Phenomenology is the cornerstone in diagnosing and treating movement disorders. In 1999, re‐emergent tremor was described as a typical phenomenon in Parkinson's disease (PD) by Jankovic and colleagues, 1 characterized as “a rest tremor that re‐emerges after a variable delay while maintaining posture.” This definition is also used in the International Parkinson and Movement Disorders Society consensus statement on the classification of tremors. In this classification, re‐emergent tremor is considered to be an action tremor. 2 However, by definition, the presence of rest tremor is required for the construct re‐emergent tremor. Four features commonly define re‐emergent tremor (Fig. 1B): presence of rest tremor (1); occurrence during posture (2); short pause or reduction in tremor amplitude during the transition from rest to posture (3); and frequency of postural tremor is similar to or slightly higher than rest tremor (4). 1 , 3 The first three features, which are described in the Movement Disorder Society (MDS) consensus statement, can be seen with the naked eye. 2 The fourth feature, which is supported by several studies, requires neurophysiology and is, therefore, not commonly incorporated in operational definitions of re‐emergent tremor. 1 , 3 , 4 Identification of re‐emergent tremor in a patient has important clinical implications, as it can discriminate PD from essential and dystonic tremor. 1 , 5 , 6 An excellent demonstration of proper assessment for re‐emergent tremor has been provided earlier. 7 Re‐emergent tremor appears to be less dopa‐responsive than rest tremor and may require different pharmacological or non‐pharmacological (eg, deep brain stimulation, high intensity focused ultrasound, or botulinum toxin) management than pure postural tremor in PD. 3 , 8 At a circuit level, the cerebellum is thought to be more strongly involved in re‐emergent versus rest tremor. 9 Hence, it is important to be aware of the defining characteristics of re‐emergent tremor. However, we became concerned that the term “re‐emergent tremor” might often be used inadequately, to describe various types of tremors including isolated postural tremor with a delayed onset after posturing, isolated postural tremor that attenuates on voluntary movement and any combination of rest and postural tremor. Here, we address this concern and propose a more unifying concept for PD tremor that may widen the current definition.
FIG. 1.
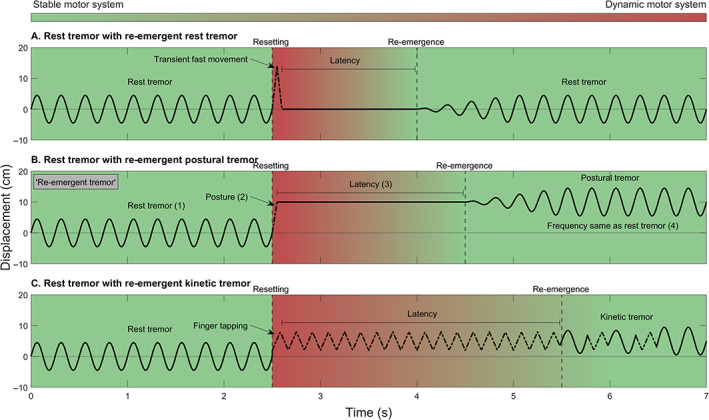
Re‐emergence in Parkinson's disease (PD) tremor. Three instances of PD rest tremor followed by a transient (A) or sustained (B), (C) voluntary movement are depicted. The x‐axis defines time (seconds), the y‐axis defines displacement (centimeters) of the involved body part along an undetermined axis. The background color indicates the stability of the somatotopically involved motor system; green indicates a stable motor system, red indicates an unstable/dynamic motor system. Note that “resetting” occurs during motor transitions (ie, when a voluntary action is made that is novel given the prior motor history). In contrast, “re‐emergence” occurs when the motor system has reached a stable state (eg, rest, stable posturing, or performance of the same movement again and again). (A) Rest tremor is followed by a transient fast voluntary movement, with the body part immediately returning to rest afterward. Coinciding with a surge in motor dynamics (red), the rest tremor is suppressed (resetting). After a few seconds of rest (latency), coinciding with the motor system returning to a stable state (green), the rest tremor re‐emerges. (B) Rest tremor is followed by a vigorous change to posture holding of the body part, and is an example of classical “re‐emergent tremor.” The four defining characteristics of re‐emergent tremor are depicted here: (1) presence of a Parkinsonian rest tremor; (2) transiently suppressed on movement and re‐appearance after repositioning of the limb; (3) latency between movement and re‐appearance of tremor; and (4) similar frequency as tremor during rest. Note that the latency is longer than in (A), because the motor system needs more time to reach stability (red to green). (C) Rest tremor is followed by a repetitive finger tapping. Note that the motor system needs even more time than in (B) to return to stability, leading to a very long latency. Note as well that re‐emergence may be stuttering. Figure created using functions implemented in MATLAB R2022b (The MathWorks, Natick, MA).
