Abstract
The growing homebound population may particularly benefit from video telehealth. However, some patients do not have the ability or resources to successfully use this modality. This report presents the experience of a large urban home-based primary care program disseminating cellular-enabled tablets with basic instruction to a subset of its patients who would not otherwise have had the ability to engage in video telehealth. Program goals included: increasing the number of patients able to engage in video encounters and leveraging technology to help achieve greater equity. While 123 homebound patients received devices for telehealth, only one-third successfully utilized them. We identified multiple barriers to telehealth utilization beyond physical access to a device, including a lack of skill. Efforts to increase video encounters among patient groups who are less experienced with technology cannot simply rely on device provision or basic instruction but must include reinforced learning strategies combined with ongoing technical assistance.
The 2019 (COVID-19) pandemic resulted in a massive shift to utilizing video telehealth. Research has shown that video telehealth is feasible and acceptable in delivering care to older adults (Abrashkin et al., 2020; Batsis et al., 2019; Hawley et al., 2020; Kalicki et al., 2021). However, some patients do not have the ability or resources to use video telehealth. For other patients, although these technologies are available and feasible, video telehealth services may be difficult to utilize. In addition to higher rates of chronic illness and cognitive impairment, which can limit use of technology, older adults may in particular face higher barriers to telehealth use given changes in vision, hearing, and manual dexterity, which may hinder the use of video telehealth services, (Berry & Steinman, 2004) and limited computer skills and inexperience with technology in general. Approximately 13 million older adults in the United States may have difficulty utilizing video telehealth services and a significant proportion of this group lack basic resources (Lam et al., 2020; Stringer, 2019). Taken together, a significant digital inequity exists for the older population.
One group that may particularly benefit from the use of video telehealth encounters is the growing homebound population. Every year in the United States, more older adults become homebound than enter nursing homes (Ornstein et al., 2020). Homebound patients experience disability, cognitive impairment, and increased rates of hospitalization (Schuchman et al., 2018). While home-based primary care providers serve private residences and assisted living facilities, the need for in-home care often surpasses availability, resulting in many homebound adults with limited access to health care. Prior research has indicated that there are advantages of video telehealth visits among the homebound population including quickly triaging patient needs, easily collecting patient information, and increasing the capacity for scheduling (Franzosa et al., 2021; Jacobs et al., 2019). Additionally, patients report that video telehealth visits save time and money (Jacobs et al., 2020). However, digital inequity may be exacerbated in this population given their medial complexity combined with the more general challenges older adults face.
The present study examines the video telehealth device dissemination experience of the Mount Sinai Visiting Doctors (MSVD), a large urban home-based primary care program in New York City. For over 25 years, MSVD has provided care to homebound adults. Utilizing an interdisciplinary team comprised of physicians, social workers, nurses, and nurse practitioners, MSVD provides care with the goal of improving the quality of life for homebound patients and their caregivers. MSVD provided cellular-enabled tablets and basic instruction to a subset of its patients who would not otherwise have had the ability to engage in a video telehealth encounter with the goals of increasing the number of patients engaging in video encounters and of leveraging technology to help achieve greater equity in access and use of telehealth. Our hypothesis was that providing technology to patients who otherwise did not have access to it would lead to an increase in video telehealth encounters. This paper reports on our experience in disseminating the tablets and their usage.
Methods
Setting
MSVD presently serves a population of 1406 homebound older adults with multiple comorbidities in Manhattan using physician and nurse practitioner-led primary care services in the home with nurse and social work support. During the first NYC COVID-19 surge in the spring of 2020, MSVD transitioned almost exclusively to remote care provision, with few urgent in-person care encounters occurring from March through May 2020. Following May 2020, in-person encounters resumed but were limited to ensure patient safety.
