Abstract
Background:
A diagnosis of prostate cancer (PC) may cause psychosocial distress that worsens quality of life; however, long-term mental health outcomes are unclear.
Objective:
To determine the long-term risks of major depression and death by suicide in a large population-based cohort.
Design, setting, and participants:
This was a national cohort study of 180 189 men diagnosed with PC during 1998–2017 and 1 801 890 age-matched, population-based, control men in Sweden.
Outcome measurements and statistical analysis:
Major depression and death by suicide were ascertained from nationwide outpatient, inpatient, and death records up to 2018. Cox regression was used to compute hazard ratios (HRs) adjusted for sociodemographic factors and comorbidities. Subanalyses assessed differences by PC treatment during 2005–2017.
Results and limitations:
Men diagnosed with high-risk PC had higher relative rates of major depression (adjusted HR [aHR] 1.82, 95% confidence interval [CI] 1.75–1.89) and death by suicide (aHR 2.43, 95% CI 2.01–2.95). These associations persisted for ≥10 yr after PC diagnosis. The relative increase in major depression was lower among those treated with radiation (aHR 1.44, 95% CI 1.31–1.57) or surgery (aHR 1.60, 95% CI 1.31–1.95) in comparison to androgen deprivation therapy (ADT) alone (aHR 2.02, 95% CI 1.89–2.16), whereas the relative rate of suicide death was higher only among those treated solely with ADT (aHR 2.83, 95% CI 1.80–4.43). By contrast, men with low- or intermediate-risk PC had a modestly higher relative rate of major depression (aHR 1.19, 95% CI 1.16–1.23) and higher relative rate of suicide death at 3–12 mo after PC diagnosis (aHR 1.88, 95% CI 1.11–3.18) but not across the entire follow-up period (aHR 1.02, 95% CI 0.84–1.25). This study was limited to Sweden and will need replication in other populations.
Conclusions:
In this large cohort, high-risk PC was associated with substantially higher relative rates of major depression and death by suicide, which persisted for ≥10 yr after PC diagnosis. PC survivors need close follow-up for timely detection and treatment of psychosocial distress.
Patient summary:
In a large Swedish population, men with aggressive prostate cancer had higher long-term relative rates of depression and suicide.
Keywords: Depression, Prostate cancer, Prostatic neoplasms, Suicide
1. Introduction
Prostate cancer (PC) is the most commonly diagnosed cancer among men in the USA, Europe, and most countries worldwide [1,2]. Because of greater screening rates and earlier diagnosis, most men with PC now survive for more than 15–20 yr after their diagnosis [2,3].
However, PC may adversely affect long-term mental health because of the psychosocial distress of the diagnosis, physical symptoms, treatment side effects, sexual and social concerns, and the financial burden [4,5]. The long-term mental health sequelae may cause substantial suffering and poor quality of life in the growing number of PC survivors [6,7]. A better understanding of these sequelae is needed to guide timely interventions and improve long-term outcomes.
Most prior studies of mental health among PC survivors have focused on depression and had small samples of <300 patients with <2 yr of follow-up. A meta-analysis of 27 such studies with an average study size of 158 men reported 15–18% prevalence of clinically significant depression among men with PC [8]. It has also been reported that PC survivors have moderately higher risks of hospitalization for depression and use of antidepressant medication [9,10]. Psychosocial distress among men with PC may potentially lead to higher risk of suicide. The largest meta-analysis to date reported a twofold higher risk of suicide within 1 yr after PC diagnosis but was unable to assess longer-term risks [11]. Most studies of depression and suicide risks among PC survivors have lacked sufficient sample sizes and/or follow-up time to estimate long-term (≥5 yr) risks and delineate the highest-risk subgroups who might benefit the most from intervention. Large population-based cohorts are needed for well-powered assessments of long-term mental health outcomes, susceptible time periods, and high-risk subgroups among PC survivors.
We sought to address these knowledge gaps using nationwide data from Sweden. Our goals were to: (1) determine the risks of major depression and death by suicide associated with aggressive and low- or intermediate-risk PC in a large population-based cohort; (2) identify periods of heightened risk after PC diagnosis; and (3) assess for age-specific differences. We hypothesized that aggressive PC is associated with higher long-term risks of major depression and suicide among men of all ages.
2. Patients and methods
2.1. Study population and PC ascertainment
In the National Prostate Cancer Register (NPCR) of Sweden, we identified 183 495 men who were diagnosed with PC during 1998–2017. The NPCR has captured 98% of all incident PC cases since 1998 according to comparison to the Swedish National Cancer Register, to which reporting is mandated by law [12]. The NPCR contains data on cancer characteristics including tumor grade according to Gleason score; disease stage according to the tumor, node, metastasis (TNM) classification; and prostate-specific antigen (PSA) level at diagnosis. We excluded 3306 men (2%) for whom data were missing for any of these characteristics, leaving 180 189 men (98%) for analysis.
PC risk groups were defined at the time of diagnosis according to the criteria in the National Comprehensive Cancer Network practice guidelines [12,13]. Low-risk PC was defined as clinical stage T1–2, Gleason score 2–6, and PSA <10 ng/ml; intermediate-risk PC was defined as clinical stage T1–2 with Gleason score 7 and/or PSA of 10 to <20 ng/ml. High-risk PC was defined as clinical stage T3–4, Gleason score ≥8, and/or PSA ≥20 ng/ml at the time of diagnosis, and was further stratified as locally advanced (stage T3 and PSA 20 to <50 ng/ml), very advanced/regionally metastatic (stage T4 and/or N1 and/or PSA 50 to <100 ng/ml in the absence of distant metastases [M0 or Mx]), or distant metastases (stage M1 and/or PSA <100 ng/ml) [12,13]. Primary treatment within 6 mo after diagnosis was also identified from the NPCR. Androgen deprivation therapy (ADT) was further identified using Anatomical Therapeutic Chemical codes L02AE (gonadotropin-releasing hormone [GnRH] analogs), L02BB (antiandrogens), and L02BX (other hormone antagonists) in the Swedish Prescribed Drug Register, which contains all medication prescriptions dispensed nationwide since July 1, 2005. ADT use was modeled in a time-dependent manner as a yes/no variable according to the earliest prescription date, and subanalyses examined GnRH analogs versus monotherapy with antiandrogens separately.
Each PC case was matched to ten men randomly sampled from the general population who had the same birth year and month and were living in Sweden on the date of PC diagnosis for the corresponding case (ie, the index date). This study was approved by the Regional Ethical Review Board in Lund, Sweden. Participant consent was not required because the study used only pseudonymized registry-based secondary data.
