Abstract
Background:
Participation and active engagement in meaningful activities supports the emotional and physical well-being of older adults. In 2020, the onset of the COVID-19 pandemic altered lives, including ability to participate in meaningful activities. This study compared meaningful activity engagement before and at the beginning of the COVID-19 pandemic in a nationally representative, diverse sample >65 years between 2015–2020.
Methods:
We described the proportions and characteristics of National Health and Aging Trends Study participants and their engagement in four activities: visiting friends or family, attending religious services, participating in clubs/classes/other organized activities, and going out for enjoyment. We used mixed effects logistic regressions to compare probabilities of activity engagement before 2020 and in 2020, adjusting for age, sex, functional status, income, geographic region, anxiety-depression, and transportation issues.
Results:
Of 6,815 participants in 2015, the mean age was 77.7 (7.6) years; 57% of participants were female; 22% were Black, 5% Hispanic, 2% American Indian, and 1% Asian; 20% had disability; and median income was $33,000. Participation in all four activities remained consistent between 2015–2019 and declined in 2020. Significant differences existed in attending religious services (p<0.01) and going out for enjoyment (p<0.001) by race and ethnicity, before and after the start of COVID-19. Black and Hispanic participants experienced the largest decline in attending religious services (−32%, −28%) while Asian and White participants experienced the largest decline in going out for enjoyment (−49%, −56%).
Conclusions:
Potential quality of life tradeoffs should be considered to a greater extent in future pandemic emergencies.
Keywords: Meaningful activities, racially and ethnically diverse older adults, COVID-19
Background
Participation in meaningful activities – personally chosen activities that engage the individual and provide a sense of enjoyment1 – is beneficial to the physical, emotional, and mental health of older adults.2,3 In aging adults, a combination of personal and external factors may limit or facilitate their ability to participate in meaningful activities.4,5 Personal, individual-level factors include functional limitations, cognitive impairment, psychological motivation,6 and income7 while other aspects include neighborhood-level factors (e.g. the built environment, transportation availability),8,9 social support systems,10 and policies that support adult day services programs and formal paid caregivers such as in-home support services.11
In 2020, the start of the COVID-19 pandemic profoundly altered all our lives. Containment measures such as shelter-in-place and physical distancing may have reduced mortality and morbidity, but at the same time limited the ability of older adults in particular to stay physically active,12,13 and increased social isolation and feelings of loneliness;14 all of which can further exacerbate psychological stress and increase risk for cognitive decline and depression.15 In addition, the pandemic exposed disparities in health and healthcare resulting from factors such as structural racism, with a higher number of COVID-19 cases, decreased access to testing, and greater rates of deaths from COVID-19 in Black and Hispanic Americans compared to White Americans;16–19 and intensified anti-Asian xenophobia violence.20–22 Numerous studies examined pandemic effects in nursing homes,23,24 but less work has observed the impact of the pandemic in diverse, community-dwelling older adults.
As COVID-19 restrictions ease, it is essential to identify and acknowledge the distinct needs and preferences of diverse older adults to adapt potential interventions. Homebound status and social isolation may differ by race,25 and older adults may experience difficulties navigating video- and Internet-based technologies.14 We therefore aimed to compare meaningful activity engagement between 2015–2020 in a nationally representative, diverse sample of older adults aged 65+ years and the effect of the COVID-19 pandemic on activity engagement.
Methods
Data and study population
This is a prospective cohort study of National Health and Aging Trends Study (NHATS) respondents who were surveyed annually from 2015–2020. NHATS is a Medicare-based nationally representative annual survey of US adults 65 years and older that seeks to understand change over time in older adults’ physical and cognitive capacity; physical, social, technological, and economic environment; and participation in valued activities.
The initial sample was first interviewed either in English or Spanish in 2011 and replenishment of the sample occurred in 2015. NHATS used a stratified sample design from the Medicare enrollment database, with oversamples of the oldest age groups (ages 85+) and of non-Hispanic Black (hereafter, Black) persons. The probabilities of selection were designed to yield the targeted sample sizes for sampling domains to support the key analytic goals of trends and trajectories defined by age group and race and ethnicity.26 Data collection procedures were described previously.27
This study’s sample included participants residing in the community in 2015 (Round 5). NHATS participants were categorized by self-reported racial and ethnic groupings: American Indian; Asian; Black; Hispanic; Other (including bi/multi-racial); non-Hispanic White (hereafter, White). We excluded participants living in nursing homes or residential care facilities (n=913, 11%) and those with missing data for race and ethnicity (n=255, 3%). The UCSF Institutional Review Board approved this study.
Measures
The primary outcomes were categorical variables denoting participation in four different activities within the last month (yes/no): (i) visiting friends or family not living with the participant; (ii) attending religious services; (iii) participating in clubs, classes, other organized activities; (iv) going out for enjoyment such as going to dinner, a movie, to gamble, hear music, or to see a play. These activities represent “elective but valued activities” that enhance quality of life and are an extension beyond the basics of self-care and activities performed in the home.28 Transportation problems were used as a covariate. In unadjusted analyses, we used raw data to determine the activity prevalence for each year and overall (averaged across all years 2015–2020).
