Abstract
Purpose:
To describe a novel presentation of conjunctival smooth muscle hamartoma and review the histopathologic findings of this entity.
Methods:
A 17-year-old African American male presented with a pink, non-tender lesion of the right bulbar conjunctiva that did not improve with medical management. He had no previous medical or ocular history. The lesion was excised.
Results:
Histopathologic examination disclosed morphologically benign smooth muscle bundles within the substantia propria that stained positively for smooth muscle actin, vimentin, and desmin consistent with the diagnosis of a smooth muscle hamartoma.
Conclusions:
While congenital smooth muscle hamartomas of the conjunctiva have been rarely reported in the literature, this is the first described case of a smooth muscle hamartoma presenting in adolescence in the bulbar conjunctiva. This lesion should be considered in the differential diagnosis for adolescents with similar appearing lesions.
Keywords: Smooth muscle hamartoma, conjunctiva, subepithelial conjunctival lesion, smooth muscle lesion, immunohistochemistry
Introduction
A variety of conjunctival lesions may arise in pediatric patients. It is important to rule out malignant pathologies, such as melanoma or lymphoma, in growing masses with concerning features. However, in children, lesions of the conjunctiva are generally benign or pre-malignant and nevus is the most common diagnosis.1
Other benign pathologies may be rarely present. One uncommonly reported lesion of the epibulbar tissue is a smooth muscle hamartoma, a disorderly expansion of smooth muscle cells, which has been discussed sparingly in the literature. While conjunctival smooth muscle hamartomas have been reported previously as congenital lesions in infants, to our knowledge, herein we report the first case of a conjunctival smooth muscle hamartoma presenting after infancy.
Case Presentation
A 17-year-old African American male presented with a complaint of a non-tender lesion on the surface of his right eye with the age of onset at approximately 16 years old. On examination, the patient had a 1.5cm reddish lesion on the inferonasal bulbar conjunctiva of the right eye (Figure 1A). The patient and family stated that the lesion was not present at birth and denied any relevant local trauma or medical history. Suspecting a pyogenic granuloma, topical prednisolone acetate 1% was used for several weeks with no improvement. The lesion continued to grow to approximately 2.0 cm with surrounding inflammation after follow up at nine months after presentation (Figure 1B). The lesion was then excised surgically. Histopathology demonstrated conjunctiva with a mild, chronic inflammatory infiltrate within the substantia propria and overlying non-neoplastic epithelium. CD31 immunohistochemical staining highlighted the blood vessel endothelium within the substantia propria (not shown). Irregular smooth muscle fibers were present within the substantia propria that stained red with Gomori trichrome and stained positively for vimentin, desmin, and smooth muscle actin (Figure 2). Ki-67 staining, a marker for cell proliferation, was negative within lesional tissue (not shown). No morphologic or immunohistochemical evidence of cellular atypia nor malignancy was present. These findings were most consistent with a diagnosis of a smooth muscle hamartoma of the conjunctiva.
Figure 1. External Photograph of Conjunctival Lesion.
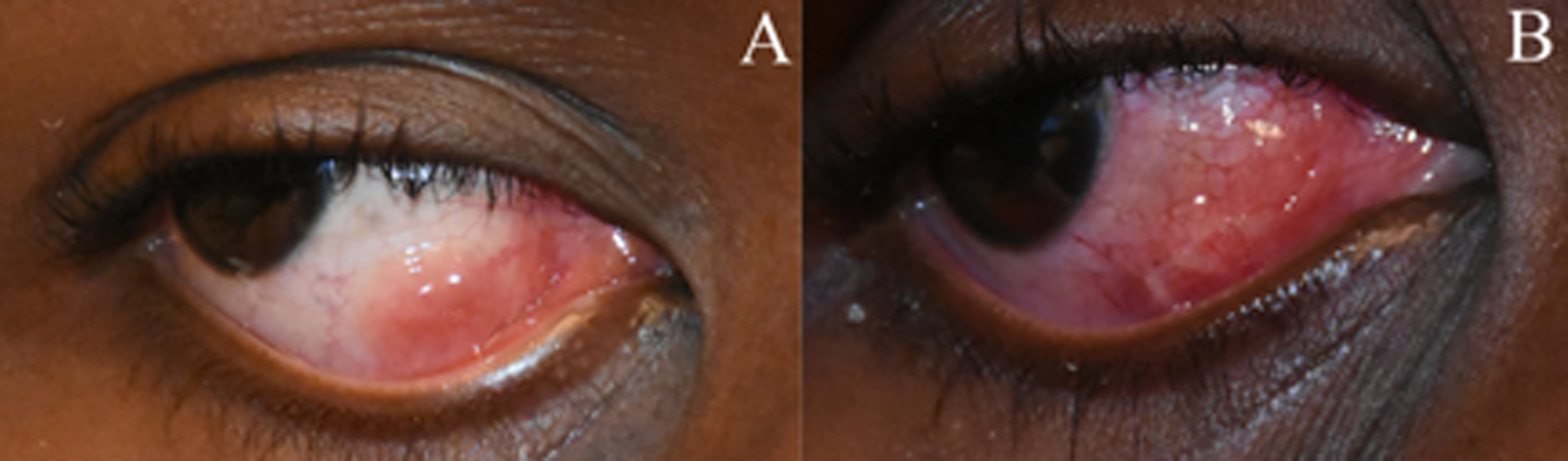
Clinical photograph of the right eye on initial presentation demonstrates a pink, red elevated lesion in the nasal bulbar conjunctiva (A). Nine months later, the lesion is larger in size with surrounding injection (B).