Use of “Re‐Emergent Tremor” in the Literature
On September 21, 2022, we performed a literature search in PubMed with the search term “re‐emergent tremor,” delivering 42 hits. Three studies were excluded because of unrelatedness to re‐emergent tremor. For the remaining 39 studies, the definition of re‐emergent tremor was extracted from descriptive sections (eg, introduction and discussion) and original data (eg, results and case descriptions). Adequate (ie, use of the defining characteristics) and consistent (eg, between introduction and results) use of the definition was assessed.
Twenty‐two of 39 studies used the three clinically appreciable elements (first three columns of Fig. S1 ). In only 17 of 39 studies all four elements defining re‐emergent tremor have been implemented (fourth column of Fig. S1). In only 13 of these 17 studies, the adequate definition of re‐emergent tremor was used consistently throughout the study (sixth column of Fig. S1). The remaining studies exhibited various operational definitions of re‐emergent tremor, among others: postural and rest tremor (n = 2), postural tremor with onset latency (n = 2), tremor with onset latency (n = 2), tremor that is transiently suppressed on movement or repositioning of a limb (n = 2), postural tremor with a frequency similar to a parkinsonian rest tremor, but without actual presence of rest tremor (n = 2).
Importance of Adhering To Re‐Emergent Tremor Definition
These results suggest that the construct “re‐emergent tremor” is used differently across studies. This may have implications regarding clinical and investigational findings in patients claimed to have re‐emergent tremor. For instance, various claims of re‐emergent tremor in disorders other than PD, like post‐stroke tremor, 10 , 11 neuroleptic‐induced parkinsonism, 12 dystonic tremor, 13 and neurodegeneration with iron accumulation, 14 can be questioned as an inadequate definition has been used in these studies. 10 , 11 , 12 , 14 Studies showing the diagnostic use of re‐emergent tremor in PD compared to other disorders have used an adequate definition. 1 , 5 , 6
Toward a New Construct of Re‐Emergent and Classical PD Tremor?
Stretching the construct of re‐emergent tremor, one can conceptualize classical PD tremor as a tremor occurring at any state of “motor stability” (Fig. 1); that is, stable rest (“rest tremor” [Video 1, part 1], stable posture (“re‐emergent tremor” [Video 1, part 2]), but also stable kinetic action. 15 The latter can be observed in clinical practice, where it is often seen that PD tremor re‐appears during prolonged repetitive finger and hand tapping (Video 1, parts 4 and 5). This observation and a previous report of re‐emergent tremor during spiral drawing and when attempting to drink, suggests that “re‐emergent kinetic tremor” exists, which currently does not fall under the definition. 16 In line with the idea that tremor emerges only during motor stability, tremor did not re‐emerge when the patient was asked to tap alternatingly with different fingers (ie, increased motor dynamics) (Video 1, part 6). In this framework, “resetting” (ie, discontinuation/suppression of the tremor) may mark the transition from “motor stability” to “motor dynamics” in the motor network controlling that body part (Fig. 1). For resetting to be most effective, a certain degree of motor vigor/complexity is required (Video 1, part 3). In our experience, a rapid wrist extension is more effective in resetting tremor than (slow) lifting of the arms. 17 This may help clinicians to better recognize re‐emergent tremor, which in turn can help discriminate PD from essential tremor or dystonic tremor. 18 In a similar vein, “re‐emergence” of tremor may mark the transition from “motor dynamics” to “motor stability.” Motor stability refers to situations when the tremulous muscles are relaxed (“rest”) (Fig. 1A) or when a simple, “automatic” motor program is being performed (eg, when the arm is held in a stable posture) (Fig. 1B), or when a simple tapping movement is made again and again (Fig. 1C). In contrast, motor dynamics refers to situations when actions are selected that are novel with respect to the prior motor history (eg, when transitioning from rest to posture or when performing more complex sequences that involve transitions between different fingers).
Video 1.
Rest tremor, resetting and re‐emergence in a Parkinson's disease (PD) patient. Part 1 (00:00–00:06). Classical PD rest tremor in the right hand. Part 2 (00:06–00:11). Re‐emergence of right PD tremor during posture holding with a delay of ~2 s. Part 3 (00:11–00:16). Resetting of tremor with brisk voluntary wrist dorsiflexion. Part 4 (00:16–00:36). Progressive re‐emergence of tremor during finger tapping with a delay of ~ 6 s. Part 5 (00:36–1:01). Progressive and somewhat stuttering re‐emergence of tremor during hand tapping with a delay of ~10–20 s. Part 6 (1:01–1:29). No re‐emergence of tremor during alternating finger tapping.