2.2. Major depression and suicide ascertainment
The primary outcomes were (1) earliest diagnosis of major depression and (2) death by suicide, which were ascertained from the index date (PC diagnosis date for each case) up to December 31, 2018. Major depression was identified using International Classification of Diseases, 10th revision (ICD-10) codes F32–F33 in the Swedish In-Patient and Out-Patient Registers and primary care records. The earliest available source of these diagnoses was the In-Patient Register, which contains all primary and secondary hospital discharge diagnoses, with 86% coverage of the Swedish population starting in 1973 and 100% coverage since 1987 [14]. Psychiatric diagnoses in this register are highly reliable, with most positive predictive values in the 85–95% range [14]. In addition, the Swedish Out-Patient Register contains all diagnoses from specialty clinics nationwide starting in 2001. Primary care diagnoses previously collected by our group [15] were also used to identify major depression, and were available for 20% of the Swedish population starting in 1998, 45% starting in 2001, and 90% starting in 2008 and onwards. The validity of major depression diagnoses in these data sources is supported by their prevalence, sex ratio, and sibling and twin correlations [15,16].
Death by suicide was identified using nationwide data from the Swedish Cause of Death Register, which includes deaths and ICD codes for cause of death among all persons registered in Sweden, with compulsory reporting nationwide. All intentional deaths were identified using ICD-10 codes X60–X84, and deaths of undetermined intent were identified using ICD-10 codes Y10–Y34. Prior studies have indicated that many suicide deaths are misclassified as deaths of undetermined intent [17]. In the present study, intentional deaths and deaths of undetermined intent were analyzed together in the primary analysis and separately in a sensitivity analysis.
2.3. Covariates
Other characteristics that may be associated with PC and depression or suicide were identified using Swedish national census and health registry data, which are linked using a pseudonymous personal identification number. Covariates included birth date (continuous and categorical by decade), birth country (Sweden/other), marital status (married/not married), education level (≤9, 10–12, >12 yr), income (quartiles), region (large cities, other/Southern, other/Northern, unknown), Charlson comorbidity index (0, 1, ≥2) [18], and history of bipolar disorder, schizophrenia, anxiety disorder, or major depression at the index date (each modeled as a separate covariate). The Charlson comorbidity index was included because comorbidities are common among men with PC and are associated with higher risks of depression and suicide [19] independently of other known risk factors. Psychiatric disorders were ascertained from the Swedish In-Patient and Out-Patient Registers and primary care records using ICD-10 codes (bipolar disorder: F31; schizophrenia: F20; anxiety disorder: F40–F42; major depression: F32–F33). Data for all covariates were >96% complete. Missing data were modeled as a separate category and had little effect on risk estimates because of their rarity.
2.4. Statistical analysis
Cox regression was used to compute hazard ratios (HRs) and 95% confidence intervals (CIs) for major depression and death by suicide associated with PC diagnosis while stratifying on matched sets. The observation period for each study participant (PC cases and their matched controls) began at the index date (ie, date of PC diagnosis for the respective case) and ended at the date of the respective outcome (ie, earliest registration of major depression or suicide death, examined in separate models) or December 31, 2018, whichever came first. In analyses of major depression, men were censored at the date of death as identified in the Swedish Death Register (n = 537 484) or the date of emigration as determined by absence of a Swedish residential address in census data (n = 11 458). In analyses of suicide death, men were censored at the date of death from other causes (n = 574 483) or of emigration (n = 11 707). All analyses were adjusted for covariates (as defined above). In a secondary analysis, we also explored the association between PC and “new-onset” major depression (ie, excluding 8275 [5%] PC cases and 91107 [5%] controls who had a prior diagnosis of major depression before the index date).
The proportional hazards assumption was evaluated by testing for interaction between PC status and follow-up time and by examining log-log survival plots. For suicide death, the time interaction term was nonsignificant (p = 0.14) and no substantial departure from proportional hazards was found. For major depression, the time interaction term was statistically significant (p = 0.01), but the departure from proportional hazards was minor, as illustrated in log-log plots (Supplementary Fig. 1). Thus, the HR from a model that includes the entire follow-up period represents an average HR over time. To assess periods of heightened susceptibility during the follow-up period, HRs also were estimated within narrower time intervals after PC diagnosis (<3 and 3 to <12 mo; 1 to <2, 2 to <5, 5 to <10, and ≥10 yr) in separate landmark analyses (ie, among men still at risk of the outcome at the beginning of the respective interval). In addition, the outcomes were examined after stratifying on primary treatment modality (ADT only, radiation with or without adjuvant ADT, surgery, or both radiation and surgery), modeled in a time-dependent manner using treatment data available during 2005–2017, in comparison to controls. Age-specific differences were assessed by stratifying on age at the index date (<55, 55–64, 65–74, 75–84, ≥85 yr) while adjusting for age as a continuous variable within each stratum.
In exploratory analyses, we assessed for interactions between PC and other covariates in relation to major depression or suicide death, which potentially could reveal other subgroups of PC survivors who are more susceptible to these outcomes. We also examined associations between high-risk PC and major depression or suicide death after stratifying on calendar year of PC diagnosis (1998–2004, 2005–2009, 2010–2017). All statistical tests were two-sided and used a significance level of 0.05. All analyses were conducted using Stata v15.1.
3. Results
Among 180 189 men with PC, 56% had low- or intermediate-risk disease and 44% had high-risk disease. Among those with low- or intermediate-risk disease, the median age at PC diagnosis was 67.4 yr (interquartile range [IQR] 62.1–72.9) and median follow-up was 7.1 yr (IQR 3.8–11.2). Among all men with high-risk disease, the median age at PC diagnosis was 75.0 yr (IQR 68.3–81.1) and median follow-up was 4.3 yr (IQR 2.0–8.0). Men with distant metastases had a median age of 76.8 yr (IQR 69.8–82.7) at PC diagnosis and median follow-up of 2.6 yr (IQR 1.3–5.0).
Over 8.0 million person-years of follow-up, a total of 164 608 men (with or without PC) were diagnosed with major depression and 2728 died by suicide. At 10-yr follow-up, the cumulative incidence of major depression and suicide death was 7.9% and 0.2% among men with PC, and 5.8% and 0.1% among control men, respectively. The median ages at diagnosis of major depression or death by suicide were 72.8 and 72.1 yr for men with low- or intermediate-risk PC, 79.1 and 79.3 yr for men with high-risk PC, and 74.0 and 72.8 yr, respectively, for control subjects. The median follow-up time was 6.7 yr (IQR 3.3–11.1) among all men who were not diagnosed with major depression and 7.7 yr (IQR 4.0–12.2) among all men who did not die.
