Abstract
Objective.
Since the start of the coronavirus pandemic, some US adults have increased alcohol and cannabis use frequency to cope with distress. Among sexual minoritized young adults (SM YAs), coping-related use may be greater due to disproportionate negative social and financial consequences of the pandemic. Nonetheless, it remains unclear whether pandemic substance use has increased among SM YAs compared to non-SM YAs relative to pre-pandemic levels, and whether heightened coping motives mediate these potential differences.
Method.
A total of 563 YAs (18–24 years at baseline; 31.0% SM) provided survey data collected across twelve bi-monthly assessments. Six assessments were measured in 2015 or 2016 and six across the coronavirus pandemic (2020–2021). Controlling for pre-pandemic assessments matched by calendar month, latent structural equation models examined group differences in alcohol and cannabis frequency and consequences across the COVID period and tested coping motives as mediators of these differences.
Results.
Substance use and consequences were similar during the pandemic relative to pre-pandemic levels across groups. Nonetheless, compared to non-SM individuals, SM participants reported greater cannabis frequency, consequences, and cannabis coping motives during the pandemic independent of pre-pandemic levels. Cannabis use and consequences were each explained largely by coping motives during the pandemic among SM compared to non-SM YAs. These patterns were not found for alcohol outcomes.
Conclusions.
The COVID pandemic has widened cannabis disparities between SM and non-SM YAs, due in part to pandemic-related increases in coping motives. Responsive public policy is needed that may prevent and remit SM cannabis disparities during societal crises.
Keywords: COVID-19, Sexual and gender minority, substance use, cannabis use
The coronavirus (COVID-19) outbreak has resulted in substantial changes in adult substance use behaviors in the United States since being declared a pandemic in March 2020. Although there is significant heterogeneity in substance use change resulting from the pandemic, studies have shown that up to 75% of adults reported increasing their alcohol use by at least one day per month (Pollard et al., 2020) and over 33% reported increases in cannabis use (Knell et al., 2020). Among young adult (YA) populations (ages 18–26 years), the pandemic has led to substantial disruptions to academic, social, and financial well-being (O’Reilly et al., 2021) during a crucial developmental period in the emergence and escalation of problem substance use behaviors (Arnett, 2005). These disruptions coincided with marked changes in alcohol and cannabis use among YAs, with national samples suggesting decreases in alcohol use from 2019 to 2020 yet historic peaks in YA cannabis use (Schulenberg et al., 2021). Studies have further shown that depression and boredom coping motives for alcohol and cannabis use have increased among YAs during the pandemic compared to pre-pandemic levels (e.g., Graupensperger et al., 2021), with up to 33% reporting having started or increased substance use as a strategy to cope with coronavirus-related stressors (Czeisler et al., 2021; Sharma et al., 2020).
Sexual minoritized (SM; e.g., lesbian, gay, bisexual, queer, questioning) adults may be a YA population especially vulnerable to compromised health across the coronavirus pandemic, including substance misuse (Bochicchio et al., 2021; Kantamneni, 2020; Salerno, Devadas, et al., 2020). Prior to the onset of the pandemic, SM adults were between 2 and 4 times more likely to endorse lifetime alcohol dependence, between 2 and 5 times more likely to report cigarette use, and as high as 11 times more likely to report cannabis use relative to non-SM populations (Marshal et al., 2008; McCabe et al., 2005; Meyer, 2003). SM adults have been disproportionately affected by economic, social, and health consequences of the pandemic (Kamal et al., 2021), which may have downstream effects on maladaptive coping behaviors such as substance use (Hatzenbuehler, 2009) that have exacerbated these pre-existing substance use disparities. For instance, national polls have shown that two-thirds of SM households reported serious financial problems from the pandemic, nearly half reported difficulties coping with social isolation, and over a third reported clinically significant increases in depressive and/or anxiety symptoms (Movement Advancement Project, 2020). Compared to heterosexual populations, SM groups have reported greater stress and mental health concerns associated with the pandemic, with nearly half (44%) reporting difficulties coping with social isolation versus 23% in non-SM adults (Movement Advancement Project, 2020) and over a third (38%) reporting clinically significant increases in depressive and/or anxiety symptoms versus 14% in non-SM populations (Moore et al., 2021). Among YAs specifically, social distancing mandates have reduced access to supportive and affirming resources known to mitigate mental health and substance use risk, such as community spaces and public venues affirming of SM identity (Drabble & Eliason, 2021; Grant et al., 2021). During the pandemic, many SM YAs also reported financial strain and/or experience university closures that prompted many to return home, often into isolating and unsupportive family environments (Fish et al., 2020; Gonzales et al., 2020). Consistent with minority stress theory (Meyer, 2003), these disparities are attributed to structural heterosexism and discrimination that has exacerbated the health burden in SM populations resulting from the pandemic (Kline, 2020). The cumulative effects of these pandemic stressors (i.e., greater social and financial strains) may in turn tax coping demands for managing pandemic-related stressors, and increase risk for maladaptive health risk behaviors among SM YAs such as substance use and misuse (Hatzenbuehler, 2009).
Studies to-date have suggested SM adults show greater perceived increases in coping demands and substance use during the pandemic (Moore et al., 2021). Surveys of Canadian adults have also shown that a greater proportion of SM adults reported substance use impacts of the coronavirus pandemic relative to non-SM adults (Goodyear et al., 2021), and that nearly one in four SM participants reported subjective increases in alcohol use since the pandemic and nearly one in five reported increases in cannabis use (Slemon et al., 2022). Addressing coping-related substance use specifically, SM adults in the US have also reported subjective increases in alcohol and cannabis use, consequences, and substance coping motives during the pandemic relative to pre-pandemic levels (Dyar, Morgan, et al., 2021), and qualitative work has suggested concerns about risk of heavier alcohol and cannabis use during the coronavirus pandemic is a common theme among SM communities (Bochicchio et al., 2021).
Despite these emerging findings, several gaps remain in understanding pandemic-related risk of substance use among SM YAs. First, to our knowledge, only one study to-date has directly compared substance use rates between SM and non-SM YAs (Goodyear et al., 2021), and most have focused solely on risk among SM women (e.g., Dyar, Morgan, et al., 2021). This has precluded assessment of whether substance use behaviors are disproportionately affected by the pandemic in the SM community relative to a non-SM comparison group and whether differences generalize in more sex-diverse samples. Second, while coping motives and substance behaviors may be elevated among SM YAs across the pandemic, none have tested coping as a mediator explaining elevations in use. A lack of focus on mechanisms has limited understanding of targets for prevention and intervention of substance misuse that may aid in remitting these disparities during future global health crises (Holmes et al., 2020). Finally, several studies have used retrospective reports of changes in substance behaviors since the start of the pandemic (Dyar, Morgan, et al., 2021; Goodyear et al., 2021; Slemon et al., 2022), which may be prone to recall bias (Van den Bergh & Walentynowicz, 2016). Accurate assessment of change may be enhanced by longitudinal rather than retrospective comparison of substance use rates.
The purpose of this study was to assess the relation between SM status and alcohol and cannabis use behaviors across the chronic phase of the first year of the COVID-19 pandemic, independent of pre-pandemic patterns of use. Noting these associations may be driven by stress-related coping motives resulting from the pandemic (e.g., Dyar, Morgan, et al., 2021; Graupensperger et al., 2021), we further examined the mediating role of coping motives during the pandemic in this relation. Addressing a recognized need to assess pandemic-related health behaviors longitudinally (Robinson et al., 2022), study aims were pursued using bi-monthly data collected in a longitudinal community sample of YAs with a relatively high representation of SM YAs (31.0%), measured both before and during the pandemic. Importantly, this design permitted estimation of pandemic-related coping and substance behaviors controlling for identical measures provided in pre-pandemic periods. Given accumulating evidence that the pandemic has worsened pre-existing health disparities among SM adults, we hypothesized that coping motives and enacted substance behaviors (i.e., alcohol and cannabis use and consequences) would be higher among SM compared to non-SM YAs during the coronavirus pandemic period independent of pre-pandemic levels. We expected further that pandemic coping motives would in turn explain later substance use and consequences during the pandemic among SM YAs. Given increasing evidence that disparities between SM and non-SM populations are greatest for cannabis use (compared to alcohol and cigarette use; McCabe et al., 2021; Meyer, 2003), we anticipated that effects would be strongest for cannabis-related outcomes.
