Abstract
Objective:
We assessed the preference for two behavioral weight loss programs, Diabetes Prevention Program (DPP) and Healthy Weight for Living (HWL) in adults with obesity.
Methods:
A cross-sectional survey was fielded on the Amazon Mechanical Turk. Eligibility criteria included reporting BMI ≥ 30 and at least two chronic health conditions. Participants read about the programs, selected their preferred program, and answered follow-up questions.
Results:
The estimated probability of choosing either program was not significantly different from 0.5 (N=1,005, 50.8% DPP and 49.2% HWL, p=0.61). Participants’ expectations about adherence, weight loss magnitude, and dropout likelihood were associated with their choice (p<0.0001). Non-White participants (p=0.040) and those with monthly income greater than $4,999 (p=0.002) were less likely to choose DPP. Participants who had postgraduate education (p=0.007), did not report high serum cholesterol (p=0.028), and reported not having tried losing weight before (p=0.025) were more likely to choose DPP. Those who chose HWL were marginally more likely to report that being offered two different programs rather than one would likely affect their decision to enroll in one of the two (p=0.052).
Conclusions:
The enrollment into DPP and HWL was balanced, but race, educational attainment, income, previous attempt to lose weight, and serum cholesterol levels had significant associations with the choice of weight loss program.
Keywords: Behavioral Intervention, Self-selection, Obesity, Preference, Weight Loss
Introduction
Traditional interventions for weight loss, including the Diabetes Prevention Program (DPP), are based on goal setting, improving self-efficacy, and fostering self-regulation skills. As part of their core strategies, such programs encourage participants to identify goals for energy intake, physical activity, and weight loss; to keep daily food and activity logs; and to give the logs to intervention counselors weekly for review and accountability [1]. Despite this recognized conceptual foundation, the mean weight loss achieved by participants of such lifestyle intervention programs (2–4%) [1, 2] is relatively lower than the amounts needed for clinically impactful benefits [3, 4]. In addition, weight regain is common [5]. The limited effectiveness of traditional weight loss programs may be due to limitations of the underlying health behavior change model [4] or the burdensome nature of the core program activities [6]. These concerns justify the development and testing of alternative types of behavioral interventions.
Members of our team developed the Healthy Weight for Living (HWL) program [7, 8], which is based on a revised health behavior change model with emphasis on biological factors that influence energy regulation (i.e., reducing hunger and food craving) and reducing participant burden (i.e., minimal emphasis on logging activities), as well as the psychological, environmental, and practical factors that are recognized in traditional models. In the two randomized trials evaluating its weight loss effectiveness, HWL resulted in weight loss of 8.0 kg [9] and 8.5% [8]. However, neither of these trials was designed to provide a rigorous evaluation of HWL against a traditional program.
Furthermore, the two programs, DPP and HWL, are so different in their implementation that they may appeal to different types of individuals, which complicates interpretation of results. Participants who are not assigned to a program they prefer may have different adherence than those who are, affecting their dropout rates and ultimately response to the treatment. Thus, as stated by Brewin and Bradley [10], “it will be difficult to distinguish between a treatment that failed because it was not inherently effective and one that failed because it was not targeted towards patients who […] were suitably motivated.” If participants are given the chance to self-select between programs, each intervention will potentially be given its best chance at supporting meaningful weight loss in a clinical setting. Moreover, giving participants the chance to choose their preferred program in research settings more closely replicates the choice between different types of weight loss options in the real-world clinical setting.
Despite those potential advantages, incorporating self-selection in a randomized trial comes with a risk of unbalanced enrollment into each intervention (that is, a different N in each group), which could result in an underpowered study (and thus an inability to detect differences between the two programs) or require the research team to make strong assumptions during the analysis [11]. Our motivation to conduct the current study was to inform the design of a two-stage randomized trial to examine the interacting effect of three qualities on weight loss outcomes of DPP and HWL: (1) preferred vs. nonpreferred, (2) self-selected vs. randomly assigned, and (3) DPP vs. HWL. In this pilot cross-sectional study, we provided the details of HWL and DPP to a broad and roughly representative sample of US adults with obesity and asked them to select one in which to enroll. Our primary hypothesis was that equal proportions of participants would prefer each program. We also examined potential associations of sociodemographic, health condition, and weight history characteristics with enrollment preference, and participants’ projected consequence of how programs are offered on their enrollment, retention, and weight loss success.
Methods
Study Design and Setting
This study was a crowdsourced cross-sectional survey. Participants were recruited through the Amazon Mechanical Turk (MTurk) platform from May 2021 through September 2021. MTurk is a crowdsourcing service by Amazon where one (as a requester) can outsource tasks to users (i.e., workers) to be performed virtually (see www.mturk.com). The types of tasks requested can include survey participation, content moderation, data validation, or similar work. Eligibility assessment and data capture were conducted by using a questionnaire designed by the research team and developed on Qualtrics (See Supplemental Table S1). Participants were not informed about the eligibility criteria or that the study was related to preference of weight loss programs. All procedures were approved by the Indiana University Institutional Review Board (#10502).
Participants
Sample size
We calculated that a sample size of 1,000 could provide a margin of error ±0.03 (3.0%) for the estimated proportion who would choose either of the two weight loss programs. For example, if the observed proportion who preferred DPP was 0.5 (50%), the 95% confidence interval (95% CI) for our estimate in the population would be 0.47 to 0.53 (47% to 53%).
Recruitment, Measures, and Procedures
We specified a set of qualification and exclusion criteria based on prior recommendations for improving the validity of data provided by MTurk workers [12]. Qualified workers needed to claim U.S. residency, have a successful task completion rate of >95% on MTurk, and have a minimum of 100 and a maximum of 10,000 completed tasks. Workers must be 18 years of age or older to join MTurk, which set a default age criterion for this study.
Screening
Inclusion criteria were a BMI of 30 kg/m2 or higher (calculated on the basis of self-reported weight and height) and reporting at least any two of the following conditions: diabetes, hypertension or using medications to lower blood pressure, high cholesterol level or using medications to reduce cholesterol, history of heart disease or stroke, arthritis with limitations for walking or activities of daily living such as personal care, and any cancer requiring treatment within past 5 years. Those reporting having a history of gastric bypass surgery, being pregnant, or being “very unlikely” to enroll in a weight loss program offered at no cost by their health care provider or employer were excluded.
In addition, those who failed to pass checks for inattention, possible virtual private network (VPN) use, or untruthfulness were also excluded [12]. These questions were embedded at the beginning of the survey. For participants who failed one or more checks, the survey ended, and ineligible participants were instructed to return the task (i.e., Human Intelligence Task (HIT)) to MTurk and not to file for payment. When they completed the survey, eligible participants were given a randomly generated 10-digit code to use when they submitted a payment claim. Participants who submitted valid completion codes (i.e., codes that matched in the Qualtrics survey and MTurk platforms) were paid $3.00.
