Abstract
Simple Summary
Growth factors promote angiogenesis, which is a critical process in the development of tumors. One of the therapeutic techniques being investigated in the treatment of cancer is the inhibition of angiogenesis through the inhibition of growth factors. This article aims to summarize the mechanisms by which growth factors influence the unfavorable evolution of lung cancers via angiogenesis as well as the therapeutic approaches that have been developed or are currently being developed in order to provide a foundation for researchers to investigate this question further and for practitioners to discuss therapeutic strategies when confronted with a lung cancer patient.
Abstract
Research has shown the role of growth factors in lung cancer angiogenesis. Angiogenesis promotes lung cancer progression by stimulating tumor growth, enhancing tumor invasion, contributing to metastasis, and modifying immune system responses within the tumor microenvironment. As a result, new treatment techniques based on the anti-angiogenic characteristics of compounds have been developed. These compounds selectively block the growth factors themselves, their receptors, or the downstream signaling pathways activated by these growth factors. The EGF and VEGF families are the primary targets in this approach, and several studies are being conducted to propose anti-angiogenic drugs that are increasingly suitable for the treatment of lung cancer, either as monotherapy or as combined therapy. The efficacy of the results are encouraging, but caution must be placed on the higher risk of toxicity, outlining the importance of personalized follow-up in the management of these patients.
Keywords: angiogenesis, growth factors, lung cancer, tumor microenvironment, anti-angiogenic therapy
1. Introduction
With an estimated 2.2 million new cases and 1.8 million deaths, lung cancer was the second most commonly diagnosed cancer and the leading cause of cancer death in 2020 according to GLOBOCAN [1]. This cancer is broadly classified into two main types: the Non-Small Cell Lung Cancer (NSCLC) accounting for approximately 85% of cases, and the Small Cell Lung Cancer (SCLC), which is the most aggressive type, counts for about 15% of cases [2,3,4]. Despite the advancement of numerous therapeutic modalities, such as surgery, radiation therapy, chemotherapy, immunotherapy, and targeted therapy, the last two decades have been marked by a relatively low survival rate ranging from 10% to 20% in most countries, making lung cancer one of the deadliest cancers and a public health concern [1,5]. To address this issue, numerous treatment possibilities are being investigated, including those related to angiogenesis.
Angiogenesis is the development of new blood vessels that originate from already existing vasculature and is an important process in both normal and pathological conditions [6]. It has a significant impact in the progression and spread of cancers, particularly lung cancer [7,8]. Angiogenesis has been investigated for several years in several aspects, most notably its morphological characteristics, as determined by MRI, and its biological aspects, as determined by biomarker assays [9,10]. Researchers are interested in this phenomenon because it plays a substantial role in all tumoral processes and represents a new therapeutic avenue, as various compounds with anti-angiogenic properties are presently proposed as cancer treatments [7,11,12,13]. Many studies have proven the critical roles of Growth Factors in angiogenesis; nevertheless, the molecular processes underlying these roles, as well as how these mechanisms might be targeted in lung cancer therapy, are still to be fully understood. Furthermore, despite promising and encouraging results, medications targeting angiogenesis have only had limited clinical success in lung cancer treatment highlighting the need for a deeper understanding of this phenomenon and the therapeutic opportunities that arise from inhibiting the effects of Growth Factors [14,15,16,17].
2. Angiogenesis Affects the Lung Cancer Pattern through Several Mechanisms
Angiogenesis is essential in the development of lung cancer because it allows oxygen and nutrients to flow to rapidly developing tumor cells, contributing to tumor invasion and dissemination [7,18,19]. Angiogenesis may affect lung cancer pattern with a variety of methods.
2.1. Tumor Growth Enhancement
According to various study findings, angiogenesis provides cancer cells with an essential supply of oxygen and nutrients, aiding their rapid growth, and has been associated with an increase in tumor volume and a higher tumor grade in lung cancer [19,20]. This mechanism has been linked with numerous major angiogenic factors, including fibroblast growth factor 2 (FGF-2), epidermal growth factor (EGF), and vascular endothelial growth factor (VEGF). Indeed, the former growth factor promotes angiogenesis in lung cancer by stimulating endothelial cell migration and proliferation, which leads to the development of new blood vessels that support tumor growth [21,22].
2.2. Metastasis Promotion
Many studies agree that angiogenesis has a significant impact on tumorigenesis and metastatic processes by allowing tumor cells to spread through the creation of new blood circulation paths. Thus, the greater the neovascularization process, the greater the chance of metastasis. This indicates that there is a correlation between the amount of blood vessels that develop around the tumor and the metastatic potential of lung cancer [7,19,23]. Angiogenic factors including VEGF, FGF-2, and hypoxia-inducible factors (HIF) can also directly stimulate tumor cell proliferation, migration, and invasion [21,23,24,25,26].
2.3. Changes in Immunological Response in the Microenvironment
Indeed, angiogenesis can influence the immune response by promoting inflammation, which causes the release of pro-inflammatory cytokines, which promote cell survival and proliferation. These cytokines will also interact with immune cells, such as neutrophils and macrophages, encouraging the recruitment and infiltration of immune cells while also activating signaling pathways that promote angiogenesis. As a result, a vicious circle is formed, in which angiogenesis maintains the inflammatory process and the inflammatory process maintains angiogenesis [27,28]. Furthermore, these immune cells may help to build new blood vessels via a process known as vasculogenesis [19,29].
In addition to the aforementioned factors, new research has highlighted the contribution of epigenetic alterations in lung cancer angiogenesis, specifically how microRNAs influence pro- and anti-angiogenic factors [30,31,32]. During the typical immune response, the system generates a kind of self-tolerance that prevents immune cells from attacking indiscriminately via immune checkpoints. Tumor cells will stimulate checkpoint targets to protect themselves from being attacked in cancer. A preclinical trial combining angiogenesis inhibitors and immune checkpoint inhibitors produced promising results in targeting the intricate interplay between angiogenesis and immunological responses in lung cancer, demonstrating the potential for combination therapy to improve patient outcomes [31,33,34,35]. All of this emphasizes the significance of this research, which aims to reassess growth factors in order to better understand their role in the spectrum of lung cancer angiogenesis.
3. The Epidermal Growth Factor (EGF) Family, Their Receptors, and the Downstream
The EGF family is a group of glycoproteins that play roles in cell growth, survival, proliferation, and differentiation. These molecules are distinguished by a structural feature known as the “EGF-like domain,” which differentiates them from the others. This domain is in charge of the binding and activation of EGF receptors (EGFR) or similar receptors. Transforming growth factor alpha (TGF-alpha), amphiregulin (AREG), heparin-binding EGF-like growth factor (HB-EGF), beta-cellulin (BTC), epiregulin (EREG), and epigene (EPGN) are all members of the EGF family. Although each of these proteins has a unique biological function, they all have the ability to interact with EGFR to activate the downstream signaling pathways that drive cell proliferation, migration, and invasion [36,37,38].
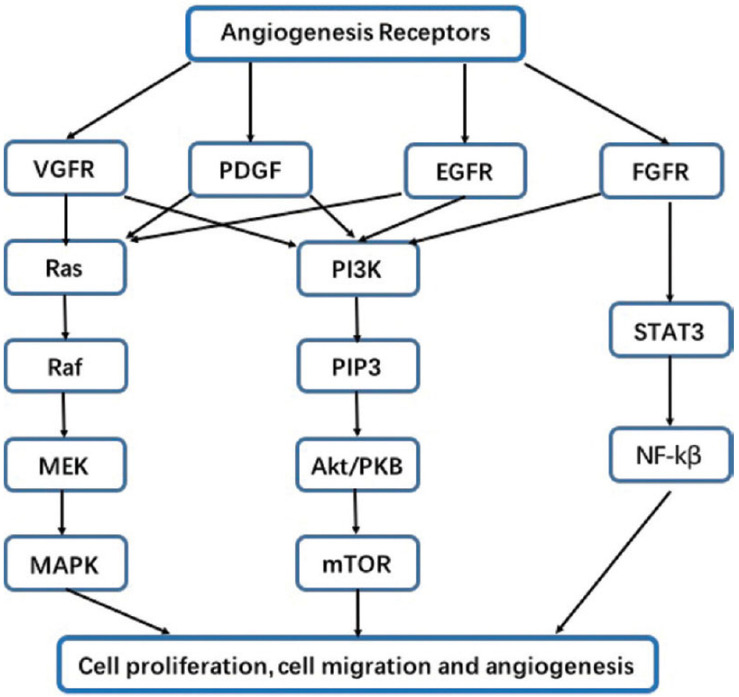
In a number of malignancies, including lung cancer, EGFR have been shown to be found in very high concentrations and also play an important role in angiogenesis, tumor formation, and progression. Indeed, members of the EGF family are especially prevalent in lung cancer, not only because of the cancerous inflammatory process, but also because these patients are vulnerable to external attacks by various pathogens, which maintain the inflammatory reaction and thus constantly stimulate EGF production. All these thereby promote the occurrence of EGF mutations [39,40,41]. When EGFR are activated, multiple downstream signaling pathways are activated, including the PI3K-Akt and MAPK-ERK pathways, which have been found to stimulate the production of pro-angiogenic factors, such as VEGF and bFGF (basic Fibroblast Growth Factor). Furthermore, stimulation of EGFR can activate downstream transcription factors, such as hypoxia-induced factor 1 (HIF-1), which will stimulate the production of VEGF genes, genes that will trigger the synthesis of pro-angiogenic VEGF molecules via the translation process. Pro-angiogenic molecules, such as VEGF, bFGF, and HIF-1, are thus boosted through these several processes, promoting the proliferation, migration, and formation of new blood vessels [25,42,43,44,45]. Figure 1 depicts the several pathways that will be activated upon receptor stimulation that ultimately contribute to the process of angiogenesis.