The primary predictor was onset of the COVID-19 pandemic (pre-pandemic=2015–2019 vs. after start of pandemic=2020). To compare activity prevalence before and after the start of COVID-19, we used the predictive margins method29 to determine average predicted probability of each of the four activities in the entire cohort. Adjusted probabilities and differences in adjusted probabilities are often more easily interpreted than raw logistic regression coefficients and are thus a useful post-estimation technique to presenting the results from multivariable regression models.29 Covariates included age; sex; functional status; income; geographic region; anxiety and depression; and presence of transportation problems. Participant sex (male/female) and geographic region (Northwest/Midwest/South/West) were from the 2015 (Round 5 baseline) survey while the other variables were time-varying covariates, taken from each survey round: age (continuous), functional status (derived continuous variable of total number of activities of daily living (ADLs) for which they received help (yes/no), including eating, bathing, toileting, dressing, walking outside, moving around inside, and getting out of bed [range 0–7 ADLs]), income (quintiles), anxiety-depression (none to minimal [score 0–2]; mild [3–5]; moderate [6–8]; severe [9–12]), and presence of transportation problems (yes/no). For income, we used an imputed value for annual income when total annual income was unavailable.30 Anxiety and depression were assessed with the Patient Health Questionnaire 4-item (PHQ-4), a 4-item instrument that combines the PHQ-2 and the Generalized Anxiety Disorder 2-item (GAD-2) and asks whether the participant has over the last month, had little interest or pleasure in doing things; felt down, depressed, or hopeless; felt nervous, anxious, or on edge; or been unable to stop or control worrying.27 Scores were based on symptom frequency (1=not at all; 2=several days; 3=more than half of the days; 4=nearly every day) and totaled across the four items.31,32
Analysis
We summarized and compared baseline characteristics of participants using standard descriptive statistics. We used sampling weights provided by the NHATS to adjust for any potential bias related to nonresponses and to account for differential probabilities of selection.27
We used weighted, mixed effects logistic regression with random intercept for each subject to separately determine unadjusted and adjusted probabilities and 95% confidence intervals (CIs) for engagement in the four activities. We created a series of models for each activity that adjusted for the potential confounders of age and sex and selected factors that potentially mediate meaningful activity engagement.6–9 These models also included an interaction term of race and ethnicity and indicator of pre-COVID-19 vs. after start of COVID-19. The first models included age and sex; the second models included age, sex, and functional status; the third models included age, sex, and income; the fourth models included age, sex, and geographic region; the fifth models included age, sex, and anxiety-depression; and the sixth models included age, sex, and presence of transportation problems. The final models included all covariates from the previous models. All analyses were conducted using Stata statistical software version 16.1 (StataCorp), with two-tailed tests at p<0.05 used to define statistical significance.
Results
Of 6,815 participants, 127 participants (2%) were American Indian, 75 participants (1%) were Asian; 1,470 participants (22%) were Black; 359 participants (5%) were Hispanic; 65 participants (1%) were classified as Other; and 4,719 participants (69%) were White. Ninety-six percent of the interviews were conducted in English. The mean age for the whole sample was 77.7 (standard deviation 7.6) years, 3,906 (57%) were women, and 20% needed assistance with one or more ADLs. Demographic characteristics differed between the racial and ethnic groups, except for the characteristic of having daughters (Table 1). Characteristics that were significantly different between the racial and ethnic groups included education, income, geographic region, health status, speaking English very well or well, presence of cancer, multimorbidity, functional impairment, homebound status, presence of anxiety and depression, and living alone. By 2020, 3,715 participants (55%) remained in our study, 1,966 participants (29%) died, and 1,134 participants (16%) were lost to follow-up.
Table 1.
Baseline characteristics of NHATS participants in 2015, characterized by racial and ethnic groups
| Characteristic | Total n (%)a |
American Indian n (%)a |
Asian n (%)a |
Black, n (%)a |
Hispanic n (%)a |
Other n (%)a |
White, n (%)a |
|---|---|---|---|---|---|---|---|
| Total Sample | 6,815 (100) | 127 (2) | 75 (2) | 1,470 (8) | 359 (6) | 65 (1) | 4,719 (80) |
|
| |||||||
| Age, mean (SD) 65–69 70–74 75–79 80–84 85–89 90+ |
77.7 (7.6) 991 (30) 1,662 (28) 1,484 (19) 1,268 (12) 878 (7) 532 (4) |
75.4 (7.3) 35 (44) 27 (27) 21 (11) 26 (12) 17 (7) NR |
74.8 (6.6) 18 (36) 22 (34) 16 (16) 13 (10) NR NR |
77.6 (7.6) 218 (30) 357 (28) 334 (19) 263 (12) 185 (7) 113 (4) |
77.9 (7.7) 52 (29) 82 (27) 80 (20) 71 (13) 44 (7) 30 (4) |
75.4 (8.4) 22 (50) 15 (25) 11 (13) 6 (5) 5 (4) 6 (3) |
77.9 (7.6) 646 (29) 1,159 (28) 1,022 (19) 889 (12) 623 (8) 380 (4) |
| Female | 3,906 (55) | 70 (52) | 36 (50) | 915 (60) | 207 (57) | 29 (39) | 2,649 (55) |
| Education >high school graduate | 5,305 (83) | 60 (61) | 60 (86) | 921 (69) | 146 (44) | 31 (48) | 4,072 (89) |
| Income $0-$18,000 $18,001-$32,000 $32,001-$51,400 $51,401-$86,200 >$86,200 |
1,923 (22) 1,553 (21) 1,248 (20) 1,084 (19) 1,007 (19) |