Measures and Procedures
Question wording and response options for all items are available in Supplemental Table 1. Participants’ self-reported sociodemographic characteristics were collected for gender, ethnicity, race, age, highest completed level of education, state of residence, household monthly income, and employment status. Additional self-reported data were collected for the following: current weight; weight 1 year ago; height; having diabetes, hypertension, high serum cholesterol, history of heart disease or stroke, arthritis with limitations for walking or daily living activities, or any cancer requiring treatment within past 5 years; likeliness to participate in a cost-free weight loss program; influence of cost on interest in participating in a weight loss program; previous attempt(s) to lose weight; and type(s) and number of previous attempts to lose weight.
Participants were then shown summaries of two weight loss programs (DPP as Program A, HWL as Program B; see Supplemental Table 1 on the next page) and were asked three questions to improve and examine their understanding of the programs. Finally, they were asked to choose which program they preferred and to answer exploratory questions about their preferences. For readers’ convenience in navigating questions and corresponding results, and to avoid text redundancy, exploratory questions are outlined in the Results section.
Statistical Analyses
Data analysis was done using R version 4.1.3(2022-03-10). Independent sample t-tests and Pearson Chi-square tests of independence were used to compare BMI, sociodemographic characteristics, health conditions, weight history, performance in comprehension questions, and exploratory metrics of program preference between participants who chose DPP and those who chose HWL. To assess the main hypothesis, we tested whether the proportion of those choosing DPP or HWL was significantly different from 0.5 using a two-sided exact binomial test of one proportion (i.e., an exact test of a null hypothesis about the probability of success in a Bernoulli experiment). We then compared DPP and HWL groups in terms of proportions of reported likeliness to enroll when the only choice was the not-preferred program using a two-proportions z-test. A Wilcoxon rank sum test was used to test whether the two groups’ ranking of delivery methods had the same distribution. Associations of BMI, sociodemographic characteristics, health conditions, weight history, and their interactions with choosing DPP vs. HWL were assessed in a multiple logistic regression model. Significance tests were 2-tailed with alpha=0.05. Raw (unadjusted) p-values are reported throughout, and Bonferroni adjustment is used for multiple comparisons of each demographic category vs the reference level where applicable (e.g. for education and income) in the logistic regression.
Results
Participants
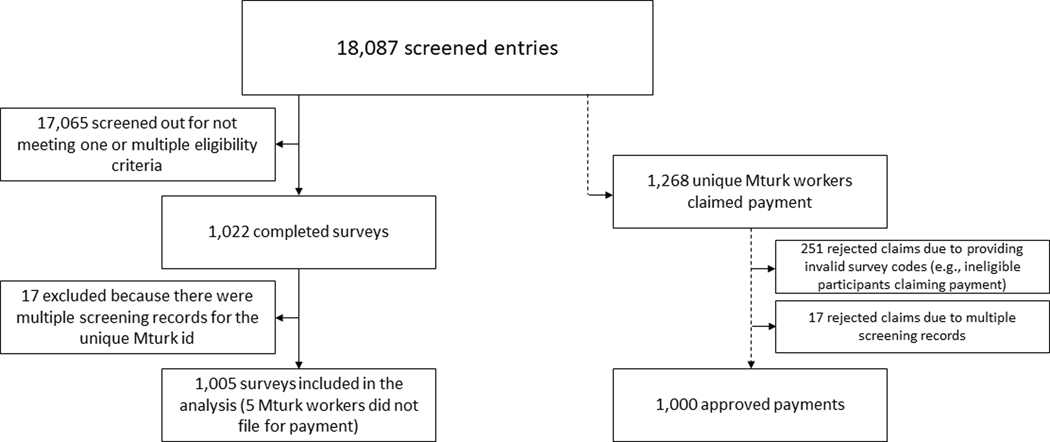
A total of 18,087 survey forms were initiated on Qualtrics, and 1,022 completed surveys were recorded (Figure 1). Separately, 1,268 unique MTurk workers submitted the HIT within MTurk to claim payment. Among those, 1,000 submissions were approved and 268 were rejected. Among the rejected HITs, 251 were rejected because they did not submit a valid 10-digit code. The remaining 17 had multiple screening records (i.e., multiple attempts to pass screening). These 17 entries were also excluded from completed surveys on the survey platform. In addition, 5 participants fully completed the survey in Qualtrics but did not submit a request for payment. These cases were retained for analysis. Thus, 1,005 surveys were confirmed to be included in the analysis. For the core concepts underlying our data cleaning discrepancy resolution, see [12].
Figure 1:
Flow of participant screening, inclusion, and payment approval on the Amazon Mechanical Turk (MTurk) worker platform
Descriptive Data
The sociodemographic characteristics, chronic health conditions, and weight change histories of the participants are shown in Table 1. There were no statistically significant differences between participants who chose either of the two programs in BMI (DPP: mean [sd]= 39.02 [7.17] kg/m2; HWL: mean [sd]= 38.51 [7.07] kg/m2, t=1.14, p=0.253), sociodemographic characteristics, health conditions, or weight change history. The distribution of included participants by U.S. state normalized per 1 million adult residents is illustrated in Supplemental Figure S1.