Figure 1.
Associated receptors and their signaling pathways involved in angiogenesis. On the figure we can identify the different angiogenesis receptors and the pathways they stimulate. These stimulations ultimately lead to a variety of processes involved in angiogenesis, such as cell proliferation, migration, and survival. EGFR stimulates the RAS/RAF/ERK/MAPK (also called MAPK-ERK) and the PI3K/Akt signaling pathways. These pathways are also stimulated by VGFR, PDGF, and FGFR. The latter (FDFR) also triggers the STAT3/NF-κβ pathway. Data source: Review article “Molecular mechanisms involved in angiogenesis and potential target of anti-angiogenesis in human glioblastomas” by Xu Y, Yuan FE, Chen QX, and Liu BH [46] and published in an open access journal.
Gefitinib, the first approved EGFR-TKI (EGFR—Tyrosine Kinase Inhibitors), was shown to be effective in treating non-small cell lung cancer (NSCLC) patients with EGFR mutations, leading to improved progression-free survival and response rates. Since then, many generations have been developed, and the fourth generation is now on the pre-clinical stage of development and aims to solve not only the problem of mutation of EGFR, but also resistance to the drugs of the third generation (Rociletinib and Osimertinib) [39,47].
Recent laboratory and clinical studies, such as that of Nakagawa et al. and that of Subbiah et al., have revealed new targets and therapeutic treatments centered on EGF family members and their influence on lung cancer angiogenesis [48,49,50]. In 2022, a study published by Nakagawa et al. found that targeting the EGF receptor in conjunction with anti-VEGF medication results in improved survival rates in lung cancer patients, pinpointing the potential advantage of targeting several pro-angiogenic pathways [48]. However, this should be approached with caution because certain studies have identified the possibility of toxicity leading to therapeutic termination [48,51]. Other studies also found that the EGF-like domain of HB-EGF increases angiogenesis in lung cancer by stimulating VEGF production and then driving endothelial cell migration and neovascularization [21,52].
In a clinical trial conducted by Rosell in 2017, the combination of the EGFR inhibitor erlotinib and the VEGFR inhibitor bevacizumab led to an increase in survival in individuals having advanced NSCLC, probably due to the synergistic effects of blocking both the EGF and VEGF pro-angiogenic pathways [53]. Other clinical trials have focused on the development of new EGF/EGFR targeted therapies, such as monoclonal antibodies and TKI, which may provide patients with lung cancer with better therapeutic alternatives [54,55].
Many clinical trials have primarily targeted the EGF pathway alone or in conjunction with other neighboring pathways, the leader of which is VEGF. Table 1 is a collection of some intriguing research on lung cancer, gathered from freely accessible American and European databases that cover many studies, among which clinical trials have been conducted or are in progress around the world [56,57].
Table 1.
Some additional researches in the subject of growth factor-based targeted therapy in lung cancer (data consulted on 6 July 2023) [56,57].
| Last Update | Location and Study Identifier | Study Type | Study Title | Condition | Intervention | Status | Findings |
|---|---|---|---|---|---|---|---|
| May 2023 |
United Kingdom NCT04179890 |
Observational and retrospective | The study observes how long patients with non-small cell lung cancer (NSCLC) benefit from treatment with epidermal growth factor tyrosine kinase inhibitor (EGFR-TKI) when given either for uncommon mutations or for common mutations in the sequence afatinib followed by osimertinib (UpSwinG) | Non-squamous, Non-Small Cell Lung Cancer, | Observation of EGFR-TKI: -Afatinib -Erlotinib -Gefitinib -Osimertinib |
Complete | treatment with EGFR-TKI should be considered as standard for most patients with uncommon mutations |
| February 2023 |
USA NCT05062980 |
Clinical Trial | Quaratusugene Ozeplasmid (Reqorsa) in combination with Pembrolizumab in previously treated Non-Small Cell Lung Cancer (Acclaim-2) Phase I/II |
Non-Small Cell Lung Cancer | A: Quaratusugene ozeplasmid (pan-TKI: EGFR and Akt inhibitor) + Pembrolizumab (VEGFR downstream inhibitor: PD1 inhibitor) B: Docetaxel (microtubule inhibitor) + ramucirumab (VEGFR inhibitor) + 3rd molecule proposed by physician |
On going | / |
| May 2019 |
United Kingdom NCT02109016 |
Clinical Trial | A single arm, open-label, phase II study to assess the efficacy of the dual VEGFR-FGFR tyrosine kinase inhibitor, Lucitanib, given orally as a single agent to patients with FGFR1-driven lung cancer. | Advance stage of Small and Non-small cell lung cancer with adenomatous, squamous, and large cell histologies, as well as FGF, VEGF, or PDGF genetic alterations. |
Lucitanib, a VEGFR-FGFR tyrosine kinase inhibitor | Terminated | Interim analysis was either impossible (due to short time data collection) or showed low probability of clinically significant result |
| January 2013 |
USA NCT00862134 |
Clinical Trial | Randomized, Multi-center, Open-label, Study of PR104 Versus PR104/Docetaxel in Non-Small Cell Lung Cancer (NSCLC) Phase II |
Non-Small Cell Lung Cancer | A: Docetaxel (microtubule inhibitor) B: Docetaxel + PR104 (hypoxia-activated prodrug) + G-CSF for prophylaxis |
Terminated | Interim analysis indicated low probability of clinically significant result |
4. Vascular Endothelial Growth Factor (VEGF)
VEGF are growth factors that stimulate the formation of new blood vessels from pre-existing ones. Several VEGF family members have been identified, each with distinct and partially overlapping activities [58,59].
Today, we know that the VEGF family consists of six separate members, which are VEGF-A, VEGF-B, VEGF-C, VEGF-D, VEGF-E, and placental growth factor (PlGF). The different members differ in their binding affinity and specificity to the three receptors VEGFR1, VEGFR2, and VEGFR3. The most intensively researched member of the family, VEGF-A, has been found to be a powerful proangiogenic agent. It is expressed by a wide range of cells, including tumor cells, and binds to its endothelial cell receptors, VEGFR1 and VEGFR2, to drive blood vessel growth [58,60].
The mechanism of action of VEGF in angiogenesis is complex and involves the interaction of VEGF with its receptors on endothelial cells. The interaction triggers a series of events that promote endothelial cells to multiply, relocate, and to survive, ultimately leading to the formation of new blood vessels [60,61,62]. VEGF also promotes the formation of the extracellular matrix and the recruitment of pericytes, both of which help to stabilize newly created vessels [63,64].
The overexpression of VEGF, frequently seen in lung cancer, is associated with enhanced angiogenesis, tumor development, and metastasis. Anti-VEGF medication bevacizumab has been approved as one of the possible choice to treat advanced cases of NSCLC [65]. Anti-VEGF medication improves progression-free survival and overall survival in people with advanced NSCLC, according to several trials. Novel anti-angiogenic drugs and combination therapies that target several pathways involved in tumor angiogenesis have recently been investigated in the field of angiogenesis in lung cancer. In a phase II clinical trial lead by Horn L. et al., for example, the VEGFR inhibitor bevacizumab was added to etoposide and cisplatin and used as a first-line therapy for people with advanced stage small cell lung cancer (SCLC), and this resulted in an increase in the survival rate compared to historical controls who received this chemotherapy regimen without bevacizumab [66]. Furthermore, combining the EGFR inhibitor, erlotinib, with the VEGFR inhibitor, bevacizumab, has also been shown to improve survival rates in advanced cases of non-small cell lung cancer [53]. For more information, see Table 1.
5. Colony Stimulating Factors (CSF)
CSF are a group of cytokines that regulate the production, differentiation, and function of white blood cells. They have been demonstrated to play a role in angiogenesis in addition to their involvement in regulating white blood cell formation and differentiation. [67,68]. There are four canonical members in the family, including [69]:
-
-
Granulocyte colony-stimulating factor (G-CSF): A cytokine that promotes the creation and development of neutrophils, a kind of white blood cell, from bone marrow progenitor cells;
-
-
Granulocyte-macrophage colony-stimulating factor (GM-CSF): A cytokine that stimulates the development and differentiation of bone marrow progenitor cells into neutrophils, monocytes, and macrophages;
-
-
Macrophage colony-stimulating factor (M-CSF): A cytokine that induces the production and maturation of macrophages from bone marrow progenitor cells;
-
-
Interleukin 3 (IL-3 or multi-CSF): A hematopoietic cytokine and colony-stimulating factor that aids in the growth and maturation of erythroid, myeloid, megakaryocyte, and lymphoid progenitors.
