Abstract
Perceived ethnic discrimination (PED) is predictive of chronic pain-related outcomes. Less is known about pathways through which these constructs interact. The goal of this study was to test whether PED was predictive of chronic pain-related outcomes (pain interference, pain intensity, and symptoms related to central sensitization), whether depression mediated the relationship between PED and pain outcomes, and if these relationships were maintained across sex in a sample of racially and ethnically minoritized adults (n = 77). PED significantly predicted pain interference, pain intensity, and symptoms related to central sensitization. Sex accounted for a significant proportion of the variance in pain interference only. Depression explained the relationship between PED and pain interference and pain intensity. Sex moderated the indirect pathway, such that for men, the relationship between PED and pain interference and pain intensity was explained via depression. Depression partially explained the relationship between PED and symptoms related to central sensitization. Sex did not moderate this mediational effect. This study provided a unique contribution to the pain literature by providing a contextual analysis of PED and pain. Addressing and validating experiences of lifetime discrimination may be a clinically relevant tool in the management of chronic pain for of racially and ethnically minoritized adults.
Keywords: Ethnic Discrimination, Chronic Pain, Depression, Sex, Health Disparities
Introduction
Perceived ethnic discrimination (PED) is a form of psychosocial stress that is estimated to impact approximately 75% of Black, Hispanic/Latinx, Native, and Asian Americans (Findling et al. 2019; Lee et al. 2019). A growing body of literature has begun to explore the prevalence and impact of PED on the mental and physical health of adults who identify as belonging to a racially or ethnically minoritized group (Carter et al. 2019). PED has been directly linked to depression (Trost et al. 2019), psychological distress (Garcia, David, and Mapaye 2019), cardiovascular deficits (Panza et al. 2019), reduced overall health (Nicholson 2020), and pain outcomes (Brown et al. 2018).
Chronic pain is a public health problem that impacts 20% of the U.S. population (Dahlhamer et al. 2018). Disparities in chronic pain experience have been found across race, sex, and age, with a higher prevalence reported in Non-Hispanic White and Black respondents, older adults, and women (Dahlhamer et al. 2018; Zelaya et al. 2020). Despite increased reports of chronic pain among Non-Hispanic White individuals relative to racially and ethnically minoritized groups, Black and African Americans report the highest levels of generalized pain-related disability (Janevic et al. 2017) and pain sensitivity (Meints and Edwards 2018b) and racially minoritized groups are generally undertreated for pain-related issues (Morales and Yong 2021). Recent findings have provided evidence for the role of psychosocial stress on experiences of generalized pain (Meints and Edwards 2018b) and related constructs, such as central sensitization (CS) (Güereca et al. 2022). Despite growing evidence demonstrating the pernicious impact of PED on pain outcomes, less is known about potential mediators through which these processes influence outcomes (Boring et al. 2021; Walker Taylor et al. 2018).
Preliminary evidence suggests that depression may play a role in explaining how psychosocial stress influences pain outcomes. Depression has been found to be related to experiences of ethnic discrimination and pain-related injustice appraisals (Ziadni et al. 2020), greater pain catastrophizing (Dong et al. 2020), pain interference (Rahman et al. 2020) and generalized experience of chronic pain (Tappe-Theodor and Kuner 2019). There is initial evidence that it may also mediate the relationships between psychosocial stress and pain interference (Morasco et al. 2013; Walker Taylor et al. 2018), pain intensity (Piontek et al. 2020), chronic pain diagnoses (Earnshaw et al. 2015), and probability of developing generalized chronic pain (Brown et al. 2018).
There is preliminary, but conflicting, evidence that the psychological impact of exposure to racial discrimination differs between sexes, and it is currently unclear whether these potential sex differences are associated with differential experiences of chronic pain. In an early study, exposure to racial discrimination was found to be associated with anxiety and obsessive-compulsive symptoms, but not depression, for African American women compared to men (Greer, Laseter, and Asiamah 2009) and in a later study increases in racial discrimination across the lifespan was found to predict depression symptoms in males compared to females (Assari et al. 2017). Additionally, exposure to racial discrimination has consistently been found to have a stronger association with chronic pain experience among women compared to men (Boring et al. 2021; Merriwether et al. 2021). Pain researchers have begun to identify the unique contributions of perceived discrimination, depression, and sex on pain-related constructs in chronic pain populations, however, more research is needed to elucidate the exact pathways through which these constructs relate and how they interact for different sociodemographic groups.
Aims and hypotheses
The primary aim of this study was to assess if PED predicts pain-related outcomes among a national sample of people who endorse chronic pain and identify as being a member of an ethno-racial minoritized group. The secondary aim was to evaluate depression as a mediator of the relationship between PED and pain-related outcomes. The third aim was to assess if sex identified at birth moderated the relationships between PED and pain-related outcomes, and to assess if sex identified at birth moderated the mediational pathways from PED to depression and depression to pain-related outcomes.
We hypothesized that,
PED would significantly predict pain intensity, pain interference, and symptoms related to CS
Depression would mediate the relationships between PED and pain intensity, pain interference, and symptoms related to CS
Sex would moderate the relationships between PED and pain intensity, pain interference, and symptoms related to CS such that (3a) PED would predict outcomes for females and not for males and (3b) sex would moderate the mediational pathways from PED to pain intensity, pain interference, and symptoms related to CS, such that for females, depression would mediate the relationship between PED and pain outcomes and for males it would not.
Method
In this cross-sectional study, we conducted secondary analyses using a subsection of a larger survey battery designed to examine the psychometric properties of a new self-report survey instrument. The parent study and secondary analyses were approved by the Oregon Health & Science University’s institutional review board. Written informed consent was obtained from all participants prior to participating in the study. Qualtrics (Qualtrics 2020) was contracted to recruit a randomly-selected, United States national sample. Strategic quota sampling was used to target respondents as to reflect the 2010 census stratified in domains of race, ethnicity, geographic location, age, sex identified at birth, education, and income. Eligible participants were English-speaking adults, ages 18–70, had internet access, and reported chronic pain, as defined by the National Institute of Health Task Force for Research Standards for Chronic Pain (Deyo et al. 2015). The RTF recommends that “chronic pain” be defined as a pain problem that has persisted at least three months and has resulted in pain at least half the days over the past six months. Following RTF guidelines, we included two questions to define chronicity: “How long has pain has been an ongoing problem for you?” and “How often has pain been an ongoing problem for you over the past 6 months?” A response of “greater than 3 months” to question one and a response of “at least half the days in the past 6 months” to question two indicated chronic pain. Exclusion criteria included the endorsement of being currently involved with a workers’ compensation claim or currently undergoing a disability application or claim.
Qualtrics recruited 2,743 participants to take the survey. Of these individuals, 301 participants met inclusionary criteria, consented to the study, and completed an online battery of validated questionnaires. Questionnaires were presented in a randomized order to reduce ordering effects. All surveys were completed remotely online in a single administration session lasting an average of 29 minutes. Of the 301 participants, 77 individuals identified as being a member of an ethno-racial minoritized group (i.e. Hispanic, Latinx, Spanish, Black, Asian, Native American, or multiple ethnicities identified). No missing data was found in the dataset.
