Abstract
Introduction:
Irritable bowel syndrome (IBS) is a common disorder of gut-brain interaction, characterized by symptoms of abdominal pain and changes in bowel habits. It often co-occurs with extra-intestinal somatic and psychological symptoms. However, the nature of the inter-relationships among these symptoms is unclear. Although prior studies have noted age differences in IBS prevalence and specific symptom severity, it remains unknown whether specific symptoms and symptom relationships may differ by age.
Methods:
Symptom data were collected in 355 adults with IBS (mean age 41.4 years, 86.2% female). Network analysis was used to examine the inter-relationships among 28 symptoms and to identify the core symptoms driving the symptom structure between young (≤ 45 years) versus older (> 45 years) adults with IBS. We evaluated three network properties between the two age groups: network structure, edge (connection) strength, and global strength.
Results:
In both age groups, fatigue was the top core symptom. Anxiety was a second core symptom in the younger but not the older age group. Intestinal gas and/or bloating symptoms also exerted considerable influences in both age groups. The overall symptom structure and connectivity were found to be similar regardless of age.
Conclusion:
Network analysis suggests fatigue is a critical target for symptom management in adults with IBS, regardless of age. Comorbid anxiety is likely an important treatment focus for young adults with IBS. Rome V Criteria update could consider the importance of intestinal gas and bloating symptoms. Additional replication with larger diverse IBS cohorts is warranted to verify our results.
Keywords: Irritable Bowel Syndrome, Network Analysis, Age Difference, Symptoms
INTRODUCTION
Irritable bowel syndrome (IBS) is a common disorder of gut-brain interaction (DGBI), characterized by chronic, recurrent abdominal pain/discomfort associated with defecation or a change in bowel habits (1). Currently, the pathophysiology of IBS is considered heterogeneous with interacting biological, psychological and environmental factors contributing to fluctuations in symptoms and their severity. A significant subgroup of individuals with IBS also experience a variety of co-morbid symptoms some of which are considered gastrointestinal (e.g., nausea, bloating) but others such as fatigue, anxiety, poor sleep, headache, and backache may represent a more systemic pathophysiology, that may be related to hypervigilance, increased pain sensitivity and/or mood (2). Unmasking the inter-relationships among the full range of symptoms profiles in persons with IBS may assist in the development of precision interventions.
Although the overlap between IBS abdominal pain and bowel symptoms and other symptoms in individuals with IBS is acknowledged, the nature of these relationships (i.e., unidirectional or bidirectional) is not well understood. Cluster analysis, factor analysis and principal component analysis are common analytic methods used to classify “clustering” symptoms, that is, certain symptoms cluster together due to a shared underlying mechanism (3). Han et al. (4) used an exploratory factor analysis to classify 26 symptoms in people with IBS; 6 symptom clusters (abdominal pain/gas, extra‐intestinal somatic pain, psychological distress, upper gastrointestinal, fatigue/miscellaneous, and diarrhea/urgency) were identified. While these analytic methods provide an understanding of how IBS symptoms may cluster together, whether these symptoms interconnect and which symptoms are most influential remains unanswered.
A novel method to assess the complex phenomena of a symptom-based condition is network analysis which is a graphical statistical approach to visualize the relationships among multiple variables (5, 6). This approach provides an alternative way to visualize symptom relationships and determine central (core) symptoms which are hypothesized to drive or maintain the network (3, 6). Investigating symptom networks in IBS can help elucidate which symptoms are most influential and potentially provide a new avenue for the development and/or refinement of symptom management strategies. Furthermore, there is the potential that age-related differences may contribute to differences in symptom reports. For instance, age-related changes occur in motility, visceral sensitivity, and gut microbiota composition, perhaps driven (in women) by decreases in ovarian hormones (7–10). Prior studies also have noted age-related differences in IBS prevalence and specific symptom severity (11–14). When using an age cutoff of 45 years, it was found that postmenopausal women had greater symptom severity and poorer quality of life compared to premenopausal women (11). Thus, there is a need to examine the impact of symptom network structures based on age.
Therefore, the first aim of the study was to investigate through network visualization the relationships among IBS abdominal pain and bowel symptoms, extra-intestinal somatic, and psychological symptoms and to determine core symptoms of persons with IBS. The second aim was to examine whether core symptoms and symptom relationships vary by age. Better understanding of age differences in core symptoms and symptom relationships potentially can provide insight into age-specific symptom interventions.
METHODS
Design and participants
This secondary data analysis used symptom diary data over 28 consecutive days from baseline data collection from two randomized controlled trials (Cohort I and II) and a cross-sectional study (Cohort III) among adults with IBS who were recruited through both community-based advertisements and mailings to patients in a university-based gastroenterology practice in the pacific northwest (United States). The procedures and methods of these studies are reported in detail elsewhere (15–17). The current analysis included a total sample of 355 adults with a healthcare provider diagnosis of IBS (Cohort I = 224, Cohort II = 108, Cohort III = 23). Further details are provided in the Supplementary Methods.
