Abstract
Using antibiotics without medical guidance (non-prescription antibiotic use) may contribute to antimicrobial resistance. Hispanic individuals are a growing demographic group in the United States (US) with a high prevalence of non-prescription antibiotic use. We investigated the effects of acculturation and subjective norms on Hispanic individuals’ intentions to use antibiotics without a prescription from the following sources: (1) markets in the United States (not legal), (2) other countries (abroad), (3) leftovers from previous prescriptions, and (4) friends/relatives. We surveyed self-identified Hispanic outpatients in eight clinics from January 2020 to June 2021 using the previously validated Short Acculturation Scale for Hispanics (SASH). Of the 263 patients surveyed, 47% reported previous non-prescription use, and 54% expressed intention to use non-prescription antibiotics if feeling sick. Individuals with lower acculturation (Spanish-speaking preferences) expressed greater intentions to use antibiotics from abroad and from any source. Individuals with more friends/relatives who obtain antibiotics abroad were over 2.5 times more likely to intend to use non-prescription antibiotics from friends/relatives (p = 0.034). Other predictors of intention to use non-prescription antibiotics included high costs of doctor visits and perceived language barriers in the clinic. Antibiotic stewardship interventions in Hispanic communities in the United States should consider the sociocultural and healthcare barriers influencing non-prescription use and promote language-concordant healthcare.
Keywords: acculturation, subjective norms, socio-cultural factors, antibiotic resistance, non-prescription antibiotic use, antibiotic stewardship
1. Introduction
Using antibiotics without a prescription (non-prescription antibiotic use) is a common practice worldwide and is a safety threat to individuals and the public health [1,2,3]. Non-prescription antibiotic use can potentially increase the risks of adverse drug reactions or interactions, superinfection, gut dysbiosis, and the development of antimicrobial resistance [4,5,6].
Recent studies have documented the determinants of non-prescription antibiotic use across low-, middle-, and high-income countries and found that patient-level (sociocultural and sociodemographic) factors and healthcare system barriers contribute to non-prescription antibiotic use [7,8,9]. In the United States (US), Hispanic communities have one of the highest reported prevalence rates of non-prescription antibiotic use, with the prevalence ranging from 19 to 66% [9]. Prior studies have identified that these Hispanic communities use non-prescribed antibiotics from a variety of sources, including leftover prescriptions (e.g., from self, friends, or family); purchasing illegally under-the-counter through informal sources in the US (e.g., flea markets and ethnic or herbalist shops); or outside the US without a prescription (e.g., across the border in another country, including Mexico) [3,9,10,11,12].
Sociocultural factors include an individual’s level of acculturation and their subjective norms. Acculturation and subjective norms can impact health behaviors in Hispanic communities [10,11,12]. Acculturation is “the process by which individuals adopt the attitudes, values, customs, beliefs, and behaviors of another culture” [13,14]. For example, less-acculturated individuals may continue certain health practices (e.g., non-prescription antibiotic use) that they had in their home countries. Subjective norms are often classified as the “expectations set by groups of important people (such as family, relatives, and friends) in terms of whether an individual should or should not engage in a behavior” [15]. For instance, individuals may engage in non-prescription antibiotic use because their friends and family also routinely engage in that behavior.
A recent study of a Hispanic community along the Texas border found that a higher generation score, a proxy measure of acculturation, was associated with lower cross-border purchases of antibiotics [11]. Another qualitative study of Hispanic primary care patients in Houston found that patients’ subjective norms (e.g., friends and family frequently purchase non-prescription antibiotics) and social networks (e.g., friends, family, or other “trusted” persons) influenced their decisions to use non-prescription antibiotics [12]. However, these studies included medically underserved, impoverished Hispanic individuals and did not study the independent effects of sociocultural and healthcare system factors on non-prescription antibiotic use in sociodemographically diverse Hispanic communities.
2. Materials and Methods
We investigated the effects of Hispanic patients’ sociocultural factors (acculturation and subjective norms) and the barriers to healthcare on the intention to use non-prescription antibiotics from four sources: (1) markets in the United States (under the counter, not legal), (2) other countries, (3) leftovers from previous prescriptions, and (4) friends/relatives.
2.1. Design and Recruitment
We conducted a large, cross-sectional survey to assess non-prescription antibiotic use in sociodemographically diverse outpatients. Data collection occurred between January 2020 and June 2021 in eight outpatient clinic waiting rooms (six public primary care and two private emergency departments) in Harris County, Texas [3]. Clinic staff gave flyers to patients who checked in for primary care visits. The flyer summarized the study, and interested patients volunteered to participate. Surveys were conducted anonymously in person when permitted during the pandemic or remotely via teleconferencing in patients’ preferred language (English or Spanish). Each respondent was given a list of brand name and generic antibiotics that were accompanied by images of the most commonly used antibiotics in the US and Latin American countries.
Individuals who self-identified as Hispanic or Latino in the larger survey were included for analysis in this study [3]. This study was approved by the Institutional Review Board for Baylor College of Medicine and Affiliated Hospitals (protocol H-45709). Additional details on recruitment, survey design information, sample size calculations, response rate, and additional information were published elsewhere [3].
2.2. Survey Instrument
The survey instrument is available in Appendix A. Non-prescription antibiotic use was defined as the consumption of antibiotics not prescribed to that individual for his or her current health condition [3]. Intended use was defined as a professed intention for future non-prescription antibiotic use [9,16]. Individuals classified as non-prescription antibiotic users reported having “ever taken” oral antibiotics without a prescription. Individuals classified as intended users endorsed using antibiotics from one of four sources presented via the question “If you were feeling sick, would you take antibiotics in the following situations without contacting a doctor/nurse/dentist/clinic?” The sources presented to the patients were: (1) you can buy antibiotics without a prescription in the United States, (2) you can buy antibiotics without a prescription in another country, (3) friends or relatives give you antibiotics, and (4) you have leftover antibiotics from a previous prescription.
Survey questions were mapped to factors in the Kilbourne Framework for Advancing Health Disparities Research, including the patient, healthcare system, and clinical encounter factors [17]. Subjective norms and acculturation are patient factors that may contribute to non-prescription antibiotic use in Hispanic populations. Healthcare system barriers included lacking transportation to the doctor visits, long clinic waits, not having a regular doctor, and the high cost of doctor visits. Clinical encounter factors included language barriers at the clinic and during doctor visits.
2.3. Patient Factors
2.3.1. Sociodemographic Factors
Sociodemographic characteristics included age, gender, race/ethnicity, education, yearly household income, health insurance status, country of birth, and health literacy (Table 1). Individuals’ insurance status was categorized into three groups: (1) private insurance or Medicare, (2) Medicaid (i.e., public health insurance for low-income children, families, seniors, and people with disabilities) or county financial assistance program (CFAP) (provides healthcare coverage/access to publicly funded clinics at very low or no cost to patients), or (3) self-pay (no insurance or CFAP). For health literacy, we used the Brief Health Literacy Screen measure validated in primary care settings [18,19]. Inadequate health literacy was defined as an answer to any of three screening questions that endorsed having problems associated with health literacy some or all of the time.
Table 1.
