Abstract
Background:
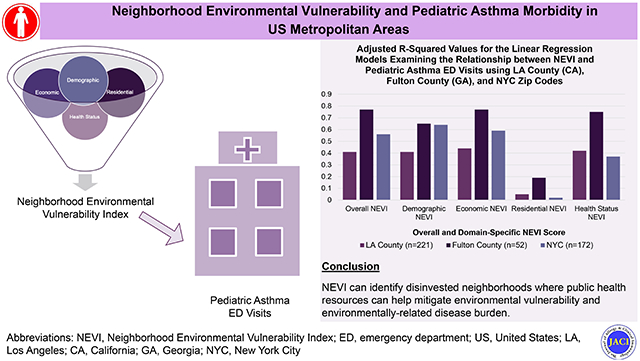
Research suggests demographic, economic, residential, and health-related factors influence vulnerability to environmental exposures. Greater environmental vulnerability may exacerbate environmentally-related health outcomes. We developed a neighborhood environmental vulnerability index (NEVI) to operationalize environmental vulnerability on a neighborhood-level.
Objective:
We explored the relationship between NEVI and pediatric asthma emergency department (ED) visits (2014-2019) in three US metropolitan areas: Los Angeles (LA) County, California (CA); Fulton County, Georgia (GA); and New York City (NYC), New York (NY).
Methods:
We performed separate linear regression analyses examining the association between overall NEVI score and domain-specific NEVI scores (demographic, economic, residential, health status) with pediatric asthma ED visits (per 10,000) across each area.
Results:
Linear regression analyses suggest that higher overall and domain-specific NEVI scores were associated with higher annual pediatric asthma ED visits. Adjusted R-squared values suggest that overall NEVI scores explained at least 40% of the variance in pediatric asthma ED visits. Overall NEVI scores explained more of the variance in pediatric asthma ED visits in Fulton County. NEVI scores for the demographic, economic, and health status domains explained more of the variance in pediatric asthma ED visits in each area, compared to the NEVI score for the residential domain.
Conclusion:
Greater neighborhood environmental vulnerability was associated with greater pediatric asthma ED visits in each area. The relationship differed in effect size and variance explained across the areas. Future studies can use NEVI to identify populations in need of greater resources to mitigate the severity of environmentally-related outcomes, such as pediatric asthma.
Keywords: pediatric asthma, environmental vulnerability, neighborhood, racial disparities
Graphical Abstract
Capsule Summary
Greater vulnerability to environmental exposures, measured via a neighborhood environmental vulnerability index (NEVI), is associated with greater pediatric asthma morbidity. NEVI can identify disinvested neighborhoods where resources may be needed to mitigate environmental vulnerability and disease burden.
Introduction
Asthma is a common chronic disease among children1-3 and the third most common cause of hospitalization among children under the age of 15 years.4 Pediatric asthma is the second highest cause of pediatric healthcare expenditures as direct costs of pediatric asthma were nearly $6 billion in 2013, driven by asthma-related emergency department (ED) visits and hospital admissions.4, 5 Epidemiological data demonstrate racial and ethnic disparities in US pediatric asthma health outcomes.6-8 Studies suggest that Black and Hispanic children have higher incidence and earlier onset of pediatric asthma compared to White children.9 Furthermore, Black and Hispanic children have higher rates of asthma-related ED and inpatient visits compared to White children.10, 11 The racial, ethnic, and geographic disparities in pediatric asthma morbidities may be driven by differential vulnerability to environmental exposures.1, 12, 13 14
Accordingly, there is a public health need to understand drivers of ED use among children with asthma to reduce racial, ethnic, and geographic disparities in pediatric asthma outcomes. Populations’ differential vulnerability to environmental exposures may stem from systemic racism, defined as the implicit and explicit systems that sustain barriers to health and wellness for communities of color.15 Systemic racism may underlie why communities of color have greater susceptibility to environmental exposures,15-17 as systemic racism has influenced historical policies, such as residential redlining where the US federal government discouraged insuring housing loans to individuals who resided in predominantly Black neighborhoods.18-22 This contributed to a disinvestment in predominantly Black communities, concentrating poverty and reducing their options for housing mobility.23-25 Communities in disinvested neighborhoods are exposed to a range of adverse factors,18-22, 26-28 including overcrowding in residential units,29 greater population density,30, 31 greater urbanization,12, 32 and lower socioeconomic levels,33, 34 which contribute to greater vulnerability to environmental exposures. Greater vulnerability to environmental exposures may then be associated with a higher burden of pediatric asthma morbidity, such as higher pediatric asthma ED visits.
Therefore, we developed the neighborhood environmental vulnerability index (NEVI) to gauge a population’s susceptibility to the influence of environmental exposures in four domains pertaining to demographics, economic indicators, residential characteristics, and health characteristics.35 The NEVI captures built and social environmental features independent of air pollution and allergens that are known triggers of asthma morbidity and ED utilization.35 In creating the NEVI, we used a multi-model approach to identify how a combination of these factors may altogether define the vulnerability of populations to environmental exposures,36, 37 and thereby, contribute to higher pediatric asthma morbidity.38-40 Given that populations are exposed to a combination of adverse factors that likely occur together especially in the context of disinvested neighborhoods, it is more logical to look at the combination of social and structural factors that influence environmentally-related health outcomes.
