Abstract
Objective:
To assess which potential future outcomes are most important to parents of children with bronchopulmonary dysplasia (BPD), a disease that affects future respiratory, medical, and developmental outcomes for children born preterm.
Study Design:
We recruited parents from two children’s hospitals’ neonatal follow-up clinics and elicited their importance rating for 20 different potential future outcomes associated with BPD. These outcomes were identified and selected through a literature review and discussions with panels of parents and clinician stakeholders, via a discrete choice experiment.
Results:
One hundred and five parents participated. Overall, parents ranked “Will my child be more vulnerable to other problems because of having lung disease?” as the most important outcome, with other respiratory health related outcomes also highly ranked. Outcomes related to child development and effects on the family were among the lowest ranked. Individually, parents rated outcomes differently, resulting in a broad distribution of importance scores for many of the outcomes.
Conclusions:
The overall rankings suggest that parents prioritize future outcomes related to physical health and safety. Notably, for guiding research, some top-rated outcomes are not traditionally measured in outcome studies. For guiding individual counseling, the broad distribution of importance scores for many outcomes highlights the extent to which parents differ in their prioritization of outcomes.
Keywords: ethics/bioethics, neonatology, pulmonology
Bronchopulmonary dysplasia (BPD) is the most common chronic morbidity of preterm birth, with an incidence of nearly 10,000 neonates per year in the United States.[1,2] As advances in neonatal medicine improve survival, researchers and clinicians must increasingly consider medium- and long-term outcomes for infants with this complex disease.[3] Information about potential future outcomes shapes how parents envision their child’s future, influencing their medical decisions. BPD affects not only respiratory outcomes but also other medical and neurodevelopmental outcomes ranging from vision impairment[4] to difficulty with activities of daily living[5] to poor school performance.[6] In defining severity and evaluating therapies for BPD, researchers must choose among many possible outcomes. Outcomes must have scientific (e.g. be sensitive and stable) and practical (e.g. measurable within study duration) validity. Researchers have flexibility in choosing among various measurable outcomes. There is no consensus on which to select.[3] Clinicians similarly have flexibility in the outcomes they prioritize in counseling parents, but they are limited to the information produced by research.
The choice of which outcomes to measure is subjective and value laden. Historically, researchers chose feasible and valid outcomes based on research precedents and their own perception of importance.[7,8] Parents and other professionals, such as nurses, psychologists, and ethicists, have largely been excluded from outcome selection.[3,7] Even instruments intended to measure quality of life often lack the perspective of patients and families.[9] The very concept of an “outcome” may hold different meaning for a physician and parent.[7] However, parents’ perspective is important—perhaps primary. There is growing awareness that the outcomes physicians deem important are often not the information parents in the neonatal intensive care unit (NICU) most value, what we term parent-important outcomes.[7,10,11] A recent systematic review of qualitative NICU studies found a significant difference in the outcomes discussed by parents and healthcare professionals.[5] There is also growing evidence that qualitative and patient-reported measures, for example “being happy,” are valid, sensitive outcomes.[12] Researchers face the difficult task of choosing among numerous routinely studied and novel outcomes, with little parent-centered evidence to guide prioritization.
Our objective was to ask parents which potential future outcomes for infants with BPD are most important to them. In this context, we use the word “outcome” to indicate broad domains of concern about the future, many of which may correspond to several possible concrete outcome measures. We use a discrete choice experiment (DCE), a quantitative choice-based strategy that enables discrimination between many items, all of which are expected to be important.[13,14]
METHODS
Study Design
We conducted a cross sectional assessment of parents’ priorities regarding the importance of 20 different potential future outcomes associated with BPD. Parents were recruited from the NICU follow up clinics of two tertiary children’s hospitals, Children’s Hospital of Philadelphia (CHOP) and Nationwide Children’s Hospital.
We curated a list of medium- to long-term outcomes associated with BPD, defined as outcomes occurring months to years after NICU discharge, then refined it with panels of parents and clinicians. To create the list, one investigator (K.P.C.) systematically reviewed two sources: (1) the most-cited BPD research studies and (2) neurodevelopmental and parent-assessment measures cited in BPD research. To extract outcomes from research studies, she performed a librarian-assisted literature search in Scopus, which facilitates ranking by number of citing papers. This approach ensured inclusion of the most prominent research in this field and thus the outcomes that are prioritized by the research community. She searched using the following title keywords: “bronchopulmonary dysplasia” OR “chronic lung” AND neonat* OR newborn* OR infant* and limited results the past five years. One investigator (K.P.C.) then reviewed the 100 papers with the highest number of citations by title and abstract. If they were likely to include qualifying outcomes, she reviewed the full text to extract outcomes. If the study cited a neurodevelopmental assessment or parent report measures, she also reviewed these measures directly for additional outcomes, resulting in review of: The Bayley Scales of Infant and Toddler Development (version 4), PedsQL™, Brief Infant and Toddler Social and Emotional Assessment, Child Behavior Checklist, Adaptive Behavior Assessment System, and Brief Developmental Assessment. Finally, she added unique outcomes from the qualitative literature, which was facilitated by a published systematic review of qualitative research on parent perceptions following neonatal care.[5] She additionally reviewed all articles that cited this systematic review as a way to screen more recent literature.
Next, one investigator (K.P.C.) led two panel meetings, the first with four prior NICU parents and the second with six interdisciplinary clinician stakeholders, including neonatologists, clinical trialists, ethicists, a pediatric pulmonologist, and a psychologist. Parents were purposively sampled from an existing family advisory group. We selected for parents of varied race and educational level to increase the diversity of perspectives. Panels systematically reviewed, refined, consolidated, and added to the outcome list, and—using simple cognitive interviewing prompts—reviewed the final list to ensure each outcome was stated in a way that was comprehensible.[15] After discussion with both panels, we decided to exclude death as an outcome. Though death competes with other outcomes of interest, all other outcomes are predicated upon a child’s survival, making death inherently non-equivalent. This creates challenges in the administration and interpretation of DCE, which yields rankings of relative importance. We also decided to phrase outcomes as questions for several reasons: (1) the parent panel felt this phrasing was most comprehensible to parents with varying familiarity with medical research, (2) from parents’ perspective, they are seeking information to address questions and concerns they have about their child’s future, and (3) questions enabled us to examine parental preferences regarding different outcomes without setting thresholds or dichotomies based on value judgments.
