Abstract
Background:
Stigma surrounding opioid use disorder (OUD) is a barrier to treatment. Use of stigmatizing language may be evidence of negative views towards patients. We aimed to identify associations between language and clinical outcomes in patients admitted for infectious complications of OUD.
Methods:
We performed a retrospective medical record review at four health systems. Participants were patients with OUD admitted for infectious complications of injection opioid use from 1/1/2018–12/31/2018, identified through ICD10 codes consistent with OUD and acute bacterial/fungal infection. Discharge summaries were reviewed for language, specifically: abuse, addiction, dependence, misuse, use disorder, IVDU, and other. Binary outcomes including medication for opioid use disorder, planned discharge, naloxone provision, and an OUD treatment plan were evaluated using logistic regressions and admission duration was evaluated using Gamma regression.
Results:
A total of 1285 records were reviewed and 328 met inclusion criteria. Of those, 191 (58%) were male, with a median age of 38 years. The most common term was “abuse” (219, 67%), whereas “use disorder” was recorded in 75 (23%) records. Having “use disorder” in the discharge summary was associated with increased odds of having a documented plan for ongoing OUD treatment (AOR 4.11, 95% CI 1.89–8.93) and having a documented plan for addiction-specific follow up care (AOR 2.31, 95% CI 1.30–4.09).
Conclusions:
Stigmatizing language was common in this study of patients hospitalized for infectious complications of OUD. Best practice language was uncommon, but when used was associated with increased odds of addiction treatment and specialty care referral.
Keywords: Opioid use disorder, stigma, people who inject drugs, language, medical documentation, infections
BACKGROUND
Despite extensive efforts by healthcare providers and public health officials, recent data indicates that fewer than 20% of the approximately 2.7 million U.S. residents living with opioid use disorder (OUD) are actively engaged in treatment.1 In a 2019 report, the National Academy of Sciences identified stigma surrounding OUD as a key barrier to evidence-based treatment initiation and retention.2 Stigmatization of OUD comes in many forms. These may include public stigma characterizing the disorder as a moral failure, separating its treatment from usual medical care, or criminalizing substance use.3–6 Label avoidance, which discourages those with OUD from seeking treatment, may result from others using judgmental or pejorative language to describe individuals with OUD, or self-stigma when these attitudes are internalized.4, 7 In any form, stigma is associated with diminished treatment engagement and impaired health outcomes.5, 8
Stigma towards chronic disease is not a new problem, and has been the subject of research in mental health since the 1950s.8 While some headway has been made against stigma associated with mental health disorders and infectious diseases, namely HIV/AIDS, the same cannot be said for substance use disorders.4, 7, 9 A 2009 study of mental health care providers randomized respondents to view one of two versions of a patient vignette describing an individual with a substance use disorder. One version described the individual as a “substance abuser”, while the second referred to them as a person with a “substance use disorder”.10 Respondents who viewed the “substance abuser” vignette were more likely to view the patient as personally responsible for their condition, and also more likely to recommend punitive actions. In another large national online survey of members of the lay public, individuals described as “drug addict[s]” had higher ratings of negative affect and personal responsibility than those described as having OUD.11 Additionally, a recent cross-sectional study of more than 30,000 patients with substance-related diagnoses demonstrated that 18.4% of notes contained stigmatizing language, and 61.6% of patients had at least one note with stigmatizing language.12
Optimal language is a constantly moving target, but current best practices call for the use of person-centered language, for example using the term “person with opioid use disorder” rather than “opioid addict”.13 Under the title “Words Matter,” the National Institute on Drug Abuse (NIDA) has released specific guidelines concerning preferred language when discussing the evaluation and treatment of persons with a substance use disorder.14 Despite existing data and guidelines on the use of person-first language, use of potentially stigmatizing language by clinicians remains common. In a recent study, internal medicine residents were asked to attend a mutual support group meeting (e.g., Narcotics Anonymous) and write a brief reflection on their experience. In their reflection, residents commonly used guideline-discordant terms such as “alcoholism”, “addict”, and “clean”.15 Much of the existing literature surrounding the use of potentially stigmatizing language in OUD clinical care focuses on cross-sectional surveys and theoretical scenarios rather than real-world data.6, 7 Associations between language in clinical documentation and patient-oriented outcomes have yet to be elucidated. We sought to address this knowledge gap by evaluating clinical data from a group of patients admitted to the hospital for infectious complications of OUD and injection drug use (IDU). Specifically, the goal of this study was to determine how inpatient physicians describe hospitalized persons with OUD, and to understand associations of this language with outcomes along the OUD continuum of care.