Measures
The daily symptom diary was initially based on the Washington Women’s Health Diary (18). Symptoms were modified to include gastrointestinal symptoms. The daily diary listed 28 symptoms, i.e., IBS (abdominal pain, diarrhea, constipation), other gastrointestinal (pain after eating, abdominal distension, bloating, intestinal gas, flatulence, urgency, cramping, nausea, heartburn, stomach pain), somatic (fatigue, sleepiness, diminished sleep quality, unrefreshed sleep, hard to concentrate, backache, headache, joint/muscle pain) and mood (anxiety, depressive mood, stress, anger, decreased talk and/or move, panic). Every evening, participants recorded the severity of symptoms over the past 24 hours for 28 days (over one menstrual cycle for women, 4 weeks for men). Symptoms were aggregated as the percent of symptomatic days during 28-day diary data collection and higher scores representing greater symptom severity and frequency (4, 19–21). Further details are provided in the Supplementary Methods.
Statistical analyses
We used RStudio version 3.6.1 to conduct the statistical analyses in four phases: network estimation, network inference, network stability and network comparison. All p-values were two-tailed and < 0.05 were considered statistically significant.
Networks estimation and visualization
Regularized partial correlation networks were used through the application of graphical least absolute shrinkage and selection operator (LASSO) algorithm to estimate and visualize IBS symptom networks under the RStudio qgraph package (22). The components of network models include the nodes (i.e., symptoms included in the analysis) and edges (i.e., links/connections between nodes). Each edge reflects a weighted correlation between two nodes after conditioning all of the other nodes in the network, ranging from −1 to 1. We used the graphical LASSO algorithm in combination with the Extended Bayesian Information Criterion (EBIC) to remove spurious or false positive correlations (edges) from the models in order to make the estimated network models more robust and interpretable. In the network model graph, thicker and more saturated edges reflect stronger partial correlations between nodes. Furthermore, we chose the Fruchterman-Reingold algorithm to layout the networks that places strongly connected nodes together, and weakly connected nodes apart (23, 24).
Network inference
We used the RStudio qgraph package to estimate the strength centrality to gain the insight into the extent of a node’s connection to other nodes, as highly connected nodes were considered to have high importance in the network. Strength centrality is presented as a standardized z-scored index, and reflects how strong a specific node is directly connected to other nodes through calculating by the sum of the absolute values of the edge weights connecting a specific node (25, 26).
Network stability
We used non-parametric bootstrapping methods to examine network stability before interpreting the estimated networks. Specifically, we performed RStudio bootnet package with α = 0.05 based on 1,000 bootstrap iterations to calculate correlation stability (CS) coefficients of strength centrality which range between 0 and 1 and higher values indicate greater stability. To interpret a symptom network, CS coefficients above 0.5 are preferred, while the values below 0.25 are unstable and error-prone (27). Further, we performed bootstrapped difference tests to evaluate statistical significances between two node strength or edge weights.
Network comparisons
We used the network comparison test (NCT) with 1,000 replications under the RStudio NetworkComparisonTest package (28) to compare IBS symptom network properties those aged > 45 years compared to those aged ≤ 45 years. Age > 45 years was selected as the cut-off because it is considered the time at onset of menopausal transition for many women (29) and previous IBS literature indicating symptom differences between pre and postmenopausal women (11). The NCT is a two-tailed permutation test to examine whether significant differences exist between two network structures on the three aspects: network structure, edge (connection) strength, and global strength (28). Further details are provided in the Supplementary Methods.
RESULTS
Participant and symptom characteristics
A sample of 355 adults with IBS were included for these analyses. The mean age of the total sample was 41.4 ± 14.5 years and 86.2% were females. Of these participants, 147 participants were aged > 45 years (41.4%), and 208 participants were aged ≤ 45 years (58.6%). As shown in Table 1, the older subgroup reported a greater symptom severity on intestinal gas, joint pain, muscle pain and diminished sleep quality, while a lower symptom severity on nausea, stomach pain and decreased desire to talk/move than those in the young subgroup.
