Abstract
Objectives:
The focus of this study was to calculate and contextualize response rates for a community-based study conducted during the COVID-19 pandemic, a topic on which scant data exist, and to share lessons learned from recruiting and enrolling for implementation of future studies.
Design:
The Life+Health Study, a cross-sectional population-based study designed to advance novel methods to measure and analyze multiple forms of discrimination for population health research.
Setting:
The study recruited participants from 3 community health centers in Boston, Massachusetts, between May 2020 and July 2022.
Participants:
A total of 699 adult participants between the ages of 25 and 64 years who were born in the United States and had visited one of the health centers within the last 2 years.
Main Outcome Measures:
The response rate was calculated as follows: (number of completions + number of dropouts)/(dropouts + enrollments). To contextualize this response rate, we synthesized evidence pertaining to local COVID-19 case counts, sociopolitical events, pandemic-related restrictions and project protocol adjustments, and examples of interactions with patients.
Results:
Our study had a lower-than-expected response rate (48.4%), with the lowest rates from the community health centers serving primarily low-income patients of color. Completion rates were lower during periods of higher COVID-19 case counts. We describe contextual factors that led to challenges and lessons learned from recruiting during the pandemic, including the impact of US sociopolitical events.
Conclusions:
The Life+Health Study concluded recruitment during the pandemic with a lower-than-expected response rate, as also reported in 4 other US publications focused on the impact of COVID-19 on response rates in community-based studies. Our results provide an example of the impact of the pandemic and related US sociopolitical events on response rates that can serve as a framework for contextualizing other research conducted during the pandemic and highlight the importance of best practices in research recruitment with underserved populations.
Keywords: community health center, COVID-19, pandemic, survey response rates
Response rates are a vital aspect of study implementation and are indicators of successes in recruitment and enrollment.1 A higher response rate enables a more accurate reflection of the population that a sample is intended to represent. Although response rates are in part affected by study design,1 they can also be affected by contextual factors impacting research participation. One notable contextual candidate factor for affecting response rates is the COVID-19 pandemic, which the World Health Organization declared to be a global emergency in March 2020, leading to significant mortality, morbidity, and social and economic upheaval, including disruptions in public health research.2 Yet, as we found when seeking to contextualize response rates for a US community-based population health study designed to go into the field in March 2020, scant literature has reported on the impact of the pandemic in reporting this type of population-based health research. In our integrative review of research search using PRISMA-S extension methods,3 we could identify only 4 US observational studies of patients that reported on their response rates during the COVID-19 pandemic, none of which were conducted at community health centers (CHCs) or analyzed their response rates in relation to concurrent US sociopolitical events (see Supplemental Digital Contents 1 and 2, available at http://links.lww.com/JPHMP/B198).
In this article, we accordingly report on the COVID-19 and sociopolitical context of our study response rates among 3 diverse CHCs located in 1 US city, and our field team's assessment of contributing factors. The intent is to share lessons learned from recruiting and enrolling a diverse patient population from CHCs during the COVID-19 pandemic to inform the interpretation of results and implementation of future studies.
Methods
Contextual data: COVID-19 rates, policies, and sociopolitical events
COVID-19 data
We retrieved COVID-19 daily case counts from the Boston Public Health Commission COVID-19 Dashboard by neighborhood and wastewater data from the Massachusetts Water resources Authority Biobot Data Dashboard.4,5
COVID-19 policies and US sociopolitical events
Study staff documented local COVID-19 pandemic surges and other significant social and political events during the recruitment period in real time to help contextualize study implementation. Events were captured in list format and then sorted into thematic categories: COVID-19 Related Updates & Procedures, Sociopolitical Events, Local Implications, Project Protocol Adjustments & Progress, and Examples of Interactions with Patients.
Study implementation: recruitment and response rates
Study participants and procedures
The Life+Health Study is a cross-sectional study designed to advance novel methods to measure and analyze multiple forms of discrimination for population health research, specifically involving discrimination based on racialized group, sex, gender identity, sexual orientation, weight, and age, as experienced by working age US-born adults.6 For this study, we recruited participants from 3 partner CHCs based in Boston, Massachusetts. Fenway Health serves a high number of LGBTQ+ patients, with close to half identifying as a sexual minority (SM) and a fifth identifying as transgender or gender diverse.7 Mattapan Community Health Center (MCHC) and Harvard Street Neighborhood Health Center (HSNHC) serve patient populations comprising predominantly of people of color (POC), immigrants, and those who are underinsured, underrepresented, and economically disadvantaged.8,9 All 3 CHCs provide care regardless of patient insurance status or the ability to pay.7–9 To be eligible for participation, the patients must have visited one of the health centers within the prior 2 years of the recruitment call; be US born to ensure that participants had a comparable lifetime history of potential exposures to discrimination in the United States; and at the time of the survey be between the ages of 25 and 64 years.