57 (38) 30 (24) 22 (19) 13 (12) 5 (6) |
33 (40) 14 (20) 8 (11) 6 (10) 14 (19) |
703 (44) 356 (24) 198 (16) 124 (9) 89 (7) |
208 (53) 81 (24) 41 (12) 17 (7) 12 (5) |
33 (47) 15 (24) 9 (15) NR NR |
889 (16) 1,057 (20) 970 (21) 920 (21) 883 (22) |
| Geographic region Northeast Midwest South West |
1,148 (18) 1,640 (23) 2,805 (38) 1,222 (20) |
15 (8) 18 (13) 59 (47) 35 (33) |
13 (18) 5 (6) 19 (23) 38 (54) |
213 (15) 305 (20) 851 (58) 101 (7) |
48 (14) 18 (5) 193 (51) 100 (30) |
16 (27) 5 (7) 25 (33) 19 (32) |
843 (19) 1,289 (25) 1,658 (36) 929 (20) |
| Health status Excellent/Very Good Good/Fair Poor |
2,727 (46) 3,697 (49) 389 (5) |
40 (34) 74 (57) 13 (10) |
21 (28) 46 (63) 8 (8) |
338 (25) 1,012 (67) 118 (7) |
66 (21) 260 (70) 33 (9) |
17 (28) 44 (64) NR |
2,245 (51) 2,261 (45) 213 (4) |
| Dementia (probable) | 711 (7) | 13 (6) | 12 (11) | 228 (11) | 73 (15) | 11 (11) | 374 (5) |
| Speak English very well or well | 6,538 (95) | 113 (87) | 57 (79) | 1,456 (99) | 177 (49) | 44 (64) | 4,691 (99) |
| Cancer | 866 (23) | 27 (21) | 9 (9) | 121 (15) | 28 (15) | 13 (17) | 668 (26) |
| Stroke | 308 (7) | 20 (13) | NR | 86 (10) | 13 (7) | NR | 183 (7) |
| Multimorbidity 0 conditions 1–2 conditions 3+ conditions |
1,223 (21) 2,376 (35) 3,216 (44) |
19 (19) 30 (23) 78 (58) |
22 (35) 26 (32) 27 (33) |
242 (19) 473 (33) 755 (48) |
57 (17) 119 (34) 183 (49) |
14 (25) 26 (39) 25 (36) |
869 (21) 1,702 (35) 2,148 (44) |
| Fallen in last year | 1,416 (23) | 27 (25) | 11 (16) | 236 (17) | 68 (19) | 10 (15) | 1,064 (24) |
| Impaired activities of daily living b 0 1–2 3+ |
5,444 (85) 833 (10) 538 (6) |
97 (81) 16 (11) 14 (8) |
57 (80) 12 (15) 6 (5) |
1,093 (75) 215 (13) 162 (11) |
251 (75) 56 (13) 52 (11) |
48 (78) 9 (11) 8 (11) |
3,898 (86) 525 (9) 296 (5) |
| Homebound status Independent Leaves home with help or has difficulty Never/rarely leaves the house |
5,811 (90) 576 (6) 424 (4) |
101 (84) 14 (8) 12 (8) |
59 (84) 11 (12) 5 (4) |
1,179 (85) 153 (8) 138 (7) |
255 (76) 41 (9) 62 (16) |
51 (82) 9 (12) 5 (6) |
4,166 (91) 348 (5) 202 (3) |
| Anxiety and depression (PHQ-4) None to minimal (0–2) Mild (3–5) Moderate (6–8) Severe (9–12) |
4,858 (73) 1,403 (20) 395 (5) 159 (2) |
78 (63) 33 (23) 12 (9) NR |
54 (67) 14 (25) NR 6 (6) |
960 (67) 363 (23) 111 (8) 36 (2) |
222 (65) 72 (19) 38 (9) 27 (8) |
43 (66) 18 (27) 4 (6) NR |
3.501 (75) 903 (19) 229 (5) 86 (2) |
| Thinks people are willing to help in community c | 5,952 (91) | 101 (84) | 64 (91) | 1,233 (88) | 290 (84) | 49 (80) | 4,215 (92) |
| Had proxy respondent | 334 (3) | 5 (3) | 11 (11) | 108 (5) | 38 (7) | NR | 168 (3) |
| Number of children, mean (SD) | 2.9 (2.0) | 3.2 (2.2) | 2.6 (1.6) | 3.2 (2.4) | 3.8 (2.5) | 2.8 (2.2) | 2.8 (1.8) |
| Presence of daughters | 5,129 (73) | 97 (78) | 52 (70) | 1,101 (74) | 291 (79) | 51 (75) | 3,537 (73) |
| Lives alone | 2,144 (28) | 41 (25) | 13 (16) | 494 (33) | 74 (18) | 19 (31) | 1,503 (28) |
Data source: National Health and Aging Trends Study. NR Not reportable, as cell size is less than 5 individuals; PHQ-4 Patient Health Questionnaire 4-item; SD standard deviation
Based on weighted population estimates. b Impaired activities of daily living is defined as receiving help with bathing, dressing, eating, toileting, transferring, walking outside, and walking inside. c Adapted for NHATS as an informal social control mechanism by which residents can achieve public order and influence opportunities for interpersonal crime in a neighborhood.
Participation in each activity remained relatively stable each year from 2015 through 2019 but declined in 2020 (Table 2 and Figure 1). In the total sample, visiting friends or family was the dominant activity through the whole study time (overall average 81%) while participating in clubs/classes/organized activities was the activity with the lowest level of participation (34%) (Table 2). While going out for enjoyment and attending religious services was the second and third most popular activity, respectively between 2015–2019; the order of these activities by prevalence switched in 2020.
Table 2.
Activity prevalence for total sample, ordered from highest to lowest prevalence of participation by year and overall (2015–2020)
| Overall (average 2015–2020) | Pre-COVID, by year | After COVID start, by year | ||||||
|---|---|---|---|---|---|---|---|---|
| 2015 n=6,815 |
2016 n=5,829 |
2017 n=5,135 |
2018 n=4,594 |
2019 n=4,165 |
2020 n=3,722 |
|||
| Highest participation | Visited friends or family 81% | Visited friends or family 86% | Visited friends or family 85% | Visited friends or family 85% | Visited friends or family 85% | Visited friends or family 84% | Visited friends or family 63% | |
| Go out for enjoyment 69% | Go out for enjoyment 76% | Go out for enjoyment 76% | Go out for enjoyment 76% | Go out for enjoyment 75% | Go out for enjoyment 76% | Attend religious services 35% | ||
| Attend religious services 53% | Attend religious services 58% | Attend religious services 59% | Attend religious services 58% | Attend religious services 57% | Attend religious services 57% | Go out for enjoyment 30% | ||
| Lowest participation | Participate clubs/classes/ organized activities 34% | Participate clubs/classes/ organized activities 35% | Participate clubs/classes/ organized activities 37% | Participate clubs/classes/ organized activities 38% | Participate clubs/classes/ organized activities 38% | Participate clubs/classes/ organized activities 38% | Participate clubs/classes/ organized activities 16% | |
Data source: National Health and Aging Trends Study. We used raw data with survey weights to determine activity prevalence for each year and overall average.
Figure 1.