Table 1 shows the characteristics of PC cases, controls, and all men diagnosed with major depression or who died by suicide. Men with PC were more likely than controls to be Swedish-born, married, and/or to have multiple comorbidities. Men with high-risk PC had lower education or income levels than controls, whereas men with low- or intermediate-risk PC had higher education or income levels. In addition, men diagnosed with major depression were more likely to have two or more comorbidities, and those who died by suicide were more likely to be unmarried or have low education or income.
Table 1 –
Characteristics of the study participants, 1998–2018, Sweden
| Men by group, n (%) | |||||
|---|---|---|---|---|---|
| High-risk PC | LR/IR PC | Control subjects | Major depression | Suicide death | |
| (n = 78 951) | (n = 101 238) | (n = 1 801 890) | (n = 164 608) | (n = 2728) | |
| Age at index date | |||||
| <55 yr | 1372 (1.7) | 5728 (5.7) | 71 000 (3.9) | 6861 (4.1) | 146 (5.3) |
| 55–64 yr | 10 791 (14) | 32 406 (32) | 431 970 (24) | 36 052 (22) | 811 (29) |
| 65–74 yr | 27 258 (35) | 45 054 (45) | 723 120 (40) | 66 235 (40) | 1062 (38) |
| 75–84 yr | 30 272 (38) | 16 356 (16) | 466 280 (26) | 49 752 (30) | 655 (24) |
| ≥85 yr | 9258 (12) | 1694 (1.7) | 109 520 (6.1) | 8931 (5.3) | 109 (3.9) |
| Sweden-born | 72 846 (92) | 92 334 (91) | 1 573 042 (87) | 148 796 (89) | 2490 (91) |
| Marital status | |||||
| Married | 54 933 (70) | 72 080 (71) | 1 141 069 (63) | 111 875 (67) | 1446 (52) |
| Not married | 24 018 (30) | 29 157 (29) | 606 285 (34) | 55 944 (33) | 1337 (48) |
| Unknown | 0 (0.0) | 1 (<0.1) | 54 536 (3.0) | 12 (<0.1) | 0 (0.0) |
| Education (years) | |||||
| ≤9 | 37 659 (48) | 32 615 (32) | 748 594 (42) | 70 187 (42) | 1356 (49) |
| 10–12 | 27 165 (34) | 40 885 (40) | 648 123 (36) | 62 465 (37) | 993 (36) |
| >12 | 14 117 (18) | 27 727 (27) | 355 450 (20) | 35 119 (21) | 434 (16) |
| Unknown | 10 (<0.1) | 11 (<0.1) | 49 723 (2.8) | 60 (<0.1) | 0 (0.0) |
| Income (quartile) | |||||
| 1st quartile (highest) | 15 832 (20) | 39 920 (39) | 468 355 (26) | 34 232 (20) | 396 (14) |
| 2nd quartile | 21 091 (27) | 28 529 (28) | 462 783 (26) | 47 648 (28) | 648 (23) |
| 3rd quartile | 22 291 (28) | 20 252 (20) | 438 894 (24) | 49 874 (30) | 960 (35) |
| 4th quartile (lowest) | 19 694 (25) | 12 481 (12) | 359 227 (20) | 35 462 (21) | 773 (28) |
| Unknown | 43 (0.1) | 56 (0.1) | 72 631 (4.0) | 615 (0.4) | 6 (0.2) |
| Region | |||||
| Large city | 34 100 (43) | 53 073 (52) | 825 039 (46) | 94 652 (56) | 1279 (46) |
| Other/Southern | 29 884 (38) | 33 257 (33) | 618 625 (34) | 49 704 (30) | 1033 (37) |
| Other/Northern | 14 957 (19) | 14 899 (15) | 310 444 (17) | 23 448 (14) | 468 (17) |
| Unknown | 10 (<0.1) | 9 (<0.1) | 47 782 (2.7) | 27 (<0.1) | 3 (0.1) |
| CCI | |||||
| 0 | 54 987 (70) | 77 632 (77) | 1 397 984 (78) | 121 086 (74) | 2075 (76) |
| 1 | 9210 (12) | 12 953 (13) | 224 985 (12) | 20 877 (13) | 387 (14) |
| ≥2 | 14 754 (19) | 10 653 (11) | 178 921 (9.9) | 22 645 (14) | 266 (9.8) |
| Prior diagnoses | |||||
| Bipolar disorder | 346 (0.4) | 626 (0.6) | 11 708 (0.6) | 4563 (2.7) | 93 (3.3) |
| Schizophrenia | 247 (0.3) | 235 (0.2) | 11 808 (0.7) | 1229 (0.7) | 61 (2.2) |
| Anxiety disorder | 2814 (3.6) | 4370 (4.3) | 81 331 (4.5) | 24 322 (15) | 327 (12) |
| Major depression | 3167 (4.0) | 5108 (5.1) | 91 107 (5.1) | 46 101 (28) | 409 (15) |
CCI = Charlson comorbitity index; LR/IR = low-risk or intermediate-risk; PC = prostate cancer.
3.1. PC and major depression
Men diagnosed with high-risk PC had a 1.8-fold higher relative rate of major depression across the entire follow-up period (adjusted HR [aHR] 1.82, 95% CI 1.75–1.89; Table 2).
Table 2 –
Relative rates of major depression up to 2018 among men diagnosed with PC (1998–2017) in comparison to matched control subjects, stratified by time since index date or by PC treatment
| Major depression (n) | Adjusted modela | |||
|---|---|---|---|---|
| PC cases | Controls | HR (95% CI) | p value | |
| High-risk PCb | ||||
| Entire follow-up period | 6490 | 68 231 | 1.82 (1.75–1.89) | <0.001 |
| <3 mo | 541 | 11 600 | 2.02 (1.73–2.36) | <0.001 |
| 3 to <12 mo | 1067 | 6133 | 2.08 (1.89–2.29) | <0.001 |
| 1 to <2 yr | 1031 | 6547 | 2.21 (2.02–2.43) | <0.001 |
| 2 to <5 yr | 1784 | 15 309 | 1.84 (1.72–1.97) | <0.001 |
| 5 to <10 yr | 1461 | 17 600 | 1.57 (1.46–1.69) | <0.001 |
| ≥10 yr | 606 | 11 042 | 1.40 (1.24–1.58) | <0.001 |
| High-risk PC (2005–2017)c | ||||
| ADT only | 2231 | − | 2.02 (1.89–2.16) | <0.001 |
| Radiation | 1009 | − | 1.44 (1.31–1.57) | <0.001 |
| Surgery | 228 | − | 1.60 (1.31–1.95) | <0.001 |
| Radiation and surgery | 125 | − | 1.56 (1.20–2.03) | 0.001 |
| LR/IR PCb | ||||
| Entire follow-up period | 9644 | 80 243 | 1.19 (1.16–1.23) | <0.001 |
| <3 mo | 769 | 12 982 | 1.23 (1.08–1.40) | 0.002 |
| 3 to <12 mo | 1385 | 8 680 | 1.37 (1.26–1.49) | <0.001 |
| 1 to <2 yr | 1225 | 8 388 | 1.28 (1.18–1.39) | <0.001 |
| 2 to <5 yr | 2421 | 18 403 | 1.13 (1.06–1.19) | <0.001 |
| 5 to <10 yr | 2490 | 20 337 | 1.18 (1.11–1.25) | <0.001 |
| ≥10 yr | 1354 | 11 453 | 1.09 (1.01–1.18) | 0.04 |
| LR/IR PC (2005–2017)c | ||||
| No initial treatment | 3477 | − | 1.08 (1.03–1.13) | 0.003 |
| ADT only | 1055 | − | 1.69 (1.53–1.86) | <0.001 |
| Radiation | 1071 | − | 1.09 (1.00–1.19) | 0.06 |
| Surgery | 606 | − | 0.98 (0.88–1.10) | 0.78 |
| Radiation and surgery | 158 | − | 1.05 (0.85–1.30) | 0.65 |
ADT = androgen deprivation therapy; CI = confidence interval; HR = hazard ratio; LR/IR = low-risk or intermediate-risk; PC = prostate cancer.