The exact mechanism by which G-CSFs regulate angiogenesis is not fully understood, but it is thought to involve the recruitment and activation of bone marrow-derived endothelial progenitor cells (EPCs). EPCs are cells that help to generate new blood vessels from circulating endothelial progenitors during postnatal vasculogenesis. G-CSFs have the ability to mobilize EPCs from the bone marrow and boost their differentiation, proliferation, and migration, resulting in increased angiogenesis [67,70,71]. However, the therapeutic implication of such a discovery remains very controversial since G-CSF is used in prophylaxis to avoid the febrile neutropenia often observed during chemotherapy, and this considerably reduces the interest in developing G-CSF inhibitors [72]. For additional information, see Table 1.
G-CSFs, especially G-CSF and GM-CSF, have been studied for their potential relevance in lung cancer. G-CSF levels were discovered to be associated with an unfavorable prognosis in cases of NSCLC. Other findings revealed that G-CSF and GM-CSF can accelerate tumor development and angiogenesis in lung cancer as well as inhibiting G-CSF signaling can diminish angiogenesis and tumor growth. [67,73,74,75]. Taking these factors into account, recent advances in the study of angiogenesis in lung cancer have focused on the possible use of G-CSFs as therapeutic targets [73].
IL-3 has not been widely explored in relation to lung cancer angiogenesis. However, there are some findings stating that it may play an essential part in inducing angiogenesis in other forms of cancer. IL-3 may increase cancer cell proliferation and survival via mechanisms such as tumor microenvironment modification and the activation of cell multiplication and sustainment signaling pathways [76,77]. More research is required to fully comprehend this cytokine’s potential role in angiogenesis and lung cancer progression.
6. Bone Morphogenetic Protein (BMP)
BMPs are a type of signaling molecule that belongs to the TGF-beta (transforming growth factor-beta) family. After being recognized for its ability to stimulate bone formation, BMPs were shown to have various additional activities, including influencing cell growth, differentiation, and death [78].
It has been demonstrated that BMPs have a complex and context-dependent role in angiogenesis. They can increase angiogenesis in specific circumstances by boosting endothelial cell differentiation, proliferation, and migration [79,80,81]. In other contexts, some evidence suggests that BMPs may decrease angiogenesis by increasing the expression of angiogenesis inhibitors, but the precise mechanism remains unknown [79,82,83].
BMPs have been identified as having a key role in lung cancer tumor angiogenesis and progression. BMPs, particularly BMP-2, BMP-4, and BMP-7, have been discovered to be elevated in lung cancer tissues and have been linked to a bad prognosis in these individuals. BMPs have also been demonstrated to induce the production of pro-angiogenic factors, resulting in angiogenesis stimulation and tumor growth in lung cancer [28,84,85,86]. As a result, recent research has focused on BMP signaling targeting as a viable therapeutic for lung cancer with substantial angiogenesis [87]. In 2021, Meng et al. suggest BMP5 as a potential crucial target for lung adenocarcinoma treatment [84].
7. Fibroblast Growth Factors 1 and 2 (FGF1 and FGF2)
FGF1 and FGF2 are potent angiogenic agents that increase vascular endothelial cell development, displacement, and survival. They attach to heparan sulfate proteoglycans on endothelial cell surfaces, activating both the FGFR1 and FGFR2 endothelial cell isoforms. This activates downstream signaling pathways, such as ERK, PI3K, and PLC, which promote angiogenesis by increasing the synthesis and secretion of pro-angiogenic molecules, such as VEGF and platelet-derived growth factor (PDGF) [88,89].
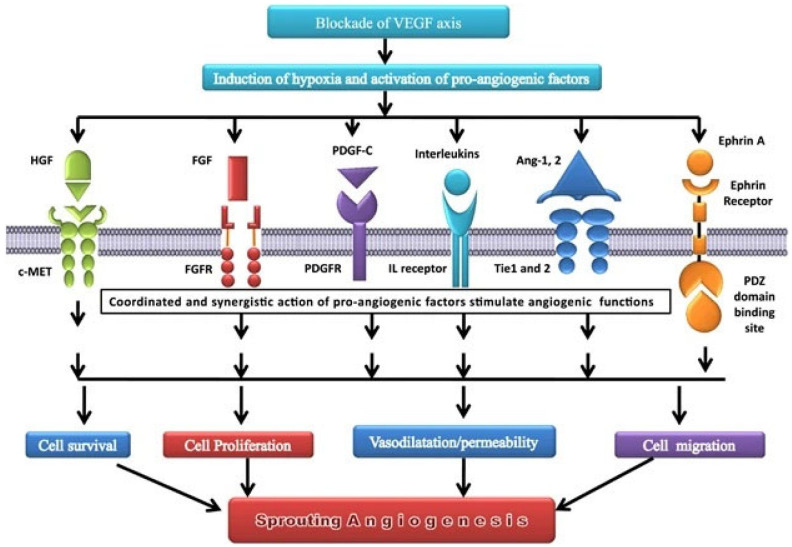
FGFs, especially FGF1 and FGF2, play a complex and context-dependent involvement role in lung cancer. FGFs have an important role in tumor angiogenesis and growth in early-stage lung cancer because they encourage the production of new blood vessels, which deliver nutrition and oxygen to the tumor cells [19,90,91]. FGF2 expression has been observed to be elevated in lung cancer and is associated with a bad prognosis [92]. FGFs can also contribute to anti-angiogenic therapy resistance since tumors can shift to an alternate angiogenic pathway that is not targeted by current therapies [19,93,94,95]. Figure 2 depicts an example where VEGFR is targeted and demonstrates the many compensatory angiogenic factors/signaling routes that tumors use to sustain the angiogenic process, with several growth factors, including FGF, being involved [96].
Figure 2.
Compensatory angiogenic factors/signaling routes, including FGF, after blockade of VEGF axis. The inhibition of the VEGF axis causes tissue hypoxia, which the body interprets as a lack of vessels, preventing blood from reaching the appropriate areas. This activates pro-angiogenic factors, such as HGF, FGF, PDGF, interleukins, Ang-1&2, and ephrin A, resulting in a cascade of events leading to angiogenesis. Data source: Review article “Compensatory angiogenesis and tumor refractoriness” by Gacche [96], published in an open access journal.
Recent research has focused on developing FGF signaling pathway inhibitors as potential lung cancer therapeutics. BGJ398, for example, is a selective inhibitor of the FGFR signaling pathway that has demonstrated potential anticancer effects in preclinical investigations and is currently being tested in clinical trials in patients with FGFR-mutant NSCLC [97,98].
8. Interleukins (IL)
Interleukins are a type of cytokine that is involved in immunological modulation as well as physiological processes, such as development, angiogenesis, and hematopoiesis. The interleukin family contains around 40 members, each with its own distinct function in the immune system [99,100].
Several interleukins, including IL-1 beta, IL-6, and IL-8, have been identified to be dysregulated in lung cancer. These interleukins have been demonstrated to stimulate tumor growth by angiogenesis as well as cell proliferation, survival, and invasion. For example, IL-6, IL-8, and IL-17 have been shown to increase VEGF expression in lung cancer cells, which increases angiogenesis [28,101,102,103].
Research has focused on targeting interleukins as a potential lung cancer therapy strategy [104,105]. Many researches have shown that IL-6 interacts with other molecules, notably VEGF to ultimately promote angiogenesis [106,107]. Figure 3 illustrates interleukin-6 in the tumor microenvironment, depicts how it interacts with other molecules as well as the VEGF pathway to promote the angiogenesis process and therefore favor the tumor progression, and also shows anti-IL-6 possible targeted molecules used in cancer therapy [106,108,109,110,111,112,113].
Figure 3.