Table 1:
Sociodemographic characteristics, chronic health conditions, and weight change history of participants (N=1,005)
| Chose DPP, n=511 n(% of total participants) | Chose HWL, n=494 n(% of total participants) | p-value | ||
|---|---|---|---|---|
| Age, years | <25 | 13 (1.3) | 13 (1.3) | 0.959 |
| 25–34 | 111 (11.0) | 100 (10.0) | ||
| 35–44 | 119 (11.8) | 111 (11.0) | ||
| 45–54 | 106 (10.5) | 104 (10.3) | ||
| 55≤ | 162 (16.1) | 166 (16.5) | ||
| Gender Identity | Female | 334 (33.2) | 319 (31.7) | 0.686 |
| Male | 169 (16.8) | 170 (16.9) | ||
| Other1 | 8 (0.8) | 5 (0.5) | ||
| Race | White | 439 (43.7) | 404 (40.2) | 0.090 |
| Black and other2 | 72 (7.2) | 90 (9.0) | ||
| Ethnicity | Non-Hispanic/Latino | 462 (46.0) | 459 (45.7) | 0.187 |
| Hispanic/Latino | 49 (4.9) | 35 (3.5) | ||
| Education | High school or less3 | 127 (12.6) | 143 (14.2) | 0.247 |
| Associate degree | 97 (9.7) | 86 (8.6) | ||
| Bachelor’s degree | 140 (13.9) | 145 (14.4) | ||
| Graduate level4 | 147 (14.6) | 120 (11.9) | ||
| Employment Status | Work full-time | 291 (29.0) | 271 (27.0) | 0.917 |
| Work part-time | 39 (3.9) | 35 (3.5) | ||
| Self-employed | 65 (6.5) | 65 (6.5) | ||
| Full-time student | 9 (0.9) | 11 (1.1) | ||
| Not working5 | 107 (10.6) | 112 (11.1) | ||
| Average monthly household income | $1,000-$1,9996 | 120 (11.9) | 97 (9.7) | 0.295 |
| $2,000-$2,999 | 97 (9.7) | 102 (10.1) | ||
| $3,000-$3,999 | 87 (8.7) | 76 (7.6) | ||
| $4,000-$4,999 | 85 (8.5) | 77 (7.7) | ||
| $5,000 and above | 122 (12.1) | 142 (14.1) | ||
| How likely to participate in a cost-free weight loss program offered by health care provider, employer, etc. in person or by videoconference? | Very likely | 318 (31.6) | 292 (29.1) | 0.217 |
| Somehow likely | 74 (7.4) | 71 (7.1) | ||
| Decision depends on program features | 103 (10.2) | 122 (12.1) | ||
| Unlikely to enroll | 16 (1.6) | 9 (0.9) | ||
| Have tried losing weight before? | Yes | 489 (48.7) | 484 (48.2) | 0.060 |
| No | 22 (2.2) | 10 (1.0) | ||
| Weight change over the past year¶ | Gained weight | 302 (30.1) | 285 (28.4) | 0.834 |
| Lost weight | 170 (16.9) | 168 (16.7) | ||
| Constant weight | 38 (3.8) | 41 (4.1) | ||
| Diabetes | Yes | 288 (28.7) | 282 (28.1) | 0.866 |
| No | 223 (22.2) | 212 (21.1) | ||
| Hypertension or using medications to lower blood pressure | Yes | 429 (42.7) | 423 (42.1) | 0.515 |
| No | 82 (8.2) | 71 (7.1) | ||
| High cholesterol or using medications to reduce cholesterol | Yes | 327 (32.5) | 345 (34.3) | 0.057 |
| No | 184 (18.3) | 149 (14.8) | ||
| History of heart disease or stroke | Yes | 164 (16.3) | 151 (15.0) | 0.650 |
| No | 347 (34.5) | 343 (34.1) | ||
| Arthritis with limitations for walking or activities of daily living such as personal care | Yes | 136 (13.5) | 128 (12.7) | 0.856 |
| No | 375 (37.3) | 366 (36.4) | ||
| Any cancer requiring treatment within past 5 years | Yes | 41 (4.1) | 30 (3.0) | 0.279 |
| No | 470 (46.8) | 464 (46.2) | ||
| Influence of program’s cost on decision to participate or not | Would not do the program unless offered cost free7 | 69 (6.9) | 71 (7.1) | 0.657 |
| May do the program even if not cost-free8 | 435 (43.3) | 413 (41.1) | ||
| Non-sense response9 | 7 (0.7) | 10 (1.0) |
Chi-square test of independence.
Derived from difference of self-reported current weight and last year’s weight.
Transgender (n=8) and other (n=5) merged.
Black participants choosing DPP (n=45), Black participants choosing HWL (n=52); Other: Asian (n=20), Native Hawaiian (n=4), and other (n=41).
Less than high school (n=6) and high school/GED (n=264) merged.
Doctorate degree (n=11) and master’s degree (n=256) merged.
‘do not work’ (n=121) and retired (n=98) merged.
Less than $1,000 (n=0).
These two were merged: “Would not do the program unless offered cost free” (n=63), selected both “Would not do the program…” AND “Most interested if the program is offered cost free”(n=77).
These three were merged: “Most interested if the program is offered cost free” (n=425), “Would still enroll if there is a co-payment “ (n=179), respondent selected both “most interested […]” and “would still enroll […]” (n=244).
None-sense combinations: e.g., selected all three options or selected co-payment AND cost-free only.
Comprehension of Program Characteristics
Before choosing their preferred weight loss program, the participants answered three questions gauging their comprehension of the characteristics of the two programs. Proportions of correct answers were 85.5%, 94.5%, and 98.2% for the three questions, respectively (see Table 2). The relations between the correct answer and the selected program were statistically significant for the two multiple-choice questions with two options (e.g., identifying which program had a certain feature; p <0.001 [Pearson Chi-square test of independence]) but not for the question requiring selection of accurate statements. We further explored this in a logistic regression model with selected program as the outcome (HWL as reference) and comprehension variables as predictors. Having answered DPP on the comprehension questions regardless of whether that was the correct [OR (95% CI): 5.44 (3.54, 8.63)] or incorrect [OR (95% CI): 4.35 (2.25, 8.90)] answer was associated with choosing DPP as the preferred program.
Table 2:
Comprehension of program characteristics by participants (N=1,005)
| Question text | Variable name | Chose DPP, n=511 n(% of total participants) | Chose HWL, n=494 n(% of total participants) | p-value1 | OR (95% CI) of choosing DPP as the preferred program | |
|---|---|---|---|---|---|---|
| In which program do participants fill in daily food and physical activity logs? | Q34 | Participant’s answer: DPP (correct) | 481 (47.9) | 378 (37.6) | <0.001* | 5.44 (3.54, 8.63) |
| Participant’s answer: HWL (incorrect) | 30 (3.0) | 116 (11.5) | Ref | |||
| Which program focuses on reducing hunger and food cravings? | Q35 | Participant’s answer: DPP (incorrect) | 42 (4.2) | 14 (1.4) | <0.001* | 4.35 (2.25, 8.90) |
| Participant’s answer: HWL (correct) | 469 (46.7) | 480 (47.8) | Ref | |||
| Select all accurate statements** | Q36 | Selected all accurate statements (considered correct) | 266 (26.5) | 232 (23.1) | 0.168 | 0.87 (0.32, 2.36) |
| Selected one accurate statement about DPP | 81 (8.1) | 70 (7.0) | 0.73 (0.26, 2.05) | |||
| Selected one accurate statement about HWL | 155 (15.4) | 182 (18.1) | 0.72 (0.26, 1.96) | |||
| Selected the inaccurate statement only or in combination with an accurate statement | 9 (0.9) | 10 (1.0) | Ref |
Chi-square test of independence;
p<0.05
There were 3 statements: 2 accurate and 1 inaccurate.
Comparing Proportions of Participants Who Chose DPP or HWL
Participants were next asked to choose their preferred weight loss program from between DPP and HWL to test the main hypothesis, allowing participants to make their own assumptions about the context (e.g., the cost, who offers the program). A total of 511 (50.8%) participants chose DPP [(0.51) 95% CI= 0.48, 0.54] and 494 (49.2%) chose HWL [(0.49) 95% CI= 0.46, 0.52]. Thus, the probability of choosing either of the two programs was not significantly different from 0.5 (p=0.614). In addition, we tested the difference of proportions in the subset with a BMI ≤ 45 (n=847, mean BMI=36.33). The estimated probability of choosing either program was still not significantly different from 0.5 (p=0.68). Of 847 participants with BMI of 30–45, 50.8% chose DPP [(0.51) 95% CI= 0.47, 0.54] and 49.2% chose HWL [(0.49) 95% CI= 0.46, 0.53].
Investigating Program Preference More Specifically
Specifying the Context
Participants were then asked about their likeliness to enroll in DPP or HWL given the context that programs would be offered at no cost by (a) a health care provider or (b) their employer. Twenty-seven participants (2.7%) reported they would not have a preference. Reporting being more likely to enroll in DPP or HWL given a specified context was related to the primary selected program [p <0.001 (Pearson Chi-square tests of independence)] (Table 3).
