Over 6 million individuals are living with Alzheimer’s Disease and Related Dementias (ADRD) in the United States; by 2060, this number is projected to increase to 14 million.1 Beyond those with severe cognitive impairment, many older persons live with mild cognitive impairment (MCI) that can affect memory, language, thinking, or judgment.2 The potential causal role of stressful experiences and social adversities in developing cognitive impairment in later life is of great interest to investigators of ADRD.3–5 Even so, the influence of institutional stressors—such as the carceral system—has been largely overlooked.
Since 2002, the United States has had the highest incarceration rate in the world, perpetuating a longstanding era of mass incarceration.6,7 There are 2 million individuals incarcerated in the U.S. on any given day.8 In addition, millions of formerly incarcerated persons face stressors associated with community reintegration.9,10 Incarceration is a stressor due to the harsh and restrictive conditions of confinement and an enduring stressor after release due to stigma and the erosion of social and economic opportunities that result from incarceration.11,12 In this manner, incarceration affects multiple facets of a person’s life and well-being,6,13,16,17 and is deeply disparate across racial lines, with Black persons being five times more likely to be incarcerated than White persons.6
Mass incarceration impacts many older Americans due to cohort effects and long sentence structures. Policy shifts starting in the 1970s resulted in an overreliance on prisons and more severe sentences.6 As a result, the incarceration rate increased every year from 1973 to 2008—a 500% increase in the incarceration rate during this period.7,13 The result has been a “graying” of the prison population.14 Currently, 1-in-5 (more than 250,000) persons incarcerated in prisons in 2020 were over 50 years of age;15 estimates project this number will rise to 1-in-3 by 2030.16 Consequently, millions of older adults are either currently or formerly incarcerated, and this number will increase further in the years to come.
Notwithstanding the trends noted above, there is limited understanding of the effects of incarceration on cognitive health or the prevalence of cognitive impairment and dementia among incarcerated or formerly incarcerated older adults. The few existing studies suggest a possible link between incarceration and cognitive impairment. Ahalt and colleagues17 studied 310 individuals aged 55 to 80 in two urban jails and found a high prevalence (78% of respondents) of MCI. Other research on U.S. veterans over 50 finds an elevated prevalence of MCI and dementia in formerly incarcerated veterans, with a small portion experiencing the onset of cognitive impairment before incarceration.18 Finally, recent work using data from the National Longitudinal Survey of Youth – 1979 finds respondents previously incarcerated at some point earlier in life had lower unadjusted cognitive functioning scores measured by the Modified Telephone Interview for Cognitive Status (TICS-m) in 2006 when respondents were 48 years old on average.19 While these studies provide important insights, there is limited research on the relationship between incarceration and cognitive impairment, with an astounding lack of research on older Black persons (those aged 65+ years) who are at a higher risk of cognitive impairment/ADRD in the general population.20 Our preliminary data analysis from the Health and Retirement Study (HRS), a large nationally representative sample of U.S. older adults, suggests that, among non-Hispanic Black individuals aged 65 and older, those who report a history of incarceration have lower cognitive performance than those who do not (Figure 1). Notably, this association was not present in any other racial or ethnic group. In addition, formerly incarcerated non-Hispanic Black persons report a maximum total congition score of 19, which is the lowest of any group in the sample. While this effect size is modest in this preliminary data, these estimates are likely conservative given that incarceration contributes to the premature mortality of Black persons.21 Furthermore, these preliminary results do not consider highly relevant factors such as duration of incarceration, number of times incarcerated, and when in the life-course incarceration took place.