Methods
Participants
Participants for this study were YAs from Project Transitions, a longitudinal community study of the impact of social role transitions in young adulthood on alcohol use (Patrick et al., 2018). Inclusion criteria were study recruitment age between 18 and 23, drinking one alcoholic beverage or more in the past year, and living within 60 miles of the study office in Seattle, WA (Lee, Cadigan, & Patrick, 2017). A total of 779 young adults were enrolled in the original project between February 2015 and January 2016 and asked to complete ongoing monthly surveys for up to 24 months of data collection. A follow-up project was then conducted to examine the health and well-being of these participants during the pandemic, in which participants were invited to complete six bi-monthly assessments. Participants were reconsented and randomly assigned to a starting month of September or October of 2020 and completed bi-monthly assessments thereafter through July or August of 2021. To address hypotheses of the present study, bi-monthly pandemic data were then combined with identical assessments matched by calendar month that were collected in the pre-pandemic period, totaling 12 bi-monthly assessments. Most participants from the larger study (n=563, 72.3%) provided at least one timepoint of data collection for these surveys conducted during the pandemic and were included in the current study. Missing data ranged from 3.5% to 19.1% across pandemic assessments and from 2.3% to 8.8% across the pre-pandemic assessments. The majority (63.7%) of the sample provided data at all 12 survey timepoints, and 90.8% of the analyzed sample responded to at least 8 out of 12 surveys. To assess whether non-participation in the pandemic supplement was associated with systematic missingness across study variables, we preformed independent samples tests (t-tests for continuous measures and Wilcoxon Rank Sum tests for polytomous measures) on all demographic and pre-pandemic study measures and compared responses on these measures between the parent sample and the subsample used in the current study. Results indicated that although alcohol coping motives were lower in the present sample compared to the parent sample (; d = 0.30, p < 0.001), no statistically significant differences were found for marijuana coping motives (d = 0.02, p = 0.72), for demographic variables (SGM status: d = 0.07, p = 0.024; race: d = 0.01, p = 0.87, ethnicity; d = 0.02; p = 0.71), or across monthly measures of substance use at each month (heavy episodic drinking: ds = 0.01 – 0.05; alcohol use: ds = 0.03 – 0.07; marijuana use: ds = 0.01 – 0.03; all ps > 0.05). This suggested little evidence of systematic missingness in study variables among pandemic survey respondents.
In this study sample, 58.7% identified as White/Caucasian, 18.4% as Asian/Asian American, and 22.9% as another or mixed race. Further, 8.1% of the sample identified their ethnicity as Hispanic/Latino(a). By Spring of 2021, 67.7% had obtained at least a bachelor’s degree, and 14.1% reported being enrolled in university. All procedures were reviewed and approved by the Institutional Review Board. All participants received comprehensive information statements outlining study procedures and elements of informed consent for both the parent and follow-up study.
Measures
SM status.
Endorsement of sexual minoritized status was measured using a sexual orientation item assessed at COVID month 1 of data collection. A total of 15.3% (n=86) identified as bisexual, 5.2% (n=30) identified as gay or lesbian, and 10.3% (n=58) identified as queer, questioning, or other (e.g., pansexual, asexual, or demisexual). Given the small cell sizes available for specific SM identities, SM status was characterized as a binary variable indicating endorsement of non-heterosexual identity (n=174) in primary analyses, which comprised nearly a third (31.0%) of the sample.
Substance use.
Monthly substance use outcomes included past month frequency and consequences of cannabis and alcohol use. We selected frequency of cannabis and alcohol use as our measure of use given recent work suggesting drinking quantity has changed little since the pandemic in YAs (Dumas et al., 2020; Graupensperger et al., 2021). Cannabis use was measured using the prompt “On how many occasions (if any) have you used marijuana (weed, pot) or hashish (hash, hash oil) during the past 30 days?” and ordinal response options ranged from 0 (“0 occasions”) to 6 (“40 or more [occasions]”). Past month alcohol use was measured using the prompt “How many days of the week did you drink alcohol during the past month?” with ordinal response options ranging from 0 (“I did not drink at all”) to 9 (“6 days a week or every day”).
Consequences of cannabis use were measured using the Marijuana Consequences Checklist (Lee et al., 2019), a 26-item questionnaire measuring whether given cannabis use consequences were experienced within the past month. Sample consequences included having trouble sleeping, spending too much money on cannabis, having the “munchies,” or making decisions that one later regretted. Alcohol consequences were measured using the Brief Young Adult Alcohol Consequences Questionnaire (Kahler et al., 2005). This measure consisted of 24 items indicating whether a given consequence was experienced within the past month. Sample items included having a hangover the morning after drinking, engaging in impulsive behaviors that one regretted after, or finding difficulty in limiting how much one drinks. Responses for each measure were dichotomized to indicate whether at least one consequence was experienced within the past month.
Substance coping motives.
Cannabis coping motives in the past month were measured using the coping subscale of the Comprehensive Marijuana Motives Questionnaire (Lee et al., 2009). This subscale was measured as a mean of three Likert items indicating coping reasons for having used cannabis (i.e., “To forget your problems”, “Because you were depressed”, and “To escape from your life”). Alcohol coping motives were measured by computing a mean of the coping motives subscales (i.e., depression (9 items) and anxiety (4 items) subscales) of the Modified Drinking Motives Questionnaire-Revised (Cooper, 1994; Grant et al., 2007). Pre- and during-pandemic measures of coping motives were each defined as means of each subscale across the first five assessment points of each data collection period. Across timepoints, Cronbach’s alpha reliability ranged from 0.82 to 0.92 for drinking coping motives and from 0.62 to 0.80 for cannabis use motives, indicating at least adequate reliability of these measures across the study period.
Analytic Strategy
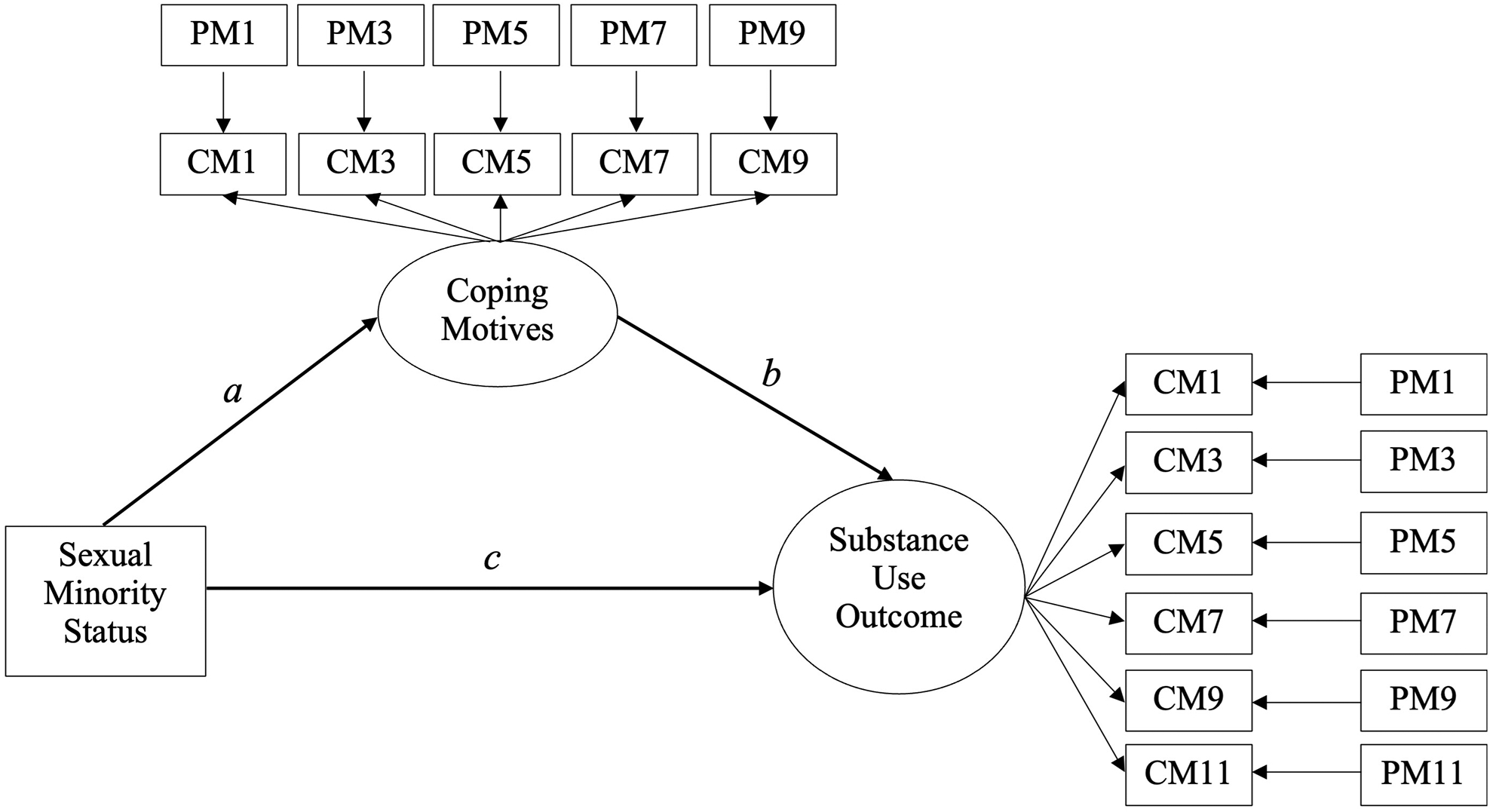
Primary hypotheses were addressed using latent structural equation models (SEMs) to estimate latent average levels in alcohol and cannabis use, consequences, and coping motives across the coronavirus pandemic period.1 Importantly, each monthly observation of pandemic measures were regressed on responses reported in the most recent same calendar month provided during the parent study, when data were collected prior to the onset of the pandemic (e.g., September 2020 substance use and motives were matched to September 2015 or 2016 responses, July 2021 substance use and motives were matched to July 2016 or 2017 responses, etc.). This allowed estimation of each participant’s coping motives and substance use controlling for their previous report at an identical period in a prior year. A total of 55.5% of participants provided responses beginning in 2016 and the remaining in 2015. SEMs were specified across two models. First, SEMs were specified without the inclusion of coping motives to establish the total effect of SM status on each use or consequence outcome. Coping motives were then included in a second model to estimate mediation of alcohol and cannabis outcomes via alcohol and cannabis coping motives, respectively (e.g., see schematic SEM provided in Figure 1).