Table 1.
Overview of Participant Characteristics and 28 Included Symptoms in Adults with Irritable Bowel Syndrome
| Variables | Symptom abbreviation | All participants (n=355) |
Older participants (n=147) |
Young participants (n=208) |
p a | |
|---|---|---|---|---|---|---|
|
| ||||||
| Female gender, n (%) | 304 (86.2%) | 131 (89.1) | 175 (84.1) | .212 | ||
| Age in years, Mean (SD) | 41.4 (14.5) | 56.5 (6.7) | 30.7 (7.3) | < 0.001 | ||
|
| ||||||
| Individual symptom severity | Mean (SD) | Mean (SD) | Mean (SD) | |||
|
| ||||||
| Abdominal painb | AbdPn | 38.0 (26.3) | 36.1 (26.8) | 39.3 (26.0) | .251 | |
| Pain after eatingb | PnEat | 29.9 (25.8) | 28.1 (26.9) | 31.1 (25.1) | .285 | |
| Abdominal distensionb | AbdDist | 31.2 (31.9) | 35.0 (33.5) | 28.4 (30.4) | .059 | |
| Bloatingb | Bloat | 33.4 (30.7) | 36.8 (32.4) | 31.0 (29.2) | .083 | |
| Constipationb | Const | 21.3 (24.1) | 20.4 (23.8) | 21.9 (24.3) | .572 | |
| Intestinal gasb | Gas | 38.8 (30.1) | 44.1 (31.5) | 35.0 (28.5) | .005 | |
| Flatulenceb | Flatu | 42.5 (30.2) | 45.6 (30.6) | 40.2 (29.8) | .102 | |
| Backacheb | Backache | 16.3 (23.8) | 18.1 (25.1) | 15.1 (22.8) | .237 | |
| Headacheb | Headache | 13.6 (18.7) | 12.3 (18.4) | 14.4 (19.0) | .299 | |
| Joint painb | JointPn | 14.7 (24.3) | 23.5 (29.4) | 8.1 (17.0) | < 0.001 | |
| Muscle painb | MusclePn | 17.0 (25.0) | 23.9 (30.0) | 12.2 (19.3) | < 0.001 | |
| Anxietyb | Anx | 19.9 (23.3) | 19.2 (23.7) | 20.4 (23.1) | .636 | |
| Depressive moodb | Depress | 10.4 (18.0) | 9.5 (17.8) | 11.0 (18.1) | .441 | |
| Stressb | Stress | 26.6 (26.0) | 24.5 (24.6) | 28.1 (26.9) | .198 | |
| Heartburnb | Heartburn | 7.3 (16.2) | 8.7 (18.4) | 6.4 (14.4) | .180 | |
| Nauseab | Nausea | 8.8 (15.7) | 6.0 (12.7) | 10.8 (17.2) | .004 | |
| Stomach painb | StomPn | 22.5 (25.1) | 19.1 (22.7) | 25.1 (26.4) | .026 | |
| Angerb | Anger | 7.6 (13.7) | 6.4 (14.0) | 8.6 (13.5) | .151 | |
| Decreased desire to talk/moveb | DecTalk | 11.2 (16.2) | 9.1 (14.93) | 12.8 (16.9) | .035 | |
| Fatigueb | Fatig | 35.1 (27.5) | 36.6 (29.5) | 34.0 (26.0) | .386 | |
| Hard to concentrateb | HardConc | 14.7 (21.9) | 14.3 (22.4) | 15.0 (21.6) | .769 | |
| Panicb | Panic | 6.4 (14.6) | 5.0 (12.3) | 7.5 (16.1) | .109 | |
| Sleepyb | Sleepy | 27.5 (26.6) | 25.7 (26.4) | 28.8 (26.6) | .287 | |
| Diarrheab | Diarr | 15.7 (20.3) | 14.3 (20.7) | 16.6 (19.9) | .296 | |
| Urgencyb | Urgency | 19.7 (23.2) | 17.5 (23.0) | 21.3 (23.2) | .137 | |
| Crampingb | Cramp | 10.9 (17.2) | 9.0 (16.6) | 12.3 (17.5) | .067 | |
| Diminished sleep qualityc | SQ | 41.0 (27.1) | 44.9 (29.2) | 38.2 (25.2) | .021 | |
| Unrefreshed sleepd | Refres | 49.1 (27.2) | 51.7 (29.2) | 47.1 (25.5) | .125 | |
p values for testing differences of descriptive characteristics between older (> 45 years) and young (≤ 45 years) participants, calculated by independent t test or χ2test.
Means (SDs) for each symptom severity were defined as the percentage of days rated as “moderate” to “very severity” of each symptom severity over 28 days.
Means (SDs) for diminished sleep quality were defined as the percentage of days rated as “poor” to “fair” sleep quality over 28 days.
Mean (SD) for unrefreshed sleep were defined as the percentage of days rated as “not at all refreshed” or “somewhat refreshed” sleep over 28 days.
Network models and centrality
Supplementary Figure S1 shows the estimated networks of 28 symptoms in the combined sample (A), in the young (B) and older subgroups (C), respectively. Strength CS coefficient was 0.67, 0.29, and 0.44 for the combined sample, and the older and young subgroups, respectively. All of strength CS coefficients in the three networks were above the acceptable threshold of 0.25, suggesting strength index was relatively stable in all networks.
Core symptoms between young and older adults with IBS
Figure 1 shows the standardized values of strength centrality in the combined sample (A), in young (B) and older (C) subgroups, respectively. In the combined sample, the top five symptoms with strength centrality were: fatigue, anxiety, abdominal pain, intestinal gas and hard to concentrate (Figure 1A). As shown in Figure 2A, when comparing the values of strength centrality between symptoms in the combined sample, fatigue and anxiety did not significantly differ, but the strength centrality of fatigue was significantly higher than the other symptoms.
Figure 1.