Measures
Demographic information collected included age, sex identified at birth, gender, race/ ethnicity, education, employment, income, relationship status, chronic pain duration, and pain location.
The PROMIS Pain Interference Short Form (PROMIS Pain Interference 4a; Amtmann et al. 2010) is a four-item scale that measures the degree to which pain interferes in daily living. Items are rated on a 5-point Likert-type scale ranging from 1 (Not at all) to 5 (Very much). Total scores range from 4 to 20. A total score is calculated by summing scores across all items, with higher scores indicating more pain interference. The measure demonstrates excellent reliability (α = 0.90) and expected correlations with bodily pain and pain interference (Amtmann et al. 2010).
The PROMIS Pain Intensity Scale (PROMIS Pain Intensity 1a; Cella et al. 2019) is a one-item scale that assesses pain intensity over the last seven days using a numerical rating scale of 0 (No Pain) to 10 (Worse Imaginable Pain). Higher scores indicate greater pain intensity.
The Central Sensitization Inventory- Part A (CSI; Mayer et al. 2012) is a 25-item self-report measure that assesses key polysomatic symptoms associated with hyperactivity of pain processing in the central nervous system, present in many chronic pain disorders. Items are rated on a 5-point Likert-type scale ranging from 1 (Never) to 5 (Always). Two example items include, “I feel pain all over my body,” and “My muscles feel stiff and achy.” Total scores range from 25 to 125. A total score is calculated by summing scores across all items, with higher scores indicating greater symptom severity. The CSI has been shown to discriminate between pain patients and non-pain patients and is shown to be associated with pain disability and pain severity The CSI demonstrates excellent reliability (α = 0.93) and expected correlations with the Widespread Pain Inventory and Pain Catastrophizing scale (Van Wilgen et al. 2018).
The Brief Perceived Ethnic Discrimination Questionnaire - Community Version (Brief PEDQ-CV; Brondolo et al. 2005) is a 17-item measure derived from the full-length 70-item PEDQ-CV measure that assesses perceived exposure to ethnic discrimination from peoples of any ethnic/racial background. The Brief PEDQ-CV consists of five factors: Lifetime Exposure, Exclusion/Rejection, Stigmatization/Devaluation, Discrimination at Work/School, and Threat/Aggression. Items are responded to on a five-point Likert-style scale ranging from 1 (Never happened) to 5 (Happened very often). Total scores range from 17 to 85. Higher scores indicate a higher perception of lifetime racism. The Brief PEDQ-CV demonstrates good internal consistency (α = 0.88) and convergent validity with the Perceived Racism Scale (Collado-Proctor 1999).
The PROMIS Depression Scale Short Form (PROMIS Depression 4a; Cella et al. 2019) is a four-item scale that assesses symptoms of depression. Items are rated on a 5-point Likert-type scale ranging from 1 (Never) to 5 (Always). Total scores range from 4 to 20. A total raw score is calculated by summing scores across all items, with higher scores indicating greater symptom severity. While raw scores can be converted into T-scores, the raw scores were used in the current study. The measure demonstrates excellent reliability (α = 0.93) and convergent validity with the Center for Epidemiological Studies Depression Scale and Patient Health Questionnaire (Pilkonis et al. 2014).
Statistical analyses
All statistical analyses were performed using IBM SPSS for Windows version 26.0 (IBM Corp 2019) at an alpha level of 0.05. Prior to data analyses, all variables were examined to evaluate data compliance with parametric analysis assumptions. Pearson’s correlations were conducted to characterize the overall relationship between variables (see Table 2). To test hypothesis one, three hierarchical multiple regression analyses were conducted to investigate if: (1) PED predicted pain intensity, pain interference, and symptoms related to CS. To test hypothesis two, three path analyses using the PROCESS procedure for SPSS (Hayes, 2013) were conducted to assess if depression mediated the relationships between PED and pain intensity, pain interference, and symptoms related to CS. To test hypothesis 3a, an interaction term between PED and sex was added to the three primary regression models. To test hypothesis 3b, we examined the moderating impact of sex on the mediational pathways from PED to pain intensity, pain interference, and symptoms related to CS through depression. For all mediation models, we employed a bootstrapping method to compute an estimate of the indirect effects. Bootstrapping is a non-parametric resampling method that bypasses assumptions of normality common to traditional tests of mediation, and is, thus, more powerful (Preacher & Hayes, 2004, 2008). Specifically, 5,000 samples of the original size were taken from the obtained data (with replacement after each specific number was selected), and indirect effects were calculated in each sample. The mean indirect effect computed over each of these 5,000 samples was used to compute the point estimate. The bias corrected and accelerated 95% confidence intervals (CI; i.e., with z score-based corrections for bias due to the underlying distribution) were then examined, and if these intervals did not contain 0, the point estimate of the indirect effect was considered significant. Sample size was based on statistical power analysis conducted using G*Power software tool (Faul, Erdfelder, Lang, & Buchner 2007). Using the number of predictors as four, a medium effect size level (0.15), a moderate significance level (α =0.05), and a power requirement of 0.80, the minimum required sample size was 80.
Table 2.
Mean, Standard Deviation, Range, Confidence Interval, and Zero-order Correlations Matrix of Outcome Variables (n = 77)
| Variable | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| M | SD | Range | CI | 1 | 2 | 3 | 4 | 5 | |
| 1. ED | 29.08 | 12.22 | 41 | 25.61 – 30.33 | - | .41** | .24* | .46** | .34** |
| 2. PI | 9.80 | 4.10 | 15 | 8.84 – 10.71 | - | - | .72** | .57** | .46** |
| 3. PIN | 4.97 | 2.34 | 9 | 4.45 – 5.49 | - | - | - | .44** | .34** |
| 4. CS | 63.93 | 18.33 | 82 | 59.77 – 68.09 | - | - | - | - | .67** |
| 5. Depression | 8.87 | 4.61 | 16 | 7.99 – 10.13 | - | - | - | - | - |
p < .01
p < .05
ED = Ethnic Discrimination, PI = Pain Interference, PIN = Pain Intensity, CS = Central Sensitization.
Pain duration was controlled for in the regression models due to its predictive capacity on the outcome measures of interest. Age and education were not found to be predictive. The alpha level was set at 0.05 (two-tailed) for all analyses.
Results
Participant demographics are reported in Table 1. The mean age was 47.61 (SD = 15.40) and 65% identified as female. All participants in the sample reported moderate pain intensity (M = 4.97; SD = 4.10) and moderate to severe CS-related symptoms, indexed by a score greater than 40 on the CSI (Neblett et al. 2013) (M = 63.93; SD = 18.33). Males and females did not differ in reported pain outcomes. Respondents reported an average Brief PEDQ-CV score of 29.08 (SD = 12.22), Pain Interference score of 9.80 (SD = 4.10), Pain Intensity score of 4.97 (SD = 2.34), CSI score of 63.90 (SD = 18.33), and Depression score of 8.87 (SD = 4.61). All correlations among study variables were in the expected direction. Descriptive statistics of the variables of interest are reported in Table 2.
Table 1.