Patient Selection and Video Telehealth Device Distribution and Assistance
As reported previously (Kalicki et al., 2021), MSVD physicians completed an 11-item questionnaire to assess which homebound patients who were enrolled in the MSVD program would be a good fit for a cellular-enabled video telehealth device. In brief, physicians were asked who could benefit from receiving a device as well as barriers to access including internet connectivity and ability to pay for data plans. Questions aimed to identify which patients 1) did not have access to another device that could be used for video encounters, and 2) had sufficient comfort with technology or caregiver support to operate the tablet. After the completion of the initial questionnaire, physicians could continue to recommend patients who were identified to benefit from receipt of a device on an ongoing basis to program coordinators if they met the aforementioned criteria. Telehealth devices were purchased under a grant from the Federal Communications Commission and included a cellular-enabled (at no cost to the patient) tablet with a HIPAA-compliant telemedicine application (that was not integrated with the electronic medical record), blood pressure cuff and pulse oximeter that could connect to the tablet wirelessly. Tablets did not include other functionality such as internet browsing. Following the identification of patients eligible to receive a device, program coordinators called the patient or caregiver, as appropriate, to gauge interest and schedule device drop off. The recipient was provided with instructions (in English or in Spanish), either in person or later by phone, on how to operate the device, turn the device on and off, navigate to the telemedicine application, and answer a telehealth call. If a device was to be returned by the patient, program coordinators asked participants the reason for return of the device. These patients were also asked if they would participate in future focus groups to identify barriers to use of the device and provide feedback as how to improve the program. Program coordinators were available as needed via telephone to assist patients with the device after the initial instruction. This study received an exempt determination from the Mount Sinai Program for the Protection of Human Subjects (IRB-21-00157).
Sample
A total of 1406 patients were active in MSVD from November 1, 2020 to October 31, 2021. From this census, MSVD physician providers identified 137 patients via REDCap questionnaire and direct recommendation to supply with a video telehealth device (Kalicki et al., 2021). Eligible participants did not have access to another telehealth device, reported feeling comfortable with technology to operate the device, or indicated they had a support person (i.e., caregiver, family member, health aide) to assist them. Remaining patients either owned a telehealth device or were deemed to be incapable of conducting a video encounter, did not have someone to assist them, or that they would not likely engage in a video encounter even if provided a video telehealth device. Video telehealth devices were distributed beginning in November 2020.
Data Collection
Demographics (age, sex, race, primary language, Medicaid status, public housing status, and dementia status), health services usage, and tablet distribution data were collected for the purpose of program operations and released as a limited dataset (only including data for the aforementioned period) for descriptive analysis. Missing values were removed from the denominators of percentages calculated. Demographic and health services usage data were determined by the electronic medical record (encounters billed by providers), telehealth usage was determined via the usage logs of the telehealth device, and tablet distribution data were tracked by a project coordinator.
Data Analysis
All data were deidentified and descriptive analyses were conducted for those who were deemed to benefit from the device, accepted the device, refused the device, used the device, and did not use the device. To determine whether demographic variables (age, gender, race, primary language, Medicaid status, dementia status, public housing status) were associated with the acceptance of and use of the telehealth video device, we used chi-square and t-tests (where applicable).
Results
As seen in Table 1, on average, patients (n=137) who were deemed to benefit from the device were 80.8 years old (SD 13.5), predominantly female (87%), nonwhite (62%), English speaking (86%), and on Medicaid (51%). Twenty-six percent of patients had a diagnosis of dementia and 24% lived in public housing. Of these 137 patients, most (123, 90%) accepted the device. When comparing those that accepted the device to those that refused the device, refusers were on average older than acceptors [86.6 years old (SD 9.4) vs 78 years old (SD 13.9), p<.05]. The proportion of participants who accepted the video telehealth device did not significantly differ by sex, race, primary language, Medicaid status, public housing status, and dementia status (Table 1). Reasons for device refusal included, not useful, prefers other application options, prefers in person visits, and not comfortable with new technology. As shown in Figure 1, the predominant mode of communication for billed telehealth encounters between physicians across all MSVD homebound patients was via telephone, while the least used mode of communication was video telehealth device visits. Other video visits consisted of telehealth encounters between physicians and MSVD patients utilizing some other device such as a patient or caregivers cell phone. Patients returned their device to the practice in 22% of cases.
