic/Latinx | 90 (13.66%) | 92.75 (13.70%) |
| Non-Hispanic/Latinx | 569 (86.34) | 586.25 (86.30%) |
| Income, n (%) | ||
| <$30,000 | 125 (18.97%) | 128.68 (18.95%) |
| $30,000−$50,000 | 120 (18.21%) | 123.62 (18.21%) |
| $51,000−$75,000 | 137 (20.79%) | 141.31 (20.81%) |
| $76,000−$100,000 | 121 (18.36%) | 124.58 (18.35%) |
| >$100,000 | 156 (23.67%) | 160.81 (23.68%) |
| International student, n (%) | 5 (0.74%) | 5.00 (0.74%) |
| First generation college student, n (%) | 244 (36.09%) | 245.04 (36.09%) |
| Clinical Factors | ||
| Pre-existing medical condition, n (%) | 124 (18.29%) | 124.19 (18.29%) |
| Pre-existing mental health condition, n (%) | 164 (24.26%) | 164.72 (24.26%) |
| Receiving mental health services, n (%) | 148 (21.83%) | 148.23 (21.83%) |
| Access to mental health services, n (%) | 576 (84.83%) | 576.00 (84.83%) |
| ACES, n (%) | ||
| ≥4 | 109 (16.05%) | 109.00 (16.05%) |
| ≥7 | 21 (3.09%) | 21.00 (3.09%) |
| History of suicide attempt, n (%) | 57 (8.42%) | 57.20 (8.42%) |
| Family history of suicide, n (%) | ||
| Yes | 88 (12.98%) | 88.12 (12.98%) |
| No | 535 (78.91%) | 535.80 (78.91%) |
| Unsure | 55 (8.11%) | 55.08 (8.11%) |
| Trusted family member, n (%) | 608 (89.68%) | 608.90 (89.68%) |
| Access to guns or firearms, n (%) | 215 (31.71%) | 215.29 (31.71%) |
| Alcohol use on weekdays, n (%) | 145 (21.35%) | 145.00 (21.35%) |
| Alcohol use on weekends, n (%) | 389 (57.29%) | 389.00 (57.29%) |
| Prescription misuse, n (%) | 54 (7.95%) | 54.17 (7.98%) |
| Marijuana or other illegal drug use, n (%) | 33 (4.89%) | 33.20 (4.89%) |
| Mediator | ||
| Depression | n = 662 | |
| Mean (SD) | 15.87 (13.99) | 15.87 (13.99) |
| Median [Min, Max] | 12.00 [0.00, 60.00] | 12.00 [0.00, 60.00] |
| Predictor | ||
| Moral distress | n = 619 | |
| Mean (SD) | 2.14 (2.20) | 2.14 (2.20) |
| Median [Min, Max] | 2.00 [0.00, 9.00] | 2.00 [0.00, 9.00] |
Note. Max, maximum; Min, minimum; SD, standard deviation.
This represents the total number of students who responded to the survey who were 18 years or older, enrolled in an undergraduate nursing program at a college or university, were at the junior or senior level or equivalent for those in accelerated or part-time programs or had completed at least one nursing clinical rotation, and were willing to provide informed consent.
Stepwise Linear Regression
Stepwise linear regression was used to identify control variables for the mediation models. Table 2 depicts results of regressing suicide risk on all control variables while retaining moral distress in the model. Moral distress is not statistically significantly associated with suicide risk with p value = .3402. In the model, older age, presence of family trust, first generation college students, and White students have negative estimates leading to a decrease in suicide risk holding all other variables constant. All other variables in the model have positive estimates leading to an increase in suicide risk. Among these, international student status and a prior history of suicide attempt have the largest estimates at 6.96 and 5.13, respectively. The results of regressing depression on all other control variables while retaining moral distress in the model are provided in Table 2. In addition, moral distress is statistically significantly associated with depression with a 0.66 increase in depression for each one unit increase in moral distress. Most of the independent variables have positive estimates leading to an increase in depression. Among these, international student and pre-existing mental health conditions have the largest estimates at 7.88 and 7.22, respectively. The presence of family trust variable was associated with an 8.13 decrease in depression.