Funded in June 2019, the study was designed to start recruitment in March 2020 and end in April 2022, with an anticipated response rate of 80%, based on the 82.4% response rate achieved in an earlier study conducted by members of the current team, which had recruited from our Boston CHCs in 2008-2011.10 Because of the declaration of a public health emergency in March 2020 due to the COVID-19 pandemic (Table 1), we delayed the start of recruitment until May 2020 and extended it through July 2022 (see Table, Supplemental Digital Content 3, available at http://links.lww.com/JPHMP/B199, which presents an extended table of project protocol adjustments and progress). To ensure that a sufficient number of individuals were recruited across the social groups relevant to the types of discrimination being studied (eg, POC, sexual and gender minorities), we employed stratified sampling. Patients were emailed or mailed a study invitation, offered contact information if they wanted to opt out of the follow-up call, and informed that they would receive a phone call to determine their interest and eligibility for enrollment. Potential participants were called up to 5 times, alternating between weeknights, weekdays, and weekends, and were screened via a predetermined script to determine eligibility. Once enrolled, the study protocol consisted of 2 online surveys: a self-report questionnaire administered through Qualtrics and a validated digital Brief Implicit Associations Test.11 Participants were initially compensated $25 in the form of an Amazon or grocery gift card; in November 2021, we increased the compensation to $40, in light of COVID-19 burdens and low response rates. The study was approved by the Institutional Review Board at Harvard T.H. Chan School of Public Health (IRB-18-1128).
TABLE 1. Life+Health Study Table of Examples of Contextual Factors During the Study Recruitment Period: Boston, Massachusetts, March 2020 to July 2022.
| COVID-19–Related Updates and Protocols13 | Sociopolitical Events | Local Implications | Project Protocol Adjustments and Progress | Examples of Interactions With Patients | |
|---|---|---|---|---|---|
| 2020 | US COVID-19 deaths pass the 100 00 mark. COVID-19 case numbers surge past 11 million, CDC recommends stay home for thanksgiving. FDA agrees to EUA for COVID-19 vaccine from Pfizer, BioNTech, then Moderna. |
Protests that last throughout the early months of the summer begin after the murder of George Floyd, following the deaths of Ahmaud Arbery and Breonna Taylor earlier in the year. | State of emergency declared. Governor directed all of Massachusetts' residents to stay at home and make only essential trips. Boston declared racism a public health issue.16 |
Original recruitment start time delayed. Research assistants begin making calls at Fenway Health. |
Fenway Health: distressed and distraught over the political and social times. Was really hoping to help and participate but was very consumed by the current state of the world. We spoke about hope and solidarity. |
| 2021 | CDC Director Walensky releases a statement on racism and health amid the pandemic. WHO identifies the omicron variant. Stimulus bill expands unemployment benefits, rental assistance, vaccines, child tax credits, and direct payments of up to $1400. |
HRC cites 2020 as the worst year on record for anti–trans violence/murders, and 2021 saw an increase in proposed anti-LGBTQ bills and antitransgender laws.18 Storming of the US capitol; Congress reconvenes and certifies Biden and Harris. |
Boston Public Schools move remote due to case counts.17 Boston Public Schools go full-time in-person learning starts for grades kindergarten-8th.17 All people older than 19 years become eligible for the COVID-19 vaccine in Massachusetts.19 |
First Mattapan CHC participants called. Added a local community grocery store gift card as an incentive option. First in-person participation at MCHC in outdoor computer station and The Fenway Institute. |
Harvard Street Neighborhood Health Center: currently residing in another state. Left the Boston area because a close friend passed away from COVID-19. Does not currently have access to a computer but does in Boston. |
| 2022 | Recorded deaths in the United States due to COVID-19 reach 1 million. | Ten Black people were killed and 3 others injured in a shooting at a supermarket chain in Buffalo, New York. | State programs, facilities, and personnel subject to COVID-19. Vaccination requirements must receive a COVID-19 booster vaccination.19 |
Recruitment period extended to July 2022 due to COVID-19 delays. | Mattapan Community Health Center: Refused: sick and caring for sick family members; too busy to be involved in a study. |
Abbreviations: CDC, Centers for Disease Control and Prevention; CHC, Community Health Center; EUA, Emergency Use Authorization; FDA, Food and Drug Administration; HRC, Human Rights Campaign; MCHC, Mattapan Community Health Center; WHO, World Health Organization.
