Abstract
Among the various zoonotic pathogens that infect horses, Anaplasma phagocytophilum, Borrelia spp. and Leishmania spp. have gained scientific interest, and relevant molecular and serological studies in horses have been conducted worldwide. Moreover, human and veterinary medicine have extensively applied alternatives to serum diagnostic samples—such as saliva—for detecting pathogens or antibodies. In this study, we investigated the exposure of horses in Greece to A. phagocytophilum, B. burgdorferi, and L. infantum, and we assessed the diagnostic accuracy of saliva compared to serum in detecting IgG antibodies against the abovementioned pathogens. Paired saliva and serum samples were collected from 317 horses from different regions in Greece. The paired samples were examined using the indirect fluorescent antibody test (IFAT) for detecting IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum. Sensitivity, specificity, positive likelihood ratio (PLR), and negative likelihood ratio (NLR) were determined to assess the validity of saliva as an alternative to serum. The receiver operating characteristic (ROC) curve revealed that the optimal cut-off value for detecting antibodies against all the examined pathogens in saliva was 1/10. Higher seropositivity rates were found for B. burgdorferi (15.14%) and A. phagocytophilum (14.19%) compared to L. infantum (1.26%). The detection of IgG antibodies using IFAT in saliva samples had a good test performance compared to serum. The two sample types had a substantial to almost perfect agreement. Although the sensitivity was moderate (70.83–75.56%) in all cases, the specificity was almost perfect to perfect (99.63–100%). This study provides the first evidence that horses in Greece are exposed to A. phagocytophilum and B. burgdorferi and confirms that the seroprevalence of L. infantum in horses in Greece remains low. Our findings suggest that saliva sampling coupled with IFAT could be successfully applied for detecting IgG antibodies against these important zoonotic pathogens in large-scale epidemiological studies in horses, at the population level, as an alternative to serum.
Keywords: Anaplasma phagocytophilum, Borrelia burgdorferi, horse, indirect fluorescence antibody test, Leishmania infantum, saliva
1. Introduction
The close contact of horses with humans, the global increase in horse movements, and the subsequent potential to spread zoonotic and equine diseases, coupled with the economic importance of this species, resulted in the investigation of its role in the epidemiology of significant human and equine pathogens in a One Health context [1,2]. Among the various zoonotic pathogens that infect horses, Anaplasma phagocytophilum, Borrelia spp., and Leishmania spp. have gained scientific interest, and relevant reports on equine infection and/or exposure have been produced all over the world [3,4,5,6].
Equine granulocytic anaplasmosis caused by A. phagocytophilum leads to subclinical or clinical disease [7]. The latter manifests as acute febrile illness with loss of appetite, lethargy, hemorrhages, and lameness, which is usually self-limiting [8]. Thrombocytopenia is a common laboratory finding that results in characteristic petechial hemorrhages on the mucosal surface of the lips and gums [6]. Diagnosis is usually based on history, clinical signs, and laboratory findings [9]. Anaplasma phagocytophilum morulae appear in the cytoplasm of neutrophils during the acute phase of the disease and can be detected through microscopy [6]. Molecular methods are also helpful for the diagnosis of equine granulocytic anaplasmosis as well as the detection of subclinical infections. The indirect fluorescent antibody test (IFAT) and enzyme-linked immunosorbent assay (ELISA) are the serological methods most commonly employed for detecting anti-A. phagocytophilum antibodies in horses [6,8]. Although serology presents limitations in individual diagnostics of subclinical cases, seroprevalence studies provide essential information about the serological status of the horse population globally [6,8]. The recorded seroprevalences differ among the countries, ranging from 4% in Switzerland to 72.8% in the Czech Republic [8,10]. Notably, previous studies suggested that equine A. phagocytophilum strains are similar or identical to those causing disease in humans and dogs [11].
Borrelia burgdorferi infection is usually asymptomatic in horses but naturally occurring syndromes with a broad spectrum of clinical manifestations, including arthritis, lameness, anterior uveitis, encephalitis, and cutaneous pseudolymphoma, have been documented. Although the causal relationship has not been proven in most cases [8], and there is a paucity of conclusive clinical equine borreliosis data in Europe, several case reports of equine neuroborreliosis with B. burgdorferi detection in the central nervous system have been reported in North America [12,13]. Furthermore, dual infections with A. phagocytophilum [14,15,16] have also been recorded, and are considered to increase the disease severity [17]. Studies in various countries globally have reported serological evidence of exposure to B. burgdorferi s.l in horses: from 0% in different regions in Africa to 48% in France [18].
Since the first case of equine cutaneous leishmaniosis in 1927 in Argentina, several studies have reported equine subclinical and cutaneous leishmaniosis cases [4]; Leishmania infantum in the Old World and L. (Viannia) braziliensis in the New World were the most frequently involved species. Leishmania infantum was also reported in Brazil when Soares et al. identified three autochthonous cases of mixed infection with L. braziliensis [19]. Leishmania (Mundinia) martiniquensis infection was detected in horses in Germany [20] and Florida [21]. As for the seroprevalence studies in horses, their findings vary significantly among different countries depending on the geographical area and the serological method used; seroprevalence ranges from 0.3% for L. infantum in Greece to 76.3% for L. (V.) braziliensis in Paraná State, Brazil [22,23,24,25,26]. The clinical signs of the disease are similar irrespective of the geographical location and the responsible Leishmania species; single or multiple papules or nodules located in the eyes, muzzle, neck, pinnae, scrotum, and legs are the most frequently reported manifestations, while visceral lesions have not been described until now [4]. Horses are considered a resistant host to Leishmania infections since both subclinical and clinical diseases are characterized by a lack of antibodies or low antibody titers [4,27,28]. Among the different serological methods, IFAT, direct agglutination test (DAT), and ELISA were the most frequently used in seroprevalence studies in horses [4,22,23,24].
Oral fluid or saliva has been extensively used for detecting pathogens or antibodies in infected individuals; human immunodeficiency virus, measles, rubella, and hepatitis A, B, and C viruses are some of the applications in human medicine up to now [29,30,31]. The body of literature is also increasing in veterinary medicine with oral fluid or saliva samples being used for the detection of infectious agents such as foot-and-mouth disease virus in cattle and porcine reproductive and respiratory syndrome virus in pigs but also antibodies against Actinobacillus pleuropneumoniae, PRRSV, and Toxoplasma gondii in pigs [32,33,34], L. infantum in dogs [35], feline immunodeficiency virus (FIV) and Bartonella henselae [36,37] in cats, and Gasterophilus intestinalis and tapeworms in horses [38,39]. The different studies show variable results regarding the performance of this alternative sample type ranging from poor to perfect agreement with the traditional serum samples.
The oral fluid or saliva sampling procedure is noninvasive, substantially easier, quicker, less stressful, and painless [39,40]. Although horses are generally tolerant to blood collection, oral fluid could be a useful alternative diagnostic sample type in cases where a massive collection of samples is needed in a straightforward and timely manner, such as epidemiological and surveillance studies and for the examination of show and racehorses, especially during international events. Moreover, oral fluid samples are easy to collect even from pet owners [39] or horse breeders, as adverse effects resulting from the sampling procedure and subsequent treatment recommendations from a qualified veterinarian are not anticipated. However, this alternative biological sample needs to be validated case-by-case against current gold standard methods to be used as a diagnostic tool.
In this study, we provide for the first time seropositivity data against A. phagocytophilum and B. burgdorferi in horses in Greece, and we report updated data on the seroprevalence of L. infantum in horses from different regions of the country. We also assess the diagnostic accuracy of saliva compared to serum when using IFAT to detect antibodies against these three important zoonotic pathogens in horses.
2. Materials and Methods
2.1. Animals
A total of 317 domestic horses aged 1 to 15 years old from two regions of Greece, Thessaly and Crete, were enrolled in the study. The horses were categorized into age ranges as follows: young (≤3 years), adult (>3 and <12 years), or senior (≥12 years). The regions are located at about 39°40′ Ν, 22°30′ Ε and 35°20′ N, 24°30′ E, respectively. The climate in Thessaly is continental, with a cool winter and warm summer, while in Crete, it is typically Mediterranean, with a mild winter and warm and dry summer. The horses were clinically healthy at the sampling time, except for being infested by ticks. The sampling took place from spring to summer.
2.2. Serum and Saliva Sampling
Saliva samples were collected using a Salivette® (Sarstedt, Nümbrecht, Germany) saliva collection kit as previously described [40], with minor modifications. In brief, following washing with tap water to remove any feed remnants, the cotton swab was maintained in the horse’s mouth vestibule for 30–40 s over and under the tongue, across the third or fourth maxillary premolar. Paired blood samples were obtained with an 18-G needle and 1 1/2 inches from the external jugular vein into a vacutainer tube (BD, Franklin Lakes, NJ, USA), without anticoagulant, for serum collection.