Table 1:
Demographics of patients deemed eligible for a telemedicine device, those who accepted the device and those who refused the device
| Variable | Deemed eligible (137) | Accepted device (123) | Refused device (14) | Test of independence Acceptance vs Refusal (N=137) |
|---|---|---|---|---|
| Age, mean (sd) | 80.8 (13.5) | 78 (13.9) | 86.6 (9.4) | t=2.16, p=0.03 |
| Female, n (%) | 119 (87%) | 103 (84%) | 13 (93%) | χ2=1, p=0.4 |
| Race, n (%) | χ2=2.9, p=0.6 | |||
| White | 42 (31%) | 33 (27%) | 5 (36%) | |
| African American | 35 (26%) | 39 (32%) | 3 (21%) | |
| Hispanic | 20 (15%) | 23 (19%) | 1 (7%) | |
| Other | 24 (18%) | 21 (17%) | 2 (14%) | |
| Unknown | 4 (3%) | 3 (2%) | 1 (7%) | |
| Language, n (%) | χ2=1.8, p=.2 | |||
| English | 118 (86%) | 106 (86%) | 13 (93%) | |
| Spanish | 14 (10%) | 15 (12%) | 0 (0%) | |
| Medicaid, n (%) | 70 (51%) | 69 (56%) | 4 (29%) | χ2=3.3, p=0.1 |
| Public Housing, n (%) | 33 (24%) | 30 (24%) | 1 (7%) | χ2=1.7, p=0.2 |
| Dementia, n (%) | 36 (26%) | 30 (24%) | 3 (21%) | χ2=.01, p=0.9 |
To assess group differences by demographics, chi-square analyses (gender, race, language, Medicaid status, public housing status, and dementia status) and a t-test (age) were performed between those who accepted and refused the video telehealth device.
Figure 1:
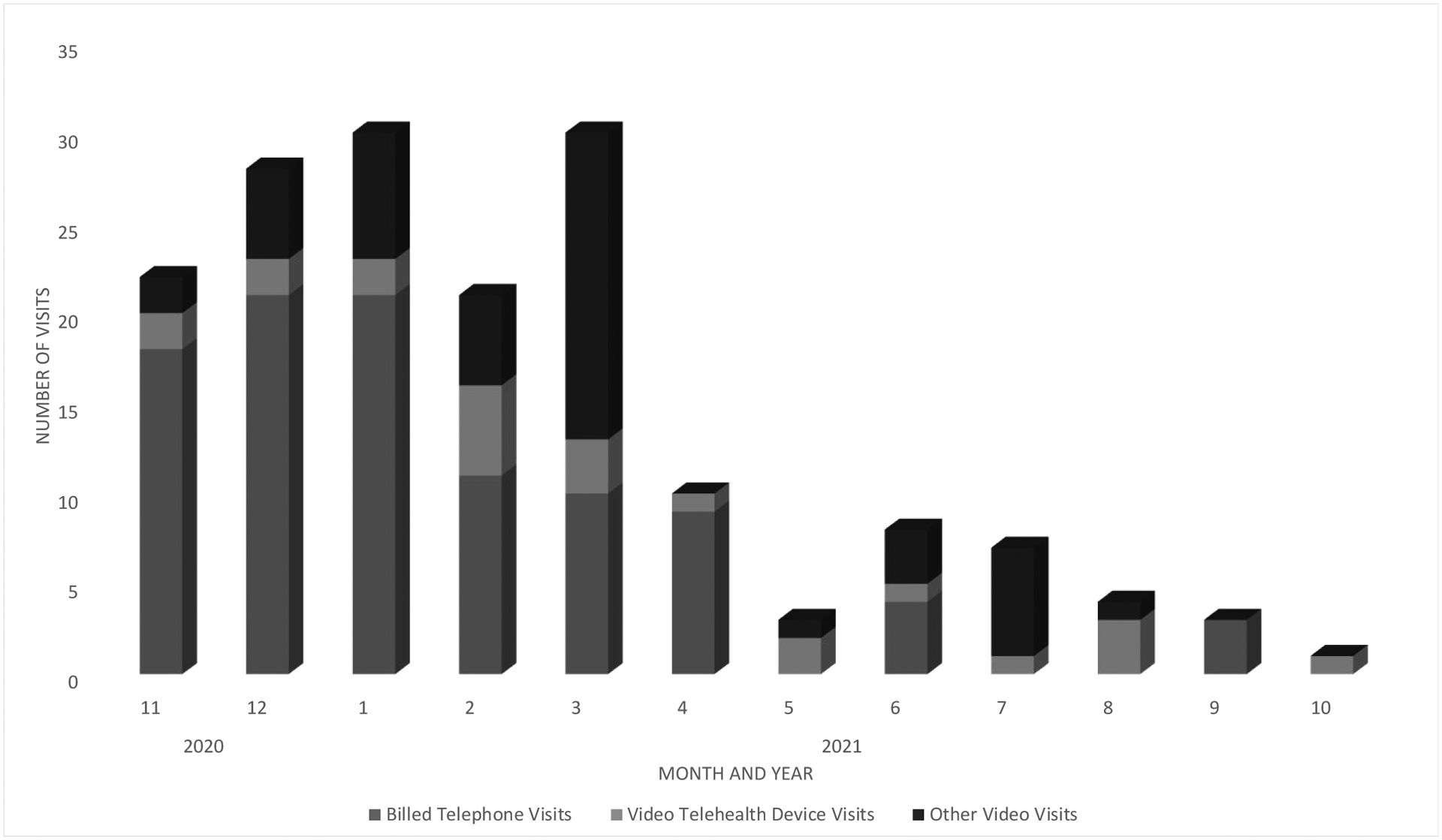
Telemedicine Visits by Type Across Participants Who Accepted the Device
As seen in Table 2, of the 123 patients who accepted the device, 48 (39%) participants actively used the device at least one time. The proportion of participants who reported using the video telehealth device did not significantly differ by age, sex, race, primary language, Medicaid status, and public housing status (Table 2). However, we found a statistically significant difference between the proportion of patients with dementia among device users and non-users with users more likely to have dementia than non-users (χ2 (1, N = 123) = 7.1, p < .01).