Study response rates and recruitment protocols
To have adequate statistical power (≥80%, with 2-sided α < .05) to test the study hypotheses, we aimed to enroll a target number of 1092 total participants, with at least 350 per social comparison group, for categories pertaining to gender identity, racialized group, age, sexual orientation, and weight. Each week we monitored study completions concerning our target number of participants who self-identify by racialized group (White, Hispanic, Latino/Latina/Latinx, Spanish, Black or African American, Asian, American Indian or Alaska Native, Middle Eastern or North African, Native Hawaiian or Pacific Islander or some other race, ethnicity, or origin); gender identity (cis women, cis men, gender minority [GM], or transgender nonconforming [TGNC]); age (25-44 years, 45-64 years); and sexual orientation (SM or lesbian, gay, bisexual, queer [LGBQ], heterosexual). Height and weight measurements were either self-reported or obtained through medical records upon completion of the study.
Throughout recruitment, we monitored the weekly overall response rate using definition 6 from the American Association for Public Opinion Research (AAPOR)12 by calculating the following: (number of completions + number of dropouts)/(dropouts + enrollments). Guided by these data, research assistants recorded implementation-relevant information during recruitment calls, while maintaining privacy and confidentiality per institutional review board protocol, to guide future outreach, such as optimal times for future calls to the participant and other information relevant to recruiting and availability (eg, participant works overnight shifts, needs childcare coverage). As a result of these interactions, we made appropriate institutional review board–approved adjustments to the protocol, for example, in May 2021, when the data indicated that only 19% of participants identified as GM/TGNC, we prioritized their recruitment, increasing their proportion to 59.6% by September 2021.
Results
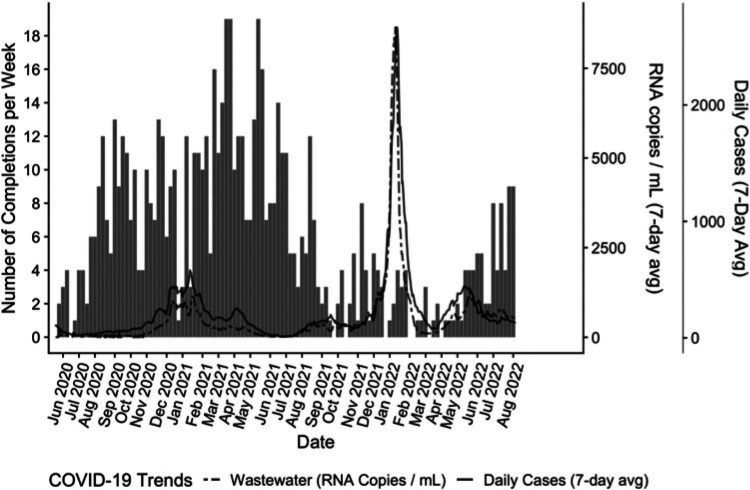
Contextualizing response rates: completions by local COVID-19 wastewater data
Our tabulation of weekly completion reports by weekly COVID-19 data indicated that completion rates declined as COVID-19 case counts climbed and wastewater levels (RNA copies/mL) increased (Figure). Boston Public Health Commission data revealed that the primary neighborhoods of our participant population served by the CHCs experienced a higher case count during variant surges than neighboring communities. For example, the primary neighborhoods served by the study's CHCs—Dorchester A (zip codes 02121, 02125), Dorchester B (zip codes 02122, 02124), and Fenway/Kenmore (zip code 02215)—had case counts more than 2000 per week during the height of the Omicron variant surge. Nearby neighborhoods, Mattapan, Roxbury, Hyde Park, Roslindale, and Jamaica Plain, whose residents are served by these CHCs, reported between 850 and 1472 cases during the same week. Other neighborhoods not served by the recruiting CHCs reported lower case counts during the Omicron surge, for example, Charlestown: 405 and South Boston: 785.4
FIGURE.
Life+Health Study completions, Wastewater, and Daily Case Trends, Boston, Massachusetts, June 2020 to August 2022a
aThe number of Life+Health Study completions reported by week juxtaposed with the counts of RNA copies detected per milliliter and COVID-19 cases by day from June 2020 to August 2022.4,5
Contextualizing response rates: sociopolitical context, pandemic and local restrictions, and study procedure adjustments
We additionally identified 4 sets of contextual conditions affecting response rates during the pandemic in our recruitment and enrollment documentation (Table 1): (1) Challenges of Remote Recruitment and Participation; (2) Respondent Burden, COVID-19, and Sociopolitical Context; (3) Equity and Tailored Outreach Strategies; and (4) Flexibility, Responsiveness, and Adaptability (Table 2).