Table2 –
Stepwise Linear Regression Models* to Select Mediation Model Covariates
| Dependent Variable | Predictor | Effect Estimate | 95% CI | p Value† |
|---|---|---|---|---|
|
| ||||
| Suicide risk | Moral distress | 0.06 | (−0.07, 0.19) | .3402 |
| Depression | 0.16 | (0.13, 0.18) | <.0001† | |
| ACES ≥ 4 (Yes vs. No) | 1.14 | (0.28, 2.00) | .0096† | |
| Age | −0.06 | (−0.11, −0.02) | .0090† | |
| Currently receiving mental health services (Yes vs. No) | 1.10 | (0.38, 1.82) | .0028† | |
| Family history of suicide (Unsure vs. No) | 1.43 | (0.37, 2.48) | .0081† | |
| Family history of suicide (Yes vs. No) | 0.55 | (−0.30, 1.41) | .2061 | |
| Family trust (Yes vs. No) | −0.99 | (−1.95, −0.03) | .0433† | |
| First generation student (Yes vs. No) | −1.10 | (−1.71, −0.49) | .0004† | |
| History of suicide attempt (Yes vs. No) | 5.13 | (4.06, 6.19) | <.0001† | |
| International student (Yes vs. No) | 6.96 | (3.67, 10.26) | <.0001† | |
| White/Caucasian (Yes vs. No) | −0.85 | (−1.53, −0.170.65) | .0141† | |
| Depression | Moral distress | 0.66 | (0.24, 1.08) | .0021† |
| ACES ≥ 4 (Yes vs. No) | 5.57 | (2.85, 8.29) | <.0001† | |
| Age | −0.33 | (−0.48, −0.18) | <.0001† | |
| Currently receiving mental health services (Yes vs. No) | 4.70 | (2.17, 7.23) | .0003† | |
| Family trust (Yes vs. No) | −8.13 | (−11.19, −5.07) | <.0001† | |
| History of suicide attempt (Yes vs. No) | 6.72 | (3.28, 10.15) | .0001† | |
| International student (Yes vs. No) | 7.88 | (−2.81, 18.57) | .1492 | |
| Pre-existing mental health condition (Yes vs. No) | 7.22 | (4.72, 9.73) | <.0001† | |
| Prescription misuse (Yes vs. No) | 5.99 | (2.55, 9.42) | .0007† | |
| White/Caucasian (Yes vs. No) | −2.78 | (−4.94, −0.61) | .0121† | |
All stepwise procedures began with all collected variables; Moral Distress was retained in all models as a predictor of interest.
Effect estimate is statistically significant at the p < .05 level.
Mediation Analysis
Linear modeling was used to examine the mediation model using Baron and Kenny’s (1986) four step mediation analysis plan. For the Baron and Kenny step 1, step 2, and step 3, the set of control variables was composed of the union of the sets of individual and clinical covariates selected in the stepwise regressions of suicide risk regressed on all independent variables and depression regressed on all independent variables. Moral distress was retained in the modeling as a predictor of interest. A summary of the mediation analysis is provided in Table 3 and a visual representation is given in Figure 2.
Table 3 –
Mediation Model Effects* for Suicide Risk Outcome
| Model | Dependent Variable | Predictor | Effect | Estimate† | 95% CI |
|---|---|---|---|---|---|
|
| |||||
| 1 | Suicide risk | Moral distress | Effect of moral distress on suicide risk | 0.1600† | (0.0100,0.3100) |
| 2 | Depression | Moral distress | Effect of moral distress on depression | 0.6600† | (0.2100,1.1000) |
| 3 | Suicide risk | Moral distress | Direct effect of moral distress on suicide risk | 0.1048 | (−0.0796, 0.1904) |
| Depression | Effect of depression on suicide risk | 0.1600† | (0.1400, 0.1800) | ||
| Moral distress | Effect of moral distress on suicide risk mediated by depression | 0.1048† | (0.0337, 0.1791) | ||
| Moral distress | Total effect of moral distress on suicide risk | 0.1604† | (0.0083, 0.3117) | ||
| Moral distress | Proportion of total effect mediated | 64.46% | (48%, 83%)** | ||
All models adjusted for ACES ≥ 4, Age, Currently receiving mental health services, Family history of suicide, Family trust, History of suicide attempt, First generation student, International student, Pre-existing mental health condition, Prescription misuse, White Caucasian.
The 95% confidence interval for proportion of total effect mediated is based on 2.5% and 97.5% quantiles of bootstrapped estimates for proportion mediated from 1,000 imputed datasets.
Effect estimate is statistically significant at the alpha = 0.05 level.
Figure 2 – Mediation model effect of depression on the relationship between moral distress and suicide risk.