We tested mediation via computation of indirect effects using the product of-the-coefficients approach, and standard errors were generated using bias-corrected bootstrapping (MacKinnon et al., 2002). All SEM analyses were conducted in MPlus version 8.6 (Muthen & Muthen, 2021) and descriptive statistics were generated in R (R Core Team, 2019). Models were estimated using ordinal specifications for cannabis and alcohol use frequencies. Binomial specifications were used for alcohol and cannabis use consequences to accommodate the dichotomous nature of these variables. Covariates across models included participant sex at birth, race (White vs. non-White), Hispanic ethnicity, age, college student status before and during the pandemic, and data collection year of pre-pandemic assessments (2015 vs. 2016). To emulate study inclusion criteria for alcohol use in the parent study, models for cannabis use and consequences outcomes were analyzed with only those reporting lifetime cannabis use by the first month of pandemic data collection (n=468, 33.6% SM).
Results
Descriptive statistics.
Table 1 provides means and standard deviations of study variables stratified by substance use and SM identity. Plots corresponding with these descriptions are provided in Supplemental Figures A and B. T-tests were used to examine mean differences in study outcomes across timepoints. Results showed that SM participants reported higher levels of cannabis use, consequences, and coping motives across most months prior to and during the pandemic, and no differences emerged between groups in alcohol measures. Evidence also suggested that the likelihood of alcohol consequences generally decreased during the pandemic, on average, by approximately 7% among SM YAs (p = 0.05) and approximately 10% among non-SM YAs (p = 0.001), though there was little evidence of change in cannabis consequences during the pandemic across groups.
Table 1.
Sample means/proportions of key study variables across sexual orientation groups.
| Alcohol Use (n = 563) | Cannabis Use (n = 468) | |||||
|---|---|---|---|---|---|---|
| Full Sample | SM | Non-SM | Full Sample | SM | Non-SM | |
| Past Month Frequency - COVID | ||||||
| September/October (Month 1) | 3.26 (2.43) | 3.08 (2.65) | 3.34 (2.32) | 1.42 (2.08) | 1.93 (2.34) | 1.15 (1.88) |
| November/December (Month 3) | 2.96 (2.36) | 3.04 (2.49) | 2.94 (2.29) | 1.31 (2.01) | 1.55 (2.14) | 1.19 (1.94) |
| January/February (Month 5) | 2.98 (2.45) | 3.05 (2.65) | 2.96 (2.36) | 1.25 (2.01) | 1.60 (2.20) | 1.05 (1.87) |
| March/April (Month 7) | 2.70 (2.43) | 2.76 (2.60) | 2.67 (2.35) | 1.15 (2.00) | 1.41 (2.13) | 1.01 (1.91) |
| May/June (Month 9) | 3.00 (2.43) | 2.99 (2.62) | 3.02 (2.33) | 1.18 (1.99) | 1.63 (2.24) | 0.93 (1.80) |
| July/August (Month 11) | 3.30 (2.41) | 3.41 (2.53) | 3.26 (2.36) | 1.16 (1.95) | 1.60 (2.17) | 0.92 (1.77) |
| COVID Mean Frequency: | 3.13 (2.20) | 3.13 (2.39) | 3.14 (2.11) | 1.36 (1.94) | 1.75 (2.09) | 1.15 (1.83) |
| Past Month Frequency - Pre-COVID | ||||||
| September/October (Month 1) | 2.94 (2.25) | 2.92 (2.28) | 2.96 (2.24) | 1.19 (1.98) | 1.44 (2.09) | 1.06 (1.92) |
| November/December (Month 3) | 2.95 (2.22) | 2.90 (2.22) | 2.96 (2.22) | 1.09 (1.92) | 1.41 (2.05) | 0.91 (1.81) |
| January/February (Month 5) | 3.08 (2.12) | 3.00 (2.14) | 3.13 (2.11) | 1.23 (1.92) | 1.54 (2.05) | 1.06 (1.82) |
| March/April (Month 7) | 2.78 (2.20) | 2.69 (2.15) | 2.83 (2.22) | 1.21 (1.95) | 1.42 (2.05) | 1.09 (1.89) |
| May/June (Month 9) | 2.81 (2.23) | 2.62 (2.30) | 2.88 (2.20) | 1.26 (1.96) | 1.56 (2.07) | 1.09 (1.88) |
| July/August (Month 11) | 2.99 (2.26) | 3.05 (2.39) | 2.97 (2.20) | 1.13 (1.91) | 1.45 (2.10) | 0.95 (1.78) |
| Pre-COVID Mean Frequency: | 2.96 (1.90) | 2.89 (1.90) | 3.00 (1.90) | 1.23 (1.83) | 1.48 (1.90) | 1.08 (1.77) |
| Past Month Consequences - COVID | ||||||
| September/October (Month 1) | 0.40 (0.49) | 0.36 (0.48) | 0.42 (0.49) | 0.39 (0.49) | 0.45 (0.50) | 0.35 (0.48) |
| November/December (Month 3) | 0.34 (0.48) | 0.34 (0.48) | 0.35 (0.48) | 0.34 (0.48) | 0.39 (0.49) | 0.31 (0.47) |
| January/February (Month 5) | 0.35 (0.48) | 0.36 (0.48) | 0.35 (0.48) | 0.32 (0.47) | 0.34 (0.48) | 0.31 (0.46) |
| March/April (Month 7) | 0.32 (0.47) | 0.29 (0.46) | 0.34 (0.47) | 0.27 (0.45) | 0.34 (0.48) | 0.23 (0.42) |
| May/June (Month 9) | 0.37 (0.48) | 0.33 (0.47) | 0.38 (0.49) | 0.31 (0.46) | 0.39 (0.49) | 0.26 (0.44) |
| July/August (Month 11) | 0.40 (0.49) | 0.40 (0.49) | 0.40 (0.49) | 0.31 (0.46) | 0.38 (0.49) | 0.28 (0.45) |
| COVID Mean Consequences: | 0.37 (0.39) | 0.36 (0.38) | 0.38 (0.39) | 0.35 (0.41) | 0.41 (0.42) | 0.32 (0.40) |
| Past Month Consequences - Pre-COVID | ||||||
| September/October (Month 1) | 0.44 (0.50) | 0.43 (0.50) | 0.44 (0.50) | 0.30 (0.46) | 0.40 (0.49) | 0.25 (0.43) |
| November/December (Month 3) | 0.53 (0.50) | 0.55 (0.50) | 0.51 (0.50) | 0.31 (0.46) | 0.39 (0.49) | 0.27 (0.45) |
| January/February (Month 5) | 0.47 (0.50) | 0.40 (0.49) | 0.51 (0.50) | 0.39 (0.49) | 0.48 (0.50) | 0.35 (0.48) |
