Abstract
Objective:
Despite increased awareness, osteoporosis screening rates remain low. The objective of this survey study was to identify physician-reported barriers to osteoporosis screening.
Methods:
We conducted a survey of 600 physician members of the Endocrine Society, American Academy of Family Practice, and American Geriatrics Society. The respondents were asked to rate barriers to osteoporosis screening in their patients. We performed multivariable logistic regression analyses to determine correlates with the most commonly reported barriers.
Results:
Of 566 response-eligible physicians, 359 completed the survey (response rate, 63%). The most commonly reported barriers to osteoporosis screening included patient nonadherence (63%), physician concern about cost (56%), clinic visit time constraints (51%), low on the priority list (45%), and patient concern about cost (43%). Patient nonadherence as a barrier was correlated with physicians in academic tertiary centers (odds ratio [OR], 2.34; 95% confidence interval [CI], 1.06–5.13), whereas clinic visit time constraints were correlated with physicians in both community-based academic affiliates and academic tertiary care ([OR, 1.96; 95% CI, 1.10–3.50] and [OR, 2.48; 95% CI, 1.22–5.07], respectively). Geriatricians (OR, 0.40; 95% CI, 0.21–0.76) and physicians with >10 years in practice were less likely to report clinic visit time constraints as a barrier (11–20 years: OR, 0.41; 95% CI, 0.20–0.85; >20 years: OR, 0.32; 95% CI, 0.16–0.65). Physicians with more patient-facing time (3–5 compared with 0.5–2 d/wk) were more likely to place screening low on the priority list (OR, 2.66; 95% CI, 1.34–5.29).
Conclusion:
Understanding barriers to osteoporosis screening is vital in developing strategies to improve osteoporosis care.
Keywords: osteoporosis, screening, barriers, survey
Introduction
It has been estimated that >10 million Americans have osteoporosis and >40 million are at risk.1 Approximately one half of women and one third of men aged >50 years sustain an osteoporotic fracture in their lifetime, resulting in disability, financial burden, reduced quality of life, and an increased risk of mortality.2,3 In an effort to address this growing public health issue, multiple medical societies and organizations have issued guidelines regarding osteoporosis screening aimed at reducing fracture-related morbidity and mortality.4–7 For example, the Endocrine Society recommends osteoporosis screening for women aged ≥65 years and higher-risk men, ie, those aged ≥70 years and those aged 50 to 69 years with risk factors.4,7
Despite the high prevalence and significant impact of osteoporosis in the aging population as well as multiple existing guidelines and increased awareness, overall screening rates remain low in both older women and men.8–13 A large study of >1.5 million women in the United States found that only 26.5% of women aged 65 to 79 years and 12.8% of women aged ≥80 years were screened for osteoporosis between 2008 and 2014 despite recommendations for universal screening.10 Our team has previously shown that there is significant heterogeneity in osteoporosis screening in men, with more underscreening in some scenarios than in women.14
There are multiple factors involved in the decision to screen for osteoporosis, including physician factors (such as awareness of guidelines) and patient factors (age, risk factors, willingness to undergo screening, patient preferences, etc). The objective of this study was to better understand physician-level barriers to osteoporosis screening in women and men in real-world settings by conducting a nationwide survey of a diverse cohort of physicians caring for patients with osteoporosis, including primary care physicians, endocrinologists, and geriatricians. Understanding these barriers will help facilitate improved care for patients with osteoporosis.
Methods
Study Population
A total of 600 randomly selected physician members of the Endocrine Society, American Academy of Family Practice, and American Geriatrics Society were surveyed. Similar to prior work by our team, we employed a modified Dillman method of survey administration and provided a $25 cash incentive in order to enhance our response rate.14–16
Data from the survey were deidentified and electronically entered using a double-entry method to ensure a <1% error. Overall, 34 physicians were ineligible because they were deceased, ill, or not treating patients with osteoporosis or had an incorrect mailing address. Of the remaining 566 response-eligible physicians, 359 completed the survey, with a 63% (359/566) response rate. The study was granted exemption by the University of Michigan Institutional Review Board.