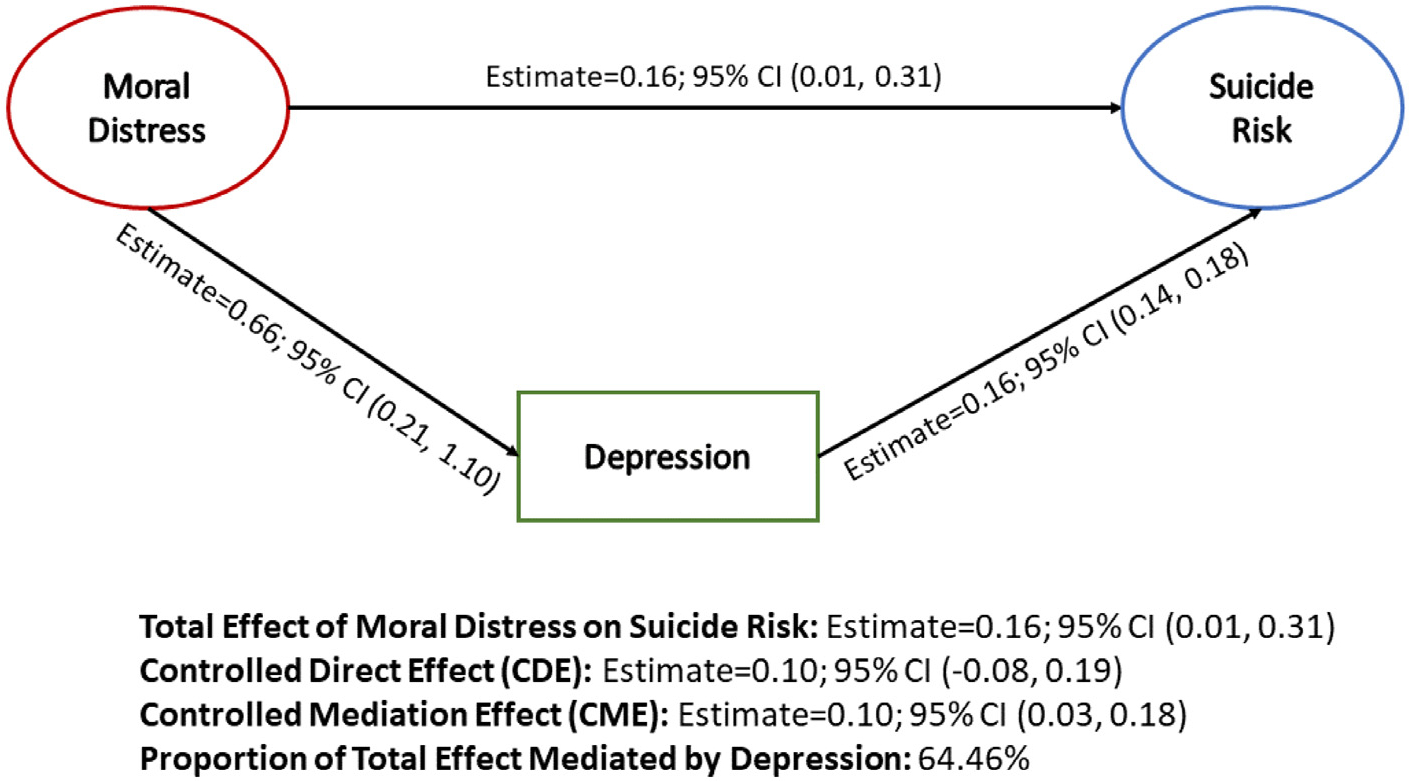
First, suicide risk was regressed on moral distress and control variables, not considering depression. Modeling was performed using each imputed dataset; and the weighted sum of coefficients was calculated as the reported modeling estimates. The modeling results in Table 3, Effect of Moral Distress on Suicide Risk, show that moral distress is statistically significantly associated with suicide risk with 95% confidence interval (0.01, 0.31) that does not include zero.
Next, depression was regressed on moral distress and control variables to examine the association between moral distress and depression. The weighted sum of coefficients was again calculated from modeling on each imputed dataset. In Table 3, Effect of Moral Distress on Depression, shows that moral distress is statistically significantly associated with depression with 95% confidence interval (0.21, 1.10) that does not include zero. Finally, using each imputed dataset, suicide risk was regressed on moral distress, while adjusting for depression as a potential mediator, and the control variables. Mediation statistics were calculated from the modeling results performed on each imputed dataset using 1,000 bootstrap iterations. The weighted sum of all modeling results across all imputed datasets are provided in Table 3. Here, the Direct Effect of Moral Distress on Suicide Risk is no longer statistically significant with zero contained in the 95% confidence interval (−0.08, 0.19). However, the Effect of Depression on Suicide Risk is statistically significant with 95% confidence interval (0.14, 0.18). Finally, the Proportion of Total Effect Mediated by Depression is 64.46% with 95% bootstrapped CI (48%, 83%), indicating statistical significance with 0% not included in the confidence interval.
These results show that both conditions required to be satisfied by Baron and Kenny to demonstrate mediation have been met; and moral distress is statistically significantly associated with both suicide risk and depression after adjusting for covariates; and the proportion of the total effect of moral distress accounted for by the controlled mediated effect of depression is statistically significantly different from zero. Further, because moral distress is no longer statistically significant in the face of depression, it can be determined that full mediation exists.
Discussion
To date, this is one of the first studies to examine the relationship between moral distress, depression, and suicide risk for nursing students. The findings suggest three important points. First, moral distress is a risk factor for depression and suicide risk with a special alarm for nursing students. Second, the significant relationship between moral distress and suicide risk was fully mediated by depression. Finally, individual and clinical factors, such as pre-existing mental health conditions, history of suicide attempt, and family suicide history, may further contribute to the risk of depression and suicide risk among undergraduate nursing students.