The final list of outcomes was incorporated into a DCE questionnaire, which presents participants with multiple small subsets of attributes, in this case 20 sets of three outcomes, and asks them to pick the most and least important from each set (Figure 1, available at www.jpeds.com). The final DCE was piloted by five panelists, including three parents, and revised accordingly. The DCE was housed in Lighthouse Studio (Version 9.14.2, Sawtooth Software, Provo, UT), which is a cloud-based survey platform. Sample size estimation for DCE is typically based on simulation studies and precedent. Data from a previous DCE with parents of children with serious illness at CHOP suggest sample sizes as low as 20 yielded stable results.[16] Most DCE studies include roughly 100 participants,[17] so we opted for a target of 100.
Figure 1—
(online only) How questions display to participants in the discrete choice experiment. This figure displays a sample question as participants would have seen it.
We collected, through parent report, the child’s chronologic age and sex and the parent’s relationship to the child, race, ethnicity, educational level, marital status, employment status, and type of health insurance. Information about both diaper and food insecurity (having insufficient funds to access these resources) were also obtained via validated self-report questions with the intention of elucidating whether resource stressors changed parents’ priorities.[18] Parents who reported diaper or food insecurity were referred to appropriate supportive resources in follow up clinic.
Parents (biological, adoptive, and foster parents) were eligible if they spoke English and had a child who had been hospitalized in the NICU for prematurity and diagnosed with BPD, defined as requiring oxygen or other respiratory support at 36 weeks postmenstrual age.[19] A research coordinator screened the clinic schedule for eligible participants and approached parents while they were waiting or before or between components of their routine appointment. Parents were encouraged to complete the questionnaire during their time in clinic but were also offered the option of completing it later from home. The study team followed up with consented participants who had not yet completed the questionnaire 1 and 2 weeks later. Participants were compensated with a $20 gift card. This study received Institutional Review Board exemption from CHOP and Nationwide Children’s Hospital.
Statistical Analysis
Lighthouse Studio incorporated participants’ choices across the numerous sets of outcomes to calculate importance scores for each outcome using a hierarchical Bayesian application of multinomial logistic regression. The output of this analysis was relative importance scores on a 0 to 100 scale, where the total importance of all outcomes sums to 100 (an outcome scored 10 is perceived as twice as important as one scored 5[16]). We exported all data to Stata, version 17.1 (StataCorp, College Station, TX) and ranked outcomes by importance scores. We also calculated and graphed the interquartile range and outliers to explore variation in respondents’ preferences. We performed stratified analyses by institution, child’s age, and food and/or diaper insecurity. We performed descriptive statistics for demographic data for the full sample and by institution.
RESULTS
The final DCE questionnaire contained 20 potential future outcomes of BPD phrased as questions (Table 1). Two outcomes added from the parent panel were not found in the literature. One hundred and five parents of 92 children completed the DCE questionnaire. In most cases, only one parent attended the appointment and was available for enrollment. Only two parents declined to participate, representing a 98% participation rate. Most participating parents (Table 2) were mothers (74%) and self-reported as either White (54%) or Black (33%). A minority of families sometimes or often experienced diaper insecurity (17%) and food insecurity (13%). Most children of participants were either <1 year of age (44%) or 1 to 2 years of age (24%). On average, parents rated their child’s overall health 4.2 on a 5-point Likert scale ranging from poor to excellent. Compared with the Nationwide sample, the sample at CHOP included more parents who identified as Black (50% versus 15%, p=0.001), fewer children under one year of age (27% versus 62%, p<0.001), and more families who sometimes or often experienced diaper insecurity (21% versus 12%, p=0.012).
Table 1—
Full outcome list
| Outcome Question | Source |
|---|---|
| Will my child need technology to help with breathing (e.g. oxygen, tracheostomy)? | Literature, Qualitative |
| Will my child have trouble with breathing (e.g. wheezing)? | Literature, Qualitative |