METHODS
This study is part of the larger Continuum of Care in Hospitalized Patients with Opioid Use Disorder and Infectious Complications of Drug Use (CHOICE) collaboration. CHOICE is a retrospective cohort investigation of adults hospitalized with an infectious complication of injection opioid use at University of Maryland Baltimore, George Washington University, University of Alabama Birmingham, and Emory University. At the time of the study, two sites provided addiction consultation services daily, one site had addiction consultation available some but not all days, and one site did not have a bedside addiction consultation service. The primary aim of CHOICE is to understand the impact that medication for opioid use disorder (MOUD) provision (including either continuation of outpatient treatment or initiation in the hospital) and addiction consultation had on this population’s outcomes, including premature discharge, readmission, and post-discharge linkage to MOUD treatment.
Included patients were hospitalized from 1/1/2018–12/31/2018 and had ICD-10 diagnosis codes consistent with OUD and acute bacterial/fungal infection (i.e. skin and soft tissue infection, endocarditis, bacteremia/sepsis, osteoarticular infections, spinal/epidural abscess; full list provided in Supplemental Materials). ICD-9 diagnosis codes were mapped to ICD-10 codes using General Equivalence Mappings and manual review by the study team.16, 17 We reviewed the medical record to verify active diagnoses of both opioid use disorder and one or more bacterial or fungal infections associated with injection drug use at the time of hospitalization. The project was deemed exempt by the University of Maryland, Baltimore Institutional Review Board.
Trained, nonblinded research assistants abstracted data regarding demographics, inpatient interventions, and transitions of care. Site leads (JEC, JC, EE, IK, AS, SK, ER) were responsible for monitoring data abstractors. The lead site (CB, ER) performed data cleaning and followed up with sites to address missing data points. Discharge timing was defined as planned versus premature (i.e. discharge against medical advice or patient-directed discharge). Abstractors also reviewed narrative text and problem-based plans of the inpatient hospital discharge summary for language used to describe the patient. Data abstractors could choose one or multiple options from a list including the following terms: abuse, addiction, dependence, misuse, use disorder, IVDU, and other. Abuse and misuse were considered potentially stigmatizing, while use disorder was considered best practice.14, 18 Other terms (addiction, dependence, IVDU, other) were considered neutral. For the purposes of analysis, discharge summaries containing any mention of “use disorder” were categorized as containing best practice language, even if potentially stigmatizing language was also found in the same document.
Outcomes reviewed included hospital-based provision of MOUD (both new starts and continuation of outpatient medication), planned versus premature discharge, MOUD prescribing upon discharge, provision of naloxone, documentation of an OUD treatment plan, documentation of addiction-specific referral, and admission duration. Documentation of an OUD treatment plan was a holistic outcome encompassing formal referrals to or appointments made with medical providers, narcotics anonymous or support groups, counseling regarding harm reduction, or provision of educational materials. Addiction-specific referral was defined as having a documented referral to or follow up date with a clinician to provide ongoing addiction-specific care.
Statistical Analyses
Patient characteristics were described using frequencies and percentages for categorical variables and medians and interquartile ranges (IQR) for continuous variables. The primary analytic goal was to determine whether operational outcomes differed as a function of language use, specifically when there was any use of best practice language. The binary outcomes were evaluated using separate logistic regression models with fixed-effects for site. Odds ratios and 95% confidence intervals are presented from each regression model. Because admission duration is positively skewed, inherently positive, and heteroscedastic, this outcome was evaluated using a fixed-effects Gamma regression. Coefficients were converted to mean differences and corresponding 95% confidence intervals. Regressions were also adjusted for age, race, ethnicity, gender, insurance status, and diagnosis (soft tissue infection, bacteremia, endocarditis, osteomyelitis, septic arthritis, and epidural abscess). Natural cubic splines were used to allow for non-linear effects of age. 95% confidence intervals were computed using bias-corrected and accelerated bootstrap resamples (10,000 resamples). Across the entire data set, 1.9% of data points were missing. The pattern of missingness was consistent with missingness completely at random (Little’s p = .99). Five complete data sets were imputed using fully conditional specification;19 all variables were included in the imputation model. Analyses were conducted using R (v. 4.2.0; R Core Team, 2022).