Participant Demographics (n = 77)
| Variable | ||||
|---|---|---|---|---|
|
| ||||
| M | SD | Range | CI | |
|
|
||||
| Age | 47.61 | 15.40 | 51 | 44.02 – 51.21 |
| n | % | |||
|
|
||||
| Sex at Birth | ||||
| Male | 25 | 32.50 | ||
| Female | 50 | 64.90 | ||
| Intersex | 2 | 2.50 | ||
| Race/Ethnicity | ||||
| Hispanic/Latinx/Spanish | 15 | 19 | ||
| Black | 33 | 42 | ||
| Asian | 13 | 17 | ||
| Native American | 9 | 12 | ||
| Multiple Ethnicities Identified | 7 | 10 | ||
| Education | ||||
| Less than High school | 1 | 1 | ||
| High school or equivalent | 19 | 24 | ||
| Some College | 20 | 26 | ||
| 2-yr associate degree | 9 | 12 | ||
| 4-yr bachelor’s degree | 17 | 22 | ||
| Master’s degree | 9 | 12 | ||
| Doctoral/ Professional degree | 2 | 3 | ||
| Employment | ||||
| Employed | 24 | 31 | ||
| Temporarily laid off/ Unemployed | 15 | 20 | ||
| Retired | 21 | 27 | ||
| Disabled | 8 | 10 | ||
| Not working- Other | 9 | 12 | ||
| Income | ||||
| Less than 30,000 | 17 | 22 | ||
| 30,000 – 50,000 | 30 | 25 | ||
| 50,000 – 70,000 | 17 | 22 | ||
| 80,000 – 100,000 | 3 | 4 | ||
| 100,000 – 150,000 | 10 | 13 | ||
| Relationship Status | ||||
| Married | 27 | 35 | ||
| Divorce/Separated | 13 | 17 | ||
| Never Married | 35 | 45 | ||
| Chronic Pain Duration | 5 | 5.25 – 6.02 | ||
| 3–6 months | 11 | 14 | ||
| 6–12 months | 10 | 13 | ||
| 1–3 years | 17 | 22 | ||
| 3–5 years | 13 | 17 | ||
| 5–10 years | 10 | 13 | ||
| More than 10 years | 16 | 20 | ||
| Pain Location | ||||
| Neck and Back Pain | 62 | 80 | ||
| Migraines | 1 | 1 | ||
| Hip/ Pelvis | 5 | 6 | ||
| Other | 10 | 13 | ||
Regression analyses
Consistent with hypothesis 1, when controlling for pain duration, PED significantly predicted pain interference, R2 = 0.21, F (2,74) = 9.52, p < .001, β = 0.39; pain intensity, R2 = 0.17, F (2,74) = 7.72, p = .05, β = 0.21; and symptoms related to CS, R2 = 0.33, F (2,74) = 18.53, p < .001, β = 0.57, (Displayed in Tables 3–5). When adding the PED X Sex interaction term to the three regression models, it significantly predicted pain interference, ΔR2 = 0.06, ΔF (1, 72) = 5.91, p = .02, b = −0.16, but not pain intensity, ΔR2 = 0.02, ΔF (1, 72) = 2.19, p = .14 or symptoms related to CS, ΔR2 = 0.004, ΔF (1, 72) = 0.43, p = .51. A simple slope analysis of PED predicting pain interference for females and males demonstrated that the impact of PED on pain interference was significantly different between males and females, revealing a significant relationship for males, β = 0.18, SE = 0 .05, p = .001, but not females β = 0.07, SE = 0.04, p = .06 (Figure 1).
Table 3.
Evaluating Effects of Perceived Ethnic Discrimination on Pain Interference Using Linear Regression Analysis (n = 77)
|
Unstandardized Coefficients
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Step | Predictor | B | SE | β | sr2 | p | R2 | F |
|
| ||||||||
| .21 | 9.52 | |||||||