| March/April (Month 7) | 0.44 (0.50) | 0.41 (0.49) | 0.45 (0.50) | 0.34 (0.47) | 0.38 (0.49) | 0.32 (0.47) |
| May/June (Month 9) | 0.43 (0.50) | 0.41 (0.49) | 0.43 (0.50) | 0.38 (0.49) | 0.43 (0.50) | 0.36 (0.48) |
| July/August (Month 11) | 0.44 (0.50) | 0.46 (0.50) | 0.44 (0.50) | 0.32 (0.47) | 0.41 (0.49) | 0.28 (0.45) |
| Pre-COVID Mean Consequences: | 0.46 (0.38) | 0.44 (0.37) | 0.47 (0.38) | 0.35 (0.39) | 0.41 (0.41) | 0.31 (0.38) |
| Coping Motives – COVID | ||||||
| September/October (Month 1) | 1.71 (0.79) | 1.71 (0.87) | 1.71 (0.76) | 1.25 (0.65) | 1.41 (0.84) | 1.17 (0.52) |
| November/December (Month 3) | 1.53 (0.69) | 1.59 (0.78) | 1.50 (0.65) | 1.16 (0.53) | 1.26 (0.70) | 1.11 (0.41) |
| January/February (Month 5) | 1.49 (0.69) | 1.57 (0.80) | 1.46 (0.64) | 1.18 (0.62) | 1.34 (0.82) | 1.11 (0.47) |
| March/April (Month 7) | 1.45 (0.70) | 1.47 (0.69) | 1.44 (0.71) | 1.14 (0.46) | 1.19 (0.52) | 1.11 (0.43) |
| May/June (Month 9) | 1.44 (0.64) | 1.50 (0.74) | 1.41 (0.59) | 1.11 (0.43) | 1.22 (0.56) | 1.06 (0.33) |
| COVID Mean Coping Motives: | 1.52 (0.56) | 1.57 (0.62) | 1.51 (0.54) | 1.17 (0.42) | 1.28 (0.55) | 1.11 (0.33) |
| Coping Motives – Pre-COVID | ||||||
| September/October (Month 1) | 1.54 (0.70) | 1.52 (0.73) | 1.55 (0.69) | 1.15 (0.56) | 1.18 (0.60) | 1.13 (0.54) |
| November/December (Month 3) | 1.56 (0.73) | 1.54 (0.74) | 1.57 (0.72) | 1.14 (0.74) | 1.17 (0.58) | 1.12 (0.81) |
| January/February (Month 5) | 1.58 (0.74) | 1.60 (0.78) | 1.58 (0.72) | 1.18 (0.80) | 1.22 (0.87) | 1.16 (0.76) |
| March/April (Month 7) | 1.54 (0.73) | 1.56 (0.72) | 1.54 (0.74) | 1.18 (0.84) | 1.26 (0.96) | 1.14 (0.74) |
| May/June (Month 9) | 1.52 (0.75) | 1.51 (0.76) | 1.51 (0.75) | 1.12 (0.78) | 1.16 (1.08) | 1.09 (0.57) |
| Pre-COVID Mean Coping Motives: | 1.55 (0.58) | 1.55 (0.59) | 1.55 (0.58) | 1.15 (0.41) | 1.20 (0.50) | 1.13 (0.36) |
Note. SM = Sexual minority. Bolded values indicate significant mean differences between SM and non-SM groups at α = 0.05. Cannabis frequency response options ranged from 0 (“0 occasions”) to 6 (“40 or more [occasions]”) and alcohol frequency responses ranged from 0 (“I did not drink at all”) to 9 (“6 days a week or every day”).
SEM Results.
Models were first estimated to describe the total effect of SM status on substance use outcomes during the pandemic (i.e., without the inclusion of coping motives as a mediator), controlling for pre-pandemic levels. Above and beyond levels reported in a pre-pandemic year, SM compared to non-SM participants reported greater cannabis use (b = 0.80, p = 0.035, 95% CI = [0.05, 1.55], β = 0.13) and SM status was marginally associated with greater cannabis consequences (b = 0.58, p = 0.07, 95% CI = [−0.04, 1.20], β = 0.14). There were no significant differences between SM and non-SM YAs in alcohol use frequency (b = −0.14, p = 0.67, 95% CI = [−0.68, 0.45], β = −0.02) or consequences (b = −0.11, p = 0.69, 95% CI = [0.−0.04, 1.20], β = −0.02).
When including coping motives as a mediator, cannabis coping motives mediated associations between SM status and cannabis frequency and consequences during the pandemic (see Tables 2 and 3). Specifically, compared to non-SM individuals, SM participants reported greater cannabis coping motives during COVID (cannabis use frequency model: b = 0.21, p < 0.001, 95% CI = [0.10, 0.33], β = 0.21; cannabis consequences model: b = 0.17, p < 0.01, 95% CI = [0.05, 0.30], β = 0.18) controlling for their pre-COVID levels. Beyond these direct effects, significant indirect pathways indicated that the effect of SM status conferred an additional 0.65 unit increase in past month cannabis frequency (p = 0.002, 95% CI = [0.31, 1.16], β = 0.11) and an additional 0.42 increase in past month consequences (p = 0.02, 95% CI = [0.08, 0.75], β = 0.10) through its impact on coping motives. This indirect pathway explained 67.1% of the relation between SM status and pandemic increases in cannabis frequency and 90.1% of this relation for cannabis consequences. Inclusion of these pathways reduced the direct effect of SM status on each to non-significance (cannabis frequency: b = 0.06, p = 0., 95% CI = [−0.59, 0.72], β = 0.01; cannabis consequences: b = 0.20, p = 0.46, 95% CI = [−0.34, 0.74], β = 0.05). Although coping motives for alcohol use were associated with greater change in alcohol frequency (b = 3.15, p < 0.001, 95% CI = [2.38, 3.92], β = 0.52) and consequences (b = 2.46, p < 0.001, 95% CI = [1.62, 3.30], β = 0.59), and SM status was marginally associated with greater alcohol coping motives during the pandemic (alcohol use model: b = 0.11, p = 0.06, 95% CI = [0.00, 0.22], β = 0.10; Alcohol consequences model: b = 0.11, p = 0.05, 95% CI = [0.00, 0.22], β = 0.10), no indirect effects were significant for alcohol outcomes (summary of alcohol models are provided in Supplemental Tables A and B).
Table 2.
Sexual Minority Status predicting pandemic-related change in Cannabis Use Frequency and Coping Motives.