Patient sociodemographic characteristics.
| Characteristic | Total (N = 263) |
|---|---|
| Median age (y) (range) | 51 (20–80) |
| No. (%) of female respondents | 194 (73.8) |
| No. (%) of respondents with education level | |
| Less than high school | 84 (31.9) |
| High school or GED | 104 (39.5) |
| Some college and above | 75 (28.5) |
| No. (%) of respondents with insurance status | |
| Private or Medicare | 74 (28.1) |
| Medicaid or county financial assistance program * | 173 (60.8) |
| Self-pay | 16 (6.1) |
| No. (%) of patients attending Healthcare system | |
| Private | 41 (15.6) |
| Public | 222 (84.4) |
| No. (%) of patients attending clinic type | |
| Continuity clinic | 102 (38.8) |
| Emergency Department | 41 (15.6) |
| Walk in Clinic | 120 (45.6) |
| No. of respondents with income/total no. of respondents (%) | |
| <$20,000 | 127 (48.3) |
| ≥$20,000 but <$40,000 | 58 (22.1) |
| ≥$40,000 but <$60,000 | 11 (4.2) |
| ≥$60,000 but <$100,000 | 8 (3.0) |
| ≥$100,000 | 6 (2.3) |
| Don’t know/prefer not to say | 53 (20.2) |
| No. (%) of questionnaires completed in Spanish | 155 (58.9) |
| No. (%) of respondents born in the United States/Other | |
| United States | 81 (30.8) |
| Other † | 182 (69.2) |
| Median years lived in the United States for the respondents born in other countries (y) (range) (n = 182) |
23 (0–58) |
| No. (%) of respondents reporting non-prescription antibiotic use | |
| Reported prior non-prescription use | 123 (46.8) |
| No. (%) Health Literacy § | |
| Adequate Health Literacy | 198 (75.3) |
| Inadequate Health Literacy | 65 (24.7) |
* County financial assistance program includes those who have benefits from the county allowing access to public clinic providers at either very low cost or no cost. † Includes 1 Columbia, 1 Costa Rica, 6 Cuba, 1 Dominican Republic, 14 El Salvador, 6 Guatemala, 15 Honduras, 131 Mexico, 2 Nicaragua, 1 Panama, 1 Peru, and 3 Venezuela (countries are listed in alphabetical order). § Calculated using the three questions from the Brief Health literacy Screen measure [18,19].
2.3.2. Acculturation
Acculturation was assessed using the Short Acculturation Scale for Hispanics (SASH) developed and validated by Marin et al. and included the Language Use, Television and Media, and Social and Ethnic Relations subscale scores [20]. The SASH questionnaire contains 12 questions of equal weight: 5 assessing language preferences, 3 assessing media preferences, and 4 assessing social and ethnic preferences (Appendix A. Survey Instrument).
Each question was scored on Likert-type scales, ranging from 1 (Only Spanish/all Hispanic individuals) to 5 (Only English/all non-Hispanic individuals). Subscores with lower values (closer to 1) reflect preferences for Spanish-speaking interactions or Hispanic social interactions or entertainment. Higher scores (closer to 5) reflect a preference for English-speaking interactions or entertainment. The total points per subscale were averaged over the number of questions answered to generate the numerical score for that subscale. Cronbach’s alpha was computed to determine the internal consistency of the set of questions representing each construct; one question was excluded from the ethnic and social relations subscale (Appendix B. SASH Reliability Statistics). The overall acculturation score was calculated using the sum of the language, television and media use, and ethnic and social relations subscores (Table 2).
Table 2.
Acculturation by subscale means, interquartile range, and internal consistency †.
| Acculturation Subscales | Intended Use from Any Source | Cronbach’s Alpha | |
|---|---|---|---|
| Yes (n = 95) Median (IQR *) |
No (n = 167) Median (IQR *) |
||
| Language Use Subscale Score | 2.0 (1.2–3.4) | 2.0 (1.4–3.2) | 0.939 |
| Media Subscale Score | 3.0 (1.7–4.0) | 3.0 (1.0–4.0) | 0.969 |
| Ethnic Social Relations Subscale Score | 2.3 (2.0–2.7) | 2.3 (2.0–3.0) | 0.817 |
| Total Acculturation (Overall, Aggregate Score) | 2.5 (1.6–3.4) | 2.4 (1.7–3.3) | 0.939 |
* Interquartile Range. † The Short Acculturation Scale for Hispanics is comprised of three subscales (Language Use, Media, and Ethnic Social Relations). Scores range from 1 (all Latinos/Hispanics) to 5 (all non-Latinos/Hispanics). Higher score indicates higher levels of acculturation [20].
2.3.3. Subjective Norms
Subjective norms were identified by the following proxy questions: (1) “How many of your friends or relatives use antibiotics without contacting a doctor?” and (2) “How many of your friends or relatives get antibiotics from another country?” Each question was scored using Likert-type scales ranging from 1 (none/don’t remember/don’t know) to 4 (all/most/about half) (Table 3).
Table 3.
Subjective norms (N = 263).
| Total No. (%) | |
|---|---|
| How many of your friends or relatives use antibiotics without contacting a doctor? | |
| None/Don’t Remember/Don’t Know | 105 (39.9) |
| Some | 98 (37.3) |
| About Half | 15 (5.7) |
| Most | 33 (12.5) |
| All | 12 (4.6) |
| How many of your friends or relatives get antibiotics from another country? | |
| None/Don’t Remember/Don’t Know | 123 (46.8) |
| Some | 97 (36.9) |
| About Half | 15 (5.7) |
| Most | 28 (10.6) |
2.4. Healthcare System and Clinical Encounter Factors
Healthcare barriers were assessed using five questions relevant to our safety net patient population, including transportation, language barriers, long clinic waits, not having a regular doctor, and the high cost of doctor visits. Each question was scored dichotomously as “not a problem” or “a problem” (i.e., included answering that the barrier was a minor or major problem) (Appendix C).
2.5. Statistical Analysis
Descriptive statistics were performed on all study variables using SPSS version 28 (Chicago, IL, USA) [21]. Cronbach’s alpha was computed to analyze the internal consistency of the set of questions representing the acculturation scale. We used univariate logistic regression to assess the patient and healthcare system factors associated with patients’ intention to use non-prescription antibiotics from each source. Predictor variables that showed a univariate relationship (p < 0.2) with each source of intended non-prescription antibiotic use were considered for the multivariate analyses (Appendix D. Univariate Regression Results).
Multivariate logistic regression assessed the effects of patients’ acculturation and subjective norms on their intention to use antibiotics without a prescription from one of the following sources: (1) stores or markets in the US, (2) another country, (3) friends/relatives, (4) a leftover prescription, and (5) any of these four sources (Table 4, Table 5, Table 6, Table 7 and Table 8).
3. Results
3.1. Patient Factors
3.1.1. Sociodemographic Characteristics
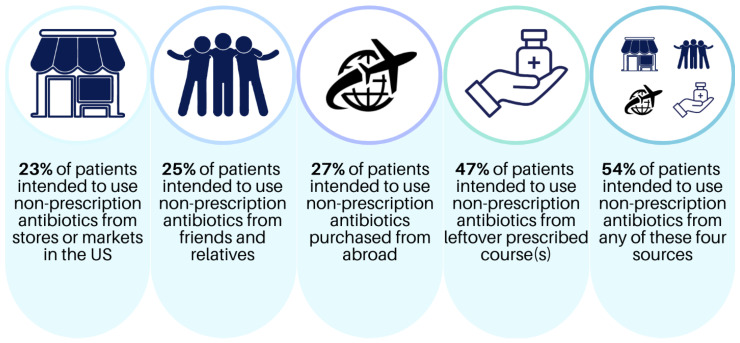
Table 1 shows the sociodemographic characteristics of the 263 patients surveyed. Most respondents were female (74%) and educated at the high school level (40%) or some college and above (29%). Approximately 61% of the patients had healthcare coverage through Medicaid or county financial assistance, followed by private insurance or Medicare (28%) and self-pay (6%). Most patients who reported their income had household incomes below 40,000 USD/year (70%). Approximately 59% of all patients preferred being surveyed in Spanish. More patients were born outside the US (69%) in Mexico (n = 131), followed by Honduras (n = 15) and El Salvador (n = 14). Foreign-born patients lived in the US for a median of 23.5 years. Nearly half (47%) of the participants reported prior non-prescription antibiotic use, and over 75% of patients were classified as having “adequate” health literacy levels (Table 1). Overall, 54% professed an intention to use/obtain non-prescription antibiotics if feeling sick from at least one source (Figure 1).
Figure 1.
Prevalence of the intention to use non-prescription antibiotics in Hispanic patients surveyed (N = 263).
3.1.2. Acculturation
Table 2 includes the mean acculturation subscale and Cronbach’s alpha scores for language use, TV and media, ethnic and social relations, and the total acculturation (overall, aggregate score). The median total acculturation score for respondents who professed intention for future non-prescription antibiotic use was 2.5/5.0 (IQR 1.6–3.4), and the Cronbach’s alpha for the total acculturation was 0.939 (Table 2).