Figure 1:
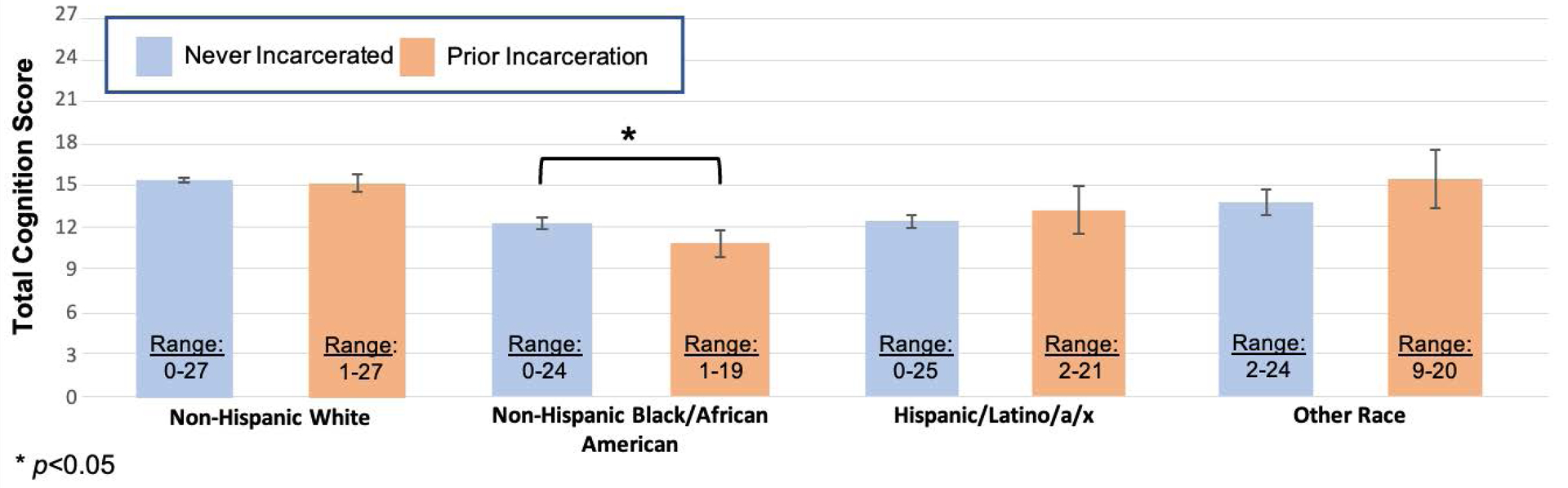
Comparison of cognitive performance between those previously vs. never incarcerated across racial groups, Health and Retirement Study, 2012, 2014; N=8,272
Notes: All data presented are for those aged 65+ years. “Total Cognition Score” (range from 0–27) is a sum of scores on immediate and delayed word recall, serial 7’s and backwards counting. Ranges for each subgroup on the “Total Cognition Score” are reported in the figure. Participants were asked about prior incarceration in either 2012 and 2014 HRS interviews, and data represent cognitive performance at the wave at which history of incarceration was reported.
Given the grim projections of rising rates of cognitive impairment,1 population aging,22 and the growth of older adults experiencing current or former incarceration,16 it is critical to carefully investigate the association between incarceration and cognitive impairment and ADRD. Below we identify seven areas that merit additional research.
First, research must investigate how earlier-life incarceration might contribute to cognitive decline, including ADRD. Incarceration influences health, serving as a psychological stressor, eroding social networks and connections to close interpersonal relationships, and exacerbating economic disadvantage.6,23,24 Considering that each is a social determinant of ADRD,25 it is critical to evaluate them as candidate pathways. Doing so could help build an understanding of how collateral consequences that stem from incarceration serve as a pathway from earlier-life incarceration to later-life cognitive impairment.
Second, it is important to consider the “dose” of incarceration, including the length of time served, the number of times incarcerated, and experiences endured while incarcerated. Theoretically, prolonged and repeated exposures to incarceration can result in greater stress and wear and tear on the body, potentially heightening ADRD risk. Alternatively, a longer duration of incarceration may result in adaptation to the carceral environment and the development of stable peer relationships, potentially reducing the incidence of stress-related illness,26–28 including perhaps ADRD. Research addressing these possibilities is lacking.
Third, researchers must assess how prior experiences with incarceration influence the risk of ADRD among older, formerly incarcerated persons living in the community. Around 95% of those incarcerated are eventually released, residing in the community rather than behind bars.29 While incarceration is a stressful experience that affects health,23,24 the stress and stigma endured after release30,31 often exacerbate health problems.24,32,33 Yet, the narrow literature on the cognitive consequences of incarceration primarily focuses on MCI among small samples of currently incarcerated persons,17,34 and the existing research among formerly incarcerated populations centers on individuals below age 65, leaving links between incarceration and post-release ADRD among older adults unexplored.19
Fourth, mass incarceration disproportionately affects Black and Brown Americans.35,36 Regarding healthy aging, research shows that among Black men, incarceration exposure is associated with accelerated aging.35 Accordingly, if incarceration contributes to the advanced epigenetic aging of Black persons,35,36 incarceration may also contribute to cognitive aging including development of ADRD among Black individuals through the weathering process,37 yet limited research examines this possibility.
Fifth, understanding the prevalence of cognitive impairment—including MCI and ADRD—among currently incarcerated populations is imperative. There are presently no estimates of the prevalence of MCI or ADRD in correctional settings or how that prevalence varies by race and ethnicity. Moreover, there is a lack of knowledge about the care received behind bars for incarcerated persons with cognitive impairment. Such work is necessary to illuminate the best practices in providing care for incarcerated persons with ADRD.
