Abstract
This study aimed to characterize within-person pre-COVID-19 and COVID-19 transdiagnostic anxiety and depression symptom trajectories in emerging adults and determine the roles of neuroticism and behavioral activation in predicting these COVID-19-related changes. We recruited a sample of 342 emerging adults (ages 18-19 at baseline) who were screened on neuroticism and behavioral activation and completed symptom questionnaires on multiple occasions before and after the start of the pandemic. We examined estimates of the symptom factors of General Distress, Anhedonia-Apprehension and Fears at each wave. The Stress Amplification Model predicts a multiplicative neuroticism-adversity interaction with those high on neuroticism showing the greatest symptom increases to the pandemic. The Stably Elevated Negative Affect Model is an additive model and predicts that persons high on neuroticism will display elevated symptoms at every wave. General Distress and Anhedonia-Apprehension showed large increases from the pre-COVID-19 to COVID-19 transition then decreased thereafter. The increase brought the average General Distress score to clinical levels at the first COVID-19 wave. There was a small decrease in Fears from the pre-COVID-19 to COVID-19 transition followed by a large increase. Thus, COVID-19 was associated with both increases in psychological symptoms and some resilience. Neuroticism positively predicted the pre-COVID-19 to COVID-19 transition change in Fears but was associated with a dampening of increases in General Distress and Anhedonia-Apprehension. The results disconfirmed the stress amplification model of neuroticism but partially supported the stably elevated negative affect model.
Keywords: neuroticism, behavioral activation, COVID-19, transdiagnostic symptoms, stably elevated negative affect model
General Scientific Summary
Research on the mental health effects of the COVID-19 pandemic on the average individual remains an urgent priority and little is known about the factors predicting changes in anxiety and depression associated with the COVID-19 pandemic. This study documented that COVID-19 was associated with both increases in anxiety and depression symptoms and some resilience. Elevations on the personality trait of neuroticism predicted smaller initial pre-COVID-19 to COVID-19 transition decreases in Fears but surprisingly were associated with a dampening of initial increases in other dimensions of anxiety and depression symptoms.
The coronavirus pandemic (COVID-19) has had wide-spread effects on our lives. To protect physical health, many have spent considerable time apart from friends and family. The World Health Organization reports about half a billion confirmed cases of the virus and about 6 million individuals have already died from it (World Health Organization, 2021). Schools, offices, gyms, restaurants, and more were closed, and large social gatherings were prohibited. Additionally, unemployment sky-rocketed and childcare was scarce. In short, the pandemic created chronic and pervasive stressors for the average individual. And as many social and physical activities were restricted, there were significant barriers to enacting positive coping strategies and partaking in rewarding activities. Therefore, we expect the average individual experienced significant declines in mental health during the pandemic. However, research on the mental health effects of the COVID-19 pandemic on the average individual remains an urgent priority (Holmes et al., 2020).
Preliminary research suggests that this pandemic has had psychological effects on the average individual (e.g., Jones et al., 2021). For example, as of May 2020, the American Psychiatric Association (American Psychiatric Association, 2020) reported that 36% of respondents believed the pandemic was having a serious impact on their mental health. Additionally, 48% of Americans reported anxiety about getting COVID-19 and 62% reported anxiety about family and loved ones contracting COVID-19. Other negative psychological effects endorsed include confusion, frustration, boredom and stigma (Brooks et al., 2020). However, while this work provides a snapshot of mental health, there is need for comparisons of average pre-COVID-19 and COVID-19 trajectories to elucidate whether there have been average within-person changes in symptoms and how large they have been.
Existing data tells us little about what factors render some more vulnerable to the adverse consequences of this pandemic. Some evidence suggests that adolescents and emerging adults are at elevated risk (e.g., Kujawa et al., 2020; Nocentini, Palladino & Menesini, 2021). One study found that higher levels of early life stress and current perceptions of stress among adolescents further elevated their risk (Gotlib et al., 2021). Another study found that trait disgust proneness may be a diathesis for anxiety responses to COVID-19 (Cox et al., 2020). Of most relevance to the current study, one study found that neuroticism significantly predicted the total score on depression, anxiety and stress scales among the elderly measured during the COVID-19 pandemic, adjusting for pre-pandemic levels (Gonneaudet al., 2021). More evidence regarding neuroticism is needed, especially from studies that compare pre-COVID-19 to COVID-19 trajectories and focus on additional age groups.
We conceptualize neuroticism as a personality trait or a propensity that is relatively temporally stable in contrast to symptoms of anxiety and depression, which may be more time-varying states. Neuroticism is associated with high levels of negative affect, is heritable (40-60%) and has overlapping genetic liability with major depression (e.g., Shackman et al., 2016). Two alternative diathesis-stress conceptualizations of neuroticism have been proposed: the Stress Amplification Model and the Stably Elevated Negative Affect Model (e.g., Shackman et al., 2016). The Stress Amplification Model posits that neuroticism is associated with greater sensitivity to stress and predicts a multiplicative neuroticism-adversity interaction (e.g., Kendler et al., 2004; Lahey, 2009; Mineka & Zinbarg, 2006). In contrast, the Stably Elevated Negative Affect Model (e.g., Bolger & Shilling, 1991; Watson & Clark, 1984) is an additive diathesis-stress model and posits that persons high in Neuroticism will display elevated negative affect under any circumstances. Though these two models are not necessarily mutually exclusive, pre-COVID-19 pandemic results in young adults provide more support for the stably elevated negative affect model than for the stress amplification model (e.g., Mineka et al., 2020). Whereas Gonneaudet al. (2021) reported on neuroticism as a predictor of negative affect symptoms during COVID-19, they didn’t report their results in a manner permitting the stress amplification and stably elevated negative affect models to be contrasted. Thus, more work on this important theoretical question is needed.
Other individual difference predictors remain largely unknown, and more work is needed to identify vulnerabilities. Another personality factor closely related to individual differences in affectivity is behavioral activation system (BAS) strength. BAS is a psychological construct linked to reward sensitivity and the motivational system responsible for regulating positive affect and approach motivation (Gray & McNaughton, 2000). Of particular relevance to this investigation, low reward sensitivity may underlie anhedonia (Rizvi et al., 2016). Thus, low BAS scores may predict COVID-19-related increases in anhedonia.
An important consideration when studying symptoms of depressive and anxiety disorders is that these disorders have high rates of comorbidity (Kalin, 2020). This comorbidity can be modeled by a relatively small number of transdiagnostic symptom factors (Krueger & Eaton, 2015). The tri-level model of the structure of anxiety and depression symptoms contains three transdiagnostic factors: General Distress, Anhedonia-Apprehension and Fears (Prenoveau et al., 2010; Naragon-Gainey et al., 2016). General Distress taps symptoms common to all the anxiety and depressive disorders; Anhedonia-Apprehension is more specific to unipolar depression, social anxiety disorder and generalized anxiety disorder; and Fears taps symptoms more specific to agoraphobia, the specific phobias, social anxiety disorder and obsessive-compulsive disorder. By focusing on these transdiagnostic factors, we address symptoms common to many of the anxiety and depressive disorders in a parsimonious fashion.
The tri-level model also has significant overlap with the Hierarchical Taxonomy of Psychopathology (HiTOP; Kotov et al., 2017) - a consensual model of the structure of mental disorders that is becoming very influential. The key substantive difference between these two models is that HiTOP is broader than the tri-level model, including many forms of psychopathology in addition to anxiety and unipolar depressive disorders. However, the HiTOP Internalizing Spectrum is highly similar to the tri-level model with the primary differences being in terminology used (e.g., spectra versus a broad factor, subfactor versus an intermediate breadth factor, syndrome/disorder versus narrow breadth factor) and that the HITOP Internalizing Spectrum includes additional forms of internalizing that are not represented in the tri-level model (e.g., sexual problems, eating problems). Almost certainly, however, the tri-level General Distress, Anhedonia-Apprehension and Fears factors overlap substantially, respectively, with the HiTOP Internalizing spectra factor, Distress and Fear subfactors.