TABLE 2. Life+Health Study: Challenges Faced and Lessons Learned in Recruitment and Enrollment at Community Health Centers During the Pandemic.
| Recruitment and Enrollment During the Pandemic | |||
|---|---|---|---|
| Challenges Faced | Lessons Learned | ||
| Remote Recruitment and Participation | Respondent Burden, COVID-19 and Sociopolitical Context | Equity and Tailored Outreach Strategies | Flexibility, Responsiveness, and Adaptability |
| Delays in study recruitment. Limited in-person participation and recruitment opportunities. Social media and Internet advertisement. |
Overstudied populations. Competing priorities (economic and health burdens). Increased exposure to discrimination. |
|
|
Challenges of remote recruitment and participation
Efforts to conduct recruitment were delayed and limited during the COVID-19 pandemic. This was largely due to CHC staff response to the public health crisis, including rapid scale-up of telehealth, demands for COVID-19 testing and care, and increased COVID-19 case tracking and reporting requirements at CHCs. Our study design required CHC staff to create a roster of potentially eligible patients from the electronic health records of all eligible patients. The CHC staff had understandably limited time for data programming and extraction, which caused delays in beginning recruitment at 1 health center until March 2021, 10 months after recruitment began at the first CHC.
Moreover, because the health centers' safety protocols restricted patient visits, patients who lacked familiarity with technology and email or had limited or unreliable Internet or computer access could not utilize study-provided computers at the CHCs from 2020 into the early months of 2021 (Table 1). Similarly, the on-site PhysioLab at the Harvard T.H. Chan School of Public Health, where we would have hosted in-person participation, was inaccessible throughout the recruitment period. Because of the study's electronic-based data capture and the complexity of survey question sets, a laptop or computer was required to complete the survey, and a tablet or smartphone could not be used. Some participants who took the surveys at home needed extensive technical assistance that research assistants provided over the phone. However, this assistance might have been more effective in person.
Because of facility closures, study staff were unable to work collaboratively in person, which increased the time required to prepare and mail study recruitment materials, impeding recruitment call efforts. Because of the limited ability to utilize clinic-based advertisement materials to recruit participants, the team focused solely on remote recruitment activities. To enhance remote recruitment efforts, we piloted social media and Internet advertisement of the study to bolster recruitment and enrollment but did not shift to this approach for 2 reasons: (a) online advertising attracted Internet bots; and (b) drew the attention of ineligible participants, increasing the burden on study staff as a result of needing to screen a number of people who were ultimately ineligible.
Respondent burden, COVID-19, and sociopolitical context
CHCs serve large numbers of underserved patients at high risk for exposure to COVID-19, imposing a competing priority to research participation. CHC patients reported experiencing significant economic impacts and other vulnerabilities due to the COVID-19 pandemic and US sociopolitical events leading to daily distress and anxiety (Table 1; see Table, Supplemental Digital Content 3, available at http://links.lww.com/JPHMP/B199, which presents an extended table of contextual factors during recruitment). Because the study required participants to report on multiple experiences of discrimination, the team recognized the need to be mindful of the potential respondent burden while recruiting from underserved patient populations during the pandemic and within the sociopolitical climate. Notable events during recruitment and enrollment included the police murder of George Floyd on May 25, 2020, and subsequent racial justice demonstrations; passage of anti-LGBT policies in numerous states; a contentious election cycle; and additionally, racially based attacks and shootings (see Table, Supplemental Digital Content 3, available at http://links.lww.com/JPHMP/B199, which presents an extended table of contextual factors during recruitment).13–21 In response to both police violence perpetrated on Black men and the inequitable impact of COVID-19 on Black, Indigenous, and People of Color, in June 2020, Boston declared racism a public health emergency, and in April 2021, the Centers for Disease Control and Prevention declared racism a public health threat nationally (Table 1). During recruitment calls, the participants remarked on their inability to remember or concentrate on the study, given this larger sociopolitical context and its direct impact on their lives. For example, in the fall of 2020, a Fenway patient unable to participate shared that they were “distressed and distraught over the political and social times,” and “very consumed by the current state of the world.”
Equity and tailored outreach strategies
A tailored outreach was needed for specific patient populations to recruit and enroll participants effectively and equitably. For example, during note-taking and real-time study team discussions, we identified the need to schedule and prioritize callbacks and reminder calls that accommodated the potential participant's unique schedules, particularly those who work nontraditional hours. This allowed us to successfully reach participants, build trust and rapport, and maintain engagement. Through conversations with participants and discussions with CHC leadership, we were also able to identify participant preferences for incentives. As a result, we implemented multiple choices for grocery cards, including a community-specific local grocery store. After many participants suggested that the original amount was insufficient compensation, we increased the incentive from $25 to $40 in November 2021. This led to more favorable reactions citing that the changed amount was a worthwhile amount of money for the time required to participate. In October 2022, with the help of MCHC and HSNHC leadership and staff, following reductions in COVID-19 rates and increases in vaccination rates, we were permitted to recruit for and conduct the study on-site at Fenway Health and MCHC. At Fenway Health, we operated out of a research office. At MCHC, we augmented an indoor study location by setting up an outdoor computer station for participants who needed assistance or access or were reluctant to participate inside. Although participants from all 3 CHCs were invited to participate in-person at either health center, we found that most in-person participants were MCHC or HSNHC patients, suggesting a higher need for in-person support in those communities.