Adjusted for age, country of birth, marital status, education, income, region, Charlson comorbidity index, and prior history of psychiatric disorders (bipolar disorder, schizophrenia, anxiety disorder, major depression) at the index date.
In separate models, the outcome was examined across the entire follow-up period and within narrower time intervals after PC diagnosis.
Subanalyses based on treatment data available during 2005–2017.
This increase was similar among men with locally advanced disease (aHR 1.71, 95% CI 1.64–1.79), very advanced/regionally metastatic disease (aHR 2.11, 95% CI 1.94–2.30), or distant metastases (aHR 2.01, 95% CI 1.82–2.23; Supplementary Table 1). The relative rate of major depression peaked at 1–2 yr after diagnosis with high-risk PC (aHR 2.21, 95% CI 2.02–2.43) but persisted even ≥10 yr after diagnosis (aHR 1.40, 95% CI 1.24–1.58; Table 2). By contrast, men with low- or intermediate-risk PC had only a modestly higher relative rate of major depression across the entire follow-up period (aHR 1.19, 95% CI 1.16–1.23). Men with high-risk PC had higher relative rates of major depression regardless of PC treatment, but with significant heterogeneity (p < 0.001; Table 2). Those treated with radiation (aHR 1.44, 95% CI 1.31–1.57) or surgery (aHR 1.60, 95% CI 1.31–1.95) had lower relative rates than those treated with ADT (aHR 2.02, 95% CI 1.89–2.16; p < 0.001 and p = 0.03, respectively, for comparisons with ADT). The relative rate of major depression was higher among those treated with GnRH analogs (aHR 2.15, 95% CI 2.00–2.31) than with antiandrogen monotherapy (aHR 1.52, 95% CI 1.30–1.79; p < 0.001 for difference in HRs). Among men with low- or intermediate-risk PC, the relative rate of major depression was substantially higher only among those treated with ADT alone (aHR 1.69, 95% CI 1.53–1.86), especially with GnRH analogs (aHR 1.83, 95% CI 1.61–2.08), in comparison to antiandrogen monotherapy (aHR 1.52, 95% CI 1.31–1.76; p = 0.06 for difference in HRs). In a secondary analysis, new-onset major depression was assessed by excluding men with a prior diagnosis of major depression before the index date (8275 [5%] PC cases and 91 107 [5%] control subjects). Most HRs were slightly attenuated but remained significantly elevated (Supplementary Table 2). Across the entire follow-up period, the aHR for new-onset major depression associated with high-risk PC was 1.45 (95% CI 1.40–1.51).
3.2. PC and suicide death
Men diagnosed with high-risk PC had a 2.4-fold higher relative rate of death by suicide across the entire follow-up period (aHR 2.43, 95% CI 2.01–2.95; Table 3). Within the first 2 yr after diagnosis with high-risk PC, the relative rate of suicide death was similar among men with locally advanced disease (aHR 2.71, 95% CI 1.81–4.07), very advanced/regionally metastatic disease (aHR 2.34, 95% CI 1.22–4.46), or distant metastases (aHR 2.74, 95% CI 1.47–5.09; Supplementary Table 3). The relative rate of suicide death had bimodal peaks at <3 mo (aHR 3.60, 95% CI 1.60–8.07) and ≥10 yr (aHR 3.51, 95% CI 1.56–7.90) after diagnosis with high-risk PC (Table 3). By contrast, men with low- or intermediate-risk PC had a higher relative rate of suicide death only at 3–12 mo after PC diagnosis (aHR 1.88, 95% CI 1.11–3.18) but not across the entire follow-up period (aHR 1.02, 95% CI 0.84–1.25). Figure 1 shows aHRs and 95% CIs for major depression or suicide death by time since the index date, fitted using spline curves.
Table 3 –
Relative rates of suicide death up to 2018 among men diagnosed with PC (1998–2017) in comparison to matched control subjects, stratified by time since the index date or by PC treatment
| Suicide deaths (n) | Adjusted modela | |||
|---|---|---|---|---|
| PC cases | Controls | HR (95% CI) | p value | |
| High-risk PCb | ||||
| Entire follow-up period | 184 | 917 | 2.43 (2.01–2.95) | <0.001 |
| <3 mo | 13 | 55 | 3.60 (1.60–8.07) | 0.002 |
| 3 to <12 mo | 29 | 148 | 2.45 (1.47–4.08) | 0.001 |
| 1 to <2 yr | 35 | 174 | 2.78 (1.77–4.38) | <0.001 |
| 2 to <5 yr | 56 | 314 | 2.54 (1.79–3.59) | <0.001 |
| 5 to <10 yr | 36 | 189 | 1.91 (1.25–2.93) | 0.003 |
| ≥10 yr | 15 | 37 | 3.51 (1.56–7.90) | 0.002 |
| High-risk PC (2005–2017)c | ||||
| ADT only | 40 | − | 2.83 (1.80–4.43) | <0.001 |
| Radiation | 12 | − | 1.08 (0.55–2.10) | 0.83 |
| LR/IR PCb | ||||
| Entire follow-up period | 154 | 1473 | 1.02 (0.84–1.25) | 0.83 |
| <3 mo | 11 | 69 | 1.83 (0.82–4.06) | 0.14 |
| 3 to <12 mo | 27 | 171 | 1.88 (1.11–3.18) | 0.02 |
| 1 to <2 yr | 18 | 223 | 0.87 (0.49–1.53) | 0.63 |
| 2 to <5 yr | 41 | 486 | 0.82 (0.57–1.20) | 0.31 |
| 5 to <10 yr | 47 | 424 | 1.04 (0.72–1.49) | 0.84 |
| ≥10 yr | 10 | 100 | 0.70 (0.33–1.48) | 0.35 |
| LR/IR PC (2005–2017)c | ||||
| Deferred treatment | 45 | − | 1.02 (0.71–1.47) | 0.92 |
| ADT only | 10 | − | 1.05 (0.47–2.33) | 0.90 |
| Radiation | 9 | − | 0.53 (0.25–1.12) | 0.10 |
ADT = androgen deprivation therapy; CI = confidence interval; HR = hazard ratio; LR/IR = low-risk or intermediate-risk; PC = prostate cancer.