The blood and saliva samples collected in the nearby areas were promptly transferred directly to the Laboratory of the Clinic of Medicine, Faculty of Veterinary Medicine, School of Health Sciences, University of Thessaly, Greece. The samples collected from distant regions were centrifuged in local veterinary clinics, and then transported to the Laboratory of the Clinic of Medicine for further analysis and processing.
The blood samples were subjected to centrifugation at 400× g for 10 min, allowing for the separation of serum. The obtained serum samples were then transferred to plastic vials and refrigerated at −20 °C pending analysis. The saliva samples underwent centrifugation at 3000× g for 10 min at 4 °C and were subsequently stored at −80 °C until further testing.
2.3. IFAT in Serum and Saliva Samples
The serum and saliva samples were tested for the presence of IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum using IFAT. The IFAT was performed following the instructions provided by the manufacturer (MegaFLUO® ANAPLASMA ph., MegaFLUO® BORRELIA horse, and MegaFLUO® LEISH, Horbranz, Austria). The positive and negative controls with the respective conjugates provided by the manufacturer were used in each analysis. In the case of serum samples, cut-off values of 1/80 and 1/64 were used for A. phagocytophilum and B. burgdorferi, respectively, based on the instructions provided. For L. infantum, a cut-off value of 1/40 was employed as previously described [24]. As for the saliva samples, three dilutions were tested for all three pathogens: 1/10, 1/20, and 1/40. The observations were made using a Nikon Eclipse E-400 fluorescence (Nikon, Badhoevedorp, The Netherlands) microscope with a 100× objective.
2.4. Statistical Analysis
Sensitivity, specificity, positive likelihood ratio (PLR), and negative likelihood ratio (NLR) were determined to assess the validity of detecting antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum in saliva compared to serum, using the MedCalc Statistical Software version 14.8.1 (MedCalc Software bvba, Ostend, Belgium)). PLR values > 10 and NLR values < 0.1 indicated good performance [41]. The agreement between the antibody detection results in the two biological materials was measured using Cohen’s kappa (κ) value [42,43]. A value of 0 to 1 indicated a fair to perfect agreement, respectively. The same software was used to generate receiver operating characteristic (ROC) curves and areas under the curve (AUCs) and to determine the optimal threshold for the cut-off values used to detect antibodies against the previously mentioned pathogens. The accuracy based on the AUC values was categorized as low (0.5 < AUC ≤ 0.7), moderate (0.7 < AUC ≤ 0.9), or high (0.9 < AUC ≤ 1) [44]. The “N−1” chi-squared test was employed to determine the significance of the difference in the percentage of seropositivity among different age groups [45,46], using the abovementioned statistical software.
3. Results
Table 1 shows the numbers and percentages of positive samples for IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum and their combinations in both serum and saliva samples. Compared to serum, the number of positive saliva samples for anti-A. phagocytophilum and anti-B. burgdorferi antibodies was lower for all three cut-off values. Similarly, the number of positive saliva samples for anti-L. infantum antibodies was lower for the 1/20 and 1/40 cut-off values. However, the number of positive saliva samples for anti-L. infantum antibodies was the same as in serum for the 1/10 cut-off value. In all cases, the use of higher cut-off values resulted in a lower number of positive samples. Co-exposure was observed in six horses and concerned only A. phagocytophilum and B. burgdorferi.
Table 1.
The numbers and the percentages of positive samples for IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum and their combinations in both serum and saliva samples at the corresponding cut-off values.
| Pathogen | Serum | Saliva | ||
|---|---|---|---|---|
| Cut-Off | ||||
| 1/10 | 1/20 | 1/40 | ||
| A. phagocytophilum | 45/317 (14.20%) a | 35/317 (11.04%) a,b | 30/317 (9.46%) a,b | 23/317 (7.23%) b |
| B. burgdorferi | 48/317 (15.14%) a | 34/317 (10.73%) a.b |
31/317 (9.78%) b | 27/317 (8.25%) b |
| L. infantum | 4/317 (1.26%) a | 4/317 (1.26%) a |
2/317 (0.63%) a | 1/317 (0.32%) a |
|
A. phagocytophilum +
B. burgdorferi |
6/317 (1.89%) a | 4/317 (1.26%) a |
2/317 (0.63%) a |
1/317 (0.32%) a |
|
A. phagocytophilum +
L. infantum |
0% | 0% | 0% | 0% |
|
B. burgdorferi +
L. infantum |
0% | 0% | 0% | 0% |
|
A. phagocytophilum +
B. burgdorferi + L. infantum |
0% | 0% | 0% | 0% |
a,b Different superscripts next to percentages in different columns of the same row denote significant difference, p < 0.05.
Table 2 summarizes the number of positive serum samples per age group for IgG antibodies against A. phagocytophilum, B. burgdorferi, L. infantum, and their combinations. Statistical analysis showed that senior horses presented statistically significantly higher seropositivity for A. phagocytophilum and B. burgdorferi than the other two age categories. Similarly, the seropositivity rates for the co-exposure to A. phagocytophilum and B. burgdorferi were statistically significantly different among the three age groups with the senior group presenting the highest number of seropositive horses for both pathogens.
Table 2.
The numbers and percentages of positive samples per age group for IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum and their combinations in serum.
| Age Group Seropositive N * (%) |
|||
|---|---|---|---|
| Pathogen | ≤3 Years Old | 3–12 Years Old | ≥12 Years Old |
| A. phagocytophilum | 3 (6.7%) a | 25 (12.0%) a | 17 (26.6%) b |
| B. burgdorferi | 2 (4.4%) a | 26 (12.5%) a | 20 (31.3%) b |
| L. infantum | 0 (0%) a | 2 (1.0%) a | 2 (3.1%) a |
| A. phagocytophilum + B. burgdorferi | 0 (0%) a,b | 2 (1.0%) a | 4 (6.3%) b |
|
A. phagocytophilum +
L. infantum |
0 (0%) | 0 (0%) | 0 (0%) |
|
B. burgdorferi +
L. infantum |
0 (0%) | 0 (0%) | 0 (0%) |
|
A. phagocytophilum +
B. burgdorferi + L. infantum |
0 (0%) | 0 (0%) | 0 (0%) |
* N = Number. a,b Different superscripts next to percentages in different columns of the same row denote significant difference, p < 0.05.
The sensitivity, specificity, PLR, and NLR values for detecting anti-A. phagocytophilum, anti-B. burgdorferi, and anti-L. infantum antibodies in saliva when using three different cut-off values and when considering the detection of antibodies in serum as the reference method are presented in Table 3a–c.
Table 3.
(a) Sensitivity, specificity, positive likelihood ratio (PLR), and negative likelihood ratio (NLR) for detecting antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum in saliva with a cut-off value of 1/10, taking the results in serum as a reference. (b) Sensitivity, specificity, positive likelihood ratio (PLR), and negative likelihood ratio (NLR) for detecting antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum in saliva with a cut-off value of 1/20, taking the results in serum as a reference. (c) Sensitivity, specificity, positive likelihood ratio (PLR), and negative likelihood ratio (NLR) for detecting antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum in saliva with a cut-off value of 1/40, taking the results in serum as a reference.
| (a) | |||
| A. phagocytophilum | B. burgdorferi | L. infantum | |
| Sens. % (95% CI) | 75.56 (60.46–87.12) |
70.83 (55.94–83.05) |
75.00 (19.41–99.37) |
| Spec. % (95% CI) | 99.63 (97.97–99.99) |
100.00 (98.64–100.00) |
99.68 (98.23–99.99) |
| PLR (95% CI) | 205.51 (28.85–1464.02) |
- | 234.75 (30.62–1800.00) |
| NLR (95% CI) | 0.25 (0.15–0.41) |
0.29 (0.19–0.45) |
0.25 (0.05–1.37) |
| (b) | |||
| A. phagocytophilum | B. burgdorferi | L. infantum | |
| Sens. % (95% CI) | 64.44% (48.78–78.13) |
64.58% (49.46–77.84) |
50.00 (6.76–93.24) |
| Spec. % (95% CI) | 99.63 (97.97–99.99) |
100.00 (98.64–100.00) |
100.00 (98.83–100.00) |
| PLR (95% CI) | 175.29 (24.48–1254.92) |
- | - |
| NLR (95% CI) | 0.36 (0.24–0.53) |
0.35 (0.24–0.52) |
0.50 (0.19–1.33) |
| (c) | |||
| A. phagocytophilum | B. burgdorferi | L. infantum | |
| Sens. % (95% CI) | 51.11% (35.77–66.30) |
56.25% (41.18–70.52) |
25.00 (0.63–80.59) |
| Spec. % (95% CI) | 100.00 (98.65–100.00) |
100.00 (98.64–100.00) |
100.00 (98.83–100.00) |
| PLR (95% CI) | - | - | - |
| NLR (95% CI) | 0.49 (0.36–0.66) |
0.44 (0.32–0.60) |
0.75 (0.43–1.32) |
When using a cut-off value of 1/10, the sensitivity for detecting antibodies against A. phagocytophilum and L. infantum (75.56% and 75.00%, respectively) was higher than that for B. burgdorferi (70.83%). As for the specificity, it was perfect for detecting anti-B. burgdorferi antibodies, and almost perfect for detecting antibodies against the other two pathogens (99.63% and 99.98%, respectively). When a cut-off value of 1/20 was used, the sensitivity for detecting antibodies against A. phagocytophilum and B. burgdorferi was similar (64.44% and 64.58%, respectively), while it was 50% for detecting anti-L. infantum antibodies. The sensitivity for all the pathogens was even lower for the cut-off value of 1/40. On the contrary, the specificity was perfect or almost perfect when the 1/20 and 1/40 cut-off values were used.