Survey Design and Measures
The survey instrument was developed based on our team’s prior experience with surveying physicians who provide care for patients with osteoporosis and after a systematic review of existing literature. We employed standard techniques to ensure content validity, including reviews by clinicians (endocrinologists, primary care physicians, and geriatricians) and survey methodologists, and performed pilot testing of the survey questionnaire among a selected multidisciplinary group of physicians involved in osteoporosis screening at the University of Michigan.
The physicians were asked about their specialty, practice setting, years in practice since completion of residency, percentage of male versus female patients treated in clinics, and number of days spent providing patient care in an average week as well as whether they had read specific guidelines on osteoporosis screening. Physician specialty was categorized as endocrinology, primary care (including internal medicine and family medicine), and geriatrics. Practice setting was categorized as private practice, community-based academic affiliates, and academic tertiary care centers. Because physicians who see more female patients may be more likely to screen for osteoporosis, the physicians were categorized by self-reported percentage of patients who were men versus those who were women. With regard to guidelines, all physicians were asked to state whether they had read any of the following guidelines: 2008 Screening for Osteoporosis in Men: A Clinical Practice Guideline from the American College of Physicians, 2008 National Osteoporosis Foundation Clinical Practice Guidelines, 2012 Osteoporosis in Men: An Endocrine Society Clinical Practice Guideline, 2014 National Osteoporosis Foundation: Clinician’s Guide to Prevention and Treatment of Osteoporosis, and 2017 Treatment of Low Bone Density or Osteoporosis to Prevent Fractures in Men and Women: A Clinical Practice Guideline Update from the American College of Physicians.4,17–19
The physicians were also asked to rate how likely the following factors were to be barriers to offering osteoporosis screening to their patients by ordering a bone density scan: patient nonadherence, physician concern about cost, clinic visit time constraints, low on the priority list, patient concern about cost, lack of patient education, lack of clinical decision support tools to determine whether the patient would benefit from osteoporosis screening, patient requests for tests/treatments, unawareness of guidelines, patients relying on physicians for recommendations (as a barrier to shared decision making), uncertainty about patient involvement in the decision-making process, uncertainty about patient preferences, concern about patient dissatisfaction, and concern about radiation exposure from bone density scan. The response categories were based on a 5-point Likert scale as follows: very likely, likely, somewhat likely, unlikely, or not at all likely.
Statistical Analyses
Descriptive data were generated with frequencies and percentages. Then, multivariable logistic regression analyses were performed to determine the association between physician characteristics and the 5 most highly rated barriers, including patient nonadherence, physician concern about cost, clinic visit time constraints, low on the priority list, and patient concern about cost. The 5-point Likert scale was dichotomized as very likely, likely, and somewhat likely versus unlikely or not at all likely. Missing data were <5% per survey item and not included in the analyses. All statistical analyses were performed using R, version 3.5.2. A 95% CI not including the null value was considered to be statistically significant. A P value of <.05 was considered to be statistically significant.
Results
The response rate was 63% (359/566). The respondent characteristics are shown in Table 1, with each physician specialty equally represented in our sample. The majority (82%) of the physicians reported seeing patients for at least 3 to 5 d/wk. More than half (54%) of the respondents reported having read at least 1 of the guidelines mentioned above on osteoporosis screening.
Table 1.