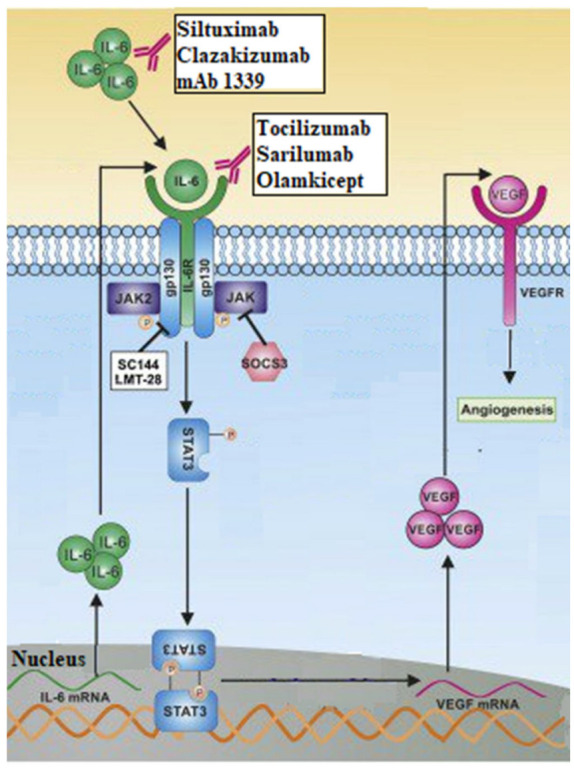
Interleukin-6 in the tumor microenvironment and its action on VEGF axis. The formation of IL-6 from stimulated IL-6 mRNA, leads to a release of IL-6, in high concentration, in the extracellular milieu. After connecting to its receptors, IL-6 initiates a chain of reactions that will ultimately lead to the synthesis of VEGF and therefore to angiogenesis. The figure also shows the different therapeutic molecules used to inhibit this pathway and therefore treat cancer. Data source: Adapted figure from the article “Cross-talk between EGFR and IL-6 drives oncogenic signaling and offers therapeutic opportunities in cancer” by Ray K, Ujvari B, Ramana V and Donald J. [113]. Re-use License number 5615250558075.
Researchers currently believe that certain interleukins have diagnostic and prognostic value when combined with other molecules. In 2022, a study lead by Yan X., for example, found that IL-6 and IL-8 could be used as possible molecular biomarkers to diagnose and predict lung cancer metastasis regardless of pathological type or to improve the specificity and sensitivity for the diagnosis of lung cancer when paired with Carcinoembryonic antigen (CEA) [114].
9. Others Growth Factors
-
-
Hepatocyte Growth Factor (HGF): It is a cytokine with two different domains, one N-terminal and one C-terminal, each with its own set of biological activity. The C-terminal domain of HGF mediates its ability to induce angiogenesis by activating subsequent signaling pathways, such as the PI3K/Akt and MAPK/ERK pathways [115,116]. Its rise in lung cancer has been linked to a poor prognosis and resistance to anti-angiogenic therapy. Recent research found that an anti-HGF monoclonal antibody can inhibit HGF-induced angiogenesis and tumor growth in preclinical models of lung cancer, providing a potential therapeutic strategy for lung cancer patients [116,117].
-
-
Human Epidermal Growth Factor Receptors 2 and 3 (HER2 and HER3): These two belong to the family of tyrosine kinases receptors and are overexpressed or mutated in many cancers and increase angiogenesis by activating both the PI3K/Akt and MAPK/ERK signaling pathways [118]. Several HER2-targeting therapy treatments, including monoclonal antibodies and tyrosine kinase inhibitors (TKIs), such as afatinib and neratinib, have demonstrated success in preclinical and clinical trials. Moreover, many researchers are working to bring out new therapies targeting HER-2 in the field of lung cancer [119,120].
-
-
Platelet Derived Growth Factor (PDGF) α/β: They belong to the PDGF receptor tyrosine kinase family and have been linked to lung cancer angiogenesis. PDGFR-alpha and PDGFR-beta are both overexpressed in lung cancer, and their presence has been linked to a bad prognosis. In preclinical lung cancer models, blocking PDGF signaling has been shown to diminish tumor formation and angiogenesis [22,121]. As for the others, combination treatments targeting both the PDGF and VEGF signaling pathways in lung cancer have been examined. In one trial, the anti-PDGF agent nintedanib was coupled with the anti-VEGF agent bevacizumab in lung cancer patients, resulting in an improvement in progression-free survival when compared to bevacizumab alone [122].
-
-
Soluble Tie 2 (sTie2) is a shortened version of the Tie2 receptor, which is an angiopoietin receptor expressed on endothelial cells and is involved in angiogenesis and vascular stabilization [123]. Its expression has been linked to unfavorable outcomes in several malignancies, including lung cancer, and research is being conducted to see how it can be targeted for therapy [124].
-
-
Soluble Neuropilin 1 (sNRP1) is a shortened version of the neuropilin 1 receptor that is produced on endothelial cells and impacts angiogenesis by acting as a VEGF coreceptor [125]. As with soluble Tie 2, large levels of sNRP1 expression have been linked to a worse prognosis, and it is also a molecule of interest in the realm of targeted therapeutics for lung cancer [126,127].
10. Conclusions and Perspectives
Growth factors have a strong pro-angiogenic effect because they encourage the development of new vessels through many pathways, resulting in tumor progression and metastasis: That is why they constitute one of the therapeutic targets against cancers.
In lung cancer, in view of the rapid and unfavorable evolution sometimes observed, even in patients undergoing treatment, new therapeutic approaches have been proposed, and the first evaluations are encouraging.
Considering the complexity of the processes involved in angiogenesis and the multitude of growth factors that promote the therapeutic escape mechanism, combined therapies and therapies targeting the downstream signaling pathways are now being extensively explored as potentially of interest in the management of this disease. In the meantime, the literature remains favorable on the central role of EGFR-TKI-based treatment, even in the case of uncommon mutations.
A personalized approach with a prior analysis of genetic and molecular profiles in search of the presence of mutations in patients (EGFR mutations) is strongly recommended. Special attention should also be paid to the risk of toxicity when launching a therapeutic regimen because it constitutes one of the main complications of combined therapies and can thus justify the discontinuation of the treatment regimen.
Finally, we believe it is critical to emphasize the importance of continuing to conduct research in search of new lung cancer biomarkers, identifying all of the factors and mechanisms responsible for mutation occurrence, and deepening our understanding of the processes by which lung cancer cells develop resistance to anti-angiogenic therapies.
Acknowledgments
Ministry of Science and Higher Education of the Russian Federation within the framework of state support for the creation and development of World-Class Research Centers “Digital biodesign and personalized healthcare” №075-15-2022-304.
Abbreviations
| Akt | Protein Kinase B |
| Ang 1 and 2 | Angiopoietin 1 and 2 |
| AREG | amphiregulin |
| bFGF | basic Fibroblast Growth Factor |
| BMP | Bone Morphogenetic Protein |
| BTC | beta-cellulin |
| CEA | Carcinoembryonic antigen |
| c-MET | cellular Mesenchymal-Epithelial Transition factor |
| CSF | Colony Stimulating Factor |
| EGF | Epidermal Growth Factor |
| EGFR | Epidermal Growth Factor Receptor |
| EPCs | bone marrow-derived endothelial progenitor cells |
| EPGN | Epigene protein |
| EREG | Epiregulin |
| ERK | Extracellular Signal-Regulated Kinase |
| FGF (1 and 2) | Fibroblast Growth Factor (1 and 2) |
| FGFR (1 and 2) | Fibroblast Growth Factor Receptor (1 and 2) |
| G-CSF | Granulocyte Colony-Stimulating Factor |
| GLOBOCAN | Global Cancer Observatory |
| GM-CSF | Granulocyte-Macrophage Colony-Stimulating Factor |
| GP | glycoprotein |
| HB-EGF | Heparin-Binding EGF-like Growth Factor |
| HER (2 and 3) | Human Epidermal Growth Factor Receptors (2 and 3) |
| HGF | Hepatocyte Growth Factor |
| HIF | Hypoxia-Inducible Factors |
| IL | Interleukin |
| JAK | Janus Kinase |
| MAPK | Mitogen Activated Protein Kinase |
| M-CSF | Macrophage Colony-Stimulating Factor |
| MRI | Magnetic Resonance Imaging |
| NSCLC | Non-Small Cell Lung Cancer |
| PDGF | Platelet-Derived Growth Factor |
| PDGF-c | Platelet-Derived Growth Factor C |
| PDGFR | Platelet-Derived Growth Factor Receptor |
| PDZ | Postsynaptic density protein of 95 kDa (PSD95), Drosophila disc large tumor suppressor (DlgA), and Zonula occludens-1 protein (Zo-1) |
| PI3k | Phosphatidylinositol 3-kinase |
| PIGF | Phosphatidylinositol-glycan F or Placental Growth Factor |
| PLC | Phospholipase C |
| SCLC | Small Cell Lung Cancer |
| sNRP1 | Soluble Neuropilin 1 |
| SOCS3 | Suppressor Of Cytokine Signaling 3 |
| STAT | Signal Transducer and Activator of Transcription |
| sTie 2 | Soluble Angiopoietin receptor |
| TGF-alpha | Transforming growth factor alpha |
| TGF-beta | Transforming Growth Factor-beta |
| Tie 2 | Angiopoietin receptor |
| TKI | Tyrosine Kinase Inhibitors |
| VEGF | Vascular Endothelial Growth Factor |
| VEGFR | Vascular Endothelial Growth Factor Receptor |
Author Contributions