First, this analysis found a positive and significant association between moral distress and depression. Moral distress is often reported in the clinical arena whereby one is involved in what one perceives to be a morally undesirable situation and experiences negative self-directed attitudes or emotions such as regret, shame, or anger (Campbell et al., 2016). These negative emotions may be internalized by nursing students and contribute to depressive symptomology. This is consistent with other studies that cite negative emotional and psychological consequences of moral distress, such as frustration, sadness, guilt, anger, and hurt (Henrich et al., 2017). While many studies have focused on nurses or other health care providers, this study demonstrates the need to expand our perspective on moral distress to include nursing and allied health professional students, who are in morally distressing or comprising situations, and how this may impact their mental and emotional health and well-being.
Second, the significant relationship between moral distress and suicide risk was fully mediated by depression. This reinforces the importance of these psychological variables and developing interventions to address and mitigate all three of them within nursing programs. To the authors’ knowledge, this is the first study to demonstrate a direct relationship between moral distress and suicide risk using a meditation model. While other studies have demonstrated a relationship between (a) moral distress and depression (Petrișor et al., 2021) and (b) depression and suicide risk (Melhem et al., 2019), this study revealed an important finding on the significant impact of moral distress on suicide risk within nursing students. This contributes to the body of advancing knowledge on moral distress and is an important direction for further research on suicide risk. From this study alone, however, it is unclear how morally distressing encounters may potentially exacerbate pre-existing mental health conditions or contribute to emergent psychological or emotional distress for students. More research is needed to better understand these responses and identify supportive mechanisms within academic and practice environments.
Lastly, individual and clinical factors may further contribute to the risk of depression and suicide risk among undergraduate nursing students. About a quarter of nursing students had a pre-existing mental health condition, which is consistent with the growing body of students on college campuses with identifiable mental health conditions (Lipson et al., 2019). While this can be a risk factor for suicide, with clear identification and prompt intervention, this risk can be lowered for students (Wolitzky-Taylor et al., 2020). In this study, it was promising that 85% of students reported having access to mental health services. However, less than a quarter of students were currently receiving mental health treatment (21.8%). Prior research suggests that privacy and confidentiality, stigma, cost, time, and cultural sensitivity could be potential barriers for students to access mental health services on college campuses (Horwitz et al., 2020). This could be an avenue of further study to understand the barriers to seeking available mental health care. Furthermore, a history of a previous suicide attempt and family suicide history were associated with higher risk for suicide, which is consistent with current research and practice.
Another concerning clinical factor was the high number of nursing students who reported access to firearms. With firearms-related suicide deaths on the rise for female nurses (Davidson et al., 2021), it is important to address firearms safety for nursing students, especially those who may be at high risk for suicide. Alcohol use and misuse of prescription medications was also a clinical factor identified in this study and a target for risk mitigation. Substance use increases the risk for suicide among all age groups; with today’s prevalence of substance use—especially on college campuses—it is imperative to discuss how alcohol and substance use may negatively impact nursing students and their mental health (Rattner, 2021). This may be especially relevant for nursing students who experience morally distressing events or those with a history of adverse childhood experiences (Kameg et al., 2020; Kameg & Mitchell, 2021), which may exacerbate or increase the risk for depression and suicide in their academic programs.
Implications for Nursing Education and Practice
As nurse leaders, educators, and clinicians, it is important to adequately address the issues that nursing students are facing in their academic and practice environments (Robichaux et al., 2022). A multipronged and dimensional approach to mitigate the risk for moral distress, depression, and suicide risk is recommended. To begin, providing comprehensive ethics education may afford students an opportunity to discuss troubling issues in an accepting atmosphere with other students to share their thoughts on sensitive topics. Hoskins, Grady, and Ulrich (2018) note that “Nursing practice is inextricably entwined with moral complexity.” Nurse educators should closely examine (and revise, if needed) their ethics curriculums to better prepare nursing students to meet the ethical challenges inherent in clinical practice. This may mitigate the negative consequences of moral distress, which may, in turn, decrease the risk for depression and suicide, especially for high-risk students. Furthermore, receiving feedback and support from peers and faculty on ethical issues may externalize, rather than internalize, some of their fears, worries, and self-blame and decrease their heavy burden; thus, potentially, lowering the risk for depression and other mental health concerns.
Next, identifying students who are experiencing depressive symptomology is a critical first step for addressing mental health concerns in nursing education. As Tung et al. (2018) reported, a prevalence of depression of 34% among nursing students is highly concerning and warrants intervention. This may include routine depression screening measures for nursing students at health appointments on campus or referral solutions for faculty and peers who are concerned about a student’s mental health. Furthermore, access to mental health care on college campuses and tailoring resources to nursing students is a priority along with destigmatizing care-seeking behaviors (Eisenberg et al., 2012), especially for health-professional students. Strategies, such as colocated mental health services embedded into nursing schools, may be an innovative solution to increase access and lower stigma for mental health services. Other novel approaches, such as telepsychiatry services for students who live off campus, may be a viable option to increase engagement in mental health services and treatment (Hadler et al., 2021).