Physician Characteristics (N = 359)a
| Physician characteristics | n (%) |
|---|---|
|
| |
| Specialty | |
| Primary care | 128 (36.1) |
| Endocrinology | 114 (32.1) |
| Geriatrics | 113 (31.8) |
| Practice setting | |
| Private practice | 173 (50.6) |
| Community-based academic affiliate | 106 (31.0) |
| Academic tertiary care center | 63 (18.4) |
| Years in practice (y) | |
| 0–10 | 67 (18.9) |
| 11–20 | 102 (28.7) |
| >20 | 186 (52.4) |
| Days per week providing patient care (d/wk) | |
| 0.5–2 | 62 (17.6) |
| 3–5 | 290 (82.4) |
| Percentage of patients who are men (%) | |
| 0–25 | 44 (12.4) |
| 26–50 | 259 (73.2) |
| 51–100 | 51 (14.4) |
| Read guidelines on osteoporosis | |
| No | 165 (46.0) |
| Yes | 194 (54.0) |
The Figure shows the factors reported by the physicians to be somewhat likely to very likely barriers to offering screening for osteoporosis to their patients. The most commonly reported barriers to screening for osteoporosis included patient nonadherence (63%), physician concern about cost (56%), clinic visit time constraints (51%), low on the priority list (45%), and patient concern about cost (43%). Concern regarding radiation exposure from bone density scans was reported to be the least likely barrier to offering osteoporosis screening (5%).
Fig.
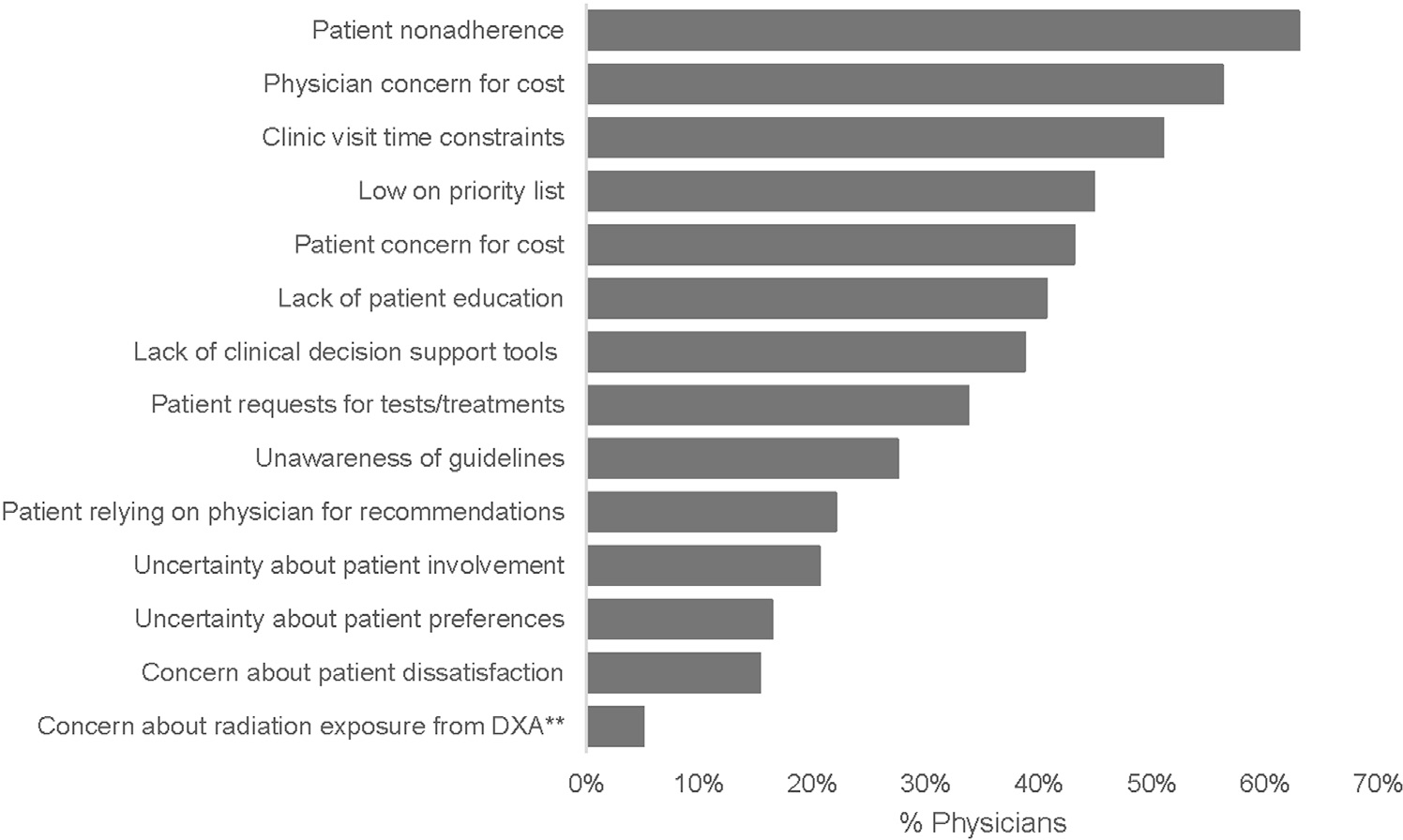
Physician-reported barriers to screening for osteoporosis in men and women*. *Factors reported as somewhat likely, likely, or very likely to be barriers to osteoporosis screening. **Dual-energy x-ray densitometry, also known as bone density scan. DXA = dual-energy x-ray densitometry.