Our study objective was to examine the relationship between neighborhood environmental vulnerability (measured via NEVI) and pediatric asthma morbidity for three metropolitan areas: 1) Los Angeles (LA) County, California (CA); 2) Fulton County, Georgia (GA), and 3) New York City (NYC), New York (NY). We measured pediatric asthma morbidity via ED visits, as pediatric asthma can generally be managed in an outpatient setting via controlling exposures to factors that trigger exacerbations, adequate pharmacological management, continual monitoring of disease, and patient education in healthcare. Therefore, frequent pediatric asthma ED visits can highlight shortcomings in effective management for vulnerable populations in certain areas.41-43
We chose to study LA County (CA), Fulton County (GA), and NYC as these three metropolitan areas encompass populations that are upwards of 1 million to 10 million people and have a varied distribution of neighborhood vulnerability levels, which may contribute to a better understanding of the NEVI’s utility in explaining pediatric asthma ED visit rates. Additionally, these regions comprise some of the most racially and ethnically diverse US populations with White, Black, Asian, and Hispanic representation.44-46 Using these three metropolitan areas can allow for better generalizability of the findings regarding the relationship between NEVI and pediatric asthma ED visits.
We hypothesized that higher overall NEVI score, meaning greater environmental vulnerability, would be associated with higher pediatric asthma ED visits. Disinvested neighborhoods are exposed to adverse factors that may increase their vulnerability to environmental exposures, which may be associated with greater exacerbations of environmentally-related diseases, such as pediatric asthma. We also hypothesized that the economic NEVI score, which includes many socioeconomic variables, would have the strongest relationship with pediatric asthma ED visits, in comparison to the demographic, residential, and health NEVI scores, as the literature suggests low education, unemployment, and low socioeconomic status are strongly associated with increased vulnerability to adverse environmental exposures.47-49
Methods
Data Sources
Features for the NEVI were prepared using publicly available data from the 2015-2019 U.S. Census American Community Survey (ACS) 5-year estimates and the 2020 data release from the Centers for Disease Control and Prevention (CDC) PLACES Project. The US Census ACS provides social and economic data across states, cities, counties, census tracts, and block groups. The PLACES project generates model-based, population-level analyses and community health indices for all counties, places, census tracts, and ZIP Code Tabulation Areas (ZCTAs) across the US.50
Annual average pediatric asthma ED visit data was retrieved at the zip code level from the following sources: 1) California Department of Public Health for LA County;51 2) Georgia Department of Public Health for Fulton County;52 and 3) New York State Department of Health for NYC.53
Study Population
We limited the data to zip codes that had both NEVI and pediatric asthma ED visit data. We included 221 zip codes in LA County (>77% of LA County zip codes),51 52 zip codes in Fulton County (>62% of Fulton County zip codes),52 and 172 zip codes in NYC (>95% of NYC zip codes).53 In collating the NEVI data by zip code, we excluded census tracts that had a population of less than 20 or had a population greater than 20 but had missing data for at least one of the NEVI features of interest.54
Measures
Exposure: Neighborhood Environmental Vulnerability Index (NEVI) Score by Zip Code
Development of the NEVI was first reported by Uong et al.54 We adapted the methodology as outlined in their study.54 The NEVI was calculated using 54 features organized into four domains: 1) demographics, 2) economic indicators, 3) residential characteristics, and 4) health status. Within each domain, we summarized the selected features (Supplemental Table 1).35 A higher NEVI score suggests a higher level of neighborhood vulnerability to environmental exposures. The NEVI is standardized to each individual area, which indicates that a 0.30 NEVI score in an NYC zip code will not suggest the same level of vulnerability to environmental exposures as a 0.30 NEVI score in a Fulton County zip code. We intentionally did not standardize NEVI to the combined data across the three metropolitan areas, as a NEVI standardized to each individual metropolitan area has more potential utility. For example, a NEVI standardized to Fulton County can help researchers identify disinvested neighborhoods in Fulton County that may need more resources to mitigate environmental vulnerability, compared to other neighborhoods in Fulton County.
Outcome: Pediatric Asthma ED Visits
Pediatric asthma ED visit data were obtained by zip code based on available participant age and calendar year ranges. For LA County (CA), pediatric asthma ED visit data were obtained for children (age 0-17 years) in 2019.51 For Fulton County (GA), pediatric asthma ED visit data were obtained for children (0-19 years) averaged over the years 2014-2018. For NYC, pediatric asthma ED visit data were obtained for children (0-17 years) averaged over the years 2017-2019.
Descriptive and Statistical Analyses
We examined descriptive statistics, including the mean, median, standard deviation, interquartile range, minimum, and maximum, for the overall NEVI scores, NEVI domain-specific scores, and pediatric asthma ED visits per 10,000 in LA County, Fulton County, and NYC. For each of the three areas, we constructed five separate linear regression models examining the relationships between the NEVI scores and pediatric asthma ED visits (per 10,000). Each linear regression model was composed of only one explanatory variable, which included either the overall NEVI score or one of the four domain-specific NEVI scores (demographic NEVI score, economic NEVI score, residential NEVI score, or health status NEVI score).
For each model, we produced the standardized beta coefficient, corresponding 95% confidence interval, and the adjusted R-squared value. We plotted a heatmap of the adjusted R-squared values across the 15 linear regression models, with the x-axis designating the region and the y-axis designating the NEVI score used as the explanatory variable in the model.
Lastly, we explored how NEVI scores related to characteristics of specific areas within LA County, Fulton County, and NYC to understand how social and demographic context may be related to NEVI scores. We implemented our analyses using the R (version 4.1.2) statistical software program.55
Results
Summary Statistics
Table 1 provides the summary statistics for overall NEVI scores, NEVI domain-specific scores, and pediatric asthma ED visits across LA County, Fulton County, and NYC. Fulton County exhibited the largest range in overall NEVI scores (0.15-0.53) compared to that of LA County and NYC. NYC had the highest average pediatric asthma ED visits (155.78 per 10,000) and LA County had the lowest average pediatric asthma ED visits (70.59 per 10,000).
Table 1.