Table 3:
Investigating preference of program more specifically
| DPP, n=511 | HWL, n=494 | p-value† | ||
|---|---|---|---|---|
| n (%¥) | n (%¥) | |||
| The program they would most likely enroll in if both programs were offered at no cost by health care provider or worksite * | Much more likely DPP | 302 (30.0) | 12 (1.2) | <0.001 |
| Somewhat more likely DPP | 159 (15.8) | 27 (2.7) | ||
| Much more likely HWL | 13 (1.3) | 317 (31.5) | ||
| Somewhat more likely HWL | 22 (2.2) | 126 (12.5) | ||
| No preference | 15 (1.5) | 12 (1.2) | ||
| Think they would be more adherent to | DPP | 445 (44.3) | 49 (4.9) | <0.001 |
| HWL | 66 (6.6) | 445 (44.3) | ||
| Think they would lose greater weight with | DPP | 442 (44.0) | 97 (9.7) | <0.001 |
| HWL | 69 (6.9) | 397 (39.5) | ||
| Think they are more likely to drop out of | DPP | 90 (9.0) | 451 (44.9) | <0.001 |
| HWL | 421 (41.9) | 43 (4.3) | ||
| Effect of having both programs offered at the same time on decision to enroll in one of the two | Very likely that it would affect my decision | 48 (4.8) | 75 (7.5) | 0.052 |
| Likely that it would affect my decision | 199 (19.8) | 188 (18.7) | ||
| I cannot say | 93 (9.3) | 92 (9.2) | ||
| Somewhat unlikely that it would affect my decision | 85 (8.5) | 66 (6.6) | ||
| Very unlikely that it would affect my decision | 86 (8.6) | 73 (7.3) | ||
| Ever experienced praise/positive comments about weight loss efforts | Yes | 436 (43.4) | 414 (41.2) | 0.563 |
| No | 75 (7.5) | 80 (8.0) | ||
| Ever experienced stigmatizing/shaming comments about weight loss efforts | Yes | 308 (30.6) | 296 (29.5) | 0.960 |
| No | 203 (20.2) | 198 (19.7) |
Pearson Chi-square tests of independence.
Percent of total (n=1005) unless specified otherwise.
Adherence, Dropping Out, and Expected Success
Participants’ expectations about their adherence, weight loss magnitude, and likelihood of dropping out were associated with participating in their preferred program (p<0.001). That is, greater proportions (87.1% and 90.1% of those preferring DPP and HWL, respectively) thought they would be more adherent to the program of their choice (p<0.001), greater proportions (86.5% and 80.4% of those preferring DPP and HWL, respectively) expected to have greater weight loss with their program of choice (p<0.001), and smaller proportions (17.6% and 8.7% of those preferring DPP and HWL, respectively) thought they were more likely to drop out of the program they chose (p<0.001) (Table 3).
Only Choice Being the Nonpreferred Program
Those who chose DPP as their preferred program were asked how likely they would be to enroll in HWL if offered at no cost through their employer and health care provider, and vice versa for those who chose HWL. For these questions, we were interested in investigating the importance of settings and likeliness of enrolling if the participant did not like the program characteristics. Within the context that their nonpreferred program was the only choice, 48.1% to 52.0% of participants in each group reported being likely or very likely to enroll, and the proportion of “undecided” participants ranged from 26.9% to 29.1% within each group. There was no significant difference between those who preferred DPP or HWL in terms of their likeliness to enroll in the other program (Table 4).
Table 4:
Reported likeliness to enroll when the only choice is the nonpreferred program
| DPP, n=511 | HWL, n=494 | p-value† | ||
|---|---|---|---|---|
| n (%¥) | n (%¥) | |||
| How likely are you to enroll in [your nonpreferred program] if offered at no cost through your health care provider? | Very likely | 39 (7.6) | 47 (9.5) | 0.340 |
| Likely | 220 (43.0) | 210 (42.5) | 0.912 | |
| Undecided | 145 (28.4) | 133 (26.9) | 0.657 | |
| Unlikely | 79 (15.5) | 72 (14.6) | 0.761 | |
| Very unlikely | 28 (5.5) | 32 (6.5) | 0.593 | |
| How likely are you to enroll in [your nonpreferred program] if offered at no cost through your employer? | Very likely | 66 (12.9) | 70 (14.2) | 0.625 |
| Likely | 180 (35.2) | 181 (36.6) | 0.688 | |
| Undecided | 149 (29.2) | 137 (27.7) | 0.667 | |
| Unlikely | 74 (14.5) | 66 (13.4) | 0.673 | |
| Very unlikely | 42 (8.2) | 40 (8.1) | 1.000 |
Two-proportions z-test.
Percent of each group (n=511 for DPP and n=494 for HWL), Column sums up to 100 for each of the two questions.
Positive and Negative Experiences About Weight Loss Efforts
A total of 60.1% (30.6% DPP and 29.5% HWL) of participants reported having experienced shaming or stigmatizing comments about their weight loss efforts, and 84.6% (43.4% DPP and 41.2% HWL) reported experiencing praise or positive comments for their weight loss or weight loss efforts. There were no significant relationships between choosing either of the programs and previous experiences with positive or negative comments (Table 3).
Preference of Delivery Methods
Participants were asked to rank five types of program delivery options from 1 (most attractive) to 5 (least attractive), thinking about the program they chose. Among the five options, ranking distributions of “in-person group class led by coach” (p=0.015) and “web-based without coach” (p<0.001) were statistically significantly different between the two groups. That is, proportions of those ranking “in-person group class led by coach” as their least favorite and “web-based without coach” as their most favorite were significantly larger among those who preferred HWL. Program delivery preference rankings are summarized in Table 5. We also examined interactions of rankings with sociodemographic characteristics as predictors of choosing DPP or HWL and found no significant associations.
Table 5:
Rankings of the attractiveness of program delivery methods by respondents grouped by program of choice
| Program of choice | Ranked 1 n (%)¥ | Ranked 2 n (%)¥ | Ranked 3 n (%)¥ | Ranked 4 n (%)¥ | Ranked 5 n (%)¥ | p-value† | |
|---|---|---|---|---|---|---|---|
| Group class led by coach in person | DPP, n=511 | 74 (14.5) | 82 (16.0) | 102 (20.0) | 128 (25.0) | 125 (24.5) | 0.015 |
| HWL, n=494 | 59 (11.9) | 84 (17.0) | 74 (15.0) | 113 (22.9) | 164 (33.2) | ||
| Group class led by coach via videoconference | DPP, n=511 | 70 (13.7) | 80 (15.7) | 121 (23.7) | 176 (34.4) | 64 (12.5) | 0.532 |
| HWL, n=494 | 39 (7.9) | 99 (20.0) | 127 (25.7) | 164 (33.2) | 65 (13.2) | ||
| Individual sessions with a coach in person | DPP, n=511 | 142 (27.8) | 115 (22.5) | 97 (19.0) | 92 (18.0) | 65 (12.7) | 0.205 |
| HWL, n=494 | 122 (24.7) | 110 (22.3) | 91 (18.4) | 106 (21.5) | 65 (13.2) | ||
| Individual sessions with a coach via videoconference | DPP, n=511 | 101 (19.8) | 183 (35.8) | 110 (21.5) | 72 (14.1) | 45 (8.8) | 0.807 |
| HWL, n=494 | 101 (20.4) | 157 (31.8) | 123 (24.9) | 84 (17.0) | 29 (5.9) | ||
| Web-based without coach | DPP, n=511 | 124 (24.3) | 51 (10.0) | 81 (15.9) | 43 (8.4) | 212 (41.5) | <0.001 |
| HWL, n=494 | 173 (35.0) | 44 (8.9) | 79 (16.0) | 27 (5.5) | 171 (34.6) |
Wilcoxon rank sum test.