Table 2 shows the results of the multivariable regression analyses of correlates with the most common physician-reported barriers to screening for osteoporosis. Of the 5 most commonly reported barriers, physicians practicing in academic tertiary care settings were more likely to report patient nonadherence as a barrier than those practicing in private practice (odds ratio [OR], 2.34; 95% CI, 1.06–5.13). Compared with primary care physicians, geriatricians were less likely to report concern about cost as a barrier to screening (OR, 0.48; 95% CI, 0.26–0.89). Compared with primary care physicians, geriatricians and those who had been in practice for >11 years were less likely to report clinic visit time constraints as a barrier ([OR, 0.40; 95% CI, 0.21–0.76] and [OR, 0.41; 95% CI, 0.20–0.85], respectively). Conversely, physicians practicing in community-based academic affiliates and academic centers were more likely to report clinic visit time constraints as a barrier to screening ([OR, 1.96; 95% CI, 1.10–3.50] and [OR, 2.48; 95% CI, 1.22–5.07], respectively). In addition, physicians seeing patients 3 to 5 d/wk were more likely to place screening for osteoporosis low on the priority list (OR, 2.66; 95% CI, 1.34–5.29) than those seeing patients 0.5 to 2 d/wk. None of the commonly reported barriers differed between the endocrinologists and our reference group, primary care physicians. Detailed results of the multivariable regression analyses are outlined in Table 2.
Table 2.
Physician Characteristics Associated With Common Physician-Reported Barriers to Osteoporosis Screeninga
| Patient nonadherence |
Physician concern for cost |
Clinic visit time constraints |
Low on the priority list |
Patient concern for cost |
|
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
|
| |||||
| Physician characteristics | |||||
| Specialty | |||||
| Primary care | Ref | Ref | Ref | Ref | Ref |
| Endocrinology | 0.69 (0.35–1.36) | 1.23 (0.65–2.35) | 0.80 (0.42–1.50) | 1.14 (0.60–2.17) | 1.20 (0.64–2.25) |
| Geriatrics | 0.65 (0.34–1.25) | 0.48 (0.26–0.89)b | 0.40 (0.21–0.76)b | 0.59 (0.31–1.12) | 0.65 (0.35–1.21) |
| Practice setting | |||||
| Private practice | Ref | Ref | Ref | Ref | Ref |
| Community-based academic affiliate | 1.60 (0.87–2.96) | 1.60 (0.89–2.89) | 1.96 (1.10–3.50)b | 1.59 (0.89–2.83) | 0.67 (0.38–1.18) |
| Academic tertiary care center | 2.34 (1.06–5.13)b | 0.68 (0.34–1.36) | 2.48 (1.22–5.07)b | 1.72 (0.84–3.53) | 0.63 (0.31–1.27) |
| Years in practice (y) | |||||
| 0–10 | Ref | Ref | Ref | Ref | Ref |
| 11–20 | 0.53 (0.24–1.16) | 0.43 (0.21–0.88)b | 0.41 (0.20–0.85)b | 0.51 (0.25–1.03) | 0.38 (0.19–0.77)b |
| >20 | 0.59 (0.28–1.23) | 0.72 (0.37–1.42) | 0.32 (0.16–0.65)b | 0.35 (0.18–0.69)b | 0.53 (0.28–1.02) |
| Days per week providing patient care (d/wk) | |||||
| 0.5–2 | Ref | Ref | Ref | Ref | Ref |
| 3–5 | 1.79 (0.88–3.61) | 1.48 (0.77–2.85) | 1.80 (0.93–3.51) | 2.66 (1.34–5.29)b | 0.90 (0.46–1.73) |
| Percentage of male patients (%) | |||||
| 0–25 | Ref | Ref | Ref | Ref | Ref |
| 26–50 | 0.62 (0.27–1.41) | 0.64 (0.31–1.34) | 0.49 (0.24–1.00) | 0.73 (0.35–1.54) | 0.49 (0.23–1.04) |
| 51–100 | 0.95 (0.34–2.65) | 0.87 (0.35–2.18) | 0.93 (0.37–2.33) | 0.69 (0.27–1.74) | 0.59 (0.24–1.48) |
| Read guidelines on osteoporosis | |||||
| No | Ref | Ref | Ref | Ref | Ref |
| Yes | 1.61 (0.93–2.79) | 0.93 (0.56–1.56) | 1.13 (0.68–1.89) | 0.41 (0.24–0.70)b | 0.74 (0.44–1.24) |
Abbreviations: OR = odds ratio; Ref = reference.
Missing data not included.