Summary Statistics Across Overall NEVI and NEVI Domain-Specific Scores, and Annual Rates of Pediatric Asthma1 ED visits (per 10,000) using LA County (CA), Fulton County (GA), and NYC Zip Codes
| LOS ANGELES COUNTY | ||||||
|---|---|---|---|---|---|---|
| Mean | SD | Median | IQR | Min. | Max | |
| Overall NEVI | 0.30 | 0.07 | 0.29 | 0.25–0.34 | 0.18 | 0.47 |
| Domain-Scores | ||||||
| Demographic | 0.30 | 0.04 | 0.30 | 0.28-0.33 | 0.21 | 0.44 |
| Economic | 0.27 | 0.08 | 0.26 | 0.21-0.32 | 0.13 | 0.46 |
| Residential | 0.23 | 0.06 | 0.22 | 0.19-0.25 | 0.09 | 0.43 |
| Health Status | 0.39 | 0.12 | 0.39 | 0.30-0.48 | 0.17 | 0.69 |
| Rates of Pediatric Asthma ED Visits (per 10,000) | 70.59 | 32.60 | 67.70 | 47.20-83.90 | 15.60 | 178.20 |
| FULTON COUNTY (GA) | ||||||
| Mean | SD | Median | IQR | Min. | Max | |
| Overall NEVI | 0.32 | 0.10 | 0.30 | 0.23–0.40 | 0.15 | 0.53 |
| Domain-Scores | ||||||
| Demographic | 0.36 | 0.09 | 0.37 | 0.28-0.43 | 0.19 | 0.53 |
| Economic | 0.29 | 0.12 | 0.26 | 0.19-0.39 | 0.13 | 0.54 |
| Residential | 0.25 | 0.10 | 0.25 | 0.18-0.30 | 0.11 | 0.53 |
| Health Status | 0.36 | 0.17 | 0.35 | 0.21-0.49 | 0.10 | 0.71 |
| Rates of Pediatric Asthma ED Visits (per 10,000) | 109.59 | 67.06 | 91.96 | 49.95-159.00 | 23.93 | 293.37 |
| NEW YORK CITY | ||||||
| Mean | SD | Median | IQR | Min. | Max | |
| Overall NEVI | 0.33 | 0.07 | 0.32 | 0.28–0.38 | 0.21 | 0.50 |
| Domain-Scores | ||||||
| Demographic | 0.28 | 0.06 | 0.27 | 0.24-0.32 | 0.17 | 0.46 |
| Economic | 0.36 | 0.10 | 0.35 | 0.30-0.42 | 0.19 | 0.60 |
| Residential | 0.33 | 0.07 | 0.34 | 0.27-0.38 | 0.13 | 0.51 |
| Health Status | 0.36 | 0.12 | 0.36 | 0.29-0.44 | 0.13 | 0.64 |
| Rates of Pediatric Asthma ED Visits (per 10,000) | 155.78 | 120.64 | 134.65 | 53.77-205.30 | 17.40 | 597.20 |
Pediatric Asthma ED Visits pertain to those between 0 to 19 years of age
Acronyms: NEVI = Neighborhood Environmental Vulnerability Index (higher NEVI score means higher vulnerability to environmental exposures), LA = Los Angeles, CA = California, GA = Georgia, NYC = New York City, ED = emergency department, SD = standard deviation, IQR = interquartile range
Linear Regression Estimates
Table 2 identifies the linear regression estimates corresponding to the relationship between NEVI score (overall and domain-specific) and pediatric asthma ED visits for LA County, Fulton County, and NYC. Across each area, we found that a 0.1 increase in NEVI score, indicating greater environmental vulnerability, corresponded with greater pediatric asthma ED visits. The magnitude of beta coefficients is not directly comparable across the three areas as NEVIs are calculated within each area separately and each area has a different magnitude of pediatric asthma ED visits. However, in examining the relationship between NEVI and pediatric asthma ED visits, the demographic NEVI score consistently produced the beta coefficient of the greatest magnitude while the residential NEVI score consistently produced the beta coefficient with the lowest magnitude across all three metropolitan areas.
Table 2.