Table 2:
Demographics of patients who accepted the device by use
| Variable | Accepted, used device (48) | Accepted, did not use device (75) | Test of independence (N=123) |
|---|---|---|---|
| Age, mean (sd) | 76.3 (15.1) | 79.2 (13.1) | t=1.1, p=0.3 |
| Female, n (%) | 39 (81%) | 64 (86%) | χ2=.4, p=0.6 |
| Race, n (%) | χ2=5.5, p=0.2 | ||
| White | 9 (19%) | 24 (32%) | |
| African American | 20 (42%) | 19 (25%) | |
| Hispanic | 8 (17%) | 15 (20%) | |
| Other | 8 (17%) | 13 (17%) | |
| Unknown | 2 (4%) | 1 (1%) | |
| Language, n (%) | χ2=1.1, P=.3 | ||
| English | 43 (90%) | 63 (84%) | |
| Spanish | 4 (8%) | 11 (15%) | |
| Medicaid, n (%) | 29 (60%) | 40 (56%) | χ2=0.7, p=0.4 |
| Public Housing, n (%) | 10 (38%) | 20 (28%) | χ2=.6, p=0.4 |
| Dementia, n (%) | 18 (38%) | 12 (16%) | χ2=7.1, p=0.01 |
To assess group differences by demographics, chi-square analyses (gender, race, language, Medicaid status, public housing status, and dementia status) and a t-test (age) were performed.
Discussion
The COVID-19 pandemic quickly highlighted the need to incorporate telemedicine as a tool in home-based healthcare. The need to provide video telehealth care coupled with the rapid changes of the pandemic meant that government funding was made available to provide care to vulnerable populations. The present study examined an innovative program providing remote video telehealth devices to a homebound population following the receipt of federal grant support. Overall, MSVD was able to disseminate devices to 123 patients who were deemed to benefit from receiving a video telehealth device. However, the devices were used by less than half of the patients who received them, and almost a third of those non-users returned them, indicating several important implications for telehealth implementation in the homebound population.