Adjusted for age, country of birth, marital status, education, income, region, Charlson comorbidity index, and prior history of psychiatric disorders (bipolar disorder, schizophrenia, anxiety disorder, major depression) at the index date.
In separate models, the outcome was examined across the entire follow-up period and within narrower time intervals after PC diagnosis.
Subanalyses based on treatment data available during 2005–2017.
Fig. 1 –
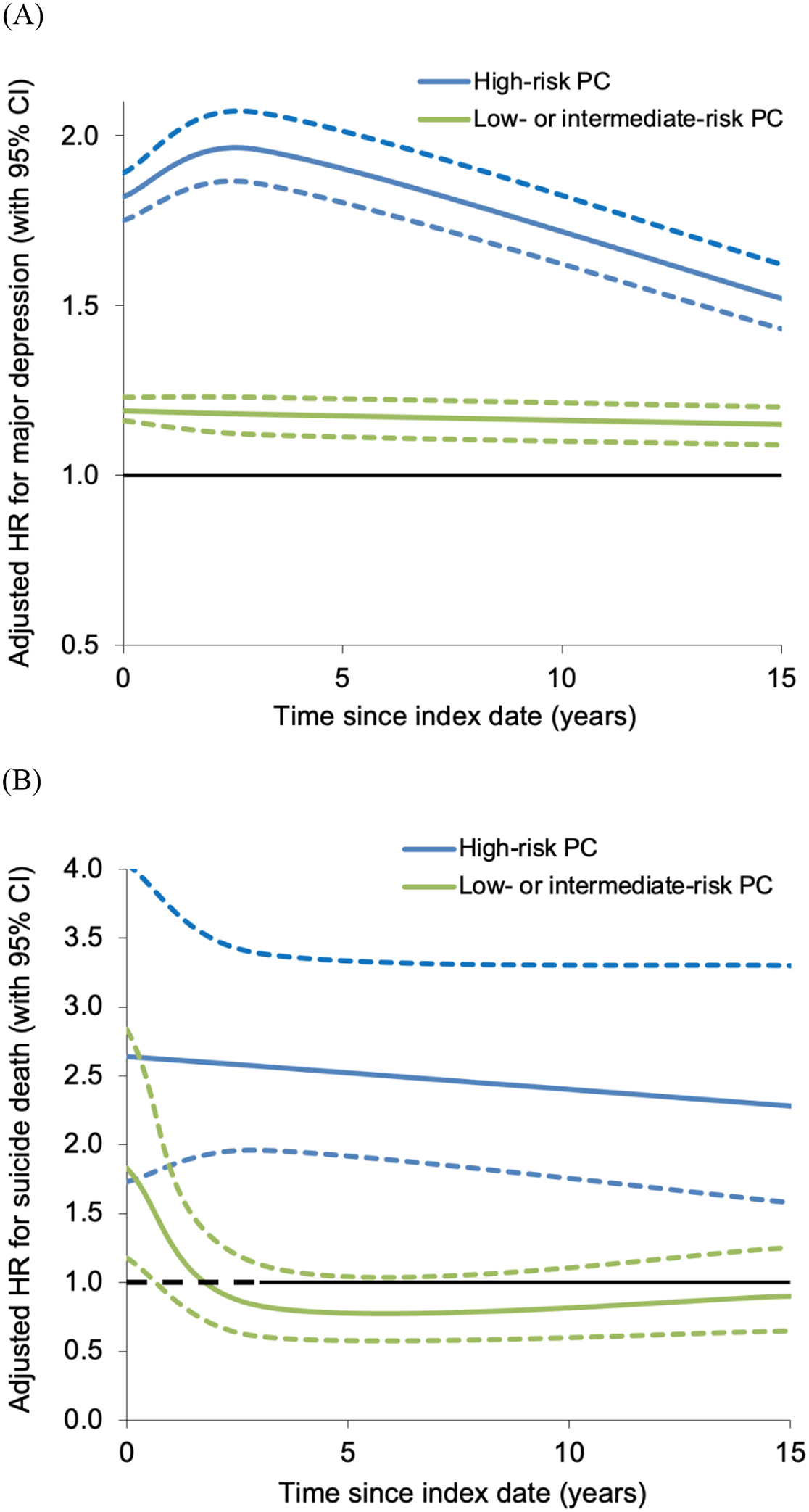
Adjusted hazard ratios (HRs) for (A) major depression and (B) suicide death associated with high-risk prostate cancer (PC) or low- to intermediate-risk PC by time since index date, 1998–2018, Sweden. CI = confidence interval.
The relative rate of suicide death varied significantly by PC treatment (p < 0.001). High-risk PC was associated with a higher relative rate of suicide death only among men treated with ADT alone (aHR 2.83, 95% CI 1.80–4.43), and not those treated with radiation (aHR 1.08, 95% CI 0.55–2.10; p = 0.02 for comparison with ADT; Table 3). All other treatment categories had fewer than five suicide deaths, which were too few for analysis. Men with low- or intermediate-risk PC did not have a higher relative rate of suicide death, regardless of primary treatment.
Among all men who died by suicide, 28% of those with PC and 24% of control subjects had a prior diagnosis of major depression during the follow-up period. Among men with PC who died by suicide, those who lacked a prior diagnosis of major depression were more likely to have the lowest education level (51% vs 41%; p < 0.001) or be in the lowest income quartile (30% vs 20%; p < 0.001), and were nonsignificantly less likely to be married (45% vs 49%; p = 0.12) in comparison to men previously diagnosed with major depression.