This novel framework of PD tremor deserves and requires further attention and investigation. Electrophysiological studies are needed to corroborate our observation of PD tremor during repetitive movements. The anatomical and neurophysiological underpinnings of motor stability will also need to be defined to improve our understanding of PD tremor, as well as the cerebral motor circuit from which it originates. An important conundrum is the lack of correlation between power in the β frequency range (13–35 Hz)—the most robust electrophysiological marker of “motor stability”—and PD tremor. 15 However, neurophysiological and neuroimaging evidence suggest that pathological activity (eg, increased β power) within the basal ganglia precedes the (re‐)emergence of tremor. 19 In periods of sustained tremor, the tremor is maintained and amplified by the cerebello‐thalamo‐cortical circuit. 20 These periods of sustained tremor are associated with increased low β power in the premotor cortex. 21 Resetting might (also) be mediated by proprioceptive input, occurring in parallel to movement‐related β‐desynchronization on movement. 22 Additionally, differences in the latency to tremor emergence between conditions 4 and individuals 3 may be because of variability in the tendency of neural motor networks to reach stability, but the underlying mechanisms are unclear. It needs to be defined how the concept of motor stability fits with the observation that the duration of the pause is inversely related to the amplitude of the rest tremor. 23
Altogether, we endorse the original description and assessment of re‐emergent tremor by Jankovic and colleagues, 1 which integrates all four essential features (ie, postural, latency, presence of rest tremor, and frequency similar to the rest tremor) (Fig. 1B) when describing re‐emergent tremor. However, the term “re‐emergent tremor” is somewhat confusing, because it does not specify during what condition the tremor re‐emerges (ie, rest, posture, or action). It only covers the characteristics “latency” and “frequency similar to the rest tremor” of this construct. This could be a reason for the low rate of adequate definitions used (Fig. S1). Perhaps it would be more formally correct to add the condition in which the tremor re‐emerges, for example “rest tremor with re‐emergent rest, postural or kinetic tremor” (Fig. 1). This nomenclature is in line with activation conditions defined in the MDS consensus on tremor. 2 When assessing and describing PD tremor, it is probably best to describe the phenomenology as detailed as possible. This encompasses not only the typical static characteristics of a tremor (ie, condition, amplitude, and frequency), but also dynamic characteristics (ie, resetting, latency, and re‐emergence) (Fig. 1). Future studies could extend the construct of re‐emergent tremor by unifying the clinical phenomena of resetting and re‐emergence as pivotal elements for classical PD tremor, whether occurring during rest or action.
Author Roles
(1) Conception; (2) Literature Review; (3) Video: A. Recording, B. Editing; (4) Manuscript: A. Writing of the First Draft, B. Review and Critique.
B.E.K.S.: 1, 2, 3B, 4A
R.M.A.B.: 1, 4B
M.H.: 4B
R.C.H.: 1, 3A, 4B
A.W.G.B.: 1, 4A
Disclosures
Ethical Compliance Statement: The authors confirm that the approval of an institutional review board was not required for this work. Written informed consent has been obtained from the patient. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflicts of Interest: The authors declare that there are no funding sources or conflicts of interest to report.
Financial Disclosures for Previous 12 Months: R.H. reports consultancies for U.C.B. in the last 12 months and was supported by the following funding bodies: ParkinsonNL (P2023‐14), Netherlands Organization for Scientific Research (09150172010044), EU‐JPND (10510062110006), and The Michael J. Fox Foundation (MJFF‐021001). M.H. is an inventor of a patent held by National Institutes of Health (NIH) for the H‐coil for magnetic stimulation for which he receives license fee payments from the NIH (from Brainsway). He is on the Medical Advisory Boards of Brainsway, QuantalX, and VoxNeuro. The other authors declare that there are no disclosures to report.
Supporting information
Data S1. Supporting information.
Figure S1. Operational definitions of re‐emergent tremor in literature. The first four columns relate to the presence/absence of the four essential elements defining re‐emergent tremor. The fifth column indicates consistent use of the definition. The sixth column indicates an overall judgment on the consistent use of an adequate definition. Color legend: green, present; red, absent; gray, no/unclear description. 1, frequency similar to a Parkinsonian rest tremor; 2, also in the jaw and the tongue; 3, also in the legs on standing; 4, weight‐dependent (weight‐holding tremor); 5, transiently suppressed on movement; 6, after repositioning of the limb; 7, “with a re‐emergent component.” References are displayed in Supplementary Material S1.
Relevant disclosures and conflict of interest are listed at the end of this article.