The primary aims of this project are threefold. The first is to examine COVID-19-associated changes in transdiagnostic symptoms of depression and anxiety by characterizing within-person average pre-COVID-19 and COVID-19 tri-level model trans-diagnostic symptom trajectories in a sample of emerging adults. The second is to test neuroticism’s role in vulnerability to these COVID-19-related changes and, in doing so, to test the Stress Amplification and Stably Elevated Negative Affect Models of neuroticism. The third is to test whether BAS is a predictor of COVID-19-related changes in Anhedonia-Apprehension.
Method
Participants
Participants were recruited from the Brain, Motivation and Personality Development (BrainMAPD) project, a NIMH-funded study examining threat- and reward-related neural circuitries in relation to anxiety and depression symptom dimensions. Initial eligibility was assessed by quasi-orthogonal screening questionnaires measuring reward sensitivity and threat sensitivity (Behavioral Activation Scale, BAS; Eysenck Personality Questionnaire-Neuroticism, EPQ-R-N).
Recruitment ensured sampling from high/mid/low ranges (tertiles) on both scales, with oversampling from the two diagonals of their bivariate space (i.e., high EPQ-R-N/high BAS, low EPQ-R-N/low BAS, mid EPQ-R-N/mid BAS, high EPQ-R-N/low BAS and low EPQ-R-N/high BAS). To be eligible, participants had to be between the ages of 18-19, right-handed and fluent in English. Those who met diagnostic criteria for DSM-5 (American Psychiatric Association, 2013) bipolar disorder or psychotic disorder, or current, severe substance use disorder were excluded, as were participants with MRI contraindications, and color-blindness. Eligible individuals were invited to participate and scheduled for a diagnostic interview conducted by trained research coordinators or graduate-level students. The current sample consisted of 342 individuals (66.3 % females, 33.4% males, and .31% transgender). The racial composition of the sample was 51.3% White, 30% Asian, 7.5% Multiracial, 9% Black, 1.9% Native American, and 0% Pacific Islander with 25.9% identifying their ethnicity as Hispanic/Latino.
Measures
Self-report Assessment of Symptoms
Participants completed 101 questionnaire items from anxiety and depression measures. Sixty-seven were those used to create the tri-level hierarchical model originally (Prenoveau et al., 2010), originating from five questionnaires: the Fear Survey Schedule-II (FSS; Geer, 1965), the Albany Panic and Phobia Questionnaire (APPQ; Rapee et al., 1994), the Self-Consciousness subscale of the Social Phobia Scale (SPS; Mattick & Clarke, 1998; Zinbarg & Barlow, 1996), the Inventory to Diagnose Depression (IDD; Zimmerman & Coryell, 1987), and the Mood and Anxiety Symptom Questionnaire (MASQ; Watson et al., 1995). The remaining 34 items included the 16 Penn State Worry Questionnaire items (PSWQ; Meyer et al., 1990) and the 18 Obsessive-Compulsive Inventory Revised items (OCI-R; Foa et al., 2002). The validity and reliability of each of these measures has been supported (e.g., Foa et al., 2002; Geer, 1965; Mattick & Clarke, 1998; Meyer et al., 1990; Prenoveau et al., 2010; Rapee et al., 1994; Watson et al., 1995; Zimmerman & Coryell, 1987; Zinbarg & Barlow, 1996).
Behavioral Activation
The 13-item Behavioral Activation System (BAS) Scale assesses components of reward sensitivity with empirical evidence supporting its reliability and validity (Carver & White, 1994; Kelley et al., 2019). Of the personality dimensions in the highly influential Big Five Factor Model (e.g., Goldberg, 1993), Extraversion has been most frequently related to reward sensitivity (e.g., DeYoung et al., 2007). Thus, as a secondary assessment with some relevance to reward sensitivity, we also administered the 20-item Extraversion Scale from the Big Five Aspects Scales (BFAS-E; DeYoung et al., 2007). Empirical evidence supports the reliability and validity of the BFAS-E (DeYoung et al., 2007). Given its secondary status as a measure of reward sensitivity, we considered the BFAS-E results to be exploratory and present them in the online Supplement.
Neuroticism
We administered 12 items from the Neuroticism scale of the Eysenck Personality Questionnaire (EPQ-R-N; Eysenck & Eysenck, 1975) Empirical evidence supports the reliability and validity of the original, 24-item EPQ-R-N (Eysenck & Eysenck, 1975). As a screening instrument to be administered to as large a sample as possible, we thought it important to use as brief a version as possible. Hence, with the permission of the publisher (EdITS), we shortened the instrument based on the results from Mor et al. (2008) – our previous study with a similar age group sampled from the identical geographical locations. Thus, we selected items to (a) equally represent each of Mor et al.'s three group factors and (b) have strong loadings on their group factors and the General Neuroticism Factor. To minimize the loss of information associated with shortening the scale, we also switched the response format from the original yes/no to a 0 to 3 scale. Item Response Theory (e.g., Lord, 1980) predicts – and Rodebaugh et al.’s (2004) Brief Fear of Negative Evaluation Scale results illustrate – that this response format change should increase the information provided by each item. A confirmatory factor analysis (CFA) of a hierarchical model containing three group factors and a general factor of the 12-item version in the screening sample for this study provided adequate fit (CFI=.92, RMSEA=.099, SRMR = .046). Based on that CFA, we estimated coefficient omegahierarchical (ωh; Zinbarg et al., 2006); ωh equaled .88 (which compares favorably to the value reported by Mor et al., 2008).
T1 Diagnoses of Unipolar Depression and Anxiety Disorders
The Structured Clinical Interview for DSM-5, Research Version (SCID-RV; First et al., 2015) was used to assess for psychiatric diagnoses. All interviewers had at least a bachelor’s degree and underwent extensive training and supervision, and interviewers presented each completed SCID at a supervision meeting led by a doctoral-level supervisor to arrive at consensus. We have previously shown good inter-rater agreement for our DSM diagnoses (e.g., Prenoveau et al., 2010). At T1, 18.42% of the participants (n=61) met criteria for a current diagnosis of an anxiety disorder and 6.34% (n=21) met criteria for a current diagnosis of a unipolar depressive disorder (with 4.53% of the participants, n=15, meeting criteria for current diagnoses of an anxiety disorder and a unipolar depressive disorder).
Procedure
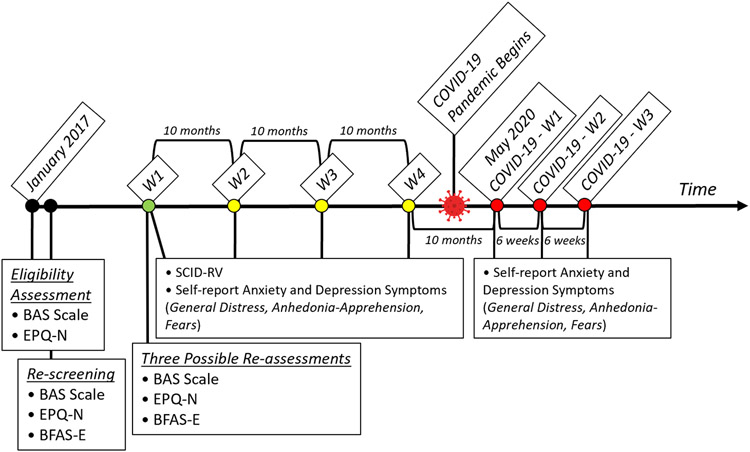
Participants who provided consent were invited to complete our self-report battery at baseline starting in January 2017. The BAS and EPQ-R-N scales were administered at baseline (T1) twice as screening assessments and three times during experimental sessions along with other questionnaires and laboratory tasks for a total of five possible administrations. Participants who completed the T1 battery were originally asked to retake it three times (n = 254, 241 and 190, respectively) at 10-month intervals following the baseline session. We re-contacted participants in May 2020 (40 months post-baseline) to ask them to consent to retake the battery at that time (n = 187), approximately 6 weeks later (n = 191) and a final time after approximately another 6 weeks later (n = 184). Figure 1 summarizes which measures were administered at each assessment wave. Participants were emailed a Qualtrics link to the battery at each wave and were compensated financially for their time upon completing each one.