All of the authors mentioned above made notable contributions to the creation and writing of this article. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Herbst R.S., Morgensztern D., Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018;553:446–454. doi: 10.1038/nature25183. [DOI] [PubMed] [Google Scholar]
- 3.Navada S., Lai P., Schwartz A.G., Kalemkerian G.P. Temporal trends in small cell lung cancer: Analysis of the national Surveillance, Epidemiology, and End-Results (SEER) database. J. Clin. Oncol. 2006;24:7082. doi: 10.1200/jco.2006.24.18_suppl.7082. [DOI] [Google Scholar]
- 4.Sher T., Dy G.K., Adjei A.A. Small Cell Lung Cancer. Mayo Clin. Proc. 2008;83:355–367. doi: 10.4065/83.3.355. [DOI] [PubMed] [Google Scholar]
- 5.Allemani C., Matsuda T., Di Carlo V., Harewood R., Matz M., Nikšić M., Bonaventure A., Valkov M., Johnson C.J., Estève J., et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37,513,025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023–1075. doi: 10.1016/S0140-6736(17)33326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adair T.H., Montani J.-P. Angiogenesis. Morgan & Claypool Life Sciences; San Rafael, CA, USA: 2010. Overview of Angiogenesis. [PubMed] [Google Scholar]
- 7.Nishida N., Yano H., Nishida T., Kamura T., Kojiro M. Angiogenesis in cancer. Vasc. Health Risk Manag. 2006;2:213–219. doi: 10.2147/vhrm.2006.2.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajabi M., Mousa S. The Role of Angiogenesis in Cancer Treatment. Biomedicines. 2017;5:34. doi: 10.3390/biomedicines5020034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hyodo F., Chandramouli G.V., Matsumoto S., Matsumoto K., Mitchell J.B., Krishna M.C., Munasinghe J.P. Krishna Estimation of tumor microvessel density by MRI using a blood pool contrast agent. Int. J. Oncol. 2009;35:797–804. doi: 10.3892/ijo_00000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Folkman J. Advances in Cancer Research. Volume 43. Elsevier; Amsterdam, The Netherlands: 1985. Tumor Angiogenesis; pp. 175–203. [DOI] [PubMed] [Google Scholar]
- 11.Gupta M.K. Mechanism and its regulation of tumor-induced angiogenesis. World J. Gastroenterol. 2003;9:1144. doi: 10.3748/wjg.v9.i6.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shoari A., Khodabakhsh F., Ahangari Cohan R., Salimian M., Karami E. Anti-angiogenic peptides application in cancer therapy; a review. Res. Pharm. Sci. 2021;16:559. doi: 10.4103/1735-5362.327503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mukherjee A., Madamsetty V.S., Paul M.K., Mukherjee S. Recent Advancements of Nanomedicine towards Antiangiogenic Therapy in Cancer. Int. J. Mol. Sci. 2020;21:455. doi: 10.3390/ijms21020455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Irvin M.W., Zijlstra A., Wikswo J.P., Pozzi A. Techniques and assays for the study of angiogenesis. Exp. Biol. Med. 2014;239:1476–1488. doi: 10.1177/1535370214529386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roudsari L.C., West J.L. Studying the influence of angiogenesis in in vitro cancer model systems. Adv. Drug Deliv. Rev. 2016;97:250–259. doi: 10.1016/j.addr.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Ucuzian A.A., Gassman A.A., East A.T., Greisler H.P. Molecular Mediators of Angiogenesis. J. Burn Care Res. 2010;31:158–175. doi: 10.1097/BCR.0b013e3181c7ed82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carmeliet P., Jain R.K. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saman H., Raza S.S., Uddin S., Rasul K. Inducing Angiogenesis, a Key Step in Cancer Vascularization, and Treatment Approaches. Cancers. 2020;12:1172. doi: 10.3390/cancers12051172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lugano R., Ramachandran M., Dimberg A. Tumor angiogenesis: Causes, consequences, challenges and opportunities. Cell. Mol. Life Sci. 2020;77:1745–1770. doi: 10.1007/s00018-019-03351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horn L., Sandler A.B. Angiogenesis in the Treatment of Non-Small Cell Lung Cancer. Proc. Am. Thorac. Soc. 2009;6:206–217. doi: 10.1513/pats.200807-066LC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niu G., Chen X. Vascular Endothelial Growth Factor as an Anti-Angiogenic Target for Cancer Therapy. Curr. Drug Targets. 2010;11:1000–1017. doi: 10.2174/138945010791591395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raica M., Cimpean A.M. Platelet-Derived Growth Factor (PDGF)/PDGF Receptors (PDGFR) Axis as Target for Antitumor and Antiangiogenic Therapy. Pharmaceuticals. 2010;3:572–599. doi: 10.3390/ph3030572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin. Oncol. 2002;29:15–18. doi: 10.1053/sonc.2002.37263. [DOI] [PubMed] [Google Scholar]
- 24.Bielenberg D.R., Zetter B.R. The Contribution of Angiogenesis to the Process of Metastasis. Cancer J. 2015;21:267–273. doi: 10.1097/PPO.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jun J.C., Rathore A., Younas H., Gilkes D., Polotsky V.Y. Hypoxia-Inducible Factors and Cancer. Curr. Sleep Med. Rep. 2017;3:1–10. doi: 10.1007/s40675-017-0062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lv X., Li J., Zhang C., Hu T., Li S., He S., Yan H., Tan Y., Lei M., Wen M., et al. The role of hypoxia-inducible factors in tumor angiogenesis and cell metabolism. Genes Dis. 2017;4:19–24. doi: 10.1016/j.gendis.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aguilar-Cazares D., Chavez-Dominguez R., Carlos-Reyes A., Lopez-Camarillo C., Hernadez De La Cruz O.N., Lopez-Gonzalez J.S. Contribution of Angiogenesis to Inflammation and Cancer. Front. Oncol. 2019;9:1399. doi: 10.3389/fonc.2019.01399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang X., Wang J., Deng X., Xiong F., Zhang S., Gong Z., Li X., Cao K., Deng H., He Y., et al. The role of microenvironment in tumor angiogenesis. J. Exp. Clin. Cancer Res. 2020;39:204. doi: 10.1186/s13046-020-01709-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ribatti D., Crivellato E. Immune cells and angiogenesis. J. Cell. Mol. Med. 2009;13:2822–2833. doi: 10.1111/j.1582-4934.2009.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pekarek L., Torres-Carranza D., Fraile-Martinez O., García-Montero C., Pekarek T., Saez M.A., Rueda-Correa F., Pimentel-Martinez C., Guijarro L.G., Diaz-Pedrero R., et al. An Overview of the Role of MicroRNAs on Carcinogenesis: A Focus on Cell Cycle, Angiogenesis and Metastasis. Int. J. Mol. Sci. 2023;24:7268. doi: 10.3390/ijms24087268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aspriţoiu V.M., Stoica I., Bleotu C., Diaconu C.C. Epigenetic Regulation of Angiogenesis in Development and Tumors Progression: Potential Implications for Cancer Treatment. Front. Cell Dev. Biol. 2021;9:689962. doi: 10.3389/fcell.2021.689962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Annese T., Tamma R., De Giorgis M., Ribatti D. microRNAs Biogenesis, Functions and Role in Tumor Angiogenesis. Front. Oncol. 2020;10:581007. doi: 10.3389/fonc.2020.581007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Song Y., Fu Y., Xie Q., Zhu B., Wang J., Zhang B. Anti-angiogenic Agents in Combination with Immune Checkpoint Inhibitors: A Promising Strategy for Cancer Treatment. Front. Immunol. 2020;11:1956. doi: 10.3389/fimmu.2020.01956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee W.S., Yang H., Chon H.J., Kim C. Combination of anti-angiogenic therapy and immune checkpoint blockade normalizes vascular-immune crosstalk to potentiate cancer immunity. Exp. Mol. Med. 2020;52:1475–1485. doi: 10.1038/s12276-020-00500-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fang L., Zhao W., Ye B., Chen D. Combination of Immune Checkpoint Inhibitors and Anti-Angiogenic Agents in Brain Metastases from Non-Small Cell Lung Cancer. Front. Oncol. 2021;11:670313. doi: 10.3389/fonc.2021.670313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wieduwilt M.J., Moasser M.M. The epidermal growth factor receptor family: Biology driving targeted therapeutics. Cell. Mol. Life Sci. 2008;65:1566–1584. doi: 10.1007/s00018-008-7440-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schneider M.R., Wolf E. The epidermal growth factor receptor ligands at a glance. J. Cell. Physiol. 2009;218:460–466. doi: 10.1002/jcp.21635. [DOI] [PubMed] [Google Scholar]