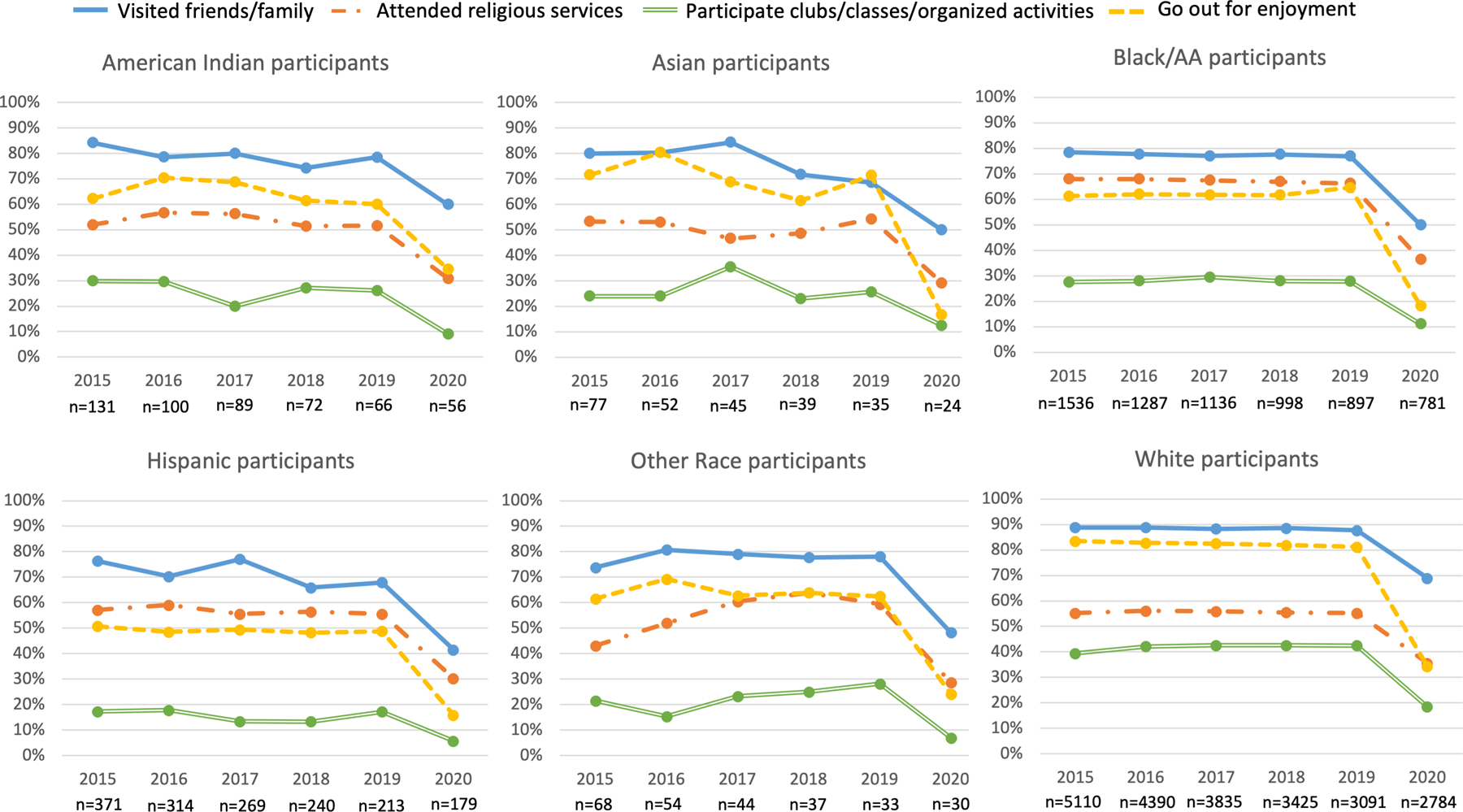
Unadjusted activity participation among racial and ethnic groups from 2015–2020
Note: We used raw data with survey weights to determine activity prevalence for each year
There were similarities and differences in these patterns by race and ethnicity (Figure 1). Among all racial and ethnic groups, visiting family and friends was the dominant activity throughout the study time (unadjusted overall percentages ranged from 66% in the Hispanic group to 85% in the White group) (Figure 1). Participating in clubs/classes/organized activities was the activity with the lowest level of participation (unadjusted overall percentages ranged from 14% in Hispanic group to 38% in the White group between 2015–2019). In unadjusted models, the second and third most popular activity overall among American Indian, Asian, Other, and White participants was the same as the total sample: going out for enjoyment as second most popular (60%, 62%, 57%, 74%, respectively) and attending religious services as third most popular (50%, 48%, 51%, 52%, respectively). Among Black and Hispanic participants, the second most prevalent activity overall was attending religious services (overall 62% and 52%, respectively). In 2020 alone, the second most prevalent activity in all racial and ethnic groups was attending religious services, except in American Indian participants where the second most prevalent activity was going out for enjoyment.
In adjusted models, we found a significant COVID-19 and race and ethnicity interaction for attending religious services (p<0.01) and going out for enjoyment (p<0.001) (Figure 2 displays the fully adjusted models and the Supplemental Appendix presents the series of weighted multivariable analyses that adjusted for age, sex, and potential mediators). Changes from before the COVID-19 pandemic to after the start of the pandemic were similar across racial and ethnic groups.
Figure 2.
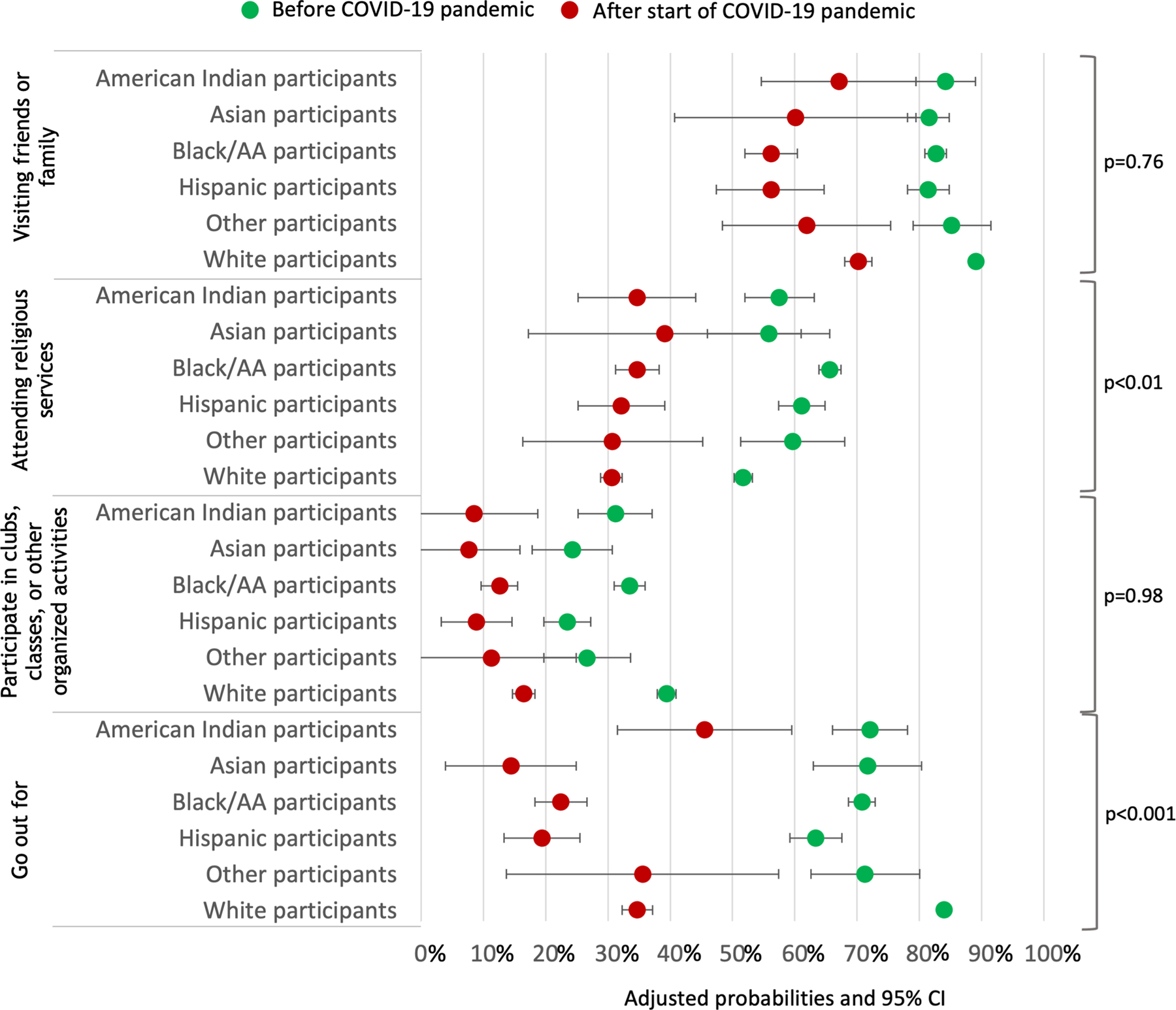
Adjusted probabilities a of activity participation before COVID-19 pandemic (2015–2019) and after start of COVID-19 pandemic (2020) b
AA African American; CI confidence interval; Proportions were adjusted for survey weighting and design.
a These models are adjusted for age, sex, impaired activities of daily living (ADLs), income, geographic region, anxiety-depression, and transportation problems.
b We used a predictive margins method to determine average predicted probability for each activity. We constructed multivariate mixed-effects logistic regression models for each activity with the interaction term and adjusted for covariates that potentially mediate meaningful activity engagement in a series of models. Then, we generated and averaged predicted probability of each activity pre-pandemic and after start of pandemic using the fitted model from the entire dataset.
The largest significant decline in activity participation across all racial and ethnic groups from before the pandemic to after the start of pandemic was in going out for enjoyment, ranging from −26% in American Indians participants to −56% in Asian participants (Figure 2). Differences also existed by race and ethnicity for the second largest decline in activity participation. For American Indian, Black, Hispanic, and Other participants, the second largest decline was in attending religious services (−24%, −32%, −28%, −26%) while for Asian participants, the second largest decline was in visiting friends and families (−24%) and in White participants, the second largest decline was in participating in clubs, classes, or organized activities (−24%).
Discussion
The COVID-19 pandemic and its aftermath resulted in physical and social isolation among older adults by limiting their ability to engage in meaningful social activities. We found that activity participation for all racial and ethnic groups remained constant between 2015–2019 and markedly declined in 2020 after the start of the pandemic. Visiting friends or family was the prevailing activity across racial and ethnic groups. Yet, it is notable that the pandemic affected racial and ethnic groups differently regarding participation in specific activities. Our study found that the largest significant decline in activity participation across all racial and ethnic groups was in going out for enjoyment, with Asian and White participants experiencing the largest decline. Attending religious services also had a significant decline in activity participation, with Black and Hispanic groups experiencing the largest decline. Unexpectedly, activity participation was not affected by factors found in previous studies6–9 such as functional status, income, anxiety and depression, and transportation problems. Thus, the inability to participate in the four activities studied here may be due to pandemic-related policies like shelter-in-place, self-imposed restrictions attributable to fear of infection and death,33 and microlevel and macrolevel manifestations of racism34 including fear of victimization from Anti-Asian American hate crimes.21,22