For students who are experiencing moral distress, tailored approaches that underscore the core identity and priorities of nursing students (e.g., protecting and advocating for patients) may be a necessary component to future interventions. Oftentimes, students are inherently distressed by witnessing or encountering an ethically fraught situation—not just for themselves—but for the others who are involved whether that is a patient, family, nursing colleague, or peer. It is important we recognize the strengths and values nursing students bring to their education and work collaboratively with them to develop interventions to support their mental health and process complex emotions related to ethically challenging or morally distressing experiences. Specific mental health interventions, such as cognitive-behavioral therapy (CBT), stress management programs, and mindfulness/meditation practices (Li et al., 2018), may be indicated for students who have intense thoughts and emotions related to morally distressing experiences.
Finally, a thoughtful approach to suicide risk and assessment is essential for suicide prevention among college-aged youth, including undergraduate nursing students. Utilizing evidence-based risk assessment tools, such as the Columbia Suicide Severity Rating Scale (C-SSRS), may be indicated in both educational and clinical settings (Horwitz et al., 2015). Initial screening measures, such as the ASQ toolkit (Ask Suicide-Screening Questions), are also freely available for use and help identify youth at risk for suicide (Horowitz et al., 2020). After screening and assessment, initiating safety interventions, such as Stanley and Brown’s Safety Planning Intervention (SPI), is an excellent way to engage students in their safety plan and promote a culture of wellness on college campuses (Stewart et al., 2020). Nursing programs can also endorse student safety and mental health by encouraging students to utilize resources and supports available on campus. Last but not least, grassroots efforts led by students and faculty, such as participating in the American Foundation for Suicide Prevention (AFSP) Out of the Darkness Community Walks, may also be a powerful strategy to raise awareness on suicide risk (Pirkis et al., 2019) and evolve the culture of mental health within undergraduate nursing programs.
Limitations
This study has several limitations. First, the cross-sectional nature of the study only allowed reporting on moral distress, depression, and suicide risk at one point in time. Longitudinal studies may provide important information on student resilience and coping for moral distress and other challenging areas of nursing education. Second, all participants belonged to the National Association of Student Nurses, which may have limited generalizability to all baccalaureate nursing students. Third, there is the potential for selection bias as those students with personal or family experience with depression, suicide risk, or ethically distressing nursing school experiences may have been more likely to respond and provide socially desirable responses. This was mitigated, in part, by using a social desirability scale.
Additionally, we utilized an online survey and received more than 800 responses within 5 hours of its opening. Given the large volume of responses within a short time, we needed to close the survey. Although we received survey data from a wide range of participants, important responses from students who were unable to access and complete the survey may have been missed. Lastly, most participants identified as non-Hispanic, heterosexual White females—which is a significant limitation of the study. While these demographics are representative of the current nursing student population in the United States, we know racism, cis-gender, and heteronormative expectations and restrictions have historically limited the numbers of racially and gender-diverse students in nursing programs (ANA, 2021). As the nursing student population continues to grow across racial, ethnic, and gender lines, it is imperative for future studies to intentionally recruit diverse samples of nursing students in regard to race/ethnicity, gender, sexuality, and other areas of identity and experience.
Conclusion
The purpose of this study was to understand the mediating effect of depression on the relationship between moral distress and suicide risk among undergraduate nursing students. As the data indicates, nursing students are experiencing moral distress and depression that may have a significant impact on their mental health and well-being, including suicide risk. As Robichaux et al. (2022) states “the preparation of nurses at all levels to be moral agents is a critical job of the profession and specifically nursing education.” It is also the job of the profession to support and promote the mental and emotional health of nursing students. Nurse leaders, educators, and clinicians should contribute to advocating for student mental health by engaging in efforts to identify depression and suicide risk and developing evidence-based interventions to support the mental and emotional health of nursing students. This may be especially important for students who are experiencing morally distressing events or encounters.
Supplementary Material
Acknowledgments
The authors thank Kevin L. McKee, PhD, of the University of California Davis Center for Neuroscience for his contributions developing the code for the mediation analyses in R.
Funding:
This study was funded by The American Nurses Foundation and Ruth L. Kirschstein NRSA Post-Doctoral Fellowship (T32NR007100) at the University of Pennsylvania School of Nursing with additional support by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR003015. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Credit Statement
Cynthia P. Paidipati: Conceptualization, Methodology, Investigation, Writing – Original Draft, Review & Editing, Project Administration, Funding Acquisition. Alicia Lozano: Formal Analysis, Writing – Original Draft, Review & Editing, Visualization. Jennifer West: Formal Analysis, Writing – Original Draft, Review & Editing, Visualization. Liming Huang: Formal Analysis, Data Curation. Alexandra Hanlon: Methodology, Supervision, Funding Acquisition. Connie M. Ulrich: Conceptualization, Methodology, Writing – Original Draft, Review & Editing, Supervision, Funding Acquisition.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.outlook.2023.101966.