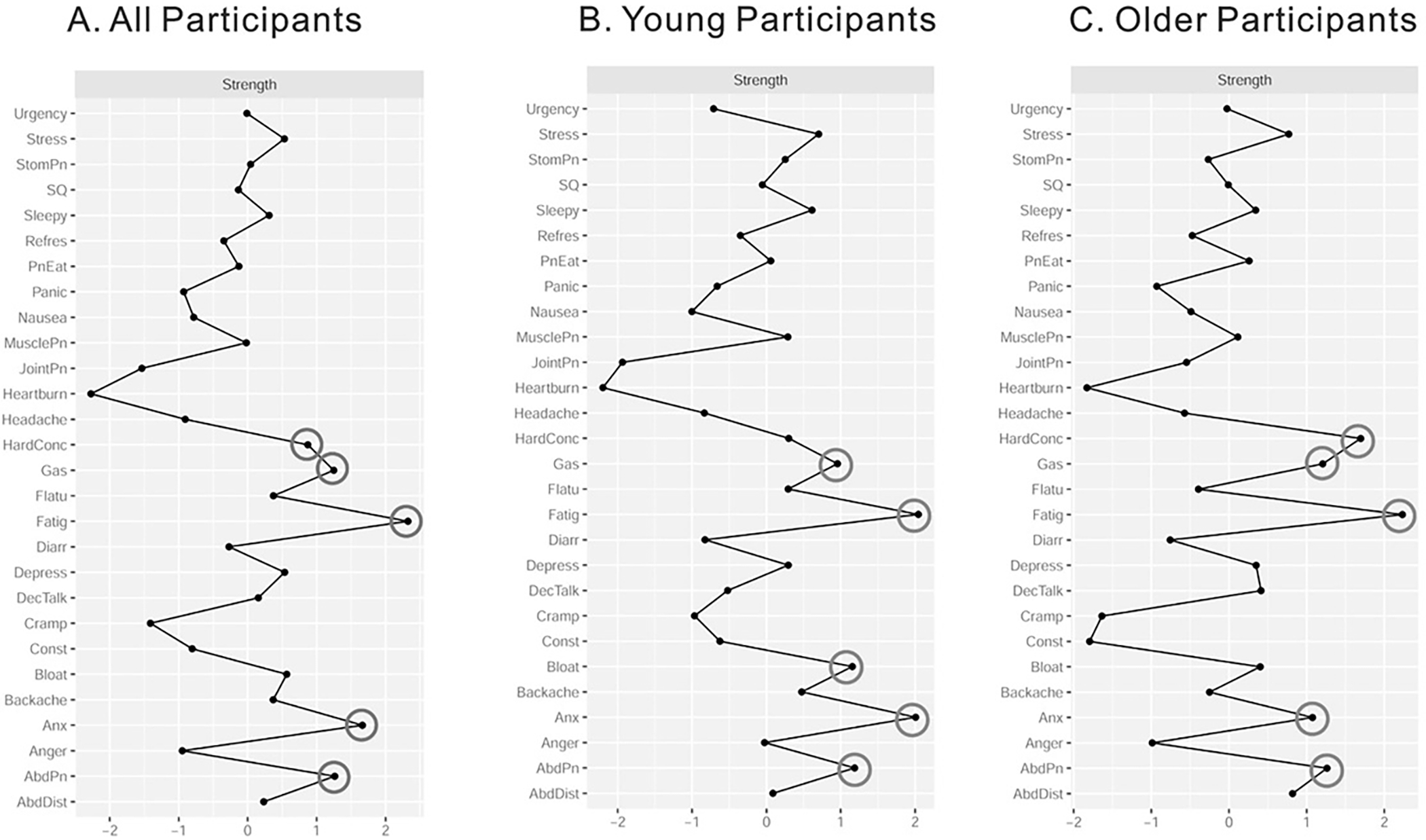
Standardized values z-scores of strength centrality for 28 symptoms in all participants (1A), young participants (1B) and older participants (1C), respectively. Higher standardized strength values indicate greater strength. Gray circles denote the top 5 core symptoms within a network. AbdPn = abdominal pain; PnEat = pain after eating; AbdDist = abdominal distension; Bloat = bloating; Const = constipation; Gas = intestinal gas; Flatu = flatulence; JointPn = joint pain; MusclePn = muscle pain; Anx = anxiety; Depress = depressive mood; StomPn = Stomach pain; DecTalk = decreased desire to talk/move; Fatig = fatigue; HardConc = hard to concentrate; Diarr = diarrhea; Cramp = cramping; SQ = diminished sleep quality; and Refres = unrefreshed sleep.
Figure 2.
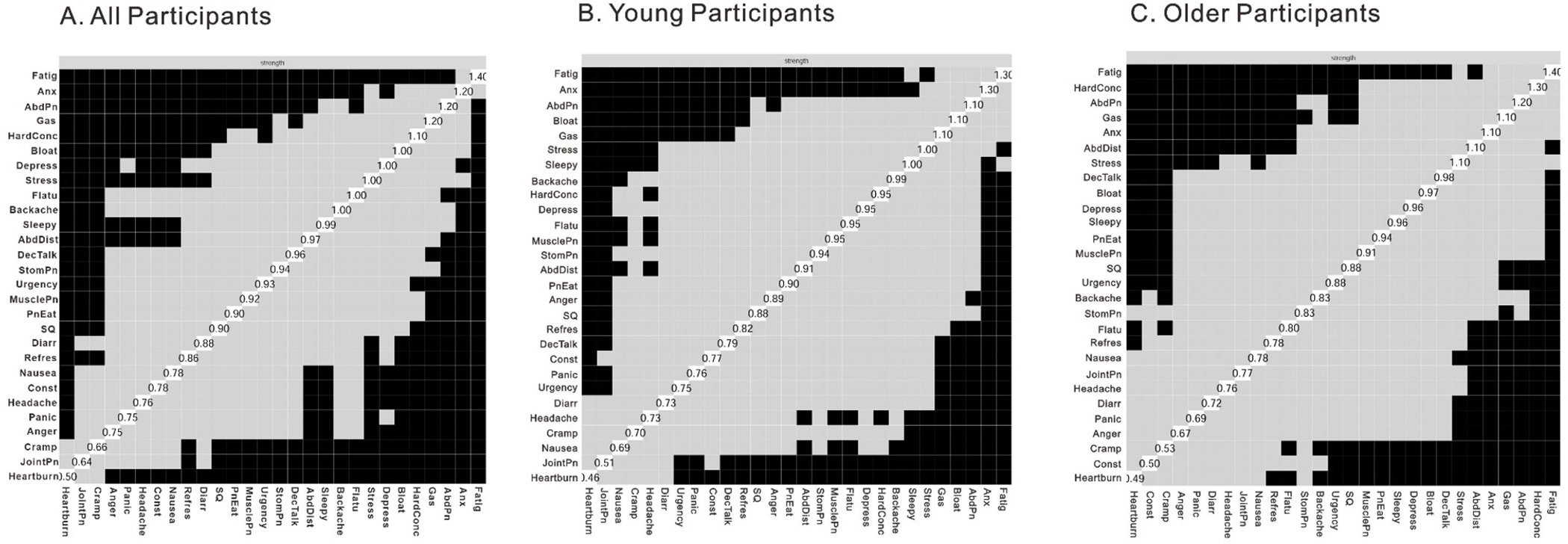
Bootstrapped strength difference results in all participants (2A), young participants (2B) and older participants (2C), respectively. Note. Values on the diagonal indicate the unstandardized strength values for each symptom. Black boxes indicate significant strength differences, meaning that the bootstrapped strength difference 95 % confidence interval does not span 0. Gray boxes indicate nonsignificant strength differences, meaning that the bootstrapped strength difference 95 % confidence interval spans 0.