Figure 1. Assessment Timeline for pre-COVID-19 and COVID-19 Waves.
Note. The present study used an assessment schedule that involved an initial screening phase where participants completed two screening measures. Beginning at the pre-COVID-19 wave 1 assessment, participants were assessed with the Structured Clinical Interview for DSM-5, Research Version (SCID-RV; First et al., 2015) and completed a self-report inventory of anxiety and depression symptoms. There were also three laboratory sessions where participants who participated in those sessions completed the screening measures again (for a maximum of 3 re-assessments). After this point, the screening measures were not re-administered as part of future waves’ assessments. Participants were again assessed with the SCID-RV and completed the self-report symptom assessment about every 10 months up through wave 4. About three months (May 2020) after the start of the pandemic (March 11, 2020), participants were contacted again and asked to complete the same self-report inventory of anxiety and depression symptoms on three occasions over the span of 12 weeks.
Assessments are indicated with colored circles in the timeline. Note that the distances between assessment circles are not always to scale; rely on the accurate, bracketed time estimates.
We examined potential associations between missing data and key study variables. First, we computed the total number of missing observations for each participant (pre-COVID waves 1 – 4 and COVID waves 1 – 3). Then, we examined whether there were significant differences between those with complete data (n=132) vs those missing at least one wave of data (n=205) on the following variables measured at baseline: the average neuroticism item score, the average BAS item score, General Distress, Anhedonia-Apprehension and Fears. None of these differences were statistically significant and all were small in magnitude (∣Cohen’s d∣ ≤ .16). Next, we computed correlations between the total number of missing observations and the following variables, measured at baseline: the average neuroticism item score, the average BAS item score, General Distress, Anhedonia-Apprehension and Fears. None of these correlations were statistically significant and all were small in magnitude (ranging from −.06 to .06). Thus, there was no evidence for differential attrition as a function of baseline levels of neuroticism, BAS, General Distress, Anhedonia-Apprehension or Fears.
Data Analysis
All analyses were conducted in Mplus version 8.7 (Muthén & Muthén, 2015) using full-information maximum likelihood to accommodate missing data and we interpreted fit using the following three fit indices: the comparative fit index (CFI), the standardized root-mean-square residual (SRMR), and the root-mean-square error of approximation (RMSEA). Following published conventions (Hu & Bentler, 1999), cutoffs for adequate fit were CFI ≥ .90, RMSEA ≤ .06, and SRMR ≤ .08. Following the recommendations of leading methodologists (Hu & Bentler, 1999, Marsh et al., 2004), we applied these standards flexibly rather than as rigid rules (i.e., we accepted a model as providing acceptable fit if it met the cutoffs for two of our three indices).
Tri-level Symptom Factor Scores
We fit the tri-level model at T1 (as reported by Zinbarg et al., 2022, fit was good - CFI = .98, RMSEA = .022, SRMR = .06 – and better than several comparison models). Supplement Table 1 presents the unstandardized factor loadings for the General Distress, Anhedonia-Apprehension and Fears factors and Supplement Table 2 presents the unstandardized factor loadings for the narrow group factors. Next, we extracted factor score estimates of General Distress and Anhedonia-Apprehension and Fears at each wave by specifying a version of the model at each subsequent wave that was scalar invariant in relation to the first. That is, we constrained unstandardized loadings and thresholds to equal the values at T1 (Supplement Table 1 presents the unstandardized factor loadings at T1). Our constraining of loadings and thresholds at every wave subsequent to the first allowed interpretation of standardized change with respect to the original factor score estimation derived at T1 (with all factors having M = 0 and SD = 1 at T1). Supplement Tables 3 - 5 present the correlations among the factor score estimates for each factor with itself over time.
Examination of the relative frequency distributions of General Distress factor scores at T1 suggested that a score of approximately .5 was where the distributions for those with a current diagnosis of an anxiety disorder or unipolar depressive disorder and those without such a diagnosis crossed and therefore is a reasonable cutoff for clinical levels (Jacobson & Truax, 1991). Indeed, a cutoff of .5 on T1 General Distress significantly discriminated among (1) those without a T1 current diagnosis of an anxiety disorder or unipolar depressive disorder, (2) those with one of these two types of diagnosis, and (3) with both of these types of diagnoses (χ2 = 56.53, df = 2, p ≤ .001). The percentage of individuals scoring at or above this cutoff for these three groups, respectively, were 21.1%, 59.6% and 100%. Based on this cutoff, 29.1% of the overall sample scored within the clinical range on T1 General Distress, suggesting that clinical elevations were relatively common in this sample.
Piecewise Latent Growth Curve Models (PLGCMs)
Our PLGCMs focused on one symptom dimension at a time. In other words, unconditional and conditional trajectory modeling was always limited to one factor of interest, using factor scores as described above. We began the unconditional modeling for each factor with a single piece PLGCM and examined progressively more complex models up to a three-piece PLGCM with the first piece corresponding to the pre-COVID-19 waves (from 0 to 30 months), the second piece to the pre-COVID-19 to COVID-19 transition (i.e., the change from the last pre-COVID-19 wave, at 30 months, to the first COVID-19 wave, at 40 months) and the final piece to our COVID-19 maintenance period (i.e., from the first COVID-19 wave, at 40 months, to the third COVID-19 wave, at 43 months).
Measurement Models for Neuroticism and Behavioral Activation
A general neuroticism factor and general behavioral activation factor were modeled from EPQ-R-N and BAS items, respectively, as latent variables in our conditional PLGCMs. To generate latent variables corresponding to neuroticism and behavioral activation, we carried out several processing steps. First, we computed means of each neuroticism and behavioral activation item based on the available data at T1 (as stated above, both the EPQ-R-N and BAS were administered five times at T1). Data from at least one of the T1 screening assessments and at least one of the T1 experimental sessions were required to compute item means (when this rule was not met, data were treated as missing). After means were computed for each item, we used these means to fit hierarchical models of neuroticism and behavioral activation.
For the neuroticism model, we specified three group factors which were labeled Depression (4 items). Self-Consciousness (3 items), and Anxiety (4 items) in accordance with the results of Mor et al. (2008). All these indicators also loaded on a general factor in addition to a single item not used as an indicator of any group factor for a total of 12 general factor loadings. All factors were constrained to be orthogonal. We also constrained two item residual variances to zero. Model fit was adequate on two of our three fit indices (χ2(45) = 170.99, CFI = .96, RMSEA = .094, SRMR = .03). Table 1 presents the standardized factor loadings for the neuroticism model.
Table 1.