| Effect | Estimate | SE | p | 95% CI | Std. |
|---|---|---|---|---|---|
| Lags (Pre-COVID vs. COVID) – Coping Motives | |||||
| Month 1 | 0.012 | 0.045 | 0.792 | [−0.077, 0.101] | 0.011 |
| Month 3 | 0.010 | 0.025 | 0.693 | [−0.040, 0.060] | 0.015 |
| Month 5 | 0.095 | 0.039 | 0.014 | [0.020, 0.171] | 0.099 |
| Month 7 | 0.032 | 0.024 | 0.177 | [−0.014, 0.078] | 0.058 |
| Month 9 | −0.018 | 0.028 | 0.517 | [−0.073, 0.036] | −0.031 |
| Lags (Pre-COVID vs. COVID) – Cannabis Use Frequency | |||||
| Month 1 | 0.435 | 0.084 | <0.001 | [0.269, 0.600] | 0.238 |
| Month 3 | 0.423 | 0.110 | <0.001 | [0.208, 0.638] | 0.167 |
| Month 5 | 0.482 | 0.137 | <0.001 | [0.214, 0.751] | 0.152 |
| Month 7 | 0.474 | 0.108 | <0.001 | [0.262, 0.687] | 0.202 |
| Month 9 | 0.183 | 0.104 | 0.080 | [−0.022, 0.388] | 0.087 |
| Month 11 | 0.356 | 0.094 | <0.001 | [0.171, 0.541] | 0.187 |
| Path Effects – COVID Cannabis coping motives | |||||
| SM Status (a) | 0.213 | 0.060 | <0.001 | [0.095, 0.330] | 0.210 |
| Female | −0.015 | 0.056 | 0.790 | [−0.125, 0.095] | −0.015 |
| Hispanic | 0.092 | 0.101 | 0.362 | [−0.106, 0.289] | 0.052 |
| White | 0.008 | 0.056 | 0.883 | [−0.102, 0.118] | 0.008 |
| Age | −0.009 | 0.016 | 0.564 | [−0.040, 0.022] | −0.035 |
| Pre-pandemic Year (2015 vs. 2016) | −0.030 | 0.056 | 0.590 | [−0.140, 0.080] | −0.031 |
| College Student Status (pre-COVID; 1 = yes) | −0.010 | 0.065 | 0.875 | [−0.138, 0.118] | −0.009 |
| College Student Status (During COVID; 1 = yes) | 0.038 | 0.060 | 0.531 | [−0.080, 0.156] | 0.040 |
| Path Effects – COVID Cannabis Use Frequency | |||||
| Cannabis Coping Motives (b) | 3.051 | 0.481 | <0.001 | [2.108, 3.994] | 0.504 |
| SM Status (c) | 0.065 | 0.336 | 0.846 | [−0.594, 0.724] | 0.011 |
| Female | −0.154 | 0.318 | 0.627 | [−0.778, 0.469] | −0.026 |
| Hispanic | 0.434 | 0.550 | 0.429 | [−0.643, 1.512] | 0.041 |
| White | 0.337 | 0.321 | 0.295 | [−0.293, 0.966] | 0.057 |
| Age | −0.158 | 0.067 | 0.018 | [−0.288, −0.027] | −0.099 |
| Pre-pandemic Year (2015 vs. 2016) | −0.006 | 0.305 | 0.984 | [−0.603, 0.591] | −0.001 |
| College Student Status (pre-COVID; 1 = yes) | 1.018 | 0.391 | 0.009 | [0.251, 1.785] | 0.148 |
| College Student Status (During COVID; 1 = yes) | 0.332 | 0.338 | 0.326 | [−0.331, 0.995] | 0.058 |
| Indirect Effect | |||||
| SM Status → Coping Motives → CF Month 11 (a*b) | 0.736 | 0.219 | 0.001 | [0.307, 1.164] | 0.068 |
Note: SE = Standard error, CI = Confidence interval, Std.=Standardized, CF = Cannabis use frequency. Intercepts and residual (co)variance estimates are omitted for parsimony. Boldface type indicates significant effects at the 95% level of confidence.
Table 3.
Sexual Minority Status predicting pandemic-related change in Cannabis Consequences and Coping Motives.
| Effect | Estimate | SE | p | 95% CI | Std. |
|---|---|---|---|---|---|
| Lags (Pre-COVID vs. COVID) – Coping Motives | |||||
| Month 1 | 0.037 | 0.054 | 0.492 | [−0.069, 0.144] | 0.032 |
| Month 3 | 0.022 | 0.025 | 0.383 | [−0.027, 0.071] | 0.036 |
| Month 5 | 0.065 | 0.042 | 0.122 | [−0.018, 0.148] | 0.068 |
| Month 7 | 0.026 | 0.029 | 0.367 | [−0.030, 0.082] | 0.045 |
| Month 9 | −0.008 | 0.023 | 0.727 | [−0.054, 0.037] | −0.019 |
| Lags (Pre-COVID vs. COVID) – Cannabis Consequences | |||||
| Month 1 | 1.202 | 0.394 | 0.002 | [0.430, 1.974] | 0.196 |
| Month 3 | 1.529 | 0.513 | 0.003 | [0.523, 2.535] | 0.184 |
| Month 5 | 1.597 | 1.512 | 0.291 | [−1.367, 4.561] | 0.065 |
| Month 7 | 1.045 | 0.574 | 0.069 | [−0.081, 2.171] | 0.114 |
| Month 9 | 0.702 | 0.476 | 0.140 | [−0.231, 1.634] | 0.099 |
| Month 11 | 1.226 | 0.435 | 0.005 | [0.372, 2.079] | 0.196 |
| Path Effects – COVID Cannabis Coping Motives | |||||
| SM Status (a) | 0.174 | 0.063 | 0.006 | [0.050, 0.298] | 0.179 |
| Female | 0.014 | 0.059 | 0.817 | [−0.103, 0.130] | 0.015 |
| Hispanic | 0.052 | 0.113 | 0.648 | [−0.170, 0.274] | 0.029 |
| White | 0.062 | 0.059 | 0.293 | [−0.053, 0.176] | 0.067 |
| Age | −0.014 | 0.016 | 0.380 | [−0.046, 0.018] | −0.058 |
| Pre-pandemic Year (2015 vs. 2016) | −0.027 | 0.059 | 0.645 | [−0.143, 0.088] | −0.029 |
| College Student Status (pre-COVID; 1 = yes) | 0.045 | 0.063 | 0.478 | [−0.079, 0.169] | 0.049 |
| College Student Status (During COVID; 1 = yes) | −0.051 | 0.068 | 0.455 | [−0.183, 0.082] | −0.047 |
| Path Effects – COVID Cannabis Consequences | |||||
| Cannabis Coping Motives (b) | 2.390 | 0.519 | <0.001 | [1.374, 3.407] | 0.538 |
| SM Status (c) | 0.202 | 0.274 | 0.461 | [−0.335, 0.739] | 0.047 |
| Female | −0.133 | 0.261 | 0.610 | [−0.644, 0.378] | −0.032 |
| Hispanic | 0.591 | 0.480 | 0.218 | [−0.350, 1.533] | 0.074 |
| White | 0.039 | 0.258 | 0.881 | [−0.467, 0.544] | 0.009 |
| Age | −0.097 | 0.052 | 0.059 | [−0.198, 0.004] | −0.088 |
| Pre-pandemic Year (2015 vs. 2016) | 0.075 | 0.25 | 0.763 | [−0.414, 0.565] | 0.018 |
| College Student Status (pre-COVID; 1 = yes) | 0.086 | 0.277 | 0.756 | [−0.458, 0.630] | 0.021 |
| College Student Status (During COVID; 1 = yes) | 0.929 | 0.335 | 0.006 | [0.273, 1.584] | 0.195 |
| Indirect Effect | |||||
| SM Status → Coping Motives → CF Month 11 (a*b) | 0.415 | 0.173 | 0.016 | [0.026, 0.167] | 0.096 |
Note: SE = Standard error, CI = Confidence interval, Std.=Standardized, CF = Cannabis use frequency. Intercepts and residual (co)variance estimates are omitted for parsimony. Boldface type indicates significant effects at the 95% level of confidence.
Discussion
The coronavirus pandemic has significantly impacted YA substance use, yet disproportionate exposure to pandemic-related stressors may have led to particularly heightened risk for SM YAs. The present study examined pandemic-related disparities in alcohol and cannabis use and consequences between SM and non-SM YAs and tested coping motives as mechanisms of these disparities. While prior work has suggested that coping motives for substance use have increased since the pandemic in YAs broadly (Czeisler et al., 2021; Sharma et al., 2020) and both use and coping motives have increased among certain SM adult populations specifically (Dyar, Morgan, et al., 2021; Goodyear et al., 2021; Slemon et al., 2022), studies have not established whether and through what mechanisms pandemic substance use may be more pronounced among SM YAs. Our results showed that, on average, substance use and consequences were similar during the pandemic relative to pre-pandemic levels, with some evidence that alcohol consequences decreased during the pandemic in SM and non-SM groups. Nonetheless, findings also indicated that cannabis frequency, consequences, and coping motives were each higher among SM participants compared to non-SM participants preceding the pandemic, and that SM participants also reported greater levels of each above and beyond their patterns observed in identical pre-pandemic months. Coping motives explained much of the direct relations between SM status and cannabis frequency and consequences, highlighting that depression and anxiety reduction motives for use may be central drivers exacerbating pandemic disparities in cannabis use and problems experienced by SM YAs.
To our knowledge, this research is the first to test coping motives as a mechanism of substance use and consequences in SM and non-SM populations while comparing prospectively assessed pre- and during-pandemic measures. Results were generally aligned with retrospective studies of SM adults suggesting correlations between coping motives and alcohol and cannabis use (Dyar, Morgan, et al., 2021; Goodyear et al., 2021; Slemon et al., 2022) and add that pandemic-related coping motives may serve a mechanistic role in driving pandemic cannabis disparities among SM compared to non-SM communities. These findings highlight the need for increasing access to more adaptive coping resources tailored to the needs of SM communities that may help reduce cannabis misuse and associated mental health concerns in the present and future societal crises (Peterson et al., 2020).