| Will my child need to be hospitalized frequently? | Literature, Qualitative |
| Will my child need a nurse or other extra people at home to help care for him/her? | Clinician Panel |
| Will my child be safe at home given his/her medical needs? | Parent Panel |
| Will my child have trouble seeing? | Literature, Qualitative |
| Will my child have trouble hearing? | Literature, Qualitative |
| Will my child have trouble eating and growing? | Literature, Qualitative |
| Will my child be more vulnerable to other problems because of having lung disease? | Parent Panel |
| Will my child have trouble communicating? | Literature, Neurodevelopmental Assessment, Qualitative |
| Will my child have trouble performing everyday activities (e.g. getting dressed)? | Literature, Neurodevelopmental Assessment, Qualitative |
| Will my child have trouble making friends? | Literature, Neurodevelopmental Assessment, Qualitative |
| Will my child have trouble learning in school? | Literature, Neurodevelopmental Assessment, Qualitative |
| Will my child have trouble with behavior? | Literature, Neurodevelopmental Assessment, Qualitative |
| Will my child have trouble with moving and getting around? | Literature, Neurodevelopmental Assessment, Qualitative |
| Will my child have trouble with pain? | Qualitative |
| Will my child be happy? | Qualitative, Neurodevelopmental Assessment |
| Will my family have trouble with everyday activities as a result of caring for my child? | Neurodevelopmental Assessment, Qualitative |
| Will my family experience Financial trouble as a result of caring for my child? | Qualitative |
| Will my family experience family or personal conflict as a result of caring for my child? | Neurodevelopmental Assessment, Qualitative |
Table 2—
Demographic characteristics
| Parental Respondent Characteristics | All Parents (%, N=105) | Hospital | P value | |
|---|---|---|---|---|
| CHOP (%, n=53) | Nationwide (%, n=52) | |||
| Relationship | ||||
| Mother | 74 | 71 | 77 | 0.10 |
| Father | 23 | 29 | 17 | |
| Other caregiver | 3 | 0 | 6 | |
| Education level | ||||
| Grade school | 4 | 6 | 2 | 0.16 |
| High school | 36 | 27 | 44 | |
| College | 45 | 54 | 37 | |
| Graduate degree | 15 | 13 | 17 | |
| Employment | ||||
| Employed | 66 | 71 | 62 | 0.30 |
| Unemployed | 34 | 29 | 38 | |
| Insurance type | ||||
| Medicaid | 44 | 40 | 48 | 0.35 |
| Other government | 9 | 12 | 6 | |
| Private or employer | 44 | 42 | 46 | |
| None | 1 | 2 | 0 | |
| Not sure | 2 | 4 | 0 | |
| Race | ||||
| American Indian or Alaska Native | 0 | 0 | 0 | 0.001 |
| Asian | 9 | 10 | 8 | |
| Black or African American | 33 | 50 | 15 | |
| Pacific Islander | 0 | 0 | 0 | |
| White | 54 | 38 | 69 | |
| Mixed race or other | 5 | 2 | 8 | |
| Ethnicity | ||||
| Hispanic | 4 | 6 | 2 | 0.31 |
| Not Hispanic | 96 | 94 | 98 | |
| Marital status | ||||
| Married or partnered | 63 | 58 | 67 | 0.31 |
| Single | 38 | 42 | 33 | |
| Divorced or separated | 0 | 0 | 0 | |
| Widowed | 0 | 0 | 0 | |
| Child’s gender | ||||
| Female | 40 | 40 | 40 | 0.60 |
| Male | 59 | 60 | 58 | |
| Nonbinary or other | 1 | 0 | 2 | |
| Child’s age | ||||
| <1 year | 44 | 27 | 62 | <0.001 |
| 1 year | 24 | 23 | 25 | |
| 2 years | 15 | 17 | 13 | |
| 3 years | 1 | 2 | 0 | |
| 4 years | 5 | 10 | 0 | |
| ≥5 years | 11 | 21 | 0 | |
| Mean rating of child’s health (5-point Likert scale) | 4.2 | 4.3 | 4.2 | 0.52 |
| Diaper insecurity | ||||
| Often | 8 | 6 | 10 | 0.012 |
| Sometimes | 9 | 15 | 2 | |
| Never | 80 | 71 | 88 | |
| Don’t use diapers | 4 | 8 | 0 | |
| Food insecurity | ||||
| Often | 2 | 2 | 2 | 0.63 |
| Sometimes | 11 | 13 | 8 | |
| Never | 88 | 85 | 90 | |
Average Outcome Importance Scores and Ranking
Parents ranked “Will my child be more vulnerable to other problems because of having lung disease?”, which was an outcome added during the parent panel, as most important (Figure 2; mean=10.3, 95% confidence interval [CI]=9.8–10.8). Trouble with breathing (mean=9.9, 95% CI=9.4–10.5) and needing respiratory technology (mean=7.9, 95% CI=7.3–8.5) ranked second and third, respectively. The lowest ranked outcomes were “Will my child have trouble making friends?” (mean=0.8, 95% CI=0.6–1.0), “Will my family experience family or personal conflict as a result of caring for my child?” (mean=1.7, 95% CI=1.3–2.1), and “Will my child have trouble with behavior?” (mean=2.1, 95% CI=1.6–2.5). In terms of relative importance, parents rated “Will my child be more vulnerable to other problems because of having lung disease?” as being twice as important as “Will my child have trouble communicating?” (mean=5.1, 95% CI=4.5–5.6) and over ten times as important as “Will my child have trouble making friends?”
Figure 2—
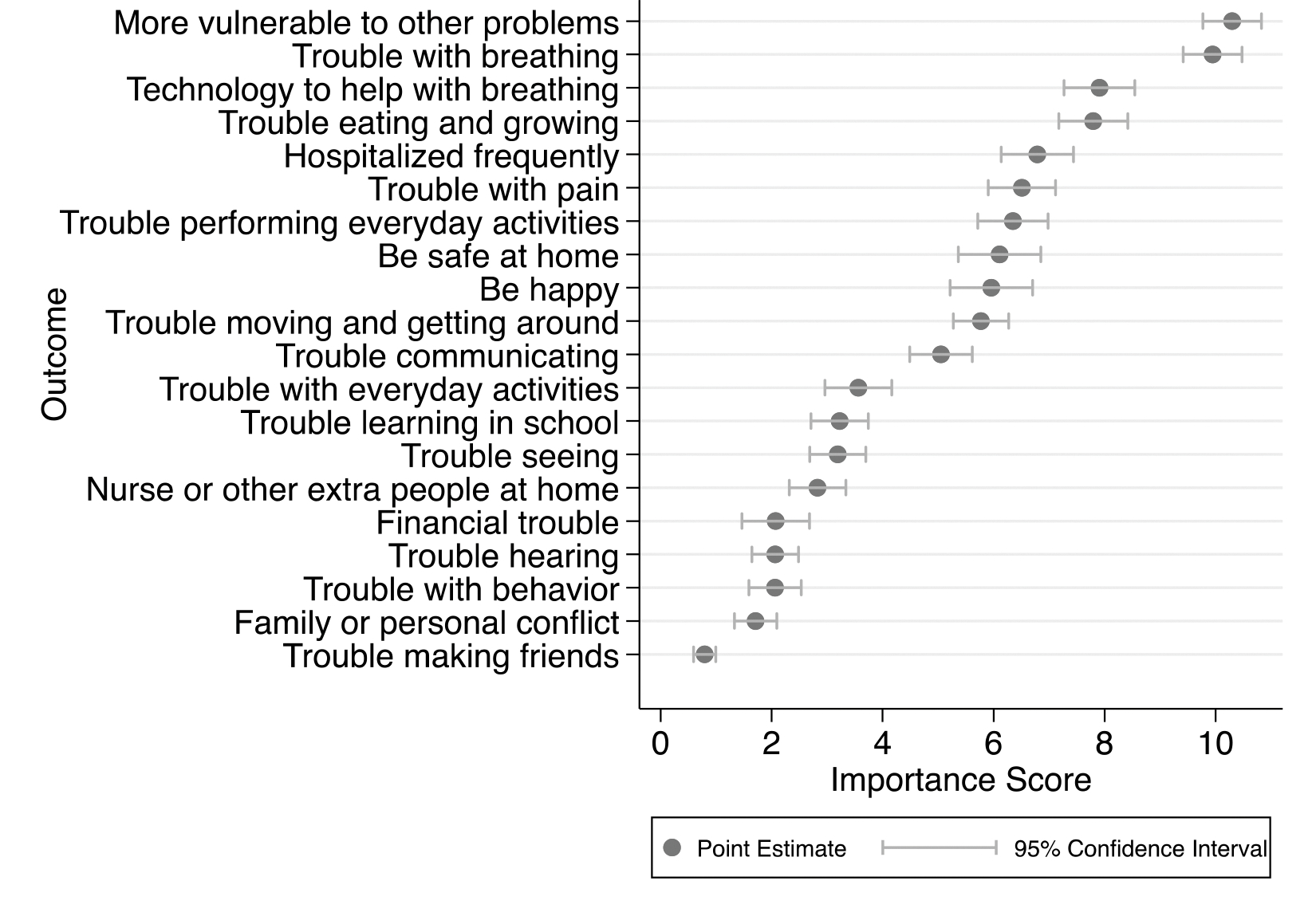
Average Importance Scores Across Respondents.