Standardized Factor Loadings from the Hierarchical Neuroticism Model
| Neuroticism Factor | |||||
|---|---|---|---|---|---|
| EPQ-R-N Item | Paraphrased Item Text | Depression | Self-Consciousness | Anxiety | General |
| 1 | mood up and down? | .46 | .72 | ||
| 2 | “miserable”? | .58 | .71 | ||
| 5 | feel sick of things? | .36 | .71 | ||
| 12 | lonely? | .48 | .58 | ||
| 3 | concerned about things you said? | .33 | .80 | ||
| 4 | feelings hurt? | .02a | .72 | ||
| 10 | concerned about embarrassing experiences? | .67 | .74 | ||
| 7 | nervous? | .62 | .78 | ||
| 8 | worry a lot? | .33 | .80 | ||
| 9 | feel tense often? | .23 | .70 | ||
| 11 | have “nerves”? | .42 | .72 | ||
| 6 | feel guilty? | .79 | |||
Note. EPQ-R-N = Eysenck Personality Questionnaire – Neuroticism scale (Eysenck & Eysenck, 1975). Residual variances of items 7 and 10 were constrained to zero. All loadings were significant (p < .001) unless noted otherwise. Items
Item loading was not significant (p = .619).
In the behavioral activation model, there were also three group factors. They were labeled Drive (4 items), Reward Responsivity (5 items), and Fun Seeking (4 items) in accordance with the original scale guidelines (Carver & White, 1994). The general factor (13 items) was defined by all those items that loaded on the group factors with no additional items beyond these indicators. All factors were constrained to be orthogonal. This hierarchical structure was found to fit best in a previous study (Kelley et al., 2019). We observed adequate fit of the behavioral activation model on each examined fit index, except RMSEA (χ2(52) = 193.19, CFI = .94, RMSEA = .093, SRMR = .05). Table 2 displays the standardized factor loadings for the behavioral activation model. Measurement model results for the BFAS-E are presented in the Supplement.
Table 2.
Standardized Factor Loadings from the Hierarchical Behavioral Activation System Model
| Behavioral Activation System Factor | |||||
|---|---|---|---|---|---|
| BAS Item | Item Text | Drive | Reward Responsiveness |
Fun Seeking | General |
| 1 | I go out of my way to get the things I want. | .56 | .60 | ||
| 5 | When I want something, I usually go all-out to get it. | .75 | .62 | ||
| 7 | If I see a chance to get something I want, I move on it right away. | .20a | .76 | ||
| 12 | When I go after something, I use a “no holds barred” approach. | .36 | .65 | ||
| 2 | When I’m doing well at something, I love to keep at it. | .42 | .51 | ||
| 4 | When I get something I want, I feel excited and energized. | .65 | .65 | ||
| 8 | When I see an opportunity for something I like, I get excited right away. | .32 | .76 | ||
| 10 | When good things happen to me, it affects me strongly. | .55 | .56 | ||
| 13 | It would excite me to win a contest. | .60 | .43 | ||
| 3 | I’m always willing to try something new if I think it will be fun. | .59 | .46 | ||
| 6 | I will often do things for no other reason than that they might be fun. | .81 | .34 | ||
| 9 | I often act on the spur of the moment. | .49 | .48 | ||
| 11 | I crave excitement and new sensations. | .54 | .50 | ||
Note. BAS = Behavioral Activation Scale (Carver & White, 1994). All loadings were significant (p < .001) unless noted otherwise.
p = .007.
Transparency and openness
The raw data on which study conclusions are based are available upon request from RZ. The Mplus input (and output) files containing the syntax to reproduce the analyses conducted for this study are also available upon request from RZ. The materials described in the methods section are also available upon request from RZ with the exception of our revision of the EPQ-R-N scale as the EPQ-R-N scale is copyrighted. This study was not pre-registered.
Results
Unconditional PLGCMs
General Distress
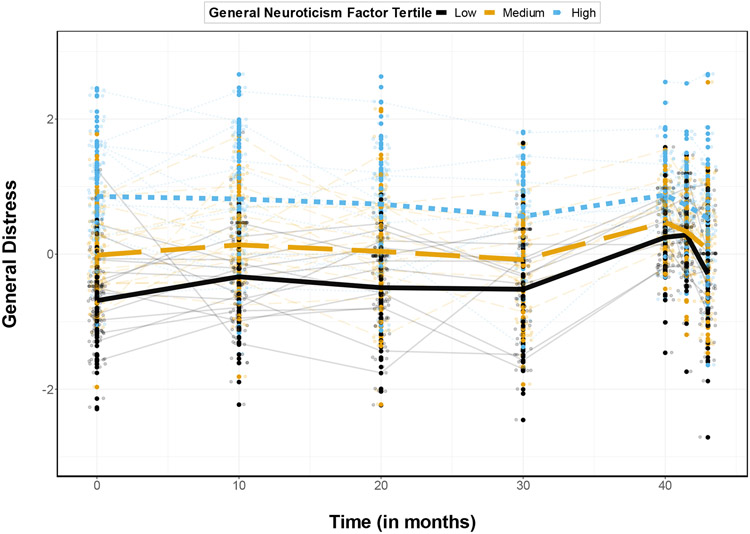
The best fitting PLGCM for General Distress was a 3-piece model with the first piece consisting of only an intercept and with the slope of the second piece regressed on the intercept (see Table 3). As can be seen in Figure 2, the trajectory of General Distress was relatively flat over the pre-COVID-19 waves. As shown in Figure 2 and Table 4, there was a large (almost .5 SD) increase in General Distress from the pre-COVID-19 to COVID-19 transition that brought the unconditional PLCGM at the first COVID-19 wave to the cutoff (.5) for clinical levels of General Distress. This increase was followed by a large decrease in General Distress over the COVID-19 maintenance period back to around pre-COVID-19 levels.
Table 3.
Unconditional Piecewise Latent Growth Curve Model Fit Indices and Comparisons for Trans-diagnostic Tri-level Model Dimensions
| Model | χ2 | df | p | CFI | SRMR | RMSEA [90% CI] |
|---|---|---|---|---|---|---|
| General Distress | ||||||
| 1-piece, Int Only | 349.29 | 24 | .70 | .187 | .199 [.181 – .218] | |
| 2-piece, s2 on i | 170.22 | 21 | .86 | .131 | .144 [.124 – .165] | |
| Difference | 179.07 | 3 | < .001 | .16 | .056 | .055 |
| 3-piece, s2 on i | 47.41 | 19 | .97 | .046 | .066 [.043 – .090] | |
| Difference | 122.81 | 2 | < .001 | .11 | .085 | .078 |
| 3-piece, s2 on I, s3 fixeda | 63.24 | 20 | .96 | .055 | .080 [.058 – .102] | |
| Difference | 15.83 | 1 | < .001 | .01 | .009 | .014 |
| Anhedonia-Apprehension | ||||||
| 1-piece | 190.31 | 23 | .63 | .182 | .146 [.127 – .165] | |
| 2-piece | 95.19 | 21 | .84 | 186 | .102 [.081 – .123] | |
| Difference | 95.12 | 2 | < .001 | .21 | −.004 | .044 |
| 2-piece, s2 on I | 33.74 | 20 | .97 | .057 | .045 [.015 – .070] | |
| Difference | 61.45 | 1 | < .001 | .13 | .129 | .057 |
| 3-piece, s2 on I | 20.88 | 18 | .99 | .047 | .022 [.000 – .055] | |
| Difference | 12.86 | 2 | < .01 | .02 | .010 | .023 |
| Fears | ||||||
| 1-piece, Int Only | 137.16 | 27 | .91 | .081 | .109 [.091 – .128] | |
| 2-piece | 102.32 | 25 | .94 | .067 | .095 [.076 – .115] | |
| Difference | 34.84 | 2 | < .001 | .03 | .014 | .014 |
| 3-piece | 43.74 | 23 | .98 | .044 | .051 [.027 – .074] | |
| Difference | 58.58 | 2 | < .001 | .04 | .023 | .044 |
Note. CFI = Comparative Fit Index; SRMR = Standardized Root Mean Squared Residual; RMSEA = Root Mean Squared Error of Approximation.