Prior work has shown that increasing access to supportive social networks (e.g., Rosario et al., 2004, 2011) or community resources supporting sexual and gender minority health (e.g., Heck et al., 2014) may reduce substance involvement among SM YAs. In the pandemic context, general population studies suggest a link between isolation and cannabis use (Bartel et al., 2020), and among SM populations, and that isolation and loneliness may be a particular burden for SM YAs (e.g., Salerno et al., 2020b, Fish et al., 2021). Taken together with the present findings, promoting prosocial connections during the pandemic among SM YAs may be especially crucial in mitigating coping-related cannabis risk. Given social distancing mandates and business closures observed throughout the pandemic, these interventions may be better accessed and utilized via electronic communication methods (Baumel et al., 2021) when in-person resources are unavailable. Understanding other specific pandemic-related stressors (e.g., poorer mental health, isolation, and discrimination experiences) driving coping motives among SM individuals could also help inform personalized intervention efforts. Aligned with calls to promote advocacy in pandemic SM mental health (Drabble & Eliason, 2021; Martino et al., 2021), tailored public messaging that addresses pandemic consequences on substance risk is also crucial in preventing and remitting substance disparities among SM communities.
Consistent with one prior study (Peterson et al., 2020), there was little evidence that pandemic change in alcohol use or consequences differed between SM and non-SM YA groups. Although somewhat surprising, this may have been driven by several factors. First, there was little overall change in alcohol use and consequences in the sample from pre- to during-pandemic periods across sexual orientation groups, suggesting there was relatively little variance in alcohol-related outcomes across analyses. This has been attributed to contextual shifts relevant to specific alcohol compared to cannabis use that have constricted opportunities for use. For instance, findings from a large, nationally-representative sample of YAs suggested that alcohol use decreased from 2019 to 2020, which researchers hypothesized may have been due to decreased time spent socializing with peers, especially during national and local shutdown periods (Schulenberg et al., 2021). This is supported by prior work utilizing the present sample (Graupensperger et al., 2021) that demonstrated significant reductions in social drinking motives between January 2020 (pre-COVID) and April/May of 2020 (during COVID). By contrast, daily cannabis use increased to an all-time high among 19 to 30 year old adults (Schulenberg et al., 2021), and pandemic-related limitations to socialization has coincided with increases in solitary cannabis use both in the general adult population (e.g., Sznitman, 2022) and among SM populations (Dyar, Morgan, et al., 2021).
Second, cannabis use may be a preferred substance for coping with stressors associated with pandemic compared to alcohol use. For instance, one study using the Monitoring the Future data found that while 8.2% of young adults endorsed using alcohol to cope with the pandemic, this was nearly double (15.7%) for cannabis use, and that only cannabis use coping motives were associated with isolation experienced during the pandemic (Patrick et al., 2022). It is notable that certain SM groups were already engaging in higher rates of solitary cannabis use (Tucker et al., 2008) and cannabis coping motives (Walukevich-Dienst et al., 2021) compared to their non-SM peers before the pandemic. Certain SM groups also report higher rates of solitary cannabis use than solitary drinking (Dyar, Feinstein, et al., 2021). As such, SM individuals may have been especially vulnerable to increasing solitary cannabis use in response to pandemic-related social limitations and increased stressors. Taken together, our results may suggest that the coronavirus pandemic heightened YA cannabis use due to coping-related shifts in isolated use, although changed minimally for both SM and non-SM groups for alcohol due to relatively lesser coping-related motives for use as well as restrictions in social opportunities for drinking. We encourage that hypotheses addressing social isolation as a mechanism of SM YA cannabis use across the pandemic be tested directly in future work.
Limitations and Future Directions
There were several limitations in the current study. First, because of statistical power concerns, we did not test differences between subgroups of SM populations, such as comparing effect size estimates between lesbian/gay and bisexual YAs or across racial/ethnic groups. We acknowledge, however, that significant heterogeneity in substance use risk exists across SM subgroups that may confer differential pandemic use patterns. For instance, substance use and misuse may be greater among bisexual compared to lesbian/gay populations (Green & Feinstein, 2012), with some evidence demonstrating greatest risk among bisexual YA women (Schuler et al., 2018, 2019; Vrangalova & Savin-Williams, 2014). This has been attributed to minority stressors resulting from negative attitudes and stereotypes held uniquely about bisexuality (i.e., binegativity; Feinstein & Dyar, 2017; Katz-Wise & Hyde, 2012). Though substance use across the pandemic may be especially heightened among bisexual and/or SM women, this remains a crucial area of inquiry. Similarly, intersectional frameworks emphasize that interlocking social positions are central drivers of heterogeneity in mental health risk, particularly among marginalized populations (Bauer et al., 2021; Bowleg, 2008; Crenshaw, 1991). Given this framework, we acknowledge that our findings may vary across intersectional groups. It is notable that the social and economic consequences of the pandemic may have been greatest among SM groups holding multiple disadvantaged social positions, with (for instance) up to 95% of Black and 70% of Latinx SM households reporting serious financial problems from the pandemic (Movement Advancement Project, 2020). Race and ethnicity may therefore be critical social positions that moderate risk among SM communities for pandemic substance and mental health concerns. Second, and relatedly, the current sample was predominantly White, non-Hispanic, and lived in a state with legalized cannabis use for adults. Thus, findings may not be fully representative of the general YA population. Replicating the current study in more diverse and nationally representative samples will help ensure that findings are generalizable across a more diverse range of communities.
Finally, we acknowledge that assessment of substance use during the pandemic while controlling for pre-pandemic levels may not have been sufficient to describe nuanced patterns of change across the pandemic period, and that data were assessed across the more chronic phase of the pandemic (Fall 2020 through Spring of 2021) rather than during the more acute phase (Spring 2020). For instance, one study (Goodyear et al., 2021) provided descriptive evidence that alcohol and cannabis use among SM individuals tended to peak between Spring and Fall 2020 followed by decreases between Fall 2020 and Winter 2021. Future work is encouraged to utilize more flexible modeling approaches for assessing change over time, such as exploratory latent growth modeling (Grimm et al., 2013) or nonlinear longitudinal recursive partitioning (Stegmann et al., 2018). This may be particularly relevant in studies involving more intensive (e.g., weekly or monthly) repeated measures design across the pandemic.
Conclusions
This study was designed to assess substance disparities between SM and non-SM YAs during the coronavirus pandemic and identify a potential target for reducing these disparities via relative change in coping motives. We consider this work a single step toward an understanding of substance disparities among SM populations that arise from stressors associated with global health and other societal crises. For instance, addressing the direct impacts of financial and social strains experienced among SM communities on substance use remains a critical area of inquiry, which may have given rise to coping-related motives and subsequent increases in use. Further, this work may stimulate study of additional mechanisms and moderators driving pandemic substance disparities, including shifts in social norms around substance use and extensions of findings to other at-risk age groups (e.g., SM adolescents; Dumas et al., 2020). Finally, we note that health consequences associated with the pandemic may extend well beyond its course, particularly among non-majority communities (Galea et al., 2020; Jager & Keyes, 2021; Kathirvel, 2020). Thus, future work will be needed to continue addressing pandemic-related factors associated with both persistence in and recovery from the health compromises experienced by marginalized groups during this global health crisis.
Supplementary Material
Public Health Significance Statement.
This study indicates that the coronavirus pandemic has widened pre-existing gaps in coping motives for cannabis use and cannabis use frequency among sexual minoritized compared to sexual non-minoritized young adults. This study also shows that cannabis use is largely explained by heighted coping motives for use during the pandemic, independent of pre-pandemic levels of use and motives, highlighting need for responsive intervention and policy aimed at reducing impacts of societal crises on substance use among sexual minoritized communities.
Acknowledgements:
We are grateful to all participants who took part in this study and to the Project Transitions study team.
Primary funding:
Data collection and manuscript preparation was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (R01AA022087, PI: C. M. Lee and R01AA027496, PI: C. M. Lee). Manuscript preparation was also supported by NIAAA (T32 AA007455; PI: Larimer; K99AA030052; PI: McCabe). The content of this manuscript is solely the responsibility of the author(s) and does not necessarily represent the official views of the University of Washington, National Institute on Alcohol Abuse and Alcoholism and the National Institutes of Health.