Older adults and those who care for them have learned to manage the balance between quality and quantity of life. We know from other studies that some older adults value quality of life as much as or in some cases more than the quantity of life.35,36 The COVID-19 pandemic put this balance in stark relief as the preventative public health measures of lockdown and shelter-in-place before the availability of vaccinations limited one’s ability to be socially active and led to a decrease in engagement in meaningful activities.12 While much was unknown during the early months of the pandemic, the potential costs of sweeping public health measures should be considered to a greater extent in future pandemic emergencies. Two studies suggest self-imposed measures such as voluntary mobility restrictions, handwashing, and mask-wearing are effective strategies to mitigate COVID-19 infections and may reduce fatalities on the same order of magnitude as government-mandated restrictions37,38 Additional strategies include efforts to reduce disparities related to access and receipt of vaccinations that help both mortality and quality of life.39,40
This novel study provides valuable insights into pandemic effects on racially and ethnically diverse community-dwelling older adults and underscores the need for tailored interventions to reengage these older adults into meaningful activities safely. For example, our study found the second largest decline was in attending religious services for Black and Hispanic participants. Other prior research found that for some Black older adults, the religious church operates as a meaningful, healthy, and safe place due to the people who are present, memories of family or friends, and feelings of peace and relaxation. These Black older adults also attributed attending religious services as a form of coping particularly with American societal racism41 compared with White older adults.33 In a separate study, some Hispanic older adults felt the church setting nurtured community bonds and felt motivated and connected when faith-based approaches were integrated into health promotion programs.42 Yet, shelter-in-place and physical distancing policies along with church closures and limited abilities of some churches to convert to online platforms prevented some older adults from engaging in this valued activity and negatively impacted the mental health of these older Black and Hispanic adults.33,41,43 Though technology-based social interactions are available as a potential solution, disparities in access to the Internet, devices, and skills still need to be addressed.12
Tailored interventions for reengagement may include addressing technology challenges and acknowledging and addressing anxiety, depression, social isolation, and loneliness in racially and ethnically diverse older adults as a result of the pandemic.12 Older adults may need regular classes or tutoring in order to increase comfort and access to evolving technology.14 For anxiety and depression, medical providers may need to be aware that some Black older adults may express depression differently than what is on questionnaires in both primary care and mental health settings.41 Akinyemi and colleagues found Black older church-going adults may express irritability, social isolation, loneliness, loss of control, or not even recognize they are anxious or sad.44
The need for cultural sensitivity and appropriateness is critical in the larger racial and ethnic groups and smaller subgroups. For example, providers need to be informed about the historical mistrust some Black older adults may have about medical providers and public officials and practice cultural humility in assessment and treatment approaches.19 Providers could recognize how stigma, negative attitudes toward mental health treatment, and language barriers may deter and prevent different racial and ethnic groups from accessing and utilizing mental health treatment.45 In some Hispanic groups, this may include the use of community health workers and advocates like promotores/promotoras,46 ensuring the appropriate language is used in materials and services, and that respect for elders and past traditions is present.46 In some Asian groups, use of the appropriate language and respect for elders and past traditions was also important.47 Additionally, results from a meta-analysis found that the largest effects associated with treatment outcomes were in treatments tailored specifically for Asian subgroups than those with no cultural tailoring. Cultural tailoring approaches previously applied to mental health interventions for Asian older adults include using Buddhist-type mindfulness for Cambodian immigrants or culturally appropriate visualization instructions for Vietnamese refugees.47
Our study also found that Asian older adults experienced the largest decline in going out for enjoyment. The pandemic intensified anti-Asian xenophobia and violence as Asian Americans were blamed for the pandemic, causing those who self-identify as Asian and Asian American to feel anxious and fearful for their lives.20–22 Antiracist policies include making the reporting of hate crimes more accessible at the local and state levels, for example through legislation like the COVID-19 Hate Crimes Act that has a particular emphasis on the increase in violence on self-identifying Asian people and Asian Americans,48 targeting aid to racial and ethnic groups that are most in need (e.g. essential frontline workers who are majority people of color49), avoiding cuts in existing services, like Medicaid,50 and continued research support on the effects of racism and efforts to mitigate these effects in different racial and ethnic groups.34