For the young subgroup, the top five symptoms with the greatest strength centrality were: fatigue, anxiety, abdominal pain, bloating, and intestinal gas (Figure 1B). As shown in Figure 2B, when comparing the values of strength centrality between symptoms in the young subgroup, fatigue, anxiety, abdominal pain, bloating, and intestinal gas did not significantly differ from one another; but in addition to fatigue, anxiety was significantly higher than the other symptoms.
For the older subgroup, the top five symptoms with the greatest strength centrality in were: fatigue, hard to concentrate, abdominal pain, intestinal gas and anxiety (Figure 1C). As shown in Figure 2C, when comparing the values of strength centrality between symptoms in the older subgroup, fatigue, hard to concentrate, abdominal pain, intestinal gas, anxiety and stress did not significantly differ from one another, but the strength centrality of fatigue was significantly higher than the other symptoms.
Network comparison
We examined the differences between older and young subgroups regarding the network structure of symptoms and its global strength. As shown in Table 2, the omnibus test of network structure invariance revealed that the overall networks were not different across the two age groups (all p-values > 0.05). The network comparison test for global strength invariance also showed no significant age group difference in global strength of the network connectivity (all p-values > 0.05). These results suggest that the global connections and the overall relationships among IBS symptoms seemed to be similar between older and young participants with IBS.
Table 2.
Global Characteristics of the Estimated Networks and Network Comparison Results by Age Group
| All participants (n=355) |
Older participants (n=147) |
Young participants (n=208) |
Network1 vs. 2 | Network 1 vs. 3 |
Network 2 vs. 3 |
|
|---|---|---|---|---|---|---|
|
| ||||||
| Global strength | 13.38 | 12.74 | 12.74 | |||
| Top 5 most central nodes (strength centrality) | Fati (2.23) | Fati (2.23) | Fati (2.04) | |||
| Anx (1.66) | HardConc (1.70) | Anx (2.01) | ||||
| AbdPn (1.26) | AbdPn (1.26) | AbdPn (1.19) | ||||
| Gas (1.25) | Gas (1.21) | Bloat (1.15) | ||||
| HardConc (0.87) | Anx (1.08) | Gas (0.96) | ||||
| NCT results | ||||||
| Omnibus test of network structure invariance p-value | ~ 1.000 | 0.979 | 0.867 | |||
| Global strength invariance test p-value | 0.471 | 0.356 | 0.907 | |||
Note See Table 1 for symptom abbreviation; NCT = network comparison test; Network 1 = all participants; Network 2 = older (> 45 years) participants; Network 3 = young (≤ 45 years) participants.
Subgroup Analysis
We also considered the potential role of gender by comparing the core symptoms and the network structure among women only versus all participants that included both women and men. Results are presented in the Supplemental Table and do not significantly differ from the core symptoms and the network structure among all participants.
DISCUSSION
To the best of our knowledge, this is the first study using network analysis to visualize symptoms among individuals with IBS and test core symptoms and symptom relationships between young versus older adults with IBS based on 28-day diary data. In both young (aged ≤ 45 years) and older adults (aged > 45 years) with IBS, fatigue was the top core symptom (quantitatively assessed by strength centrality) among the 28 symptoms including IBS symptoms of abdominal pain, diarrhea and constipation, other gastrointestinal, extra-intestinal somatic and psychological symptoms. However, for young adults with IBS, not only fatigue but also anxiety exhibited greater influence than other symptoms in the network structure. In addition, our network analysis suggests the overall symptom structure and the connectivity of symptoms remain invariant in adults with IBS, regardless of age.