3.1.3. Subjective Norms
Table 3 lists the proportion of patients (N = 263) that reported friends/relatives that used non-prescribed antibiotics or purchased antibiotics from other countries (outside the US). Over 60% of patients reported that some to all of their friends or relatives had used antibiotics without contacting a doctor. About 53% reported that some to most of their friends or relatives have used or purchased non-prescribed antibiotics from another country (Table 3).
3.2. Healthcare System Factors
Appendix C displays the patient-reported barriers to healthcare in the last 12 months. Of the barriers to access, patients frequently expressed that long waiting times (26%), transportation (16%), and the high cost of doctor visits (16%) were problematic, followed by language barriers (8%) and not having a regular doctor (5%) (Appendix C).
3.3. Multivariate Results
Table 4, Table 5, Table 6, Table 7 and Table 8 display the multivariate logistic regression results of patient intentions to use non-prescription antibiotics from each of the four sources and overall.
Table 4.
Multivariate results of the intended use of antibiotics from stores or markets in the US.
| Intended Use of Antibiotics from Stores or Markets in the United States | ||
|---|---|---|
| Predictors § | OR (95% CI) | p-Value |
| Prior Non-prescription Use | ||
| No Prior Use | 1 (reference) | 1 (reference) |
| Prior Use | 6.26 (3.13–12.51) | <0.001 |
| Barriers To Healthcare Access For your medical appointments in the last 12 months, how much of a problem are: High cost of doctor visits |
||
| Not a problem | 1 (reference) | 1 (reference) |
| A problem | 3.1 (1.43–6.69) | 0.004 |
§ The following predictors were not significant in the multivariate model: Acculturation (Language Use Subscale, Media Subscale, and Ethnic Social Relations Subscale); Subjective Norms (How many of your friends or relatives get antibiotics without contacting a doctor? How many of your friends or relatives get antibiotics from another country?); Sociodemographics (Age, Healthcare System, Insurance, Language, Education, and Country of Birth); and Barriers to Healthcare Access (For your medical appointments in the last 12 months, how much of a problem is not having a regular doctor?).
Table 5.
Multivariate results of the intended use of antibiotics bought without a prescription from another country.
| Intended Use of Antibiotics Bought without a Prescription from Another Country | ||
|---|---|---|
| Predictors § | OR (95% CI) | p-Value |
| Acculturation ¶ | ||
| Ethnic Social Relations Subscale | 0.54 (0.33–0.86) | 0.009 |
| Prior Non-prescription Use | ||
| No Prior Use | 1 (reference) | 1 (reference) |
| Prior Use | 10.49 (5.13–21.46) | <0.001 |
¶ The Short Acculturation Scale for Hispanics is comprised of three subscales (Language Use, Media, and Ethnic Social Relations). Scores range from 1 (all Latinos/Hispanics) to 5 (all non-Latinos/Hispanics). Higher score indicates higher levels of acculturation [20]. § The following predictors were not significant in the multivariate model: Acculturation (Language Use Subscale and Media Subscale); Subjective Norms (How many of your friends or relatives get antibiotics without contacting a doctor? How many of your friends or relatives get antibiotics from another country?); Sociodemographics (Age, Years lived in the US, and Education); and Barriers to Healthcare Access (For your medical appointments in the last 12 months, how much of a problem are high cost of doctor visits, a language barrier, and not having a regular doctor?).
Table 6.
Multivariate results of the intended use of antibiotics from friends and relatives.
| Intended Use of Antibiotics from Friends and Relatives | ||
|---|---|---|
| Predictors § | OR (95% CI) | p-Value |
| Social Norms | 0.054 | |
| How many of your friends or relatives get antibiotics from another country? | ||
| None | 1 (reference) | 1 (reference) |
| Some | 2.52 (0.92–6.93) | 0.072 |
| All/Most/About Half | 2.51 (1.07–5.85) | 0.034 |
| Don’t Know/Don’t remember | 0.95 (0.34–2.64) | 0.918 |
| Sociodemographics | ||
| Education | 0.017 | |
| Less than High School | 1 (reference) | 1 (reference) |
| High school or GED | 0.53 (0.24–1.19) | 0.126 |
| Some College or Above | 0.32 (0.14–0.7) | 0.004 |
| Prior Non-prescription Use | ||
| No Prior Use | 1 (reference) | 1 (reference) |
| Prior Use | 10.59 (5.0–22.43) | <0.001 |
| Barriers To Healthcare Access | ||
| For your medical appointments in the last 12 months, how much of a problem are: | ||
| High cost of doctor visits | ||
| Not a problem | 1 (reference) | 1 (reference) |
| A problem | 3.16 (1.38–7.21) | 0.006 |
§ The following predictors were not significant in the multivariate model: Acculturation (Language Use Subscale, Media Subscale, and Ethnic Social Relations Subscale); Subjective Norms (How many of your friends or relatives get antibiotics without contacting a doctor?); Sociodemographics (Age, Sex, Insurance, and Country of Birth); and Barriers to Healthcare Access (For your medical appointments in the last 12 months, how much of a problem are transportation, a language barrier, and not having a regular doctor?).
Table 7.
Multivariate results of the intended use of antibiotics from leftover antibiotic courses.
| Intended Use of Antibiotics from Leftover Courses | ||
|---|---|---|
| Predictors § | OR (95% CI) | p-Value |
| Prior Non-prescription Use | ||
| No Prior Use | 1 (reference) | 1 (reference) |
| Prior Use | 7.51 (4.15–13.26) | <0.001 |
| Barriers To Healthcare Access | ||
| For your medical appointments in the last 12 months, how much of a problem are: A language barrier |
||
| Not a problem | 1 (reference) | 1 (reference) |
| A problem | 3.08 (1.03–9.26) | 0.006 |
§ The following predictors were not significant in the multivariate model: Acculturation (Language Use Subscale, Media Subscale, and Ethnic Social Relations Subscale); Subjective Norms (How many of your friends or relatives get antibiotics without contacting a doctor? How many of your friends or relatives get antibiotics from another country?); Sociodemographics (Healthcare System, Insurance, and Country of Birth); and Barriers to Healthcare Access (For your medical appointments in the last 12 months, how much of a problem are long waiting times or the high cost of doctor visits?).
Table 8.
Multivariate results of the intended use of antibiotics from any source (US, abroad, friends and relatives, and leftover courses).
| Intended Use of Antibiotics from Any Source (US, Abroad, Friends and Relatives, and Leftover Courses) | ||
|---|---|---|
| Predictors § | OR (95% CI) | p-Value |
| Acculturation ¶ | ||
| Language Use Subscale | 0.61 (0.39–0.96) | 0.031 |
| Sociodemographics | ||
| Country of Birth | ||
| Born in US | 1 (reference) | 1 (reference) |
| Born in other countries ‖ | 8.47 (2.56–28.02) | <0.001 |
| Prior Non-prescription Use | ||
| No Prior Use | 1 (reference) | 1 (reference) |
| Prior Use | 12.32 (6.58–23.09) | <0.001 |
¶ The Short Acculturation Scale for Hispanics is comprised of three subscales (Language Use, Media, and Ethnic Social Relations). Scores range from 1 (all Latinos/Hispanics) to 5 (all non-Latinos/Hispanics). Higher score indicates higher levels of acculturation [20]. ‖ Includes 1 Columbia, 1 Costa Rica, 6 Cuba, 1 Dominican Republic, 14 El Salvador, 6 Guatemala, 15 Honduras, 131 Mexico, 2 Nicaragua, 1 Panama, 1 Peru, and 3 Venezuela (countries are listed in alphabetical order). § The following predictors were not significant and therefore not included in this model: Acculturation (Media Subscale and Ethnic Social Relations Subscale); Social Norms (How many of your friends or relatives get antibiotics from another country?); Sociodemographics (Education); and Barriers to Healthcare Access (For your medical appointments in the last 12 months, how much of a problem are the high cost of doctor visits and a language barrier).