Percent of total 1,005 participants.
Factors Associated With Choice of Weight Loss Program
Race, educational attainment, household income, (not) having tried losing weight before, and (not) reporting high serum cholesterol levels had significant associations with the choice of weight loss program (Table 6): Blacks, Asians, Native Hawaiians, and other races (all grouped together) were less likely than White participants to prefer DPP to HWL [OR (95% CI): 0.68 (0.48–0.98), p=0.040]. Those reporting an average monthly household income of greater than $4,999 were less likely than those with an income of less than $2,000 to choose DPP [OR (95% CI): 0.50 (0.32–0.78), p=0.002]. However, participants with postgraduate education attainment (master’s and doctorate degrees) were more likely to prefer DPP than were those with a high school diploma or less education [OR (95% CI): 1.83 (1.18–2.84), p=0.007]. Those who did not report a high serum cholesterol level or using cholesterol-lowering medications were more likely than those who reported that condition to choose DPP [OR (95% CI): 1.40 (1.04–1.89), p=0.028]. Participants who reported not having tried losing weight before were more likely to choose DPP [OR (95% CI): 2.47 (1.15–5.68), p=0.025]. Other variables had no association with choice of weight loss program. We did not find any significant interaction effects for the associations between predictive factors and choice of weight loss program.
Table 6:
Factors associated with choice of weight loss program
| Variables | Levels | Odds Ratios (OR) of choosing DPP rather than HWL (HWL as the reference), n=1,005 |
p-value‡ | ||
|---|---|---|---|---|---|
| OR§ | 95% CI | p-value | |||
| BMI | 1.01 | 1.00–1.03 | 0.121 | ||
| Age | <25 | Ref | 0.910 | ||
| 25–34 | 1.00 | 0.42–2.37 | 0.994 | ||
| 35–44 | 1.03 | 0.43–2.45 | 0.949 | ||
| 45–54 | 1.06 | 0.44–2.57 | 0.893 | ||
| 55≤ | 0.87 | 0.36–2.15 | 0.767 | ||
| Gender Identity | Female | Ref | 0.760 | ||
| Male | 0.96 | 0.72–1.29 | 0.789 | ||
| Other1 | 1.49 | 0.46–5.27 | 0.509 | ||
| Race | White | Ref | 0.040* | ||
| Black and other2 | 0.68 | 0.48–0.98 | 0.040* | ||
| Ethnicity | Non-Hispanic/Latino | Ref | 0.078 | ||
| Hispanic/Latino | 1.54 | 0.95–2.51 | 0.078 | ||
| Education | High school or less3 | Ref | 0.047* | ||
| Associate degree | 1.34 | 0.90–1.99 | 0.146 | ||
| Bachelor’s degree | 1.20 | 0.83–1.73 | 0.343 | ||
| Graduate level4 | 1.83 | 1.18–2.84 | 0.007*† | ||
| Employment Status | Not working5 | Ref | 0.870 | ||
| Work full-time | 1.01 | 0.69–1.47 | 0.971 | ||
| Work part-time | 0.95 | 0.54–1.67 | 0.856 | ||
| Self-employed | 0.85 | 0.54–1.36 | 0.508 | ||
| Full-time student | 0.67 | 0.25–1.77 | 0.423 | ||
| Average monthly household income | $1,000-$1,9996 | Ref | 0.035* | ||
| $2,000-$2,999 | 0.63 | 0.41–0.96 | 0.031* | ||
| $3,000-$3,999 | 0.75 | 0.48–1.18 | 0.221 | ||
| $4,000-$4,999 | 0.69 | 0.43–1.09 | 0.111 | ||
| $5,000 and above | 0.50 | 0.32–0.78 | 0.002*† | ||
| Likeliness to participate in a cost-free weight loss program offered by health care provider, employer, etc. in person or by videoconference | Very likely | Ref | 0.160 | ||
| Somehow likely | 0.97 | 0.66–1.44 | 0.892 | ||
| Decision depends on program features | 0.75 | 0.54–1.05 | 0.099 | ||
| Unlikely to enroll | 1.81 | 0.77–4.48 | 0.181 | ||
| Have tried losing weight before | Yes | Ref | 0.025* | ||
| No | 2.47 | 1.15–5.68 | 0.025* | ||
| Weight change over the past year | Gained weight | Ref | 1.000 | ||
| Lost weight | 1.00 | 0.74–1.35 | 0.995 | ||
| Constant weight | 0.98 | 0.60–1.62 | 0.954 | ||
| Diabetes | Yes | Ref | 0.340 | ||
| No | 1.15 | 0.86–1.53 | 0.340 | ||
| Hypertension or using medications to lower blood pressure | Yes | Ref | 0.440 | ||
| No | 1.16 | 0.79–1.71 | 0.440 | ||
| High cholesterol or using medications to reduce cholesterol | Yes | Ref | 0.028* | ||
| No | 1.40 | 1.04–1.89 | 0.028* | ||
| History of heart disease or stroke | Yes | Ref | 0.968 | ||
| No | 1.01 | 0.73–1.38 | 0.968 | ||
| Arthritis with limitations for walking or activities of daily living such as personal care | Yes | Ref | 0.319 | ||
| No | 1.19 | 0.85–1.68 | 0.319 | ||
| Any cancer requiring treatment within past 5 years | Yes | Ref | 0.183 | ||
| No | 0.70 | 0.42–1.18 | 0.183 | ||
| Influence of program’s cost on decision on whether to participate? | Would not do the program unless offered cost free7 | Ref | 0.570 | ||
| May do the program even if not cost-free8 | 1.08 | 0.73–1.59 | 0.703 | ||
| Non-sense response9 | 0.64 | 0.21–1.85 | 0.413 | ||
Model includes all reported covariates in the table.
Overall effect of covariates with more than two levels by Wald test.
P-values reported are unadjusted, where ‘*’ indicates unadjusted p<0.05, and ‘†’ indicates Bonferroni adjusted p<0.05 (i.e., p-value multiplied by the number of comparisons for the variable).
Transgender (n=8) and other (n=5) merged.
Other: Asian (n=20), Native Hawaiian (n=4), and other (n=41).
Less than high school (n=6) and high school/GED (n=264) merged.
Doctorate degree (n=11) and master’s degree (n=256) merged.