| 1 | Pain Duration | .58 | .27 | .24 | .24 | < .05 | ||
| 2 | Ethnic Discrimination | .15 | .41 | .39 | .38 | < .001 | ||
Table 5.
Evaluating Effects of Perceived Ethnic Discrimination on CS Using Linear Regression Analysis (n = 77)
|
Unstandardized Coefficients
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Step | Predictor | B | SE | β | sr2 | p | R2 | F |
|
| ||||||||
| .33 | 18.53 | |||||||
| 1 | Pain Duration | 1.39 | 1.23 | .13 | .13 | .26 | ||
| 2 | Ethnic Discrimination | .10 | .17 | .57 | .56 | < .001 | ||
Figure 1:
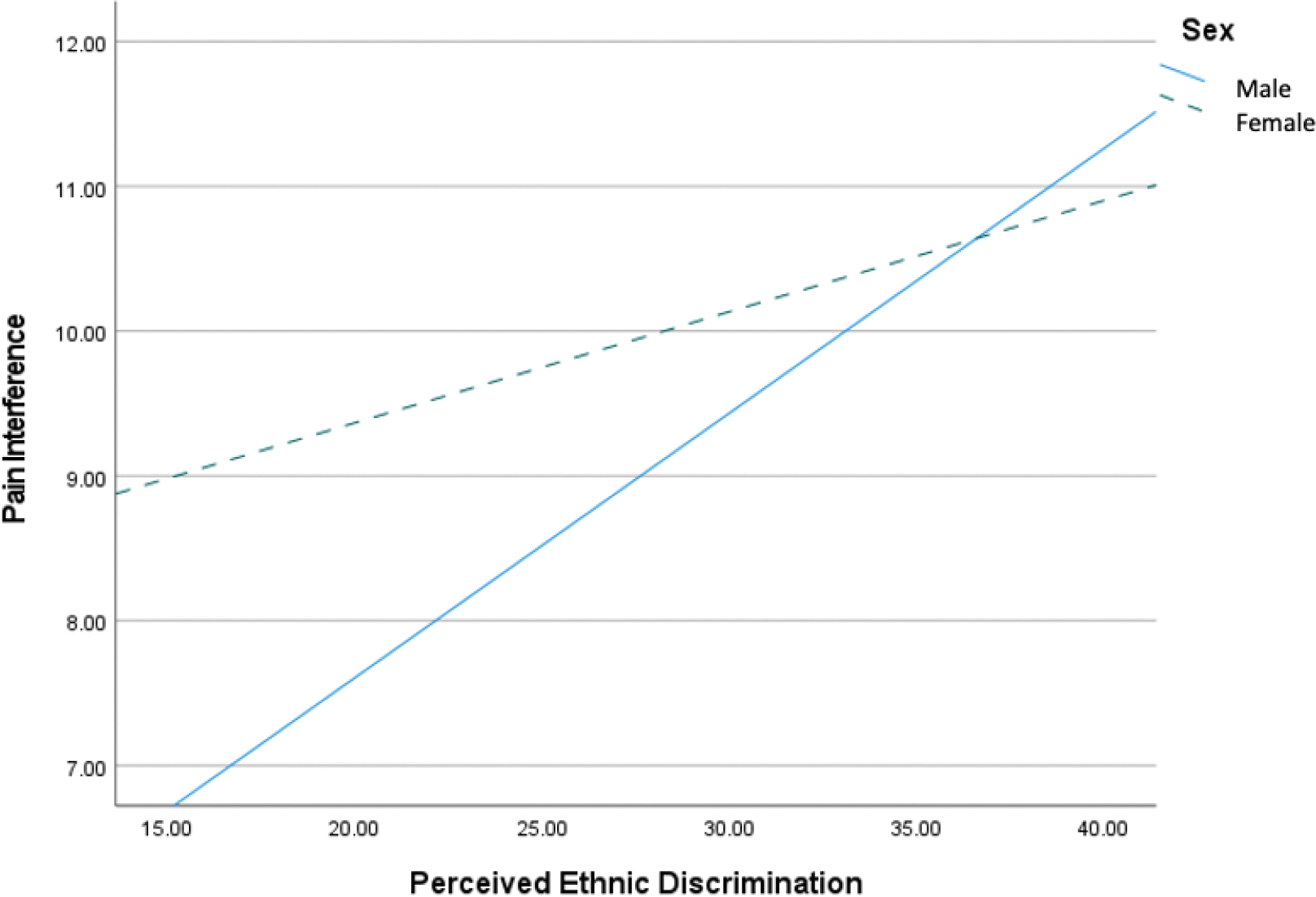
Sex moderates the Relationship between Perceived Ethnic Discrimination and Pain Interference
Path analyses
To assess depression as a mediator of the relationship between PED and pain-related outcomes, we conducted three path analyses in which PED was entered as the independent variable, the pain-related outcome (i.e., pain interference, symptoms related to CS, or pain intensity) as the dependent variable, depression as the mediator, and pain duration as a covariate. Results from the first path analysis demonstrated that scores in depression completely mediated the relationship between PED and pain interference [point estimate = 0.07; 95% bootstrap CI = 0.02, 0.14], displayed in Table 6. After accounting for depression, the relationship between PED and pain interference was no longer significant. Results from a moderated mediation analysis found that sex at birth moderated the mediation ΔR2 = 0.05, ΔF (1,71) = 5.60, p = .02 such that for males, the relationship between PED and pain interference was explained via depression β = 0.58 SE = 0.14, 95% CI (0.29, 0.86); however, for females, depression did not significantly explain this relationship β = 0.20, SE = 0.10, 95% CI (−0.001, 0.43) (Figure 2).
Table 6.
Mediation Effects of Depression on the Relationship Between Perceived Ethnic Discrimination and Pain Interference
| 95% CI |
|||
|---|---|---|---|
| Effect | b | Lower | Upper |
|
| |||
| Total | .16 | .07 | .24 |
| Direct | .09 | −.002 | .18 |
| Indirect (mediation) | .07 | .02 | .14 |
Figure 2:
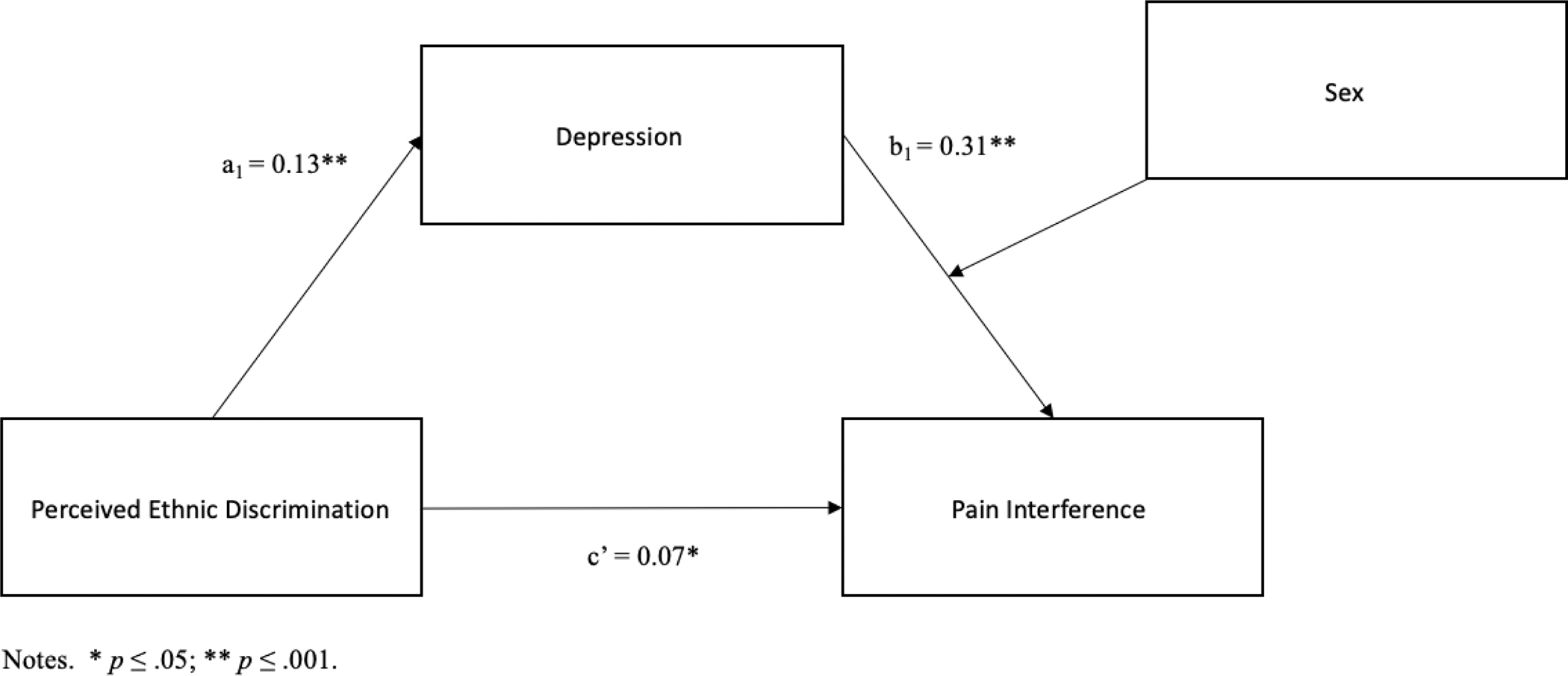
Pain Interference Moderated Meditation
Results from the second path analyses demonstrated that scores in depression completely mediated the relationship between PED and pain intensity [point estimate = 0.02; 95% bootstrap CI = 0.003 to 0.05]. After accounting for depression, the relationship between PED and pain intensity was no longer significant (Table 7). Results from the moderated mediation analysis found that sex at birth moderated the mediational effects ΔR2 = 0.05, ΔF (1,71) = 4.80, p = .03, such that for males, the relationship between PED and pain intensity was explained via depression β = .28 SE = 0.08, 95% CI (0.11, 0.45); however, for females, depression did not significantly explain this relationship β = 0.07, SE = 0.06, 95% CI (−0.05, 0.19) (Figure 3).
Table 7.