Footnotes
Latent growth curve models (LGCMs) were initially estimated in this study to assess bi-monthly change in substance use outcomes across the pandemic period. However, because there was little evidence of average change-over-time in these measures (see, e.g., Supplemental Figure A) and SM status did not explain heterogeneity in change, a latent structural model was employed instead for parsimony. We note that conclusions using structural analysis versus LGCMs in predicting levels of use and consequences were largely identical across approaches.
Declaration of interests: none to declare.
References
- Arnett JJ (2005). The developmental context of substance use in emerging adulthood. Journal of Drug Issues, 35, 235–254. [Google Scholar]
- Bartel SJ, Sherry SB, & Stewart SH (2020). Self-isolation: A significant contributor to cannabis use during the COVID-19 pandemic. Substance Abuse, 41(4), 409–412. 10.1080/08897077.2020.1823550 [DOI] [PubMed] [Google Scholar]
- Bauer GR, Churchill SM, Mahendran M, Walwyn C, Lizotte D, & Villa-Rueda AA (2021). Intersectionality in quantitative research: A systematic review of its emergence and applications of theory and methods. SSM - Population Health, 14(February), 100798. 10.1016/j.ssmph.2021.100798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumel K, Hamlett M, Wheeler B, Hall D, Randall AK, & Mickelson K (2021). Living Through COVID-19: Social Distancing, Computer-Mediated Communication, and Well-Being in Sexual Minority and Heterosexual Adults. Journal of Homosexuality, 68(4), 673–691. 10.1080/00918369.2020.1868190 [DOI] [PubMed] [Google Scholar]
- Bochicchio LA, Drabble LA, Riggle EDB, Munroe C, Wootton AR, & Hughes TL (2021). Understanding Alcohol and Marijuana Use among Sexual Minority Women during the COVID-19 Pandemic: A Descriptive Phenomenological Study. Journal of Homosexuality, 68(4), 631–646. 10.1080/00918369.2020.1868187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2008). When Black + lesbian + woman ≠ Black lesbian woman: The methodological challenges of qualitative and quantitative intersectionality research. Sex Roles, 59(5–6), 312–325. 10.1007/s11199-008-9400-z [DOI] [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6(2), 117–128. 10.1037/1040-3590.6.2.117 [DOI] [Google Scholar]
- Crenshaw K (1991). Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanford Law Review. 10.2307/1229039 [DOI] [Google Scholar]
- Czeisler M, Lane RI, Wiley JF, Czeisler CA, Howard ME, & Rajaratnam SMW (2021). Follow-up Survey of US Adult Reports of Mental Health, Substance Use, and Suicidal Ideation during the COVID-19 Pandemic, September 2020. JAMA Network Open, 4(2), 2–7. 10.1001/jamanetworkopen.2020.37665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drabble LA, & Eliason MJ (2021). Introduction to Special Issue: Impacts of the COVID-19 Pandemic on LGBTQ+ Health and Well-Being. Journal of Homosexuality, 68(4), 545–559. 10.1080/00918369.2020.1868182 [DOI] [PubMed] [Google Scholar]
- Dumas TM, Ellis W, & Litt DM (2020). What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. Journal of Adolescent Health, 67, 354–361. 10.1016/j.jadohealth.2020.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyar C, Feinstein BA, Crosby S, Newcomb ME, & Whitton SW (2021). Social Context of Cannabis Use: Associations With Problematic Use, Motives for Use, and Protective Behavioral Strategies Among Sexual and Gender Minorities Assigned Female at Birth. Annals of LGBTQ Public and Population Health, 2(4), 299–314. 10.1891/LGBTQ-2020-0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyar C, Morgan E, Kaysen D, Newcomb ME, & Mustanski B (2021). Risk factors for elevations in substance use and consequences during the COVID-19 pandemic among sexual and gender minorities assigned female at birth. Drug and Alcohol Dependence, 227(September), 109015. 10.1016/j.drugalcdep.2021.109015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein BA, & Dyar C (2017). Bisexuality, minority stress, and health. Current Sexual Health Reports, 9(1), 42–49. 10.1007/s11930-017-0096-3.Bisexuality [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, McInroy LB, Paceley MS, Williams ND, Henderson S, Levine DS, & Edsall RN (2020). “I’m Kinda Stuck at Home With Unsupportive Parents Right Now”: LGBTQ Youths’ Experiences With COVID-19 and the Importance of Online Support. Journal of Adolescent Health, 67(3), 450–452. 10.1016/j.jadohealth.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, Salerno J, Williams ND, Rinderknecht RG, Drotning KJ, Sayer L, & Doan L (2021). Sexual Minority Disparities in Health and Well-Being as a Consequence of the COVID-19 Pandemic Differ by Sexual Identity. LGBT Health, 8(4), 263–272. 10.1089/lgbt.2020.0489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Merchant RM, & Lurie N (2020). The Mental Health Consequences of COVID-19 and Physical Distancing. JAMA Internal Medicine, 180(6), 817. 10.1001/jamainternmed.2020.1562 [DOI] [PubMed] [Google Scholar]
- Gonzales G, Loret de Mola E, Gavulic KA, McKay T, & Purcell C (2020). Mental Health Needs Among Lesbian, Gay, Bisexual, and Transgender College Students During the COVID-19 Pandemic. Journal of Adolescent Health, 67(5), 645–648. 10.1016/j.jadohealth.2020.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodyear T, Slemon A, Richardson C, Gadermann A, Salway T, Dhari S, Knight R, & Jenkins E (2021). Increases in alcohol and cannabis use associated with deteriorating mental health among lgbtq2+ adults in the context of covid-19: A repeated cross-sectional study in canada, 2020–2021. International Journal of Environmental Research and Public Health, 18(22), 1–14. 10.3390/ijerph182212155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant R, Gorman-Murray A, & Briohny Walker B (2021). The Spatial Impacts of COVID-19 Restrictions on LGBTIQ Wellbeing, Visibility, and Belonging in Tasmania, Australia. Journal of Homosexuality, 68(4), 647–662. 10.1080/00918369.2020.1868188 [DOI] [PubMed] [Google Scholar]
- Grant VV, Stewart SH, Connor RMO, Blackwell E, & Conrod PJ (2007). Psychometric evaluation of the five-factor Modified Drinking Motives Questionnaire — Revised in undergraduates. Addictive Behaviors, 32, 2611–2632. 10.1016/j.addbeh.2007.07.004 [DOI] [PubMed] [Google Scholar]
- Graupensperger S, Fleming CB, Jaffe AE, Rhew IC, Patrick ME, & Lee CM (2021). Changes in young adults’ alcohol and marijuana use, norms, and motives from before to during the COVID-19 pandemic. Journal of Adolescent Health, Ahead of Print. 10.1016/j.jadohealth.2021.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green KE, & Feinstein BA (2012). Substance use in lesbian, gay, and bisexual populations: An update on empirical research and implications for treatment. In Psychology of Addictive Behaviors. 10.1037/a0025424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm KJ, Steele JS, Ram N, & Nesselroade JR (2013). Exploratory Latent Growth Models in the Structural Equation Modeling Framework. Structural Equation Modeling, 20(4), 568–591. 10.1080/10705511.2013.824775 [DOI] [Google Scholar]
- Hatzenbuehler ML (2009). How Does Sexual Minority Stigma “Get Under the Skin”? A Psychological Mediation Framework. Psychological Bulletin. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck NC, Livingston NA, Flentje A, Oost K, Stewart BT, & Cochran BN (2014). Reducing risk for illicit drug use and prescription drug misuse: High school gay-straight alliances and lesbian, gay, bisexual, and transgender youth. Addictive Behaviors, 39(4), 824–828. 10.1016/j.addbeh.2014.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, … Bullmore E (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 0366, 1–14. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager J, & Keyes KM (2021). Is substance use changing because of the COVID-19 pandemic? Conceptual and methodological considerations to delineating the impact of the COVID-19 pandemic on substance use and disorder. Addiction, 116(6), 1301–1303. 10.1111/add.15414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, & Read JP (2005). Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research, 29, 1180–1189. 10.1097/01.ALC.0000171940.95813.A5 [DOI] [PubMed] [Google Scholar]