Figure 2. Histopathology of Conjunctival Lesion.
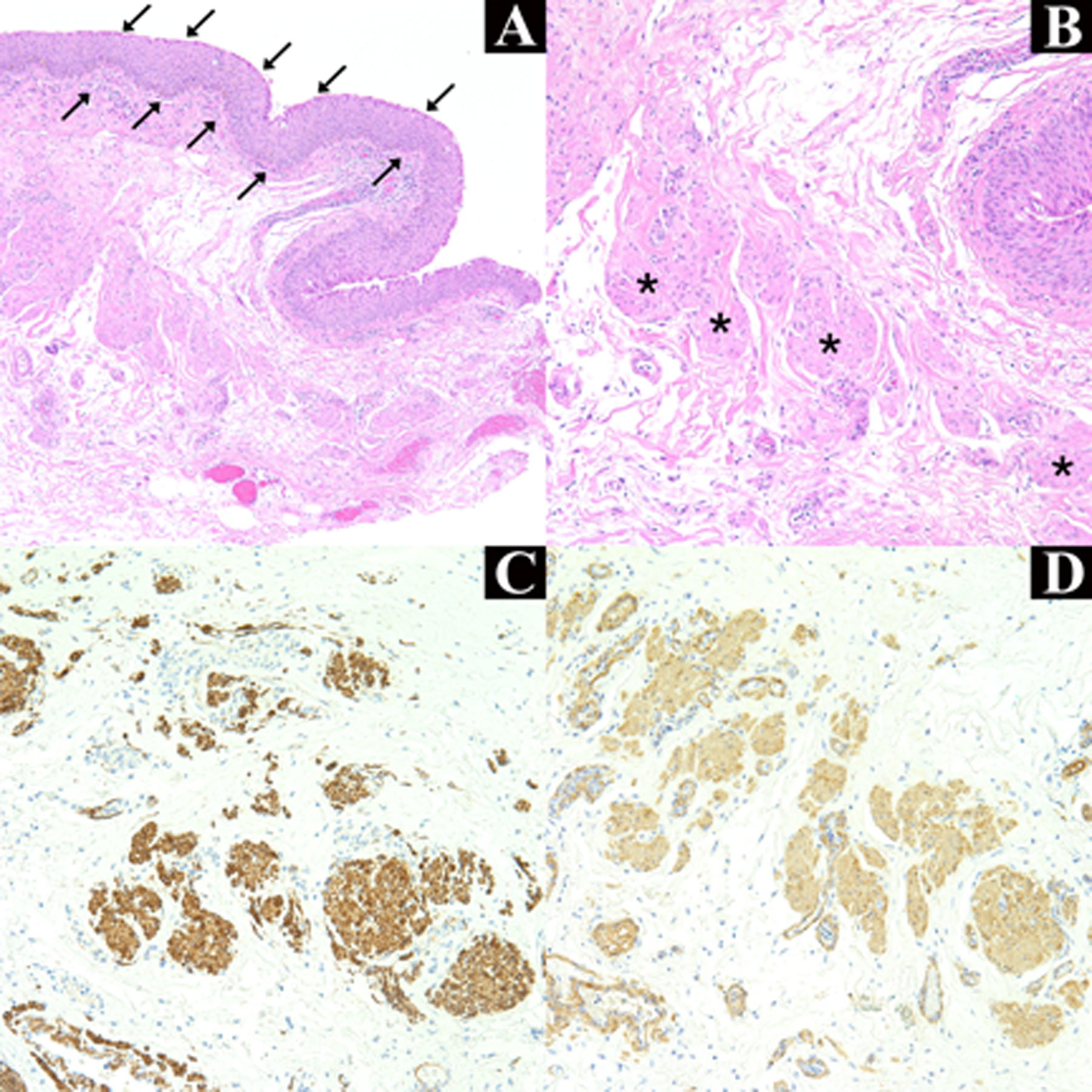
Acanthotic mucosal epithelium with squamous metaplasia (arrows) with underlying fibrovascular tissue within the substantia propria is present (A) (H&E, original magnification, × 100). Higher power demonstrates loose clusters of poorly circumscribed cells with eosinophilic cytoplasm and spindle-shaped nuclei consistent with smooth muscle (asterisks) (B) (H&E, original magnification × 200). Desmin (C) and smooth muscle actin (D) immunohistochemical stains are positive (original magnification, × 200).