The variance of the third piece slope was fixed to zero because it was estimated to be negative when not fixed.
Meaningful differences in fit: ΔCFI > 0.01, (ΔRMSEA > 0.015), and ΔSRMR > 0.015
Figure 2. Unconditional Transdiagnostic Symptom Trajectories from pre- to COVID-19 Transition.
Note. Lines that reflect change across time for each dimension were generated using a loess smoothing function.
Table 4.
Unconditional Piecewise Latent Growth Curve Model Factor Means and Variances for Trans-diagnostic Tri-level Model Dimensions
| Factor | Model | Mean | SE | p | Variance | SE | p |
|---|---|---|---|---|---|---|---|
| General Distress | Intercept | .038 (−.031 .107) | .035 | .277 | .278 (.197 .360) | .041 | < .001 |
| Covid Initial | .483 (.419 .546) | .032 | < .001 | .042 (.002 .083) | .021 | .042 | |
| Covid Maintenance | −1.459 (−1.861 −1.056) | .205 | < .001 | fixed | fixed | fixed | |
| Anhedonia-Apprehension | Intercept | .004 (−.089 .096) | .046 | .936 | .325 (.251 ..398) | .037 | < .001 |
| Pre-Covid slope | .141 (.102 .180) | .020 | < .001 | .005 (−.003 .014) | .004 | .221 | |
| Covid Initial | .594 (.475 .712) | .060 | < .001 | .299 (.205 .393) | .048 | < .001 | |
| Covid Maintenance | −.112 (−3.413 2.658) | 1.684 | .947 | 1.632 (−3.799 7.063) | 2.771 | .556 | |
| Fears | Intercept | .016 (−.061 .093) | .039 | .688 | .438 (.355 .521) | .042 | < .001 |
| Covid Initial | −.202 (−.27 −.13) | .037 | < .001 | .108 (.061 .155) | .024 | < .001 | |
| Covid Maintenance | .842 (.58 1.10) | .132 | < .001 | .603 (−.11 1.32) | .366 | .099 |
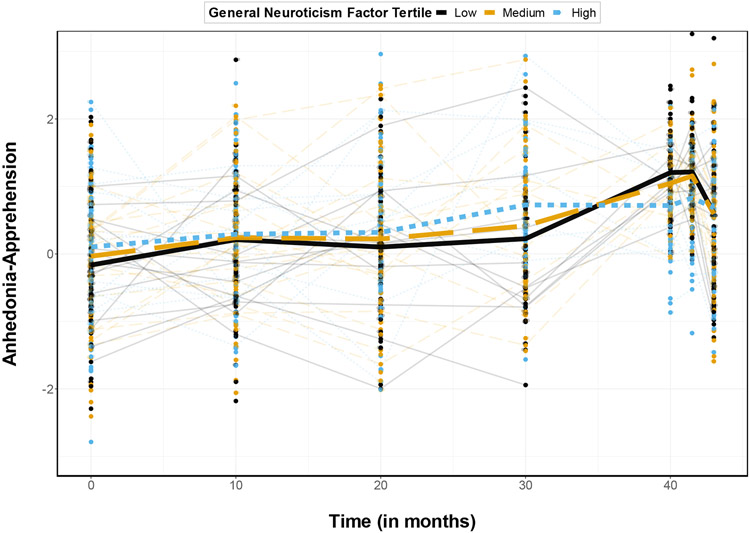
Anhedonia-Apprehension
The best fitting PLGCM for Anhedonia-Apprehension was a 3-piece model with the first piece including both an intercept and a linear slope and the slope of the second piece regressed on the intercept (see Table 3). As can be seen in Figure 2, the trajectory of Anhedonia-Apprehension increased over the pre-COVID-19 waves (with the mean slope equaling about .14 SD per wave as shown in Table 4). As shown in Figure 2 and Table 4, there was a large (almost .6 SD) increase in Anhedonia-Apprehension from the pre-COVID-19 to COVID-19 transition followed by a large decrease in Anhedonia-Apprehension over the COVID-19 maintenance period (back to around the level they would have been had the Anhedonia-Apprehension pre-COVID-19 trajectory continued).
Fears
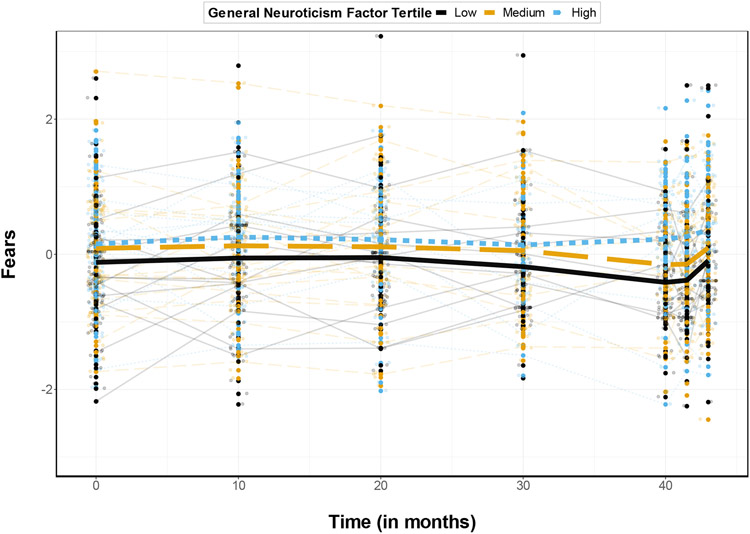
The best fitting PLGCM for Fears was a 3-piece model with the first piece consisting of only an intercept (see Table 3). As can be seen in Figure 2, the trajectory of Fears was relatively flat over the pre-COVID-19 waves (as reflected in the intercept-only first piece of the model). As shown in Figure 2 and Table 4, there was a small (approximately .2 SD) decrease in Fears from the pre-COVID-19 to COVID-19 transition followed by a large increase in Fears over the COVID-19 maintenance period.
Conditional PLGCMs
Prediction by the General Neuroticism Factor
Conditional PLGCMs including the General Neuroticism Factor as a predictor of the trajectory parameters fit adequately (except that the RMSEA point estimate for the General Distress model fell just short of the conventional cutoff; see Table 5). As shown in Table 6 and Figures 3 - 5, the General Neuroticism Factor significantly and positively predicted the intercept of all three symptom dimensions. In addition, the General Neuroticism Factor was a significant and positive predictor of the initial pre-COVID-19 to COVID-19 transition change in Fears (Table 6 and Figure 5). Thus, the higher one’s General Neuroticism Factor score, the smaller the decrease in Fears over the pre-COVID-19 to COVID-19 transition. The General Neuroticism Factor was also a significant negative predictor of the pre-COVID-19 to COVID-19 transition change in General Distress and Anhedonia-Apprehension (Table 6 and Figures 3 and 4). That is, the higher one’s General Neuroticism Factor score, the smaller the increases in General Distress and Anhedonia-Apprehension over the pre-COVID-19 to COVID-19 transition. It should also be noted that based on the parameter estimates in Table 6, those who were at least 1 SD above the mean on the General Neuroticism Factor began the study (that is, had an intercept) in the clinical range on General Distress and tended to remain in the clinical range throughout the entire study.
Table 5.