Statistically significant results.
Discussion
Our findings from this large nationwide survey of primary care physicians, endocrinologists, and geriatricians underscore that barriers to osteoporosis screening still exist at the physician level. The most commonly reported barriers were patient nonadherence, physician concern about cost, clinic visit time constraints, and osteoporosis screening being placed low on the priority list. The physician-reported barriers to osteoporosis screening varied by specialty, practice setting, years in practice, number of days spent seeing patients in clinics, and whether pertinent guidelines were read.
Prior studies on barriers to guideline adherence have found that physician knowledge, attitudes, and behavior can impact guideline adherence, with primary barriers differing by setting.10,20–24 The current study illustrates the importance of external barriers, such as patient factors (eg, adherence) and environmental factors (eg, clinic visit time constraints and costs), in adherence to osteoporosis guidelines. Prior studies examining barriers to osteoporosis screening focused on primary care physicians only, reporting difficulty in communicating with patients about the risk of osteoporosis, fracture prevention, time constraints, and competing health issues as main barriers.21,22 In contrast to these prior studies, we examined physician-level barriers to osteoporosis screening across a diverse group of both primary care and specialty physicians to better reflect real-world settings.
Patient nonadherence was the most commonly reported barrier to osteoporosis screening among the surveyed physicians in our study, with physicians working in academic centers being more likely to report this as a barrier. Although this is an ongoing concern for preventive care in general and not limited to screening for osteoporosis, there are, likely, a multitude of factors that play a role. The fear of side effects and lack of perceived benefits of osteoporosis medications if initiated, poor physician understanding of patients’ concerns leading to nonadherence, and insufficient awareness of disease-related consequences have all been implicated.25–27 Further examination of the perceptions of patients and circulation of information (and misinformation) are necessary to fully understand the reasons behind patient nonadherence as a barrier to osteoporosis screening. Additionally, it is important to provide physician training to enable clear physician-patient communication and patient education to help patients understand their risk and empower them to actively participate in shared decision making and support adherence.
Longer clinic visits have been shown to be associated with greater patient centeredness and improved provider-patient communication to allow for more attention to preventive health, suggesting a direct relationship between visit duration and the quality of screening-based care.28,29 In accordance, prior studies have found that when faced with limited time, primary care physicians would generally recommend fewer preventive care services.30,31 We found that physicians practicing in community-based academic affiliates and academic centers were more likely to report clinic visit time constraints as a barrier to osteoporosis screening, whereas geriatricians were less likely to report this than primary care physicians. How physicians prioritize specific health issues per clinic visit could be related to their training, specific patient cohort, and clinic setting.