Our study had limitations. First, we may not have included other domains of factors that impact activity participation. For example, availability of informal (caregiver) and formal services like in-home supportive services were not included, which may have greater social and emotional impacts. However, formal and informal supports like family caregivers and adult day services were abruptly cut off or withdrawn during the pandemic.11,13 Second, while we speak of meaningful activities, NHATS questions asked strictly about activity participation and participation may not equate to meaningfulness. However, NHATS specifically chose these activities as they are elective but valued and meaningful to older adults.27,28 As the survey was not designed to ask about meaningful activities during a public health emergency when prior options were not available, we do not know how and if older adults replaced previous meaningful activities with other activities. In presenting this work to the UCSF Centers for Aging in Diverse Communities Community Advisory Board, community organization leaders recommended that we pursue qualitative research to understand how meaningful activity engagement may have changed for the diverse older adult. Further research is needed to guide policy and program development of culturally appropriate and relevant programs and opportunities for diverse communities of older adults. Third, we acknowledge that while the drop in activity participation from 2019 to 2020 is likely due to the pandemic, the NHATS is observational data and thus we cannot establish causality.
Conclusions
In this cohort study, we found the COVID-19 pandemic affected racial and ethnic groups differently regarding meaningful activity engagement and that activity engagement declined markedly across racial and ethnically diverse groups of older adults because of the pandemic. Life-saving public health measures and modified behaviors, like physical isolation due to fear, may have lengthened the older adults’ lives with the trade-off of a significant decrease in meaningfulness of the older adults’ lives. Policies to support community-based programs and increase access to mental health services with specific cultural, linguistic, and financial considerations should be considered to preserve the diverse older adults’ quality of life.
Supplementary Material
1. Unadjusted and adjusted percent change in activity participation by race and ethnicity from before COVID-19 pandemic (2015–2019) and after start of pandemic (2020) a, with covariates added separately in a series of models
Key points.
In a nationally representative, racially and ethnically diverse cohort sample of older adults (n=6,815), meaningful activity engagement declined markedly overall in 2020 with differences in the nature of the decline across racial and ethnically diverse groups of older adults.
Life-saving public health measures and modified behaviors, like physical isolation due to fear, may have lengthened the older adults’ lives with the trade-off of a significant decrease in meaningfulness of the older adults’ lives.
Why does this matter?
Policies to support community-based programs and increase access to mental health services with specific cultural, linguistic, and financial considerations should be considered to preserve the diverse older adults’ ability to participate in meaningful activities.
Acknowledgements
This work was supported by the National Institute on Aging (NIA) of the National Institutes of Health under grant number P30AG015272 (University of California San Francisco, Center for Aging in Diverse Communities) and VA Office of Academic Affiliations under grant number AF-3Q-09-2019-C (VA Quality Scholars). Dr. Smith was supported by NIA K24AG068312. Drs. Oh, Smith, Gan, and Boscardin were supported by the UCSF NIA Claude D. Pepper Older Americans Independence Center (P30AG044281).
Funding
This work was supported by the National Institute on Aging (NIA) of the National Institutes of Health under grant number P30AG015272 (University of California San Francisco, Center for Aging in Diverse Communities) and VA Office of Academic Affiliations under grant number AF-3Q-09-2019-C (VA Quality Scholars). Dr. Smith was supported by NIA K24AG068312. Drs. Oh, Smith, Gan, and Boscardin were supported by the UCSF NIA Claude D. Pepper Older Americans Independence Center (P30AG044281).
Footnotes
Presentations
This work was presented at the 2022 Claude D. Pepper Older Americans Independence Centers Annual Meeting (April 28–29, 2022, Washington D.C.) and 2022 Resource Centers for Minority Aging Research Annual Meeting (March 30–31, 2022, virtual).
Conflict of Interest
All authors report no conflict of interest
Sponsor’s Role
The sponsor had no role in the design, methods, data collection, analysis, or preparation of the article.