Linear Regression Estimates Regarding the Relationship between NEVI (Overall & Domain-Specific) and Annual Rates of Pediatric Asthma1 ED Visits (per 10,000) using LA County (CA), Fulton County (GA), and NYC Zip Codes2
| LOS ANGELES COUNTY (CA) | ||
|---|---|---|
| Pediatric Asthma ED Visit Rate (per 10,000) | Beta Coefficient (95% CI)3 | Adjusted Model R-Squared4 |
| Model 1: Overall NEVI | 31.87 (26.78, 36.96) | 0.41 |
| Model 2: Demographic NEVI | 51.48 (43.35, 59.60) | 0.41 |
| Model 3: Economic NEVI | 28.07 (23.85, 32.29) | 0.44 |
| Model 4: Residential NEVI | 13.53 (6.26, 20.80) | 0.05 |
| Model 5: Health Status NEVI | 18.04 (15.23, 20.85) | 0.42 |
| FULTON COUNTY (GA) | ||
| Pediatric Asthma ED Visit Rate (per 10,000) | Beta Coefficient (95% CI) | Adjusted Model R-Squared |
| Model 1: Overall NEVI | 56.25 (47.56, 64.94) | 0.77 |
| Model 2: Demographic NEVI | 60.39 (47.85, 72.92) | 0.65 |
| Model 3: Economic NEVI | 48.22 (40.87, 55.56) | 0.77 |
| Model 4: Residential NEVI | 32.20 (14.37, 50.03) | 0.19 |
| Model 5: Health Status NEVI | 35.23 (29.57, 40.89) | 0.75 |
| NEW YORK CITY | ||
| Pediatric Asthma ED Visit Rate (per 10,000) | Beta Coefficient (95% CI) | Adjusted Model R-Squared |
| Model 1: Overall NEVI | 134.47 (116.56, 152.39) | 0.56 |
| Model 2: Demographic NEVI | 161.05 (142.76, 179.34) | 0.64 |
| Model 3: Economic NEVI | 97.42 (85.10, 109.73) | 0.59 |
| Model 4: Residential NEVI | 29.36 (3.45, 55.26) | 0.02 |
| Model 5: Health Status NEVI | 63.36 (50.72, 76.00) | 0.37 |
Pediatric Asthma ED Visits pertain to those between 0 to 19 years of age
Results correspond to a 0.1 increase in NEVI and domain-specific NEVI indicators
All standardized beta coefficients are significant with p-values <0.05
All R-coefficients of determination are significant with p-values <0.05
Acronyms: NEVI = Neighborhood Environmental Vulnerability Index, LA = Los Angeles, CA = California, GA = Georgia, NYC = New York City, ED = emergency department, SD = standard deviation, IQR = interquartile range
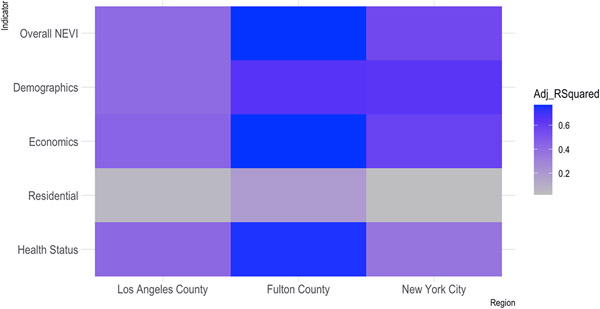
Adjusted R-Squared Values
We presented a heatmap to plot the distribution of the adjusted R-squared values by model and region (Figure 1). Higher adjusted R-squared values suggest that the model explained higher variance of the outcome. Overall NEVI scores explained at least 40% of the variance in pediatric asthma ED visits across LA County, Fulton County, and NYC. The residential NEVI score explained the least variance in pediatric asthma ED visits across each area. Overall and domain-specific NEVI scores explained more of the variance in pediatric asthma ED utilization in Fulton County, when compared to the variance that the NEVI scores explained for LA County or NYC. Overall, we found that Fulton County exhibited the highest adjusted R-squared values corresponding to linear regression models that either included the overall NEVI score, or a domain-specific NEVI score.
Figure 1. Heatmap of the Variance Explained (Adjusted R-Squared Values) Using the Linear Regression Models Examining the Relationship between NEVI and Pediatric Asthma ED Visits (per 10,000)1.
1 Adjusted R-squared values are plotted by metropolitan area (Los Angeles County, Fulton County, New York City) on the x-axis and by the individual explanatory variable included in the linear regression model (e.g., overall NEVI score, type of domain-specific NEVI score) on the y-axis
Acronyms: NEVI = Neighborhood Environmental Vulnerability Index; ED = emergency department
Location-Specific Results
In exploratory analyses, we examined location-specific findings among the three metropolitan areas. In Fulton County, the city of East Point, GA yielded an overall NEVI score of 0.40 and the fourth highest pediatric asthma ED visit rate in Fulton County (209.3 per 10,000), while Milton, GA yielded a lower overall NEVI score of 0.19 and the lowest pediatric asthma ED visit rate in Fulton County (28.1 per 10,000). In NYC, the Upper East Side yielded an overall NEVI score of 0.27, and the second lowest pediatric asthma ED visit rate in NYC (20.2 per 10,000), while Harlem yielded an overall NEVI score of 0.38, and the highest pediatric asthma ED visit rate in NYC (597.2 per 10,000). In LA County, we found an inverse association between NEVI and pediatric asthma ED visit rates in Antelope Valley (Northeastern LA County), as the pediatric asthma ED visit rate was relatively high (163.7 per 10,000), while the overall NEVI score (0.32) was average. As the NEVI scores are not standardized across cities, each metropolitan area’s scores are comparable only to themselves for better local contextualization.
Discussion
We found that greater neighborhood-level vulnerability to environmental exposures is associated with greater pediatric asthma morbidity within each of the three US metropolitan areas, including LA County, Fulton County, and NYC, as higher overall and domain-specific NEVI scores were associated with greater pediatric asthma ED visit rates. This suggests that NEVI may have utility in capturing the built and social environment characteristics to operationalize neighborhood-level vulnerability to environmental exposures, and thereby, can help identify neighborhoods with greater burden of environmentally-related health outcomes, such as pediatric asthma morbidity. Thus, NEVI can be used to identify neighborhoods in need of greater public health resources to help mitigate vulnerability to environmental exposures, and the burden of environmentally-related health outcomes in the future.
We found that overall and domain-specific NEVI scores explained more of the variance in pediatric asthma ED visits in Fulton County than in LA County and NYC. Thus, the overall and domain-specific NEVI scores had better predictive power in determining pediatric asthma ED visits in Fulton County than in LA or NYC, as the NEVI scores explained more of the variation in pediatric asthma ED visit rates in Fulton County than in LA County or NYC. In addition, we found that the economic, demographic, and health status domain-specific NEVI scores explained more of the variance in pediatric asthma ED visits, than the residential domain-specific NEVI score, for these three metropolitan areas. This finding may suggest that the economic, demographic, and health status domain-specific NEVI scores may better characterize vulnerability to environmental exposures, and better explain variation in morbidity of environmentally-related outcomes.