- 38.Stoll S.W., Rittié L., Johnson J.L., Elder J.T. Heparin-Binding EGF-Like Growth Factor Promotes Epithelial–Mesenchymal Transition in Human Keratinocytes. J. Investig. Dermatol. 2012;132:2148–2157. doi: 10.1038/jid.2012.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu T.-C., Jin X., Wang Y., Wang K. Role of epidermal growth factor receptor in lung cancer and targeted therapies. Am. J. Cancer Res. 2017;7:187–202. [PMC free article] [PubMed] [Google Scholar]
- 40.Sasaki T., Hiroki K., Yamashita Y. The Role of Epidermal Growth Factor Receptor in Cancer Metastasis and Microenvironment. BioMed Res. Int. 2013;2013:546318. doi: 10.1155/2013/546318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Spano J.P., Fagard R., Soria J.-C., Rixe O., Khayat D., Milano G. Epidermal growth factor receptor signaling in colorectal cancer: Preclinical data and therapeutic perspectives. Ann. Oncol. 2005;16:189–194. doi: 10.1093/annonc/mdi057. [DOI] [PubMed] [Google Scholar]
- 42.Ardizzone A., Bova V., Casili G., Repici A., Lanza M., Giuffrida R., Colarossi C., Mare M., Cuzzocrea S., Esposito E., et al. Role of Basic Fibroblast Growth Factor in Cancer: Biological Activity, Targeted Therapies, and Prognostic Value. Cells. 2023;12:1002. doi: 10.3390/cells12071002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khodabakhsh F., Merikhian P., Eisavand M.R., Farahmand L. Crosstalk between MUC1 and VEGF in angiogenesis and metastasis: A review highlighting roles of the MUC1 with an emphasis on metastatic and angiogenic signaling. Cancer Cell Int. 2021;21:200. doi: 10.1186/s12935-021-01899-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang Z., Yao L., Yang J., Wang Z., Du G. PI3K/Akt and HIF-1 signaling pathway in hypoxia-ischemia (Review) Mol. Med. Rep. 2018;18:3547–3554. doi: 10.3892/mmr.2018.9375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Franke T.F., Hornik C.P., Segev L., Shostak G.A., Sugimoto C. PI3K/Akt and apoptosis: Size matters. Oncogene. 2003;22:8983–8998. doi: 10.1038/sj.onc.1207115. [DOI] [PubMed] [Google Scholar]
- 46.Xu Y., Yuan F.-E., Chen Q.-X., Liu B.-H. Molecular mechanisms involved in angiogenesis and potential target of antiangiogenesis in human glioblastomas. Glioma. 2018;1:35. doi: 10.4103/glioma.glioma_10_17. [DOI] [Google Scholar]
- 47.Nan X., Xie C., Yu X., Liu J. EGFR TKI as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer. Oncotarget. 2017;8:75712–75726. doi: 10.18632/oncotarget.20095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakagawa K., Garon E.B., Gao L., Callies S., Zimmermann A., Walgren R., Visseren-Grul C., Reck M. RELAY, ramucirumab plus erlotinib versus placebo plus erlotinib in untreated EGFR-mutated metastatic non-small cell lung cancer: Exposure–response relationship. Cancer Chemother. Pharmacol. 2022;90:137–148. doi: 10.1007/s00280-022-04447-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nakagawa K., Garon E.B., Seto T., Nishio M., Ponce Aix S., Paz-Ares L., Chiu C.-H., Park K., Novello S., Nadal E., et al. Ramucirumab plus erlotinib in patients with untreated, EGFR-mutated, advanced non-small-cell lung cancer (RELAY): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:1655–1669. doi: 10.1016/S1470-2045(19)30634-5. [DOI] [PubMed] [Google Scholar]
- 50.Subbiah V., Dumbrava E.I., Jiang Y., Thein K.Z., Naing A., Hong D.S., Fu S., Piha-Paul S.A., Tsimberidou A.M., Janku F., et al. Dual EGFR blockade with cetuximab and erlotinib combined with anti-VEGF antibody bevacizumab in advanced solid tumors: A phase 1 dose escalation triplet combination trial. Exp. Hematol. Oncol. 2020;9:7. doi: 10.1186/s40164-020-00159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ansari M.J., Bokov D., Markov A., Jalil A.T., Shalaby M.N., Suksatan W., Chupradit S., AL-Ghamdi H.S., Shomali N., Zamani A., et al. Cancer combination therapies by angiogenesis inhibitors; a comprehensive review. Cell Commun. Signal. 2022;20:49. doi: 10.1186/s12964-022-00838-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mehta V.B., Besner G.E., Mehta V.B., Besner G.E. HB-EGF promotes angiogenesis in endothelial cells via PI3-kinase and MAPK signaling pathways. Growth Factors. 2007;25:253–263. doi: 10.1080/08977190701773070. [DOI] [PubMed] [Google Scholar]
- 53.Rosell R., Dafni U., Felip E., Curioni-Fontecedro A., Gautschi O., Peters S., Massutí B., Palmero R., Aix S.P., Carcereny E., et al. Erlotinib and bevacizumab in patients with advanced non-small-cell lung cancer and activating EGFR mutations (BELIEF): An international, multicentre, single-arm, phase 2 trial. Lancet Respir. Med. 2017;5:435–444. doi: 10.1016/S2213-2600(17)30129-7. [DOI] [PubMed] [Google Scholar]
- 54.Wang X., Goldstein D., Crowe P.J., Yang J.-L. Next-generation EGFR/HER tyrosine kinase inhibitors for the treatment of patients with non-small-cell lung cancer harboring EGFR mutations: A review of the evidence. OncoTargets Ther. 2016;9:5461–5473. doi: 10.2147/OTT.S94745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meng Y., Bai R., Cui J. Precision targeted therapy for EGFR mutation-positive NSCLC: Dilemmas and coping strategies. Thorac. Cancer. 2023;14:1121–1134. doi: 10.1111/1759-7714.14858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.National Library of Medicine Home|Beta ClinicalTrials.gov. [(accessed on 7 June 2023)]; Available online: https://beta.clinicaltrials.gov/
- 57.European Medicines Agency Clinical Trials Register. [(accessed on 7 June 2023)]. Available online: https://www.clinicaltrialsregister.eu/ctr-search/search.
- 58.Holmes D.I.R., Zachary I. The vascular endothelial growth factor (VEGF) family: Angiogenic factors in health and disease. Genome Biol. 2005;6:209. doi: 10.1186/gb-2005-6-2-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ye X., Gaucher J.-F., Vidal M., Broussy S. A Structural Overview of Vascular Endothelial Growth Factors Pharmacological Ligands: From Macromolecules to Designed Peptidomimetics. Molecules. 2021;26:6759. doi: 10.3390/molecules26226759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shibuya M. Vascular Endothelial Growth Factor (VEGF) and Its Receptor (VEGFR) Signaling in Angiogenesis: A Crucial Target for Anti- and Pro-Angiogenic Therapies. Genes Cancer. 2011;2:1097–1105. doi: 10.1177/1947601911423031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cébe-Suarez S., Zehnder-Fjällman A., Ballmer-Hofer K. The role of VEGF receptors in angiogenesis; complex partnerships. Cell. Mol. Life Sci. 2006;63:601. doi: 10.1007/s00018-005-5426-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Duffy A.M., Bouchier-Hayes D.J., Harmey J.H. Madame Curie Bioscience Database [Internet] Landes Bioscience; Austin, TX, USA: 2013. Vascular Endothelial Growth Factor (VEGF) and Its Role in Non-Endothelial Cells: Autocrine Signalling by VEGF. [Google Scholar]
- 63.Evensen L., Micklem D.R., Blois A., Berge S.V., Aarsæther N., Littlewood-Evans A., Wood J., Lorens J.B. Mural Cell Associated VEGF Is Required for Organotypic Vessel Formation. PLoS ONE. 2009;4:e5798. doi: 10.1371/journal.pone.0005798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stratman A.N., Malotte K.M., Mahan R.D., Davis M.J., Davis G.E. Pericyte recruitment during vasculogenic tube assembly stimulates endothelial basement membrane matrix formation. Blood. 2009;114:5091–5101. doi: 10.1182/blood-2009-05-222364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lind J.S.W., Smit E.F. Angiogenesis inhibitors in the treatment of non-small cell lung cancer. Ther. Adv. Med. Oncol. 2009;1:95–107. doi: 10.1177/1758834009338633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Horn L., Dahlberg S.E., Sandler A.B., Dowlati A., Moore D.F., Murren J.R., Schiller J.H. Phase II Study of Cisplatin Plus Etoposide and Bevacizumab for Previously Untreated, Extensive-Stage Small-Cell Lung Cancer: Eastern Cooperative Oncology Group Study E3501. J. Clin. Oncol. 2009;27:6006–6011. doi: 10.1200/JCO.2009.23.7545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cetean S., Căinap C., Constantin A.-M., Căinap S., Gherman A., Oprean L., Hangan A., Oprean R. The importance of the granulocyte-colony stimulating factor in oncology. Med. Pharm. Rep. 2015;88:468–472. doi: 10.15386/cjmed-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ray A. Cytokines and their Role in Health and Disease: A Brief Overview. MOJ Immunol. 2016;4:00121. doi: 10.15406/moji.2016.04.00121. [DOI] [Google Scholar]