The PLR values for detecting antibodies against A. phagocytophilum (cut-off values of 1/10 and 1/20) and L. infantum (cut-off value of 1/10) were above 10. PLR value could not be calculated in in all the other cases that specificity was 100%, because specificity is the denominator (1-specificity) of the equation. In all these cases, the test performance was good based on PLR values, while the best NLR value was observed for the detection of anti-A. phagocytophilum and anti-L. infantum antibodies (0.25) when the cut-off value was 1/10.
As shown in Table 4, there was an almost perfect agreement between serum and saliva samples for detecting antibodies against A. phagocytophilum and B. burgdorferi (>0.80) with a cut-off value of 1/10. In all the other cases, there was a substantial agreement (0.61–0.80), except for detecting anti-L. infantum antibodies with a 1/40 cut-off value in which the agreement was fair (0.21–0.40).
Table 4.
Agreement between the detection of antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum, in serum and saliva samples, taking the results in serum as a reference.
| Cut-Off | κ Value (95% CI) | |||
|---|---|---|---|---|
| Pathogen | 1/10 | 1/20 | 1/40 | |
| A. phagocytophilum | 0.829 (0.735–0.923) |
0.744 (0.630–0.859) |
0.642 (0.507–0.777) |
|
| B. burgdorferi | 0.805 (0.707–0.903) |
0.756 (0.646–0.865) |
0.686 (0.562–0.809) |
|
| L. infantum | 0.747 (0.408–1.000) |
0.664 (0.226–1.000) |
0.397 (−0.145–0.939) |
|
The number of true and false positive and negative samples for detecting antibodies against the three pathogens in serum and saliva, with the results in serum taken as a reference, is presented in Table 5. Using lower cut-off values resulted in an increase in true positive samples for detecting anti-A. phagocytophilum and anti-B. burgdorferi antibodies and a decrease in false negatives. False positive results were recorded for the anti-A. phagocytophilum and anti-L. infantum antibodies, with cut-off values of 1/10 and 1/20, and 1/10, respectively.
Table 5.
Number of true and false positive and negative samples for detecting antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum in saliva samples, using different cut-off values and taking the results in serum as a reference.
| A. phagocytophilum | B. burgdorferi | L. infantum | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cut-Off Value | 1/10 | 1/20 | 1/40 | 1/10 | 1/20 | 1/40 | 1/10 | 1/20 | 1/40 |
| TP | 34 | 29 | 23 | 34 | 31 | 27 | 3 | 2 | 1 |
| FP | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| TN | 271 | 271 | 272 | 269 | 269 | 269 | 312 | 313 | 313 |
| FN | 11 | 16 | 22 | 14 | 17 | 21 | 1 | 2 | 3 |
TP: true positive; FP: false positive; TN: true negative; FN: false negative.
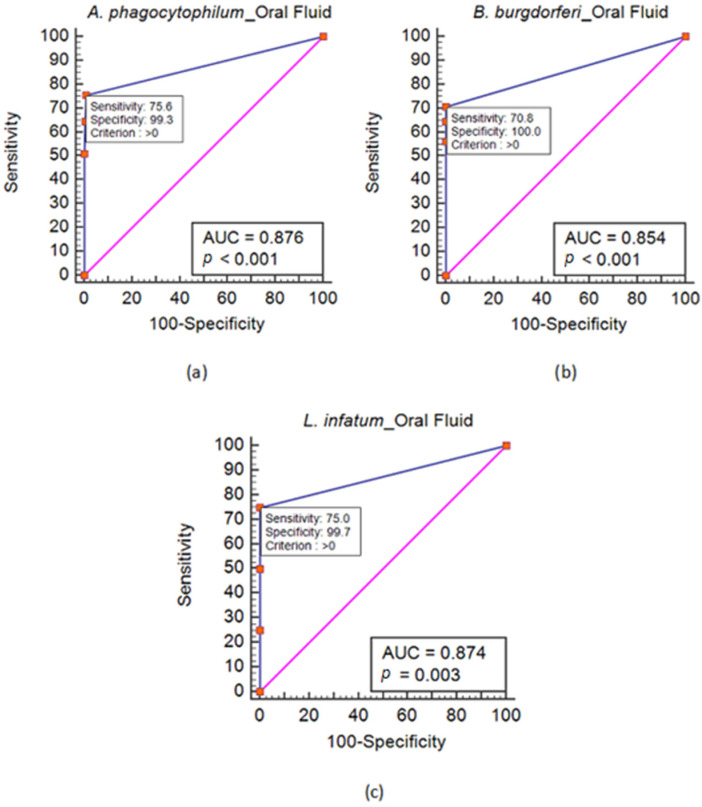
Figure 1 shows the ROC curve analysis for detecting antibodies against these three pathogens in saliva. The ROC analysis revealed that the cut-off value closest to the upper-left corner of the AUC plot corresponded to the optimal criterion (>0). The sensitivity and specificity of these spots indicate that the best cut-off value was 1/10. Moreover, the accuracy interpreted by the AUC values was categorized as moderate (0.7 < AUC ≤ 0.9).
Figure 1.
Receiver operating characteristic (ROC) curve analysis for detecting antibodies against A. phagocytophilum (a), B. burgdorferi (b), and L. infantum (c) in saliva.
4. Discussion
In this study, we showed that IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum circulate in detectable levels in equine saliva samples. We also determined the diagnostic accuracy of this alternative sample type compared to serum, using IFAT. Based on the serological investigation, horses in Greece are exposed to A. phagocytophilum, B. burgdorferi, and L. infantum. Co-exposure was observed in six horses, and it only concerned A. phagocytophilum and B. burgdorferi. Senior horses (≥12 years of age) presented higher seropositivity rates against A. phagocytophilum and B. burgdorferi separately as well as in combination compared to the other two age groups. We herein provide, for the first time, seropositivity data against A. phagocytophilum and B. burgdorferi in horses in Greece, and we also report updated data on the seroprevalence of L. infantum in this animal species from different regions of the country.
The ROC analysis revealed that the 1/10 cut-off value was optimal for detecting antibodies against all the examined pathogens, taking the results in serum as a reference. Moreover, we chose to evaluate the performance of the saliva samples in detecting antibodies by measuring the PLR and NLR values. These values are independent of the disease prevalence, and they do not vary among the different populations and settings [41]. According to the PLR values for the 1/10 cut-off value, the detection of anti-A. phagocytophilum, anti-B. burgdorferi, and anti-L. infantum antibodies using IFAT in saliva samples had a good test performance compared to serum. Antibodies against the abovementioned pathogens will likely be detected in saliva samples in seropositive animals. The best (lowest) NLR values were observed for detecting anti-A. phagocytophilum and anti-L. infantum antibodies. However, the NLR values were, in all cases, indicative of a moderate power to identify seronegative animals when saliva samples were negative. Thus, a negative saliva sample cannot rule out seropositivity. Overall, the two sample types had an almost perfect agreement in detecting antibodies against A. phagocytophilum and B. burgdorferi, while there was a substantial agreement in detecting anti-L. infantum antibodies. The sensitivity values were higher for detecting antibodies against A. phagocytophilum and L. infantum than anti-B. burgdorferi antibodies. Although the sensitivity was moderate in all cases, the specificity was perfect for detecting anti-B. burgdorferi antibodies, and almost perfect for detecting antibodies against the other two pathogens.
In cats, saliva samples were less sensitive than serum for detecting anti-B. henselae antibodies when using IFAT. In that case, saliva was considered of limited utility for epidemiological or diagnostic purposes since oral fluid antibodies were detected more often in cats with high B. henselae serum antibody titers [36]. The use of saliva for the detection of anti-Mycobacterium bovis IgG antibodies by dual path platform (DPP) in experimentally infected cattle also had a low diagnostic value due to relatively low specific IgG levels (100–300 times lower than paired serum samples) and variable detection rates [47]. Additionally, anti-Salmonella antibodies were not detected in oral fluid samples from pigs, while the paired serum samples were positive. In the same study, the detection of specific antibodies against the hepatitis E virus showed poor agreement with serum samples at the first sampling and significant agreement in the second sampling [48].