Mediation Effects of Depression on the Relationship Between Perceived Ethnic Discrimination and Pain Intensity
| 95% CI |
|||
|---|---|---|---|
| Effect | b | Lower | Upper |
|
| |||
| Total | .05 | .004 | .10 |
| Direct | .02 | −.03 | .07 |
| Indirect (mediation) | .02 | .003 | .05 |
Figure 3:
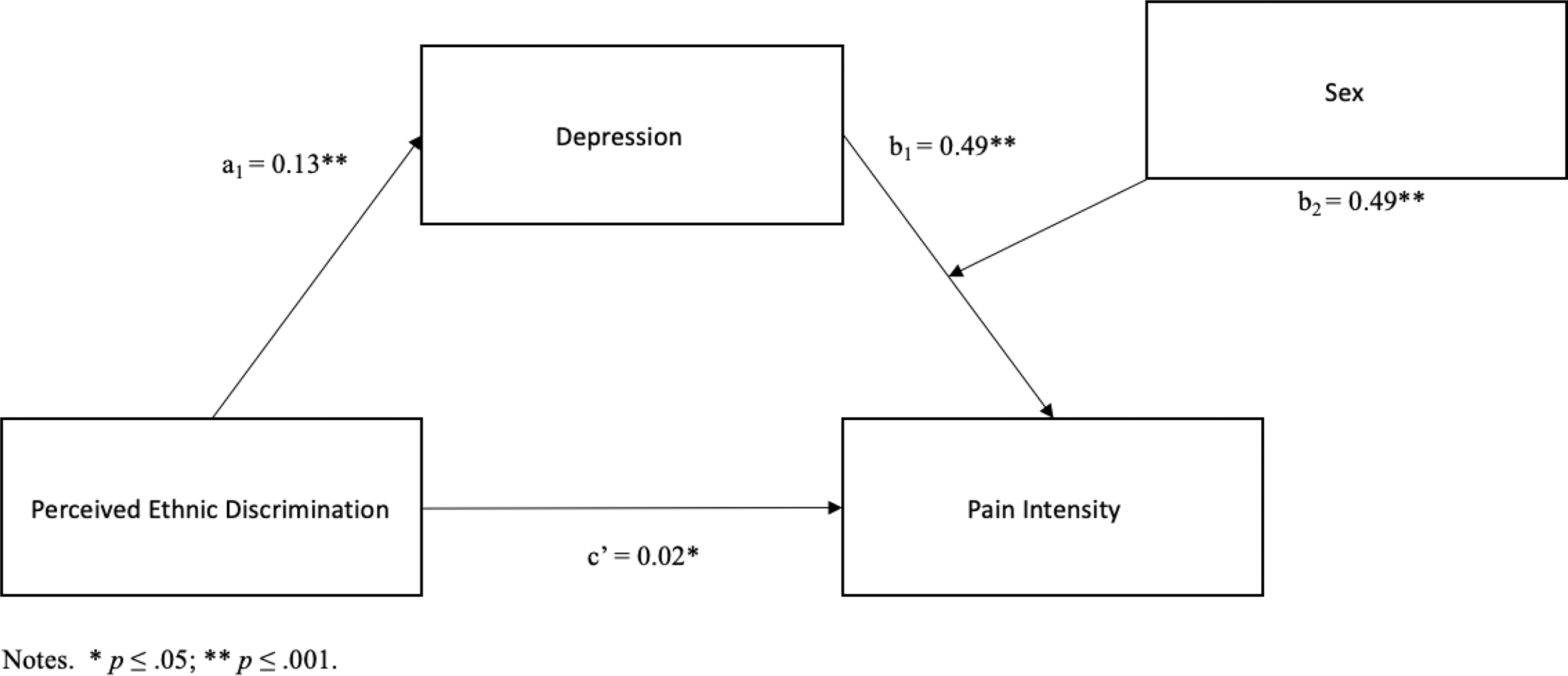
Pain Intensity Moderated Meditation
Results from the third path analyses demonstrated depression partially mediated the relationship between PED and symptoms related to CS, point estimate = 0.42, 95% CI = 0.21 to 0.68 (Table 8). Sex at birth did not moderate this mediational effect ΔR2 = 0.004, ΔF (1,71) = 0.67, p =. 41.
Table 8.
Mediation Effects of Depression on the Relationship Between Perceived Ethnic Discrimination and CS
| 95% CI |
|||
|---|---|---|---|
| Effect | b | Lower | Upper |
|
| |||
| Total | 1.01 | .67 | 1.34 |
| Direct | .58 | .27 | .90 |
| Indirect (mediation) | .42 | .21 | .67 |
Discussion
There is a growing body of research that has provided evidence for the deleterious effects of ethnic discrimination on physical health, mental health, and well-being. The current study adds to the existing literature by examining whether depression is a mediator through which lifetime PED impacts pain-outcomes in a sample of racially diverse participants diagnosed with chronic pain. We hypothesized that: (1) PED would predict pain-related outcomes among a national sample of racially and ethnically minoritized adults who endorse chronic pain; (2) depression would explain the relationship between PED and pain-related outcomes; and (3) the relationships between these variables would not be consistent across sex at birth.
The current findings supported our first and second hypotheses. PED significantly predicted pain interference, pain intensity, and symptoms related to CS. Depression was found to fully mediate the relationship between ethnic discrimination and two outcomes: pain interference and pain intensity. Depression partially mediated the relationship between ethnic discrimination and symptoms related to CS. These results provide preliminary evidence for depression as a candidate mediator in this model. The third hypothesis was partially supported, albeit in the opposite than expected direction. PED significantly predicted pain interference for males, but not for females, and the mediational path through PED, depression, and pain interference was significant for males only. No sex differences were found in relation to the predictive capacity of PED on either pain intensity or symptoms related to CS when depression was excluded from the model. However, sex did moderate the mediational pathway between PED, depression, and pain intensity, such that this relationship was significant for males and nonsignificant for females. Sex did not moderate the mediational pathway for symptoms related to CS. These findings suggest that the impact of PED on the pain experience of racially minoritized adults with chronic pain differs between males and females. PED and depression may be particularly salient constructs when assessing pain interference and pain intensity in males.
Together, the findings of the current study partially align with prior research on the impacts of discrimination on pain-related outcomes. This is one of the first studies to address the predictive capacity of PED on symptoms related to CS in a sample of racially and ethnically minoritized adults living with chronic pain. One study to date has directly addressed the relative role of PED on CS. In a sample of 71 adults living with sickle cell disease, greater lifetime racial discrimination experienced in healthcare settings predicted enhanced mechanical temporal summation, an indicator of CS, through enhanced pain severity (Mathur et al. 2016). The results of the current study provide support for the potential role of PED on CS in a clinically broader sample of adults.
PED has been found to be predict bodily pain among African American male veterans, ethnically diverse samples of women, and Hispanic/Latinx samples (Burgess et al. 2009; Carlisle 2015; Dugan et al. 2017). Contrary to the findings of the current study, heightened experiences of daily interpersonal discrimination, but not major experiences of lifetime discrimination, were found to be predictive of pain interference in adults with chronic pain in a national survey (Boring et al. 2021). These results may reflect how differences in PED measurement (i.e., lifetime or daily PED) may impact the level of association between these constructs and pain outcomes. Recent findings have also concluded that discrimination is weakly associated with pain intensity and may be explained by fluctuations in pain experience over time (Ziadni et al. 2020). Of note, one prior study of exclusively older African American women found that perceived discrimination experienced over the past one year was significantly associated with pain intensity, demonstrating that sex may be a contributing factor in this relationship (Walker Taylor et al. 2018).