RESULTS
A total of 1285 electronic medical records were reviewed based upon ICD9/10 diagnosis codes consistent with OUD and acute bacterial/fungal infection. Upon chart review, 521 were excluded as there was not clear evidence for opioid use disorder, 109 were excluded as there was no evidence for an active infection, 255 were excluded as the active infection was unrelated to injection opioid use, and 70 were excluded for other reasons. Three hundred and twenty-eight (25%) were ultimately included (Figure 1). Of the included participants, 191 (58%) were male and 214 (65%) were white, with a median age of 38 years (IQR: 31–51) (Table 1). Most (189, 58%) were publicly insured and 110 (34%) were uninsured. Skin and soft tissue infections were the most common infection observed, diagnosed in 209 (64%) patients. Unplanned discharge occurred in 79 (24%) cases, and the median hospital length of stay (LOS) was 6 days (IQR: 3–13). Ninety-seven (30%) were on MOUD at baseline. MOUD was provided during hospitalization to 151 (46%) patients; 67 (20%) were newly started on MOUD and 84 (26%) were continued on their existing outpatient medication during hospitalization.
Figure 1:
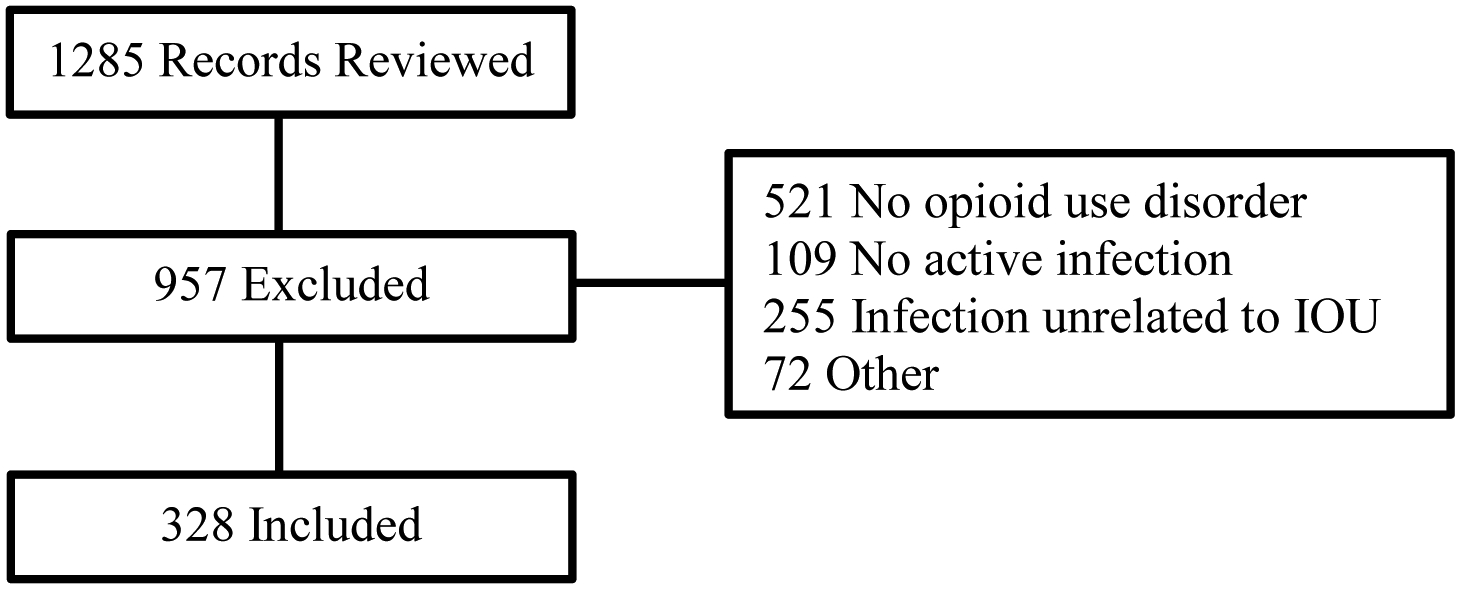
Participant Enrollment. IOU: Injection opioid use
Table 1.