Core symptoms of IBS in young and older adults
Our study found fatigue to be the most influential symptom among 28 symptoms commonly reported by the young and older adults with IBS. This finding aligns with previous studies showing fatigue as one of the most common and distressing non-gastrointestinal symptoms in adults living with IBS (30–33). For example, Piche et al. (33) reported that almost two-thirds of 51 patients with IBS (mean age = 53.7 years, 78.4% female) experience fatigue, 51% viewed fatigue as distressing as their gastrointestinal symptoms, and 17.4% considered fatigue their worst symptom. Lackner et al. (30) found in a sample of 107 IBS patients (mean age = 41.0 years, 78.4% female) that fatigue was less severe than abdominal pain and more frequent bowel movements. In addition, in a larger sample (n = 234, mean age =41 years, 78% female), adjusting for selected demographic (e.g., age, gender, education level) and clinical variables (e.g., duration of IBS, IBS subtype), fatigue was more strongly associated with patients’ health perceptions than IBS symptom severity (34). While it has been repeatedly shown that fatigue is a major symptom for those with IBS, its significance in terms of pathophysiology or impact on treatment outcomes remains understudied. Inflammatory markers such as cytokines have been hypothesized to be one pathophysiologic factor in IBS and also linked fatigue in other populations. However, elevations in pro-inflammatory cytokines have not been consistently found in IBS studies (35). Fatigue may also be subsequent to pain and toileting efforts. On the other hand, IBS may be a consequence of fatigue (36). This current study extends prior work in IBS population by examining the statistical index of strength centrality of 28 co-occurring symptoms in IBS, and further shows fatigue as a core symptom necessitating further study as to whether it is an outcome of IBS or a contributing risk factor.
In addition to fatigue, our results also found anxiety exerted a considerable influence driving the symptom network structure of young adults with IBS. Comorbid anxiety and other psychological distress (i.e., stress, depression) have considered as risk factors for the presence and persistence of IBS and/or abdominal pain-related DGBI (37, 38). Stress-induced fluctuations in symptoms and their severity currently are considered to involve the bidirectional gut-brain axis (38). Psychological distress, particularly anxiety or gut specific anxiety influence visceral perception and gastrointestinal functioning through brain-to-gut pathways, which in turn worsen IBS symptoms and other gastrointestinal symptoms (38). These brain-to-gut pathways serve as core mechanisms of cognitive behavioral therapy for improving IBS symptom severity and psychological distress through modifying gut-specific maladaptive cognition, emotions and behaviors (38).
In our sample of persons with Rome II or III diagnoses, anxiety emerged a core symptom comparable to fatigue in young adults with IBS, but not in older adults with IBS. Several studies have noted age differences in exposure to daily stressors, contributing to negative and positive emotional responses (39–42). In particular, young individuals are more likely to report more frequent negative affect and anxiety during daily stressor than do older adults. Posserud et al. (43) suggested that persons with IBS tend to have more hypervigilance to gastrointestinal symptoms and negative emotional states than those with organic gastrointestinal diseases. Of note, hard to concentrate emerged as the second core symptom in older participants, as opposed to anxiety as the second core symptoms in young participants. It may reflect different expression of anxiety in older adults from young adult, that is, older adults generally may be more likely to express anxiety symptoms as somatic symptoms, including cognitive complaints, rather than psychological distress (44). Whether age plays a role in hypervigilance, daily stressor processes and/or anxiety symptom expression in IBS populations remains to be answered by future research.
Of note, intestinal gas emerged as one of the top five core symptoms in both young and older adults with IBS, and in addition, bloating was another core symptom in young adults with IBS. However, based on the Rome IV criteria the report of intestinal gas and/or bloating symptoms is not required for a diagnosis of IBS. Given the current findings regarding core symptoms in IBS identified through a network analysis approach, the Rome V Criteria update may want to consider the importance of intestinal gas and bloating symptoms.
IBS networks in young and older adults
We found similarities in the overall symptom network structure and its global strength between young and older adults. In terms of symptom visualizations, in all of the estimated symptom network structures, IBS symptoms such as abdominal pain, diarrhea, and constipation do not appear to be directly associated with other extra-intestinal somatic and psychological symptoms. This lack of a direct relationship underscores the importance of a holistic, comprehensive approach to the management of IBS. Extrapolating from this network analysis, our results suggest that bowel dysfunction pharmacotherapies alone may not directly address the numerous other symptoms that are experienced by individuals with IBS. As such, our results support the Rome Foundation Working Team’s recommendation that optimal IBS management should include pharmacotherapies in conjunction with cognitively focused behavior therapies (e.g., self-management program, cognitive-behavioral theory) that address the modifiable psychological and behavioral factors underlying gut-brain axis dysregulation (38).
Study limitations
There are several limitations in the current study. First, the network stability in terms of strength index in the older adults with IBS although acceptable was relatively low resulting from our small size of older adults with IBS (27). The majority of our community sample of the adults with IBS were females and thus we were not able to examine whether and how the core symptoms and symptom relationships in IBS would vary by gender. Therefore, additional replication in a larger and more diverse IBS sample including older adults and/or more men with IBS is warranted to verify our results. The sample size for each IBS subtype in this current study is insufficient to conduct further network analysis by IBS subtypes. Future, large IBS cohorts with the most recent IBS Rome criteria is warranted to confirm whether the core symptoms and symptom relationships vary by IBS subtypes. In this study, anxiety was measured with a diary item, reflecting a severity of worry, nervous or unease about a variety of events and situations. As Black et al. (45) suggested gastrointestinal symptom-specific anxiety may drive IBS symptom severity, additional network analysis is needed to clarify gastrointestinal-specific anxiety in the symptom network structures in adults with IBS, particularly for those aged ≤ 45 years. In this study, sleep assessment relied on sleep self report. An objective measure such as actigraphy to determine sleep duration, and/or the diagnosis of obstructive sleep apnea would provide greater insight into whether sleep is a major factor driving fatigue in IBS. The contributors to fatigue in IBS is an intriguing question bearing future research. Finally, we used a cross-sectional network analysis and the causal inferences between symptoms cannot be confirmed.