Flexibility, responsiveness, and adaptability
Our goal was to provide as positive an experience as possible for participants in the study while minimizing unintended harm: this required flexibility, responsiveness, and adaptation in study implementation. We actively sought and welcomed feedback from participants and CHC staff on why our recruitment rates were lower than expected. Over time, we adjusted our recruitment script to emphasize the study's focus on their respective CHCs and the relevance of the patient population's experiences during this particularly challenging time. We improved screener questions to be more inclusive and all-encompassing to ensure patient-centeredness and enhance trust with potential participants. For example, during our demographic screening questions over the phone, we altered forced-choice answers to include open-ended responses regarding identity categories. This was particularly important to patients regarding race, ethnicity, and gender identity questions, 2 groups with lower engagement. We monitored completion rates for subgroups of patients and shifted efforts to strategically engage underrepresented groups via prioritizing recruitment calls.
Response rates and target completion numbers per self-identified social group
During the study's recruitment period (May 2020 to July 2022), the Life+Health Study was able to enroll 699 participants from the 3 CHCs, 64% of the target of 1092 participants.
The overall response rate for the study was 48.4%, 60.5% of the desired 80% response rate. The response rate for each health center was calculated as 61.9% at Fenway Health, 17.4% at MCHC, and 21.9% at HSNHC. Among the self-identified social group categories, 95.2% of the target count was achieved for participants younger than 44 years, and 80.6% and 80.4% of the target count for White/non-Hispanic and SM/LGBQ people, respectively. Only 32.6% of the target participants older than 45 years and 44.2% of POC completed the study (Table 3). Based on height and weight measurements (90% using medical chart data, 6% by self-report), 247 (38%) were at risk of weight-based discrimination (categorized as having a BMI of ≥30), and 400 (62%) were not at risk of weight-based discrimination (categorized as having a BMI of <30). Updated power calculations based on continuous rather than categorical variables indicate that we will have sufficient power to test our primary hypotheses, and we will report these results in our future analytic papers.
TABLE 3. Life+Health Study Response Rates and Completions, Boston, Massachusetts, 2020-2022 (n = 699).
| n = 699 | Target (n = 1092) Response Rate |
||
|---|---|---|---|
| Life+Health Study | |||
| Overall | 48.4% | ||
| Community Health Center | |||
| Fenway Health | 61.9% | ||
| Mattapan Community Health Center | 17.4% | ||
| Harvard Street Neighborhood Health Center | 21.9% | ||
| Group | Target Count, n | Total Completions, n | Target, % |
| Race and ethnicity | |||
| People of color | 500 | 221 | 44.2 |
| White, non-Hispanic | 592 | 477 | 80.6 |
| Gender identity | |||
| Cis women | 370 | 213 | 57.6 |
| Cis men | 370 | 264 | 71.4 |
| Gender minority/transgender nonconforminga | 352 | 222 | 63.1 |
| Age, y | |||
| <44 | 546 | 520 | 95.2 |
| >45 | 546 | 178 | 32.6 |
| Sexual orientation | |||
| Sexual minority/LGBQ | 598 | 481 | 80.4 |
| Heterosexual | 494 | 224 | 45.3 |
aThis group includes transgender, trans man, trans woman, genderqueer, nonbinary.
Discussion
As our results reveal, conducting a population-based study during a global pandemic both magnifies existing challenges of recruitment and enrollment and presents new ones for public health researchers, especially for studies seeking to enroll populations disproportionately impacted by the pandemic and social adversity. Despite the challenges associated with recruitment during the pandemic, the Life+Health Study enrolled 699 participants with an overall response rate of 48.4%. This response rate aligns with other population-based surveys conducted during the pandemic: (a) it is midway between the response rates of the 4 studies we reviewed (see Supplemental Digital Contents 1 and 2, available at http://links.lww.com/JPHMP/B198); (b) on par with the Massachusetts Behavioral Risk Factor Surveillance System, which reported a response rate of 48.8%22; and (c) higher than the Massachusetts Health Survey, a statewide online survey commissioned by the Blue Cross Blue Shield of Massachusetts Foundation, which reported a response rate of 6.5%.23
Suboptimal declines in response rates during the pandemic were not unique to our study.24 For example, among other national surveys, the US National Health Interview Survey reported a decrease from 60% prepandemic to 42.7%.24,25 The US Annual Social and Economic Supplement of the Current Population Survey experienced a drop in response rates from 83.2% in 2020 to 72% in 2022 and reported lower pandemic response rate among households with low income.26 Prior research has documented that lower income, lower education levels, poorer health, older age, and membership in groups subjected to racial discrimination have lower response rates27–29; to our knowledge, research is lacking on documenting how response rates vary by such contextual factors as neighborhood socioeconomic conditions, residential segregation, or access to transportation, and none of these contextual factors were discussed in the articles we identified with data on patient response rates (see Supplemental Digital Contents 1 and 2, available at http://links.lww.com/JPHMP/B198) or national survey response rates.24 In our study, lower response rates of 17.4% and 21.95% were from the 2 CHCs whose patients are primarily low-income populations of color. In contrast, Fenway Health had a response rate of 61.9%. Here, the study successfully recruited 80.4% of the target number of SM/LGBQ self-identified participants and 63.1% of the target number of self-identified GM/TGNC participants, both populations typically underrepresented in population health research (Table 3).