Conditional Piecewise Latent Growth Curve Models: Fit of Models with the General Neuroticism Factor (GNF) and the General Behavior Activation System (BAS) Factor as Predictors
| Model | χ2 | df | CFI | SRMR | RMSEA [90% CI] |
|---|---|---|---|---|---|
| General Distress | |||||
| GNF | 403.55 | 169 | .95 | .055 | .064 [.056 – .072] |
| BAS | 389.73 | 186 | .94 | .056 | .057 [.049 – .064] |
| Anhedonia-Apprehension | |||||
| GNF | 313.04 | 166 | .96 | .049 | .051 [.042 – .059] |
| BAS | 353.02 | 183 | .94 | .062 | .052 [.044 – .060] |
| Fears | |||||
| GNF | 310.00 | 172 | .97 | .050 | .048 [.040 – .057] |
| BAS | 341.34 | 189 | .96 | .073 | .049 [.040 – .057] |
Note. CFI = Comparative Fit Index; SRMR = Standardized Root Mean Squared Residual; RMSEA = Root Mean Squared Error of Approximation.
Table 6.
Conditional Piecewise Latent Growth Curve Models: The General Neuroticism Factor’s Prediction of Intermediate- to General-Breadth Trilevel Model Dimension Growth Factors
| Dimension | Factor | β | b (SE) | 95% CI | p |
|---|---|---|---|---|---|
| General Distress | Intercept | .87 | .63 (.035) | [.56, .69] | < .001 |
| Covid Initial | −.39 | −.20 (.079) | [−.35, −.04] | .013 | |
| Covid Maintenance | a | .10 (.211) | [−.32, .51] | .654 | |
| Anhedonia-Apprehension | Intercept | .18 | .11 (.051) | [.01, .21] | .026 |
| Pre-Covid slope | .29 | .03 (.022) | [−.02, .07] | .245 | |
| Covid Initial | −.52 | −.34 (.065) | [−.46, −.21] | < .001 | |
| Covid Maintenance | .29 | .58 (.394) | [−.19, 1.35] | .143 | |
| Fears | Intercept | .21 | .14 (.042) | [.05, .22] | .001 |
| Covid Initial | .39 | .13 (.038) | [.05, .20] | .001 | |
| Covid Maintenance | −.28 | −.23 (.153) | [−.53, .07] | .138 |
Note. β = standardized regression coefficient; b = unstandardized regression coefficient.
a = the standardized standard error was estimated to equal 0 so the standardized regression coefficient was not interpretable.
Figure 3. General Distress Trajectories by General Neuroticism Factor Tertile.
Note. To create this figure, participants were separated into tertiles based on their baseline General Neuroticism Factor scores (analyses treated General Neuroticism Factor scores as a continuous variable). Bolded lines reflect the mean observed trajectories of each dimension by General Neuroticism Factor tertile. The smaller, fainter lines (also called spaghetti plot “strands”) show observed change in a randomly selected sub-sample of 60 participants.
Figure 5. Fears Trajectories by General Neuroticism Factor Tertile.
Note. To create this figure, participants were separated into tertiles based on their baseline General Neuroticism Factor scores (analyses treated General Neuroticism Factor scores as a continuous variable). Bolded lines reflect the mean observed trajectories of each dimension by General Neuroticism Factor tertile. The smaller, fainter lines (also called spaghetti plot “strands”) show observed change in a randomly selected sample of 60 participants.
Figure 4. Anhedonia-Apprehension Trajectories by General Neuroticism Factor Tertile.
Note. To create this figure, participants were separated into tertiles based on their baseline General Neuroticism Factor scores (analyses treated General Neuroticism Factor scores as a continuous variable). Bolded lines reflect the mean observed trajectories of each dimension by General Neuroticism Factor tertile. The smaller, fainter lines (also called spaghetti plot “strands”) show observed change in a randomly selected sample of 60 participants.
Prediction by the General BAS Factor
Conditional PLGCMs including the general BAS factor as a predictor of the trajectory parameters fit adequately or better (see Table 5). The only significant effect involving the general BAS factor was a significant, negative prediction of the Anhedonia-Apprehension intercept (Table 7). That is, the higher one’s general BAS factor score, the lower the baseline Anhedonia-Apprehension score. (Results for the correlations of each observed personality trait item with the symptom scores are available upon request from REZ)
Table 7.
Conditional Latent Growth Curve Models: The General Behavioral Activation System Factor’s Prediction of Intermediate- to General-Breadth Trilevel Model Dimension Growth Factors
| Dimension | Factor | β | b (SE) | 95% CI | p |
|---|---|---|---|---|---|
| General Distress | Intercept | −.04 | −.03 (.050) | [−.13, .07] | .523 |
| Covid Initial | .06 | .03 (.030) | [−.03, .09] | .324 | |
| Covid Maintenance | a | −.14 (.167) | [−.46, .19] | .416 | |
| Anhedonia-Apprehension | Intercept | −.45 | −.29 (.052) | [−.39, −.19] | < .001 |
| Pre-Covid slope | .28 | .02 (.022) | [−.02, .07] | .298 | |
| Covid Initial | −.08 | −.05 (.075) | [−.19, .10] | .537 | |
| Covid Maintenance | .00 | .00 (.225) | [−.44, .44] | .989 | |
| Fears | Intercept | −.02 | −.01 (.046) | [−.10, .08] | .815 |
| Covid Initial | .04 | .01 (.041) | [−.07, .09] | .737 | |
| Covid Maintenance | .36 | .27 (.145) | [−.01, .56] | .062 |
Note. β = standardized regression coefficient; b = unstandardized regression coefficient.
a = the standardized standard error was estimated to equal 0 so the standardized regression coefficient was not interpretable.
Discussion
The unconditional PLGCMs showed large increases in General Distress and Anhedonia-Apprehension over the pre-COVID-19 to COVID-19 transition. Indeed, this increase was large enough to bring the unconditional PLGCM at the first COVID-19 wave to the previously derived cutoff for clinical levels of General Distress (.5). In contrast, there was an initial small decrease in Fears over the pre-COVID-19 to COVID-19 transition followed by a large increase in Fears over our COVID-19 maintenance period. Thus, there was a significant increase in symptoms at some point during our COVID-19 measurement waves for each of these three symptom dimensions. The present data therefore add to the growing literature documenting that COVID-19 has been associated with an increase in psychological distress (e.g., Aknin et al., 2021; Ettman et al., 2020;). Indeed, our General Distress results suggest that these elevations have often reached clinical levels.
The unconditional PLGCMs also showed large decreases in General Distress and Anhedonia-Apprehension following the initial increases, suggesting a relatively rapid recovery process for these two dimensions. In addition, as stated above, the unconditional PLGCMS showed an initial small decrease in Fears over the pre-COVID-19 to COVID-19 transition. Accordingly, the present data for all three dimensions also add to a growing literature documenting at least some resilience in the face of the massive, widespread stress and hardship associated with COVID-19 (Aknin et al., 2021).
The neuroticism findings for General Distress and Anhedonia-Apprehension disconfirm the Stress Amplification model of neuroticism. Rather than amplifying the symptom increases in these two dimensions as that model predicts, neuroticism was associated with a significant dampening of these symptom increases. That the Anhedonia-Apprehension results show a cross-over pattern with the medium and low neuroticism participants having at least as high of Anhedonia-Apprehension elevations as the high neuroticism individuals in the first two waves of COVID-19 data collection even rules out a scaling artifact as an explanation for the Anhedonia-Apprehension neuroticism findings. And the Fears results do not provide much support for the stress amplification results as Figure 4 reveals a relatively flat trajectory over the pre-COVID-19 to COVID-19 transition for the high neuroticism participants (whereas the less neurotic participants showed a decrease in Fears over this transition).