In conclusion, this study provides the visualizations of inter-relationships of 28 co-occurring symptoms by age. Network analysis results suggest fatigue is a critical target for IBS symptom management, regardless of age. Similarly, comorbid anxiety is likely important treatment target for young adults with IBS. Our findings add to current knowledge in IBS symptom management by identifying age differences in core symptoms, and sheds new insight into age-specific symptom interventions for IBS populations. Given our network analysis findings, the future Rome V Criteria update could consider the importance of intestinal gas and bloating symptoms. Additional replication in a larger sample with more men with IBS is warranted to verify our results.
Supplementary Material
Study Highlights.
WHAT IS KNOWN
IBS is characterized by symptoms of abdominal pain and changes in bowel habits, and it often co-occurs with extra-intestinal somatic and psychological symptoms.
Prior studies have also noted age-related differences in IBS prevalence and specific symptom severity.
It remains unknown whether and how specific symptoms and symptom relationships in individuals with IBS may by age.
WHAT IS NEW HERE
Network analysis is a graphical statistical approach to visualize symptom relationships and to determine core symptoms driving or maintaining the symptom network.
Network analysis suggests fatigue is the top core symptom in both young and older adults with IBS; anxiety is a second core symptom comparable to fatigue in young adults with IBS, but not in older adults with IBS.
Although intestinal gas and bloating are the core symptoms in both young and older adults with IBS, their presence is not included in the Rome IV Criteria for IBS.
The overall symptom structure and connectivity of symptoms remain constant in adults with IBS, regardless of age.
This study adds to current knowledge in IBS symptom management by investigating symptom network and identifying age differences in core symptoms, and it provides a new avenue for the development and/or refinement of age-specific symptom management strategies.
Financial support:
The parent studies included in this secondary data analysis were funded by National Institute of Nursing Research, National Institutes of Health, USA (Grant No. NR004110, NR004142 and P30 NR04001). K.J.K was funded, in part, by National Institutes of Nursing Research, National Institutes of Health, USA (Grant No. K23NR020044).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest with this publication.
REFERENCES
- 1.Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical Features, and Rome IV. Gastroenterology 2016;150:1262–1279.e2. [DOI] [PubMed] [Google Scholar]
- 2.Ohlsson B Extraintestinal manifestations in irritable bowel syndrome: A systematic review. Therap Adv Gastroenterol 2022;15:17562848221114558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris CS, Dodd M, Kober KM, et al. Advances in conceptual and methodological issues in symptom cluster research: A 20-year perspective. ANS Adv Nurs Sci 2022;45:309–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han CJ, Pike K, Jarrett ME, et al. Symptom-based latent classes of persons with irritable bowel syndrome. Res Nurs Health 2019;42:382–391. [DOI] [PubMed] [Google Scholar]
- 5.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol 2013;9:91–121. [DOI] [PubMed] [Google Scholar]
- 6.Borsboom D A network theory of mental disorders. World Psychiatry 2017;16:5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beckers AB, Wilms E, Mujagic Z, et al. Age-related decrease in abdominal pain and associated structural- and functional mechanisms: An exploratory study in healthy Individuals and irritable bowel syndrome patients. Front Pharmacol 2021;12:806002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeJong EN, Surette MG, Bowdish DME. The gut microbiota and unhealthy aging: disentangling cause from consequence. Cell Host Microbe 2020;28:180–189. [DOI] [PubMed] [Google Scholar]
- 9.O’Mahony D, O’Leary P, Quigley EM. Aging and intestinal motility: a review of factors that affect intestinal motility in the aged. Drugs Aging 2002;19:515–27. [DOI] [PubMed] [Google Scholar]
- 10.Soenen S, Rayner CK, Jones KL, et al. The ageing gastrointestinal tract. Curr Opin Clin Nutr Metab Care 2016;19:12–8. [DOI] [PubMed] [Google Scholar]
- 11.Lenhart A, Naliboff B, Shih W, et al. Postmenopausal women with irritable bowel syndrome (IBS) have more severe symptoms than premenopausal women with IBS. Neurogastroenterol Motil 2020;32:e13913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang YR, Yang WW, Liang ML, et al. Age-related symptom and life quality changes in women with irritable bowel syndrome. World J Gastroenterol 2012;18:7175–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol 2012;10:712–721. e4. [DOI] [PubMed] [Google Scholar]
- 14.Kosako M, Akiho H, Miwa H, et al. Impact of symptoms by gender and age in Japanese subjects with irritable bowel syndrome with constipation (IBS-C): a large population-based internet survey. Biopsychosoc Med 2018;12:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarrett ME, Cain KC, Barney PG, et al. Balance of autonomic nervous system predicts who benefits from a self-management intervention program for irritable bowel syndrome. J Neurogastroenterol Motil 2016;22:102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jarrett ME, Cain KC, Burr RL, et al. Comprehensive self-management for irritable bowel syndrome: randomized trial of in-person vs. combined in-person and telephone sessions. Am J Gastroenterol 2009;104:3004–3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jarrett ME, Han CJ, Cain KC, et al. Relationships of abdominal pain, reports to visceral and temperature pain sensitivity, conditioned pain modulation, and heart rate variability in irritable bowel syndrome. Neurogastroenterol Motil 2016;28:1094–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitchell ES, Woods NF. Symptom experiences of midlife women: observations from the Seattle Midlife Women’s Health Study. Maturitas 1996;25:1–10. [DOI] [PubMed] [Google Scholar]