- 69.Fleetwood A.J., Achuthan A., Hamilton J.A. Encyclopedia of Immunobiology. Elsevier; Amsterdam, The Netherlands: 2016. Colony Stimulating Factors (CSFs) pp. 586–596. [Google Scholar]
- 70.George A.L., Bangalore-Prakash P., Rajoria S., Suriano R., Shanmugam A., Mittelman A., Tiwari R.K. Endothelial progenitor cell biology in disease and tissue regeneration. J. Hematol. Oncol. 2011;4:24. doi: 10.1186/1756-8722-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gao D., Nolan D., McDonnell K., Vahdat L., Benezra R., Altorki N., Mittal V. Bone marrow-derived endothelial progenitor cells contribute to the angiogenic switch in tumor growth and metastatic progression. Biochim. Biophys. Acta BBA Rev. Cancer. 2009;1796:33–40. doi: 10.1016/j.bbcan.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aapro M., Crawford J., Kamioner D. Prophylaxis of chemotherapy-induced febrile neutropenia with granulocyte colony-stimulating factors: Where are we now? Support. Care Cancer. 2010;18:529–541. doi: 10.1007/s00520-010-0816-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Karagiannidis I., Salataj E., Said Abu Egal E., Beswick E.J. G-CSF in tumors: Aggressiveness, tumor microenvironment and immune cell regulation. Cytokine. 2021;142:155479. doi: 10.1016/j.cyto.2021.155479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang Y., Fang C., Chen R., Yuan S., Chen L., Qiu X., Qian X., Zhang X., Xiao Z., Wang Q., et al. rhG-CSF is associated with an increased risk of metastasis in NSCLC patients following postoperative chemotherapy. BMC Cancer. 2022;22:741. doi: 10.1186/s12885-022-09850-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kowanetz M., Wu X., Lee J., Tan M., Hagenbeek T., Qu X., Yu L., Ross J., Korsisaari N., Cao T., et al. Granulocyte-colony stimulating factor promotes lung metastasis through mobilization of Ly6G+Ly6C+ granulocytes. Proc. Natl. Acad. Sci. USA. 2010;107:21248–21255. doi: 10.1073/pnas.1015855107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Terceiro L.E.L., Edechi C.A., Ikeogu N.M., Nickel B.E., Hombach-Klonisch S., Sharif T., Leygue E., Myal Y. The Breast Tumor Microenvironment: A Key Player in Metastatic Spread. Cancers. 2021;13:4798. doi: 10.3390/cancers13194798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dentelli P., Rosso A., Olgasi C., Camussi G., Brizzi M.F. IL-3 is a novel target to interfere with tumor vasculature. Oncogene. 2011;30:4930–4940. doi: 10.1038/onc.2011.204. [DOI] [PubMed] [Google Scholar]
- 78.Wang R.N., Green J., Wang Z., Deng Y., Qiao M., Peabody M., Zhang Q., Ye J., Yan Z., Denduluri S., et al. Bone Morphogenetic Protein (BMP) signaling in development and human diseases. Genes Dis. 2014;1:87–105. doi: 10.1016/j.gendis.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dyer L.A., Pi X., Patterson C. The role of BMPs in endothelial cell function and dysfunction. Trends Endocrinol. Metab. 2014;25:472–480. doi: 10.1016/j.tem.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Suzuki Y., Montagne K., Nishihara A., Watabe T., Miyazono K. BMPs Promote Proliferation and Migration of Endothelial Cells via Stimulation of VEGF-A/VEGFR2 and Angiopoietin-1/Tie2 Signalling. J. Biochem. 2008;143:199–206. doi: 10.1093/jb/mvm215. [DOI] [PubMed] [Google Scholar]
- 81.Chen W.-C., Chung C.-H., Lu Y.-C., Wu M.-H., Chou P.-H., Yen J.-Y., Lai Y.-W., Wang G.-S., Liu S.-C., Cheng J.-K., et al. BMP-2 induces angiogenesis by provoking integrin α6 expression in human endothelial progenitor cells. Biochem. Pharmacol. 2018;150:256–266. doi: 10.1016/j.bcp.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 82.Carreira A.C., Lojudice F.H., Halcsik E., Navarro R.D., Sogayar M.C., Granjeiro J.M. Bone Morphogenetic Proteins: Facts, Challenges, and Future Perspectives. J. Dent. Res. 2014;93:335–345. doi: 10.1177/0022034513518561. [DOI] [PubMed] [Google Scholar]
- 83.Scharpfenecker M., Van Dinther M., Liu Z., Van Bezooijen R.L., Zhao Q., Pukac L., Löwik C.W.G.M., Ten Dijke P. BMP-9 signals via ALK1 and inhibits bFGF-induced endothelial cell proliferation and VEGF-stimulated angiogenesis. J. Cell Sci. 2007;120:964–972. doi: 10.1242/jcs.002949. [DOI] [PubMed] [Google Scholar]
- 84.Meng W., Xiao H., Zhao R., Li D., Li K., Meng Y., Chen J., Wang Y., Liao Y. The Prognostic Value of Bone Morphogenetic Proteins and Their Receptors in Lung Adenocarcinoma. Front. Oncol. 2021;11:608239. doi: 10.3389/fonc.2021.608239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shen W., Pang H., Xin B., Duan L., Liu L., Zhang H. Biological effects of BMP7 on small-cell lung cancer cells and its bone metastasis. Int. J. Oncol. 2018;53:1354–1362. doi: 10.3892/ijo.2018.4469. [DOI] [PubMed] [Google Scholar]
- 86.Ehata S., Miyazono K. Bone Morphogenetic Protein Signaling in Cancer; Some Topics in the Recent 10 Years. Front. Cell Dev. Biol. 2022;10:883523. doi: 10.3389/fcell.2022.883523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Katagiri T., Watabe T. Bone Morphogenetic Proteins. Cold Spring Harb. Perspect. Biol. 2016;8:a021899. doi: 10.1101/cshperspect.a021899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Farooq M., Khan A.W., Kim M.S., Choi S. The Role of Fibroblast Growth Factor (FGF) Signaling in Tissue Repair and Regeneration. Cells. 2021;10:3242. doi: 10.3390/cells10113242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ornitz D.M., Itoh N. The Fibroblast Growth Factor signaling pathway. WIREs Dev. Biol. 2015;4:215–266. doi: 10.1002/wdev.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Korc M., Friesel R. The Role of Fibroblast Growth Factors in Tumor Growth. Curr. Cancer Drug Targets. 2009;9:639–651. doi: 10.2174/156800909789057006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pardo O.E., Wellbrock C., Khanzada U.K., Aubert M., Arozarena I., Davidson S., Bowen F., Parker P.J., Filonenko V.V., Gout I.T., et al. FGF-2 protects small cell lung cancer cells from apoptosis through a complex involving PKCε, B-Raf and S6K2. EMBO J. 2006;25:3078–3088. doi: 10.1038/sj.emboj.7601198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Behrens C., Lin H.Y., Lee J.J., Raso M.G., Hong W.K., Wistuba I.I., Lotan R. Immunohistochemical Expression of Basic Fibroblast Growth Factor and Fibroblast Growth Factor Receptors 1 and 2 in the Pathogenesis of Lung Cancer. Clin. Cancer Res. 2008;14:6014–6022. doi: 10.1158/1078-0432.CCR-08-0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Haibe Y., Kreidieh M., El Hajj H., Khalifeh I., Mukherji D., Temraz S., Shamseddine A. Resistance Mechanisms to Anti-angiogenic Therapies in Cancer. Front. Oncol. 2020;10:221. doi: 10.3389/fonc.2020.00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zahra F.T., Sajib M.S., Mikelis C.M. Role of bFGF in Acquired Resistance upon Anti-VEGF Therapy in Cancer. Cancers. 2021;13:1422. doi: 10.3390/cancers13061422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Terai H., Soejima K., Yasuda H., Nakayama S., Hamamoto J., Arai D., Ishioka K., Ohgino K., Ikemura S., Sato T., et al. Activation of the FGF2-FGFR1 Autocrine Pathway: A Novel Mechanism of Acquired Resistance to Gefitinib in NSCLC. Mol. Cancer Res. 2013;11:759–767. doi: 10.1158/1541-7786.MCR-12-0652. [DOI] [PubMed] [Google Scholar]
- 96.Gacche R.N. Compensatory angiogenesis and tumor refractoriness. Oncogenesis. 2015;4:e153. doi: 10.1038/oncsis.2015.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chae Y.K., Pai S.G., Sun P., Costa R., Matsangou M., Agulnik M., Giles F. Fibroblast growth factor receptor (FGFR) as a therapeutic target in lung and head and neck cancer. Am. J. Hematol. Oncol. 2016;12:13–19. [Google Scholar]