3.3. Age-specific differences
Significant interactions were found between PC status and age in relation to either major depression or suicide death (p < 0.01 for each). High-risk PC was associated with higher relative rates of major depression regardless of age at PC diagnosis, but the rates were higher at ages ≥65 yr and especially ≥75 yr (Table 4). Low- or intermediate-risk PC was associated with higher relative rates of major depression only for ages ≥65 yr at PC diagnosis, and the rates were highest at ages ≥75 yr (Supplementary Table 4).
Table 4 –
Relative rates of major depression or suicide death among men diagnosed with high-risk PC (1998–2017) in comparison to matched control subjects, stratified by age at the index date
| Age at index date | Men with the outcome (n) | Adjusted modela | ||
|---|---|---|---|---|
| PC cases | Controls | HR (95% CI) | p value | |
| Major depression | ||||
| <55 yr | 148 | 1162 | 1.54 (1.25–1.88) | <0.001 |
| 55–64 yr | 968 | 8301 | 1.58 (1.45–1.73) | <0.001 |
| 65–74 yr | 2226 | 23 455 | 1.73 (1.62–1.84) | <0.001 |
| 75–84 yr | 2533 | 28 635 | 1.98 (1.86–2.10) | <0.001 |
| ≥85 yr | 615 | 6678 | 2.21 (1.94–2.52) | <0.001 |
| Suicide death | ||||
| <55 yr | 5 | 19 | 2.23 (0.73–6.83) | 0.16 |
| 55–64 yr | 23 | 186 | 1.42 (0.88–2.31) | 0.15 |
| 65–74 yr | 62 | 327 | 2.79 (1.97–3.94) | <0.001 |
| 75–84 yr | 74 | 319 | 2.68 (1.96–3.68) | <0.001 |
| ≥85 yr | 20 | 66 | 4.36 (2.06–9.22) | <0.001 |
CI = confidence interval; HR = hazard ratio; PC = prostate cancer.
Adjusted for age, country of birth, marital status, education, income, region, Charlson comorbidity index, and prior history of psychiatric disorders (bipolar disorder, schizophrenia, anxiety disorder, major depression) at the index date.
High-risk PC was associated with significantly higher relative rates of suicide death only among men diagnosed at ages ≥65 yr, but analyses were limited by small numbers of suicide deaths at younger ages (Table 4). By contrast, across the entire follow-up period, men with low- or intermediate-risk PC did not have higher relative rates of suicide death regardless of age at diagnosis (Supplementary Table 4). Supplementary Figure 2 shows aHRs for major depression or suicide death associated with high-risk PC by age at the index date.
3.4. Other secondary analyses
Exploratory analyses to assess interactions with other covariates revealed positive additive and multiplicative interactions between high-risk PC and low education level in relation to major depression (p < 0.001 for each; Supplementary Table 5). High-risk PC had a positive multiplicative (but not additive) interaction with low income (p < 0.001), negative additive and multiplicative interactions with being foreign-born or unmarried (p ≤ 0.02 for each), and a negative multiplicative (but not additive) interaction with Charlson comorbidity index ≥2 (p < 0.001) in relation to major depression. No interactions were found between high-risk PC and any covariates in relation to suicide death.
Stratifying on year of PC diagnosis, the relative rates of major depression and suicide death were lower among men diagnosed with high-risk PC in 2010–2017 in comparison to earlier years (1998–2009; Supplementary Table 6), which corresponds to a shift towards earlier stage at diagnosis in later years.
In a sensitivity analysis that assessed confirmed suicides (n = 2402) and deaths of undetermined intent (n = 326) separately, PC was significantly associated with both outcomes with relative rates of similar magnitude. The aHR was 2.48 (95% CI 2.03–3.01; p < 0.001) for confirmed suicide associated with high-risk PC and 2.35 (95% CI 1.63–3.60; p < 0.001) for deaths of undetermined intent.
4. Discussion
In this large population-based cohort, men with high-risk PC had an approximately 80% higher relative rate of major depression and more than twofold higher relative rate of death by suicide in comparison to men without PC, after adjusting for sociodemographic factors and comorbidity burden. These relative rates remained elevated even ≥10 yr after PC diagnosis. Men with high-risk PC had a higher relative rate of major depression regardless of PC treatment, but the relative rate of suicide death was higher only among those treated with ADT alone. High-risk PC was more strongly associated with major depression and suicide death among older men (≥75 yr). By contrast, men with low- or intermediate-risk PC had a modestly higher relative rate of major depression (1.2-fold) and a higher relative rate of suicide death (1.9-fold) only at 3–12 mo after PC diagnosis, but not across the entire follow-up period.
To the best of our knowledge, this is the first study to examine the long-term (≥5 yr) risks of both major depression and death by suicide in association with PC in a large population-based cohort. Most prior studies of depression among PC survivors have had small samples of <300 PC patients with <2 yr of follow-up [8]. A meta-analysis of 27 studies with a pooled sample size of 4494 (average study size of 158 men) reported 15–18% prevalence of clinically significant depression among men with PC [8]. A study of 72 613 PC survivors and 217 839 control subjects in Sweden also reported that men with PC had higher risks of hospitalization for depression (HR 1.29, 95% CI 1.14–1.45) and antidepressant medication use (odds ratio [OR] 1.65, 95% CI 1.54–1.77) [9]. A study of 12 082 PC survivors and 57 127 control subjects in Canada reported higher odds of antidepressant use up to 5 yr after treatment with surgery (OR 1.49, 95% CI 1.35–1.64) or radiation (OR 1.33, 95% CI 1.21–1.47), but not active surveillance [10]. A Surveillance, Epidemiology and End Results-Medicare study of 50 856 men with localized PC and 2–7 yr of follow-up reported that 20% developed mental illness (a composite of depression, anxiety, or suicide), but did not include a comparison group [20].
A higher risk of suicide within 1 yr after PC diagnosis has been reported in some [21–27] but not all [28,29] studies. A meta-analysis of eight studies with a pooled sample size of 1 281 393 men with PC and 842 294 control subjects reported a twofold higher risk of suicide within 1 yr after PC diagnosis (relative risk 2.01, 95% CI 1.52–2.64), with the highest risk among men aged ≥75 yr, but was unable to assess longer-term risks [11]. Another meta-analysis reported that men with PC had pooled prevalence of 5.8% for depressive disorders (655,149 PC patients in 11 studies) and 9.9% for suicidal ideation (6173 PC patients in 8 studies) [30].