- 19.Hertig VL, Cain KC, Jarrett ME, et al. Daily stress and gastrointestinal symptoms in women with irritable bowel syndrome. Nurs Res 2007;56:399–406. [DOI] [PubMed] [Google Scholar]
- 20.Han CJ, Jarrett ME, Heitkemper MM. Relationships between abdominal pain and fatigue with psychological distress as a mediator in women with irritable bowel syndrome. Gastroenterol Nurs 2020;43:28–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang PL, Burr RL, Buchanan DT, et al. Indirect effect of sleep on abdominal pain through daytime dysfunction in adults with irritable bowel syndrome. J Clin Sleep Med 2020;16:1701–1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Epskamp S, Cramer AOJ, Waldorp LJ, et al. qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software 2012;48:1–18. [Google Scholar]
- 23.Fruchterman TM, Reingold EM. Graph drawing by force‐directed placement. Softw Pract Exp 1991;21:1129–1164. [Google Scholar]
- 24.Papachristou N, Barnaghi P, Cooper B, et al. Network analysis of the multidimensional symptom experience of oncology. Sci Rep 2019;9:2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hevey D Network analysis: a brief overview and tutorial. Health Psychol Behav Med 2018;6:301–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol J 2016;125:747–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods 2018;50:195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Borkulo CD, van Bork R, Boschloo L, et al. Comparing network structures on three aspects: A permutation test. Psychol Methods 2022. [DOI] [PubMed] [Google Scholar]
- 29.Talaulikar V Menopause transition: Physiology and symptoms. Best Pract Res Clin Obstet Gynaecol 2022;81:3–7. [DOI] [PubMed] [Google Scholar]
- 30.Lackner JM, Gudleski GD, Dimuro J, et al. Psychosocial predictors of self-reported fatigue in patients with moderate to severe irritable bowel syndrome. Behav Res Ther 2013;51:323–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frändemark Å, Jakobsson Ung E, Törnblom H, et al. Fatigue: a distressing symptom for patients with irritable bowel syndrome. Neurogastroenterol Motil 2017;29:e12898. [DOI] [PubMed] [Google Scholar]
- 32.Han CJ, Yang GS. Fatigue in irritable bowel syndrome: A systematic review and meta-analysis of pooled frequency and severity of Fatigue. Asian Nurs Res (Korean Soc Nurs Sci) 2016;10:1–10. [DOI] [PubMed] [Google Scholar]
- 33.Piche T, Huet P-M, Gelsi E, et al. Fatigue in irritable bowel syndrome: characterization and putative role of leptin. Eur J Gastroenterol Hepatol 2007;19:237–243. [DOI] [PubMed] [Google Scholar]
- 34.Lackner JM, Gudleski GD, Thakur ER, et al. The impact of physical complaints, social environment, and psychological functioning on IBS patients’ health perceptions: looking beyond GI symptom severity. Am J Gastroenterol 2014;109:224–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martin-Viñas JJ, Quigley EM. Immune response in irritable bowel syndrome: A systematic review of systemic and mucosal inflammatory mediators. J Dig Dis 2016;17:572–581. [DOI] [PubMed] [Google Scholar]
- 36.Lakhan SE, Kirchgessner A. Gut inflammation in chronic fatigue syndrome. Nutr Metab (Lond) 2010;7:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zia JK, Lenhart A, Yang P-L, et al. Risk factors for abdominal pain–related disorders of gut–brain interaction in adults and children: A systematic review. Gastroenterology 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keefer L, Ballou SK, Drossman DA, et al. A Rome Working Team Report on Brain-Gut Behavior Therapies for Disorders of Gut-Brain Interaction. Gastroenterology 2022;162:300–315. [DOI] [PubMed] [Google Scholar]
- 39.Stawski RS, Sliwinski MJ, Almeida DM, et al. Reported exposure and emotional reactivity to daily stressors: the roles of adult age and global perceived stress. Psychol Aging 2008;23:52–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klaiber P, Wen JH, DeLongis A, et al. The ups and downs of daily life during COVID-19: age differences in affect, stress, and positive events. J Gerontol B Psychol Sci Soc Sci 2020;76:e30–e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Uchino BN, Berg CA, Smith TW, et al. Age-related differences in ambulatory blood pressure during daily stress: evidence for greater blood pressure reactivity with age. Psychol Aging 2006;21:231–9. [DOI] [PubMed] [Google Scholar]
- 42.Charles ST, Luong G, Almeida DM, et al. Fewer ups and downs: daily stressors mediate age differences in negative affect. J Gerontol B Psychol Sci Soc Sci 2010;65b:279–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Posserud I, Svedlund J, Wallin J, et al. Hypervigilance in irritable bowel syndrome compared with organic gastrointestinal disease. J Psychosom Res 2009;66:399–405. [DOI] [PubMed] [Google Scholar]
- 44.Bassil N, Ghandour A, Grossberg GT. How anxiety presents differently in older adults. Curr Psychiatr 2011;10:1–8. [Google Scholar]
- 45.Black CJ, Yiannakou Y, Houghton LA, et al. Anxiety-related factors associated with symptom severity in irritable bowel syndrome. Neurogastroenterol Motil 2020;32:e13872. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