‘Do not work’ (n=121) and retired (n=98) merged.
Less than $1,000 (n=0).
These two were merged: “Would not do the program unless offered cost free” (n=63), selected both “Would not do the program…” and “Most interested if the program is offered cost free”(n=77).
These three were merged: “Most interested if the program is offered cost free” (n=425), “Would still enroll if there is a co-payment “ (n=179), respondent selected both “most interested…” and “would still enroll…” (n=244).
Non-sense combinations: e.g., selected all three options or selected co-payment AND cost-free only).
We note that all results are presented (and interpreted) based on unadjusted p-values. While there is no commonly agreed upon method for adjustment in multiple regression models [13], we performed a Bonferroni correction for statistically significant unadjusted p-values (p<0.05). Bonferroni adjustment is used for multiple comparisons of each demographic category vs the reference level where applicable (e.g. for education and income) in the logistic regression. Significance is then determined against a 0.05 significance level threshold. To adjust for the total number of predictor variables tested in the model, one could adjust for 18 significance tests. While the Bonferroni method (multiplying each p-value by 18) may be overly conservative the Benjamini-Hochberg procedure [14] can be used to control the False Discovery Rate.
Discussion and Conclusion
Behavioral weight loss interventions are the first-line treatment for obesity, but results of scaled DPP interventions have observed weight loss of 2%−4%, which is below the 5% threshold recognized by some as a threshold for clinical benefits [1, 2]. In this study, we provided participants a hypothetical choice between DPP and HWL, intending to inform the development of a two-stage randomized trial to compare these two programs. We found that the probability of choosing either program did not differ significantly from 50%, supporting the feasibility of testing the interactions of treatment self-selection, preference, and treatment assignment in a randomized clinical trial. Furthermore, the participants anticipated that they would lose more weight and be less likely to drop out if they enrolled in their preferred program, indicating a potential public health benefit of providing choice in public health initiatives. Race, educational attainment, household income, previous attempt to lose weight, and reporting high serum cholesterol levels were predictors of the choice between these programs. Only 2.4% of participants had “no preference” if both programs were offered at the same time. Additionally, the proportion of those who were unlikely or very unlikely to enroll in the nonpreferred program was not significantly different between those who chose DPP and those who chose HWL, which supports providing treatment options to promote enrollment and suggests that the two groups were equally strict about their preferred program.
Importance of Providing Treatment Options for Enrollment
In this study, most participants preferred either HWL or DPP, and only a small proportion (2.4%) reported having no preference. Also, more than 50% of all participants reported that being offered two options would likely affect their decision to enroll in one. Those who chose HWL were marginally more likely to report that being offered two options would likely affect their decision to enroll in one of the two. These results support that the two programs appeal differently to individuals, and someone preferring one may not prefer the other. Thus, regardless of the effect of preference on weight loss outcomes, providing treatment options could improve enrollment rates. In general, organisms have a preference for freedom of choice among alternatives even if they do not have preferences among the alternatives [15]. We studied only two choices. Situations with more than two choices might produce different results [16].
Our Motivating Circumstance for This Study
We note that receiving one’s preferred treatment and having the chance to self-select one’s preferred treatment are not the same event. The effect of receiving a (preferred) treatment one has self-selected to receive on weight loss may differ from the effect of receiving the same treatment (still preferred) if one has not self-selected to receive it. Our motivating circumstance for the current study is that preference, allowing self-selection, and being assigned to treatment A or treatment B create a 2×2×2 contingency table. From the eight hypothetical groups, six groups can be observed:
Having chance of self-selection, receiving treatment A/B, receiving preferred treatment;
Not having chance of self-selection, receiving treatment A/B, receiving preferred treatment;
Not having chance of self-selection, receiving treatment A/B, receiving nonpreferred treatment.
Two other cells from the contingency table where one has the chance to self-select, receives treatment A/B, and receives their nonpreferred treatment cannot functionally be observed. Previous studies that incorporated self-selection and preference elements have not specifically studied these interactions.
Why it Is Important to Know Preference Proportions
Testing the effects of the interaction terms discussed above on weight loss outcomes requires a two-stage randomization procedure. That is, participants should first be asked about their preference for A or B, then be randomly assigned on the basis of allowing self-selection, and finally be randomly assigned to treatment A or B within the no-self-selection arm. As stated before, this two-stage randomization comes with a risk for unbalanced numbers of those who prefer A vs. B or vice versa. As an example, Burke et al. [17] conducted a two-stage randomized study to assess the impact of preference on weight loss outcomes. In the first stage, they randomized participants to being assigned to their preferred treatment or being randomly assigned (second randomization stage) to one of the two treatments. That stage used a 3:2 randomization ratio because of expected unbalanced preference for the treatments. Twenty-four percent of participants who were randomly assigned to the preference arm were finally excluded to overcome the unbalanced number of participants who preferred a standard diet over a vegetarian diet. Moreover, it has been demonstrated that the optimal proportion of participants to be allowed treatment self-selection in a two-stage randomized setting to allow sufficient power to detect all the effects of interest (e.g., treatment and self-selection effects) depends on the proportions who prefer each of the treatments and the proportion of undecided (i.e., no preference) participants [18, 19].
Evidence on the Effect of Being Assigned to the Preferred Treatment on Weight Loss Outcomes
Weight loss studies that incorporate participants’ preference to test the effect of preference on weight loss outcomes do not provide strong evidence that receiving a preferred treatment leads to or is associated with better outcomes compared with receiving a randomly assigned treatment or the nonpreferred treatment [20–25]. For example, Renjilian et al. [21] randomly assigned adult participants with obesity to the weight loss treatments for which they expressed preference within a 2×2 factorial design (individual/group treatment × preferred/nonpreferred). They found no significant effects for treatment preference on weight loss outcome. Borradaile et al. [22] assessed preference for treatments (low-carbohydrate or low-fat diet) before and independent of randomization. They found that those who were assigned to their preferred treatment lost less weight than those who were not assigned to their preference. Similarly, Burke et al. [17] found that participants who were assigned to a weight loss intervention lost more weight than those who received their preferred intervention. None of the studies discussed above found an interaction between receiving one’s preferred treatment and treatment assignment on weight loss outcome.
Incorporation of Preference in Trial Design
The standard randomization process ensures that the differences between treatment arms for all known and unknown factors are due to chance [26]. Randomization along with intention-to-treat analysis, under the existing circumstances of the study conduct and having participants blinded to their assignment, yield an unbiased estimate of the effect of treatment “assignment” [27]. On the other hand, clinicians do not assign treatments at random, and elements of preference for one treatment over another are involved in those decisions in real-world settings. Moreover, in a randomized trial, given the countless personal preferences of individuals, some will be assigned to their preferred treatment and some to their nonpreferred treatment, potentially leading to factors that affect response to the treatment [28]. For instance, in a weight loss intervention, participants who do not perceive their assigned treatment as preferred may be less adherent, which complicates interpretations of the treatment effect. Incorporating participants’ preference in the randomization process is a suggested approach to distinguish between the effects of motivational factors [10]. Other methodological choices are excluding participants with strong preference for a treatment or participants with mild or no preference for one intervention over the other (in cases where participants’ preference is incorporated in the study design). Both can undermine the external validity (i.e., generalizability) of the study [17, 22].