The findings do provide some support for the Stably Elevated Negative Affect Model of neuroticism. Specifically, participants with high neuroticism showed elevated General Distress and Fears relative to those low in neuroticism at every wave. Finding greater support for the Stably Elevated Negative Affect Model than the Stress Amplification model of neuroticism replicates the pattern of findings reported by Mineka et al. (2020) and extends them to dimensional measures of transdiagnostic symptoms of anxiety and depression (Mineka et al. reported results for categorical diagnoses) and to the serious and widespread stressor of the COVID-19 pandemic.
The Anhedonia-Apprehension results, however, clearly do not support the Stably Elevated Negative Affect Model of neuroticism. Perhaps this is because Anhedonia-Apprehension primarily reflects (the absence of) positive affect and we need a separate theoretical model of neuroticism’s association with positive affect than for its association with negative affect. One speculative explanation rests on neuroticism being associated with avoidant tendencies in general (Dunkley et al., 2006) with some evidence that this extends to avoidance of socializing (Danvers et al., 2020). Thus, those high on neuroticism may experience less of a drop in positive affect from socializing when socializing was severely restricted given they were avoidant of socializing prior to this pandemic. As this speculation - which we call the socially avoidant model of neuroticism and positive affect - was a post-hoc explanation of the current pattern of Anhedonia-Apprehension results, the present results cannot be said to either test or support it. Rather, the present results motivated the development of this hypothesis. Thus, future empirical tests are needed to interrogate the validity of the socially avoidant model of neuroticism and positive affect.
Limitations and Conclusion
Our study has at least six limitations. First, our initial wave of COVID-19 data occurred approximately three months after COVID-19 was declared a public health emergency and our final COVID-19 wave occurred only 3 months later. It is possible, therefore, that the increases in Anhedonia-Apprehension and General Distress preceded the start of this pandemic and that there were subsequent increases in these symptoms later in this pandemic. Second, as this study was not an experiment, something other than the COVID-19 pandemic may have accounted for the symptom increases we observed even if we were certain that the Anhedonia-Apprehension and General Distress increases followed the start of the pandemic. All research into the mental health effects of the pandemic suffers from this same limitation, however. Third, we cannot pinpoint the reasons why symptoms changed. We cannot say, for example, whether the increases we observed were more due to disruptions in people’s social lives, worry about infection, or loss of loved ones. Fourth, our sample consisted of young adults who were not selected on the basis of risk factors for the deleterious physical effects of COVID-19. It is possible that the effects described here could differ across development or among those more vulnerable to the physical effects of COVID-19. Fifth, demand may have played a role in the observed results given our sole reliance on self-report symptom measures, although the pattern of findings suggests otherwise. That is, demand biases would be more plausible had Fears initially increased (rather than decreased) and had General Distress and Anhedonia-Apprehension remained elevated (rather than declined) over the COVID-19 maintenance period.
The final limitation discussed here is that we oversampled on the two diagonals of the bivariate space defined by the EPQ-R-N and BAS such that the sample is not representative of any known population. Whereas some recommend using sampling weights to analyze oversampled data, doing so is a controversial practice that has been heavily criticized as limited in both applicability and interpretability (e.g., Gelman, 2007). Additionally, simulations reported by Hauner et al. (2014, p. 797) showed that “oversampling does not bias effect sizes to a degree that would typically impact results in behavioral research”.
This study also has several strengths, including well-characterized transdiagnostic symptom trajectories in individuals over a several year period prior to the start of the COVID-19 pandemic and multiple waves of symptom assessment during the COVID-19 pandemic. As a result of these design features, this study documents within-participant increases in young adults in transdiagnostic symptoms of anxiety and depression above and beyond their pre-COVID-19 trajectories. Importantly, these increases were large enough to bring the unconditional PLCGM at the first COVID-19 wave to the cutoff for clinical levels of General Distress. In addition, the decreases we observed in General Distress and Anhedonia-Apprehension during our COVID-19 maintenance period point to at least some resilience among young adults. Because General Distress, Anhedonia-Apprehension and Fears almost certainly overlap substantially with the HiTOP dimensions of the Internalizing spectrum, Distress subfactor, and Fear subfactor, respectively, our results likely also have implications for how these HiTOP dimensions change over time and in response to potent stressors. Aspects of the present results also disconfirm the Stress Amplification Model of neuroticism and provide some support for the Stably Elevated Negative Affect Model of neuroticism. Finally, the present results generated a hypothesis, the socially avoidant model of neuroticism and positive affect, that awaits testing in future research.
Supplementary Material
Acknowledgments:
This work was supported by the National Institute of Mental Health (NIMH) under award number R01MH100117, awarded to MC, Susan Bookheimer, RN, and REZ. Additional funding for this work came from a private donation by Fasano Associates to Northwestern University.
Footnotes
Some of the material in this article were presented at the 2021 Society for Research in Psychopathology Meeting, Virtual Meeting, September 23-26. This study was approved by IRB at University of California, Los Angeles (IRB#13-001606) and Northwestern University (IRB#STU00086226). The raw data on which study conclusions are based are available upon request from RZ. The Mplus input (and output) files containing the syntax to reproduce the analyses conducted for this study are also available upon request from RZ. The materials described in the methods section are also available upon request from RZ with the exception of our revision of the EPQ-R-N scale as the EPQ-R-N scale is copyrighted. This study was not pre-registered.
Conflict of Interest Disclosures: None
References
- Aknin L, De Neve JE, Dunn E, Fancourt D, Goldberg E, Helliwell JF, Jones SP, Karam E, Layard R, Lyubomirsky S, Rzepa A, Saxena S, Thornton EM, VanderWeele TJ, Whillans AV, Zaki J, Caman OK, & Ben Amor Y (2021). Mental health during the First Year of the COVID-19 pandemic: a review and recommendations for moving forward. Perspectives on Psychological Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- American Psychiatric Association. (2020). New Poll: COVID-19 impacting mental Well-being: Americans feeling anxious, Especially for Loved ones; older adults are less anxious. American Psychiatric Association-News Releases. [Google Scholar]
- Bolger N, & Schilling EA (1991). Personality and the problems of everyday life: The role of neuroticism in exposure and reactivity to daily stressors. Journal of personality, 59(3), 355–386. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The lancet, 395(10227), 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & White TL (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. Journal of Personality and Social Psychology, 67(2), 319–333. [Google Scholar]
- Cox RC, Jessup SC, Luber MJ, & Olatunji BO (2020). Pre-pandemic disgust proneness predicts increased coronavirus anxiety and safety behaviors: Evidence for a diathesis-stress model. Journal of Anxiety Disorders, 76, 102315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danvers AF, Sbarra DA, & Mehl MR (2020). Understanding Personality through Patterns of Daily Socializing: Applying Recurrence Quantification Analysis to Naturalistically Observed Intensive Longitudinal Social Interaction Data. European Journal of Personality, 34(5), 777–793. [Google Scholar]
- DeYoung CG, Quilty LC & Peterson JB (2007). Between facets and domains: 10 Aspects of the Big Five. Journal of Personality and Social Psychology, 93, 880–896. [DOI] [PubMed] [Google Scholar]