3.3.1. Intended Use of Antibiotics from Stores or Markets in the United States
The high costs of doctor visits (OR 3.1, 95% CI [1.43–6.69], p = 0.004) and prior non-prescription antibiotic use (OR 6.3, 95% CI [3.13–12.51], p < 0.001) were significant predictors of the intended use of non-prescribed antibiotics purchased in the US. Neither the acculturation subscales nor subjective norms were significant predictors of the intended use of non-prescription antibiotics from stores or markets in the US (Table 4).
3.3.2. Intended Use of Antibiotics Bought without a Prescription from Another Country
Individuals with lower Ethnic and Social Relations subscale scores indicating higher preferences to socialize and associate with other Hispanic individuals had higher odds of the intention to use non-prescribed antibiotics from another country compared to those with higher Ethnic and Social Relations subscale scores (OR 0.54 95% CI [0.33–0.86], p = 0.009). In addition, patients with prior non-prescription antibiotic use had 10.5 times higher intended use from other countries (95% CI [5.13–21.46], p < 0.001) (Table 5).
3.3.3. Intended Use of Antibiotics from Friends and Relatives
More educated patients with a high school, college, or above education were 68% less likely to use antibiotics from a friend or relative (OR 0.32, 95% CI [0.14–0.70], p = 0.004). The high cost of doctor visits during medical appointments was a significant predictor of intention (OR 3.16, 95% CI [1.38–7.21], p = 0.006). Patients who reported at least some of their friends or relatives getting non-prescribed antibiotics from other countries had 2.5 times higher odds of intention to use non-prescription antibiotics from friends and relatives (95% CI [1.07–5.85], p = 0.034). Additionally, patients with prior non-prescription antibiotic use had over 10.6 times higher odds of intended use from friends and relatives (95% CI [5.0–22.4], p < 0.001) (Table 6).
3.3.4. Intended Use of Antibiotics from Leftover Courses
Patients reporting language barriers as a problem during their medical appointment had over three times higher odds of the intention to use antibiotics from leftover prescription sources than patients who did not (95% CI [1.03–9.26], p = 0.006). Prior non-prescription antibiotic use was a strong predictor of the intention from leftover courses (OR 7.5 95% CI [4.15–13.26], p < 0.001). Neither acculturation subscales nor social norms were significant predictors of the intended use from leftover antibiotic courses (Table 7).
3.3.5. Intended Use of Antibiotics from Any Source (US, Abroad, Friends and Relatives, and Leftover Courses)
Patients born outside the US had 8.5 times higher intention to use non-prescription antibiotics (95% CI [2.56–28.02], p < 0.001). Individuals with a higher preference to socialize in Spanish (lower Language Use subscale scores) expressed a higher intention to use non-prescribed antibiotics from any source (overall) in the future compared to those that had a lower preference to socialize in Spanish (higher Language Use subscale scores) (OR 0.61 95% CI [0.39–0.96], p = 0.031). Across all sources, prior non-prescription antibiotic use was a very strong predictor of the intention to use non-prescription antibiotics, with patients who reported previous non-prescription antibiotic use having over 12.3 times more intention to use non-prescription antibiotics in the future than patients who did not report prior non-prescription antibiotic use (95% CI [6.6–23.1], p < 0.001) (Table 8).
4. Discussion
This study investigated the effects of acculturation and subjective norms on Hispanic individuals’ intentions to use antibiotics without a prescription from the following sources: (1) markets in the United States (illegal), (2) other countries, (3) leftovers from previous prescriptions, and (4) friends/relatives. Our results underscore the alarmingly high proportion of Hispanic patients that have reported non-prescription antibiotic use in the past (47%) or intended to use them in the future (54%). We found that lower acculturation (i.e., language use and ethnic and social relations) and subjective norms favoring non-prescription antibiotic use were associated with higher patient intentions to use non-prescription antibiotics in the future. Simultaneously, healthcare system obstacles (i.e., high doctor visit costs and language barriers at the clinics) were associated with higher intended non-prescription antibiotic use.
Individuals of Hispanic heritage are one of the fastest-growing and largest foreign-born ethnic groups and are estimated to represent 25% of the entire US population by 2050 [22]. Across all sources, Hispanic patients born outside the US had nearly 8.5 times more intention to use non-prescribed antibiotics in our study. Similarly, studies in the US, Australia, and the United Kingdom have shown that immigrants may continue to practice self-medication behaviors that were common in their home countries, including using antibiotics without a prescription, for familiarity, convenience, sociocultural, and financial reasons [23,24,25]. Thus, it is imperative to understand the sociocultural factors that contribute to non-prescription antibiotic use to prevent this potentially unsafe practice. In addition, our results showed that patients’ prior non-prescription antibiotic use in the past year was a strong predictor of the intention to use non-prescription antibiotics in the future across all sources (OR 6.26 to 12.32, p < 0.001). These collective results pose an opportunity to develop antibiotic stewardship messaging based on the emerging recognition of the role of acculturation and social norms on non-prescription antibiotic use [26]. Healthcare professionals and health educators can promote safe antibiotic use as a social norm during patient–clinician counseling while also providing information on the individual-level harms and risks associated with antibiotic use, including Clostridium difficile infection, adverse effects, or drug interactions [26].
This research complements a growing body of literature on the association(s) between acculturation, subjective norms, and health behavior in Hispanic populations. Most prior research on these associations has focused on other health outcomes, including postpartum depression, nutrition, exercise, obesity, and cardiovascular disease (CVD), rather than inappropriate antibiotic use [11,13,27,28]. In this study, acculturation and subjective norms played an important role in Hispanic patients’ decisions to use non-prescription antibiotics. Specifically, we found correlations between lower acculturation (language use and ethnic and social relations subscale scores) and higher patient intentions to use non-prescribed antibiotics in the future, which is a novel finding. Similar to our results, a study in Texas found that less acculturated (by generational scores) Hispanic individuals were more likely to purchase antibiotics across the US–Mexico border, presumably without a prescription [11]. The lack of studies exploring the effects of acculturation on antibiotic use warrants further investigation into other ethnic groups across the US and other countries.
Our findings also highlight some specific healthcare barriers, including the high costs of doctor visits, long clinic waits (e.g., to schedule appointments or during doctor visits), and a lack of health insurance or health coverage, which impact Hispanic patients’ decisions to use non-prescription antibiotics [3,12]. Patients who experience the burden of high costs during a doctor’s visit also had three times higher intended non-prescription antibiotic use from the US and friends and relatives in comparison to patients that did not report high costs during a doctor’s visit as a problem. Another study also found that individuals without health insurance were over three times more likely to purchase antibiotics outside the US, presumably without a prescription [11]. In our previous qualitative study, high copayments (for a doctor’s visit and subsequent prescription medications), regardless of patients having healthcare coverage, drove some patients to seek informal medical advice and source non-prescription medications using their social networks [12]. Future research should leverage and promote appropriate antibiotic use as a social norm for Hispanic patients with and without healthcare coverage [13,29]. Specifically, engaging Hispanic communities with individuals whom they trust, such as community pharmacists and community healthcare workers (i.e., “promotoras”), in community stewardship interventions can help patients navigate the complex healthcare system [12,29]. A comprehensive approach that improves access to primary care may reduce non-prescription antibiotic use [12,29]. Moreover, antimicrobial stewardship programs administered by multidisciplinary teams [30] in hospital settings have led to beneficial clinical and economic impacts [31,32]. Therefore, implementing stewardship programs in outpatient settings could lead to similar outcomes, such as reducing inappropriate antibiotic use and limiting antimicrobial resistance.
Our study also identified the language barriers that Hispanic individuals may face during a doctor’s visit. Patients reporting language barriers as a problem during their healthcare visit reported three times more intended non-prescription antibiotic use from leftover sources. Hispanic patients’ negative healthcare experiences can have detrimental consequences. For instance, a recent Pew research study showed that approximately 50% of Hispanic Americans had negative healthcare experiences and difficulties getting needed healthcare, and 30% of Hispanic adults reported having to “speak up” (voice their concerns) to their doctors to get appropriate care [33]. For patients experiencing language barriers or limited English proficiency, this could be particularly discouraging, promoting alternative medical-seeking behaviors [12]. Similarly, compared to bilingual or English-only speaking Hispanic individuals surveyed, about 81% of the Spanish-speaking adults preferred seeing Spanish-speaking healthcare providers [33]. Addressing language barriers with language-concordant healthcare initiatives is important to mitigate communication pitfalls in medical care and has been shown to improve health outcomes [34].