References
- 1.Tierney L, Beattie E. Enjoyable, engaging and individualised: A concept analysis of meaningful activity for older adults with dementia. Int J Older People Nurs 2020;15(2):e12306. doi: 10.1111/opn.12306 [DOI] [PubMed] [Google Scholar]
- 2.Hooker SA, Masters KS, Vagnini KM, Rush CL. Engaging in personally meaningful activities is associated with meaning salience and psychological well-being. J Posit Psychol 2020;15(6):821–831. doi: 10.1080/17439760.2019.1651895 [DOI] [Google Scholar]
- 3.Irving J, Davis S, Collier A. Aging With Purpose: Systematic Search and Review of Literature Pertaining to Older Adults and Purpose. Int J Aging Hum Dev 2017;85(4):403–437. doi: 10.1177/0091415017702908 [DOI] [PubMed] [Google Scholar]
- 4.Rowe JW, Kahn RL. Successful Aging. The Gerontologist 1997;37(4):433–440. doi: 10.1093/geront/37.4.433 [DOI] [PubMed] [Google Scholar]
- 5.Michel JP, Sadana R. “Healthy Aging” Concepts and Measures. J Am Med Dir Assoc 2017;18(6):460–464. doi: 10.1016/j.jamda.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 6.Oh A, Gan S, Boscardin WJ, et al. Engagement in Meaningful Activities Among Older Adults With Disability, Dementia, and Depression. JAMA Intern Med Published online January 25, 2021. doi: 10.1001/jamainternmed.2020.7492 [DOI] [PMC free article] [PubMed]
- 7.Ciro CA, Smith P. Improving Personal Characterization of Meaningful Activity in Adults with Chronic Conditions Living in a Low-Income Housing Community. Int J Environ Res Public Health 2015;12(9):11379–11395. doi: 10.3390/ijerph120911379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yen IH, Shim JK, Martinez AD, Barker JC. Older people and social connectedness: how place and activities keep people engaged. J Aging Res 2012;2012:139523. doi: 10.1155/2012/139523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Won J, Lee C, Forjuoh SN, Ory MG. Neighborhood safety factors associated with older adults’ health-related outcomes: A systematic literature review. Soc Sci Med 1982 2016;165:177–186. doi: 10.1016/j.socscimed.2016.07.024 [DOI] [PubMed] [Google Scholar]
- 10.Kinney AR, Graham JE, Eakman AM. Participation Is Associated With Well-Being Among Community-Based Veterans: An Investigation of Coping Ability, Meaningful Activity, and Social Support as Mediating Mechanisms. Am J Occup Ther Off Publ Am Occup Ther Assoc 2020;74(5):7405205010p1–7405205010p11. doi: 10.5014/ajot.2020.037119 [DOI] [PubMed] [Google Scholar]
- 11.Sadarangani TR, Gaugler JE, Dabelko-Schoeny H, Marx KA. Adult Day Services, Health Equity for Older Adults With Complex Needs, and the COVID-19 Pandemic. Am J Public Health 2022;112(10):1421–1428. doi: 10.2105/AJPH.2022.306968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karliner LS, Ponce A, Nguyen TT, Kaplan CP. The Impact of COVID-19: Multiethnic Older Adults and the Community-Based Organizations Serving Them, Policy Implications The Center for Aging in Diverse Communities and the Multiethnic Health Equity Research Center, University of California San Francisco; 2021. Accessed October 18, 2022. https://cadc.ucsf.edu/sites/g/files/tkssra881/f/Policy%20Brief%20Multiethnic%20Older%20Adults%20CBOs%20and%20Covid19%20Impact.pdf [Google Scholar]
- 13.Steinman MA, Perry L, Perissinotto CM. Meeting the Care Needs of Older Adults Isolated at Home During the COVID-19 Pandemic. JAMA Intern Med 2020;180(6):819–820. doi: 10.1001/jamainternmed.2020.1661 [DOI] [PubMed] [Google Scholar]
- 14.Kotwal AA, Holt-Lunstad J, Newmark RL, et al. Social Isolation and Loneliness Among San Francisco Bay Area Older Adults During the COVID-19 Shelter-in-Place Orders. J Am Geriatr Soc 2021;69(1):20–29. doi: 10.1111/jgs.16865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Batsis JA, Daniel K, Eckstrom E, et al. Promoting Healthy Aging During COVID-19. J Am Geriatr Soc 2021;69(3):572–580. doi: 10.1111/jgs.17035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carethers J m. Insights into disparities observed with COVID-19. J Intern Med 2021;289(4):463–473. doi: 10.1111/joim.13199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egede LE, Walker RJ. Structural Racism, Social Risk Factors, and Covid-19 — A Dangerous Convergence for Black Americans. N Engl J Med 2020;383(12):e77. doi: 10.1056/NEJMp2023616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ibrahimi S, Yusuf KK, Dongarwar D, Maiyegun SO, Ikedionwu C, Salihu HM. COVID-19 Devastation of African American Families: Impact on Mental Health and the Consequence of Systemic Racism. Int J MCH AIDS 2020;9(3):390–393. doi: 10.21106/ijma.408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Novacek DM, Hampton-Anderson JN, Ebor MT, Loeb TB, Wyatt GE. Mental health ramifications of the COVID-19 pandemic for Black Americans: Clinical and research recommendations. Psychol Trauma Theory Res Pract Policy 2020. June 11;12(5):449. doi: 10.1037/tra0000796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma KPK, Bacong AM, Kwon SC, Yi SS, Doàn LN. The Impact of Structural Inequities on Older Asian Americans During COVID-19. Front Public Health 2021;9. doi: 10.3389/fpubh.2021.690014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lantz B, Wenger MR. Anti-Asian Xenophobia, Hate Crime Victimization, and Fear of Victimization During the COVID-19 Pandemic. J Interpers Violence Published online May 11, 2022:8862605221086651. doi: 10.1177/08862605221086651 [DOI] [PMC free article] [PubMed]
- 22.Han S, Riddell JR, Piquero AR. Anti-Asian American Hate Crimes Spike During the Early Stages of the COVID-19 Pandemic. J Interpers Violence Published online June 3, 2022:8862605221107056. doi: 10.1177/08862605221107056 [DOI] [PMC free article] [PubMed]
- 23.Levere M, Rowan P, Wysocki A. The Adverse Effects of the COVID-19 Pandemic on Nursing Home Resident Well-Being. J Am Med Dir Assoc 2021;22(5):948–954.e2. doi: 10.1016/j.jamda.2021.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bergman C, Stall NM, Haimowitz D, et al. Recommendations for Welcoming Back Nursing Home Visitors During the COVID-19 Pandemic: Results of a Delphi Panel. J Am Med Dir Assoc 2020;21(12). doi: 10.1016/j.jamda.2020.09.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cudjoe TKM, Prichett L, Szanton SL, Roberts Lavigne LC, Thorpe RJ. Social isolation, homebound status, and race among older adults: Findings from the National Health and Aging Trends Study (2011–2019). J Am Geriatr Soc 2022;70(7):2093–2100. doi: 10.1111/jgs.17795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DeMatteis JM, Freedman VA, Kasper JD. National Health and Aging Trends Study Round 5 Sample Design and Selection Johns Hopkins University School of Public Health; 2016. http://www.nhats.org [Google Scholar]