This figure contains the point estimates of the mean importance score for each outcome. The 95% CI around each point estimate represents our level of confidence that the interval captures the true point estimate.
Stratified analyses were most notable for consistency of rankings across hospitals, child’s age, and presence/absence of food and diaper insecurity (Figure 3, available at www.jpeds.com). Parents of children who were 1 year or older ranked outcomes related to development, such as trouble learning in school, higher and ranked being safe at home lower than parents of younger children. Parents who reported food and/or diaper insecurity placed greater importance on family-centered outcomes, such as family or personal conflict.
Figure 3—
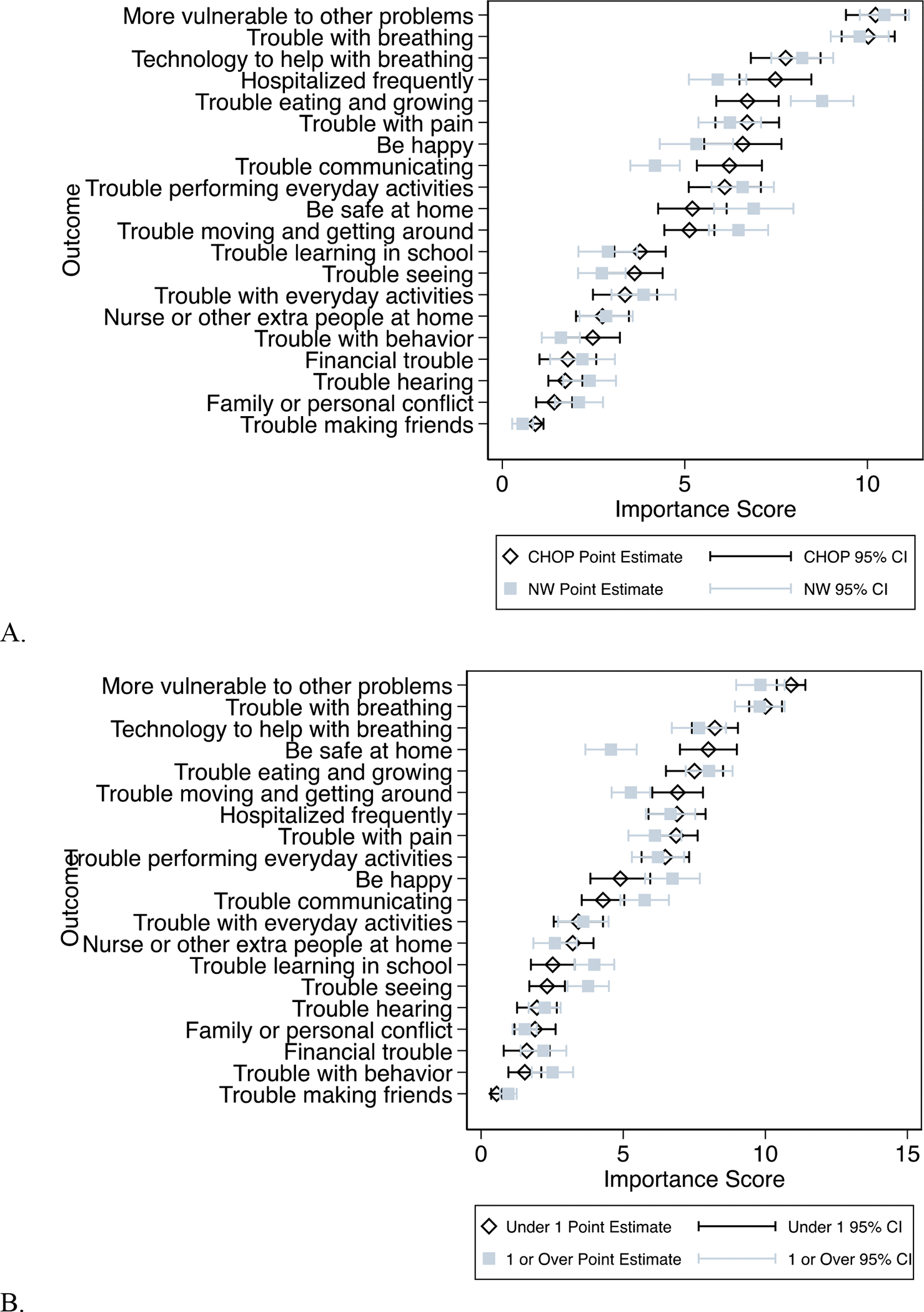
(online only) Importance Scores Stratified by Hospital, Child’s Age, and Diaper/Food Insecurity.