Our findings are also congruent with previous mediation studies exploring causal relationships between depression and pain, and support Pincus et al.’s (2010) depression pathway model (Hall et al. 2011; Lee et al. 2016). In this model, PED and depressive symptoms give rise to behavioral withdrawal and general tiredness, which leads to greater fear. Greater fear heightens cognitive mechanisms that result in selective attention to threatening stimuli (catastrophizing), leading to increased pain (Currie and Wang 2005).
The findings of the current study related to sex differences in the mediational impact of depression align with existing literature. A previous longitudinal study found that Black male adults who experienced increased racial discrimination from adolescence to adulthood demonstrated an increase in anxiety and depression over time, whereas heightened anxiety and depression were not found in relation to increased experiences of racial discrimination in Black female adults (Assari et al. 2017). However, the current findings are contrary to previous research that have addressed sex differences in relation to the impact of discrimination on mental health and chronic-pain experience. For example, early cross-sectional studies found that gender differences played a role in the impact of discrimination on mental health, such that women experienced early and heightened deleterious mental health symptoms when compared to men (Greer, Laseter, and Asiamah 2009). In accordance with this, Boring and colleagues (2021) found that the association between daily PED and pain interference was strongest among women in their sample, highlighting that both gender and discrimination measurement type (daily or lifetime) may play a role in the predictive relationship between these constructs. Lastly, prior research also indicates that discrimination may be associated to a higher degree with pain outcomes in women when compared with men in a sample with generalized chronic pain (Boring et al. 2021).
Results of the current study were surprising, given previous findings in the scientific literature and socio-cultural inequities experienced by females that may compound with ethnic discrimination to impact health (McClendon et al. 2021). Findings of the current study may be due to differences in the contribution of discrimination timeframe between males and females on pain outcomes. Congruent with this hypothesis, lifetime PED has been found to be predictive of pain in men, whereas daily PED may better predict pain in women (Edwards 2008).
Limitations of the current study must be noted. All study variables were all captured at the same time point, and thus, because of the cross-sectional design, causality could not be determined. Though longitudinal data are preferred to cross-sectional evidence for testing associations between changes in latent traits, theoretical contributions can come from cross-sectional mediation analyses when viewed as a type of variance partitioning, rather than a proxy for longitudinal relations, and can be useful even if none of the variables involve a temporal dimension. Though we provided a theorical rational for our path analyses, the study design did not rule out the possibility of the path being more accurately described as PED > Pain> Depression. Since study variables were all measured at the same time point, we conducted a post-hoc analysis to provide more evidence for our hypothesized model, in which pain was entered as a mediator of the relationship between PED and depression. Results demonstrated that this model was not supported [point estimate = 0.23; 95% bootstrap CI = −.02-.58]. A second limitation to note is that our sample did not have adequate power to analyze the impacts of PED on pain-outcomes between ethno-racial minoritized groups, likely masking important differences between groups.
Future research should analyze between and within minoritized group differences and address the differential protective factors that buffer specific cultural or ethno-racial minoritized groups against the impacts of race-based stress on pain-related outcomes. Future studies may also benefit from utilizing an intersectional methodology to better address how multiple identity factors may shape the experience of discrimination, its impacts on pain-related outcomes, the mediators in this process, and protective factors. A plethora of research has highlighted the role of biological, psychological, and social factors that contribute to experiences of chronic pain (Meints and Edwards 2018a). Individual factors such as epigenetics may play a role in the differential experiences of pain among various ethno-racial groups due to longstanding group differences in environment and psychosocial variables (Aroke et al. 2019). Disparities in treatment due to systemic racism also impact the chronic pain experience of racially and ethnically minoritized adults. Prior research has indeed found that individuals who hold multiple minoritized identities are at risk for experiencing heightened discrimination (Casey et al. 2019), which may impact chronic pain experience. Lastly, the duration, timeframe, and type of PED experienced by racially and ethnically minoritized adults might also be used as separate predictors to better understand which components of PED have a greater impact on pain-outcomes, mental health, and physical health.
In sum, this study has provided a unique contribution to the pain literature by providing a contextual analysis of PED and chronic pain. Further, we expanded on prior findings by addressing the contribution of ethno-racial identity and sex in the relationship between ethnic discrimination, depression, and pain outcomes among a sample of racially diverse individuals with chronic pain. Addressing and validating experiences of lifetime ethnic discrimination may be a clinically relevant tool in the management of chronic pain for ethno-racial minoritized adults.
Table 4.
Evaluating Effects of Perceived Ethnic Discrimination on Pain Intensity Using Linear Regression Analysis (n = 77)
|
Unstandardized Coefficients
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Step | Predictor | B | SE | β | sr2 | p | R2 | F |
|
| ||||||||
| .17 | 7.72 | |||||||
| 1 | Pain Duration | .48 | .14 | .33 | .36 | < .05 | ||
| 2 | Ethnic Discrimination | .49 | .02 | .21 | .21 | .05 | ||
Funding:
This study was supported by Oregon Health & Science University and by a grant from the National Institutes of Health [T32 AT002688]. The authors report there are no competing interests to share.