- Dunkley DM, Sanislow CA, Grilo CM, & McGlashan TH (2006). Perfectionism and depressive symptoms 3 years later: Negative social interactions, avoidant coping, and perceived social support as mediators. Comprehensive Psychiatry, 47(2), 106–115. [DOI] [PubMed] [Google Scholar]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, & Galea S (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA network open, 3(9), e2019686–e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ, & Eysenck SBG (1975). Manual of the Eysenck Personality Questionnaire (junior and adult). London: Hodder and Stoughton. [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL. (2015): Structured Clinical Interview for DSM-5—Research Version. Arlington, VA: American Psychiatric Association. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, & Salkovskis PM (2002). The Obsessive-Compulsive Inventory: development and validation of a short version. Psychological Assessment, 14(4), 485–496. [PubMed] [Google Scholar]
- Geer JH (1965). The development of a scale to measure fear. Behaviour Research and Therapy, 3(1), 45–53. [DOI] [PubMed] [Google Scholar]
- Gelman, 2007 [Google Scholar]
- Goldberg LR (1993). The structure of phenotypic personality traits. American Psychologist, 48, 26–34. [DOI] [PubMed] [Google Scholar]
- Gonneaud J, Paly L, Delarue M, Mézenge F, Fauvel S, Lefranc V, Cognet A, de Flores R, Touron E, Marchant NL, Poisnel G, Chetelat G, & Medit-Ageing Research group. (2021). Neuroticism is the best predictor of lower emotional resilience during the COVID–19-related confinement periods. Alzheimer's & Dementia, 17, e053954. [Google Scholar]
- Gotlib IH, Borchers LR, Chahal R, Gifuni AJ, Teresi GI, & Ho TC (2021). Early life stress predicts depressive symptoms in adolescents during the COVID-19 pandemic: The mediating role of perceived stress. Frontiers in Psychology, 11, 603748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray J, & McNaughton N (2000). The Neuropsychology of Anxiety: An Enquiry into the Functions of the Septo-Hippocampal System (2nd ed.) Oxford: Oxford University Press. [Google Scholar]
- Hauner K, Zinbarg R & Revelle W (2014). A latent variable model approach to estimating systematic bias in the oversampling method. Behavior Research Methods, 46, 786 – 797. [DOI] [PubMed] [Google Scholar]
- Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Silver RC, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, … & Bullmore E (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L. t., & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal, 6(1), 1–55. [Google Scholar]
- Jacobson NS, & Truax P (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. [DOI] [PubMed] [Google Scholar]
- Kalin NH (2020). The critical relationship between anxiety and depression. American Journal of Psychiatry, 177(5), 365–367. [DOI] [PubMed] [Google Scholar]
- Kelley NJ, Kramer AM, Young KS, Echiverri-Cohen AM, Chat IKY, Bookheimer SY, Nusslock R, Craske MG, & Zinbarg RE (2019). Evidence for a general factor of behavioral activation system sensitivity. Journal of research in personality, 79, 30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Kuhn J, & Prescott CA (2004). The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. American Journal of Psychiatry, 161(4), 631–636. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, Brown TA, Carpenter WT, Caspi A, Clark LA, Eaton NR, Forbes MK, Forbush KT, Goldberg D, Hasin D, Hyman SE, Ivanova MY, Lynam DR, Markon K, … & Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of abnormal psychology, 126(4), 454–477. [DOI] [PubMed] [Google Scholar]
- Krueger RF, & Eaton NR (2015). Transdiagnostic factors of mental disorders. World Psychiatry, 14(1), 27–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa A, Green H, Compas BE, Dickey L, & Pegg S (2020). Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depression and Anxiety, 37(12), 1280–1288. [DOI] [PubMed] [Google Scholar]
- Lahey BB (2009). Public health significance of neuroticism. American Psychologist, 64(4), 241–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord FM (1980). Applications of Item Response Theory to Practical Testing Problems. Hillsdale, NJ: Erlbaum [Google Scholar]
- Marsh HW, Hau K-T, & Wen Z (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Structural equation modeling, 11(3), 320–341. [Google Scholar]
- Mattick RP, & Clarke JC (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy, 36(4), 455–470. [DOI] [PubMed] [Google Scholar]
- McLelland GH & Judd CM (1993). Statistical difficulties of detecting interactinos and moderator effects. Psychological Bulletin, 114, 376–390. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy, 28(6), 487–495. [DOI] [PubMed] [Google Scholar]
- Mineka S, & Zinbarg R (2006). A contemporary learning theory perspective on the etiology of anxiety disorders: it's not what you thought it was. American Psychologist, 61(1), 10–26. [DOI] [PubMed] [Google Scholar]
- Mineka S, Williams AL, Wolitzky-Taylor K, Vrshek-Schallhorn S, Craske MG, Hammen C, & Zinbarg RE (2020). Five-year prospective neuroticism–stress effects on major depressive episodes: Primarily additive effects of the general neuroticism factor and stress. Journal of abnormal psychology, 129(6), 646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor N, Zinbarg R, Craske M, Mineka S, Griffith J, Uliaszek A, Rose R & Waters A (2008). Factor structure and factorial invariance of the EPQ-R Neuroticism Scale in high school juniors. Journal of Personality Assessment, 90, 66–75. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2015). Mplus User’s Guide. (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Naragon-Gainey K, Prenoveau JM, Brown TA, & Zinbarg RE (2016). A comparison and integration of structural models of depression and anxiety in a clinical sample: Support for and validation of the tri-level model. Journal of Abnormal Psychology, 125(7), 853–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nocentini A, Palladino BE, & Menesini E (2021). Adolescents’ stress reactions in response to COVID-19 pandemic at the peak of the outbreak in Italy. Clinical Psychological Science, 9(3), 507–514. [Google Scholar]
- Prenoveau JM, Zinbarg RE, Craske MG, Mineka S, Griffith JW, & Epstein AM (2010). Testing a hierarchical model of anxiety and depression in adolescents: A tri-level model. Journal of Anxiety Disorders, 24(3), 334–344. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Craske MG, & Barlow DH (1994). Assessment instrument for panic disorder that includes fear of sensation-producing activities: The Albany Panic and Phobia Questionnaire. Anxiety, 1(3), 114–122. [DOI] [PubMed] [Google Scholar]
- Rizvi SJ, Pizzagalli DA, Sproule BA, & Kennedy SH (2016). Assessing anhedonia in depression: Potentials and pitfalls. Neuroscience and Biobehavioral Reviews, 65, 21–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodebaugh TL, Woods CM, Thissen D, Heimberg RG, Chambless DL, & Rapee RM (2004). More information from fewer questions: The factor structure and item properties of the original and brief fear of negative evaluation scales. Psychological Assessment, 16, 169–181. [DOI] [PubMed] [Google Scholar]
- Shackman AJ, Stockbridge MD, Tillman RM, Kaplan CM, Tromp DP, Fox AS, & Gamer M (2016). The neurobiology of dispositional negativity and attentional biases to threat: Implications for understanding anxiety disorders in adults and youth. Journal of experimental psychopathology, 7(3), 311–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1984). Negative affectivity: the disposition to experience aversive emotional states. Psychological Bulletin, 96(3), 465–490. [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, & McCormick RA (1995). Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology, 104(1), 3–14. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2021). COVID-19 weekly epidemiological update, edition 58, 21 September 2021. https://covid19.who.int/ [Google Scholar]
- Zimmerman M, & Coryell W (1987). The Inventory to Diagnose Depression (IDD): a self-report scale to diagnose major depressive disorder. Journal of Consulting and Clinical Psychology, 55(1), 55–59. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, & Barlow DH (1996). Structure of anxiety and the anxiety disorders: a hierarchical model. Journal of Abnormal Psychology, 105(2), 181–193. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Kramer A, Kelley N, Williams A, Schmidt M, Chat I, Young K, Nusslock R & Craske M (2022). Conceptual replication and multi-method extension of a tri-level model of anxiety and depression in a sample of young adults. Manuscript in preparation. [Google Scholar]
- Zinbarg R, Yovel I, Revelle W & McDonald R (2006). Estimating generalizability to a universe of indicators that all have an attribute in common: A comparison of estimators for ωh. Applied Psychological Measurement, 30, 121–144. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.