The present study extends prior evidence by examining long-term risks of major depression, suicide death, and periods of heightened risk associated with PC risk groups in a large population-based cohort. The findings show substantially higher relative rates of major depression and suicide death for men with high-risk PC, which persisted for ≥10 yr after PC diagnosis. These associations were stronger among older men (≥75 yr), consistent with several prior studies [11,20,31]. We also found higher relative rates among men treated with ADT, consistent with a meta-analysis that reported an association between ADT use and depression, even among men with localized disease [32]. Men with low- or intermediate-risk PC had a higher rate of suicide death within the first year after PC diagnosis, but not later. Most men with PC who died by suicide, especially those of low socioeconomic status, had no prior diagnosis of depression, suggesting underdiagnosis and the importance of clinical assessment for depression among PC patients. Fortunately, despite higher relative rates of suicide death, only a small percentage (0.2%) of PC patients experienced this outcome, and 9% of PC patients overall were diagnosed with major depression.
These findings add to prior evidence that PC survivors may suffer psychosocial distress that worsens quality of life [33] and long-term health outcomes [8,11,30,31,34]. Depression not only imposes a psychological burden but also has other health consequences such as treatment nonadherence [35], higher use of emergency services [36], and higher risk of suicide [21–26]. The American Cancer Society has previously recommended periodic screening (at least annually) for psychosocial distress and depression in all men with PC [35]. More recently, the US Preventive Services Task Force recommended routine screening for depression in the general adult population, while emphasizing that patients with cancer are at higher risk [37]. Unfortunately, such screening is not consistently implemented and remains underutilized [35]. Our findings underscore the importance of long-term screening [38] for psychosocial distress and depression among PC survivors of all ages. Older men and those with a low education level or who lack social support may particularly be at higher risk [20,26,39]. Patients with a positive screen need prompt referral for psychiatric treatment, followed by close monitoring for treatment adherence for both their mental and physical health. It has been reported that interventions among PC survivors with psychosocial distress improve quality of life [40], and routine screening and referral have been effective in reducing psychosocial distress over time [41].
4.1. Strengths and limitations
A key strength of the present study is its large national cohort design, which provided the high statistical power needed to examine PC risk groups and narrowly defined periods of susceptibility. Clinical diagnoses from all health care settings, including primary care, allowed more complete ascertainment of major depression, thus allowing more valid risk estimates based on a national population. We were able to assess long-term relative rates of both major depression and suicide death while controlling for multiple potential confounders. Previously reported incidence rates for depression and suicide are comparable between Sweden and the USA [15,42,43].
The study also has several limitations. Major depression diagnoses were identified using nationwide ICD codes, and more detailed clinical data were unavailable for validation. However, the validity of ICD codes is supported by their prevalence, sex ratio, sibling and twin correlations, and associations with well-documented psychosocial risk factors [15,16]. Depression is often undiagnosed, and such cases could not be identified in this study.
However, the inclusion of diagnoses from primary care settings, where most depression is diagnosed and treated [15], allowed more complete capture than in prior studies. As in other large population-based studies, the reporting of suicides also involves some misclassification. However, data available on intentional deaths and deaths of undetermined intent allowed separate analyses of these outcomes in a sensitivity analysis, which showed little difference in risk estimates. Lastly, our study was limited to one country and will need replication in other diverse populations when feasible.
5. Conclusions
In this large population-based cohort, men diagnosed with high-risk PC had substantially higher rates of major depression and death by suicide relative to men without PC. These relative rates remained elevated for ≥10 yr after PC diagnosis. Men with low- or intermediate-risk PC had a modestly higher relative rate of major depression and a higher relative rate of suicide death within the first year after PC diagnosis, but not later. PC survivors need close clinical monitoring for timely detection and treatment of psychosocial distress and depression.
Supplementary Material
Acknowledgments:
This project was made possible by the continuous work of the National Prostate Cancer Register of Sweden steering group: David Robinson (register holder), Ingela Franck Lissbrant (chair), Johan Styrke (co-chair), Johan Stranne, Jon Kindblom, Camilla Thellenberg, Andreas Josefsson, Ingrida Verbiene, Hampus Nugin, Stefan Carlsson, Anna Kristiansen, Mats Andén, Thomas Jiborn, Olof Ståhl, Olof Akre, Per Fransson, Eva Johansson, Magnus Törnblom, Fredrik Jäderling, Marie Hjälm Eriksson, Lotta Renström, Jonas Hugosson, Ola Bratt, Maria Nyberg, Fredrik Sandin, Camilla Byström, Mia Brus, Mats Lambe, Anna Hedström, Nina Hageman, Christofer Lagerros, and the patient representatives Hans Joelsson and Gert Malmberg.
Financial disclosures:
Casey Crump certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor:
This work was supported by the National Cancer Institute (R01 CA269553 to C.C., K.S., and W.S.); the National Institute on Alcohol Abuse and Alcoholism (R01 AA027522 to A.C.E. and K.S.) at the National Institutes of Health; the Swedish Research Council; and an ALF project grant (Region Skåne/Lund University, Sweden). The funding agencies had no direct role in the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Cancer facts & figures 2020. Atlanta, GA: American Cancer Society; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin 2019;69:363–85. [DOI] [PubMed] [Google Scholar]
- 4.Pitman A, Suleman S, Hyde N, Hodgkiss A. Depression and anxiety in patients with cancer. BMJ 2018;361:k1415. [DOI] [PubMed] [Google Scholar]
- 5.Fervaha G, Izard JP, Tripp DA, Rajan S, Leong DP, Siemens DR. Depression and prostate cancer: a focused review for the clinician. Urol Oncol 2019;37:282–8. [DOI] [PubMed] [Google Scholar]
- 6.Baumeister H, Hutter N, Bengel J, Harter M. Quality of life in medically ill persons with comorbid mental disorders: a systematic review and meta-analysis. Psychother Psychosom 2011;80:275–86. [DOI] [PubMed] [Google Scholar]
- 7.Baumeister H, Balke K, Harter M. Psychiatric and somatic comorbidities are negatively associated with quality of life in physically ill patients. J Clin Epidemiol 2005;58:1090–100. [DOI] [PubMed] [Google Scholar]