References
- Amtmann D, Cook KF, Jensen MP, Chen WH, Choi S, Revicki D, Cella D, Rothrock N, Keefe F, Callahan L, and Lai JS. 2010. “Development of a PROMIS item bank to measure pain interference.” Pain 150 (1): 173–182. 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aroke Edwin N., Joseph Paule V., Roy Abhrarup, Overstreet Demario S., Tollefsbol Trygve O., Vance David E., and Goodin Burel R.. 2019. “Could epigenetics help explain racial disparities in chronic pain?” Journal of pain research 12: 701–710. 10.2147/JPR.S191848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari Shervin, Ehsan Moazen-Zadeh Cleopatra Howard Caldwell, and Zimmerman Marc A.. 2017. “Racial Discrimination during Adolescence Predicts Mental Health Deterioration in Adulthood: Gender Differences among Blacks.” Frontiers in Public Health 5 (104). 10.3389/fpubh.2017.00104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boring Brandon L., Nanavaty Namrata, Walsh Kaitlyn T., Guzman Hanan, and Mathur Vani A.. 2021. “Daily, but not lifetime discrimination is associated with greater pain interference in those with chronic pain.” The Journal of Pain 22 (5): 599. 10.1016/j.jpain.2021.03.087. [DOI] [Google Scholar]
- Brondolo Elizabeth, Kelly Kim P., Coakley Vonetta, Gordon Tamar, Thompson Shola, Levy Erika, Cassells Andrea, Tobin Jonathan N., Sweeney Monica, and Contrada Richard J.. 2005. “The Perceived Ethnic Discrimination Questionnaire: Development and Preliminary Validation of a Community Version1.” Journal of Applied Social Psychology 35 (2): 335–365. 10.1111/j.1559-1816.2005.tb02124.x. [DOI] [Google Scholar]
- Brown Timothy T., Partanen Juulia, Chuong Linh, Villaverde Vaughn, Griffin Ann Chantal, and Mendelson Aaron. 2018. “Discrimination hurts: The effect of discrimination on the development of chronic pain.” Social Science & Medicine 204: 1–8. 10.1016/j.socscimed.2018.03.015. [DOI] [PubMed] [Google Scholar]
- Burgess Diana J., Grill Joseph, Noorbaloochi Siamak, Griffin Joan M., Ricards Jennifer, Van Ryn Michelle, and Partin Melissa R.. 2009. “The Effect of Perceived Racial Discrimination on Bodily Pain among Older African American Men.” Pain Medicine 10 (8): 1341–1352. 10.1111/j.1526-4637.2009.00742.x. 10.1111/j.1526-4637.2009.00742.x. [DOI] [PubMed] [Google Scholar]
- Carlisle SK 2015. “Perceived discrimination and chronic health in adults from nine ethnic subgroups in the USA.” Ethn Health 20 (3): 309–26. 10.1080/13557858.2014.921891. [DOI] [PubMed] [Google Scholar]
- Carter Robert T., Johnson Veronica E., Kirkinis Katherine, Roberson Katheryn, Muchow Carrie, and Galgay Corinne. 2019. “A Meta-Analytic Review of Racial Discrimination: Relationships to Health and Culture.” Race and Social Problems 11 (1): 15–32. 10.1007/s12552-018-9256-y. [DOI] [Google Scholar]
- Casey Logan S., Reisner Sari L., Findling Mary G., Blendon Robert J., Benson John M., Sayde Justin M., and Miller Carolyn. 2019. “Discrimination in the United States: Experiences of lesbian, gay, bisexual, transgender, and queer Americans.” Health Services Research 54 (S2): 1454–1466. 10.1111/1475-6773.13229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella David, Choi Seung W., Condon David M., Schalet Ben, Hays Ron D., Rothrock Nan E., Yount Susan, Cook Karon F., Gershon Richard C., Amtmann Dagmar, DeWalt Darren A., Pilkonis Paul A., Stone Arthur A., Weinfurt Kevin, and Reeve Bryce B.. 2019. “PROMIS® Adult Health Profiles: Efficient Short-Form Measures of Seven Health Domains.” Value in Health 22 (5): 537–544. 10.1016/j.jval.2019.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado-Proctor Shirley Miguelina. 1999. “The Perceived Racism Scale for Latina/os: A multidimensional assessment of the experience of racism among latina/os.” 60, ProQuest Information & Learning. [Google Scholar]
- Currie SR, & Wang J 2005. “More data on major depression as an antecedent risk factor for first onset of chronic back pain”. Psychological medicine, 35(9): 1275–1282. [DOI] [PubMed] [Google Scholar]
- IBM SPSS Statistics for Windows 26, Armonk, NY. [Google Scholar]
- Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, Kerns R, Von Korff M, Porter L, and Helmick C. 2018. “Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults - United States, 2016.” MMWR Morb Mortal Wkly Rep 67 (36): 1001–1006. 10.15585/mmwr.mm6736a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyo RA, Dworkin SF, Amtmann D, Andersson G, Borenstein D, Carragee E, Carrino J, Chou R, Cook K, Delitto A, Goertz C, Khalsa P, Loeser J, Mackey S, Panagis J, Rainville J, Tosteson T, Turk D, Von Korff M, and Weiner DK. 2015. “Report of the NIH Task Force on research standards for chronic low back pain.” Phys Ther 95 (2): e1–e18. 10.2522/ptj.2015.95.2.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong HJ, Gerdle B, Bernfort L, Levin LÅ, and Dragioti E. 2020. “Pain Catastrophizing in Older Adults with Chronic Pain: The Mediator Effect of Mood Using a Path Analysis Approach.” J Clin Med 9 (7). 10.3390/jcm9072073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugan Sheila A., Lewis Tené T., Everson-Rose Susan A, Jacobs Elizabeth A, Harlow Siobán D., and Janssen Imke. 2017. “Chronic discrimination and bodily pain in a multiethnic cohort of midlife women in the Study of Women’s Health Across the Nation.” Pain 158 (9): 1656–1665. 10.1097/j.pain.0000000000000957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw Valerie A., Rosenthal Lisa, Amy Carroll-Scott Alycia Santilli, Gilstad-Hayden Kathryn, and Ickovics Jeannette R.. 2015. “Everyday discrimination and physical health: Exploring mental health processes.” Journal of Health Psychology 21 (10): 2218–2228. 10.1177/1359105315572456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, & Buchner A (2007). G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior research methods, 39(2), 175–191. [DOI] [PubMed] [Google Scholar]
- Findling MG, Casey LS, Fryberg SA, Hafner S, Blendon RJ, Benson JM, Sayde JM, and Miller C. 2019. “Discrimination in the United States: Experiences of Native Americans.” Health Services Research 54 Suppl 2 (Suppl 2): 1431–1441. 10.1111/1475-6773.13224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia Gabriel M., David EJR, and Mapaye Joy C., 2019, “Internalized racial oppression as a moderator of the relationship between experiences of racial discrimination and mental distress among Asians and Pacific Islanders,.” Asian American Journal of Psychology. doi: 10.1037/aap0000124. [DOI] [Google Scholar]
- Greer Tawanda M., Laseter Adrian, and Asiamah David. 2009. “Gender as a Moderator of the Relation between Race-Related Stress and Mental Health Symptoms for African Americans.” Psychology of Women Quarterly 33 (3): 295–307. 10.1177/036168430903300305. [DOI] [Google Scholar]
- Güereca Yvette M., Kell Parker A., Kuhn Bethany L., Hellman Natalie, Sturycz Cassandra A., Toledo Tyler A., Huber Felicitas A., Demuth Mara, Lannon Edward W., Palit Shreela, Shadlow Joanna O., and Rhudy Jamie L.. 2022. “The Relationship Between Experienced Discrimination and Pronociceptive Processes in Native Americans: Results From the Oklahoma Study of Native American Pain Risk.” The journal of pain. 10.1016/j.jpain.2021.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall AM, Kamper SJ, Maher CG, Latimer J, Ferreira ML, & Nicholas MK 2011. “Symptoms of depression and stress mediate the effect of pain on disability.” Pain, 152(5), 1044–1051. [DOI] [PubMed] [Google Scholar]
- Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, and Piette JD. 2017. “Racial and Socioeconomic Disparities in Disabling Chronic Pain: Findings From the Health and Retirement Study.” Jourrnal of Pain 18 (12): 1459–1467. 10.1016/j.jpain.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Mansell G, McAuley JH, Kamper SJ, Hübscher M, Moseley GL, & Williams CM 2016. “Causal mechanisms in the clinical course and treatment of back pain”. Best Practice & Research Clinical Rheumatology, 30(6), 1074–1083. [DOI] [PubMed] [Google Scholar]
- Lee Randy T., Perez Amanda D., Malik Boykin C, and Mendoza-Denton Rodolfo. 2019. “On the prevalence of racial discrimination in the United States.” PLOS ONE 14 (1): e0210698. 10.1371/journal.pone.0210698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur Vani A., Kiley Kasey B., Haywood Carlton Jr., Bediako Shawn M., Lanzkron Sophie, Carroll C. Patrick, Buenaver Luis F., Pejsa Megan, Edwards Robert R., Haythornthwaite Jennifer A., and Campbell Claudia M.. 2016. “Multiple Levels of Suffering: Discrimination in Health-Care Settings is Associated With Enhanced Laboratory Pain Sensitivity in Sickle Cell Disease.” The Clinical journal of pain 32 (12): 1076–1085. 10.1097/AJP.0000000000000361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer TG, Neblett R, Cohen H, Howard KJ, Choi YH, Williams MJ, Perez Y, and Gatchel RJ. 2012. “The development and psychometric validation of the central sensitization inventory.” Pain Practice 12 (4): 276–85. 10.1111/j.1533-2500.2011.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClendon J, Essien UR, Youk A, Ibrahim SA, Vina E, Kwoh CK, and Hausmann LRM. 2021. “Cumulative Disadvantage and Disparities in Depression and Pain Among Veterans With Osteoarthritis: The Role of Perceived Discrimination.” Arthritis Care Res (Hoboken) 73 (1): 11–17. 10.1002/acr.24481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie Kwame. 2006. “Racial discrimination and mental health.” Psychiatry 5 (11): 383–387. 10.1053/j.mppsy.2006.08.002. [DOI] [Google Scholar]
- Meints SM, and Edwards RR. 2018a. “Evaluating psychosocial contributions to chronic pain outcomes.” Progress in neuro-psychopharmacology & biological psychiatry 87 (Pt B): 168–182. 10.1016/j.pnpbp.2018.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merriwether Ericka N., Wittleder Sandra, Cho Gawon, Bogan Eushavia, Thomas Rachel, Bostwick Naja, Wang Binhuan, Ravenell Joseph, and Jay Melanie. 2021. “Racial and weight discrimination associations with pain intensity and pain interference in an ethnically diverse sample of adults with obesity: a baseline analysis of the clustered randomized-controlled clinical trial the goals for eating and moving (GEM) study.” BMC Public Health 21 (1): 2201. 10.1186/s12889-021-12199-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales ME, and Yong RJ. 2021. “Racial and Ethnic Disparities in the Treatment of Chronic Pain.” Pain Med 22 (1): 75–90. 10.1093/pm/pnaa427. [DOI] [PubMed] [Google Scholar]
- Morasco Benjamin J., Lovejoy Travis I., Lu Mary, Turk Dennis C., Lewis Lynsey, and Dobscha Steven K.. 2013. “The relationship between PTSD and chronic pain: Mediating role of coping strategies and depression.” PAIN 154 (4): 609–616. 10.1016/j.pain.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neblett Randy, Cohen Howard, Choi YunHee, Hartzell Meredith M., Williams Mark, Mayer Tom G., and Gatchel Robert J.. 2013. “The Central Sensitization Inventory (CSI): Establishing Clinically Significant Values for Identifying Central Sensitivity Syndromes in an Outpatient Chronic Pain Sample.” The Journal of Pain 14 (5): 438–445. 10.1016/j.jpain.2012.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson Harvey L. 2020. “Associations Between Major and Everyday Discrimination and Self-Rated Health Among US Asians and Asian Americans.” Journal of Racial and Ethnic Health Disparities 7 (2): 262–268. 10.1007/s40615-019-00654-0. [DOI] [PubMed] [Google Scholar]
- Panza Gregory A., Puhl Rebecca M., Taylor Beth A., Zaleski Amanda L., Livingston Jill, and Pescatello Linda S.. 2019. “Links between discrimination and cardiovascular health among socially stigmatized groups: A systematic review.” PLOS ONE 14 (6): e0217623. 10.1371/journal.pone.0217623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA, Yu L, Dodds NE, Johnston KL, Maihoefer CC, and Lawrence SM. 2014. “Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS) in a three-month observational study.” Journal of Psychiatry Research 56: 112–9. 10.1016/j.jpsychires.2014.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus T, Smeets R, Simmonds M, Sullivan M 2010. “The Fear Avoidance Model Disentangled: Improving the Clinical Utility of the Fear Avoidance Model.” The Clinical Journal of Pain 26(9): 739–746, [DOI] [PubMed] [Google Scholar]
- Piontek Katharina, Apfelbacher Christian, Ketels Gesche, Brünahl Christian, and Löwe Bernd. 2020. “Depression Partially Mediates the Association of Adverse Childhood Experiences with Pain Intensity in Patients with Chronic Pelvic Pain Syndrome: Results from a Cross-Sectional Patient Survey.” Pain Medicine 22 (5): 1174–1184. 10.1093/pm/pnaa325. [DOI] [PubMed] [Google Scholar]
- Qualtrics. 2020. Provo, Utah, USA. Available at https://www.qualtrics.com
- Rahman R, Ibaseta A, Reidler JS, Andrade NS, Skolasky RL, Riley LH, Cohen DB, Sciubba DM, Kebaish KM, and Neuman BJ. 2020. “Changes in patients’ depression and anxiety associated with changes in patient-reported outcomes after spine surgery.” Journal of Neurosurgy. Spine: 1–20. 10.3171/2019.11.Spine19586. [DOI] [PubMed] [Google Scholar]
- Tappe-Theodor A, and Kuner R. 2019. “A common ground for pain and depression.” Nature Neuroscience 22 (10): 1612–1614. 10.1038/s41593-019-0499-8. [DOI] [PubMed] [Google Scholar]
- Trost Zina, Sturgeon John, Guck Adam, Ziadni Maisa, Nowlin Liza, Goodin Burel, and Scott Whitney. 2019. “Examining Injustice Appraisals in a Racially Diverse Sample of Individuals With Chronic Low Back Pain.” The journal of pain 20 (1): 83–96. 10.1016/j.jpain.2018.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Wilgen Cornelis P., Vuijk Pieter J., Kregel Jeroen, Voogt Lennard, Meeus Mira, Descheemaeker Filip, Keizer Doeke, and Nijs Jo. 2018. “Psychological Distress and Widespread Pain Contribute to the Variance of the Central Sensitization Inventory: A Cross-Sectional Study in Patients with Chronic Pain.” Pain Practice 18 (2): 239–246. 10.1111/papr.12600. [DOI] [PubMed] [Google Scholar]
- Taylor Walker Janiece L., Campbell Claudia M., Thorpe Roland J., Whitfield Keith E., Nkimbeng Manka, and Szanton Sarah L.. 2018. “Pain, Racial Discrimination, and Depressive Symptoms among African American Women.” Pain Management Nursing 19 (1): 79–87. 10.1016/j.pmn.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelaya CE, Dahlhamer JM, Lucas JW, and Connor EM. 2020. “Chronic Pain and High-impact Chronic Pain Among U.S. Adults, 2019.” NCHS Data Brief (390): 1–8. [PubMed] [Google Scholar]
- Ziadni Maisa S., Sturgeon John A., Bissell Daniel, Guck Adam, Martin Kelly J., Scott Whitney, and Trost Zina. 2020. “Injustice Appraisal, but not Pain Catastrophizing, Mediates the Relationship Between Perceived Ethnic Discrimination and Depression and Disability in Low Back Pain.” The journal of pain 21 (5–6): 582–592. 10.1016/j.jpain.2019.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