REFERENCES
- American Nurses Association (ANA). (2021). National Commission to Address Racism in Nursing. Report Series: Racism in Nursing. Report #3 of 6: “How does racism in nursing show up in the education space?” https://www.nursingworld.org/~49b97e/globalassets/practiceandpolicy/workforce/commission-to-address-racism/3racismintheeducationspace.pdf [Google Scholar]
- American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders: DSM-5: Vol. 5. American Psychiatric Association Publishing. [Google Scholar]
- Aradilla-Herrero A, Tomás-Sábado J, & Gómez-Benito J (2014). Associations between emotional intelligence, depression and suicide risk in nursing students. Nurse Education Today, 34(4), 520–525, doi: 10.1016/j.nedt.2013.07.001. [DOI] [PubMed] [Google Scholar]
- Brand JPL (1999). Development, Implementation and Evaluation of Multiple Imputation Strategies for the Statistical Analysis of Incomplete Data Sets. Erasmus University; Rotterdam. Retrieved from http://hdl.handle.net/1765/19790. [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Campbell SM, Ulrich CM, & Grady C (2016). A broader understanding of moral distress. The American Journal of Bioethics, 16(12), 2–9, doi: 10.1080/15265161.2016.1239782. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2022). Suicide mortality in the United States, 2000–2020. https://www.cdc.gov/nchs/products/databriefs/db433.htm
- Center for Innovative Public Health Research. (2022). CESD-R: The Center for Epidemiologic Studies Depression Scale Revised. https://cesd-r.com
- Chen CJ, Chen YC, Sung HC, Hsieh TC, Lee MS, & Chang CY (2015). The prevalence and related factors of depressive symptoms among junior college nursing students: A cross-sectional study. Journal of Psychiatric and Mental Health Nursing, 22(8), 590–598, doi: 10.1111/jpm.12252. [DOI] [PubMed] [Google Scholar]
- Chernomas WM, & Shapiro C (2013). Stress, depression, and anxiety among undergraduate nursing students. International Journal of Nursing Education Scholarship, 10(1), 255 266, doi: 10.1515/ijnes-2012-0032. [DOI] [PubMed] [Google Scholar]
- Davidson JE, Ye G, Deskins F, Rizzo H, Moutier C, & Zisook S (2021). Exploring nurse suicide by firearms: A mixed-method longitudinal (2003–2017) analysis of death investigations. Nursing Forum, 56(2), 264–272, doi: 10.1111/nuf.12536. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Smith C, Ybarra M, Muntaner C, & Tien A (2004). Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD-R). In Maruish ME (Ed.), The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults (pp. 363–377). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Eisenberg D, Hunt J, & Speer N (2012). Help seeking for mental health on college campuses: Review of evidence and next steps for research and practice. Harvard Review of Psychiatry, 20(4), 222–232, doi: 10.3109/10673229.2012.712839. [DOI] [PubMed] [Google Scholar]
- Giannetta N, Villa G, Pennestrì F, Sala R, Mordacci R, & Manara DF (2020). Instruments to assess moral distress among healthcare workers: A systematic review of measurement properties. International Journal of Nursing Studies, 111, 1–34, doi: 10.1016/j.ijnurstu.2020.103767. [DOI] [PubMed] [Google Scholar]
- Grady C, Danis M, Soeken KL, O’Donnell P, Taylor C, Farrar A, & Ulrich CM (2008). Does ethics education influence the moral action of practicing nurses and social workers? The American Journal of Bioethics, 8(4), 4–11. 10.1080/15265160802166017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadler NL, Bu P, Winkler A, & Alexander AW (2021). College student perspectives of telemental health: A review of the recent literature. Current Psychiatry Reports, 23(2), 6, doi: 10.1007/s11920-020-01215-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, Syu JJ, Lello OD, Chew YE, Willcox CH, & Ho RH (2015). The ABC’s of suicide risk assessment: Applying a tripartite approach to individual evaluations. PLoS One, 10(6), 1–21, doi: 10.1371/journal.pone.0127442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and work-flow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381, doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrich NJ, Dodek PM, Gladstone E, Alden L, Keenan SP, Reynolds S, & Rodney P (2017). Consequences of moral distress in the intensive care unit: A qualitative study. American Journal of Critical Care, 26(4), e48–e57, doi: 10.4037/ajcc2017786. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Snyder DJ, Boudreaux ED, He JP, Harrington CJ, Cai J, Claassen CA, Salhany JE, Dao T, Chaves JF, Jobes DA, Merikangas KR, Bridge JA, & Pao M (2020). Validation of the ask suicide-screening questions for adult medical inpatients: A brief tool for all ages. Psychosomatics, 61(6), 713–722, doi: 10.1016/j.psym.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz AG, Czyz EK, & King CA (2015). Predicting future suicide attempts among adolescent and emerging adult psychiatric emergency patients. Journal of Clinical Child & Adolescent Psychology, 44(5), 751–761, doi: 10.1080/15374416.2014.910789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz AG, McGuire T, Busby DR, Eisenberg D, Zheng K, Pistorello J, Albucher R, Coryell W, & King CA (2020). Sociodemographic differences in barriers to mental health care among college students at elevated suicide risk. Journal of Affective Disorders, 271, 123–130, doi: 10.1016/j.jad.2020.03.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoskins K, Grady C, & Ulrich CM (2018). Ethics education in nursing: Instruction for future generations of nurses. The Online Journal of Issues in Nursing, 23(1), 1–4. 10.3912/OJIN.Vol23No01Man03 [DOI] [Google Scholar]