The NEVI tool encompasses multiple strengths as it comprises of an overall index score, and four domain-specific scores, pertaining to demographics, economic indicators, residential characteristics, and health status characteristics. In contrast, other indices that measure social vulnerability, such as the Area Deprivation Index, Community Needs Index, and Distressed Communities Index cannot be stratified into smaller subdomains.56 Although the Social Vulnerability Index (SVI) can be stratified into smaller domains, the SVI is not informed by the health characteristics of a neighborhood, such as health outcomes, health behaviors, and health insurance access.56 Health characteristics is an important domain to consider given that studies suggest that neighborhood-level health outcomes can influence the health of an individual.57 Therefore, in using NEVI, we can implement a holistic approach in assessing neighborhood environmental vulnerability, and ascertain how different domains may be most strongly related with environmentally-related outcomes.
In developing NEVI, we intentionally excluded racial or ethnic origin from our contributory features as we hypothesized that race is not itself a contributory factor to vulnerability to environmental exposures; rather, systemic policies affecting demographic, economic, residential and health vulnerabilities disproportionately impact US racial minorities.39 In delving deeper into the local context of our findings, we found evidence that NEVI may be distributed along racial lines. For example, the city of East Point in Fulton County with a relatively high NEVI score and high pediatric asthma ED visit rate, is predominantly Black in terms of demographic make-up (77.75% as of 2020) and Milton, with a relatively low NEVI score and low pediatric asthma ED visit rate, is predominantly White (73.23% as at 2020). We found similar patterns in NYC, with the Upper East Side, with a relatively low NEVI score and low pediatric asthma ED visit rate, having a predominantly White population (72.5% as of 2020), in contrast to Harlem, with a relatively higher NEVI score and high pediatric asthma ED visit rate, having a predominantly Black population (54.3% as of 2020).58 Therefore, our study demonstrates the overall and domain-specific impacts of systemic racism on children’s health in three different city environments. Different NEVI domains allow these inequities to be targeted based on the infrastructural, economic, political origins of these disparities, that are locally specific.
We also found higher pediatric asthma ED visit rates in Antelope Valley (LA County, CA) than one would expect based on its NEVI score, as the pediatric asthma ED visit rate was relatively high while the overall NEVI score was average. We further found that the percent of children seeking asthma-related care in an ED setting in Antelope Valley is 65% higher than the national average.59 Antelope Valley is a rural area with high particulate matter pollution; thus, it may not have the typical urban characteristics that would drive the NEVI score to be higher, but it does have higher environmental exposures. It is possible that the low residential NEVI score (0.20) may contribute to a lower overall NEVI score, highlighting that the residential NEVI score may not have strong utility in operationalizing neighborhood environmental vulnerability in rural contexts. In contrast, the health status NEVI score, which operationalizes neighborhood environmental vulnerability driven by health behaviors, outcomes, prevention practices, and access, was the highest NEVI domain score (0.47) and better characterized the high pediatric asthma ED visit rate in Antelope Valley. This suggests that there is also value in looking at domain-specific NEVI scores when gauging the population’s environmental vulnerability.
Overall, our findings suggested that a composite measure of neighborhood environmental vulnerability and domain-specific measures of neighborhood environmental vulnerability were associated with pediatric asthma ED visits across LA County, Fulton County, and NYC. These findings are consistent with existing literature that demonstrates the impact of factors across multiple domains on pediatric asthma incidence and severity.40, 60-63 Studies have found that residential characteristics, such as household crowding and poor housing quality, are associated with higher pediatric asthma incidence. 64, 65 Similarly, studies identified low socioeconomic status to be associated with increased severity of pediatric asthma outcomes.66-68 This association is important to consider given that deleterious domain characteristics, such as poor housing quality and low socioeconomic status, occur together and cluster in racial and ethnic minority communities, as a result of place-specific, structurally racist policies. 18-25 Therefore, we must consider vulnerability to environmental exposures on a neighborhood-level using a composite index, such as the overall NEVI score or a domain-specific NEVI score that can identify groups of characteristics, specific to a given population, that impact vulnerability.
The strengths of the study include that we consistently measured NEVI and pediatric asthma outcomes by zip code unit across LA County, Fulton County, and NYC. We additionally used three major US metropolitan areas to identify the relationship between NEVI and pediatric asthma ED visits. The study limitations include the use of zip codes, which is a larger geographical unit than a census tract, and census tracts may offer more spatial granularity in studying neighborhood-level environmental vulnerability. However, pediatric asthma ED visits were not available by census tracts for all three areas that we studied. Another limitation included that each area had different data coverage, as NEVI and pediatric asthma data was available for 95% of the NYC zip codes, 77% of the LA County zip codes, and 62% of the Fulton County zip codes. Excess coverage from one area over another may mean that our findings may better characterize NYC and LA County, in comparison to Fulton County. An additional limitation is the inability to compare NEVI scores across the different metropolitan areas as the NEVI scores are standardized to each individual metropolitan area. While this allows us to capture differences in environmental vulnerability within an individual metropolitan area, NEVI scores standardized to nationwide data would allow comparability of NEVI scores across different geographical areas.
Future study directions include examining the relationship between NEVI and pediatric asthma outcomes within additional US metropolitan areas. Examining more cities may allow for more geographical heterogeneity, which may allow us to identify unique clusters of NEVI patterns across the US. Future studies can continue to assess the utility of the residential NEVI score and overall NEVI score in explaining pediatric asthma ED visits in other contexts, such as when NEVI is measured on a census tract level or in suburban and community environments. We can additionally explore the development of a residential NEVI domain score index that is more appropriate for rural communities. In regards to policy research, it is important to understand how specific policies contribute to the observed race/ethnicity-based health disparities evident in our study findings.