Our study has certain limitations. First, our study does not compare Hispanic ethnic subgroups, and these communities encompass diverse cultures, backgrounds, and experiences. However, according to the US census and the Texas Demographics Center, Mexicans are the largest ethnic subgroup, representing 62% of all Hispanic people living in the US and 83% of all Hispanic people in Texas; thus, the Hispanic patients in this survey may represent the largest US Hispanic demographic subgroup [35,36]. Second, we did not account for immigration history or generational status (e.g., we did not ask patients about their parents’ or grandparents’ ancestry or when people first came to the US). To adjust for this, we calculated the median years lived in the US, but this factor was not a significant predictor of patient intentions to use non-prescription antibiotics. Third, the SASH scale may not account for all aspects of acculturation. Additionally, the SASH scale does not have any measures regarding the cultural context surrounding where study participants received their care (e.g., clinics and pharmacies). Nevertheless, the SASH scale has been found to have both high internal consistency and validity in measuring the language, media, and ethnic and social relations aspects of acculturation in many studies across a wide array of Hispanic subgroups [13,20,28]. Lastly, a social desirability response bias may have occurred despite our best efforts to phrase questions neutrally. Thus, the true prevalence rate of non-prescription antibiotic use may be underestimated, because patients may have had concerns about the legality or otherwise disclosing these behaviors or participating in the survey.
In summary, our results indicate that lower acculturation and subjective norms favoring non-prescription antibiotic use were associated with higher Hispanic patient intentions to use non-prescription antibiotics in the future. In addition, healthcare system obstacles, such as the high costs of doctor visits and language barriers, were associated with a higher intended non-prescription antibiotic use among Hispanic patients.
In conclusion, this study adds value to the scientific literature on the association(s) between acculturation, subjective norms, and health behavior in Hispanic populations. Reducing non-prescription antibiotic use in Hispanic communities in the US will require a multifaceted approach considering the sociocultural and healthcare barriers that influence non-prescription antibiotic use. Future stewardship interventions can leverage social and cultural factors to promote appropriate antibiotic use normative behaviors in Hispanic communities to reduce adverse health effects and antimicrobial resistance.
Appendix A. Survey Questions
Sociodemographic Questions:
-
1.
How old are you? ____
-
2.Sex
-
☐Male
-
☐Female
-
☐Other: __________
-
☐
-
3.Do you consider yourself to be Hispanic/Latino?
-
☐Yes
-
☐No
-
☐
-
4.Which category best describes your race?
-
☐Black or African American
-
☐White
-
☐Declined
-
☐Other, please specify: __________________________
-
☐
-
5.What is the highest level of education you have completed?
-
☐Never attended school
-
☐Grades 1 through 5 (Elementary)
-
☐Grades 6 through 8 (Middle School)
-
☐Grades 9 through 11 (Some High School)
-
☐Grades 12 or GED (High School graduate)
-
☐College 1 year to 3 years (Some college or technical school)
-
☐College 4 years or more (College graduate)
-
☐
-
6.What was the total annual income in your household in the past year?
-
☐Less than $20,000
-
☐$20,000 or more but less than $40,000
-
☐$40,000 or more but less than $60,000
-
☐$60,000 or more but less than $100,000
-
☐More than $100,000
-
☐Don’t know/prefer not to say
-
☐
-
7.Which of the following health insurance plans do you have? (Mark all that apply)
-
☐Medicaid
-
☐Medicare
-
☐Harris Health System/Gold card* *County Financial Assistance program
-
☐None
-
☐Other: ________________________
-
☐
-
8.Where were you born?
-
☐United States
-
☐Other, please specify: _________________________
-
☐
-
9.
How many years have you lived in the United States? ________
Previous use of antibiotics without a prescription:
- When was your most recent experience with taking an antibiotic without contacting a doctor/dentist/nurse? (Please include occasions where you took leftover antibiotics)
-
☐Never
-
☐Less than 6 months ago
-
☐Between 6 and 12 months ago
-
☐More than 12 months but less than 2 years ago
-
☐At least 2 years ago
-
☐I don’t remember
-
☐
Intention to use antibiotics without a prescription:
If you were feeling sick, would you take antibiotics in the following situations without contacting a doctor/nurse/dentist/clinic?
| Yes | No | Don’t Know | |
| You can buy antibiotics without a prescription in the United States. | |||
| You can buy antibiotics without a prescription in another country. If yes, please specify: | |||
| Friends/relatives give you antibiotics. | |||
| You have leftover antibiotics from a previous prescription. |
Social Norms Questions:
-
1.How many of your friends or relatives use antibiotics without contacting a doctor? For example: Do they use leftover antibiotics from a previous prescription, use antibiotics they bought at a flea market, or use antibiotics they bought on the Internet?
-
☐All
-
☐Most
-
☐About half
-
☐Some
-
☐None
-
☐Don’t remember/Don’t know
-
☐
-
2.How many of your friends or relatives get antibiotics from another country? Please specify the country/countries:
-
☐Most
-
☐About half
-
☐Some
-
☐None
-
☐Don’t remember/ Don’t know
-
☐
Brief Health Literacy Screen measure:
-
1.How often do you have problems learning about your medical condition because of difficulty understanding written information?
-
☐Never
-
☐Occasionally
-
☐Sometimes
-
☐Often
-
☐Always
-
☐
-
2.How confident are you filling out medical forms by yourself?
-
☐Extremely
-
☐Quite a bit
-
☐Somewhat
-
☐A little bit
-
☐Not at all
-
☐
-
3.How often do you have someone help you read clinic or hospital materials?
-
☐Never
-
☐Occasionally
-
☐Sometimes
-
☐Often
-
☐Always
-
☐
Barriers to care questions specific to the patient population of the safety-net healthcare system:
For your medical appointments in the last 12 months, how much of a problem is each of the following for you?
| Not a problem |
Minor problem |
Major problem |
Not applicable |
|
| 1(a) Transportation | ||||
| 1(b) Long waiting times in the clinic | ||||
| 1(c) High cost of doctor visit | ||||
| 1(d) Language barrier | ||||
| 1(e) Not having a regular doctor |
Acculturation Questions
The following questions have been approved by previous research studies. This set of questions is used to measure the level at which an individual has adopted the traits and characteristics shared by a society. The Short Acculturation Scale for Hispanics is comprised of three subscales (Language Use, Media, and Ethnic Social Relations). Scores range from 1 (all Latinos/Hispanics)–5 (all non-Latinos/Hispanics).