- Jameton A (2017). What moral distress in nursing history could suggest about the future of health care. AMA Journal of Ethics, 19(6), 617–628, doi: 10.1001/journalofethics.2017.19.6.mhst1-1706. [DOI] [PubMed] [Google Scholar]
- Kameg BN, Lindsay D, Lee H, & Mitchell A (2020). Substance use and exposure to adverse childhood experiences in undergraduate and graduate nursing students. Journal of the American Psychiatric Nurses Association, 26(4), 354–363, doi: 10.1177/1078390320905669. [DOI] [PubMed] [Google Scholar]
- Kameg B, & Mitchell A (2021). Associations between adverse childhood experiences and substance use in nursing students. Journal of Psychosocial Nursing and Mental Health Services, 59(7), 43–47, doi: 10.3928/02793695-20210219-03. [DOI] [PubMed] [Google Scholar]
- Kimong PJ, Erford BT, & DeCino DA (2022). Psychometric synthesis of the Center for Epidemiologic Studies Depression Scale–Revised English and translated/adapted versions. Measurement and Evaluation in Counseling and Development, 1–17, doi: 10.1080/07481756.2022.2099900. [DOI] [Google Scholar]
- Krautscheid L, DeMeester DA, Orton V, Smith A, Livingston C, & McLennon SM (2017). Moral distress and associated factors among baccalaureate nursing students: A multisite descriptive study. Nursing Education Perspectives, 38(6), 313–319, doi: 10.1097/01.NEP.0000000000000214. [DOI] [PubMed] [Google Scholar]
- Lachman VD (2016). Moral resilience: Managing and preventing moral distress and moral residue. MedSurg Nursing, 25(2), 121–124. [PubMed] [Google Scholar]
- Leal SC, & Santos JC (2016). Suicidal behaviors, social support and reasons for living among nursing students. Nurse Education Today, 36, 434–438, doi: 10.1016/j.nedt.2015.09.012. [DOI] [PubMed] [Google Scholar]
- Li C, Yin H, Zhao J, Shang B, Hu M, Zhang P, & Chen L (2018). Interventions to promote mental health in nursing students: A systematic review and meta-analysis of randomized controlled trials. Journal of Advanced Nursing, 74(12), 2727–2741, doi: 10.1111/jan.13808. [DOI] [PubMed] [Google Scholar]
- Lipson SK, Lattie EG, & Eisenberg D (2019). Increased rates of mental health service utilization by U.S. college students: 10-year population-level trends (2007–2017). Psychiatric Services, 70(1), 60–63, doi: 10.1176/appi.ps.201800332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas MS, Brawner BM, Hardie TL, Beacham B, Paidipati C, Diaz M, Lauer A, Hobbie W, & Deatrick JA (2015). Assessing suicidal ideation and behaviors among survivors of childhood brain tumors and their mothers during sociobehavioral research. Oncology Nursing Forum, 42(5), E319–E329. 10.1188/15.ONF.42-05AP [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macrynikola N, Miranda R, & Soffer A (2018). Social connectedness, stressful life events, and self-injurious thoughts and behaviors among young adults. Comprehensive Psychiatry, 80, 140–149, doi: 10.1016/j.comppsych.2017.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melhem NM, Porta G, Oquendo MA, Zelazny J, Keilp JG, Iyengar S, Burke A, Birmaher B, Stanley B, Mann JJ, & Brent DA (2019). Severity and variability of depression symptoms predicting suicide attempt in high-risk individuals. JAMA Psychiatry, 76(6), 603–613, doi: 10.1001/jamapsychiatry.2018.4513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health (NIMH). (2018). Depression and college students. No longer available. https://www.nimh.nih.gov/health/publications/depression-and-college-students/index.shtml
- National Institute of Mental Health (NIMH). (2022). Suicide is a leading cause of death in the United States. https://www.nimh.nih.gov/health/statistics/suicide
- National Student Nurses Association (NSNA). (2022). NSNA: National Student Nurses Association: Insight. Inspiration. Ingenuity. https://www.nsna.org [Google Scholar]