Predictors of Choosing DPP and HWL
We found some differences in the demographics of those who preferred DPP and HWL. Black, Asian, Hawaiian, and other races (all merged compared with White participants), and those with monthly income of greater than $4,999 (compared with an average monthly income of less than $2,000) were less likely to choose DPP over HWL. On the other hand, participants with postgraduate education attainment, those who did not report high serum cholesterol levels, and those reporting not having tried losing weight before were more likely to choose DPP. These results could be informative in designing a randomized clinical trial to assess the interactions discussed above. Generally, it has been suggested that food preferences have a role in predicting the choice of weight loss treatments by most individuals, so that they are more likely to select a weight loss intervention in which dietary components are most closely in line with their food preferences [29]. Because we asked about weight loss treatment programs that included some diet modification approach and not about specific foods, it is not clear whether our results are neutral to food preferences or whether the participants made their own assumptions about the foods involved in each program. We did not observe any gender-based differences in participants’ preference for DPP or HWL. Similarly, McVay et al. [29] did not report any difference between men and women in their preference for a low-fat/low-calorie diet or a low-carbohydrate diet. Other studies have reported gender-based differences in preference for weight loss interventions, most of which attributed the differences to specific foods [23, 30].
Association of Choice of Weight Loss Program and Expectations of Adherence and Outcomes
As McVay et al. [29] suggest, a participant’s selection of a weight loss intervention is a decision that involves multiple components and expectations. Thus, the choice might be influenced by how participants envision their weight loss outcomes with each of the options. Our results support that the weight loss treatment one would choose is related to expectations of adherence, retention, and goal achievement. That is, the program in which they chose to enroll was congruent with the program they thought they would be more likely to adhere to, the program in which they expected to lose more weight, and the program they thought they would be less likely to drop out of. Regarding the association of receiving one’s preferred program with actual withdrawal rate and treatment adherence, results from previous studies are mixed. Some randomized studies that assessed treatment preference prior to randomization [22] or that randomly assigned participants to choice/no-choice arms [23] have reported no association between receiving one’s preferred treatment and retention rates. Similarly, in a two-stage randomized study [20], there was no significant difference between dietary adherence in the choice arm compared with the randomly assigned arm, allowing the inference that permitting choice among dietary treatment options did not affect dietary adherence. Other studies suggest that giving participants the choice to select their intervention can increase adherence [31, 32]. In a review of the determinants of patient adherence to medications, a finding tangentially pertinent to our study suggests that among numerous other individual and environmental factors, people’s beliefs in favor of health recommendations are related to their adherence to prescribed medication [33]. Overall, participants’ anticipation of their adherence, likeliness of dropout, and weight loss outcomes could play a role in choice, but it is unclear how being allowed to choose a treatment and enrollment in the preferred treatment affect adherence and retention rate.
Strengths and Limitations
This survey sets a background for conducting a rigorous randomized clinical trial to compare HWL and DPP, considering participants’ preference and chance of self-selection. Collecting data on the program characteristics or other factors (e.g., previous unsuccessful weight loss attempts) that prompted the participants’ choice could have been informative to characterize selection patterns, but we did not collect those data. Most of our participants identified themselves as non-Hispanic White women. Hence, our results might not be generalizable to other ethnicity, race, and gender groups.
Conclusion
Estimated proportions of participants choosing HWL and DPP did not differ statistically significantly from 50%. These results suggest the risk of unequal enrollment in the two interventions in a two-stage randomized study is minimal and provide evidence for feasibility of testing the interactions of self-selection of weight loss treatment, preference, and treatment type in a randomized clinical trial.
Supplementary Material
What is already known about this subject?
Healthy Weight for Living (HWL) has shown weight loss of 8.0 kg and 8.5% in two RCTs. HWL has not been evaluated against a traditional program like Diabetes Prevention Program (DPP).
DPP and HWL may appeal to different types of individuals. Program self-selection in RCTs helps giving each program its best chance at supporting meaningful weight loss in a clinical setting.
Self-selection comes with a risk of unbalanced enrollment into each intervention, which could result in an underpowered study.
What this study adds?
We assessed the preference for two behavioral weight loss programs, DPP and HWL, in adults with obesity through a cross-sectional survey. The enrollment into DPP and HWL was balanced. The majority preferred one of the two programs as opposed to having no preference.
Race, educational attainment, household income, previous attempt to lose weight, and serum cholesterol levels had significant associations with the choice of weight loss program.
Our results inform the design of a two-stage randomized trial to examine the interacting effect of three qualities on weight loss outcomes of DPP and HWL: (1) preference for weight loss intervention (preferred, nonpreferred), (2) self-selection of the intervention (self-selected, randomly assigned), and (3) type of intervention received (DPP, HWL).
Acknowledgements:
We thank Jennifer Holmes from Medical Editing Services for providing language editing. Data described herein, code book, and analytic code are publicly available at [doi]. Authors contributions: Survey design: All authors; Data collection: YJ-N; Statistical methods: AO, SD, YJ-N; Data analysis: YJ-N; Analysis verification: XC; Writing-first draft: YJ-N; Funding acquisition: DBA. All authors were involved in writing the paper and had final approval of the submitted and published versions.
Fundings:
YJ-N and DBA partly supported by NIH grants R25DK099080, R25HL124208, and the Gordon and Betty Moore Foundation. SBR funding from USDA agreement #8050-51000-105-01S; USDA/ARS project number 8050-51000-105-00D. The opinions expressed are those of the authors and do not necessarily represent those of the NIH, USDA, or any other organization.
Conflict of Interest:
In the last thirty-six months, Dr. Allison has received personal payments or promises for same from: Alkermes, Inc.; Amin Talati Wasserman for KSF Acquisition Corp (Glanbia); Big Sky Health, Inc.; Biofortis Innovation Services (Merieux NutriSciences); California Walnut Commission; Clark Hill PLC; Kaleido Biosciences; Law Offices of Ronald Marron; Medpace/Gelesis; Novo Nordisk Fonden; and Sports Research Corp. Donations to a foundation have been made on his behalf by the Northarvest Bean Growers Association. Dr. Roberts is the founder and owner of Instinct Health Science (www.theidiet.com): principles of weight management at Instinct Health Science are the same as one of the programs under discussion in this manuscript (Healthy Weight for Living). The institution of DBA, YJ-N, SD, and XC, Indiana University, and the Indiana University Foundation have received funds or donations to support his research or educational activities from: Alliance for Potato Research and Education; Almond Board; American Egg Board; Arnold Ventures; Boston Children’s Hospital; California Walnut Commission; Eli Lilly and Company; Haas Avocado Board; Mars, Inc.; National Cattlemen’s Beef Association; Reckitt Benckiser Group PLC; Soleno Therapeutics; WW (formerly Weight Watchers); and numerous other for-profit and non-profit organizations to support the work of the School of Public Health and the university more broadly. Other authors reported no disclosures.