Sixth, qualitative data on the reentry experiences of recently incarcerated older persons with cognitive impairment remains very limited. Accordingly, scholars have overlooked this population’s actual reentry experiences and need from the perspective of affected individuals, their caregivers, and community services providers. Such research can inform future efforts to establish a streamlined and coordinated continuum of care after an individual’s release.
Finally, it is also critical to understand the possibility of reverse causality—that reduced cognitive reserves and cognitive impairment might be key risk factors for incarceration. For instance, impulsivity,38 lower intelligence,39 and brain injury40 are predictors of criminal involvement. One study among a representative veteran sample that experienced incarceration in mid-to-later life found that 3.3% had MCI or dementia before incarceration.18 Accordingly, there is a need for longitudinal data capturing cognitive health before, during, and after incarceration to more rigorously study the complex nexus between incarceration and cognitive impairment.34
Unfortunately, few data sources include high-quality information on ADRD, incarceration, and risk factors. It is vital to invest in new data sources moving forward to answer these questions. Ideally, this would include prospective longitudinal data with details of criminal justice system involvement (i.e., incarceration, duration, number of times incarcerated, experiences endured during incarceration), validated measures of cognitive impairment (i.e., Montreal Cognitive Assessment), as well as variables measuring genetic (i.e., family history), lifestyle (i.e., social isolation; physical inactivity; smoking), harmful events (i.e., traumatic brain injury) and/or psychological factors (i.e., history of major depression; stress) critical for a thorough causal investigation between incarceration and cognitive impairment and ADRD, as well as examining effect modification, mediation—and threats to valid inferences, such as confounding and selection bias. Aside from investing in new longitudinal data sources, several current designs could also be used to study core questions on incarceration and ADRD. First, questions regarding incarceration history can be added to existing, ongoing large-scale surveys of older populations, such as the National Health and Aging Trends Study (NHATS). Indeed, questions on incarceration were included in the Health and Retirement Study in 2012 and 2014 leave-behind questionnaire but have been discontinued; they should be repeated in future surveys to facilitate further research. Second, ongoing longitudinal studies in which respondents are approaching older ages, such as the National Longitudinal Study of Adolescent to Adult Health,41 and National Longitudinal Survey of Youth – 199742 include details on incarceration and cognitive impairment. However, moving forward, including more detailed information on incarceration history and validated cognitive impairment assessments would significantly improve the potential of future research. Finally, population register data such as in Nordic countries, which covers the entire population and often includes measures of dementia, incarceration, and comorbid risk factors, are valuable untapped sources that can be fundamental to pushing forward research in this area.43,44 Using rich longitudinal data can enable quasi-experimental designs such as matching and propensity score, fixed-effects modeling, or interrupted time series designs that better establish a causal association between incarceration and cognitive impairment.
In the coming decades, the number of persons with cognitive impairment in the population will increase,4, and many people with cognitive impairment will have spent some period of their lives incarcerated.16 Despite these projections, scholarship on the intersection between incarceration and cognitive impairment—including ADRD—is only in its infancy. Greater attention from the research community and further investment in data collection efforts can spur research that provides a deeper understanding of the nexus between incarceration and cognitive impairment.