Discussion/Conclusion
Smooth muscle hamartomas are benign, disorganized overgrowths of mature smooth muscle tissue in a location where smooth muscle is typically present. They are generally observed in the skin of the trunk and proximal extremities and can be broadly classified as congenital or acquired.2 While uncommon, a smooth muscle hamartoma can manifest in the periorbita as a pink-tan lesion on the eyelid and eyebrow.3 Conjunctival smooth muscle hamartoma has also previously been reported congenitally in infants three times.4–6
The first reported congenital conjunctival case presented in a 2-year-old male with a gray, cystic lesion of the left inferior conjunctival fornix. The lesion was excised and demonstrated irregular bundles of smooth muscle consistent with a diagnosis of a congenital smooth muscle hamartoma.4
The second case involved a 5-day-old male that presented with a cystic lesion in the tarsal conjunctiva of the right upper eyelid. Histopathologic evaluation demonstrated abnormal bundles of smooth muscle among blood vessels that were positive for desmin, vimentin, and smooth muscle actin, findings consistent with congenital smooth muscle hamartoma.5
The most recently reported case was that of a 2-month-old male with a bulbar mass. A cyst was seen on prenatal ultrasound and present at birth, obscuring the cornea. Examination of the lesion showed bundles of diffusely smooth muscle actin-positive tissue consistent with a smooth muscle hamartoma. This was the first reported case in the bulbar conjunctiva and limbal tissue and was thought to arise from the vascular endothelium in the limbus.6
Our case represents the fourth recorded presentation of a smooth muscle hamartoma in the conjunctiva and the first presenting in an adolescent individual. In this patient, the lesion was not noted at birth and therefore a congenital etiology was not initially considered. After treating as a pyogenic granuloma and ruling out lymphoma via flow cytometry, the initial suspected histopathologic diagnosis was a pinguecula based on the clinical presentation. However, solar elastosis was not present and the morphology and immunohistochemistry of the bundles of eosinophilic cells within the substantia propria were inconsistent with this diagnosis. The findings were more consistent with that of a benign smooth muscle lesion. Along with smooth muscle hamartoma, leiomyoma and leiomyosarcoma of the conjunctiva must be included in the differential diagnosis for subepithelial smooth muscle lesions in the conjunctiva. A leiomyoma is another benign lesion that has previously been described as a nodule on the lower eyelid, composed of intersecting fascicles of spindle-shaped cells.7 Conjunctival leiomyomas have also been reported to arise from the palpebral and epibulbar conjunctiva.8–10 Leiomyosarcoma, a malignant smooth muscle tumor, should also be considered in the differential diagnosis. Thirteen cases of this tumor have been previously reported on the conjunctiva.11 Histopathologic evaluation of this tumor demonstrates fascicles of smooth muscle cells with nuclear pleomorphism and variably present mitotic figures. To distinguish the lesion in this case from a leiomyosarcoma, Ki-67 staining, a marker for cell proliferation, demonstrated no cell cycling within the lesion. Furthermore, in comparison to smooth muscle hamartomas, both leiomyomas and leiomyosarcomas tend to be hypercellular and well-circumscribed lesions on histopathologic examination.
This case is unique compared to previous reported conjunctival occurrences because it was not present at birth nor did it progress in infancy, as seen in the other case reports. This patient seemingly first developed the lesion at sixteen with no previous history or risk factors. It then started gradually, but consistently, enlarging until the time of excision. As previously stated, smooth muscle hamartomas in other sites have been reported as acquired lesions presenting later in life.2 The key distinguishing factor between acquired and congenital lesions is the age of onset with no significant differences noted on histopathology. This case may be the first presentation of an acquired smooth muscle hamartoma in the conjunctiva. However, while it may have not been noticed by the patient or his family, it is likely that the lesion was present since birth with subsequent enlargement in adolescence.