Patient Characteristics: Demographics, Insurance and Housing Status, Admitting Diagnoses and Service. CHOICE Study (N=328)
| Characteristic | Full Sample | Without “Use Disorder” | With “Use Disorder” |
|---|---|---|---|
| Age, M (IQR) | 38 (31 – 51) | 38 (30 – 50.5) | 41 (33 – 52) |
| Gender, N (%) | |||
| Female | 137 (41.8) | 105 (41.5) | 32 (42.7) |
| Male | 191 (58.2) | 148 (58.5) | 43 (57.3) |
| Race, N (%) | |||
| Asian | 3 (0.9) | 2 (0.8) | 1 (1.3) |
| Black | 101 (30.8) | 72 (28.5) | 29 (38.7) |
| White | 214 (65.2) | 170 (67.2) | 44 (58.7) |
| Other | 10 (3) | 9 (3.6) | 1 (1.3) |
| Hispanic, N (%) | 12 (3.7) | 8 (3.2) | 4 (5.3) |
| Insurance, N (%) | |||
| Medicaid | 164 (50) | 114 (45.1) | 50 (66.7) |
| Medicare | 25 (7.6) | 17 (6.7) | 8 (10.7) |
| Other | 15 (4.6) | 12 (4.7) | 3 (4.0) |
| Private | 14 (4.3) | 11 (4.3) | 3 (4.0) |
| Uninsured | 110 (33.5) | 99 (39.1) | 11 (14.7) |
| Housing, N (%) | |||
| Stable | 180 (54.9) | 137 (54.2) | 43 (57.3) |
| Not Stable | 148 (45.1) | 116 (45.8) | 32 (42.7) |
| Diagnoses, N (%) | |||
| Soft Tissue Infection | 209 (63.7) | 154 (60.9) | 55 (73.3) |
| Bacteremia | 110 (33.5) | 84 (33.2) | 26 (34.7) |
| Endocarditis | 51 (15.5) | 42 (16.6) | 9 (12.0) |
| Osteomyelitis | 48 (14.6) | 35 (13.8) | 13 (17.3) |
| Septic Arthritis | 14 (4.3) | 12 (4.7) | 2 (2.7) |
| Epidural Abscess | 19 (5.8) | 11 (4.3) | 8 (10.7) |
| Other | 36 (11) | 31 (12.3) | 5 (6.7) |
| Admitting Service, N (%) | |||
| ICU | 36 (11) | 33 (13.0) | 3 (4.0) |
| Medical | 256 (78) | 197 (77.9) | 59 (78.7) |
| Surgical | 21 (6.4) | 16 (6.3) | 5 (6.7) |
| Other | 15 (4.6) | 7 (2.8) | 8 (10.7) |
| MOUD at baseline | 97 (29.6) | 72 (28.5) | 25 (33.3) |
M – Median, IQR – Interquartile Range, N – Frequency, % – Percentage, MOUD – Medications for Opioid Use Disorder
“Abuse” was the most common term found in discharge summaries, used to describe 219 (67%) participants (Table 2). Potentially stigmatizing language (abuse or misuse) was noted in 223 (68%) medical records, and the best practice term “use disorder” was recorded in only 75 (23%) medical records. In 151 (46%) cases, a combination of best practice, potentially stigmatizing, and/or neutral terms were used in the same discharge summary.
Table 2.
Language Used in Patient Charts and Patient Outcomes, CHOICE Study.
| Language Used, N / % | N | %* |
|---|---|---|
| Abuse | 219 | 66.8 |
| Addiction | 12 | 3.7 |
| Dependence | 28 | 8.5 |
| IVDU | 145 | 44.2 |
| Misuse | 4 | 1.2 |
| Opioid Use Disorder | 75 | 22.9 |
| Characteristic | N | % |
| MOUD, New Initiation, N / % | 67 | 29# |
| MOUD, Continuation, N / % | 84 | 86.6# |
| Planned Discharge, N / % | 249 | 75.9 |
| OUD Treatment Plan, N / % | 219 | 66.8 |
| MOUD on Discharge, N / % | 129 | 39.3 |
| Naloxone, N / % | 24 | 7.3 |
| Addiction-Specific Follow-up, N / % | 127 | 38.7 |
| Admission Duration, M / IQR | 6 | 3 – 13 |
M – Median; IQR – Interquartile Range, N – Frequency, % – Percentage, MOUD – Medications for Opioid Use Disorder
Language types were not mutually exclusive. Thus, the sum of the percentages is greater than 100.