- Kamal K, Li JJ, Hahm HC, & Liu CH (2021). Psychiatric impacts of the COVID-19 global pandemic on U.S. sexual and gender minority young adults. Psychiatry Research, 299(November 2020), 113855. 10.1016/j.psychres.2021.113855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantamneni N (2020). The impact of the COVID-19 pandemic on marginalized populations in the United States: A research agenda. Journal of Vocational Behavior, 119(January), 103439. 10.1016/j.jvb.2020.103439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kathirvel N (2020). Post COVID-19 pandemic mental health challenges. Asian Journal of Psychiatry, 53(January). 10.1016/j.ajp.2020.102430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline NS (2020). Rethinking COVID-19 Vulnerability: A Call for LGBTQ+ Im/migrant Health Equity in the United States During and After a Pandemic. Health Equity, 4(1), 239–242. 10.1089/heq.2020.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knell G, Robertson MC, Dooley EE, Burford K, & Mendez KS (2020). Health behavior changes during covid-19 pandemic and subsequent “stay-at-home” orders. International Journal of Environmental Research and Public Health, 17(17), 1–16. 10.3390/ijerph17176268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, & Grossbard J (2009). Development and preliminary validation of a comprehensive marijuana motives questionnaire. Journal of Studies on Alcohol and Drugs, 70, 279–287. https://doi.org/10.15288%2Fjsad.2009.70.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Cadigan JM, & Patrick ME (2017). Differences in reporting of perceived acute effects of alcohol use, marijuana use, and simultaneous alcohol and marijuana use. Drug and Alcohol Dependence, 180, 391–394. 10.1016/j.drugalcdep.2017.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 10.1037/1082-989X.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino RJ, Krause KD, Griffin M, LoSchiavo C, Comer-Carruthers C, Karr AG, Bullock AF, & Halkitis PN (2021). A Nationwide Survey of COVID-19 Testing in LGBTQ+ Populations in the United States. Public Health Reports, 136(4), 493–507. 10.1177/00333549211018190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. In Psychological Bulletin. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SE, Wierenga KL, Prince DM, Gillani B, & Mintz LJ (2021a). Disproportionate Impact of the COVID-19 Pandemic on Perceived Social Support, Mental Health and Somatic Symptoms in Sexual and Gender Minority Populations. Https://Doi.Org/10.1080/00918369.2020.1868184, 68(4), 577–591. 10.1080/00918369.2020.1868184 [DOI] [PubMed] [Google Scholar]
- Moore SE, Wierenga KL, Prince DM, Gillani B, & Mintz LJ (2021b). Disproportionate Impact of the COVID-19 Pandemic on Perceived Social Support, Mental Health and Somatic Symptoms in Sexual and Gender Minority Populations. Journal of Homosexuality, 68(4), 577–591. 10.1080/00918369.2020.1868184 [DOI] [PubMed] [Google Scholar]
- Movement Advancement Project. (2020). The Disproportionate Impacts of COVID-19 on LGBTQ Households in the U.S (Issue August). [Google Scholar]
- O’Reilly A, Tibbs M, Booth A, Doyle E, McKeague B, & Moore J (2021). A rapid review investigating the potential impact of a pandemic on the mental health of young people aged 12–25 years. Irish Journal of Psychological Medicine, 38(3), 192–207. 10.1017/ipm.2020.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Rhew IC, Lewis MA, Abdallah DA, Larimer ME, Schulenberg JE, & Lee CM (2018). Alcohol Motivations and Behaviors During Months Young Adults Experience Social Role Transitions: Microtransitions in Early Adulthood. Psychology of Addictive Behaviors, 32(8), 895–903. 10.1037/adb0000411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Parks MJ, Fairlie AM, Kreski NT, Keyes KM, & Miech R (2022). Using Substances to Cope With the COVID-19 Pandemic: U.S. National Data at Age 19 Years. Journal of Adolescent Health, 70(2), 340–344. 10.1016/j.jadohealth.2021.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson ZD, Vaughan EL, & Carver DN (2020). Sexual Identity and Psychological Reactions to COVID-19. Traumatology, 27(1), 6–13. 10.1037/trm0000283 [DOI] [Google Scholar]
- Pollard MS, Tucker JS, & Green HD (2020). Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Network Open, 3(9), e2022942. 10.1001/jamanetworkopen.2020.22942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2019). R: A language and environment for statistical computing. In R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Robinson E, Sutin AR, Daly M, & Jones A (2022). A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders, 296(January), 567–576. 10.1016/j.jad.2021.09.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, & Hunter J (2004). Predictors of substance use over time among gay, lesbian, and bisexual youths: an examination of three hypotheses. Addictive Behaviors, 29(8), 1623–1631. 10.1016/j.addbeh.2004.02.032 [DOI] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, & Hunter J (2011). Cigarette smoking as a coping strategy: negative implications for subsequent psychological distress among lesbian, gay, and bisexual youths. Journal of Pediatric Psychology, 36(7), 731–742. 10.1093/jpepsy/jsp141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP, Devadas J, Pease M, Nketia B, & Fish JN (2020). Sexual and Gender Minority Stress Amid the COVID-19 Pandemic: Implications for LGBTQ Young Persons’ Mental Health and Well-Being. Public Health Reports, 135(6), 721–727. 10.1177/0033354920954511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP, Pease M, Devadas J, Nketia B, & Fish JN (2020). COVID-19-Related Stress Among LGBTQ+ University Students: Results of a U.S. National Survey. University of Maryland Prevention Research Center, September. https://doi.org/ 10.13016/zug9-xtmi [DOI] [Google Scholar]
- Schulenberg JE, Patrick ME, Johnston LD, O’Malley PM, Bachman JG, & Miech RA (2021). Monitoring the Future National Survey Results on Drug Use, 1975–2020. Volume II, College Students & Adults Ages 19–60. Institute for Social Research. [Google Scholar]
- Schuler MS, Rice CE, Evans-Polce RJ, & Collins RL (2018). Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug and Alcohol Dependence, 189(1), 139–146. 10.1016/j.drugalcdep.2018.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Stein BD, & Collins RL (2019). Differences in substance use disparities across age groups in a national cross-sectional survey of Lesbian, Gay, and Bisexual Adults. LGBT Health, 6(2), 68–76. 10.1089/lgbt.2018.0125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma P, Ebbert JO, Rosedahl JK, & Philpot LM (2020). Changes in substance use among young adults during a respiratory disease pandemic. SAGE Open Medicine, 8, 205031212096532. 10.1177/2050312120965321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slemon A, Richardson C, Goodyear T, Salway T, Gadermann A, Oliffe JL, Knight R, Dhari S, & Jenkins EK (2022). Widening mental health and substance use inequities among sexual and gender minority populations: Findings from a repeated cross-sectional monitoring survey during the COVID-19 pandemic in Canada. Psychiatry Research, 307(November 2021), 114327. 10.1016/j.psychres.2021.114327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegmann G, Jacobucci R, Serang S, & Grimm KJ (2018). Recursive Partitioning with Nonlinear Models of Change. Multivariate Behavioral Research, 53(4), 559–570. 10.1080/00273171.2018.1461602 [DOI] [PubMed] [Google Scholar]
- Sznitman SR (2022). Changes in Cannabis Use Risk Behaviors During the First and Second COVID-19 Lockdown in Israel. Journal of Addiction Medicine, Publish Ah. 10.1097/ADM.0000000000000977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, & Klein DJ (2008). Understanding Differences in Substance Use Among Bisexual and Heterosexual Young Women. Women’s Health Issues, 18(5), 387–398. 10.1016/j.whi.2008.04.004 [DOI] [PubMed] [Google Scholar]
- Van den Bergh O, & Walentynowicz M (2016). Accuracy and bias in retrospective symptom reporting. Current Opinion in Psychiatry, 29(5), 302–308. 10.1097/YCO.0000000000000267 [DOI] [PubMed] [Google Scholar]
- Vrangalova Z, & Savin-Williams RC (2014). Psychological and physical health of mostly heterosexuals: A systematic review. In Journal of Sex Research. 10.1080/00224499.2014.883589 [DOI] [PubMed] [Google Scholar]
- Walukevich-Dienst K, Dylanne Twitty T, & Buckner JD (2019). Sexual minority women and Cannabis use: The serial impact of PTSD symptom severity and coping motives. Addictive Behaviors, 92, 1–5. 10.1016/j.addbeh.2018.12.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