To our knowledge, no other studies have reported temporal associations between recruitment and COVID-19 rates. Our analyses demonstrate the utility of situating weekly completion rates in relation to neighborhood COVID-19 case rates and wastewater levels since lower completion rates strongly correlated with higher rates of these COVID-19 outcomes. Our participants reported that they were unable or less willing to complete the survey due to associated stressors consistent with higher rates and risk of COVID-19 (eg, illness, sick family members, closed schools, and financial and economic burdens) (Table 1; see Table, Supplemental Digital Content 3, available at http://links.lww.com/JPHMP/B199, which presents an extended table of contextual factors during recruitment). While CHCs played a crucial role in responding to the health needs of communities hit the hardest during the COVID-19 pandemic, temporary shutdowns, a compromised workforce, and a shift to telehealth inevitably led to delays in research study recruitment time lines and presented limitations to in-person participation.27,30–32
Given that CHC patient populations are at higher risk for exposure to COVID-19 and vulnerable to subsequent economic impacts, we were mindful of the potential burden and competing demands as contextual factors that could lead to lower engagement and participation. Respondent burden refers to the difficulty, emotional stress, and time-consuming nature of research participation on a respondent and is typically higher for social groups experiencing economic adversity and discrimination.29 Even without the pandemic, studies seeking to recruit participants from these social groups must be cognizant of addressing potential burdens and competing demands that could lead to lower engagement and participation. Furthermore, understanding mistrust of researchers due to extensive histories of researchers and medical institutions acting in untrustworthy and biased ways toward POC and low-income populations is critical.33
Notably, the recruitment period for our study coincided with national political and social upheaval involving racialized police violence, anti-LGBT policies, and other turmoil. Other studies completed during the pandemic have reported on similar strategies to respond to research fatigue, including increasing transparency, employing methods to build trust, being sensitive to previous negative research experiences, effectively communicating, and using relevant and increased incentives.29,32,34,35 Although we were mindful of the potential burden and competing demands that could lead to lower engagement and participation and altered our study recruitment protocol accordingly, it is unlikely that we—or these other studies—could have mitigated all these deterrents to successful recruitment.
Conclusion
This study of research recruitment during the COVID-19 pandemic underscores the importance of best research practices, particularly with underrepresented populations in population health research and offers practical considerations for researchers going forward. Trends of lower response rates can be expected of surveys conducted during the pandemic. Consistent with other studies, the Life+Health Study adjusted in response to the complications associated with conducting research during the COVID-19 pandemic. As supported by our findings, lower survey response rates may be found among the communities affected most by COVID-19, US sociopolitical threats, and economic adversity. Contextualizing response rates of patient populations that are often underrepresented in research within broader contextual factors, such as national health emergencies and sociopolitical events, is critical for addressing the implications of social differential in response rates, the range of exposures and outcomes observed, and interpretation of study findings.24
Implications for Policy & Practice
This study demonstrates the importance of interpreting response rates in the broader context in which the study was conducted and offers practical considerations for researchers moving forward.
Few, if any, frameworks exist for how to conduct a study during a global pandemic, which magnified existing challenges of recruitment and enrollment and presented new ones for public health researchers.
There is a need to share experiences and practices from the field in implementing research, particularly within community health center settings and with underrepresented populations in population health research.
Supplementary Material
Footnotes
The authors acknowledge, with written permission, the support for their project from the following: (a) Mattapan Community Health Center: Guale Valdez, MBA, Chief Executive Officer, and Sharon T. Callender, RN, MPH, Director, Family and Community Health Services; (b) Harvard Street Neighborhood Health Center: Tanveer Khan, MD, MHA, MPM, MSA, Interim Director and Director of Clinical Quality Improvement & Quality Assurance; and (c) The Fenway Institute: Dana J Pardee, MBA, Organizational Learning & Development Specialist (since October 2021, and, at initiation of our study, Director of Epidemiology Projects, Oct 2016-Sept 2021).