Conclusion
We found that greater neighborhood-level vulnerability to environmental exposures is associated with greater pediatric asthma morbidity across three US metropolitan areas: LA County, Fulton County, and NYC. Our findings suggest that NEVI can be used to identify the social and structural drivers contributing to environmentally-related diseases, and can help identify neighborhoods in need of greater resources to help mitigate their vulnerability to environmental exposures. NEVI can then help reduce the incidence of environmentally-related diseases in neighborhoods with a high vulnerability to environmental exposures, which may be comprised of minoritized and marginalized communities due to systemic racism. This is important as there is a current growing interest in studying racism at levels higher than interpersonal levels and researchers are grappling with measuring racism at community levels. The NEVI tool may provide an opportunity to advance thinking around this topic.
Supplementary Material
Key Messages.
We previously developed a neighborhood environmental vulnerability index (NEVI) to integrate built environment and social factors on a neighborhood-level to operationalize vulnerability to environmental exposures.
We found that greater neighborhood environmental vulnerability, measured via the NEVI tool, is associated with greater annual pediatric asthma emergency department (ED) visits and explains at least 40% of the variance of pediatric asthma ED visits in three US metropolitan areas: Los Angeles County (California), Fulton County (Georgia), and New York City (New York).
Given that vulnerability to environmental exposures are often clustered in US neighborhoods of minoritized and marginalized populations that have experienced disinvestment due to historical redlining and systemic racism, the NEVI tool provides an opportunity to disentangle contributors to racial health disparities, and identify neighborhoods in need of resources to mitigate environmentally-related disease disparities.
Funding Sources:
Funding was received from the National Institute of Environmental Health Sciences, (R00ES027022 (JAS), P30ES009089 (SLD, JAS), P30ES023515 (PES), and R01ES030717 (PES)), National Heart Lung and Blood Institute (K01HL140216 (SLD)), National Institute of Diabetes, Digestive and Kidney Disorders (K01DK107791 (SSA), P30DK111022 (EC)) and the Robert Wood Johnson Foundation-Amos Medical Faculty Development Award (SLD).) This study is a product of the HD4NYC project, a multi-institutional research platform to improve health equity in NYC, funded by Robert Wood Johnson Foundation to NYC DOHMH and New York Academy of Medicine (NYAM). Although the research described in this article was supported by an initiative funded in part by Robert Wood Johnson Foundation, it has not been subjected to review and, therefore, does not necessarily reflect the views of the foundation, and no official endorsement should be inferred.
Abbreviations
- NEVI
Neighborhood Environmental Vulnerability Index
- ED
Emergency Department
- LA
Los Angeles
- GA
Georgia
- NYC
New York City
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: All authors declare that they have no conflicts of interest.
References
- 1.Ferrante G, La Grutta S. The Burden of Pediatric Asthma. Front Pediatr. 2018;6:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sennhauser FH, Braun-Fahrlander C, Wildhaber JH. The burden of asthma in children: a European perspective. Paediatr Respir Rev. 2005;6(1):2–7. [DOI] [PubMed] [Google Scholar]
- 3.Castro-Rodriguez JA, Forno E. Asthma and COVID-19 in children: A systematic review and call for data. Pediatr Pulmonol. 2020;55(9):2412–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perry R, Braileanu G, Palmer T, Stevens P. The Economic Burden of Pediatric Asthma in the United States: Literature Review of Current Evidence. Pharmacoeconomics. 2019;37(2):155–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trivedi M, Denton E. Asthma in Children and Adults-What Are the Differences and What Can They Tell us About Asthma? Front Pediatr. 2019;7:256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guilbert T, Zeiger RS, Haselkorn T, Iqbal A, Alvarez C, Mink DR, et al. Racial Disparities in Asthma-Related Health Outcomes in Children with Severe/Difficult-to-Treat Asthma. J Allergy Clin Immunol Pract. 2019;7(2):568–77. [DOI] [PubMed] [Google Scholar]
- 7.Loftus PA, Wise SK. Epidemiology and economic burden of asthma. Int Forum Allergy Rhinol. 2015;5 Suppl 1:S7–10. [DOI] [PubMed] [Google Scholar]
- 8.Bryant-Stephens T. Asthma disparities in urban environments. J Allergy Clin Immunol. 2009;123(6):1199–206; quiz 207-8. [DOI] [PubMed] [Google Scholar]
- 9.Malleske DT, Bryant-Stephens TC, Montoya-Williams D. Childhood Asthma Disparities-Race, Place, or Not Keeping Pace? JAMA Pediatr. 2022;176(8):739–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang Q, Lamichhane R, Diggs LA. Disparities in emergency department visits in American children with asthma: 2006-2010. J Asthma. 2017;54(7):679–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sullivan PW, Ghushchyan V, Navaratnam P, Friedman HS, Kavati A, Ortiz B, et al. Exploring factors associated with health disparities in asthma and poorly controlled asthma among school-aged children in the U.S. J Asthma. 2020;57(3):271–85. [DOI] [PubMed] [Google Scholar]
- 12.Paciencia I, Cavaleiro Rufo J. Urban-level environmental factors related to pediatric asthma. Porto Biomed J. 2020;5(1):e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gelfand EW. Pediatric asthma: a different disease. Proc Am Thorac Soc. 2009;6(3):278–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vlahov D, Freudenberg N, Proietti F, Ompad D, Quinn A, Nandi V, et al. Urban as a determinant of health. J Urban Health. 2007;84(3 Suppl):i16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braveman PA, Arkin E, Proctor D, Kauh T, Holm N. Systemic And Structural Racism: Definitions, Examples, Health Damages, And Approaches To Dismantling. Health Aff (Millwood). 2022;41(2):171–8. [DOI] [PubMed] [Google Scholar]