On the contrary, a modified protocol of a commercial ELISA for detecting anti-Salmonella IgG antibodies in pig saliva samples showed a moderate correlation with the application of the assay in paired serum samples. Although antibody levels in pig sera were consistently higher, anti-Salmonella IgG antibodies were detected in all the matching saliva samples. Thus, the authors suggested that individual saliva samples can represent a suitable alternative to blood samples for detecting anti-Salmonella antibodies at an individual pig level [49]. Seemingly, when saliva samples were used to detect IgG antibodies against the FIV using IFAT and Western blot, they successfully identified the seropositive cats. However, it is worth mentioning that higher ratios of salivary IgG compared to serum IgG were found in both FIV seronegative and seropositive cats with oral lesions compared to cats without oral lesions, suggesting a possible link between positive oral fluid samples and the presence of oral inflammatory lesions [50].
Similarly, in a mixed population of vaccinated and unvaccinated cats against FIV, commercial rapid tests, based on immunochromatography, accurately diagnosed FIV infection using saliva, irrespective of FIV vaccination history [37]. The detection of antibodies against L. infantum in canine oral transudate using ELISA showed almost perfect to moderate agreement with serum samples. The authors suggested that this sample type could be used for sick dogs with high antibody titers, but the results are expected to be less optimal in apparently healthy dogs [35]. Likewise, IgG2 antibodies against L. infantum were highly correlated between saliva and serum samples using time-resolved immunofluorometric assays, and the reduction in antibody levels was related to clinical improvement [51].
In another study in horses, Lightbody et al. evaluated the performance of a commercially available test for tapeworm infections based on detecting tapeworm-specific IgG antibodies in saliva. The test showed similar sensitivity to the applied modified fecal egg count analysis when the parasitic load was high (>20 tapeworms). Notably, the assay sensitivity was higher for low parasitic burdens (>one tapeworm), possibly due to the inability of the fecal egg count method to identify immature tapeworms [38]. Likewise, in an earlier study, the saliva test was as accurate as ELISA for diagnosing low parasitic load (>one tapeworm) [52]. The authors suggested that this easy-to-use test could be widely deployed for regular tapeworm testing to reduce the frequency of praziquantel and pyrantel pamoate administration in horses [38,52].
The presence of the different antibody classes in oral fluid is not surprising. Oral fluid comprises saliva and serum transudates from capillaries in the oral mucosa and gingival tissues. Blood components (e.g., immunoglobulins) access the mucosal surface through the junction between the teeth and the mucosa. Immunoglobulins in oral fluid originate from the passage of the systemic immune system’s serum antibodies (mainly IgG, but also IgA and IgM) [53,54,55]. However, they are also produced locally (mainly IgA but also IgG and IgM at low levels). Local production is based on the blood-derived plasma cells of the secretory immune system in the major salivary glands and duct-associated lymphoid tissue of minor salivary glands distributed around the oral cavity [32,55].
This study examined the oral fluid samples only for IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum. However, previous animal studies have successfully detected IgA and IgM antibodies and showed the diagnostic utility of the different antibody classes. In horses, the researchers in one study evaluated the performance of a self-developed ELISA for detecting specific anti-G. intestinalis L3 IgG, IgM, and IgA antibodies using paired serum and saliva samples [39]. The IgA class—the main immunoglobulin class in mucosal secretions—showed the highest reaction intensity. The salivary IgG and the IgA-specific antibody reactivity was significantly higher in moderate and severe infection (>50 larvae) than in healthy horses. On the contrary, a low parasitic burden (10–50 larvae) status could not be differentiated from an infection-free status based on the IgA intensity of reaction. As for the IgM antibodies, the same level of reactivity was seen only in severely infected horses (>200 larvae). Therefore, the authors suggested that IgG and IgA antibody activity in saliva may be used for detecting horses moderately and severely infested with G. intestinalis [39].
Another study demonstrated that the mucosal IgA antibody response arises earlier than the systemic response and suggested that measuring mucosal antibodies in saliva could be applied to identify pigs infected with A. pleuropneumoniae at an early stage of infection [34]. Regarding the detection of T. gondii antibodies in oral fluid pig samples, the IgA class performed better than the IgG class. The authors suggested that this sample type, coupled with the ELISA test, could be successfully applied as a screening method at the farm level. However, its use for determining the serological status in individual animals was not supported by the findings of that study [32]. In other studies in pigs, IgG in oral fluid samples presented better diagnostic performance compared to IgA antibodies for porcine reproductive and respiratory syndrome virus [33], porcine circovirus type 2 [56], classic swine fever virus [57], and Lawsonia intracellularis infections [58]. Similarly, cats with chronic gingivostomatitis had significantly higher salivary IgM and IgG but significantly lower salivary IgA concentrations than healthy cats [59].
Many factors may influence the accuracy of oral fluid or saliva as a diagnostic tool: the targeted pathogen, the stage of infection, the method deployed, the sample collection device, and the age-related decrease in specific antibody levels [29,31,36,39,47,49,60]. In a recent study, the researchers showed that the presence of feed in horse saliva could affect the measurement of selected biomarkers. The type of the collection device (cotton or sponge) could also influence the results obtained. They suggested that clean saliva and the same collection device should ensure consistent measurements [61]. As for the IgG antibody component in oral fluid samples, it has been suggested that dental status did not affect the sensitivity and specificity values of an assay used for detecting IgG antibodies against rubella and hepatitis A viruses in humans [62].
Moreover, other studies have shown that storing oral fluid samples at environmental temperatures does not affect their integrity. When human saliva samples—collected with a specific device—were stored for one month in ambient temperatures in a tropical country, the antibodies against HIV were successfully preserved [30]. Similarly, anti-PRRSV antibodies in pig oral fluid were relatively resistant to degradation over 12 days, and the authors suggested that appropriate specimen-handling protocols, including prompt freezing or refrigeration at 4 °C, would maintain the integrity of anti-PRRSV antibodies in oral fluid samples [63].
In this study, we report serological data for A. phagocytophilum, B. burgdorferi, and L. infantum in horses from different regions in Greece. With regard to A. phagocytophilum, the recorded seroprevalences differ among the countries, ranging from 4% in Switzerland to 72.8% in the Czech Republic [8,10]. Variation in seropositivity rates is apparent in studies conducted in the same country: 11.3–18.0% in France [18,64] and 8.0–16.9% in Italy [65,66]. The seropositivity reported in our study (14.2%) is close to the data reported in other European countries.
Regarding B. burgdorferi, this is the first study to report the exposure of horses in Greece, and the recorded rate was 15.4%. Studies in various countries globally have reported serological evidence of exposure to B. burgdorferi s.l. in horses, ranging from 0% in different regions in Africa [18] to 15.5% in Bulgaria [16], 16.8% in Sweden [67], 18.8% in Romania [14], and 16.1% in Germany [68], and even higher rates of 29% in Denmark [69], 33% in southwest Virginia [70], 45.1% in the northeastern United States [71], 47.8% in Slovakia [72], and 48% in France [18]. Limited data exist on the occurrence of B. burgdorferi in Greece and no human cases have been recorded. The studies conducted up to now showed a low seroprevalence of 3.3% in humans [73] and 0.1–2.2% in dogs [74,75]. Recently, a study showed that sheep are also exposed to B. burgdorferi in Greece and provided evidence of co-exposure with A. phagocytophilum [76].
The co-exposure observed in 1.89% of the examined horses was exclusively for A. phagocytophilum and B. burgdorferi, which also share a common vector. While this finding could potentially be attributed to cross-reaction between the two agents in IFAT, the low number of horses that reacted to both agents weakens this hypothesis.
Senior horses presented higher seropositivity rates compared to adult and young horses for A. phagocytophilum and B. burgdorferi as well as for co-exposure to both agents. This finding is not surprising since older horses would have been exposed to vectors and their pathogens for prolonged periods of time compared to young and adult horses.
A lower seropositivity rate was previously reported in the country for L. infantum (0.3%) [22] compared to our findings (1.26%). Similar low seroprevalences have been recorded in other countries, including Israel (1.4%) [23], Portugal (4%), [77] and Italy (6.5%) [78]. However, a recent study in Italy reported a seroprevalence of 13.9% [24], suggesting the heterogeneity of serological findings even in the same country. Moreover, a seroprevalence of 27% was recorded in Brazil for L. infantum [25] and as high as 76.3% in Paraná State, Brazil, for L. (V.) braziliensis [26].
Vector-borne diseases in horses can exact a heavy economic toll, causing substantial losses in veterinary expenses, treatment costs, and reduced performance. Additionally, exposure to these pathogens can impact local economies by affecting tourism and horse-related outdoor activities [79]. Hence, disease prevention measures to collectively minimize the risk of exposure (i.e., the use of effective repellents, grooming practices, and alterations in pasture management) in urban and peri-urban environments could yield substantial long-term savings and prevent potential losses, safeguarding the equine industry’s financial stability. The horses included in this study inhabited regions where environmental factors encourage the proliferation of ticks and sandflies.