| Only Spanish | Spanish better than English | Both equally | English better than Spanish | Only English | |
|
|||||
|
|||||
|
|||||
|
|||||
|
|||||
|
|||||
|
|||||
|
|||||
|
|||||
|
|||||
|
|||||
|
Appendix B. Short Acculturation Scale for Hispanics Reliability Statistics
| Acculturation Scores | Median (IQR‡) |
Corrected
Cronbach’s Alpha † |
If item Deleted
Cronbach’s Alpha † |
| Short Acculturation Scale for Hispanics * (n = 259) | |||
| Language Use Subscale Score | 2.00 (1.20–3.20) | 0.939 | 0.939 |
| Individual Language Subscale Questions | |||
| In general, what language(s) do you read and speak? | 2.00 (2.00–3.00) | 0.900 | 0.916 |
| What was the language you used as a child? | 1.00 (1.00–2.00) | 0.750 | 0.939 |
| What language(s) do you usually speak at home? | 2.00 (1.00–4.00) | 0.813 | 0.929 |
| In what language do you usually think? | 2.00 (1.00–4.00) | 0.879 | 0.917 |
| What language do you usually speak with your friends? | 2.00 (1.00–4.00) | 0.862 | 0.920 |
| Media Subscale Score | 3.00 (1.33–4.00) | 0.969 | 0.969 |
| Individual Media Subscale Questions | |||
| In what language(s) are the TV programs you usually watch? | 3.00 (1.00–4.00) | 0.953 | 0.940 |
| What language(s) are the radio programs you usually listen to? | 3.00 (1.00–4.00) | 0.910 | 0.971 |
| In general, in what language(s) are the movies, TV and radio programs you prefer to watch and listen to? | 3.00 (1.00–4.00) | 0.938 | 0.951 |
| Ethnic Social Relations Subscale Score † | 2.33 (2.00–3.00) | 0.754 | 0.754 |
| Individual Ethnic Social Relation Questions | |||
| Your close friends are: | 2.00 (2.00–3.00) | 0.709 | 0.598 |
| You prefer going to social gatherings/parties at which people are: | 3.00 (2.00–3.00) | 0.593 | 0.673 |
| The persons you visit or who visit you are: | 2.00 (2.00–3.00) | 0.709 | 0.598 |
| If you could choose your children’s friends, you would want them to be: † (n = 254) | 3.00 (3.00–3.00) | 0.263 | 0.817 |
| Acculturation Subscale Aggregate Score † | 2.44 (1.67–3.29) | 0.939 | |
| * The Short Acculturation Scale for Hispanics is comprised of three subscales (Language Use, Media, and Ethnic Social Relations). Scores range from 1 (Only Spanish) to 5 (Only English) for the Language and Media Subscales and 1 (all Latinos/Hispanics) to 5 (all non-Latinos/Hispanics) for the Ethnic Social Relations subscale. A higher score indicates higher levels of acculturation [20]. ‡ Interquartile Range. † Questions relating to each subscale score were included following the Marin et al. method that uses the principal components analysis (PCA) [20]. The PCA revealed the questions that accurately described each subscore (e.g., language, television and media, and social acculturation subscores). All questions with interitem correlation (IC) scores above 0.5 (except question 12, IC = 0.3) were included in the development of the subscores with the highest reliability (Cronbach’s alpha > 0.8). | |||
Appendix C. Patient Reported Barriers to Healthcare Access and Patient-Doctor Communication (n = 262)
| Total No. (%) | |
| Barriers To Healthcare Access In The Last 12 Months (n = 262 *) | |
| For your medical appointments in the last 12 months, how much of a problem is transportation? | |
| Not a problem | 220 (83.7) |
| A problem | 42 (15.9) |
| For your medical appointments in the last 12 months, how much of a problem is long waiting times? | |
| Not a problem | 195 (74.1) |
| A problem | 67 (25.5) |
| For your medical appointments in the last 12 months, how much of a problem is high cost of doctor visits? | |
| Not a problem | 220 (83.7) |
| A problem | 42 (16.0) |
| For your medical appointments in the last 12 months, how much of a problem is a language barrier. | |
| Not a problem | 242 (92.0) |
| A problem | 20 (7.6) |
| For your medical appointments in the last 12 months, how much of a problem is not having a regular doctor? | |
| Not a problem | 250 (95.4) |
| A problem | 12 (4.6) |
| * One patient did not answer these questions. | |
Appendix D. Univariate Regression Results
| Univariate Analysis | ||||||||||
| Bought without a Prescription in the US | From Another Country | From Friends/Relatives | From Leftover | Overall Intended Use | ||||||
| Predictor | OR (95% CI) | p-Value * | OR (95% CI) | p-Value * | OR (95% CI) | p-Value * | OR (95% CI) | p-Value * | OR (95% CI) | p-Value * |
| Age (y) | 0.97 (0.95–0.10) | 0.015 | 0.98 (0.96–1.00) | 0.073 | 0.98 (0.96–1.00) | 0.056 | 0.10 (0.98–1.02) | 0.710 | 0.99 (0.97–1.01) | 0.167 |
| Sex | ||||||||||
| Female | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Male | 0.97 (0.51–1.87) | 0.931 | 1.04 (0.56–1.94) | 0.908 | 0.57 (0.31–1.04) | 0.068 | 0.82 (0.48–1.43) | 0.489 | 0.76 (0.43–1.32) | 0.328 |
| Education | ||||||||||
| Less than high school | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| High school or GED | 1.42 (0.68–2.97) | 0.352 | 0.91 (0.46–1.80) | 0.783 | 0.82 (0.40–1.65) | 0.569 | 1.28 (0.72–2.29) | 0.398 | 1.31 (0.74–2.34) | 0.358 |
| Some college and above | 2.21 (1.04–4.71) | 0.039 | 1.80 (0.90–3.58) | 0.094 | 1.92 (0.96–3.86) | 0.065 | 1.30 (0.69–2.43) | 0.414 | 1.27 (0.68–2.38) | 0.450 |
| Healthcare System | ||||||||||
| Public | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Private | 0.32 (0.11–0.94) | 0.038 | 0.74 (0.34–1.65) | 0.463 | 0.57 (0.24–1.35) | 0.202 | 0.22 (0.10–0.50) | <0.001 | 0.33 (0.16–0.67) | <0.002 |
| Insurance | ||||||||||
| Private or Medicare | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Medicaid or county assistance program § | 2.20 (1.07–4.53) | 0.032 | 1.33 (0.70–2.50) | 0.385 | 1.85 (0.94–3.68) | 0.077 | 1.35 (0.78–2.33) | 0.285 | 1.30 (0.75–2.24) | 0.350 |
| Self-pay | 0.38 (0.05–3.19) | 0.374 | 1.12 (0.32–3.92) | 0.862 | 1.56 (0.44–5.63) | 0.493 | 0.08 (0.01–0.66) | 0.019 | 0.43 (0.14–1.36) | 0.151 |
| Country of birth | ||||||||||
| Born in the US | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Born in other countries ‖ | 1.71 (0.94–3.11) | 0.081 | 1.14 (0.63–2.05) | 0.663 | 1.68 (0.94–3.01) | 0.082 | 2.19 (1.28–3.73) | 0.004 | 2.45 (1.41–4.26) | 0.002 |
| Years Lived in the USA (n = 182) | 1.00 (0.99–1.02) | 0.646 | 0.98 (0.97–1.00) | 0.077 | 1.00 (0.98–1.01) | 0.666 | 1.02 (1.00–1.03) | 0.030 | 1.01 (1.00–1.03) | 0.184 |
| Survey language | ||||||||||
| English | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Spanish | 1.75 (0.98–3.13) | 0.059 | 1.02 (0.59–1.18) | 0.942 | 1.27 (0.72–2.23) | 0.403 | 1.78 (1.08–2.92) | 0.023 | 1.81 (1.10–3.00) | 0.020 |