This study was supported by the National Institutes of Health (#1R01MD012793). The funding sources had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
The study protocol was approved by the institutional review board at the Harvard T.H. Chan School of Public Health (IRB 18–1128).
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (http://www.JPHMP.com).
Contributor Information
Merrily E. LeBlanc, Email: mleblanc@fenwayhealth.org.
Christian Testa, Email: ctesta@hsph.harvard.edu.
Pamela D. Waterman, Email: pwaterma@hsph.harvard.edu.
Sari L. Reisner, Email: sreisner@bwh.harvard.edu.
Jarvis T. Chen, Email: jarvis@hsph.harvard.edu.
Emry R. Breedlove, Email: ebreedlove@hsph.harvard.edu.
Farimata Mbaye, Email: fari.mbaye00@gmail.com.
Alicetonia Nwamah, Email: anwamah@college.harvard.edu.
Kenneth H. Mayer, Email: KMayer@fenwayhealth.org.
Apriani Oendari, Email: a.oendari@northeastern.edu.
Nancy Krieger, Email: nkrieger@hsph.harvard.edu.
References
- 1.Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer El, Tourangeau R. Survey Methodology. 2nd ed. Hoboken, NJ: John Wiley & Sons Inc; 2004. [Google Scholar]
- 2.World Health Organization. COVID-19 and the Social Determinants of Health and Health Equity: Evidence Brief. Geneva, Switzerland: World Health Organization. https://www.who.int/publications-detail-redirect/9789240038387. Published 2021. Accessed January 28, 2023. [Google Scholar]
- 3.Rethlefsen ML, Kirtley S, Waffenschmidt S, et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev. 2021;10(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boston COVID-19 Dashboard. COVID-19 cases. https://bphc-dashboard.shinyapps.io/BPHC-dashboard/. Published 2022. Accessed October 31, 2022.
- 5.Massachusetts Water Resources Authority. MWRA—wastewater COVID-19 tracking. https://www.mwra.com/biobot/biobotdata.htm. Published 2022. Accessed December 8, 2022.
- 6.Krieger N. Advancing novel methods to measure and analyze multiple types of discrimination for population health research, NIH/NIMHD grant number: 5R01MD012793-04. https://reporter.nih.gov/search/rLRUSEbFVkOP8KgB2b16Nw/project-details/10330589. Accessed January 31, 2023.
- 7.Fenway Health. Our patients—Fenway Health: health care is a right, not a privilege. https://fenwayhealth.org/about/our-patients/. Published December 27, 2018. Accessed November 25, 2022.
- 8.Mattapan Community Health Center. Our history—Mattapan CHC. https://www.mattapanchc.org/about/our-history. Published 2018. Accessed November 25, 2022.
- 9.Harvard Street Neighborhood Health Center. Who we are—Harvard Street Neighborhood Health Center. https://harvardstreet.org/who-we-are/. Published February 10, 2022. Accessed November 25, 2022.
- 10.Krieger N, Waterman PD, Kosheleva A, et al. Exposing racial discrimination: implicit & explicit measures—The My Body, My Story Study of 1005 US-born black & white community health center members. PLoS One. 2011;6(11):e27636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marini M, Waterman PD, Breedlove E, et al. The target/perpetrator brief-implicit association test (B-IAT): an implicit instrument for efficiently measuring discrimination based on race/ethnicity, sex, gender identity, sexual orientation, weight, and age. BMC Public Health. 2021;21(1):158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Association for Public Opinion Research. Standard Definitions Final Dispositions of Case Codes and Outcome Rates for Surveys. Alexandria, VA: American Association for Public Opinion Research; 2016:81. https://www-archive.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf. Accessed November 22, 2022. [Google Scholar]
- 13.David J. Sencer CDC museum: In: Association With the Smithsonian Institution. Atlanta, GA: Centers for Disease Control and Prevention. https://www.cdc.gov/museum/timeline/covid19.html. Published August 16, 2022. Accessed January 26, 2023. [Google Scholar]
- 14.Mass.gov. COVID-19 state of emergency. https://www.mass.gov/info-details/covid-19-state-of-emergency. Published 2023. Accessed January 29, 2023.
- 15.Fenway Health. Trump administration revokes non-discrimination provisions in health care that protected sexual and gender minorities—Fenway Health: health care is a right, not a privilege. https://fenwayhealth.org/trump-administration-revokes-non-discrimination-provisions-in-health-care-that-protected-sexual-and-gender-minorities/. Published June 12, 2020. Accessed January 28, 2023.
- 16.City of Boston. Racism: a public health crisis. https://www.boston.gov/government/cabinets/boston-public-health-commission/racial-justice-and-health-equity/racism-public-health-crisis. Published February 19, 2021. Accessed January 29, 2023.