Concerning the vector distribution and abundance in Greece, several studies have shown that distinct populations of ticks and sandflies exist throughout the country. A total of 26 hard tick species and subspecies have been identified in animals and humans in Greece including Ixodes ricinus and Rhipicephalus sanguineus infected with A. phagocytophilum and A. platys [80,81,82]. Based on the existing country-wide studies, I. ricinus, the common vector of B. burgdorferi and A. phagocytophilum, is not among the most prevalent tick species in the country, representing 0.07% of the ticks collected from sheep in mainland Greece and the Aegean islands [83], 2.25% from sheep, 10.47% from cattle, 3.65% from goats, and 8.41% from dogs [84] and the 15.63% from goats in northern Greece [81]. However, in two studies conducted in northern Greece, I. ricinus represented 46% [85] and 50.50% [86] of the ticks collected from sheep and goats, respectively.
Similarly, the entomological studies conducted in Greece identified eleven species belonging to the genus Phlebotomus spp. Among them, the proven or suspected vectors for L. infantum—P. perfiliewi, P. tobbi, and P. neglectus—have been repeatedly recorded [87,88,89]. The previous studies reported an infection prevalence of L. infantum in sandflies ranging from 0.41% [88] to 5.4% [90] in Attiki, Central Greece, and as low as 0.12% on the island of Corfu [91]. However, a recent study in two refugee camps in the region of Thessaloniki, in northern Greece, showed an unusually high prevalence of infection in P. perfiliewi, P. tobbi, and P. simici ranging from 43% to 52% [92].
Although data gathering on vectors is not systematic in Greece, the undertaken studies show that ticks can transmit A. phagocytophilum and B. burgdorferi, and sandfly species that are competent vectors of L. infantum are widely distributed throughout the country [80,88]. Conducting further studies on the mainland and islands of Greece would be valuable in determining the level of exposure of different animal species and humans to these pathogens, as well as the rate of infection among vectors.
5. Conclusions
Our study showed that horses in Greece are exposed to A. phagocytophilum, B. burgdorferi, and L. infantum. The IgG antibodies against A. phagocytophilum, B. burgdorferi, and L. infantum circulate in equine saliva at detectable levels. Our findings suggest that when antibodies against the abovementioned pathogens are detected in saliva samples it is nearly certain that the animal is also seropositive. Thus, saliva sampling coupled with IFAT could be successfully applied in large-scale serological studies at the population level as an alternative to serum.
Author Contributions
Conceptualization, L.V.A. and C.N.T.; methodology, E.G.K., P.T. and D.G.; software, E.G.K., P.T.; validation, L.V.A., P.T. and E.G.K.; formal analysis, K.N.A., S.M.P., K.C.G.K. and V.G.P.; investigation, K.N.A., S.M.P., K.C.G.K. and V.G.P.; resources, L.V.A.; data curation, E.G.K., P.T. and C.N.T.; writing—original draft preparation, L.V.A., E.G.K. and C.N.T. writing—review and editing, L.V.A., E.G.K., P.T., D.G., K.N.A., S.M.P., K.C.G.K., V.G.P. and C.N.T. visualization, L.V.A., E.G.K., P.T., D.G., K.N.A., S.M.P., K.C.G.K., V.G.P. and C.N.T.; supervision, L.V.A.; project administration, C.N.T.; funding acquisition, L.V.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
All procedures were performed according to the ethical standards of the Helsinki Declaration of 1975, as revised in 2000, as well as the national law, and after receiving approval from our Institutional Animal Use Ethics Committee (no. 119/14-7-2021).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the further processing required by other studies.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Dominguez M., Münstermann S., de Guindos I., Timoney P. Equine Disease Events Resulting from International Horse Movements: Systematic Review and Lessons Learned. Equine Vet. J. 2016;48:641–653. doi: 10.1111/evj.12523. [DOI] [PubMed] [Google Scholar]
- 2.Lönker N.S., Fechner K., Abd El Wahed A. Horses as a Crucial Part of One Health. Vet. Sci. 2020;7:28. doi: 10.3390/vetsci7010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butler C.M., Houwers D.J., Jongejan F., van der Kolk J.H. Borrelia Burgdorferi Infections with Special Reference to Horses. A Review. Vet. Q. 2005;27:146–156. doi: 10.1080/01652176.2002.9695196. [DOI] [PubMed] [Google Scholar]
- 4.Mhadhbi M., Sassi A. Infection of the Equine Population by Leishmania Parasites. Equine Vet. J. 2020;52:28–33. doi: 10.1111/evj.13178. [DOI] [PubMed] [Google Scholar]
- 5.Swinebroad E.L. Borreliosis in Sport Horse Practice. Vet. Clin. N. Am. Equine Pract. 2018;34:313–343. doi: 10.1016/j.cveq.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 6.Saleem S., Ijaz M., Farooqi S.H., Ghaffar A., Ali A., Iqbal K., Mehmood K., Zhang H. Equine Granulocytic Anaplasmosis 28 Years Later. Microb. Pathog. 2018;119:1–8. doi: 10.1016/j.micpath.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Madigan J.E., Gribble D. Equine Ehrlichiosis in Northern California: 49 Cases (1968–1981) J. Am. Vet. Med. Assoc. 1987;190:445–448. [PubMed] [Google Scholar]
- 8.Springer A., Glass A., Topp A.-K., Strube C. Zoonotic Tick-Borne Pathogens in Temperate and Cold Regions of Europe—A Review on the Prevalence in Domestic Animals. Front. Vet. Sci. 2020;7:604910. doi: 10.3389/fvets.2020.604910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franzén P., Aspan A., Egenvall A., Gunnarsson A., Aberg L., Pringle J. Acute Clinical, Hematologic, Serologic, and Polymerase Chain Reaction Findings in Horses Experimentally Infected with a European Strain of Anaplasma Phagocytophilum. J. Vet. Intern. Med. 2005;19:232–239. doi: 10.1111/j.1939-1676.2005.tb02687.x. [DOI] [PubMed] [Google Scholar]
- 10.Praskova I., Bezdekova B., Zeman P., Jahn P. Seroprevalence of Anaplasma Phagocytophilum in Horses in the Czech Republic. Ticks Tick-Borne Dis. 2011;2:111–115. doi: 10.1016/j.ttbdis.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Zeman P., Jahn P. An Entropy-Optimized Multilocus Approach for Characterizing the Strains of Anaplasma Phagocytophilum Infecting Horses in the Czech Republic. J. Med. Microbiol. 2009;58:423–429. doi: 10.1099/jmm.0.007831-0. [DOI] [PubMed] [Google Scholar]
- 12.James F.M., Engiles J.B., Beech J. Meningitis, Cranial Neuritis, and Radiculoneuritis Associated with Borrelia Burgdorferi Infection in a Horse. J. Am. Vet. Med. Assoc. 2010;237:1180–1185. doi: 10.2460/javma.237.10.1180. [DOI] [PubMed] [Google Scholar]
- 13.Pecoraro H.L., Felippe M.J.B., Miller A.D., Divers T.J., Simpson K.W., Guyer K.M., Duhamel G.E. Neuroborreliosis in a Horse with Common Variable Immunodeficiency. J. Vet. Diagn. Investig. 2019;31:241–245. doi: 10.1177/1040638718824146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bogdan A.M., Ionita M., Mitrea I.L. Serological Evidence of Natural Exposure to Tick-Borne Pathogens in Horses, Romania. Microorganisms. 2021;9:373. doi: 10.3390/microorganisms9020373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsachev I., Baymakova M., Pantchev N. Seroprevalence of Anaplasma Phagocytophilum, Ehrlichia Spp. and Borrelia Burgdorferi Infections in Horses: First Report from Northern Bulgaria—Short Communication. Acta Vet. Hung. 2019;67:197–203. doi: 10.1556/004.2019.021. [DOI] [PubMed] [Google Scholar]