| Prior Non-Prescription Antibiotic Use | ||||||||||
| No Prior Use | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Prior Use | 0.17 (0.08–0.33) | <0.001 | 0.11 (0.53–0.21) | <0.001 | 0.12 (0.06–0.24) | <0.001 | 0.13 (0.07–0.22) | <0.001 | 0.09 (0.05–0.15) | <0.001 |
| Acculturation Scale ¶ | ||||||||||
| Language Use Subscale | 1.18 (0.94–1.50) | 0.161 | 0.93 (0.74–1.18) | 0.561 | 1.05 (0.83–1.32) | 0.686 | 1.26 (1.02–1.55) | 0.029 | 1.24 (1.00–1.53) | 0.047 |
| Media Subscale | 1.14 (0.93–1.40) | 0.209 | 0.97 (0.80–1.18) | 0.767 | 1.10 (0.91–1.35) | 0.328 | 1.19 (1.00–1.42) | 0.052 | 1.12 (0.94–1.34) | 0.189 |
| Ethnic Social Relations Subscale | 0.80 (0.53–1.22) | 0.295 | 0.68 (0.45–1.01) | 0.057 | 0.82 (0.54–1.23) | 0.336 | 1.08 (0.75–1.54) | 0.682 | 1.00 (0.70–1.43) | 0.996 |
| Total Acculturation | 1.16 (0.86–1.57) | 0.340 | 0.88 (0.66–1.18) | 0.400 | 1.07 (0.80–1.43) | 0.674 | 1.30 (1.00–1.68) | 0.050 | 1.21 (0.94–1.57) | 0.141 |
| Social Norms Questions | ||||||||||
| How many of your friends or relatives use antibiotics without contacting a doctor? | ||||||||||
| None | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Don’t Remember/Don’t Know | 2.07 (0.69–6.19) | 0.193 | 2.02 (0.77–5.33) | 0.155 | 1.20 (0.48–3.01) | 0.693 | 1.10 (0.49–2.48) | 0.817 | 0.93 (0.42–2.06) | 0.853 |
| All/Most/About half | 2.01 (0.66–6.12) | 0.220 | 1.75 (0.65–4.73) | 0.269 | 2.27 (0.94–5.43) | 0.067 | 1.53 (0.67–3.50) | 0.309 | 1.20 (0.56–2.86) | 0.580 |
| Some | 2.26 (0.80–6.42) | 0.126 | 1.52 (0.59–3.87) | 0.384 | 2.00 (0.96–4.19) | 0.066 | 1.66 (0.78–3.56) | 0.190 | 1.11 (0.52–2.34) | 0.795 |
| How many of your friends or relatives get antibiotics from another country? | ||||||||||
| None | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Don’t Remember/Don’t Know | 1.10 (0.44–2.72) | 0.838 | 1.89 (0.82–4.39) | 0.138 | 1.41 (0.49–4.04) | 0.523 | 1.01 (0.49–2.09) | 0.974 | 1.07 (0.52–2.21) | 0.853 |
| All / Most / About half | 1.66 (0.69–4.02) | 0.262 | 1.86 (0.78–4.45) | 0.165 | 2.29 (0.81–6.42) | 0.116 | 1.19 (0.56–2.52) | 0.657 | 1.32 (0.62–2.81) | 0.478 |
| Some | 1.41 (0.67–2.96) | 0.365 | 1.74 (0.84–3.61) | 0.137 | 2.13 (0.80–5.66) | 0.128 | 1.22 (0.66–2.23) | 0.526 | 1.19 (0.65–2.18) | 0.575 |
| Barriers To Healthcare Access In The Last 12 Months | ||||||||||
| For your medical appointments in the last 12 months, how much of a problem is [ ]? | ||||||||||
| Transportation | ||||||||||
| Not a problem | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| A problem | 0.61 (0.29–1.26) | 0.178 | 0.78 (0.38–1.60) | 0.499 | 0.62 (0.30–1.26) | 0.187 | 0.79 (0.41–1.52) | 0.475 | 0.62 (0.31–1.23) | 0.171 |
| Long waiting times | ||||||||||
| Not a problem | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| A problem | 0.75 (0.39–1.42) | 0.372 | 0.99 (0.53–1.85) | 0.975 | 0.99 (0.52–1.87) | 0.968 | 1.47 (0.83–2.58) | 0.183 | 1.14 (0.65–1.98) | 0.656 |
| High cost of doctor visits | ||||||||||
| Not a problem | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| A problem | 0.36 (0.18–0.72) | 0.004 | 0.53 (0.26–1.06) | 0.072 | 0.42 (0.21–0.84) | 0.015 | 0.63 (0.32–1.22) | 0.167 | 0.62 (0.31–1.23) | 0.171 |
| A language barrier | ||||||||||
| Not a problem | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| A problem | 0.73 (0.25–2.13) | 0.568 | 0.41 (0.16–1.04) | 0.061 | 0.51 (0.19–1.34) | 0.172 | 0.33 (0.12–0.90) | 0.031 | 0.35 (0.12–0.99) | 0.049 |
| Not having a regular doctor | ||||||||||
| Not a problem | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| A problem | 2.19 (0.87–5.52) | 0.096 | 1.81 (0.75–4.38) | 0.191 | 3.52 (1.47–8.46) | 0.005 | 0.95 (0.41–2.20) | 0.207 | 1.00 (0.43–2.32) | 0.995 |
| Health Literacy | ||||||||||
| Adequate health literacy ‡ | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |||||
| Inadequate health literacy ‡ | 1.10 (0.56–2.17) | 0.778 | 0.93 (0.50–1.74) | 0.821 | 0.93 (0.49–1.76) | 0.821 | 1.15 (0.65–2.01) | 0.637 | 1.21 (0.69–2.13) | 0.502 |
| * Results shown in boldface type have a p-value of <0.2 in the univariate analyses and were thus included in the multivariate analysis. ¶ The Short Acculturation Scale for Hispanics is comprised of three subscales (Language Use, Media, and Ethnic Social Relations). Scores range from 1 (all Latinos/Hispanics) to 5 (all non-Latinos/Hispanics). Higher score indicates higher levels of acculturation [20]. § County Financial Assistance Program: Includes those who have benefits from the county, allowing access to public clinic providers at either very low cost or no cost. ‖ Includes 1 Columbia, 1 Costa Rica, 6 Cuba, 1 Dominican Republic, 14 El Salvador, 6 Guatemala, 15 Honduras, 131 Mexico, 2 Nicaragua, 1 Panama, 1 Peru, and 3 Venezuela (countries are listed in alphabetical order). ‡ Calculated using the three questions from the Brief Health literacy Screen measure [18,19]. | ||||||||||
Author Contributions
Conceptualization, L.A.L., L.G., B.W.T., S.N. and M.K.P.-O.; methodology, L.A.L. and L.G.; software, L.A.L.; validation, L.A.L.; formal analysis, L.A.L.; investigation, L.A.L.; resources, K.O. and J.S.; data curation, K.O., J.S. and O.A.; writing—original draft preparation, L.A.L.; writing—review and editing, L.A.L., L.G., B.W.T., S.N., R.Z., K.O., J.S. and M.K.P.-O.; visualization, L.A.L. and K.O.; supervision, L.G.; project administration, L.G., B.W.T., J.S. and K.O.; and funding acquisition, L.G., R.Z. and B.W.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Baylor College of Medicine and Affiliated Hospitals (protocol H-45709).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
Conflicts of Interest
B.W.T. reports grants or contracts from the VA Health Services Research & Development, Agency for Healthcare Research and Quality R18, Craig H. Neilson Foundation, Genentech, and Peptilogics, Inc.; payment from George Washington ID Board for a Review Course; travel support for meeting attendance from the VA Office of Research & Development and the Infectious Diseases Society of America; and an unpaid role on a DSMB for CSP #2004. L.G. reports grants or contracts from the Agency for Healthcare Research and Quality (AHRQ) R18, Craig H. Neilsen Foundation, and a research education grant (1R25AA028203-01) from the National Institute on Alcohol Abuse and Alcoholism Award. All other authors report no potential conflicts.