- Petrișor C, Breazu C, Doroftei M, Mărieș I, & Popescu C (2021). Association of moral distress with anxiety, depression, and an intention to leave among nurses working in intensive care units during the Covid-19 pandemic. Healthcare, 9(10), 1377, doi: 10.3390/healthcare9101377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piers RD, Azoulay E, Ricou B, Ganz FD, Decruyenaere J, Max A, Michalsen A, Maia PA, Owczuk R, Rubulotta F, Depuydt P, Meert A, Reyners AK, Aquilina A, Bekaert M, Van Den Noortgate NJ, Schrauwen WJ, & Benoit DD (2011). Perceptions of appropriateness of care among European and Israeli intensive care unit nurses and physicians. JAMA, 306(24), 2694–2703, doi: 10.1001/jama.2011.1888. [DOI] [PubMed] [Google Scholar]
- Pirkis J, Rossetto A, Nicholas A, Ftanou M, Robinson J, & Reavley N (2019). Suicide prevention media campaigns: A systematic literature review. Health Communication, 34(4), 402–414, doi: 10.1080/10410236.2017.1405484. [DOI] [PubMed] [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, Fisher P, Zelazny J, Burke A Oquendo M, & Mann JJ (2009). Columbia-Suicide Severity Rating Scale (C-SSRS) Since Last Visit. https://cssrs.columbia.edu/wp-content/uploads/C-SSRS-1-14-09-SinceLastVisit_AU5.1_eng-USori-1.pdf [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, & Mann JJ (2011). The Columbia Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry, 168(12), 1266–1277, doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rattner I (2021). A phenomenological study on substance use and misuse among nursing students. The Journal of Nursing Education, 60(11), 607–613, doi: 10.3928/01484834-20210913-01. [DOI] [PubMed] [Google Scholar]
- R Core Team. (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.r-project.org/ [Google Scholar]
- Rezayat F, & Dehghan Nayeri N (2014). The level of depression and assertiveness among nursing students. International Journal of Community Based Nursing and Midwifery, 2(3), 177–184. [PMC free article] [PubMed] [Google Scholar]
- Robichaux C, Grace P, Bartlett J, Stokes F, Saulo Lewis M, & Turner M (2022). Ethics education for nurses: Foundations for an integrated curriculum. The Journal of Nursing Education, 61(3), 123–130, doi: 10.3928/01484834-20220109-02. [DOI] [PubMed] [Google Scholar]
- Rushton CH, & Boston-Leary K (2022). Nurses suffering in silence: Addressing the stigma of mental health in nursing and healthcare. Nursing Management, 53(8), 7–11, doi: 10.1097/01.NUMA.0000853148.17873.77. [DOI] [PubMed] [Google Scholar]
- Sasso L, Bagnasco A, Bianchi M, Bressan V, & Carnevale F (2016). Moral distress in undergraduate nursing students: A systematic review. Nursing Ethics, 23(5), 523–534, doi: 10.1177/0969733015574926. [DOI] [PubMed] [Google Scholar]
- Sonis J, Pathman DE, Read S, & Gaynes BN (2022). A national study of moral distress among U.S. internal medicine physicians during the COVID-19 pandemic. PloS One, 17(5), 1–14, doi: 10.1371/journal.pone.0268375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart KL, Darling EV, Yen S, Stanley B, Brown GK, & Weinstock LM (2020). Dissemination of the safety planning intervention (SPI) to university counseling center clinicians to reduce suicide risk among college students. Archives of Suicide Research, 24 (suppl. 1), 75–85, doi: 10.1080/13811118.2018.1531797. [DOI] [PubMed] [Google Scholar]
- Thapar A, Eyre O, Patel V, & Brent D (2022). Depression in young people. The Lancet, 400(10352), 617–631, doi: 10.1016/S0140-6736(22)01012-1. [DOI] [PubMed] [Google Scholar]
- Tung YJ, Lo K, Ho R, & Tam W (2018). Prevalence of depression among nursing students: A systematic review and meta-analysis. Nurse Education Today, 63, 119–129, doi: 10.1016/j.nedt.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Ulrich CM, & Grady C (eds.) (2018). Moral Distress in the Health Professions. Springer Nature. [Google Scholar]
- Wocial LD, & Weaver MT (2013). Development and psychometric testing of a new tool for detecting moral distress: The moral distress thermometer. Journal of Advanced Nursing, 69(1), 167–174, doi: 10.1111/j.1365-2648.2012.06036.x. [DOI] [PubMed] [Google Scholar]
- Wojtowicz B, Hagen B, & Daalen-Smith V (2014). No place to turn: Nursing students’ experiences of moral distress in mental health settings. International Journal of Mental Health Nursing, 23(3), 257–264, doi: 10.1111/inm.12043. [DOI] [PubMed] [Google Scholar]
- Wolitzky-Taylor K, LeBeau RT, Perez M, Gong-Guy E, & Fong T (2020). Suicide prevention on college campuses: What works and what are the existing gaps? A systematic review and meta-analysis. Journal of American College Health, 68(4), 419 429, doi: 10.1080/07448481.2019.1577861. [DOI] [PubMed] [Google Scholar]
- Xu Y, Chi X, Chen S, Qi J, Zhang P, & Yang Y (2014). Prevalence and correlates of depression among college nursing students in China. Nurse Education Today, 34(6), e7–e12, doi: 10.1016/j.nedt.2013.10.017. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Peters A, & Chen G (2018). Perceived stress mediates the associations between sleep quality and symptoms of anxiety and depression among college nursing students. International Journal of Nursing Education Scholarship, 15(1), 1–9, doi: 10.1515/ijnes-2017-0020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