- 16.Tsachev I., Pantchev N., Marutsov P., Petrov V., Gundasheva D., Baymakova M. Serological Evidence of Borrelia Burgdorferi, Anaplasma Phagocytophilum and Ehrlichia Spp. Infections in Horses from Southeastern Bulgaria. Vector-Borne Zoonotic Dis. 2018;18:588–594. doi: 10.1089/vbz.2018.2293. [DOI] [PubMed] [Google Scholar]
- 17.Baneth G. Tick-Borne Infections of Animals and Humans: A Common Ground. Int. J. Parasitol. 2014;44:591–596. doi: 10.1016/j.ijpara.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 18.Maurizi L., Marié J.-L., Aoun O., Courtin C., Gorsane S., Chal D., Davoust B. Seroprevalence Survey of Equine Lyme Borreliosis in France and in Sub-Saharan Africa. Vector-Borne Zoonotic Dis. 2010;10:535–537. doi: 10.1089/vbz.2009.0083. [DOI] [PubMed] [Google Scholar]
- 19.Soares I.R., Silva S.O., Moreira F.M., Prado L.G., Fantini P., Maranhão R.D.P.A., Da Silva Filho J.M., Melo M.N., Palhares M.S. First Evidence of Autochthonous Cases of Leishmania (Leishmania) infantum in Horse (Equus Caballus) in the Americas and Mixed Infection of Leishmania infantum and Leishmania (Viannia) braziliensis. Vet. Parasitol. 2013;197:665–669. doi: 10.1016/j.vetpar.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Müller N., Welle M., Lobsiger L., Stoffel M.H., Boghenbor K.K., Hilbe M., Gottstein B., Frey C.F., Geyer C., Von Bomhard W. Occurrence of Leishmania sp. in Cutaneous Lesions of Horses in Central Europe. Vet. Parasitol. 2009;166:346–351. doi: 10.1016/j.vetpar.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Reuss S.M., Dunbar M.D., Mays M.B.C., Owen J.L., Mallicote M.F., Archer L.L., Wellehan J.F.X. Autochthonous Leishmania siamensis in Horse, Florida, USA. Emerg. Infect. Dis. 2012;18:1545–1546. doi: 10.3201/eid1809.120184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kouam M.K., Diakou A., Kanzoura V., Papadopoulos E., Gajadhar A.A., Theodoropoulos G. A Seroepidemiological Study of Exposure to Toxoplasma, Leishmania, Echinococcus and Trichinella in Equids in Greece and Analysis of Risk Factors. Vet. Parasitol. 2010;170:170–175. doi: 10.1016/j.vetpar.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Aharonson-Raz K., Baneth G., Lopes A.P., Brancal H., Schallig H., Cardoso L., Steinman A. Low Seroprevalence of Leishmania infantum and Toxoplasma gondii in the Horse Population in Israel. Vector-Borne Zoonotic Dis. 2015;15:726–731. doi: 10.1089/vbz.2015.1826. [DOI] [PubMed] [Google Scholar]
- 24.Gazzonis A.L., Bertero F., Moretta I., Morganti G., Mortarino M., Villa L., Zanzani S.A., Morandi B., Rinnovati R., Vitale F., et al. Detecting Antibodies to Leishmania Infantum in Horses from Areas with Different Epizooticity Levels of Canine Leishmaniosis and a Retrospective Revision of Italian Data. Parasit. Vectors. 2020;13:530. doi: 10.1186/s13071-020-04385-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biral N.V., Azevedo Santos H., Senne N.A., Paulino P.G., Camilo T.A., Tassinari W.D.S., Silva V.L., Santos F.N., Angelo I.D.C. A Cross-Sectional Study of Leishmania spp. in Draft Horses from the Distrito Federal, Brazil: Seroprevalence, Spatial Distribution, and Associated Factors. Prev. Vet. Med. 2021;195:105467. doi: 10.1016/j.prevetmed.2021.105467. [DOI] [PubMed] [Google Scholar]
- 26.Vedovello Filho D., Jorge F.A., Lonardoni M.V.C., Teodoro U., Silveira T.G.V. American Cutaneous Leishmaniasis in Horses from Endemic Areas in the North-Central Mesoregion of Paraná State, Brazil. Zoonoses Public Health. 2008;55:149–155. doi: 10.1111/j.1863-2378.2008.01106.x. [DOI] [PubMed] [Google Scholar]
- 27.Koehler K., Stechele M., Hetzel U., Domingo M., Schönian G., Zahner H., Burkhardt E. Cutaneous Leishmaniosis in a Horse in Southern Germany Caused by Leishmania Infantum. Vet. Parasitol. 2002;109:9–17. doi: 10.1016/S0304-4017(02)00246-7. [DOI] [PubMed] [Google Scholar]
- 28.Solano-Gallego L., Fernández-Bellon H., Serra P., Gállego M., Ramis A., Fondevila D., Ferrer L. Cutaneous Leishmaniosis in Three Horses in Spain. Equine Vet. J. 2010;35:320–323. doi: 10.2746/042516403776148336. [DOI] [PubMed] [Google Scholar]
- 29.Nokes D.J., Enquselassie F., Nigatu W., Vyse A.J., Cohen B.J., Brown D.W., Cutts F.T. Has Oral Fluid the Potential to Replace Serum for the Evaluation of Population Immunity Levels? A Study of Measles, Rubella and Hepatitis B in Rural Ethiopia. Bull. World Health Organ. 2001;79:588–595. [PMC free article] [PubMed] [Google Scholar]
- 30.Thwe M. Brief Report. Stability of Saliva for Measuring HIV in the Tropics. J. Trop. Pediatr. 1999;45:296–299. doi: 10.1093/tropej/45.5.296. [DOI] [PubMed] [Google Scholar]
- 31.Nokes D.J., Enquselassie F., Vyse A., Nigatu W., Cutts F.T., Brown D.W. An Evaluation of Oral-Fluid Collection Devices for the Determination of Rubella Antibody Status in a Rural Ethiopian Community. Trans. R. Soc. Trop. Med. Hyg. 1998;92:679–685. doi: 10.1016/S0035-9203(98)90811-2. [DOI] [PubMed] [Google Scholar]
- 32.Campero L.M., Schott F., Gottstein B., Deplazes P., Sidler X., Basso W. Detection of Antibodies to Toxoplasma Gondii in Oral Fluid from Pigs. Int. J. Parasitol. 2020;50:349–355. doi: 10.1016/j.ijpara.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Kittawornrat A., Prickett J., Wang C., Olsen C., Irwin C., Panyasing Y., Ballagi A., Rice A., Main R., Johnson J., et al. Detection of Porcine Reproductive and Respiratory Syndrome Virus (PRRSV) Antibodies in Oral Fluid Specimens Using a Commercial PRRSV Serum Antibody Enzyme-Linked Immunosorbent Assay. J. Vet. Diagn. Investig. 2012;24:262–269. doi: 10.1177/1040638711435679. [DOI] [PubMed] [Google Scholar]
- 34.Loftager M.K., Eriksen L., Nielsen R. Antibodies against Actinobacillus Pleuropneumoniae Serotype 2 in Mucosal Secretions and Sera of Infected Pigs as Demonstrated by an Enzyme-Linked Immunosorbent Assay. Res. Vet. Sci. 1993;54:57–62. doi: 10.1016/0034-5288(93)90011-4. [DOI] [PubMed] [Google Scholar]
- 35.Baxarias M., Viñals J., Álvarez-Fernández A., Alcover M.M., Solano-Gallego L. Detection of Specific Antibodies against Leishmania Infantum in Canine Serum and Oral Transudate Using an In-House ELISA. Parasit. Vectors. 2022;15:164. doi: 10.1186/s13071-022-05246-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Álvarez-Fernández A., Baxarias M., Prandi D., Breitschwerdt E.B., Solano-Gallego L. Bartonella Henselae Antibodies in Serum and Oral Fluid Specimens from Cats. Pathogens. 2021;10:329. doi: 10.3390/pathogens10030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Westman M.E., Malik R., Hall E., Norris J.M. Diagnosing Feline Immunodeficiency Virus (FIV) Infection in FIV-Vaccinated and FIV-Unvaccinated Cats Using Saliva. Comp. Immunol. Microbiol. Infect. Dis. 2016;46:66–72. doi: 10.1016/j.cimid.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 38.Lightbody K.L., Matthews J.B., Kemp-Symonds J.G., Lambert P.A., Austin C.J. Use of a Saliva-Based Diagnostic Test to Identify Tapeworm Infection in Horses in the UK. Equine Vet. J. 2018;50:213–219. doi: 10.1111/evj.12742. [DOI] [PubMed] [Google Scholar]
- 39.Pawlas-Opiela M., Jawor P., Galli J., Zak-Bochenek A., Gorczykowski M., Galli J., Sołtysiak Z., Stefaniak T. The Relationship between the Intensity of Gasterophilus Intestinalis Larvae Infection and the Serum and Salivary Humoral Immune Response in Horses. Sci. Rep. 2022;12:17573. doi: 10.1038/s41598-022-21482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peeters M., Sulon J., Beckers J.-F., Ledoux D., Vandenheede M. Comparison between Blood Serum and Salivary Cortisol Concentrations in Horses Using an Adrenocorticotropic Hormone Challenge: Serum and Salivary Cortisol Concentrations Using an ACTH Challenge. Equine Vet. J. 2011;43:487–493. doi: 10.1111/j.2042-3306.2010.00294.x. [DOI] [PubMed] [Google Scholar]