The inciting factors for the development and progression of the lesion in this patient are still unknown. While the pathogenesis of this lesion is still unclear, previous research has demonstrated the presence of myofibroblasts in pterygium fibrovascular tissue, which stain positively with SMA.12 It is possible that the myofibroblasts present in the periorbital fibroadipose tissue near the nasal conjunctiva could play a role in the development of this lesion. The mass may also originate from the vascular smooth muscle, as the smooth muscle bundles observed in this case are interspersed with the vascular endothelium. Furthermore, it is also possible that the cells arose from the smooth muscle or the capsulopalpebral fascia of the lower eyelid, a pathogenesis that has been postulated in prior literature.4–6 An argument for this mechanism is the histologic similarity between this lesion and the normal smooth muscle of the eyelid retractor complex. It is important to state that if the lesion originated from these eyelid retractor muscles, then it would be more precise to describe the lesion as a choristoma instead of a hamartoma, the former of which is a proliferation of mature tissue in an abnormal location. However, the proximity to the vasculature of this lesion suggests that the most likely origin of the smooth muscle cells, in the authors’ opinion, is the smooth muscle in the blood vessels.
This case shares the same immunohistochemical staining pattern as the three previous cases However, there appears to be a varied morphologic presentation and circumscription, which may be related to the potential site of origin.
It should be noted that smooth muscle hamartomas have not been reported to recur or undergo malignant transformation in the previously reported ocular cases. This case highlights the importance of including smooth muscle hamartoma in the differential diagnosis for benign appearing subepithelial reddish conjunctival lesions, which may present from birth to adolescence.
Financial Support
Supported by NIH Center Core Grant P30EY014801, Research to Prevent Blindness Unrestricted Grant, Department of Defense (DOD- Grant # W81XWH-09-1-0675 and Grant # W81XWH-13-1-0048 ONOVA), and Florida Lions Eye Bank.
Footnotes
Conflict of Interest
The authors of this manuscript certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
References
- 1.Shields CL, Alset AE, Boal NS, Casey MG, Knapp AN, Sugarman JA, Schoen MA, Gordon PS, Douglass AM, Sioufi K, Say EA, Shields JA. Conjunctival Tumors in 5002 Cases. Comparative Analysis of Benign Versus Malignant Counterparts. The 2016 James D. Allen Lecture. Am J Ophthalmol. 2017. Jan;173:106–133. [DOI] [PubMed] [Google Scholar]
- 2.González IA, Dehner LP. Smooth muscle hamartoma and striated muscle hamartoma: Clinicopathologic characterization of two rare entities and literature review. J Cutan Pathol. 2021. Feb;48(2):237–246. [DOI] [PubMed] [Google Scholar]
- 3.Johnson MD, Jacobs AH. Congenital Smooth Muscle Hamartoma: A Report of Six Cases and a Review of the Literature. Arch Dermatol. 1989;125(6):820–822. [DOI] [PubMed] [Google Scholar]
- 4.Roper GJ, Smith MS, Lueder GT. Congenital smooth muscle hamartoma of the conjunctival fornix. Am J Ophthalmol. 1999. Nov;128(5):643–4. [DOI] [PubMed] [Google Scholar]
- 5.Mora LE, Rodríguez-Reyes AA, Vera AM, Rubio RI, Mayorquín-Ruiz M, Salcedo G. Congenital smooth muscle hamartoma of the palpebral conjunctiva. Ophthalmic Plast Reconstr Surg. 2012. Jul-Aug;28(4):e102–4. [DOI] [PubMed] [Google Scholar]
- 6.Bean A, Al-Bouri A, Bradford G, Mauger T. Congenital Smooth Muscle Hamartoma Obscuring the Cornea. Case Rep Ophthalmol Med. 2021;2021:6692229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hui JI, Buchser NM, Dubovy SR. Primary eyelid leiomyoma. Ophthalmic Plast Reconstr Surg. 2011. Jul-Aug;27(4):e102–3. [DOI] [PubMed] [Google Scholar]
- 8.Barsegian A, Ahmad A, Shinder R. Leiomyoma of the Palpebral Conjunctiva. Ophthalmology. 2017. Jan;124(1):65. [DOI] [PubMed] [Google Scholar]
- 9.Brannan SO, Cheung D, Trotter S, Tyler AJ, Reuser TQ. A conjunctival leiomyoma. Am J Ophthalmol. 2003. Oct;136(4):749–50. [DOI] [PubMed] [Google Scholar]
- 10.Afghani T, Khan FA, Mansoor H. Conjunctival Leiomyoma; a Rare Tumor of the Ocular Surface. J Ophthalmic Vis Res. 2016. Oct-Dec;11(4):433–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gameiro Filho AR, Castello Branco AMP, Rigueiro MP, Morales MC, Belfort RN. Conjunctival leiomyosarcoma. Am J Ophthalmol Case Rep. 2022. May 11;26:101580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Touhami A, Di Pascuale MA, Kawatika T, Del Valle M, Rosa RH Jr, Dubovy S, Tseng SC. Characterisation of myofibroblasts in fibrovascular tissues of primary and recurrent pterygia. Br J Ophthalmol. 2005. Mar;89(3):269–74. [DOI] [PMC free article] [PubMed] [Google Scholar]