This figure contains the point estimates of the mean importance score for each outcome by stratified group. The 95% CI around each point estimate represents our level of confidence that the interval captures the true point estimate. Panel A is stratified by institution. Panel B is stratified by age (under 1 year versus 1 year or older). Panel C is stratified by resource insecurity (food and diaper security versus food and/or diaper insecurity). CHOP= Children’s Hospital of Philadelphia; NW= Nationwide Children’s Hospital.
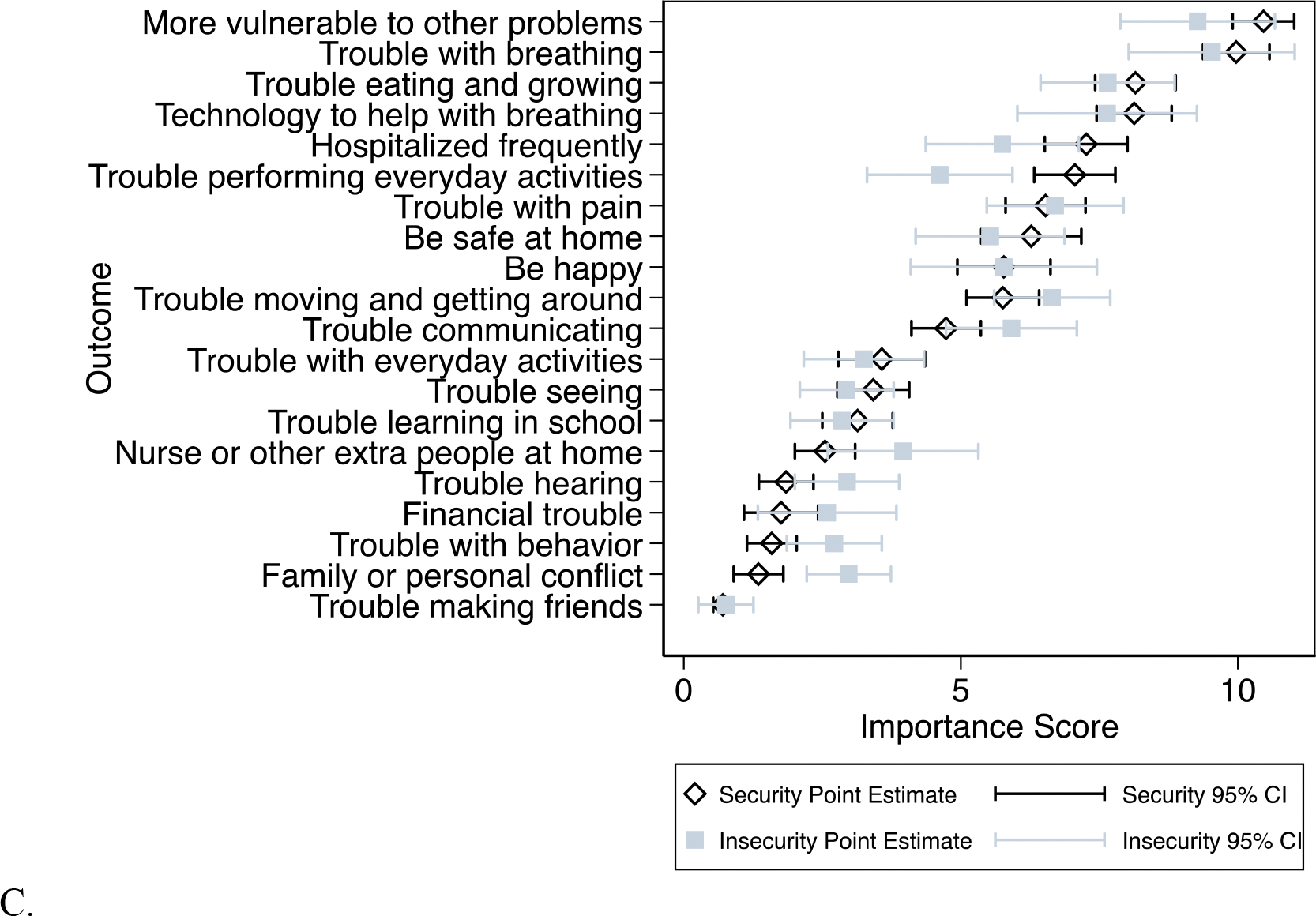
Individual-Level Variation in Outcome Importance Scores and Ranking
Although the mean score for each outcome provided an overall measure of its importance to parents, individual parents rated the outcomes differently, resulting in a broad distribution for many outcomes (Figure 4). Some outcomes were marked by greater variation in their importance across the group, and this did not clearly correlate with the overall importance of the outcome. For example, “Will my child have trouble eating and growing?” was of high importance and had a large distribution (mean=8.7, 95% CI=5.3–10.6), while “Will my family experience family or personal conflict as a result of caring for my child?” was assigned low importance and had a relatively small distribution (mean=0.8, 95% CI=0.3–2.3), yet some parents ranked it of much higher importance (outlier at 8.6).