- 41.Gardner I.A., Greiner M. Receiver-Operating Characteristic Curves and Likelihood Ratios: Improvements over Traditional Methods for the Evaluation and Application of Veterinary Clinical Pathology Tests. Vet. Clin. Pathol. 2006;35:8–17. doi: 10.1111/j.1939-165X.2006.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 42.McHugh M.L. Interrater Reliability: The Kappa Statistic. Biochem. Medica. 2012;22:276–282. doi: 10.11613/BM.2012.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Watson P.F., Petrie A. Method Agreement Analysis: A Review of Correct Methodology. Theriogenology. 2010;73:1167–1179. doi: 10.1016/j.theriogenology.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 44.Swets J.A. Measuring the Accuracy of Diagnostic Systems. Science. 1988;240:1285–1293. doi: 10.1126/science.3287615. [DOI] [PubMed] [Google Scholar]
- 45.Campbell I. Chi-Squared and Fisher–Irwin Tests of Two-by-Two Tables with Small Sample Recommendations. Stat. Med. 2007;26:3661–3675. doi: 10.1002/sim.2832. [DOI] [PubMed] [Google Scholar]
- 46.Richardson J.T.E. The Analysis of 2 × 2 Contingency Tables-Yet Again. Stat. Med. 2011;30:890. doi: 10.1002/sim.4116. [DOI] [PubMed] [Google Scholar]
- 47.Lyashchenko K.P., Sikar-Gang A., Sridhara A.A., Johnathan-Lee A., Elahi R., Greenwald R., Lambotte P., Esfandiari J., Roos E.O., Kerr T.J., et al. Use of Blood Matrices and Alternative Biological Fluids for Antibody Detection in Animal Tuberculosis. Vet. Immunol. Immunopathol. 2021;239:110303. doi: 10.1016/j.vetimm.2021.110303. [DOI] [PubMed] [Google Scholar]
- 48.Schott F., Hoffmann K., Sarno E., Bangerter P.D., Stephan R., Overesch G., Haessig M., Sidler X., Graage R. Evaluation of Oral Fluids for Surveillance of Foodborne and Zoonotic Pathogens in Pig Farms. J. Vet. Diagn. Investig. 2021;33:655–663. doi: 10.1177/10406387211021599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.De Lucia A., Cawthraw S., Davies R., Smith R.P., Bianco C., Ostanello F., Martelli F. Correlation of Anti-Salmonella Antibodies between Serum and Saliva Samples Collected from Finisher Pigs. Front. Vet. Sci. 2020;6:489. doi: 10.3389/fvets.2019.00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Poli A., Giannelli C., Pistello M., Zaccaro L., Pieracci D., Bendinelli M., Malvaldi G. Detection of Salivary Antibodies in Cats Infected with Feline Immunodeficiency Virus. J. Clin. Microbiol. 1992;30:2038–2041. doi: 10.1128/jcm.30.8.2038-2041.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cantos-Barreda A., Escribano D., Cerón J.J., Tecles F., Bernal L.J., Martínez-Subiela S. Changes in the Concentration of Anti-Leishmania Antibodies in Saliva of Dogs with Clinical Leishmaniosis after Short-Term Treatment. Vet. Parasitol. 2018;254:135–141. doi: 10.1016/j.vetpar.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 52.Lightbody K.L., Davis P.J., Austin C.J. Validation of a Novel Saliva-Based ELISA Test for Diagnosing Tapeworm Burden in Horses. Vet. Clin. Pathol. 2016;45:335–346. doi: 10.1111/vcp.12364. [DOI] [PubMed] [Google Scholar]
- 53.Brandtzaeg P. Secretory Immunity with Special Reference to the Oral Cavity. J. Oral Microbiol. 2013;5:20401. doi: 10.3402/jom.v5i0.20401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Challacombe S.J., Shirlaw P.J. 49—Immunology of Diseases of the Oral Cavity. In: Ogra P.L., Mestecky J., Lamm M.E., Strober W., McGhee J.R., Bienenstock J., editors. Handbook of Mucosal Immunology. Academic Press; Boston, UK: 1994. pp. 607–624. [Google Scholar]
- 55.Prickett J.R., Zimmerman J.J. The Development of Oral Fluid-Based Diagnostics and Applications in Veterinary Medicine. Anim. Health Res. Rev. 2010;11:207–216. doi: 10.1017/S1466252310000010. [DOI] [PubMed] [Google Scholar]
- 56.Prickett J.R., Johnson J., Murtaugh M.P., Puvanendiran S., Wang C., Zimmerman J.J., Opriessnig T. Prolonged Detection of PCV2 and Anti-PCV2 Antibody in Oral Fluids Following Experimental Inoculation. Transbound. Emerg. Dis. 2011;58:121–127. doi: 10.1111/j.1865-1682.2010.01189.x. [DOI] [PubMed] [Google Scholar]
- 57.Panyasing Y., Thanawongnuwech R., Ji J., Giménez-Lirola L., Zimmerman J. Detection of Classical Swine Fever Virus (CSFV) E2 and Erns Antibody (IgG, IgA) in Oral Fluid Specimens from Inoculated (ALD Strain) or Vaccinated (LOM Strain) Pigs. Vet. Microbiol. 2018;224:70–77. doi: 10.1016/j.vetmic.2018.08.024. [DOI] [PubMed] [Google Scholar]
- 58.Barrera-Zarate J.A., Andrade M.R., Pereira C.E.R., Vasconcellos A., Wagatsuma M.M., Sato J.P.H., Daniel A.G.S., Rezende L.A., Otoni L.A.V., Laub R.P., et al. Oral Fluid for Detection of Exposure to Lawsonia Intracellularis in Naturally Infected Pigs. Vet. J. 2019;244:34–36. doi: 10.1016/j.tvjl.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 59.Harley R., Gruffydd-Jones T.J., Day M.J. Salivary and Serum Immunoglobulin Levels in Cats with Chronic Gingivostomatitis. Vet. Rec. 2003;152:125–129. doi: 10.1136/vr.152.5.125. [DOI] [PubMed] [Google Scholar]
- 60.Nokes D.J., Nigatu W., Abebe A., Messele T., Dejene A., Enquselassie F., Vyse A., Brown D., Cutts F.T. A Comparison of Oral Fluid and Serum for the Detection of Rubella-Specific Antibodies in a Community Study in Addis Ababa, Ethiopia. Trop. Med. Int. Health. 1998;3:258–267. doi: 10.1046/j.1365-3156.1998.00227.x. [DOI] [PubMed] [Google Scholar]
- 61.Contreras-Aguilar M.D., Hevia M.L., Escribano D., Lamy E., Tecles F., Cerón J.J. Effect of Food Contamination and Collection Material in the Measurement of Biomarkers in Saliva of Horses. Res. Vet. Sci. 2020;129:90–95. doi: 10.1016/j.rvsc.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 62.Bagg J., Perry K.R., Parry J.V., Mortimer P.P., Peters T.J. The Influence of Dental Status on the Detection of IgG Class Anti-Viral Antibodies in Human Saliva. Arch. Oral Biol. 1991;36:221–226. doi: 10.1016/0003-9969(91)90089-D. [DOI] [PubMed] [Google Scholar]
- 63.Prickett J.R. Stability of Porcine Reproductive and Respiratory Syndrome Virus and Antibody in Swine Oral Fluid. J. Swine Health Prod. 2010;18:187–195. [Google Scholar]
- 64.Leblond A., Pradier S., Pitel P.H., Fortier G., Boireau P., Chadoeuf J., Sabatier P. Investigación Epidemiológica Sobre La Anaplasmosis Equina (Anaplasma phagocytophilum) En El Sur de Francia: -EN- An Epidemiological Survey of Equine Anaplasmosis (Anaplasma phagocytophilum) in Southern France -FR- Enquête Épidémiologique Sur l’anaplasmose Équine (Anaplasma phagocytophilum) Dans Le Sud de La France -ES- Rev. Sci. Tech. OIE. 2005;24:899–908. doi: 10.20506/rst.24.3.1612. [DOI] [PubMed] [Google Scholar]
- 65.Torina A., Alongi A., Naranjo V., Scimeca S., Nicosia S., Di Marco V., Caracappa S., Kocan K.M., De La Fuente J. Characterization of Anaplasma Infections in Sicily, Italy. Ann. N. Y. Acad. Sci. 2008;1149:90–93. doi: 10.1196/annals.1428.065. [DOI] [PubMed] [Google Scholar]
- 66.Ebani V., Cerri D., Fratini F., Ampola M., Andreani E. Seroprevalence of Anaplasma Phagocytophilum in Domestic and Wild Animals from Central Italy. New Microbiol. 2008;31:371–375. [PubMed] [Google Scholar]