Percentages for these characteristics are relative to the number of patients that were not (231) and were (97) on MOUD at baseline.
In the unadjusted regression analysis, any mention of “use disorder” in the discharge summary was associated with increased odds of planned discharge (OR 2.14, 95% CI 1.06–4.30;Table 3), having a documented plan for post-discharge OUD treatment (OR 4.30, 95% CI 2.03–9.14) and having a documented appointment date or referral for addiction-specific follow up care (OR 2.30, 95% CI 1.33–3.99). Mean LOS was approximately 2.5 days, or 21% longer if “use disorder” was used in the discharge summary than if not; however, this did not reach statistical significance (95% CI −7.57 – 44.15%). There were no significant associations between use of best practice language and inpatient medications for OUD (MOUD; i.e. buprenorphine, methadone) initiation or prescription of MOUD upon hospital discharge.
Table 3.
Regression Results for Best Practice Language Use and MOUD/OUD Outcomes, CHOICE Study
| Characteristic | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| MOUD in-hospital (Full Sample) | 1.48 | 0.70 – 3.09 | 1.76 | 0.82 – 3.79 |
| MOUD Initiation (New Only) | 1.32 | 0.60 – 2.89 | 1.49 | 0.61 – 3.66 |
| Planned Discharge | 2.14† | 1.06 – 4.30 | 1.74 | 0.80 – 3.79 |
| OUD Treatment Plan | 4.30† | 2.03 – 9.14 | 5.21† | 2.28 – 11.89 |
| MOUD on Discharge | 1.40 | 0.80 – 2.43 | 1.95 | 0.97 – 3.91 |
| Naloxone | 1.39 | 0.50 – 3.82 | 0.84 | 0.30 – 2.33 |
| Addiction-Specific Referral | 2.30† | 1.33 – 3.99 | 2.47† | 1.36 – 4.47 |
| Admission Duration* | 20.62 | −7.61 – 57.47 | 15.43 | −7.57 – 44.15 |
OR – Odds Ratio, 95% CI – 95% Confidence Interval
Coefficients are percent changes
p<.05
When adjusted for age, race, gender, ethnicity, diagnoses, insurance status, and baseline MOUD (Supplemental materials), use of non-stigmatizing terminology was no longer significantly associated with planned discharge, but remained significantly associated with having a documented plan for ongoing OUD treatment (AOR 5.21, 95% CI 2.28–11.89; Table 3) and having a documented plan for addiction-specific follow up care (AOR 2.47, 95% CI 1.36–4.47).
DISCUSSION
In this retrospective study of patients hospitalized with infectious complications of injection opioid use, potentially stigmatizing language was commonly used in hospital discharge summaries, observed in over two-thirds of cases. Conversely, guideline-concordant application of person-first language was observed in only 25% of medical records reviewed and was associated with higher odds of addiction specific follow-up planning and lower odds of unplanned discharge. While we cannot determine causation, these data indicate that clinicians using guideline-concordant language in discharge summaries may also be more likely to consider OUD-specific interventions in discharge planning. Our real-world results describing clinicians’ use of potentially stigmatizing and guideline-concordant language in clinical documentation are largely consistent with prior observations in cross-sectional surveys and theoretical patient care scenarios.7, 10, 15
Patients in CHOICE whose clinicians utilized guideline-concordant language in the discharge summary were more likely to have a documented plan for OUD treatment and addiction-specific follow up than those who did not utilize guideline-concordant language. While language alone cannot account for these findings, it is probable that clinicians using guideline-concordant language are generally more aware of the chronic disease model of addiction and more likely to engage in recommended practices for treatment of individuals with OUD. Taken together with the prevalence of stigmatizing language identified here, there is a demonstrated need for ongoing and amplified educational campaigns and structural interventions aimed towards appropriate use of non-stigmatizing language in the clinical setting. These interventions can be straightforward: a recent randomized clinical trial of 1842 healthcare professionals demonstrated that exposure to a “Words Matter” or “Medication Treatment Works” message frame and written narrative vignette from the perspective of a person with OUD was associated with decreased stigmatization and increased subjective “warmth rating” towards people with OUD.20
Unplanned hospital discharge is a common outcome in patients hospitalized for infectious complications of injection drug use, as high as 25% in some publications, similar to what we observed in the CHOICE study.21, 22 The reasons for this are multifactorial; failure to adequately treat cravings and withdrawal (i.e. initiation of MOUD), appropriately manage pain, and address discrimination and stigmatization of substance use by hospital staff may all increase the likelihood of an unplanned discharge.22, 23 In unadjusted analysis, patients whose discharge summary contained the term “use disorder” were more likely to undergo a planned discharge than those where the discharging provider did not use this term, however this result was no longer significant after adjusting for age, race, gender, ethnicity, diagnoses, insurance status, and baseline MOUD. This may reflect that individuals on baseline MOUD are more likely to receive hospital-based MOUD, avoiding withdrawal and increasing the chance of a planned discharge. We did not collect specific information surrounding the reason for unplanned discharge, and so cannot verify this hypothesis.