Figure 4—
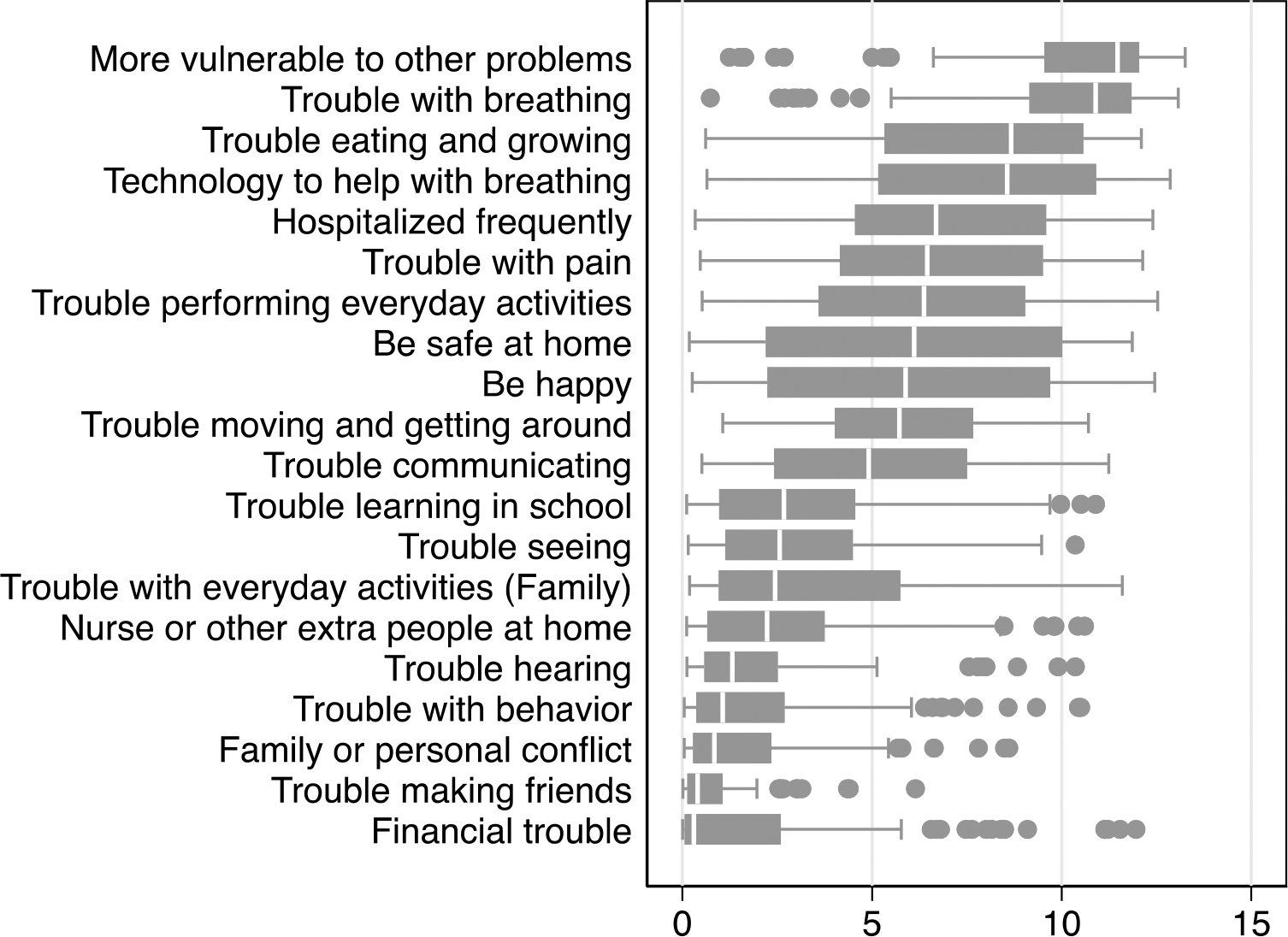
Individual-Level Variation Across Outcome Importance Scores.
This graph presents the interquartile range of outcomes, which represents the spread of the middle half of the scores in each outcome. The line within each box represents the median, the left edge of the box represents the 25th percentile, and the right edge represents the 75th percentile of scores. The whiskers extending out of the box represents minimum and maximum scores, except for outliers (more than 1.5 interquartile range beyond the 25th and 75th quartiles), which are represented with point markers.
DISCUSSION
As clinicians who take care of ill neonates and researchers who study BPD, we have a duty to provide parents with the information about the future that is most important for their decision making and preparation. BPD is a serious disease which impacts many potential future outcomes that parents may care about. As a first step toward providing parents the information they want, we evaluated the relative importance of wide-ranging medium- and long-term outcomes of BPD. The outcomes included represent broad domains of concern about the future, many of which correspond to several possible study measures. We viewed this as necessary preliminary work to identify high priority domains for creating pragmatic, concrete measures that align with parents’ priorities. DCE enabled us to build off prior work documenting many outcomes that parents may care about[5,11,20] to rank the relative importance of outcomes. Strengths of our study include the incorporation of multiple stakeholders into its design and several features indicating generalizability: high response rate, diversity of participants, and consistency of findings between hospitals with varied demographic characteristics.
Several aspects of parents’ importance rankings warrant mention. First, the ranking suggests that, overall, parents prioritize outcomes related to physical health and safety—such as those related to breathing and eating—above outcomes that reflect development. The low ranking of outcomes associated with development aligns with prior work demonstrating that parents in the NICU are more accepting of disability than neonatologists.[21] The top ranked outcome, vulnerability to other problems, is also consistent with this mindset, suggesting that parents are worried about both threats they know of and those that may arise in the future. This fear is not surprising since all parents of critically ill neonates likely experience repeated trauma and loss of control, a feeling of “waiting for the other shoe to drop.”[22–25] Parents of children with BPD may be particularly primed to focus on acute physical health because all children with this disease have been critically ill and many face ongoing physical health challenges. Breathing is vital to survival. Even compared with other complications of prematurity such as neurologic complications, parents facing BPD may therefore be particularly focused on physical health. Though we do not include death as an outcome in this study, parents seem to prioritize outcomes they might associate with death. That this focus persists even years beyond discharge is notable. Stratified analysis, even among our relatively young sample, does however suggest that developmental outcomes may gain importance over time, perhaps as parents recover from NICU trauma and developmental and behavioral problems emerge. Further work will be needed to assess how parents’ priorities evolve as children grow up. The prioritization of parents’ perspective at different time points, or even eventually the perspective of children born preterm themselves, is itself value-laden and an intriguing area for further investigation.