First, research has indicated that barriers to video telehealth extend beyond physical access to a device, and can include cognitive and sensory limitations, lack of video telehealth training, and patient concerns of privacy (Abrashkin et al., 2020; Franzosa et al., 2021; Zhai, 2021; Zulman et al., 2019). These findings seem to accord with MSVD’s telehealth tablet initiative. Despite patients being provided with cellular-enabled devices and offered instructions on their use, devices were not used by many of them, and in some cases returned. Patients chose to communicate via a method that they already knew, demonstrating the importance for a patient to understand the utility of learning something new if we expect them to adopt new health behaviors. This may also account for the subset of refusers who were found to be older than those who accepted the device. Consistent with prior research, if a patient does not perceive the usefulness and advantage over not using technology, they are less likely to use it (Gell et al., 2015; Nägle & Schmidt, 2012).
Second, it became clear that educating patients on how to use the device was important but needs tailoring to the population. While prior research has indicated there has been an increase in the use of video-based telehealth services in homebound older adults in general, there is still room for innovative, patient-centered strategies to help support patients who are unable to engage in video telehealth services, especially those without a caregiver available to assist them in the visit (Kalicki et al., 2021). Within homebound populations, declines in cognitive functioning may make technology use difficult. However, while patients noted their discomfort upon returning the device, patients rarely requested assistance, consistent with prior research (Huber & Watson, 2014). It is possible that isolation exacerbated due to COVID-19 made it difficult to ask for assistance, as research shows that older adults are more likely to ask for help from peers in their environment (Hunsaker et al., 2019; Marston et al., 2019). It is also possible that patients were only comfortable asking for assistance from someone with whom they already felt close (i.e., a support person).
Results also indicated that users and non-users of the video telehealth device differed by dementia status, in that users were diagnosed with dementia more often than non-users. As patients with dementia increasingly depend on the help of a caregiver and/or health aide, this support may have translated in increased use of the device. While patients without dementia may have had a support person, they may not have played as an active role as with a patient with dementia, which could explain decreased use of the device. Consistent with prior research, this suggests that devices may be useful for caregivers to help support patients as well as for patients to directly engage with healthcare providers (Wardlow et al., 2022). One method to increase video telehealth device usage may be utilizing a telehealth reinforced learning program. This includes repetition learning, which has been shown to increase and enhance memory performance long term in older adults (Kilb & Naveh-Benjamin, 2011) by way of fortifying chemical interactions between neurons in the brain (Grill-Spector et al., 2006). This could involve several telehealth instructional sessions following the initial presentation or instructional guidance on of the video telehealth device to repeat and reinforce information and to ensure competence and understanding (Rebok et al., 2007). Tangible forms of instructional support, such as a user manual or guide, regardless of how simple or easy-to-use a system may be, should be provided (Czaja, 2017). Increasing the amount and variety of support provided to older adults in the early stages of learning something new can be helpful to reinforce learned material. Research also indicates that older adults report more positive than negative attitudes surrounding technology, contradicting stereotypes that older adults are unwilling to utilize technology (Mitzner et al., 2010); with the right support, they may welcome learning new skills.
Finally, the devices that MSVD provided only had functionality for performing video encounters with MSVD and for recording vital signs from the blood pressure cuff and pulse oximeter. Patients could not use the device to do things like access the internet, play games, use email, etc. Consequently, patients may not have had the chance to become more familiar with the device, because they used it so infrequently. Increasing interest or activating delight (Tsai et al., 2017) may have benefits in telehealth engagement.