Funding Statement
This work was supported by grant number R01HS026901 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. L.L.’s work was supported by the Ruth L. Kirschstein National Research Service Award (NRSA T-32 6T32HC10031). B.W.T.’s work was supported in part by the U.S. Department of Veterans Affairs Health Services Research and Development Service (grant no. CIN 13-413) at the Center for Innovations in Quality, Effectiveness, and Safety. The contents presented herein do not represent the views of the U.S. Department of Veterans Affairs or the U.S. government.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Morgan D.J., Okeke I.N., Laxminarayan R., Perencevich E.N., Weisenberg S. Non-prescription antimicrobial use worldwide: A systematic review. Lancet Infect. Dis. 2011;11:692–701. doi: 10.1016/S1473-3099(11)70054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun R., Yao T., Zhou X., Harbarth S., Lin L. Non-biomedical factors affecting antibiotic use in the community: A mixed-methods systematic review and meta-analysis. Clin. Microbiol. Infect. 2022;28:345–354. doi: 10.1016/j.cmi.2021.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Grigoryan L., Paasche-Orlow M.K., Alquicira O., Laytner L., Schlueter M., Street R.L., Salinas J., Barning K., Mahmood H., Porter T.W., et al. Antibiotic use without a Prescription: A multi-site Survey of Patient, Health System, and Encounter Characteristics. Clin. Infect. Dis. 2023;77:510–517. doi: 10.1093/cid/ciad241. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal K.G., Peter J.G., Trubiano J.A., Phillips E.J. Antibiotic allergy. Lancet. 2019;393:183–198. doi: 10.1016/S0140-6736(18)32218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang L., Bajinka O., Jarju P.O., Tan Y., Taal A.M., Ozdemir G. The varying effects of antibiotics on gut microbiota. AMB Express. 2021;11:116. doi: 10.1186/s13568-021-01274-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO Antimicrobial Resistance. [(accessed on 13 September 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
- 7.Ahmed I., King R., Akter S., Akter R., Aggarwal V.R. Determinants of antibiotic self-medication: A systematic review and meta-analysis. Res. Social. Adm. Pharm. 2023;19:1007–1017. doi: 10.1016/j.sapharm.2023.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Anderson A. Antibiotic Self-Medication and Antibiotic Resistance: Multilevel Regression Analysis of Repeat Cross-Sectional Survey Data in Europe. REGION. 2021;8:121–145. doi: 10.18335/region.v8i2.339. [DOI] [Google Scholar]
- 9.Grigoryan L., Germanos G., Zoorob R., Juneja S., Raphael J.L., Paasche-Orlow M.K., Trautner B.W. Use of Antibiotics Without a Prescription in the U.S. Population: A Scoping Review. Ann. Intern. Med. 2019;171:257–263. doi: 10.7326/M19-0505. [DOI] [PubMed] [Google Scholar]
- 10.Watkins L.K.F., Sanchez G.V., Albert A.P., Roberts R.M., Hicks L.A. Knowledge and attitudes regarding antibiotic use among adult consumers, adult Hispanic consumers, and health care providers—United States, 2012–2013. Morb. Mortal. Wkly. Rep. 2015;64:767. doi: 10.15585/mmwr.mm6428a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Essigmann H.T., Aguilar D.A., Perkison W.B., Bay K.G., Deaton M.R., Brown S.A., Hanis C.L., Brown E.L. Epidemiology of Antibiotic Use and Drivers of Cross-Border Procurement in a Mexican American Border Community. Front. Public. Health. 2022;10:832266. doi: 10.3389/fpubh.2022.832266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laytner L., Chen P., Nash S., Paasche-Orlow M.K., Street R., Zoorob R., Trautner B., Grigoryan L. Perspectives on Non-Prescription Antibiotic Use among Hispanic Patients in the Houston Metroplex. J. Am. Board. Fam. Med. 2023;36:390–404. doi: 10.3122/jabfm.2022.220416R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abraído-Lanza A.F., Echeverría S.E., Flórez K.R. Latino Immigrants, Acculturation, and Health: Promising New Directions in Research. Annu. Rev. Public Health. 2016;37:219–236. doi: 10.1146/annurev-publhealth-032315-021545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abraído-Lanza A.F., Armbrister A.N., Flórez K.R., Aguirre A.N. Toward a theory-driven model of acculturation in public health research. Am. J. Public. Health. 2006;96:1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ham M., Jeger M., Frajman Ivković A. The role of subjective norms in forming the intention to purchase green food. Econ. Res.-Ekon. Istraživanja. 2015;28:738–748. doi: 10.1080/1331677X.2015.1083875. [DOI] [Google Scholar]
- 16.Zoorob R., Grigoryan L., Nash S., Trautner B.W. Nonprescription Antimicrobial Use in a Primary Care Population in the United States. Antimicrob. Agents Chemother. 2016;60:5527–5532. doi: 10.1128/AAC.00528-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kilbourne A.M., Switzer G., Hyman K., Crowley-Matoka M., Fine M.J. Advancing health disparities research within the health care system: A conceptual framework. Am. J. Public. Health. 2006;96:2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chew L.D., Bradley K.A., Boyko E.J. Brief questions to identify patients with inadequate health literacy. Fam. Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 19.Chew L.D., Griffin J.M., Partin M.R., Noorbaloochi S., Grill J.P., Snyder A., Bradley K.A., Nugent S.M., Baines A.D., Vanryn M. Validation of screening questions for limited health literacy in a large VA outpatient population. J. Gen. Intern. Med. 2008;23:561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marin G., Sabogal F., Marin B.V., Otero-Sabogal R., Perez-Stable E.J. Development of a Short Acculturation Scale for Hispanics. Hisp. J. Behav. Sci. 1987;9:183–205. doi: 10.1177/07399863870092005. [DOI] [Google Scholar]
- 21.IBM Corp . IBM SPSS Statistics for Windows, Version 28.0. IBM Corp; Armonk, NY, USA: 2021. [Google Scholar]
- 22.Zong J. A Mosaic, Not a Monolith: A Profile of the U.S. Latino Population, 2000–2020. [(accessed on 12 June 2023)]. Available online: https://latino.ucla.edu/research/latino-population-2000-2020/#:~:text=Since%20then%2C%20Latinos%20have%20been,population%20(see%20Figure%201)
- 23.Sanchez J. Self-Medication Practices among a Sample of Latino Migrant Workers in South Florida. Front. Public Health. 2014;2:108. doi: 10.3389/fpubh.2014.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu J., Wang Z. Non-prescribed antibiotic use and general practitioner service utilisation among Chinese migrants in Australia. Aust. J. Prim. Health. 2016;22:434–439. doi: 10.1071/PY15076. [DOI] [PubMed] [Google Scholar]
- 25.Lindenmeyer A., Redwood S., Griffith L., Ahmed S., Phillimore J. Recent migrants’ perspectives on antibiotic use and prescribing in primary care: A qualitative study. Br. J. Gen. Pract. 2016;66:e802–e809. doi: 10.3399/bjgp16X686809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miller B.J., Carson K.A., Keller S. Educating Patients on Unnecessary Antibiotics: Personalizing Potential Harm Aids Patient Understanding. J. Am. Board. Fam. Med. 2020;33:969–977. doi: 10.3122/jabfm.2020.06.200210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liyanage-Don N.A., Cornelius T., Romero E.K., Alcantara C., Kronish I.M. Association of Hispanic ethnicity and linguistic acculturation with cardiovascular medication adherence in patients with suspected acute coronary syndrome. Prev. Med. Rep. 2021;23:101455. doi: 10.1016/j.pmedr.2021.101455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lara M., Gamboa C., Kahramanian M.I., Morales L.S., Bautista D.E. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annu. Rev. Public. Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodriguez-Alcalá M.E., Qin H., Jeanetta S. The Role of Acculturation and Social Capital in Access to Health Care: A Meta-study on Hispanics in the US. J. Community Health. 2019;44:1224–1252. doi: 10.1007/s10900-019-00692-z. [DOI] [PubMed] [Google Scholar]
- 30.MacDougall C., Polk R.E. Antimicrobial stewardship programs in health care systems. Clin. Microbiol. Rev. 2005;18:638–656. doi: 10.1128/CMR.18.4.638-656.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nathwani D., Varghese D., Stephens J., Ansari W., Martin S., Charbonneau C. Value of hospital antimicrobial stewardship programs [ASPs]: A systematic review. Antimicrob. Resist. Infect. Control. 2019;8:35. doi: 10.1186/s13756-019-0471-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Albano G.D., Midiri M., Zerbo S., Matteini E., Passavanti G., Curcio R., Curreri L., Albano S., Argo A., Cadelo M. Implementation of A Year-Long Antimicrobial Stewardship Program in A 227-Bed Community Hospital in Southern Italy. Int. J. Environ. Res. Public Health. 2023;20:996. doi: 10.3390/ijerph20020996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cary F., Lopez M.H. Hispanic Americans’ Trust in and Engagement with Science. PEW Research Center; Washington, DC, USA: 2022. [Google Scholar]
- 34.Diamond L., Izquierdo K., Canfield D., Matsoukas K., Gany F. A Systematic Review of the Impact of Patient–Physician Non-English Language Concordance on Quality of Care and Outcomes. J. Gen. Intern. Med. 2019;34:1591–1606. doi: 10.1007/s11606-019-04847-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Office of Minority Health (OMH) Profile: Hispanic/Latino Americans. [(accessed on 11 July 2023)]; Available online: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64#:~:text=This%20group%20represents%2018.9%20percent,group%20after%20non%2DHispanic%20whites.
- 36.Texas Demographics Center (TDC) Hispanic Heritage Month: Hispanic Americans in Texas. [(accessed on 11 July 2023)]; Available online: https://demographics.texas.gov/Infographics/2021/HispanicHeritage.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.