Acknowledgments
Disclosures:
CNK is supported by the National Institute on Aging (K01AG061239). AS is supported by grants from the National Institute on Aging. He received payment for serving as a consultant for Merck and received honoraria from Springer Nature Switzerland AG for guest editing special issues of Current Sleep Medicine Reports. RT is supported by the National Institute of Aging (P30AG059298) and the National Institute on Minority Health and Health Disparities (U54MD000214)
Footnotes
Conflicts of interest: None
References
- 1.Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimers Dement. 2021;17(12):1966–1975. doi: 10.1002/alz.12362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hugo J, Ganguli M. Dementia and Cognitive Impairment: Epidemiology, Diagnosis, and Treatment. Clin Geriatr Med. 2014;30(3):421–442. doi: 10.1016/j.cger.2014.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moffitt TE, Belsky DW, Danese A, Poulton R, Caspi A. The Longitudinal Study of Aging in Human Young Adults: Knowledge Gaps and Research Agenda. J Gerontol A Biol Sci Med Sci. 2017;72(2):210–215. doi: 10.1093/gerona/glw191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sinclair DA, LaPlante MD. Lifespan: Why We Age—and Why We Don’t Have To. Simon and Schuster; 2019. [Google Scholar]
- 5.Röhr S, Pabst A, Baber R, et al. Social determinants and lifestyle factors for brain health: implications for risk reduction of cognitive decline and dementia. Sci Rep. 2022;12(1):12965. doi: 10.1038/s41598-022-16771-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Travis J, Western B, Redburn S. The Growth of Incarceration in the United States: Exploring Causes and Consequences. National Academies Press; 2014. [Google Scholar]
- 7.Garland D. Mass Imprisonment: Social Causes and Consequences. SAGE; 2001. [Google Scholar]
- 8.Kluckow R, Zeng Z. Correctional Populations in the United States, 2020. Bureau of Justice Statistics; 2020. [Google Scholar]
- 9.National Academies of Sciences E. The Effects of Incarceration and Reentry on Community Health and Well-Being: Proceedings of a Workshop.; 2019. doi: 10.17226/25471 [DOI] [PubMed] [Google Scholar]
- 10.Ahalt C, Bolano M, Wang EA, Williams B. The state of research funding from the National Institutes of Health for criminal justice health research. Ann Intern Med. 2015;162(5):345–352. doi: 10.7326/M14-2161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22(4):337–356. [PubMed] [Google Scholar]
- 12.Schnittker J, John A. Enduring stigma: the long-term effects of incarceration on health. J Health Soc Behav. 2007;48(2):115–130. doi: 10.1177/002214650704800202 [DOI] [PubMed] [Google Scholar]
- 13.Wagner P. Incremental declines can’t erase mass incarceration. Published June 5, 2018. Accessed December 27, 2022. https://www.prisonpolicy.org/blog/2018/06/05/annualchanges/
- 14.Kim K, Peterson B. Aging Behind Bars: Trends and Implications of Graying Prisoners in the Federal Prison System. Published online June 4, 2016. Accessed July 12, 2022. https://policycommons.net/artifacts/632665/aging-behind-bars/1613958/
- 15.Carson EA. Prisoners in 2020. Bureau of Justice Statistics; 2021:50. [Google Scholar]
- 16.Kuffel R, Byers A, Williams B, et al. High Occurrence of Dementia in Older Adults Returning to Community From Prison. Am J Geriatr Psychiatry. 2021;29(4):S45–S47. doi: 10.1016/j.jagp.2021.01.040 [DOI] [Google Scholar]
- 17.Ahalt C, Stijacic-Cenzer I, Miller BL, Rosen HJ, Barnes DE, Williams BA. Cognition and Incarceration: Cognitive Impairment and Its Associated Outcomes in Older Adults in Jail. J Am Geriatr Soc. 2018;66(11):2065–2071. doi: 10.1111/jgs.15521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuffel RL, Byers AL, Williams B, et al. Prevalence of dementia and mild cognitive impairment before incarceration. J Am Geriatr Soc. 2022;70(6):1792–1799. doi: 10.1111/jgs.17724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cox RJA, Wallace RB. The Role of Incarceration as a Risk Factor for Cognitive Impairment. J Gerontol B Psychol Sci Soc Sci. Published online September 25, 2022:gbac138. doi: 10.1093/geronb/gbac138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weuve J, Barnes LL, Mendes de Leon CF, et al. Cognitive aging in black and white Americans: Cognition, cognitive decline, and incidence of Alzheimer disease dementia. Epidemiol Camb Mass. 2018;29(1):151–159. doi: 10.1097/EDE.0000000000000747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bovell-Ammon BJ, Xuan Z, Paasche-Orlow MK, LaRochelle MR. Association of Incarceration With Mortality by Race From a National Longitudinal Cohort Study. JAMA Netw Open. 2021;4(12):e2133083. doi: 10.1001/jamanetworkopen.2021.33083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vespa J, Medina L, Armstrong DM. Population Estimates and Projections. United States Census Bureau; 2020:15. [Google Scholar]