References
- 1.Kramer MK, Kriska AM, Venditti EM, et al. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. Am J Prev Med 2009;37:505–11. [DOI] [PubMed] [Google Scholar]
- 2.Dunkley AJ, Bodicoat DH, Greaves CJ, et al. Diabetes prevention in the real world: effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes and of the impact of adherence to guideline recommendations: a systematic review and meta-analysis. Diabetes Care 2014;37:922–33. [DOI] [PubMed] [Google Scholar]
- 3.Dalle Grave R, Calugi S, Molinari E, et al. Weight Loss Expectations in Obese Patients and Treatment Attrition: An Observational Multicenter Study. Obesity Research 2005;13:1961–9. [DOI] [PubMed] [Google Scholar]
- 4.Anton S, Das SK, McLaren C, Roberts SB. Application of social cognitive theory in weight management: Time for a biological component? Obesity 2021;29:1982–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall KD, Kahan S. Maintenance of Lost Weight and Long-Term Management of Obesity. Medical Clinics of North America 2018;102:183–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Höchsmann C, Fearnbach N, Dorling JL, et al. Preference, Expected Burden, and Willingness to Use Digital and Traditional Methods to Assess Food and Alcohol Intake. Nutrients 2021;13. [DOI] [PMC free article] [PubMed]
- 7.Deckersbach T, Das SK, Urban LE, et al. Pilot randomized trial demonstrating reversal of obesity-related abnormalities in reward system responsivity to food cues with a behavioral intervention. Nutrition & Diabetes 2014;4:e129-e. [DOI] [PMC free article] [PubMed]
- 8.Das SK, Bukhari AS, Taetzsch AG, et al. Randomized trial of a novel lifestyle intervention compared with the Diabetes Prevention Program for weight loss in adult dependents of military service members. The American Journal of Clinical Nutrition 2021;114:1546–59. [DOI] [PubMed] [Google Scholar]
- 9.Salinardi TC, Batra P, Roberts SB, et al. Lifestyle intervention reduces body weight and improves cardiometabolic risk factors in worksites. The American Journal of Clinical Nutrition 2013;97:667–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brewin CR, Bradley C. Patient Preferences And Randomised Clinical Trials. BMJ: British Medical Journal 1989;299:313–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heo M, Meissner P, Litwin AH, et al. Preference option randomized design (PORD) for comparative effectiveness research: Statistical power for testing comparative effect, preference effect, selection effect, intent-to-treat effect, and overall effect. Statistical Methods in Medical Research 2017;28:626–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agley J, Xiao Y, Nolan R, Golzarri-Arroyo L. Quality control questions on Amazon’s Mechanical Turk (MTurk): A randomized trial of impact on the USAUDIT, PHQ-9, and GAD-7. Behavior Research Methods 2022;54:885–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Streiner DL. Best (but oft-forgotten) practices: the multiple problems of multiplicity—whether and how to correct for many statistical tests. The American Journal of Clinical Nutrition 2015;102:721–8. [DOI] [PubMed] [Google Scholar]
- 14.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society: Series B (Methodological) 1995;57:289–300. [Google Scholar]
- 15.Catania AC. Freedom of Choice: A Behavioral Analysis. In: Bower GH, editor. Psychology of Learning and Motivation. 14: Academic Press; 1980. p. 97–145. [Google Scholar]
- 16.Wood SL, Shinogle JA, McInnes MM. New choices, new information: do choice abundance and information complexity hurt aging consumers’ medical decision making? The Aging Consumer: Routledge; 2011. p. 153–70.
- 17.Burke LE, Warziski M, Styn MA, Music E, Hudson AG, Sereika SM. A randomized clinical trial of a standard versus vegetarian diet for weight loss: the impact of treatment preference. International Journal of Obesity 2008;32:166–76. [DOI] [PubMed] [Google Scholar]
- 18.Walter SD, Turner RM, Macaskill P. Optimising the two-stage randomised trial design when some participants are indifferent in their treatment preferences. Stat Med 2019;38:2317–31. [DOI] [PubMed] [Google Scholar]
- 19.Turner RM, Walter SD, Macaskill P, McCaffery KJ, Irwig L. Sample Size and Power When Designing a Randomized Trial for the Estimation of Treatment, Selection, and Preference Effects. Medical Decision Making 2014;34:711–9. [DOI] [PubMed] [Google Scholar]
- 20.Yancy WS, Mayer SB, Coffman CJ, et al. Effect of Allowing Choice of Diet on Weight Loss. Annals of Internal Medicine 2015;162:805–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Renjilian DA, Perri MG, Nezu AM, McKelvey WF, Shermer RL, Anton SD. Individual versus group therapy for obesity: Effects of matching participants to their treatment preferences. Journal of Consulting and Clinical Psychology 2001;69:717–21. [PubMed] [Google Scholar]
- 22.Borradaile KE, Halpern SD, Wyatt HR, et al. Relationship Between Treatment Preference and Weight Loss in the Context of a Randomized Controlled Trial. Obesity 2012;20:1218–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coles LT, Fletcher EA, Galbraith CE, Clifton PM. Patient freedom to choose a weight loss diet in the treatment of overweight and obesity: a randomized dietary intervention in type 2 diabetes and pre-diabetes. International Journal of Behavioral Nutrition and Physical Activity 2014;11:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jolly K, Lewis A, Beach J, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: Lighten Up randomised controlled trial. BMJ 2011;343:d6500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leavy JM, Clifton PM, Keogh JB. The Role of Choice in Weight Loss Strategies: A Systematic Review and Meta-Analysis. Nutrients 2018;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vorland CJ, Brown AW, Dawson JA, et al. Errors in the implementation, analysis, and reporting of randomization within obesity and nutrition research: a guide to their avoidance. Int J Obes (Lond) 2021;45:2335–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gadde KM, Allison DB. Long-acting amylin analogue for weight reduction. The Lancet 2021;398:2132–4. [DOI] [PubMed] [Google Scholar]
- 28.Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference: Houghton, Mifflin and Company; 2002. [Google Scholar]
- 29.McVay MA, Voils CI, Coffman CJ, et al. Factors associated with choice of a low-fat or low-carbohydrate diet during a behavioral weight loss intervention. Appetite 2014;83:117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wyant KW, Meiselman HL. Sex and race differences in food preferences of military personnel1. Journal of the American Dietetic Association 1984;84:169–75. [PubMed] [Google Scholar]
- 31.Corbett MS, Watson J, Eastwood A. Randomised trials comparing different healthcare settings: an exploratory review of the impact of pre-trial preferences on participation, and discussion of other methodological challenges. BMC Health Serv Res 2016;16:589-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sidani S, Fox M, Streiner DL, Miranda J, Fredericks S, Epstein DR. Examining the influence of treatment preferences on attrition, adherence and outcomes: a protocol for a two-stage partially randomized trial. BMC Nursing 2015;14:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kardas P, Lewek P, Matyjaszczyk M. Determinants of patient adherence: a review of systematic reviews. Front Pharmacol 2013;4:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.