- 8.Watts S, Leydon G, Birch B, et al. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open 2014;4:e003901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bill-Axelson A, Garmo H, Nyberg U, et al. Psychiatric treatment in men with prostate cancer—results from a nation-wide, population-based cohort study from PCBaSe Sweden. Eur J Cancer 2011;47:2195–201. [DOI] [PubMed] [Google Scholar]
- 10.Matta R, Wallis CJD, Goldenberg MG, et al. Variation and trends in antidepressant prescribing for men undergoing treatment for nonmetastatic prostate cancer: a population-based cohort study. Eur Urol 2019;75:3–7. [DOI] [PubMed] [Google Scholar]
- 11.Guo Z, Gan S, Li Y, et al. Incidence and risk factors of suicide after a prostate cancer diagnosis: a meta-analysis of observational studies. Prostate Cancer Prostat Dis 2018;21:499–508. [DOI] [PubMed] [Google Scholar]
- 12.Van Hemelrijck M, Wigertz A, Sandin F, et al. Cohort profile: the National Prostate Cancer Register of Sweden and Prostate Cancer Data Base Sweden 2.0. Int J Epidemiol 2013;42:956–67. [DOI] [PubMed] [Google Scholar]
- 13.Mohler J, Bahnson RR, Boston B, et al. NCCN clinical practice guidelines in oncology: prostate cancer. J Natl Compr Cancer Netw 2010;8:162–200. [DOI] [PubMed] [Google Scholar]
- 14.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sundquist J, Ohlsson H, Sundquist K, Kendler KS. Common adult psychiatric disorders in Swedish primary care where most mental health patients are treated. BMC Psychiatry 2017;17:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kendler KS, Ohlsson H, Lichtenstein P, Sundquist J, Sundquist K. The genetic epidemiology of treated major depression in Sweden. Am J Psychiatry 2018;175:1137–44. [DOI] [PubMed] [Google Scholar]
- 17.Bjorkenstam C, Johansson LA, Nordstrom P, et al. Suicide or undetermined intent? A register-based study of signs of misclassification. Popul Health Metr 2014;12:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ludvigsson JF, Appelros P, Askling J, et al. Adaptation of the Charlson comorbidity index for register-based research in Sweden. Clin Epidemiol 2021;13:21–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crump C, Sundquist K, Sundquist J, Winkleby MA. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychol Med 2014;44:279–89. [DOI] [PubMed] [Google Scholar]
- 20.Ravi P, Karakiewicz PI, Roghmann F, et al. Mental health outcomes in elderly men with prostate cancer. Urol Oncol 2014;32:1333–40. [DOI] [PubMed] [Google Scholar]
- 21.Bill-Axelson A, Garmo H, Lambe M, et al. Suicide risk in men with prostate-specific antigen-detected early prostate cancer: a nationwide population-based cohort study from PCBaSe Sweden. Eur Urol 2010;57:390–5. [DOI] [PubMed] [Google Scholar]
- 22.Carlsson S, Sandin F, Fall K, et al. Risk of suicide in men with low-risk prostate cancer. Eur J Cancer 2013;49:1588–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dalela D, Krishna N, Okwara J, et al. Suicide and accidental deaths among patients with non-metastatic prostate cancer. BJU Int 2016;118:286–97. [DOI] [PubMed] [Google Scholar]
- 24.Fall K, Fang F, Mucci LA, et al. Immediate risk for cardiovascular events and suicide following a prostate cancer diagnosis: prospective cohort study. PLoS Med 2009;6:e1000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fang F, Keating NL, Mucci LA, et al. Immediate risk of suicide and cardiovascular death after a prostate cancer diagnosis: cohort study in the United States. J Natl Cancer Inst 2010;102:307–14. [DOI] [PubMed] [Google Scholar]
- 26.Smith DP, Calopedos R, Bang A, et al. Increased risk of suicide in New South Wales men with prostate cancer: analysis of linked population-wide data. PLoS One 2018;13:e0198679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Llorente MD, Burke M, Gregory GR, et al. Prostate cancer: a significant risk factor for late-life suicide. Am J Geriatr Psychiatry 2005;13:195–201. [DOI] [PubMed] [Google Scholar]
- 28.Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med 2004;164:1179–84. [DOI] [PubMed] [Google Scholar]
- 29.Klaassen Z, Wallis CJD, Chandrasekar T, et al. Cancer diagnosis and risk of suicide after accounting for prediagnosis psychiatric care: a matched-cohort study of patients with incident solid-organ malignancies. Cancer 2019;125:2886–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brunckhorst O, Hashemi S, Martin A, et al. Depression, anxiety, and suicidality in patients with prostate cancer: a systematic review and meta-analysis of observational studies. Prostate Cancer Prostat Dis 2021;24:281–9. [DOI] [PubMed] [Google Scholar]
- 31.Prasad SM, Eggener SE, Lipsitz SR, Irwin MR, Ganz PA, Hu JC. Effect of depression on diagnosis, treatment, and mortality of men with clinically localized prostate cancer. J Clin Oncol 2014;32:2471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nead KT, Sinha S, Yang DD, Nguyen PL. Association of androgen deprivation therapy and depression in the treatment of prostate cancer: a systematic review and meta-analysis. Urol Oncol 2017;35:664.e1–9. [DOI] [PubMed] [Google Scholar]
- 33.Zenger M, Lehmann-Laue A, Stolzenburg JU, Schwalenberg T, Ried A, Hinz A. The relationship of quality of life and distress in prostate cancer patients compared to the general population. Psychosoc Med. 2010;7:Doc02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klaassen Z, Wallis CJD, Goldberg H, et al. The impact of psychiatric utilisation prior to cancer diagnosis on survival of solid organ malignancies. Br J Cancer 2019;120:840–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skolarus TA, Wolf AM, Erb NL, et al. American Cancer Society prostate cancer survivorship care guidelines. CA Cancer J Clin 2014;64:225–49. [DOI] [PubMed] [Google Scholar]
- 36.Jayadevappa R, Malkowicz SB, Chhatre S, Johnson JC, Gallo JJ. The burden of depression in prostate cancer. Psychooncology 2012;21:1338–45. [DOI] [PubMed] [Google Scholar]
- 37.Siu AL, US Preventive Services Task Force, Bibbins-Domingo K, et al. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA 2016;315:380–7. [DOI] [PubMed] [Google Scholar]
- 38.Klaassen Z, Arora K, Wilson SN, et al. Decreasing suicide risk among patients with prostate cancer: Implications for depression, erectile dysfunction, and suicidal ideation screening. Urol Oncol 2018;36:60–6. [DOI] [PubMed] [Google Scholar]
- 39.Friberg AS, Rask Moustsen I, Benzon Larsen S, et al. Educational level and the risk of depression after prostate cancer. Acta Oncol 2019;58:722–9. [DOI] [PubMed] [Google Scholar]
- 40.Badger TA, Segrin C, Figueredo AJ, et al. Psychosocial interventions to improve quality of life in prostate cancer survivors and their intimate or family partners. Qual Life Res 2011;20:833–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carlson LE, Groff SL, Maciejewski O, Bultz BD. Screening for distress in lung and breast cancer outpatients: a randomized controlled trial. J Clin Oncol 2010;28:4884–91. [DOI] [PubMed] [Google Scholar]
- 42.Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health 2008;29:115–29. [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization. Global Health Observatory data repository: suicide rate estimates, age-standardized. Geneva, Switzerland: WHO; 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