- 27.Kasper JD, Freedman VA. National Health and Aging Trends Study (NHATS) User Guide: Rounds 1–10 Final Release Johns Hopkins University School of Public Health; 2021. http://www.nhats.org [Google Scholar]
- 28.Freedman VA. Adopting the ICF language for studying late-life disability: a field of dreams? J Gerontol A Biol Sci Med Sci 2009;64(11):1172–1174; discussion 1175–1176. doi: 10.1093/gerona/glp095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics 1999;55(2):652–659. doi: 10.1111/j.0006-341x.1999.00652.x [DOI] [PubMed] [Google Scholar]
- 30.DeMatteis JM, Freedman VA, Kasper JD. National Health and Aging Trends Study Round 5 Income Imputation Johns Hopkins Bloomberg School of Public Health; 2016. www.nhats.org [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- 32.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 2010;122(1–2):86–95. doi: 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- 33.Chatters LM, Taylor RJ, Jackson JS, Lincoln KD. Religious Coping Among African Americans, Caribbean Blacks and Non-Hispanic Whites. J Community Psychol 2008;36(3):371–386. doi: 10.1002/jcop.20202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Su D, Alshehri K, Ern J, et al. Racism Experience Among American Adults During COVID-19: A Mixed-Methods Study. Health Equity 2022;6(1):554–563. doi: 10.1089/heq.2022.0070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the Treatment Preferences of Seriously Ill Patients. N Engl J Med 2002;346(14):1061–1066. doi: 10.1056/NEJMsa012528 [DOI] [PubMed] [Google Scholar]
- 36.King J, Yourman L, Ahalt C, et al. Quality of life in late-life disability: “I don’t feel bitter because I am in a wheelchair.” J Am Geriatr Soc 2012;60(3):569–576. doi: 10.1111/j.1532-5415.2011.03844.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jamison JC, Bundy D, Jamison DT, Spitz J, Verguet S. Comparing the impact on COVID-19 mortality of self-imposed behavior change and of government regulations across 13 countries. Health Serv Res 2021;56(5):874–884. doi: 10.1111/1475-6773.13688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teslya A, Pham TM, Godijk NG, Kretzschmar ME, Bootsma MCJ, Rozhnova G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: A modelling study. PLoS Med 2020;17(7):e1003166. doi: 10.1371/journal.pmed.1003166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nguyen KH, Anneser E, Toppo A, Allen JD, Scott Parott J, Corlin L. Disparities in national and state estimates of COVID-19 vaccination receipt and intent to vaccinate by race/ethnicity, income, and age group among adults ≥ 18 years, United States. Vaccine 2022;40(1):107–113. doi: 10.1016/j.vaccine.2021.11.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kirson N, Swallow E, Lu J, et al. The societal economic value of COVID-19 vaccines in the United States. J Med Econ 2022;25(1):119–128. doi: 10.1080/13696998.2022.2026118 [DOI] [PubMed] [Google Scholar]
- 41.DeSouza F, Parker CB, Spearman-McCarthy EV, Duncan GN, Black RMM. Coping with Racism: a Perspective of COVID-19 Church Closures on the Mental Health of African Americans. J Racial Ethn Health Disparities 2021;8(1):7–11. doi: 10.1007/s40615-020-00887-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwingel A, Gálvez P. Divine Interventions: Faith-Based Approaches to Health Promotion Programs for Latinos. J Relig Health 2016;55(6):1891–1906. doi: 10.1007/s10943-015-0156-9 [DOI] [PubMed] [Google Scholar]
- 43.Ge Y, Sainz M, Gore J, Epps F. “Everything is Either Sent by God or Used by God”: An Exploratory Study on the Impact of COVID-19 Upon the Religious Lives of Black Families Living with Dementia. J Relig Health 2021;60(5):3193–3208. doi: 10.1007/s10943-021-01332-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Akinyemi E, Watkins DC, Kavanagh J, Johnson-Lawrence V, Lynn S, Kales HC. A qualitative comparison of DSM depression criteria to language used by older church-going African-Americans. Aging Ment Health 2018;22(9):1149–1155. doi: 10.1080/13607863.2017.1337717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lavingia R, Jones K, Asghar-Ali AA. A Systematic Review of Barriers Faced by Older Adults in Seeking and Accessing Mental Health Care. J Psychiatr Pract 2020;26(5):367–382. doi: 10.1097/PRA.0000000000000491 [DOI] [PubMed] [Google Scholar]
- 46.De Guzman E, Woods-Giscombe CL, Beeber LS. Barriers and facilitators of Hispanic older adult mental health service utilization in the USA. Issues Ment Health Nurs 2015;36(1):11–20. doi: 10.3109/01612840.2014.939790 [DOI] [PubMed] [Google Scholar]
- 47.Huey SJ, Tilley JL. Effects of mental health interventions with Asian Americans: A review and meta-analysis. J Consult Clin Psychol 2018;86(11):915–930. doi: 10.1037/ccp0000346 [DOI] [PubMed] [Google Scholar]
- 48.COVID-19 Hate Crimes Act 2021; 2021. Accessed October 4, 2022. https://www.congress.gov
- 49.Rho HJ, Brown H, Fremstad S. A Basic Demographic Profile of Workers in Frontline Industries Center for Economic and Policy Research; 2020. https://www.eeoc.gov/sites/default/files/2021-04/4-28-21%20Meeting%20-%2005%20Ramirez%20-%20Supporting%20Materials.pdf [Google Scholar]
- 50.Sanders C, Leachman M, Williams E. Three Principles for an Antiracist, Equitable State Response to COVID-19 -- and a Stronger Recovery Center on Budget and Policy Priorities; 2021. Accessed October 4, 2022. https://www.cbpp.org/research/state-budget-and-tax/3-principles-for-an-antiracist-equitable-state-response-to-covid-19 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1. Unadjusted and adjusted percent change in activity participation by race and ethnicity from before COVID-19 pandemic (2015–2019) and after start of pandemic (2020) a, with covariates added separately in a series of models