Limitations
There were several potential limitations to the present research. First, when considering limited use of video telehealth devices, we did not assess provider related attitudes toward or comfort with the video telehealth device (e.g., lack of technological savvy). Moreover, during the pandemic, insurance companies included telephone calls as a telehealth service which afforded providers an easy option to contact patients over utilizing the telehealth device. Additionally, factors such as lack of integration of the device with the electronic health record may have impeded ease of use. Secondly, while only those who returned the devices were asked about barriers to device use, we did not conduct an in-depth survey of all patients and caregivers to understand the reasoning behind limited use of video telehealth devices, which can be an important direction for future work. Finally, the results presented are from a singular homebound primary care program in New York City, and while diverse, results may not be generalizable to homebound populations in other states or more rural locations.
Conclusions
In conclusion, video telehealth devices provided to selected patients within a home-based primary care practice during the COVID-19 pandemic were not utilized by the majority of recipients and did not lead to a significant increase in completed video telehealth encounters. This demonstrates that barriers to use of telemedicine devices go beyond not having access to them. Methods to increase older adult engagement with new technology must be considered, including the potential use of a reinforced learning program to increase repetition of newly learned information, and supporting multi-use opportunities with devices. Device use for caregiver needs may also enhance interest in and use of the device. Future research will need to be conducted to determine if the utilization of such a program would increase telemedicine device use in this population.
What this paper adds.
Description of a home-based primary care program’s experience with providing cellular-enabled tablets to a homebound population.
Further delineation of the multiple barriers to telehealth use beyond access to telehealth devices.
Suggestions for reinforced learning strategies to improve video telehealth visits.
Applications of study findings.
While the COVID-19 pandemic has highlighted the value incorporating telehealth as a tool in home-based healthcare, but this study indicates that simply providing devices with limited instruction is inadequate.
Study findings provide key directions for future telehealth device dissemination, specifically to consider how to provide ongoing education to patients on telehealth device utilization.
Efforts to increase video encounters among patient groups must include explicit reinforced learning strategies as part of education and training.
Acknowledgments
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number T32AG066598, Federal Communications Commission’s COVID-19 Telehealth Program Funding Commitment Number 0003, and the Icahn School of Medicine at Mount Sinai’s Alzheimer’s Disease Research Center P30AG066514. Authors have no conflicts of interest to disclose. Research was conducted with the approval of the Icahn School of Medicine at Mount Sinai’s Program for the Protection of Human Subjects (IRB-21-00157).
References
- Abrashkin KA, Poku A, Ball T, Brown ZJ, & Rhodes KV (2020). Ready or not: pivoting to video visits with homebound older adults during the covid-19 pandemic. Journal of the American Geriatrics Society, 68(11), 2469–2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batsis JA, DiMilia PR, Seo LM, Fortuna KL, Kennedy MA, Blunt HB, Bagley PJ, Brooks J, Brooks E, & Kim SY (2019). Effectiveness of ambulatory telemedicine care in older adults: a systematic review. Journal of the American Geriatrics Society, 67(8), 1737–1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry P, & Steinman BA (2004). Vision and hearing loss in older adults:” Double trouble”. Care Management Journals, 5(1), 35. [DOI] [PubMed] [Google Scholar]
- Czaja SJ (2017). The potential role of technology in supporting older adults. Public Policy & Aging Report, 27(2), 44–48. [Google Scholar]
- Franzosa E, Gorbenko K, Brody AA, Leff B, Ritchie CS, Kinosian B, Sheehan OC, Federman AD, & Ornstein KA (2021). “There Is Something Very Personal About Seeing Someone’s Face”: Provider Perceptions of Video Visits in Home-Based Primary Care During COVID-19. Journal of Applied Gerontology, 40(11), 1417–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gell NM, Rosenberg DE, Demiris G, LaCroix AZ, & Patel KV (2015). Patterns of technology use among older adults with and without disabilities. The Gerontologist, 55(3), 412–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grill-Spector K, Henson R, & Martin A (2006). Repetition and the brain: neural models of stimulus-specific effects. Trends in cognitive sciences, 10(1), 14–23. [DOI] [PubMed] [Google Scholar]