Our study also showed that physicians who had greater patient-facing time per week were more likely to place osteoporosis screening low on the priority list. Physicians who have less patient-facing time per week have less patient volume and may have more specialized clinics, therefore influencing prioritization. With the widespread use of electronic medical records, best practice advisories have been used to prompt screening. However, current evidence has not shown this strategy to be overwhelmingly effective,32,33 and alternative interventions may be needed.
Physician and patient concerns about the cost of tests/lack of insurance coverage were also reported by the physicians as significant barriers to osteoporosis screening. In an effort to address cost barriers, Medicare has been covering osteoporosis screening for qualified individuals at 2-year intervals since 1998, and preventive care provisions under the Affordable Care Act have been eliminating cost sharing among privately insured women and qualified Medicare beneficiaries since 2010.34,35 Despite these efforts, osteoporosis still remains markedly underdiagnosed.36,37 Identification of this barrier certainly presents an opportunity for physician and patient education on insurance coverage to help improve screening rates.
Lastly, physicians who responded as having read the guidelines were less likely to place screening for osteoporosis low on their priority list. This emphasizes the need for continued dissemination of the guidelines and the importance of keeping abreast with the latest evidence-based literature. Raising awareness of the importance of osteoporosis screening among physicians and increasing patient engagement can aid in improved rates of screening,13,38–40 suggesting that multilevel interventions are needed for successful implementation.
Our study findings provide valuable information regarding the barriers faced by physicians in osteoporosis screening practices. Our study has several strengths, including the inclusion of a diverse cohort of physicians from different specialties who care for patients with osteoporosis, sampling at a national level, and a high response rate. However, there are also potential limitations that should be considered. Although our survey included a comprehensive list of potential barriers in screening for osteoporosis, there may have been additional factors influencing physician decision making to offer osteoporosis screening that were not included in the survey. Additionally, although nonresponse bias is a known potential limitation of survey studies, the high response rate of 63% likely mitigates this risk. Lastly, participation in the survey was voluntary, and there is potential for selection bias.
In summary, our study highlights that several barriers to osteoporosis screening still exist. Identifying these barriers provides key opportunities and avenues to improve the receipt of osteoporosis screening during time-constrained clinical visits. From our survey, we have learnt that these barriers are not limited to the physician level (ie, knowledge issues) but are an amalgamation of physician, patient, and external factors. Tailored, multilevel interventions may be needed to potentially improve osteoporosis screening rates for both men and women as well as reduce the risk of fractures.
Highlights.
Despite increased awareness, osteoporosis screening rates remain low
Non-adherence, cost concerns, and time constraints were common barriers to screening
Geriatricians were less likely to report clinic visit time constraints as a barrier
Physicians with more patient-facing time placed screening low on the priority list
Understanding barriers to osteoporosis screening may improve osteoporosis care
Clinical Relevance.
Despite increased awareness, osteoporosis screening rates in the United States remain low. Our study highlights that physician-reported barriers to osteoporosis screening still exist. Thus, identifying and addressing these barriers will provide opportunities to enhance the receipt of appropriate osteoporosis screening during time-constrained clinical visits, thereby improving osteoporosis care and reducing the risk of fractures.
Acknowledgment
We would like to acknowledge David Reyes-Gastelum for statistical support. This work was supported by grant K08 AG049684 from the National Institute on Aging to Dr Papaleontiou. The funding source had no such involvement in the study design; collection of, analysis, and interpretation of data; writing of the report; and decision to submit this article for publication.
Abbreviations:
- OR
odds ratio
Footnotes
Disclosure
The authors have no multiplicity of interest to disclose.