- 16.Gee GC, Hicken MT. Structural Racism: The Rules and Relations of Inequity. Ethn Dis. 2021;31(Suppl 1):293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook Q, Argenio K, Lovinsky-Desir S. The impact of environmental injustice and social determinants of health on the role of air pollution in asthma and allergic disease in the United States. J Allergy Clin Immunol. 2021;148(5):1089–101 e5. [DOI] [PubMed] [Google Scholar]
- 18.Rauh VA, Landrigan PJ, Claudio L. Housing and health: intersection of poverty and environmental exposures. Ann N Y Acad Sci. 2008;1136:276–88. [DOI] [PubMed] [Google Scholar]
- 19.Braubach M, Fairburn J. Social inequities in environmental risks associated with housing and residential location--a review of evidence. Eur J Public Health. 2010;20(1):36–42. [DOI] [PubMed] [Google Scholar]
- 20.Jerrett M, McConnell R, Wolch J, Chang R, Lam C, Dunton G, et al. Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis. Environ Health. 2014;13:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Padula AM, Rivera-Nunez Z, Barrett ES. Combined Impacts of Prenatal Environmental Exposures and Psychosocial Stress on Offspring Health: Air Pollution and Metals. Curr Environ Health Rep. 2020;7(2):89–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Swope CB, Hernandez D, Cushing LJ. The Relationship of Historical Redlining with Present-Day Neighborhood Environmental and Health Outcomes: A Scoping Review and Conceptual Model. J Urban Health. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Novick LF. Community Segregation, Redlining, and Public Health. J Public Health Manag Pract. 2021;27(5):435–6. [DOI] [PubMed] [Google Scholar]
- 24.Lynch EE, Malcoe LH, Laurent SE, Richardson J, Mitchell BC, Meier HCS. The legacy of structural racism: Associations between historic redlining, current mortgage lending, and health. SSM Popul Health. 2021;14:100793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee EK, Donley G, Ciesielski TH, Gill I, Yamoah O, Roche A, et al. Health outcomes in redlined versus non-redlined neighborhoods: A systematic review and meta-analysis. Soc Sci Med. 2022;294:114696. [DOI] [PubMed] [Google Scholar]
- 26.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. [DOI] [PubMed] [Google Scholar]
- 27.Brewer M, Kimbro RT, Denney JT, Osiecki KM, Moffett B, Lopez K. Does neighborhood social and environmental context impact race/ethnic disparities in childhood asthma? Health Place. 2017;44:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hwa Jung K, Pitkowsky Z, Argenio K, Quinn JW, Bruzzese JM, Miller RL, et al. The effects of the historical practice of residential redlining in the United States on recent temporal trends of air pollution near New York City schools. Environ Int. 2022;169:107551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ratageri VH, Kabra SK, Dwivedi SN, Seth V. Factors associated with severe asthma. Indian Pediatr. 2000;37(10):1072–82. [PubMed] [Google Scholar]
- 30.Milligan KL, Matsui E, Sharma H. Asthma in Urban Children: Epidemiology, Environmental Risk Factors, and the Public Health Domain. Curr Allergy Asthma Rep. 2016;16(4):33. [DOI] [PubMed] [Google Scholar]
- 31.Zanobetti A, Ryan PH, Coull B, Brokamp C, Datta S, Blossom J, et al. Childhood Asthma Incidence, Early and Persistent Wheeze, and Neighborhood Socioeconomic Factors in the ECHO/CREW Consortium. JAMA Pediatr. 2022;176(8):759–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wong GW, Chow CM. Childhood asthma epidemiology: insights from comparative studies of rural and urban populations. Pediatr Pulmonol. 2008;43(2):107–16. [DOI] [PubMed] [Google Scholar]
- 33.Kozyrskyj AL, Kendall GE, Jacoby P, Sly PD, Zubrick SR. Association between socioeconomic status and the development of asthma: analyses of income trajectories. Am J Public Health. 2010;100(3):540–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grant EN, Lyttle CS, Weiss KB. The relation of socioeconomic factors and racial/ethnic differences in US asthma mortality. Am J Public Health. 2000;90(12):1923–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uong S, Zhou J, Lovinsky-Desir S, Albrecht S, Azan A, Chambers E, et al. The Creation of a Multidomain Neighborhood Environmental Vulnerability Index. medRxiv. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferreira JBB, Santos LLD, Ribeiro LC, Rodrigues Fracon BR, Wong S. Vulnerability and Primary Health Care: An Integrative Literature Review. J Prim Care Community Health. 2021;12:21501327211049705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rogers W, Lange MM. Rethinking the vulnerability of minority populations in research. Am J Public Health. 2013;103(12):2141–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beck AF, Huang B, Wheeler K, Lawson NR, Kahn RS, Riley CL. The Child Opportunity Index and Disparities in Pediatric Asthma Hospitalizations Across One Ohio Metropolitan Area, 2011-2013. J Pediatr. 2017;190:200–6 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123 Suppl 3:S174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen E, Schreier HM. Does the social environment contribute to asthma? Immunol Allergy Clin North Am. 2008;28(3):649–64, x. [DOI] [PubMed] [Google Scholar]
- 41.Lieu TA, Quesenberry CP Jr., Capra AM, Sorel ME, Martin KE, Mendoza GR. Outpatient management practices associated with reduced risk of pediatric asthma hospitalization and emergency department visits. Pediatrics. 1997;100(3 Pt 1):334–41. [DOI] [PubMed] [Google Scholar]