Second, the ranking highlights shortcomings of the way outcomes have been prioritized and categorized in research on BPD and prematurity more generally. To begin, the top ranked outcome, vulnerability to other problems, was added during the parent panel but is not traditionally measured in research. Further work would be needed to turn this concept into a reliable, reproducible research outcome, but its importance to parents indicates that such work would be worthwhile. The overall ranking also highlights the extent to which research clusters outcomes of disparate importance to parents. Outcomes included in measures of “quality of life” are dispersed across the ranking. Other researchers and ethicists have questioned whether the constellation of attributes traditionally combined into measures of “quality of life” are a meaningful representation of pediatric patients’ and families’ lived experience, and our findings add evidence to such questioning.[7,9] The rankings suggest that parents prioritize feeling that their child is nourished and growing, happy and pain free, and safe at home while they are more willing to accept problems with behavior, learning, or making friends. The composite outcome of “intact survival,” which traditionally includes medical and neurosensory sequelae, also includes outcomes of varied parent-importance. This supports ongoing skepticism about whether this composite outcome is meaningful to parents.[7,26] Collectively, these results call for greater collaboration with parents throughout the research process to improve alignment between the information parents value most and the information researchers collect and report.
Third, the large variation associated with many outcomes highlights the extent to which parents differ in their priorities based on individual values or, as highlighted by stratified analyses, demographic characteristics. There is no single answer as to which outcomes parents care most about. While we hope to draw attention to outcomes parents overall rank as important and which researchers may wish to prioritize, we also hope this will serve as a reminder to assess the individual goals, values, and preferences of each family in tailoring both counseling and care.
We acknowledge limitations of our study design in interpreting these findings. The nature of a discrete choice experiment is that it forces participants to distinguish between many attributes, all of which may be important. Low-ranking attributes are not necessarily of low importance but instead of relatively lower importance. Accordingly, their low ranking does not obviate the need to study or counsel based on these outcomes. For instance, outcomes that capture the potential effects of a sick child on family members, such as interpersonal conflict and having a nurse at home, are ranked relatively low. This is, perhaps, not surprising since “putting my child’s needs above my own when making medical care decisions” ranks relatively high among the list of attributes making parents feel like “good parents.”[13] Nevertheless, we know from other research and clinical experience that having a sick child has important impacts on families.[27,28] This may be particularly true for subgroups such as parents who experience resource limitation, as is supported by our stratified analysis. Yet, some outcomes must be prioritized over others for research, and the consistency of rankings overall, across demographic and geographic context, can help guide this prioritization. An additional limitation of a discrete choice experiments is that rankings are limited to the outcomes included initially. Soliciting outcomes from a larger group of parents or in a more systematic way may have yielded additional outcomes, and that a parent-prompted outcome rose to the top of prioritization emphasizes the extent to which this could change the rankings. Despite these limitations, we believe the rankings reveal important truths about parents’ experiences that are important for clinicians to understand and incorporate into research and practice.
Another limitation of our study is that participants may be skewed to assign importance to medical outcomes for several reasons. First, the questionnaire was administered in a healthcare context, so parents may have been primed to prioritize the outcomes they believe healthcare can address. However, that this fully explains the focus on physical health and safety seems unlikely, particularly since neonatal follow-up clinic visits place at least equal focus on developmental needs. Parents who present for elective follow-up visits may even be skewed toward those who prioritize developmental needs. Second, the children of participants were relatively young, with over 80% under age 3, which, as mentioned above, may skew them to prioritize medical outcomes. Third, this study only includes parents of children who survived despite BPD, perhaps those who opted for continued invasive care even when developmental disabilities were likely. The participating centers are tertiary referral centers which often draw parents who wish to continue invasive care despite severe disease or complications. Finally, excluding patients who do not meet traditional criteria for BPD but may nonetheless have respiratory disease may limit the generalizability of our findings to populations with fewer medical complications. Despite these limitations, our findings represent a step forward in understanding what outcomes of BPD matter to parents.
In conclusion, we establish parents’ relative ranking of the importance of potential future outcomes associated with BPD. We hope this will direct further study to create concrete outcome measures that better reflect parents’ perspective. Furthermore, the observed heterogeneity among parents about what matters most to them will guide clinicians to be open to differing perspectives when providing prognostic information or anticipatory guidance.
Acknowledgments:
We would like to thank the parents who generously shared their time to participate on our panel and complete the questionnaire. We would also like to thank Kristina Ziolkowski and Laurie Travaglini who worked diligently to distribute this questionnaire to parents.
Funding/Support:
This study was supported by T32 Training Grant No. HG009496 from the National Human Genome Research Institute (K.P.C.), a Marshall Klaus Clinical Research Award (K.P.C.), and the Ohio Perinatal Research Network (OPRN) at Nationwide Children’s Hospital (M.J.K.).