Increasingly, hospital-based initiation of MOUD, with a low threshold to initiate care, is the standard of care for patients admitted for complications of OUD.5 We did not observe an association between use of guideline-concordant language and either inpatient MOUD initiation or MOUD prescribing upon discharge. This stands in opposition to our assertion above regarding awareness of best practices by clinicians using guideline-concordant language. Facility-level factors could be at least partly responsible, despite accounting for fixed effects by site. Bedside addiction medicine consultation, for example, was not available at all sites, and access to outpatient treatment varied based upon local and regional factors. This may also be reflective of the fact that we only assessed language in the discharge summary, and given frequent provider turnover during the course of a hospitalization, the person writing the discharge summary may not have been determining inpatient management for the entirety of the admission. It is also possible that terms used to describe patients were copied from earlier entries in the medical record and do not reflect language used at the bedside by the treating provider(s). This merits further investigation to further delineate patient-, provider-, and institutional-level factors behind language and MOUD use, particularly as increasing numbers of clinicians gain competence and confidence initiating and prescribing MOUD. Further prospective research is also needed to determine the independent effects of best practice versus potentially stigmatizing language on patient-centered outcomes.
Limitations
This is a retrospective study, and the associations we noted between language and clinical outcomes must be interpreted as such, without inference of causation. Language used was determined via manual abstraction from the medical record, and it is possible that errors were introduced during the abstraction and data entry processes. In many cases multiple terms were used in discharge summaries, sometimes including both potentially stigmatizing and best-practice language, making results more difficult to interpret. It is possible that language was copied forward from prior entries in the medical record and may not reflect the views or opinions of the inpatient team. Premature discharge was common, and could have biased clinicians’ language in discharge summaries prepared after these encounters. Additionally, we did not collect information regarding the level of training or years of professional experience for the individual who wrote the discharge summary (e.g. PGY 1–3, junior attending, senior attending). We believe that this would be difficult to definitively determine given that, on inpatient academic teams, discharge summaries are often composed and edited by multiple individuals. Finally, our study was performed using admissions from 2018. It is notable that NIDA’s Words Matter guidelines had not yet been released and results might be different if the study were repeated after this guidance was disseminated.
CONCLUSIONS
Use of potentially stigmatizing language was common in this study of patients hospitalized for infectious complications of injection drug use and OUD. Application of best practice language was uncommon, but when used, it was associated with increased odds of referral to addiction specialty follow up care. Educational campaigns to emphasize evidence-based care, including non-stigmatizing language, and rigorous prospective studies are required to better understand associations between providers’ language and clinical outcomes.
Supplementary Material
Funding
Emory Center for AIDS Research (NIH P30 AI050409)
University of Alabama at Birmingham Center for AIDS Research (NIH P30 AI 027767)
NIH Office of AIDS Research (HHSN269201400012C)
District of Columbia Center for AIDS Research (NIH P30 AI117970)
Footnotes
Declarations of competing interest: The authors report no conflicts of interest.
Prior presentations: Partial results of this study were presented at IDWeek 2021, Virtual.
Ethical approval: The project was deemed exempt by the University of Maryland, Baltimore Institutional Review Board.