- 17.Boston Public Schools. Highlights from 2020-2021. https://www.bostonpublicschools.org/cms/lib/MA01906464/Centricity/Domain/162/Highlights%20from%20202021.pdf. Published 2021. Accessed February 22, 2023.
- 18.Human Rights Campaign. Fatal violence against transgender and gender non-conforming people in the United States in 2021. https://reports.hrc.org/an-epidemic-of-violence-fatal-violence-against-transgender-and-gender-non-confirming-people-in-the-united-states-in-2021. Published 2022. Accessed January 28, 2023.
- 19.Mass.gov. Massachusetts' COVID-19 vaccination phases. https://www.mass.gov/info-details/massachusetts-covid-19-vaccination-phases. Published 2023. Accessed January 29, 2023.
- 20.US News. Timeline of events since George Floyd's arrest and murder. https://www.usnews.com/news/us/articles/2022-10-23/timeline-of-events-since-george-floyds-arrest-and-murder. Published October 23, 2022. Accessed January 28, 2023.
- 21.Krieger N. ENOUGH: COVID-19, structural racism, police brutality, plutocracy, climate change-and time for health justice, democratic governance, and an equitable, sustainable future. Am J Public Health. 2020;110(11):1620–1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System 2020 Summary Data Quality Report. Atlanta, GA: Centers for Disease Control and Prevention; 2021. https://www.cdc.gov/brfss/annual_data/2020/pdf/2020-sdqr-508.pdf. Published August 2, 2021. Accessed November 14, 2022. [Google Scholar]
- 23.Massachusetts Foundation. Behavioral Health During the First Year of the COVID-19 Pandemic: An Update on Need and Access in Massachusetts 2020/2021. Boston, MA: Blue Cross Blue Shield of Massachusetts Foundation. https://www.bluecrossmafoundation.org/publication/behavioral-health-during-first-year-covid-19-pandemic-update-need-and-access-0. Published February 2022. Accessed December 11, 2022. [Google Scholar]
- 24.Krieger N, LeBlanc M, Waterman PD, Reisner SL, Testa C, Chen JT. Declining survey response rates in the time of COVID-19: implications for analyses of population health and health inequities [published online ahead of print April 6, 2023]. Am J Public Health. 2023;113(6):667–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Center for Health Statistics. 2020 National Health Interview Survey, Survey Description. Atlanta, GA: Centers for Disease Control and Prevention; 2021. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2020/srvydesc-508.pdf. Accessed November 14, 2022. [Google Scholar]
- 26.United States Census Bureau. How has the pandemic continued to affect survey response? Using administrative data to evaluate nonresponse in the 2022 current population survey annual social and economic supplement. https://www.census.gov/newsroom/blogs/research-matters/2022/09/how-did-the-pandemic-affect-survey-response.html. Published 2022. Accessed September 13, 2022.
- 27.Sheldon H. Increasing Response Rates Amongst Black and Minority Ethnic and Seldom Heard Groups. Oxford, England: Picker Institute; 2007. https://nhssurveys.org/Filestore/documents/Increasing_response_rates_stakeholder_consultation_v6.pdf. Accessed April 20, 2023. [Google Scholar]
- 28.Hathaway CA, Chavez MN, Kadono M, et al. Improving electronic survey response rates among cancer center patients during the COVID-19 pandemic: mixed methods pilot study. JMIR Cancer. 2021;7(3):e30265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prusaczyk B. Remote research hinders recruitment of a diverse sample. Narrat Inq Bioeth. 2021;11(1):37–38. [DOI] [PubMed] [Google Scholar]
- 30.Villarosa AR, Ramjan LM, Maneze D, George A. Conducting population health research during the COVID-19 pandemic: impacts and recommendations. Sustainability. 2021;13(6):3320. [Google Scholar]
- 31.Kaiser Family Foundation. Impact of coronavirus on community health centers. https://www.kff.org/coronavirus-covid-19/issue-brief/impact-of-coronavirus-on-community-health-centers/. Published May 20, 2020. Accessed November 18, 2022.
- 32.Patel SS, Webster RK, Greenberg N, Weston D, Brooks SK. Research fatigue in COVID-19 pandemic and post-disaster research: causes, consequences and recommendations. Disaster Prev Manag Int J. 2020;29(4):445–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper LA, Crews DC. COVID-19, racism, and the pursuit of health care and research worthy of trust. J Clin Invest. 2020;130(10):5033–5035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brody AA, Convery KA, Kline DM, Fink RM, Fischer SM. Transitioning to remote recruitment and intervention: a tale of two palliative care research studies enrolling underserved populations during COVID-19. J Pain Symptom Manage. 2022;63(1):151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim NH, Wilson N, Mashburn T, et al. Lessons learned recruiting a diverse sample of rural study participants during the COVID-19 pandemic. Int J Drug Policy. 2021;97:103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.