- 67.Egenvall A., Franzén P., Gunnarsson A., Engvall E.O., Vågsholm I., Wikström U.B., Artursson K. Cross-Sectional Study of the Seroprevalence to Borrelia Burgdorferi Sensu Lato and Granulocytic Ehrlichia Spp. and Demographic, Clinical and Tick-Exposure Factors in Swedish Horses. Prev. Vet. Med. 2001;49:191–208. doi: 10.1016/S0167-5877(01)00187-8. [DOI] [PubMed] [Google Scholar]
- 68.Käsbohrer A., Schönberg A. [Serologic studies of the occurrence of Borrelia burgdorferi in domestic animals in Berlin (West)] Berl. Munch. Tierarztl. Wochenschr. 1990;103:374–378. [PubMed] [Google Scholar]
- 69.Hansen M.G.B., Christoffersen M., Thuesen L.R., Petersen M.R., Bojesen A.M. Seroprevalence of Borrelia Burgdorferi Sensu Lato and Anaplasma Phagocytophilum in Danish Horses. Acta Vet. Scand. 2010;52:3. doi: 10.1186/1751-0147-52-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Funk R.A., Pleasant R.S., Witonsky S.G., Reeder D.S., Werre S.R., Hodgson D.R. Seroprevalence of Borrelia Burgdorferi in Horses Presented for Coggins Testing in Southwest Virginia and Change in Positive Test Results Approximately 1 Year Later. J. Vet. Intern. Med. 2016;30:1300–1304. doi: 10.1111/jvim.13973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Magnarelli L.A., Ijdo J.W., Van Andel A.E., Wu C., Padula S.J., Fikrig E. Serologic Confirmation of Ehrlichia Equi and Borrelia Burgdorferi Infections in Horses from the Northeastern United States. J. Am. Vet. Med. Assoc. 2000;217:1045–1050. doi: 10.2460/javma.2000.217.1045. [DOI] [PubMed] [Google Scholar]
- 72.Stefancikova A., Petko B., Nadzamova D., Stepanova G., Szestakova E., Skardova I., Leinstein R. Prevalence of Antibodies to Borrelia Burgdorferi in Horses of East Slovakia. Vet. Med.—UZPI Czech Repub. 2000;45:227–231. [Google Scholar]
- 73.Stamouli M., Totos G., Braun H.B., Michel G., Gizaris V. Very Low Seroprevalence of Lyme Borreliosis in Young Greek Males. Eur. J. Epidemiol. 2000;16:495–496. doi: 10.1023/A:1007657430880. [DOI] [PubMed] [Google Scholar]
- 74.Angelou A., Gelasakis A.I., Verde N., Pantchev N., Schaper R., Chandrashekar R., Papadopoulos E. Prevalence and Risk Factors for Selected Canine Vector-Borne Diseases in Greece. Parasit. Vectors. 2019;12:283. doi: 10.1186/s13071-019-3543-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Athanasiou L.V., Kontos V.I., Kritsepi Konstantinou M., Polizopoulou Z.S., Rousou X.A., Christodoulopoulos G. Cross-Sectional Serosurvey and Factors Associated with Exposure of Dogs to Vector-Borne Pathogens in Greece. Vector-Borne Zoonotic Dis. 2019;19:923–928. doi: 10.1089/vbz.2019.2471. [DOI] [PubMed] [Google Scholar]
- 76.Athanasiou L.V., Tsokana C.N., Gougoulis D.A., Tzivara A.H., Dedousi A., Katsoulos P.D. Natural Co-Exposure to Borrelia Burgdorferi s.l. and Anaplasma Phagocytophilum: Unraveling the Hematological Profile in Sheep. Life. 2023;13:469. doi: 10.3390/life13020469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lopes A.P., Sousa S., Dubey J., Ribeiro A.J., Silvestre R., Cotovio M., Schallig H.D., Cardoso L., Cordeiro-da-Silva A. Prevalence of Antibodies to Leishmania Infantum and Toxoplasma Gondii in Horses from the North of Portugal. Parasit. Vectors. 2013;6:178. doi: 10.1186/1756-3305-6-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sgorbini M., Bonelli F., Pizzolli I., Tognetti R., Corazza M. Seroprevalence of Leishmania Sp. Infection in Healthy Horses Housed in Endemic Areas in Tuscany. J. Equine Vet. Sci. 2014;34:572–574. doi: 10.1016/j.jevs.2013.09.009. [DOI] [Google Scholar]
- 79.Costa S.C.L., De Souza Freitas J., Carvalho F.S., Pereira M.J.S., Cordeiro M.D., Da Fonseca A.H., Gomes Jusi M.M., Machado R.Z., Munhoz A.D. Frequency and Factors Associated of Potential Zoonotic Pathogens (Borrelia spp., Rickettsia spp., Leishmania spp., and Anaplasma phagocytophilum) in Equids in the State of Bahia, Brazil. Parasit. Vectors. 2021;14:275. doi: 10.1186/s13071-021-04777-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Efstratiou A., Karanis G., Karanis P. Tick-Borne Pathogens and Diseases in Greece. Microorganisms. 2021;9:1732. doi: 10.3390/microorganisms9081732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Papa A., Tsioka K., Kontana A., Papadopoulos C., Giadinis N. Bacterial Pathogens and Endosymbionts in Ticks. Ticks Tick-Borne Dis. 2017;8:31–35. doi: 10.1016/j.ttbdis.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 82.Latrofa M.S., Angelou A., Giannelli A., Annoscia G., Ravagnan S., Dantas-Torres F., Capelli G., Halos L., Beugnet F., Papadopoulos E., et al. Ticks and Associated Pathogens in Dogs from Greece. Parasit. Vectors. 2017;10:301. doi: 10.1186/s13071-017-2225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chaligiannis I., Musella V., Rinaldi L., Cringoli G., De La Fuente J., Papa A., Sotiraki S. Species Diversity and Spatial Distribution of Ixodid Ticks on Small Ruminants in Greece. Parasitol. Res. 2016;115:4673–4680. doi: 10.1007/s00436-016-5259-z. [DOI] [PubMed] [Google Scholar]
- 84.Papadopoulos B., Morel P.C., Aeschlimann A. Ticks of Domestic Animals in the Macedonia Region of Greece. Vet. Parasitol. 1996;63:25–40. doi: 10.1016/0304-4017(95)00877-2. [DOI] [PubMed] [Google Scholar]
- 85.Pavlidou V., Gerou S., Diza E., Antoniadis A., Papa A. Genetic Study of the Distribution of Greek Goat Encephalitis Virus in Greece. Vector-Borne Zoonotic Dis. 2008;8:351–354. doi: 10.1089/vbz.2007.0215. [DOI] [PubMed] [Google Scholar]
- 86.Kachrimanidou M., Souliou E., Pavlidou V., Antoniadis A., Papa A. First Detection of Rickettsia Slovaca in Greece. Exp. Appl. Acarol. 2010;50:93–96. doi: 10.1007/s10493-009-9283-x. [DOI] [PubMed] [Google Scholar]
- 87.Ivović V., Patakakis M., Tselentis Y., Chaniotis B. Faunistic Study of Sandflies in Greece. Med. Vet. Entomol. 2007;21:121–124. doi: 10.1111/j.1365-2915.2006.00649.x. [DOI] [PubMed] [Google Scholar]
- 88.Boutsini S., Athanasiou L.V., Spanakos G., Ntousi D., Dotsika E., Bisia M., Papadopoulos E. Phlebotomine Sandflies and Factors Associated with Their Abundance in the Leishmaniasis Endemic Area of Attiki, Greece. Parasitol. Res. 2018;117:107–113. doi: 10.1007/s00436-017-5675-8. [DOI] [PubMed] [Google Scholar]
- 89.Xanthopoulou K., Anagnostou V., Ivovic V., Djurkovic-Djakovic O., Rogozi E., Sotiraki S., Papa A. Distribution of Sandflies (Diptera, Psychodidae) in Two Ionian Islands and Northern Greece. Vector-Borne Zoonotic Dis. 2011;11:1591–1594. doi: 10.1089/vbz.2011.0750. [DOI] [PubMed] [Google Scholar]
- 90.Aransay A.M., Scoulica E., Chaniotis B., Tselentis Y. Typing of Sandflies from Greece and Cyprus by DNA Polymorphism of 18S RRNA Gene. Insect Mol. Biol. 1999;8:179–184. doi: 10.1046/j.1365-2583.1999.820179.x. [DOI] [PubMed] [Google Scholar]
- 91.Léger N., Gramiccia M., Gradoni L., Madulo-Leblond G., Pesson B., Ferté H., Boulanger N., Killick-Kendrick R., Killick-Kendrick M. Isolation and Typing of Leishmania Infantum from Phlebotomus Neglectus on the Island of Corfu, Greece. Trans. R. Soc. Trop. Med. Hyg. 1988;82:419–420. doi: 10.1016/0035-9203(88)90145-9. [DOI] [PubMed] [Google Scholar]
- 92.Fotakis E.A., Giantsis I.A., Avgerinou A., Kourtidis S., Agathaggelidou E., Kapoula C., Dadakou G., Vontas J., Chaskopoulou A. Identification of Leishmania Species in Naturally Infected Sand Flies from Refugee Camps, Greece. Emerg. Infect. Dis. J. 2019;25:2. doi: 10.3201/eid2502.181359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the further processing required by other studies.