- 98.Zheng J., Zhang W., Li L., He Y., Wei Y., Dang Y., Nie S., Guo Z. Signaling Pathway and Small-Molecule Drug Discovery of FGFR: A Comprehensive Review. Front. Chem. 2022;10:860985. doi: 10.3389/fchem.2022.860985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kubick N., Klimovich P., Flournoy P.H., Bieńkowska I., Łazarczyk M., Sacharczuk M., Bhaumik S., Mickael M.-E., Basu R. Interleukins and Interleukin Receptors Evolutionary History and Origin in Relation to CD4+ T Cell Evolution. Genes. 2021;12:813. doi: 10.3390/genes12060813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ferreira V.L., Borba H.H., Bonetti A.D.F., Leonart L., Pontarolo R. Cytokines and Interferons: Types and Functions. In: Ali Khan W., editor. Autoantibodies and Cytokines. IntechOpen; Rijeka, Croatia: 2019. [Google Scholar]
- 101.Chen J.J.W., Yao P.-L., Yuan A., Hong T.-M., Shun C.-T., Kuo M.-L., Lee Y.-C., Yang P.-C. Up-regulation of tumor interleukin-8 expression by infiltrating macrophages: Its correlation with tumor angiogenesis and patient survival in non-small cell lung cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2003;9:729–737. [PubMed] [Google Scholar]
- 102.Pan B., Shen J., Cao J., Zhou Y., Shang L., Jin S., Cao S., Che D., Liu F., Yu Y. Author Correction: Interleukin-17 promotes angiogenesis by stimulating VEGF production of cancer cells via the STAT3/GIV signaling pathway in non-small-cell lung cancer. Sci. Rep. 2020;10:8808. doi: 10.1038/s41598-020-65650-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Huang Q., Duan L., Qian X., Fan J., Lv Z., Zhang X., Han J., Wu F., Guo M., Hu G., et al. IL-17 Promotes Angiogenic Factors IL-6, IL-8, and Vegf Production via Stat1 in Lung Adenocarcinoma. Sci. Rep. 2016;6:36551. doi: 10.1038/srep36551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Leung J.H., Ng B., Lim W.-W. Interleukin-11: A Potential Biomarker and Molecular Therapeutic Target in Non-Small Cell Lung Cancer. Cells. 2022;11:2257. doi: 10.3390/cells11142257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang J., Veeramachaneni N. Targeting interleukin-1β and inflammation in lung cancer. Biomark. Res. 2022;10:5. doi: 10.1186/s40364-021-00341-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Song L., Smith M.A., Doshi P., Sasser K., Fulp W., Altiok S., Haura E.B. Antitumor Efficacy of the Anti-Interleukin-6 (IL-6) Antibody Siltuximab in Mouse Xenograft Models of Lung Cancer. J. Thorac. Oncol. 2014;9:974–982. doi: 10.1097/JTO.0000000000000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gao S.P., Mark K.G., Leslie K., Pao W., Motoi N., Gerald W.L., Travis W.D., Bornmann W., Veach D., Clarkson B., et al. Mutations in the EGFR kinase domain mediate STAT3 activation via IL-6 production in human lung adenocarcinomas. J. Clin. Investig. 2007;117:3846–3856. doi: 10.1172/JCI31871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Briukhovetska D., Dörr J., Endres S., Libby P., Dinarello C.A., Kobold S. Interleukins in cancer: From biology to therapy. Nat. Rev. Cancer. 2021;21:481–499. doi: 10.1038/s41568-021-00363-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Heo T.-H., Wahler J., Suh N. Potential therapeutic implications of IL-6/IL-6R/gp130-targeting agents in breast cancer. Oncotarget. 2016;7:15460–15473. doi: 10.18632/oncotarget.7102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kim N.-H., Kim S.-K., Kim D.-S., Zhang D., Park J.-A., Yi H., Kim J.-S., Shin H.-C. Anti-proliferative action of IL-6R-targeted antibody tocilizumab for non-small cell lung cancer cells. Oncol. Lett. 2015;9:2283–2288. doi: 10.3892/ol.2015.3019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rose-John S., Jenkins B.J., Garbers C., Moll J.M., Scheller J. Targeting IL-6 trans-signalling: Past, present and future prospects. Nat. Rev. Immunol. 2023:1–16. doi: 10.1038/s41577-023-00856-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mohammed A., Dashwood R.H., Dickinson S., Disis M.L., Jaffee E.M., Johnson B.D., Khleif S.N., Pollak M.N., Schlom J., Shoemaker R.H., et al. Translational Advances in Cancer Prevention Agent Development (TACPAD) Virtual Workshop on Immunomodulatory Agents: Report. J. Cancer Prev. 2021;26:309–317. doi: 10.15430/JCP.2021.26.4.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ray K., Ujvari B., Ramana V., Donald J. Cross-talk between EGFR and IL-6 drives oncogenic signaling and offers therapeutic opportunities in cancer. Cytokine Growth Factor Rev. 2018;41:18–27. doi: 10.1016/j.cytogfr.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 114.Yan X., Han L., Zhao R., Fatima S., Zhao L., Gao F. Prognosis value of IL-6, IL-8, and IL-1β in serum of patients with lung cancer: A fresh look at interleukins as a biomarker. Heliyon. 2022;8:e09953. doi: 10.1016/j.heliyon.2022.e09953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nakamura T., Mizuno S. The discovery of hepatocyte growth factor (HGF) and its significance for cell biology, life sciences and clinical medicine. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2010;86:588–610. doi: 10.2183/pjab.86.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Balkwill F. Cancer and the chemokine network. Nat. Rev. Cancer. 2004;4:540–550. doi: 10.1038/nrc1388. [DOI] [PubMed] [Google Scholar]
- 117.Stabile L.P., Rothstein M.E., Keohavong P., Jin J., Yin J., Land S.R., Dacic S., Luong T.M., Kim K.J., Dulak A.M., et al. Therapeutic targeting of human hepatocyte growth factor with a single neutralizing monoclonal antibody reduces lung tumorigenesis. Mol. Cancer Ther. 2008;7:1913–1922. doi: 10.1158/1535-7163.MCT-07-2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Marmor M.D., Skaria K.B., Yarden Y. Signal transduction and oncogenesis by ErbB/HER receptors. Int. J. Radiat. Oncol. 2004;58:903–913. doi: 10.1016/j.ijrobp.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 119.Riudavets M., Sullivan I., Abdayem P., Planchard D. Targeting HER2 in non-small-cell lung cancer (NSCLC): A glimpse of hope? An updated review on therapeutic strategies in NSCLC harbouring HER2 alterations. ESMO Open. 2021;6:100260. doi: 10.1016/j.esmoop.2021.100260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Uy N.F., Merkhofer C.M., Baik C.S. HER2 in Non-Small Cell Lung Cancer: A Review of Emerging Therapies. Cancers. 2022;14:4155. doi: 10.3390/cancers14174155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Farooqi A.A., Siddik Z.H. Platelet-derived growth factor (PDGF) signalling in cancer: Rapidly emerging signalling landscape: PDGF-induced Signalling Cascades. Cell Biochem. Funct. 2015;33:257–265. doi: 10.1002/cbf.3120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Paluri R., Madan A., Li P., Jones B., Saleh M., Jerome M., Miley D., Keef J., Robert F. Phase 1b trial of nintedanib in combination with bevacizumab in patients with advanced solid tumors. Cancer Chemother. Pharmacol. 2019;83:551–559. doi: 10.1007/s00280-018-3761-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Makinde T., Agrawal D.K. Intra and extravascular transmembrane signalling of angiopoietin-1-Tie2 receptor in health and disease. J. Cell. Mol. Med. 2008;12:810–828. doi: 10.1111/j.1582-4934.2008.00254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Khan K.A., Wu F.T., Cruz-Munoz W., Kerbel R.S. Ang2 inhibitors and Tie2 activators: Potential therapeutics in perioperative treatment of early stage cancer. EMBO Mol. Med. 2021;13:e08253. doi: 10.15252/emmm.201708253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mehta V., Fields L., Evans I.M., Yamaji M., Pellet-Many C., Jones T., Mahmoud M., Zachary I. VEGF (Vascular Endothelial Growth Factor) Induces NRP1 (Neuropilin-1) Cleavage via ADAMs (a Disintegrin and Metalloproteinase) 9 and 10 to Generate Novel Carboxy-Terminal NRP1 Fragments That Regulate Angiogenic Signaling. Arterioscler. Thromb. Vasc. Biol. 2018;38:1845–1858. doi: 10.1161/ATVBAHA.118.311118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hong T.-M., Chen Y.-L., Wu Y.-Y., Yuan A., Chao Y.-C., Chung Y.-C., Wu M.-H., Yang S.-C., Pan S.-H., Shih J.-Y., et al. Targeting neuropilin 1 as an antitumor strategy in lung cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2007;13:4759–4768. doi: 10.1158/1078-0432.CCR-07-0001. [DOI] [PubMed] [Google Scholar]
- 127.Liu S.-D., Zhong L.-P., He J., Zhao Y.-X. Targeting neuropilin-1 interactions is a promising anti-tumor strategy. Chin. Med. J. 2021;134:508–517. doi: 10.1097/CM9.0000000000001200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.