- 23.Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. The Lancet. 2017;389(10077):1464–1474. doi: 10.1016/S0140-6736(17)30259-3 [DOI] [PubMed] [Google Scholar]
- 24.Massoglia M, Remster B. Linkages Between Incarceration and Health. Public Health Rep. 2019;134(1_suppl):8S–14S. doi: 10.1177/0033354919826563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stites SD, Midgett S, Mechanic-Hamilton D, et al. Establishing a Framework for Gathering Structural and Social Determinants of Health in Alzheimer’s Disease Research Centers. Meeks S, ed. The Gerontologist. 2022;62(5):694–703. doi: 10.1093/geront/gnab182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Porter LC, DeMarco LM. Beyond the dichotomy: Incarceration dosage and mental health*. Criminology. 2019;57(1):136–156. doi: 10.1111/1745-9125.12199 [DOI] [Google Scholar]
- 27.Porter LC, Kozlowski-Serra M, Lee H. Proliferation or adaptation? Differences across race and sex in the relationship between time served in prison and mental health symptoms. Soc Sci Med 1982. 2021;276:113815. doi: 10.1016/j.socscimed.2021.113815 [DOI] [PubMed] [Google Scholar]
- 28.Kreager DA, Young JTN, Haynie DL, Bouchard M, Schaefer DR, Zajac G. Where “Old Heads” Prevail: Inmate Hierarchy in a Men’s Prison Unit. Am Sociol Rev. 2017;82(4):685–718. doi: 10.1177/0003122417710462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Travis J. But They All Come Back: Facing the Challenges of Prisoner Reentry. The Urban Insitute; 2005. [Google Scholar]
- 30.Western B, Braga AA, Davis J, Sirois C. Stress and Hardship after Prison. AJS. 2015;120(5):1512–1547. doi: 10.1086/681301 [DOI] [PubMed] [Google Scholar]
- 31.Harding DJ, Wyse JJB, Dobson C, Morenoff JD. Making Ends Meet After Prison. J Policy Anal Manag J Assoc Public Policy Anal Manag. 2014;33(2):440–470. doi: 10.1002/pam.21741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Massoglia M. Incarceration as Exposure: The Prison, Infectious Disease, and Other Stress-Related Illnesses. J Health Soc Behav. 2008;49(1):56–71. doi: 10.1177/002214650804900105 [DOI] [PubMed] [Google Scholar]
- 33.Schnittker J, Massoglia M, Uggen C. Prisons and Health in the Age of Mass Incarceration. Oxford University Press; 2022. [Google Scholar]
- 34.Umbach R, Raine A, Leonard NR. Cognitive Decline as a Result of Incarceration and the Effects of a CBT/MT Intervention: A Cluster-Randomized Controlled Trial. Crim Justice Behav. 2018;45(1):31–55. doi: 10.1177/0093854817736345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berg MT, Rogers EM, Lei MK, Simons RL. Losing Years Doing Time: Incarceration Exposure and Accelerated Biological Aging among African American Adults. J Health Soc Behav. 2021;62(4):460–476. doi: 10.1177/00221465211052568 [DOI] [PubMed] [Google Scholar]
- 36.Berg MT, Rogers EM, Riley K, Lei MK, Simons RL. Incarceration exposure and epigenetic aging in neighborhood context. Soc Sci Med 1982. 2022;310:115273. doi: 10.1016/j.socscimed.2022.115273 [DOI] [PubMed] [Google Scholar]
- 37.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and Age Patterns of Allostatic Load Scores Among Blacks and Whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.White JL, Moffitt TE, Caspi A, Bartusch DJ, Needles DJ, Stouthamer-Loeber M. Measuring impulsivity and examining its relationship to delinquency. J Abnorm Psychol. 1994;103:192–205. doi: 10.1037/0021-843X.103.2.192 [DOI] [PubMed] [Google Scholar]
- 39.Loeber R, Menting B, Lynam D, et al. Findings From the Pittsburgh Youth Study: Cognitive Impulsivity and Intelligence as Predictors of the Age-Crime Curve. J Am Acad Child Adolesc Psychiatry. 2012;51:1136–1149. doi: 10.1016/j.jaac.2012.08.019 [DOI] [PubMed] [Google Scholar]
- 40.Williams WH, Chitsabesan P, Fazel S, et al. Traumatic brain injury: a potential cause of violent crime? Lancet Psychiatry. 2018;5(10):836–844. doi: 10.1016/S2215-0366(18)30062-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harris KM, Halpern CT. The National Longitudinal Study of Adolescent to Adult Health (Add Health): An Underused Resource for Developmental Science. Annu Rev Dev Psychol. 2022;4(1):null. doi: 10.1146/annurev-devpsych-120920-042217 [DOI] [Google Scholar]
- 42.Moore W, Pedlow S, Krishnamurty P, Wolter K. National Longitudinal Survey of Youth 1997 (NLSY97).
- 43.Anker AST, Wildeman C. Family Visitation Patterns during Incarceration in Denmark. J Fam Issues. Published online March 10, 2021. doi: 10.1177/0192513X21991187 [DOI] [Google Scholar]
- 44.Petersen JD, Wehberg S, Packness A, et al. Association of Socioeconomic Status With Dementia Diagnosis Among Older Adults in Denmark. JAMA Netw Open. 2021;4(5):e2110432. doi: 10.1001/jamanetworkopen.2021.10432 [DOI] [PMC free article] [PubMed] [Google Scholar]