References
- 1.Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520–2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hopkins RB, Pullenayegum E, Goeree R, et al. Estimation of the lifetime risk of hip fracture for women and men in Canada. Osteoporos Int. 2012;23(3): 921–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475. [DOI] [PubMed] [Google Scholar]
- 4.Watts NB, Adler RA, Bilezikian JP, et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(6): 1802–1822. [DOI] [PubMed] [Google Scholar]
- 5.US Preventive Services Task Force. Screening for osteoporosis: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2011;154(5): 356–364. [DOI] [PubMed] [Google Scholar]
- 6.Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract. 2020;26(1):1–46. [DOI] [PubMed] [Google Scholar]
- 7.The Endocrine Society recommends individualization of bone mineral density testing frequency in women over the age of 67. The Endocrine Society. Accessed December 20, 2022. https://www.endocrine.org//media/endocrine/files/advocacy/societyletters/endocrinesocietyresponsetobmdtestingfinal.pdf
- 8.Benes G, David J, Synowicz M, et al. Race and age impact osteoporosis screening rates in women prior to hip fracture. Arch Osteoporos. 2022;17(1):34. [DOI] [PubMed] [Google Scholar]
- 9.Curtis JR, Carbone L, Cheng H, et al. Longitudinal trends in use of bone mass measurement among older Americans, 1999–2005. J Bone Miner Res. 2008;23(7):1061–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gillespie CW, Morin PE. Trends and disparities in osteoporosis screening among women in the United States, 2008–2014. Am J Med. 2017;130(3): 306–316. [DOI] [PubMed] [Google Scholar]
- 11.Amarnath AL, Franks P, Robbins JA, Xing G, Fenton JJ. Underuse and overuse of osteoporosis screening in a regional health system: a retrospective cohort study. J Gen Intern Med. 2015;30(12):1733–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gallagher TC, Geling O, Comite F. Missed opportunities for prevention of osteoporotic fracture. Arch Intern Med. 2002;162(4):450–456. [DOI] [PubMed] [Google Scholar]
- 13.Lafata JE, Kolk D, Peterson EL, et al. Improving osteoporosis screening: results from a randomized cluster trial. J Gen Intern Med. 2007;22(3):346–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choksi P, Gay BL, Reyes-Gastelum D, Haymart MR, Papaleontiou M. Understanding osteoporosis screening practices in men: a nationwide physician survey. Endocr Pract. 2020;26(11):1237–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dillman DA. Mail and internet surveys: the tailored design method. 2nd ed. New York: Wiley; 2007. [Google Scholar]
- 16.Papaleontiou M, Choksi P, Reyes-Gastelum D. Practice patterns in the treatment of male osteoporosis. Endocr Pract. 2019;25(10):1077–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qaseem A, Snow V, Shekelle P, et al. Screening for osteoporosis in men: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;148(9):680–684. [DOI] [PubMed] [Google Scholar]
- 18.Watts NB, Lewiecki EM, Miller PD, Baim S. National Osteoporosis Foundation 2008 clinician’s guide to prevention and treatment of osteoporosis and the World Health Organization Fracture Risk Assessment Tool (FRAX): what they mean to the bone densitometrist and bone technologist. J Clin Densitom. 2008;11(4):473–477. [DOI] [PubMed] [Google Scholar]
- 19.Qaseem A, Forciea MA, McLean RM, Denberg TD. Clinical Guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(11):818–839. [DOI] [PubMed] [Google Scholar]
- 20.McAdam-Marx C, Unni S, Ye X, Nelson S, Nickman NA. Effect of medicare reimbursement reduction for imaging services on osteoporosis screening rates. J Am Geriatr Soc. 2012;60(3):511–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaglal SB, Carroll J, Hawker G, et al. How are family physicians managing osteoporosis? Qualitative study of their experiences and educational needs. Can Fam Physician. 2003;49(4):462e468. [PMC free article] [PubMed] [Google Scholar]