Abbreviations:
- BPD
Bronchopulmonary dysplasia
- NICU
Neonatal intensive care unit
- DCE
Discrete choice experiment
- CI
Confidence interval
- CHOP
Children’s Hospital of Philadelphia
Footnotes
Conflict of Interest Disclosures: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Abman SH, Bancalari E, Jobe A. The evolution of bronchopulmonary dysplasia after 50 years. Am J Respir Crit Care Med 2017;195:421–4. 10.1164/rccm.201611-2386ED. [DOI] [PubMed] [Google Scholar]
- [2].Kalikkot Thekkeveedu R, Guaman MC, Shivanna B. Bronchopulmonary dysplasia: A review of pathogenesis and pathophysiology. Respir Med 2017;132:170–7. 10.1016/j.rmed.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Barrington KJ, Church PT, Luu TM, Davis PG. Respiratory outcomes in preterm babies: Is bronchopulmonary dysplasia important? Acta Paediatr 2022;111:1660–3. 10.1111/apa.16417. [DOI] [PubMed] [Google Scholar]
- [4].Doyle LW, Anderson PJ. Long-term outcomes of bronchopulmonary dysplasia. Semin Fetal Neonatal Med 2009;14:391–5. 10.1016/j.siny.2009.08.004. [DOI] [PubMed] [Google Scholar]
- [5].Webbe J, Brunton G, Ali S, Longford N, Modi N, Gale C, et al. Parent, patient and clinician perceptions of outcomes during and following neonatal care: a systematic review of qualitative research. BMJ Paediatr Open 2018;2:e000343. 10.1136/bmjpo-2018-000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cheong JLY, Doyle LW. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin Perinatol 2018;42:478–84. 10.1053/j.semperi.2018.09.013. [DOI] [PubMed] [Google Scholar]
- [7].Janvier A, Farlow B, Baardsnes J, Pearce R, Barrington KJ. Measuring and communicating meaningful outcomes in neonatology: A family perspective. Semin Perinatol 2016;40:571–7. 10.1053/j.semperi.2016.09.009. [DOI] [PubMed] [Google Scholar]
- [8].Webbe JWH, Ali S, Sakonidou S, Webbe T, Duffy JMN, Brunton G, et al. Inconsistent outcome reporting in large neonatal trials: a systematic review. Arch Dis Child - Fetal Neonatal Ed 2020;105:69–75. 10.1136/archdischild-2019-316823. [DOI] [PubMed] [Google Scholar]
- [9].Tasian Gregory E., Ellison JS. Measuring patient-centered outcomes: The need to move beyond quality of life. J Pediatr Urol 2021;17:444. 10.1016/j.jpurol.2021.03.033. [DOI] [PubMed] [Google Scholar]
- [10].Pearce R, Baardsnes J. Term MRI for small preterm babies: do parents really want to know and why has nobody asked them? Acta Paediatr 2012;101:1013–5. 10.1111/j.1651-2227.2012.02767.x. [DOI] [PubMed] [Google Scholar]
- [11].Webbe JWH, Duffy JMN, Afonso E, Al-Muzaffar I, Brunton G, Greenough A, et al. Core outcomes in neonatology: development of a core outcome set for neonatal research. Arch Dis Child Fetal Neonatal Ed 2020;105:425–31. 10.1136/archdischild-2019-317501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].PROMIS: Patient-Reported Outcomes Measurement Information System - Home Page 2013. https://commonfund.nih.gov/promis/index (accessed November 10, 2021).
- [13].Feudtner C, Walter JK, Faerber JA, Hill DL, Carroll KW, Mollen CJ, et al. Good-Parent Beliefs of Parents of Seriously Ill Children. JAMA Pediatr 2015;169:39–47. 10.1001/jamapediatrics.2014.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Cohen S, Orme B. What’s Your Preference? Asking survey respondents about their preferences creates new scaling decisions. Mark Res Mag Manag Appl 2004;16. [Google Scholar]
- [15].Balza JS, Cusatis RN, McDonnell SM, Basir MA, Flynn KE. Effective questionnaire design: How to use cognitive interviews to refine questionnaire items. J Neonatal-Perinat Med 2022;15:345–9. 10.3233/NPM-210848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Boyden JY, Ersek M, Deatrick JA, Widger K, LaRagione G, Lord B, et al. What Do Parents Value Regarding Pediatric Palliative and Hospice Care in the Home Setting? J Pain Symptom Manage 2021;61:12–23. 10.1016/j.jpainsymman.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cheung KL, Wijnen BFM, Hollin IL, Janssen EM, Bridges JF, Evers SMAA, et al. Using Best–Worst Scaling to Investigate Preferences in Health Care. Pharmacoeconomics 2016;34:1195–209. 10.1007/s40273-016-0429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Belarmino EH, Malinowski A, Flynn K. Diaper need is associated with risk for food insecurity in a statewide sample of participants in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Prev Med Rep 2021;22:101332. 10.1016/j.pmedr.2021.101332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health Consensus Definition of Bronchopulmonary Dysplasia. Pediatrics 2005;116:1353–60. 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- [20].Jaworski M, Janvier A, Lefebvre F, Luu TM. Parental Perspectives Regarding Outcomes of Very Preterm Infants: Toward a Balanced Approach. J Pediatr 2018;200:58–63.e1. 10.1016/j.jpeds.2018.03.006. [DOI] [PubMed] [Google Scholar]
- [21].Adams SY, Tucker R, Clark MA, Lechner BE. “Quality of life”: parent and neonatologist perspectives. J Perinatol 2020. 10.1038/s41372-020-0654-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Plaas K. Waiting for the Other Shoe to Drop: The Lived Experience of Hope for Mothers of Premature Infants in the Neonatal Intensive Care Unit. Dr Diss 2007. [Google Scholar]
- [23].Blackburn C, Harvey M. “We Weren’t Prepared for This”: Parents’ Experiences of Information and Support Following the Premature Birth of Their Infant. Infants Young Child 2019;32:172–85. 10.1097/IYC.0000000000000142. [DOI] [Google Scholar]
- [24].O’Donovan A, Nixon E. “Weathering the storm:” Mothers’ and fathers’ experiences of parenting a preterm infant. Infant Ment Health J 2019;40:573–87. 10.1002/imhj.21788. [DOI] [PubMed] [Google Scholar]
- [25].Haward MF, Lantos J, Janvier A, for the POST Group. Helping Parents Cope in the NICU. Pediatrics 2020;145:e20193567. 10.1542/peds.2019-3567. [DOI] [PubMed] [Google Scholar]
- [26].Lemmon ME, Ubel PA, Janvier A. Estimating Neurologic Prognosis in Children: High Stakes, Poor Data. JAMA Neurol 2019;76:879–80. 10.1001/jamaneurol.2019.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Barone S, Boss RD, Raisanen JC, Shepard J, Donohue PK. Our life at home: Photos from families inform discharge planning for medically complex children. Birth 2020;47:278–89. 10.1111/birt.12499. [DOI] [PubMed] [Google Scholar]
- [28].Feudtner C, Nye RT, Boyden JY, Schwartz KE, Korn ER, Dewitt AG, et al. Association Between Children With Life-Threatening Conditions and Their Parents’ and Siblings’ Mental and Physical Health. JAMA Netw Open 2021;4:e2137250. 10.1001/jamanetworkopen.2021.37250. [DOI] [PMC free article] [PubMed] [Google Scholar]