- 42.Schultz A, Martin AC. Outpatient management of asthma in children. Clin Med Insights Pediatr. 2013;7:13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cloutier MM, Wakefield DB. Translation of a pediatric asthma-management program into a community in Connecticut. Pediatrics. 2011;127(1):11–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.QuickFacts: Los Angeles County, California: United States Census Bureau; 2021. [Available from: https://www.census.gov/quickfacts/losangelescountycalifornia. [Google Scholar]
- 45.QuickFacts: Fulton County, Georgia: United States Census Bureau; 2021. [Available from: https://www.census.gov/quickfacts/fultoncountygeorgia. [Google Scholar]
- 46.QuickFacts: New York City, New York: United States Census Bureau; 2021. [Available from: https://www.census.gov/quickfacts/newyorkcitynewyork. [Google Scholar]
- 47.Ou CQ, Hedley AJ, Chung RY, Thach TQ, Chau YK, Chan KP, et al. Socioeconomic disparities in air pollution-associated mortality. Environ Res. 2008;107(2):237–44. [DOI] [PubMed] [Google Scholar]
- 48.Hajat A, Hsia C, O'Neill MS. Socioeconomic Disparities and Air Pollution Exposure: a Global Review. Curr Environ Health Rep. 2015;2(4):440–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Munoz-Pizza DM, Villada-Canela M, Reyna MA, Texcalac-Sangrador JL, Osornio-Vargas AR. Air pollution and children's respiratory health: a scoping review of socioeconomic status as an effect modifier. Int J Public Health. 2020;65(5):649–60. [DOI] [PubMed] [Google Scholar]
- 50.PLACES: Local Data for Better Health: Centers for Disease Control and Prevention; 2020. [Available from: https://www.cdc.gov/places/about/index.html. [Google Scholar]
- 51.Asthma Emergency Department Visit Rates: California Department of Public Health; 2019. [Available from: https://data.ca.gov/dataset/asthma-emergency-department-visit-rates. [Google Scholar]
- 52.Number of Asthma ER visits by Census Tracts for 0-19 year olds in Georgia 2008-2018: Georgia Department of Public Health; 2018. [Available from: https://gisdata.fultoncountyga.gov/datasets/GARC::number-of-asthma-er-visits-by-census-tracts-for-0-19-year-olds-in-georgia-2008-2018/explore?location=32.659365%2C-83.178301%2C7.56. [Google Scholar]
- 53.Asthma Data - New York State: New York State Department of Health; 2019. [Available from: https://www.health.ny.gov/statistics/environmental/public_health_tracking/health/asthma.htm. [Google Scholar]
- 54.Uong S, Zhou J, Lovinsky-Desir S, Albrecht S, Chambers E, Sheffield P, et al. Characterizing Overall and Domain-Specific Neighborhood Vulnerability to Environmental Pollution Across an Urban Center 2022. [Available from: jstingone/nvi: Code and resources for creating a neighborhood vulnerability index (github.com). [Google Scholar]
- 55.R Core Team. R: A language and environment for statistical computing: R Foundation for Statistical Computing; 2021. [Available from: https://www.r-project.org. [Google Scholar]
- 56.Carmichael H, Moore A, Steward L, Velopulos CG. Disparities in Emergency Versus Elective Surgery: Comparing Measures of Neighborhood Social Vulnerability. J Surg Res. 2020;256:397–403. [DOI] [PubMed] [Google Scholar]
- 57.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–45. [DOI] [PubMed] [Google Scholar]
- 58.American Community Survey (ACS): United States Census Bureau; 2020. [Available from: https://www.census.gov/programs-surveys/acs. [Google Scholar]
- 59.Drake J. Breathmobile can rescue students: Antelope Valley Press; [updated March 1 2020. Available from: https://www.avpress.com/news/breathmobile-can-rescue-students/article_0171023c-5b85-11ea-b52f-8747f615a9fd.html. [Google Scholar]
- 60.Cagney KA, Browning CR. Exploring neighborhood-level variation in asthma and other respiratory diseases: the contribution of neighborhood social context. J Gen Intern Med. 2004;19(3):229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jones KK, Anderko L, Davies-Cole J. Neighborhood Environment and Asthma Exacerbation in Washington, DC. Annu Rev Nurs Res. 2019;38(1):53–72. [DOI] [PubMed] [Google Scholar]
- 62.Rosenbaum E. Racial/ethnic differences in asthma prevalence: the role of housing and neighborhood environments. J Health Soc Behav. 2008;49(2):131–45. [DOI] [PubMed] [Google Scholar]
- 63.Grunwell JR, Opolka C, Mason C, Fitzpatrick AM. Geospatial Analysis of Social Determinants of Health Identifies Neighborhood Hot Spots Associated With Pediatric Intensive Care Use for Life-Threatening Asthma. J Allergy Clin Immunol Pract. 2022;10(4):981–91 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Northridge J, Ramirez OF, Stingone JA, Claudio L. The role of housing type and housing quality in urban children with asthma. J Urban Health. 2010;87(2):211–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hughes HK, Matsui EC, Tschudy MM, Pollack CE, Keet CA. Pediatric Asthma Health Disparities: Race, Hardship, Housing, and Asthma in a National Survey. Acad Pediatr. 2017;17(2):127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ungar WJ, Paterson JM, Gomes T, Bikangaga P, Gold M, To T, et al. Relationship of asthma management, socioeconomic status, and medication insurance characteristics to exacerbation frequency in children with asthma. Ann Allergy Asthma Immunol. 2011;106(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen E, Hanson MD, Paterson LQ, Griffin MJ, Walker HA, Miller GE. Socioeconomic status and inflammatory processes in childhood asthma: the role of psychological stress. J Allergy Clin Immunol. 2006;117(5):1014–20. [DOI] [PubMed] [Google Scholar]
- 68.Eum Y, Yoo E, Bowen E. Socioeconomic determinants of pediatric asthma emergency department visits under regional economic development in western New York. Soc Sci Med. 2019;222:133–44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.