- 22.Jaglal SB, McIsaac WJ, Hawker G, et al. Information needs in the management of osteoporosis in family practice: an illustration of the failure of the current guideline implementation process. Osteoporos Int. 2003;14(8):672–676. [DOI] [PubMed] [Google Scholar]
- 23.Pritchard J, Karampatos S, Ioannidis G, et al. Osteoporosis guideline implementation in family medicine using electronic medical records: survey of learning needs and barriers. Can Fam Physician. 2016;62(6):e326–e333. [Google Scholar]
- 24.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines?: a framework for improvement. JAMA. 1999;282(15): 1458–1465. [DOI] [PubMed] [Google Scholar]
- 25.McHorney CA, Schousboe JT, Cline RR, Weiss TW. The impact of osteoporosis medication beliefs and side-effect experiences on non-adherence to oral bisphosphonates. Curr Med Res Opin. 2007;23(12):3137–3152. [DOI] [PubMed] [Google Scholar]
- 26.Seeman E, Compston JU, Adachi JO, et al. Non-compliance: the Achilles’ heel of anti-fracture efficacy. Osteoporos Int. 2007;18(6):711–719. [DOI] [PubMed] [Google Scholar]
- 27.Copher R, Buzinec P, Zarotsky V, Kazis L, Iqbal SU, Macarios D. Physician perception of patient adherence compared with patient adherence of osteoporosis medications from pharmacy claims. Curr Med Res Opin. 2010;26(4): 777–785. [DOI] [PubMed] [Google Scholar]
- 28.Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract. 2002;52(485):1012–1020. [PMC free article] [PubMed] [Google Scholar]
- 29.Chen LM, Farwell WR, Jha AK. Primary care visit duration and quality: does good care take longer? Arch Intern Med. 2009;169(20):1866–1872. [DOI] [PubMed] [Google Scholar]
- 30.Zhang JJ, Rothberg MB, Misra-Hebert AD, Gupta NM, Taksler GB. Assessment of physician priorities in delivery of preventive care. JAMA Netw Open. 2020;3(7), e2011677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pollak KI, Krause KM, Yarnall KS, Gradison M, Michener JL, Ostbye T. Estimated time spent on preventive services by primary care physicians. BMC Health Serv Res. 2008;8(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rolnick SJ, Jackson JM, Amundson JH. Development, implementation and evaluation of an electronic medical record prompt for bone density testing. Health Informatics J. 2009;15(4):296–304. [DOI] [PubMed] [Google Scholar]
- 33.El-Kareh RE, Gandhi TK, Poon EG, et al. Actionable reminders did not improve performance over passive reminders for overdue tests in the primary care setting. J Am Med Inform Assoc. 2011;18(2):160–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Public law number 105–33. (H.R. 2015). Balanced Budget Act of 1997. Accessed September 20, 2022. https://www.gpo.gov/fdsys/pkg/PLAW-105publ33/pdf/PLAW-105publ33.pdf
- 35.Public law number 111–148. (H.R. 3590). Patient Protection and Affordable Care Act. Accessed September 20, 2022. https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf
- 36.Vestergaard P, Rejnmark L, Mosekilde L. Osteoporosis is markedly underdiagnosed: a nationwide study from Denmark. Osteoporos Int. 2005;16(2): 134–141. [DOI] [PubMed] [Google Scholar]
- 37.McNally DN, Kenny AM, Smith JA. Adherence of academic geriatric practitioners to osteoporosis screening guidelines. Osteoporos Int. 2007;18(2): 177–183. [DOI] [PubMed] [Google Scholar]
- 38.Ayoub WT, Newman ED, Blosky MA, Stewart WF, Wood GC. Improving detection and treatment of osteoporosis: redesigning care using the electronic medical record and shared medical appointments. Osteoporos Int. 2009;20(1): 37–42. [DOI] [PubMed] [Google Scholar]
- 39.Denberg TD, Myers BA, Lin CT, et al. An outreach intervention increases bone densitometry testing in older women. J Am Geriatr Soc. 2009;57(2): 341–347. [DOI] [PubMed] [Google Scholar]
- 40.Warriner AH, Outman RC, Kitchin E, et al. A randomized trial of a mailed intervention and self-scheduling to improve osteoporosis screening in postmenopausal women. J Bone Miner Res. 2012;27(12): 2603–2610. [DOI] [PMC free article] [PubMed] [Google Scholar]