References
- 1. Jankovic J, Schwartz K, Ondo W. Re‐emergent tremor of Parkinson's disease. J Neurol Neurosurg Psychiatry 1999;67:646–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bhatia KP, Bain P, Bajaj N, et al. Consensus statement on the classification of tremors. From the task force on tremor of the International Parkinson and Movement Disorder Society. Mov Disord 2018;33:75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dirkx MF, Zach H, Bloem BR, Hallett M, Helmich RC. The nature of postural tremor in Parkinson disease. Neurology 2018;90:e1095–e1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wilken M, Rossi M, Rivero AD, Hallett M, Merello M. Re‐emergent tremor provocation. Park Relat Disord 2019;66:241–244. [DOI] [PubMed] [Google Scholar]
- 5. Fekete R, Li J. Clinical differentiation of essential tremor and Parkinson's disease. Clin Med Insights Case Reports 2013;6:67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schwingenschuh P, Ruge D, Edwards MJ, et al. Distinguishing SWEDDs patients with asymmetric resting tremor from Parkinson's disease: a clinical and electrophysiological study. Mov Disord 2010;25:560–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jankovic J. How do I examine for re‐emergent tremor? Mov Disord Clin Pract 2016;3:216–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Belvisi D, Conte A, Cutrona C, Costanzo M, Ferrazzano G, Fabbrini G, Berardelli A. Re‐emergent tremor in Parkinson's disease: the effect of dopaminergic treatment. Eur J Neurol 2018;25:799–804. [DOI] [PubMed] [Google Scholar]
- 9. Helmich RC, Van den Berg KRE, Panyakaew P, et al. Cerebello‐cortical control of tremor rhythm and amplitude in Parkinson's disease. Mov Disord 2021;36:1727–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee MS, Lee SH, Ahn SJ. Re‐emergent tremor without rest tremor after lenticular infarctions. Mov Disord Clin Pract 2016;3:96–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Udagedara TB, Gooneratne IK. Jaw tremor: a manifestation of vascular parkinsonism?–a case report. BMC Neurol 2018;18:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Prasad S, Holla VV, Pal PK. Re‐emergent tongue tremor in neuroleptic‐induced parkinsonism. Tremor Other Hyperkinet Mov 2019;9:632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Laat K, van de Warrenburg BP. Re‐emergent tremor in a dystonic SWEDD case. Mov Disord 2012;27:462–463. [DOI] [PubMed] [Google Scholar]
- 14. Aggarwal A, Schneider SA, Houlden H, et al. Indian‐subcontinent NBIA: unusual phenotypes, novel PANK2 mutations, and undetermined genetic forms. Mov Disord 2010;25:1424–1431. [DOI] [PubMed] [Google Scholar]
- 15. Hallett M. Tremor: pathophysiology. Park Relat Disord 2014;20:S118–S122. [DOI] [PubMed] [Google Scholar]
- 16. Gupta HV. Re‐emergent kinetic tremor in Parkinson's disease. Tremor and other hyperkinetic movements; Epub 2019. [DOI] [PMC free article] [PubMed]
- 17. Helmich RC, Hallett M, Dirkx MF. Author response: the nature of postural tremor in Parkinson disease. Neurology 2018;91:724. [DOI] [PubMed] [Google Scholar]
- 18. Papengut F, Raethjen J, Binder A, Deuschl G. Rest tremor suppression may separate essential from parkinsonian rest tremor. Park Relat Disord 2013;19:693–697. [DOI] [PubMed] [Google Scholar]
- 19. Hirschmann J, Abbasi O, Storzer L, Butz M, Hartmann CJ, Wojtecki L, Schnitzler A. Longitudinal recordings reveal transient increase of alpha/low‐beta power in the subthalamic nucleus associated with the onset of parkinsonian rest tremor. Front Neurol 2019;10:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Helmich RC. The cerebral basis of parkinsonian tremor: a network perspective. Mov Disord 2018;33:219–231. [DOI] [PubMed] [Google Scholar]
- 21. Lauro PM, Lee S, Akbar U, Asaad WF. Subthalamic–cortical network reorganization during Parkinson's tremor. J Neurosci 2021;41:9844–9858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Naros G, Grimm F, Weiss D, Gharabaghi A. Directional communication during movement execution interferes with tremor in Parkinson's disease. Mov Disord 2018;33:251–261. [DOI] [PubMed] [Google Scholar]
- 23. Wilken M, Rossi MD, Rivero AD, Hallett M, Merello M. Latency of re‐emergent tremor in Parkinson's disease is influenced by levodopa. Park Relat Disord 2019;61:166–169. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting information.
Figure S1. Operational definitions of re‐emergent tremor in literature. The first four columns relate to the presence/absence of the four essential elements defining re‐emergent tremor. The fifth column indicates consistent use of the definition. The sixth column indicates an overall judgment on the consistent use of an adequate definition. Color legend: green, present; red, absent; gray, no/unclear description. 1, frequency similar to a Parkinsonian rest tremor; 2, also in the jaw and the tongue; 3, also in the legs on standing; 4, weight‐dependent (weight‐holding tremor); 5, transiently suppressed on movement; 6, after repositioning of the limb; 7, “with a re‐emergent component.” References are displayed in Supplementary Material S1.