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21–07-01–003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2021. [Google Scholar]
- 2.National Academiies of Sciences Engineering and Medicine. Medications for opioid use disorder save lives. Washington, D.C.: National Academies Press; 2019. [PubMed] [Google Scholar]
- 3.Olsen Y, Sharfstein JM. Confronting the stigma of opioid use disorder—and its treatment. JAMA. 2014;311(14):1393–1394. [DOI] [PubMed] [Google Scholar]
- 4.Corrigan PW, Nieweglowski K. Stigma and the public health agenda for the opioid crisis in America. Int J Drug Policy. 2018;59:44–49. [DOI] [PubMed] [Google Scholar]
- 5.Gupta R, Levine RL, Cepeda JA, Holtgrave DR. Transforming Management of Opioid Use Disorder with Universal Treatment. N Engl J Med. 2022;387(15):1341–1344. [DOI] [PubMed] [Google Scholar]
- 6.Madden EF, Prevedel S, Light T, Sulzer SH. Intervention Stigma toward Medications for Opioid Use Disorder: A Systematic Review. Subst Use Misuse. 2021;56(14):2181–2201. [DOI] [PubMed] [Google Scholar]
- 7.McGinty EE, Barry CL. Stigma reduction to combat the addiction crisis—developing an evidence base. N Engl J Med. 2020;382(14):1291–1292. [DOI] [PubMed] [Google Scholar]
- 8.National Academies of Sciences Engineering and Medicine. Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change. Washington, DC: The National Academies Press; 2016. [PubMed] [Google Scholar]
- 9.Volkow ND. Stigma and the toll of addiction. N Engl J Med. 2020;382(14):1289–1290. [DOI] [PubMed] [Google Scholar]
- 10.Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010;21(3):202–207. [DOI] [PubMed] [Google Scholar]
- 11.Goodyear K, Haass-Koffler CL, Chavanne D. Opioid use and stigma: the role of gender, language and precipitating events. Drug Alcohol Depend. 2018;185:339–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiner SG, Lo Y-C, Carroll AD, et al. The Incidence and Disparities in Use of Stigmatizing Language in Clinical Notes for Patients With Substance Use Disorder. J Addict Med. 2023. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volkow ND, Gordon JA, Koob GF. Choosing appropriate language to reduce the stigma around mental illness and substance use disorders. Neuropsychopharmacology. 2021; 46:2230–2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute on Drug Abuse. Words Matter: Terms to Use and Avoid When Talking About Addiction. 2021; https://www.drugabuse.gov/sites/default/files/nidamed_words_matter_terms.pdf. [Google Scholar]
- 15.Kennedy AJ, Lombardi K, Fruehstorfer G, Hamm M, McNeil M, Carter A. Words Medicine Residents Use to Describe Substance Use Disorders After Attending a Mutual Support Group Meeting. J Gen Intern Med. 2021;36:3913–3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merchant E, Burke D, Shaw L, et al. Hospitalization outcomes of people who use drugs: One size does not fit all. J Subst Abuse Treat. 2020;112:23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Columbo JA, Kang R, Trooboff SW, et al. Validating Publicly Available Crosswalks for Translating ICD-9 to ICD-10 Diagnosis Codes for Cardiovascular Outcomes Research. Circ Cardiovasc Qual Outcomes. 2018;11(10):e004782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Recovery Research Institute. Addictionary. 2021; https://www.recoveryanswers.org/addiction-ary/. Accessed November 18, 2021. [Google Scholar]
- 19.Liu Y, De A. Multiple Imputation by Fully Conditional Specification for Dealing with Missing Data in a Large Epidemiologic Study. Int J Stats Med Res. 2015;4(3):287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kennedy-Hendricks A, McGinty EE, Summers A, Krenn S, Fingerhood MI, Barry CL. Effect of Exposure to Visual Campaigns and Narrative Vignettes on Addiction Stigma Among Health Care Professionals: A Randomized Clinical Trial. JAMA Netw Open. 2022;5(2):e2146971–e2146971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kimmel SD, Kim J-H, Kalesan B, Samet JH, Walley AY, Larochelle MR. Against Medical Advice Discharges in Injection and Non-injection Drug Use-associated Infective Endocarditis: A Nationwide Cohort Study. Clin Infect Dis. 2020;73(9):e2484–e2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan ACH, Palepu A, Guh DP, et al. HIV-Positive Injection Drug Users Who Leave the Hospital Against Medical Advice: The Mitigating Role of Methadone and Social Support. J Acquir Immune Defic Syndr. 2004;35(1):56–59. [DOI] [PubMed] [Google Scholar]
- 23.Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abus 2020;41(4):519–525. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