- Hawley CE, Genovese N, Owsiany MT, Triantafylidis LK, Moo LR, Linsky AM, Sullivan JL, & Paik JM (2020). Rapid integration of home telehealth visits amidst covid-19: what do older adults need to succeed? Journal of the American Geriatrics Society, 68(11), 2431–2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber L, & Watson C (2014). Technology: Education and training needs of older adults. Educational Gerontology, 40(1), 16–25. [Google Scholar]
- Hunsaker A, Nguyen MH, Fuchs J, Djukaric T, Hugentobler L, & Hargittai E (2019). “He explained it to me and I also did it myself”: How older adults get support with their technology uses. Socius, 5, 2378023119887866. [Google Scholar]
- Jacobs JC, Blonigen DM, Kimerling R, Slightam C, Gregory AJ, Gurmessa T, & Zulman DM (2019). Increasing mental health care access, continuity, and efficiency for veterans through telehealth with video tablets. Psychiatric Services, 70(11), 976–982. [DOI] [PubMed] [Google Scholar]
- Jacobs JC, Hu J, Slightam C, Gregory A, & Zulman DM (2020). Virtual savings: Patient-reported time and money savings from a VA national telehealth tablet initiative. Telemedicine and e-Health, 26(9), 1178–1183. [DOI] [PubMed] [Google Scholar]
- Kalicki AV, Moody KA, Franzosa E, Gliatto PM, & Ornstein KA (2021). Barriers to telehealth access among homebound older adults. Journal of the American Geriatrics Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilb A, & Naveh-Benjamin M (2011). The effects of pure pair repetition on younger and older adults’ associative memory. Journal of Experimental Psychology: Learning, Memory, and Cognition, 37(3), 706. [DOI] [PubMed] [Google Scholar]
- Lam K, Lu AD, Shi Y, & Covinsky KE (2020). Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Internal Medicine, 180(10), 1389–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marston HR, Genoe R, Freeman S, Kulczycki C, & Musselwhite C (2019). Older adults’ perceptions of ICT: Main findings from the technology in later life (TILL) study. Healthcare, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitzner TL, Boron JB, Fausset CB, Adams AE, Charness N, Czaja SJ, Dijkstra K, Fisk AD, Rogers WA, & Sharit J (2010). Older adults talk technology: Technology usage and attitudes. Computers in human behavior, 26(6), 1710–1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nägle S, & Schmidt L (2012). Computer acceptance of older adults. Work, 41(Supplement 1), 3541–3548. [DOI] [PubMed] [Google Scholar]
- Ornstein KA, Garrido MM, Bollens-Lund E, Husain M, Ferreira K, Kelley AS, & Siu AL (2020). Estimation of the incident homebound population in the US among older Medicare beneficiaries, 2012 to 2018. JAMA Internal Medicine, 180(7), 1022–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebok GW, Carlson MC, & Langbaum JB (2007). Training and maintaining memory abilities in healthy older adults: traditional and novel approaches. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62(Special_Issue_1), 53–61. [DOI] [PubMed] [Google Scholar]
- Schuchman M, Fain M, & Cornwell T (2018). The resurgence of home-based primary care models in the United States. Geriatrics, 3(3), 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringer S (2019). Census and the City: Overcoming NYC’s Digital Divide in the 2020 Census. New York, NY: Office of the New York City Comptroller. [Google Scholar]
- Tsai H.-y. S., Shillair R, & Cotten SR (2017). Social support and “playing around” an examination of how older adults acquire digital literacy with tablet computers. Journal of Applied Gerontology, 36(1), 29–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardlow L, Leff B, Biese K, Roberts C, Archbald-Pannone L, Ritchie C, DeCherrie LV, Sikka N, Gillespie SM, Telehealth, C. f., & Aging. (2022). Development of telehealth principles and guidelines for older adults: A modified Delphi approach. Journal of the American Geriatrics Society. [DOI] [PubMed] [Google Scholar]
- Zhai Y (2021). A call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychotherapy and Psychosomatics, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulman DM, Wong EP, Slightam C, Gregory A, Jacobs JC, Kimerling R, Blonigen DM, Peters J, & Heyworth L (2019). Making connections: nationwide implementation of video telehealth tablets to address access barriers in veterans. JAMIA open, 2(3), 323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]


